Abstract
Difelikefalin (Kapruvia®; Korsuva™), a novel peripheral kappa opioid receptor (KOR) agonist, is a promising emerging treatment for moderate-to-severe pruritus associated with chronic kidney disease (CKD) in adults undergoing haemodialysis. Evidence thus far indicates that difelikefalin is effective and generally well tolerated in these patients. In randomized, double-blind, placebo-controlled, multicentre phase 3 trials, difelikefalin produced clinically meaningful improvements in the intensity of itch in patients with moderate-to-severe CKD-associated pruritus. Difelikefalin was also associated with improved itch-related quality of life relative to placebo. Limited data suggest that clinical benefits are maintained over longer-term treatment. The most common treatment-emergent adverse events in difelikefalin recipients are diarrhoea, dizziness and nausea, typically of mild or moderate severity.
Plain Language Summary
Chronic kidney disease (CKD)-associated pruritus (itching that is directly related to advanced CKD and/or end-stage kidney failure) is common in patients undergoing haemodialysis and negatively impacts quality of life. Imbalances in endogenous opioid receptor activity may drive CKD-associated pruritus. Difelikefalin (Kapruvia®; Korsuva™) targets peripheral kappa opioid receptors and, in the USA and Europe, is the first drug to be specifically approved for the treatment of moderate-to-severe pruritus associated with CKD in patients undergoing haemodialysis. Difelikefalin therapy reduces itch severity in this frail patient population, based on results from clinical trials. Difelikefalin may also improve itch-related quality of life and quality of sleep. Common adverse events in recipients include diarrhoea, dizziness and nausea, which rarely require treatment discontinuation. Effective and generally well tolerated, difelikefalin is a promising emerging treatment for moderate-to-severe pruritus associated with CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features for this Adis Drug Q&A can be found at https://doi.org/10.6084/m9.figshare.20445828. |
Administered as an intravenous bolus injection at the end of each haemodialysis treatment |
Reduces itch intensity and potentially improves itch-related quality of life in patients with moderate-to-severe pruritus |
Generally well tolerated, with most treatment-emergent adverse events being of mild or moderate severity |
What is the rationale for developing difelikefalin in CKD-associated pruritus?
Chronic kidney disease (CKD)-associated pruritus (previously referred to as uraemic pruritus) is defined as itching that is directly related to CKD and not explained by any alternate cause [1,2,3]. It is highly prevalent in patients with end-stage kidney disease (ESKD) undergoing haemodialysis, affecting up to 80% and being of moderate-to-severe intensity in ≈ 40% [3]. Clinical presentations of CKD-associated pruritus vary with respect to severity, persistence, timing in relation to dialysis, and distribution pattern [1,2,3]. The itch may be localized (with areas commonly impacted including the back, face and shunt arm) or generalized [1,2,3]. CKD-associated pruritus is associated with sleep disruption, poor quality of life and depression, as well as adverse medical outcomes including a higher rate of mortality [1, 2, 4].
While the pathogenesis of CKD-associated pruritus is yet to be fully understood, endogenous opioid dysfunction is potentially involved [1, 2, 5]. Pruritus may result from an imbalance of mu opioid receptor (MOR) and kappa opioid receptor (KOR) activity due to central MOR over-stimulation or KOR under-stimulation [2, 5]. Opioid receptors have therefore been identified as potential targets in the treatment of pruritus. However, agents targeting MORs appear to be of limited therapeutic benefit for CKD-associated pruritus [1, 2, 6, 7]. Furthermore, adverse effects, including opioid withdrawal-like symptoms and gastrointestinal complaints, may restrict their use [6, 8,9,10]. Centrally acting KOR agonists also have use-limiting adverse effects (e.g. sedation, dysphoria, hallucinations) [11]. In response to these concerns, agents that exclusively activate peripheral KORs have been developed [11].
