Abstract
Oteseconazole (Vivjoa®), an orally administered azole antifungal, is a valuable, efficacious, and well tolerated treatment option for reducing the incidence of vulvovaginal candidiasis (VVC) recurrence in females with a history of recurrent VVC (RVVC) who are not of reproductive potential. It is the first drug to be approved in the USA for this indication. In phase 3 clinical trials in patients with RVVC, oteseconazole significantly reduced the incidence of VVC recurrence compared with placebo and continued to prevent VVC recurrence for over 36 weeks after the final dose of the drug. Oteseconazole was non-inferior to fluconazole for resolving acute VVC. Additionally, it has a favorable pharmacokinetic profile, has activity against fluconazole-resistant Candida strains, and is generally well tolerated in patients with RVVC.
Plain Language Summary
Recurrent vulvovaginal candidiasis (RVVC), commonly known as chronic vaginal yeast infection, causes physical discomfort and psychological distress. Current recommended treatments for RVVC, including azole antifungals (e.g., fluconazole), fail to prevent recurrence in about half of patients. Oteseconazole (Vivjoa®) is the first drug to gain approval for the treatment of RVVC in the USA after it significantly reduced the incidence of vulvovaginal candidiasis (VVC) recurrence in patients compared with placebo in pivotal phase 3 trials. Oteseconazole reduces recurrence for over 36 weeks after the final dose of the drug, has activity against Candida strains that are resistant to azole antifungals, and is generally well tolerated. Thus, oteseconazole is a valuable addition to the drugs available to treat RVVC.
Similar content being viewed by others
References
Nyirjesy P, Brookhart C, Lazenby G, et al. Vulvovaginal candidiasis: a review of the evidence for the 2021 Centers for Disease Control and Prevention of Sexually Transmitted Infections treatment guidelines. Clin Infect Dis. 2022;74(Suppl. 2):S162–8.
Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62(4):e1-50.
US Food and Drug Administration. DIFLUCAN® (fluconazole tablets) for oral use: US prescribing information. 2022. https://www.fda.gov/. Accessed 14 June 2023.
Berkow EL, Lockhart SR. Fluconazole resistance in Candida species: a current perspective. Infect Drug Resist. 2017;10:237–45.
Adis Medical Writers. Long-term use of systemic azole antifungals can result in hepatotoxicity and other serious adverse effects. Drugs Ther Perspect. 2019;36:112–5.
Mycovia Pharmaceuticals Inc. VIVJOA® (oteseconazole) capsules, for oral use: US prescribing information. 2022. https://www.fda.gov/. Accessed 14 June 2023.
US Food and Drug Administration. BREXAFEMME® (ibrexafungerp tablets), for oral use. 2022. https://www.fda.gov/. Accessed 14 June 2023.
Hoy SM. Oteseconazole: first approval. Drugs. 2022;82(9):1017–23.
Wiederhold NP. Pharmacodynamics, mechanisms of action and resistance, and spectrum of activity of new antifungal agents. J Fungi. 2022;8(857):1–20.
Lv QZ, Yan L, Jiang YY. The synthesis, regulation, and functions of sterols in Candida albicans: well-known but still lots to learn. Virulence. 2016;7(6):649–59.
Warrilow AG, Hull CM, Parker JE, et al. The clinical candidate VT-1161 is a highly potent inhibitor of Candida albicans CYP51 but fails to bind the human enzyme. Antimicrob Agents Chemother. 2014;58(12):7121–7.
Garvey EP, Hoekstra WJ, Schotzinger RJ, et al. Efficacy of the clinical agent VT-1161 against fluconazole-sensitive and -resistant Candida albicans in a murine model of vaginal candidiasis. Antimicrob Agents Chemother. 2015;59(9):5567–73.
Schell WA, Jones AM, Garvey EP, et al. Fungal CYP51 inhibitors VT-1161 and VT-1129 exhibit strong in vitro activity against Candida glabrata and C. krusei isolates clinically resistant to azole and echinocandin antifungal compounds. Antimicrob Agents Chemother. 2017;61(3):e01817-e1916.
