Abstract
Tamoxifen, a cornerstone in the adjuvant treatment of estrogen receptor-positive breast cancer, significantly reduces breast cancer recurrence and breast cancer mortality; however, its standard adjuvant dose of 20 mg daily presents challenges due to a broad spectrum of adverse effects, contributing to high discontinuation rates. Dose reductions of tamoxifen might be an option to reduce treatment-related toxicity, but large randomized controlled trials investigating the tolerability and, more importantly, efficacy of low-dose tamoxifen in the adjuvant setting are lacking. We conducted an extensive literature search to explore evidence on the tolerability and clinical efficacy of reduced doses of tamoxifen. In this review, we discuss two important topics regarding low-dose tamoxifen: (1) the incidence of adverse effects and quality of life among women using low-dose tamoxifen; and (2) the clinical efficacy of low-dose tamoxifen examined in the preventive setting and evaluated through the measurement of several efficacy derivatives. Moreover, practical tools for tamoxifen dose reductions in the adjuvant setting are provided and further research to establish optimal dosing strategies for individual patients are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Low-dose tamoxifen has a superior tolerability compared with standard-dose tamoxifen. |
There is growing evidence that lower doses of tamoxifen also have antitumor efficacy, although this depends on tumor and patient characteristics. |
Neoadjuvant window-of-opportunity trials could be used to gain more evidence regarding clinical efficacy of low-dose tamoxifen. |
1 Introduction
Tamoxifen is a selective estrogen receptor (ER) modulator frequently used in the treatment of ER-positive breast cancer. In the adjuvant setting, tamoxifen 20 mg daily for 5 years reduces the breast cancer recurrence rate by approximately 40% during the first 10 years of follow-up and decreases the annual breast cancer death rate by one-third [1, 2]. Tamoxifen is recommended for a duration of 5–10 years for premenopausal patients and 2–3 years for postmenopausal patients followed by 3–7 years of an aromatase inhibitor [3,4,5]. Tamoxifen has been registered since 1973, but is still a cornerstone in the treatment of ER-positive breast cancer, especially for premenopausal women [6].
As an ER modulator, besides being an ER-agonist, tamoxifen also acts as an ER-antagonist, depending on the specific ER-containing tissue to which it binds [7]. Several healthy tissues express ER. As a consequence, a variety of (endocrine) adverse effects can occur after tamoxifen, or its metabolites, bind to these receptors. For example, hot flashes are probably caused by an ER-antagonistic effect in the central nervous system, since ERs are also present in the brain, which leads to thermoregulatory dysfunction [8]. In contrast, tamoxifen’s ER-agonistic effect in the endometrium can cause endometrial abnormalities and vaginal discharge [7]. Other mentioned bothersome adverse effects are arthralgia, insomnia, mood alterations, weight gain and vaginal dryness [9]. Venous thromboembolism (VTE) and endometrial cancer can also occur and, although rare, are serious adverse effects of tamoxifen [10,11,12]. The aforementioned adverse effects can have a huge impact on a patient’s quality of life, especially since the duration of treatment in the adjuvant setting can be up to 10 years [13]. This becomes painfully visible as almost half of the patients discontinue tamoxifen within 5 years due to adverse effects and one-third of these patients discontinue tamoxifen already within the first year of treatment [14,15,16,17]. Another substantial group of patients adheres to tamoxifen therapy while compromising on health-related quality of life [9, 13].
Tamoxifen is a prodrug and is metabolized by cytochrome P450 (CYP) enzymes CYP2D6 and CYP3A4 to 4-hydroxy-tamoxifen, N-desmethyl-tamoxifen and endoxifen [18]. Both endoxifen and 4-hydroxy-tamoxifen have the highest affinity for the ER (more than 300 times higher than tamoxifen); however, endoxifen is considered the most important metabolite because it also has the highest plasma concentrations of all metabolites [19,20,21]. Several retrospective studies among primary breast cancer patients using tamoxifen 20 mg have indicated an exposure-response relationship between endoxifen levels and tamoxifen efficacy, with suggested endoxifen thresholds varying from 10 to 16 nM [22,23,24]. Of these thresholds, 16 nM is the most widely accepted, as shown in the largest study thus far (1370 patients [23] compared with 86 [22] and 306 patients [24]). It is also the most conservative threshold, minimizing the chance of patients inappropriately continuing to use an ineffective dose [25, 26]. However, until now no prospective study was able to confirm the ‘definitive’ endoxifen efficacy threshold, possibly due to inadequate statistical power [27,28,29]. The effect of tamoxifen and metabolite levels on the occurrence of adverse effects remains largely unclear. While some studies found no association between tamoxifen, endoxifen, 4-hydroxy-tamoxifen, N-desmethyl-tamoxifen and adverse effects [30, 31], others showed an association between elevated tamoxifen or endoxifen levels and increased adverse effects [32, 33]. Notably, none of the patients in these studies were treated with tamoxifen doses that were lower than the standard dose of 20 mg.