Difelikefalin [Kapruvia® (EU); Korsuva™ (USA)], a novel peripheral KOR agonist, is approved in the EU [12] and USA [13] for the treatment of moderate-to-severe pruritus associated with CKD in adult patients undergoing haemodialysis. Table 1 provides a summary of the prescribing information for difelikefalin in these regions. Consult local prescribing information for further details.
How should difelikefalin be used?
Difelikefalin should be restricted to use after in-centre haemodialysis treatment [12] and is intended to be administered as an intravenous bolus injection into the venous line of the dialysis circuit at the conclusion of each haemodialysis treatment (see Table 1 for details) [12, 13]. Prior to initiating difelikefalin therapy, clinicians should exclude causes of pruritus other than CKD [12]. The use of difelikefalin in patients on peritoneal dialysis has not been investigated and is not recommended [13].
How does difelikefalin work?
Difelikefalin is a peripheral KOR agonist that binds with high affinity and selectivity to KOR (Ki 0.32 nmol/L for human KOR) in vitro [14]. As the pathophysiology of CKD-associated pruritus likely involves systemic inflammation and endogenous opioid system imbalance (including KOR down-regulation), the anti-pruritic and anti-inflammatory effects of difelikefalin are attributed to its KOR activation on peripheral sensory neurons and immune cells [12]. Difelikefalin has low CNS penetration, with its physicochemical properties limiting its active transport and passive diffusion across membranes [12].
Difelikefalin potently alleviated visceral pain, inflammatory pain, neuropathic pain, evoked itch and writhing behaviour in rodent models [14]. In addition, difelikefalin was shown to inhibit cytokine release in a mouse model of sepsis. Unlike morphine (an MOR agonist), difelikefalin was not associated with any adverse gastrointestinal effects [14].
Difelikefalin administered intravenously to healthy, non-smoking volunteers (n = 15) at two-fold or ten-fold higher than the recommended dose did not produce respiratory depression in a randomized, double-blind, placebo-controlled, three-way crossover study [15]. Similarly, difelikefalin did not produce any clinically meaningful prolongation of the corrected QT interval when administered at a supratherapeutic dose six-fold higher than that recommended [13].
What potential is there for difelikefalin to be abused?
Difelikefalin appears to have low abuse potential [16]. In a dedicated human abuse potential study in healthy recreational drug users with opioid and hallucinogenic drug experience, the abuse potential profile of difelikefalin administered at supratherapeutic doses did not meaningfully differ from that of placebo and was significantly lower than that of a centrally acting opioid analgesic (a partial MOR agonist and KOR agonist). Difelikefalin had no dysphoric or hallucinogenic effects associated with CNS-penetrant KOR agonists [16].
What is the efficacy of difelikefalin in CKD-associated pruritus?
Intravenous difelikefalin is an effective treatment for moderate-to-severe CKD-associated pruritus in adults undergoing haemodialysis. Its efficacy at the recommended dosage was demonstrated in the randomized, double-blind, placebo-controlled, multicentre, phase 3 KALM-1 and KALM-2 trials [17,18,19], and supported by data from phase 2 trials [20, 21] and an open-label phase 3 study [22].
Patients eligible for enrolment in the US-only KALM-1 trial and global KALM-2 trial were adults ≥ 18 years with moderate-to-severe pruritus due to ESKD who were undergoing haemodialysis three times per week for ≥ 3 months prior to screening [17]. Moderate-to-severe pruritus was defined as a Worst Itching Intensity Numerical Rating Scale (WI-NRS) score of > 4 (KALM-1) or ≥ 5 (KALM-2). Exclusion criteria included pruritus attributed to a cause other than ESKD or its complications, localized itch restricted to the palms, or pruritus only during haemodialysis sessions. In each trial, patients were randomized to receive difelikefalin 0.5 μg/kg or placebo following haemodialysis three times per week for 12 weeks. A fourth dose per week was permitted in patients who received an additional haemodialysis treatment during a given week. Randomization was stratified by the use or non-use of concomitant medications to treat pruritus during the run-in period prior to randomization and the presence or absence of specific medical conditions (e.g. falls or fractures due to falls, gait disturbance, mental status change). Both trials included an open-label extension (OLE) phase of up to 52 weeks for patients who met certain eligibility criteria. During the OLEs, all patients received difelikefalin [17].
