Abstract
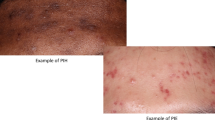
Acne-induced post-inflammatory hyperpigmentation (PIH) is a common complication of acne vulgaris in patients with darker skin and can be a cause of considerable distress. Treatment options for acne-induced PIH include topical treatments (currently the gold standard) and adjuvant procedural therapies such as chemical peels and energy-based devices. With all treatments, care needs to be taken to avoid worsening PIH. A primary strategy should be the prevention of acne-induced PIH through the effective treatment of inflammatory acne. In addition, the importance of photoprotection in preventing the worsening of PIH should not be overlooked.
Similar content being viewed by others
References
Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol. 2013;168:474–85.
Elbuluk N, Grimes P, Chien A, et al. The pathogenesis and management of acne-induced post-inflammatory hyperpigmentation. Am J Clin Dermatol. 2021;22(6):829–36.
Goh CL, Abad-Casintahan F, Chow SK. Evaluating acne-related post-inflammatory hyperpigmentation is a challenge even amongst experts. J Dermatol. 2014;41:1106–8.
Silpa-Archa N, Kohli I, Chaowattanapanit S, et al. Postinflammatory hyperpigmentation: a comprehensive overview: epidemiology, pathogenesis, clinical presentation, and noninvasive assessment technique. J Am Acad Dermatol. 2017;77(4):591–605.
Abad-Casintahan F, Chow SK, Goh CL. Frequency and characteristics of acne-related post-inflammatory hyperpigmentation. J Dermatol. 2016;43(7):926–8.
Akinboro AO, Ezejiofor OI, Olanrewaju FO. The impact of acne and facial post-inflammatory hyperpigmentation on quality of life and self-esteem of newly admitted Nigerian undergraduates. Clin Cosmet Investig Dermatol. 2018;11:245–52.
Abanmi A, Al-Enezi M, Al Hammadi A, et al. Survey of acne-related post-inflammatory hyperpigmentation in the Middle East. J Dermatolog Treat. 2019;30:578–81.
Darji K, Varade R, West D, et al. Psychosocial impact of postinflammatory hyperpigmentation in patients with acne vulgaris. J Clin Aesthet Dermatol. 2017;10(5):PMC5479473.
Callender VD, Baldwin H, Cook-Bolden FE, et al. Effects of topical retinoids on acne and post-infammatory hyperpigmentation in patients with skin of color: a clinical review and implications for practice. Am J Clin Dermatol. 2022;23:69–81.
Chaowattanapanit S, Silpa-Archa N, Kohli I, et al. Postinflammatory hyperpigmentation: a comprehensive overview: treatment options and prevention. J Am Acad Dermatol. 2017;77(4):607–21.
Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3:20–31.
Kaufman BP, Aman T, Alexis AF, et al. Postinflammatory hyperpigmentation: epidemiology, clinical presentation, pathogenesis and treatment. Am J Clin Dermatol. 2018;19:489–503.
Thomas J, Shankar K, Pujara S, et al. Consensus on management of acne-induced post-inflammatory hyperpigmentation: an Indian perspective. Int J Res Dermatol. 2021;7(2):336–45.
Ishack S, Lipner SR. Exogenous ochronosis associated with hydroquinone: a systematic review. Int J Dermatol. 2021. https://doi.org/10.1111/ijd.15878.
Cook-Bolden FE, Hamilton SF. An open-label study of the efficacy and tolerability of microencapsulated hydroquinone 4% and retinol 0.15% with antioxidants for the treatment of hyperpigmentation. Cutis. 2008;81:365-71.
Cestari TF, Hassun K, Sittart A. A comparison of triple combination cream and hydroquinone 4% cream for the treatment of moderate to severe facial melasma. J Cosmet Dermatol. 2007;6(1):36–9.
Chan R, Park KC, Lee MH, et al. A randomized controlled trial of the efficacy and safety of a fixed triple combination (fluocinolone acetonide 0.01%, hydroquinone 4%, tretinoin 0·05%) compared with hydroquinone 4% cream in Asian patients with moderate to severe melasma. Br J Dermatol. 2008;159(3):697–703.
Torok HM, Jones T, Rich P, et al. Hydroquinone 4%, tretinoin 0.05%, fluocinolone acetonide 0.01%: a safe and efficacious 12-month treatment for melasma. Cutis. 2005;75:57–62.
Lowe NJ, Rizk D, Grimes P, et al. Azelaic acid 20% cream in the treatment of facial hyperpigmentation in darker-skinned patients. Clin Ther. 1998;20:945–59.