The high incidence of tamoxifen-related adverse effects affecting quality of life, as well as the high discontinuation rate of tamoxifen among patients with ER-positive breast cancer, raises the question whether reducing the dose of tamoxifen could lead to a better toxicity profile without reducing its efficacy. In the primary (for those at increased risk for breast cancer) and secondary (for patients with premalignant lesions) chemoprevention settings, tamoxifen 20 mg is also recommended in National Comprehensive Cancer Network (NCCN) and American Society of Clinical Oncology (ASCO) guidelines, as it can reduce the risk for breast cancer development by one-third [34,35,36,37]. After a successful randomized controlled trial (RCT), low-dose tamoxifen (5 mg) is also considered an option in the primary and secondary chemoprevention settings [34, 35, 38]. In the adjuvant setting, no RCT between tamoxifen 20 mg and lower doses of tamoxifen has been performed thus far. Given the impressively large number of patients needed, together with the long duration of follow-up that would be required to obtain firm conclusions [29, 39], it is highly unlikely that such a study will ever be conducted. To determine whether there are other possibilities to solve this pressing question, the current literature was systematically reviewed to discuss two important topics: (1) tamoxifen-related adverse effects in women using low-dose tamoxifen compared with the standard adjuvant dose of 20 mg or placebo; and (2) clinical efficacy of low-dose tamoxifen compared with standard-dose tamoxifen or placebo. Finally, based on these findings, we attempted to provide practical advice on how to respond when patients experience bothersome adverse effects of tamoxifen.
2 Methods
We conducted a search of the Embase, Medline ALL, Web of Science Core Collection and Cochrane Register of Controlled Trials databases using the following search terms: ‘(tamoxifen) AND (drug dose reduction OR drug underdose) OR (tamoxifen NEAR (dose OR dosage OR reduct OR decreas OR tapering OR low OR lower OR regiment OR de-escalat OR adjustment OR modificat OR alter OR altered OR change OR dependent OR underdose OR underdosage)’ up to 1 December 2023. We excluded reviews, guidelines and editorials, prequels from other published studies, studies where no lower doses of tamoxifen (i.e. below the standard adjuvant dose of 20 mg) were investigated, studies where tamoxifen was not continuously administered, and studies where no adverse effects, clinical efficacy or suitable derivatives for clinical efficacy of tamoxifen were assessed. To qualify as a ‘suitable derivative for tamoxifen efficacy’, the following criteria had to be met: (1) the derivative had to be associated with breast cancer risk; (2) the derivative could be influenced by tamoxifen; and (3) alteration of the derivative after tamoxifen could predict the long-term efficacy of tamoxifen.
3 Results
Based on the systematic search, a total of 2081 results were found and screened by title or abstract for relevance, leading to 106 relevant abstracts; 19 articles were eventually included in this review. An overview of the article selection can be found in Fig. 1, and the studies discussed in this review can be found in Table 1.
3.1 Dose of Tamoxifen and Adverse Effects
To determine whether taking a lower dose of tamoxifen can decrease the high incidence of adverse effects, we first investigated whether low-dose tamoxifen leads to fewer adverse effects. An overview of the results considering low-dose tamoxifen and menopausal symptoms can be found in Table 2. Low-dose tamoxifen is defined as all tamoxifen doses below the standard dose of 20 mg daily.