At baseline, disease characteristics were comparable between the difelikefalin and placebo groups of the pivotal trials [12]. Patients had a mean age of 59 years and mean WI-NRS score of 7.2 [12]. Approximately 40% of patients were using medicinal products prescribed for pruritus relief (e.g. antihistamines, corticosteroids), while 14% (KALM-1) or 17% (KALM-2) reported at least one of the specific medical conditions used for stratification [17]. In both trials, the primary endpoint was the percentage of patients who achieved a ≥ 3-point improvement (i.e. reduction) from baseline in the weekly mean of the daily WI-NRS score at week 12 [18, 19].
Difelikefalin was effective in reducing itch intensity in KALM-1 and KALM-2, with a significantly (p < 0.05) higher proportion of difelikefalin recipients than placebo recipients achieving a ≥ 3-point improvement from baseline in WI-NRS score at week 12 of each trial (Table 2). In both trials, the proportion of patients achieving the more stringent ≥ 4-point improvement from baseline in WI-NRS score at week 12 was also significantly (p ≤ 0.01) higher with difelikefalin than with placebo (Table 2). Significant (p < 0.05) improvements in ≥ 3-point and ≥ 4-point WI-NRS reduction rates with difelikefalin versus placebo were apparent by week 4 in KALM-2 (Table 2). In an analysis of pooled KALM-1 and KALM-2 data, significantly (p < 0.05) higher proportions of difelikefalin recipients than placebo recipients achieved ≥ 3-point WI-NRS improvements at all time points from week 1 to week 12 and WI-NRS complete responses (i.e. ≥ 80% of daily WI-NRS scores ≤ 1 for the preceding week) at all time points from week 3 to week 12 [23].
In subgroup analyses of the primary endpoint using pooled data from KALM-1 and KALM-2, difelikefalin was effective in both patients with moderate baseline itch (i.e. WI-NRS ≥ 4 to < 7) and severe baseline itch (WI-NRS ≥ 7; p-values not available), and in both the EU and other regions (p < 0.05 vs placebo) [post hoc analyses] [17]. The treatment effect was also directionally consistent across subgroups based on:
-
age (< 65 or ≥ 65 years; p < 0.05 vs placebo for younger patients only);
-
sex (male or female; both p < 0.05 vs placebo);
-
race (white or black; both p < 0.05 vs placebo), except for in a smaller subgroup of patients of “other” race;
-
geographical region (USA or non-USA; both p < 0.05 vs placebo); and
-
randomization strata (anti-pruritus medication use or non-use, presence or absence of specific medical conditions; p < 0.05 vs placebo for all) [23].
Difelikefalin significantly improved measures of itch-related quality of life relative to placebo in KALM-1 but not KALM-2 (Table 2). At week 12 of KALM-1, improvements from baseline in the 5-D Itch Scale total score and Skindex-10 Scale total score were greater with difelikefalin than with placebo (p < 0.001) [18]. In KALM-2, the treatment difference in change from baseline in Skindex-10 Scale total score did not reach statistical significance and, due to the hierarchical testing procedure, the difference in change in 5-D Itch Scale total score was not formally assessed [12, 17]. In analyses of pooled data from KALM-1 and KALM-2, higher (p < 0.05) proportions of difelikefalin recipients than placebo recipients achieved clinically meaningful Skindex-10 responses (≥ 15-point improvements from baseline in Skindex-10 total score; 55.5% vs 40.5%) and 5-D Itch responses (≥ 5-point improvements in 5-D Itch total score; 52.1% vs 42.3%) at week 12 [23].