Nishimoto AT, Wiederhold NP, Flowers SA, et al. In vitro activities of the novel investigational tetrazoles VT-1161 and VT-1598 compared to the triazole antifungals against azole-resistant strains and clinical isolates of Candida albicans. Antimicrob Agents Chemother. 2019;63(6):1–11.
Wang L, Zhang M, Guo J, et al. In vitro activities of the tetrazole VT-1161 compared with itraconazole and fluconazole against Cryptococcus and non-albicans Candida species. Mycologia. 2021;113(5):918–25.
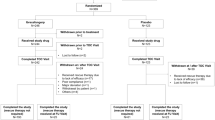
Martens MG, Maximos B, Degenhardt T, et al. Phase 3 study of the safety and efficacy of oteseconazole in treatment of recurrent vulvovaginal candidiasis and efficacy vs fluconazole in treatment of acute vulvovaginal candidiasis infections. Am J Obstet Gynecol. 2022;227(6):880.e1-11.
Sobel J, Donders G, Degenhardt T, et al. Efficacy and safety of oteseconazole in recurrent vulvovaginal candidiasis. NEJM Evid. 2022;1(8):1–13.
Brand SR, Degenhardt TP, Person K, et al. A phase 2, randomized, double-blind, placebo-controlled, dose-ranging study to evaluate the efficacy and safety of orally administered VT-1161 in the treatment of recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 2018;218(6):624.e1-9.
Brand SR, Sobel JD, Nyirjesy P, et al. A randomized phase 2 study of VT-1161 for the treatment of acute vulvovaginal candidiasis. Clin Infect Dis. 2021;73(7):e1518–24.
Sobel J, Degenhardt T, Person K, et al. Long-term observations of oteseconazole efficacy against recurrent vulvovaginal candidiasis [abstract no. 45]. Am J Obstet Gynecol. 2023;228(2 Suppl):S788–9.
Benitez LL, Carver PL. Adverse effects associated with long-term administration of azole antifungal agents. Drugs. 2019;79(8):833–53.
Rosa MI, Silva BR, Pires PS, et al. Weekly fluconazole therapy for recurrent vulvovaginal candidiasis: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;167(2):132–6.
Monk BC, Keniya MV, Sabherwal M, et al. Azole resistance reduces susceptibility to the tetrazole antifungal VT-1161. Antimicrob Agents Chemother. 2019;63(1):1–19.
Perlin DS, Rautemaa-Richardson R, Alastruey-Izquierdo A. The global problem of antifungal resistance: prevalence, mechanisms, and management. Lancet Infect Dis. 2017;17(12):e383–92.
Gamal A, Chu S, McCormick TS, et al. Ibrexafungerp, a novel oral triterpenoid antifungal in development: overview of antifungal activity against Candida glabrata. Front Cell Infect Microbiol. 2021;11: 642358.
Acknowledgements
The manuscript was reviewed by: A. Dovnik, University Clinic for Gynecology and Obstetrics, Maribor University Medical Centre, Maribor, Slovenia; S. Mahmoudi, Department of Parasitology and Mycology, School of Medicine, Iran University of Medical Sciences, Tehran, Iran; J. Rolo, CICS-UBI–Health Sciences Research Centre, Universidade da Beira Interior, Covilhã, Portugal; F. Wirth, Department of Microbiology, University of São Paulo, São Paulo, Brazil. During the peer review process, Mycovia Pharmaceuticals Inc., the marketing authorization holder of oteseconazole, was also offered an opportunity to provide a scientific accuracy review of their data. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and conflict of interest
S. Fung and M. Shirley are salaried employees of Adis International Ltd/Springer Nature and declare no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent for publication, Availability of data and material, Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fung, S., Shirley, M. Oteseconazole in recurrent vulvovaginal candidiasis: a profile of its use. Drugs Ther Perspect 39, 263–269 (2023). https://doi.org/10.1007/s40267-023-01008-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-023-01008-x