Kircik LH. Efficacy and safety of azelaic acid (AzA) gel 15% in the treatment of post-inflammatory hyperpigmentation and acne: a 16-week, baseline-controlled study. J Drugs Dermatol. 2011;10.
Monteiro RC, Kishore BN, Bhat RM, et al. A comparative study of the efficacy of 4% hydroquinone vs 0.75% kojic acid cream in the treatment of facial melasma. Indian J Dermatol. 2013;58(2):157.
Lim JT. Treatment of melasma using kojic acid in a gel containing hydroquinone and glycolic acid. Dermatol Surg. 2001;25:282–4.
Bulengo-Ransby SM, Griffiths CE, Kimbrough-Green CK, et al. Topical tretinoin (retinoic acid) therapy for hyperpigmented lesions caused by inflammation of the skin in black patients. N Engl J Med. 1993;328(20):1438–43.
Jacyk AK, Mpofu P. Adapalene gel 0.1% for topical treatment of acne vulgaris in African patients. Cutis. 2001;68:48-54.
Grimes P, Callender V. Tazarotene cream for postinflammatory hyperpigmentation and acne vulgaris in darker skin: a double-blind, randomized, vehicle-controlled study. Cutis. 2006;77:45–50.
Sarkar R, Parmar N, Kapoor S. Treatment of postinflammatory hyperpigmentation with a combination of glycolic acid peels and a topical regimen in dark-skinned patients: a comparative study. Dermatol Surg. 2017;43(4):566–73.
Sarkar R, Ghunawat S, Garg VK, et al. Comparative study of 35% glycolic acid, 20% salicylic–10% mandelic acid, and phytic acid combination peels in the treatment of active acne and postacne pigmentation. J Cutan Aesthet Surg. 2019;12(3):158–63.
Ahn HH, Kim IH. Whitening effect of salicyclic acid peels in Asian patients. Dermatol Surg. 2006;32:372–5.
Grimes PE. The safety and efficacy of salicylic acid peels in darker racial-ethnic groups. Dermatol Surg. 1999;25:18–22.
Ali BMM, Gheida SF, El Mahdy NA, et al. Evaluation of salicylic acid peeling in comparison with topical tretinoin in the treatment of postinflammatory hyperpigmentation. J Cosmet Dermatol. 2017;16(1):52–60.
Ejaz A, Raza N, Iftikhar N, et al. Comparison of 30% salicylic acid with Jessner’s solution for superficial chemical peeling in epidermal melasma. J Coll Physicians Surg Pak. 2008;18:205–8.
Kumari R, Thappa DM. Comparative study of trichloroacetic acid versus glycolic acid chemical peels in the treatment of melasma. Indian J Dermatol Venereol Leprol. 2010;76:447.
Bae YC, Rettig S, Weiss E, et al. Treatment of post-inflammatory hyperpigmentation in patients with darker skin types using a low energy 1,927 nm non-ablative fractional laser: a retrospective photographic review analysis. Lasers Surg Med. 2020;52:7–12.
Wu X, Wang X, Wu X, et al. Intense pulsed light therapy improves acne-induced post-inflammatory erythema and hyperpigmentation: a retrospective study in Chinese patients. Dermatol Ther. 2022;12:1147–56.
Chan HH, Manstein D, Yu CS, et al. The prevalence and risk factors of post-inflammatory hyperpigmentation after fractional resurfacing in Asians. Lasers Surg Med. 2007;39:381–5.
Battle EF, Hobbs LM. Laser therapy on darker ethnic skin. Dermatol Clin. 2003;21:713–23.
Alexis AF. Lasers and light-based therapies in ethnic skin: treatment options and recommendations for Fitzpatrick skin types V and VI. Br J Dermatol. 2013;169(Suppl 3):91–7.
Thiboutot DM, Dreno B, Abanmi A, et al. Practical management of acne for clinicians: an international consensus from the Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2018;78(2 (Suppl 1)):S1–S23.e1.
Lakhdar H, Zouhair K, Khadir K, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and conflict of interest
Y. N. Lamb is a salaried employee of Adis International Ltd/Springer Nature and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent for publication, Availability of data and material, Code availability
Not applicable.
Rights and permissions
About this article
Cite this article
Lamb, Y.N. Aim to prevent acne-induced post-inflammatory hyperpigmentation as treatment remains a challenge. Drugs Ther Perspect 38, 343–348 (2022). https://doi.org/10.1007/s40267-022-00932-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-022-00932-8