Improvements in mean 5-D Itch Scale scores were maintained over ≤ 52 weeks of open-label difelikefalin treatment, based on OLE data [17, 23]. At week 52 of the KALM-1 OLE, the least-squares mean change from baseline in 5-D Itch Scale total score was −6.9 in patients who had previously received placebo and were switched to difelikefalin (n = 94) and −7.8 in patients who received continuous difelikefalin treatment (n = 90) [17]. The KALM-2 OLE was terminated early, with only 5 patients completing 52 weeks of OLE treatment [17].
Results of KALM-1 and KALM-2 were supported by those of an open-label, multicentre phase 3 study of difelikefalin 0.5 μg/kg three times per week for up to 12 weeks in patients with moderate-to-severe CKD-associated pruritus undergoing haemodialysis in the USA and Europe (n = 222; mean baseline WI-NRS score 7.6) [22]. At week 12 of this study, the majority of patients achieved ≥ 3-point improvements from baseline in WI-NRS score (74%) and Sleep Quality Numerical Rating Scale (NRS) score (66%). Improvements of ≥ 4 points in WI-NRS score and Sleep Quality NRS score were achieved by 59% and 57%, respectively. Mean changes from baseline to week 12 in Skindex-10 Scale and 5-D Itch Scale total scores were −21.0 and −7.1, respectively (both p < 0.001); clinically meaningful Skindex-10 and 5-D Itch responses were achieved by 63% and 70% of patients [22].
What is the tolerability profile of difelikefalin?
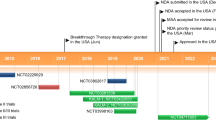
Intravenous difelikefalin is generally well tolerated in adults with moderate-to-severe CKD-associated pruritus undergoing haemodialysis, based on pooled safety data from phase 3 trials [24]. During the 12 weeks of placebo-controlled treatment in KALM-1 and KALM-2, treatment-emergent adverse events (TEAEs) were reported in 71.2% of difelikefalin recipients versus 65.3% of placebo recipients and were mostly of mild to moderate severity. The most common TEAEs in difelikefalin recipients (occurring in ≥ 2% and at an incidence ≥ 1% higher than with placebo) were diarrhoea, dizziness, gait disturbances, nausea, hyperkalaemia, headache, somnolence and mental status change (Fig. 1) [24]. In patients continuously exposed to difelikefalin over 6 and 12 months, the incidence and prevalence of diarrhoea, dizziness, somnolence, nausea and vomiting declined over time [17].
Most common treatment-emergent adverse events with difelikefalin 0.5 µg/kg three times per week (occurring in ≥ 2% and at an incidence ≥ 1% higher than with placebo) in adults with moderate-to-severe pruritus associated with chronic kidney disease undergoing haemodialysis: pooled data from KALM-1 and KALM-2 [24]
In the pooled KALM-1 and KALM-2 safety populations, TEAEs led to treatment discontinuation in 6.8% of difelikefalin recipients versus 4.0% of placebo recipients [24]. Among the adverse reactions most commonly leading to discontinuation of difelikefalin were dizziness (0.9% vs 0.2% with placebo), mental status change (0.7% vs 0.2%), nausea (0.5% vs 0%) and headache (0.5% vs 0%) [13]. Serious but non-fatal TEAEs occurred in 25.2% of difelikefalin recipients versus 22.6% of placebo recipients, while adverse events led to death in three difelikefalin recipients (0.7%) versus five placebo recipients (1.2%) [24]. The most common serious TEAEs were hyperkalaemia (1.9% of difelikefalin recipients vs 1.9% of placebo recipients), chest pain (1.9% vs 0.9%), pneumonia (1.4% vs 1.7%), sepsis (1.2% vs 1.7%), mental status changes (1.2% vs 0.5%) and chronic obstructive pulmonary disease (1.2% vs 0.5%) [17]. Serious TEAEs of diarrhoea, dizziness and somnolence occurred at low rates (< 1% of patients receiving difelikefalin or placebo), while there were no serious TEAEs of nausea or headache. None of the fatal events were considered to be due to the study treatment [17]. During the two-week discontinuation period of KALM-1, during which patients were not administered difelikefalin or placebo, there were no potential signs of physical dependence or adverse events related to withdrawal [18].