3.1.1 Menopausal Symptoms
3.1.1.1 Low-Dose Tamoxifen (<20 mg Once Daily) Compared with Standard-Dose Tamoxifen (20 mg Once Daily)
Two studies compared the adverse effects of different levels of low-dose tamoxifen with that of a standard daily dose of tamoxifen 20 mg, and both showed a trend towards fewer adverse effects with low-dose tamoxifen [40,41,42]. The first study was a large RCT randomizing 1230 healthy women with high mammographic density between placebo and tamoxifen 1, 2.5, 5, 10 or 20 mg daily for 6 months. Adverse effects were self-reported using the five-point Likert scale questionnaires assessing symptoms of antihormonal treatment of breast cancer. In this study, lower doses of tamoxifen led to fewer adverse effects, specifically in vasomotor and gynecologic symptoms as well as muscle cramps [40, 41]. This reduction was however confined to premenopausal women [41]. In the other much smaller study (n = 120), tamoxifen 1, 5 or 20 mg daily was administered for 4 weeks preoperatively to patients with invasive breast cancer. Patients in the 1 or 5 mg tamoxifen group experienced fewer hot flashes (32% and 36% in the 1 and 5 mg groups, respectively, vs. 50% in the 20 mg group) and less vaginal discharge (26% and 22% in the 1 and 5 mg groups, respectively, vs. 47% in the 20 mg group) compared with patients in the tamoxifen 20 mg group [42]; however, these differences were not statistically significant, likely because of the small numbers of patients under study (only 40 participants per dose group). From these data, it can be concluded that lower doses of tamoxifen seem to lead to fewer adverse effects than the standard dose [40,41,42].
3.1.1.2 Low-Dose Tamoxifen (<20 mg Once Daily) Compared with Placebo
The use of hormonal replacement therapy (HRT) in healthy women is associated with an increased risk for breast cancer development compared with non-users [43]. In two primary prevention studies among healthy postmenopausal women using HRT for menopausal symptoms, women were randomized between low-dose tamoxifen or placebo [44, 45]. Besides the incidence of invasive breast cancer, menopausal symptoms were assessed in detail in both studies. In the smaller study (n = 210) no difference was found in 12 menopausal symptoms between women taking low-dose tamoxifen for 1 year compared with placebo [44]. Women were randomized between tamoxifen doses of 1 mg daily, 5 mg daily, or 10 mg weekly, i.e. two-thirds of the women taking tamoxifen received a very low tamoxifen dose (1 mg tamoxifen daily or 10 mg tamoxifen weekly). There was a trend towards more hot flashes, sweating and vaginal discharge when the total weekly dose of tamoxifen increased. The second, much larger study (n = 1884) showed that using tamoxifen 5 mg daily for 5 years led to more hot flashes, nights sweats, vaginal discharge and vaginal dryness compared with placebo [45]. The question is, how generalizable these findings are for the general population, since, in this study, there was a clear preselection of women who had already proven to have complaints related to the physiological menopause for which they used HRT.
In three prevention studies of patients with ductal carcinoma in situ (DCIS) or lobular carcinoma in situ (LCIS; n = 500 [38, 47] and n = 235 [48, 49]) and patients with a history of chest irradiation (n = 72 [50]), the use of tamoxifen 5 mg daily for a period of 2–3 years was compared with placebo. Studies assessed adverse effects using the Common Terminology Criteria for Adverse Events (CTCAE), patient-reported symptoms, or menopause-related adverse effects questionnaires. In most of the over 40 evaluated adverse effects, no significant differences between tamoxifen and placebo were found. The same accounted for four menopausal quality-of-life domains. However, compared with placebo, tamoxifen did lead to increased frequency of hot flashes, but without an increase in the intensity of the hot flashes [38], as well as more fatigue and myalgia [50]. Unfortunately, in the latter study, no correction for multiple testing was performed despite comparing 26 different adverse effects.
Overall, low doses of tamoxifen (≤5 mg daily) showed a good safety profile. Although some increase in adverse effects was found with low-dose tamoxifen compared with placebo in three of five prevention studies, this was in a minority of the evaluated adverse effects [38, 45, 50].