Difelikefalin continued to be well tolerated over longer-term treatment (up to 64 weeks) in an analysis of pooled data from phase 3 trials and OLEs (n = 1306; 811.3 patient-years of exposure to the recommended dose of difelikefalin) [24]. The incidences of common TEAEs and serious TEAEs did not appear to increase over longer-term exposure. TEAEs were reported by 78.3% of difelikefalin recipients and non-fatal serious TEAEs were reported by 41.5%. TEAEs led to treatment discontinuation in 9.3% and death in 4.3%. The incidence rate of AEs leading to death was 69.0/1000 patient-years in difelikefalin recipients, which was less than the rate of death in patients undergoing haemodialysis reported by the US Renal Data System [24].
A small number of warnings and precautions pertain to the use of difelikefalin in the EU [12] and USA [13] (Table 3); consult local prescribing information for further details.
What is the role of difelikefalin in CKD-associated pruritus?
Difelikefalin is effective and well tolerated in the treatment of CKD-associated pruritus, representing a promising emerging option for patients undergoing haemodialysis. Difelikefalin administered intravenously at the end of each haemodialysis session produces clinically meaningful improvements in itch severity in patients with moderate-to-severe pruritus undergoing haemodialysis, based on results from the KALM-1 and KALM-2 clinical trials [18, 19]. The threshold for a clinically meaningful change in WI-NRS has been proposed to be either 3 points [25] or 4 points [26], and the benefit of difelikefalin over placebo for WI-NRS improvement rate was significant at each of these thresholds in KALM-1 and KALM-2 (Table 2). Based on the patient population evaluated in these pivotal trials, difelikefalin is specifically indicated for the treatment of moderate-to-severe pruritus (Table 1); a baseline WI-NRS score of > 4 can be considered to signify this severity of itch [17]. Data from OLEs, albeit limited, suggest that the clinical benefits of difelikefalin endure over long-term treatment [17, 23].
In clinical practice, CKD-associated pruritus remains under-recognised and under-treated [27, 28]. Proactively identifying patients with CKD who are experiencing pruritus is particularly important given the apparent detrimental impact of CKD-associated pruritus on health-related quality of life and medical outcomes. Symptoms such as sleep disturbance, fatigue, depression and pain tend to co-occur with pruritus in patients with CKD [27]. Alleviating one symptom may reduce the severity of other associated symptoms, thus reducing overall symptom burden and leading to improvements in health-related quality of life and other clinical outcomes [27]. While it remains to be confirmed, difelikefalin appears to have a favourable effect on itch-related quality of life [17,18,19]. Improvements in itch-related quality of life may be partially explained through the effects of alleviated itching on sleep.
Patients undergoing haemodialysis are often frail, with co-morbidities and receiving multiple medications [9, 28]. As such, it is important that their treatments for pruritus be safe with low potential for drug-drug interactions [28]. Difelikefalin is unlikely to interact with other medications (Table 1) and is generally well tolerated in patients with CKD-associated pruritus undergoing haemodialysis [24]. The most common TEAEs are gastrointestinal disorders (e.g. diarrhoea, nausea) and nervous system disorders (e.g. dizziness, headache) [24]. It is important to note that difelikefalin is specifically (and conveniently) intended for use at the end of in-centre haemodialysis sessions and should not be administered outside of this setting [12].
Difelikefalin represents the first drug to be specifically approved for the treatment of CKD-associated pruritus in the either the USA or Europe [9]. Off-label treatments typically have limited efficacy in these patients or substantial adverse effects that limit their use [9]. No direct comparisons between these agents and difelikefalin are available. Broad European guidelines on the treatment of chronic pruritus recommend various treatments (e.g. gabapentinoids) in patients with CKD [29]. These guidelines precede the approval of difelikefalin in the EU and updated treatment guidelines are awaited with interest. A recent US-based expert review specific to CKD-associated pruritus recommends that systemic therapies be utilized in patients with generalized, moderate-to-severe and/or refractory CKD-associated pruritus [30]. While gabapentinoids have historically been considered the first-line options, difelikefalin is proposed to be a safe and effective alternative to these [30].
Results from ongoing clinical trials of difelikefalin in patients with pruritus on haemodialysis, including a randomized, double-blind, phase 3 trial in Japan (NCT04711603) and its long-term OLE, will be useful in further establishing the position of difelikefalin in the treatment of CKD-associated pruritus.
Change history
12 October 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40267-022-00953-3
09 November 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40267-022-00963-1
References
Verduzco HA, Shirazian S. CKD-associated pruritus: new insights into diagnosis, pathogenesis, and management. Kidney Int Rep. 2020;5:1387–402.
Shirazian S, Aina O, Park Y, et al. Chronic kidney disease-associated pruritus: impact on quality of life and current management challenges. Int J Nephrol Renovasc Dis. 2017;10:11–26.
Kim D, Pollock C. Epidemiology and burden of chronic kidney disease-associated pruritus. Clin Kidney J. 2021;14(Suppl. 3):i1-7.
Combs SA, Teixeira JP, Germain MJ. Pruritus in kidney disease. Semin Nephrol. 2015;35:383–91.
Agarwal P, Garg V, Karagaiah P, et al. Chronic kidney disease-associated pruritus. Toxins. 2021;13(8):527.
Kremer AE. What are new treatment concepts in systemic itch? Exp Dermatol. 2019;28:1485–92.
Makar M, Smyth B, Brennan F. Chronic kidney disease-associated pruritus: a review. Kidney Blood Press Res. 2021;46:659–69.
Bergasa NV. Pruritus in primary biliary cirrhosis: pathogenesis and therapy. Clin Liver Dis. 2008;12(2):385–406.
Lipman ZM, Yosipovitch G. An evaluation of difelikefalin as a treatment option for moderate-to-severe pruritus in end stage renal disease. Expert Opin Pharmacother. 2021;22(5):549–55.
Martin CE, Clotet-Freixas S, Farragher JF, et al. Have we just scratched the surface? A narrative review of uremic pruritus in 2020. Can J Kidney Health Dis. 2020;7:1–14.
Albert-Vartanian A, Boyd MR, Hall AL, et al. Will peripherally restricted kappa-opioid receptor agonists (pKORAs) relieve pain with less opioid adverse effects and abuse potential? J Clin Pharm Ther. 2016;41(4):371–82.
European Medicines Agency. Kapruvia 50 micrograms/mL solution for injection: EU summary of product characteristics. 2022. https://www.ema.europa.eu/. Accessed 23 Aug 2022.
Vifor (International) Inc. KORSUVA™ (difelikefalin) injection, for intravenous use [US prescribing information]. 2021. https://dailymed.nlm.nih.gov/. Accessed 23 Aug 2022.
Gardell LR, Spencer R, Chalmers D, et al. Preclinical profile of CR845: a novel, long-acting peripheral kappa opioid receptor agonist [abstract no. PW-231 and poster]. In: International Association for the Study of Pain. 2008.
Viscusi ER, Torjman MC, Munera CL, et al. Effect of difelikefalin, a selective kappa opioid receptor agonist, on respiratory depression: a randomized, double-blind, placebo-controlled trial. Clin Transl Sci. 2021;14(5):1886–93.
Shram MJ, Spencer RH, Qian J, et al. Evaluation of the abuse potential of difelikefalin, a selective kappa-opioid receptor agonist, in recreational polydrug users. Clin Transl Sci. 2022;15:535–47.
European Medicines Agency. Kapruvia (international non-proprietary name: difelikefalin): public assessment report. 2022. https://www.ema.europa.eu/. Accessed 23 Aug 2022.
Fishbane S, Jamal A, Munera C, et al. A phase 3 trial of difelikefalin in hemodialysis patients with pruritus. N Engl J Med. 2020;382(3):222–32.
Wooldridge TD, McCafferty K, Schoemig M, et al. Efficacy and safety of difelikefalin for moderate-to-severe CKD-associated pruritus: a global phase 3 study in hemodialysis patients (KALM-2) [abstract no. FR-OR24]. J Am Soc Nephrol. 2020;31(Suppl.):22–3.
Fishbane S, Mathur V, Germain MJ, et al. Randomized controlled trial of difelikefalin for chronic pruritus in hemodialysis patients. Kidney Int Rep. 2020;5(5):600–10.
Narita I, Tsubakihara Y, Uchiyama T, et al. Efficacy and safety of difelikefalin in Japanese patients with moderate to severe pruritus receiving hemodialysis: a randomized clinical trial. JAMA Netw Open. 2022;5(5): e2210339.
Weiner DE, Vervloet MG, Walpen S, et al. Safety and effectiveness of difelikefalin in patients with moderate-to-severe pruritus undergoing hemodialysis: an open-label, multicenter study. Kidney Med. 2022. https://doi.org/10.1016/j.xkme.2022.100542.
Topf J, Wooldridge T, McCafferty K, et al. Efficacy of difelikefalin for the treatment of moderate to severe pruritus in hemodialysis patients: pooled analysis of KALM-1 and KALM-2 phase 3 studies. Kidney Med. 2022. https://doi.org/10.1016/j.xkme.2022.100512.
Fishbane S, Wen W, Munera C, et al. Safety and tolerability of difelikefalin for the treatment of moderate to severe pruritus in hemodialysis patients: pooled analysis from the phase 3 clinical trial program. Kidney Med. 2022. https://doi.org/10.1016/j.xkme.2022.100513.
Vernon M, Ständer S, Munera C, et al. Clinically meaningful change in itch intensity scores: an evaluation in patients with chronic kidney disease-associated pruritus. J Am Acad Dermatol. 2021;84(4):1132–4.
US Center for Drug Evaluation and Research. Risk asessment and risk mitigation review(s): application number 214916Orig1s000 (difelikefalin). 2021. http://www.accessdata.fda.gov/. Accessed 23 Aug 2022.
Ahdoot R, Kalantar-Zadeh K, Burton J, et al. Novel approach to unpleasant symptom clusters surrounding pruritus in patients with chronic kidney disease and on dialysis therapy. Curr Opin Nephrol Hypertens. 2022;31(1):63–71.
Santos-Alonso C, Maldonado Martín M, Sánchez Villanueva R, et al. Pruritus in dialysis patients. Literature review and new perspectives. Nefrologia (Engl Ed). 2021;42(1):15–21.
Weisshaar E, Szepietowski JC, Dalgard F, et al. European S2k guideline on chronic pruritus. Acta Derm Venereol. 2019;99:469–506.
Lipman ZM, Paramasivam V, Yosipovitch G, et al. Clinical management of chronic kidney disease-associated pruritus: current treatment options and future approaches. Clin Kidney J. 2021;14(Suppl. 3):i16-22.
Acknowledgements
The manuscript was reviewed by: N. Ghadamyari, Department of Exercise Physiology, Faculty of Sport Health Sciences, Ankara University, Ankara, Turkey; S. Hiremath, Department of Medicine, University of Ottawa, Ottawa, Canada; J. Nowaczyk, Infant Jesus Teaching Hospital, Medical University of Warsaw, Warsaw, Poland. During the peer review process, Cara Therapeutics and CSL Vifor, the marketing authorization holders of difelikefalin, were also offered an opportunity to provide a scientific accuracy review of their data. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and conflict of interest
Y. N. Lamb is a salaried employee of Adis International Ltd/Springer Nature and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent for publication, Availability of data and material, Code availability
Not applicable.
Additional information
The original article has been updated: Due to textual changes.
The original article has been revised due to retrospective open choice order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lamb, Y.N. Difelikefalin in pruritus associated with chronic kidney disease: a profile of its use. Drugs Ther Perspect 38, 423–430 (2022). https://doi.org/10.1007/s40267-022-00945-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-022-00945-3