3.1.1.3 Effect of Lowering the Tamoxifen Dose
Two single-arm studies assessed the effect on adverse effects of a dose reduction of the standard tamoxifen dose (20 mg) in the adjuvant setting in patients who experienced tamoxifen-related adverse effects [51, 52]. In the first study, tamoxifen dose was decreased from 20 to 10 mg daily in 20 patients with invasive breast cancer experiencing severe hot flashes. The investigators evaluated the effects using a specific hot flash diary and measured subjective improvement in hot flashes after 8 weeks of taking the reduced dose of tamoxifen 10 mg [51]. Seventeen patients (85%) reported a subjective improvement in hot flashes after dose reduction. There was a numeric difference in hot flash score (131 points with a 20 mg dose vs. 47 points with a 10 mg dose), although this did not statistically differ. In a second study from our own group, the tamoxifen dose was reduced from 20 to 10 mg daily for 3 months in 17 patients with invasive breast cancer experiencing bothersome tamoxifen-related adverse effects who also had an endoxifen level ≥32 nM (i.e. two times the conservative endoxifen efficacy threshold of 16 nM) [23, 52]. Endocrine symptoms (primary endpoint) and health-related quality of life, both measured using the FACT-ES questionnaire [53], were assessed at baseline and after 3 months of using a lower dose of tamoxifen. Both endocrine symptoms and health-related quality of life improved statistically significantly and clinically meaningful in 41% and 65% of patients, respectively. Almost three-quarters of the patients graded the improvement in tamoxifen-related adverse effects after tamoxifen dose reduction as sufficient. Endocrine symptoms and health-related quality of life were also evaluated in 60 patients who continued to take tamoxifen 20 mg for 3 months. No improvements were seen in this group over time [52]. From these two studies, it seems that lowering the dose of tamoxifen compared with a standard dose improves tolerability by reducing menopausal symptoms, although performance bias due to the fact that patients were not blinded for dose reduction cannot be fully excluded.
3.1.2 Severe Adverse Effects: Endometrial Cancer and Venous Thromboembolism
Besides menopausal symptoms, tamoxifen can also lead to some rare but severe adverse effects, such as VTE and endometrial cancer. The rate of endometrial cancer increases approximately two to three times with tamoxifen compared with breast cancer patients not using tamoxifen, although the absolute incidence is very low (1.6/1000 patients) [54]. The risk increases with a longer duration of tamoxifen therapy [55], likely due to increasing cumulative tamoxifen dose [56]. Endometrial polyps also occur more frequently with tamoxifen use compared with non-users (>10% incidence after 4 years of tamoxifen standard dose in postmenopausal patients compared with non-tamoxifen users) and can transform into endometrial cancer [57, 58]. It would be very beneficial if reducing the dose of tamoxifen due to severe menopausal symptoms could also diminish these risks.
Five studies that investigated the influence of low-dose tamoxifen on endometrial polyps [38, 45, 48] or endometrial cancer were identified [45, 59, 60]. All three studies that investigated the incidence of endometrial cancer, using low-dose (20 mg weekly, 5 mg daily) tamoxifen for 2 to 5 years with a follow-up time of at least 5 years, included a large number of women (sample sizes reaching from 500 to 1884). Two studies included patients in a secondary chemoprevention setting [59, 60] and one study investigated healthy women receiving HRT [45]. None of these studies found an increased incidence of endometrial cancer in the low-dose tamoxifen group compared with the placebo group [45, 59, 60]. Three studies investigated low-dose tamoxifen and the incidence of endometrial polyps [38, 48]. In two small studies in the secondary chemoprevention setting (n = 500 and n = 235), a trend towards a higher incidence of endometrial polyps was found in women using tamoxifen 5 mg for 3 years compared with placebo, although this was not statistically significant (11% vs. 7%, p = 0.62; and 2.8% vs. 1.6%, p = 0.54, respectively) [38, 48]. The third much larger study among women receiving HRT (n = 1884) found an almost five times higher significant increase in endometrial polyps among those taking a daily dose of tamoxifen 5 mg for 5 years compared with placebo (2.9% in the tamoxifen group vs. 0.6% in the placebo group; relative risk [RR] 4.74, 95% confidence interval [CI] 1.96–11.5) [45]. These findings imply that there is an increased risk of developing endometrial polyps when using low-dose tamoxifen compared with placebo, although it is unknown how the low-dose tamoxifen polyp incidence compares with that of standard-dose tamoxifen.
A tamoxifen dose of 20 mg daily results in an RR for VTE ranging from 1.6 to 3.0 [61,62,63,64]. The reported VTE incidence was 1–3% during standard dose tamoxifen treatment, and most events occur within the first 2 years of treatment [65, 66]. Two studies compared the incidence of VTE between tamoxifen 5 mg daily for 3–5 years and placebo. One study was performed in healthy women receiving HRT (n = 1884) and the other study was performed in patients with carcinoma in situ (n = 500). No significant difference was found (0.5% for tamoxifen vs. 0.2% for placebo [RR 2.64, 95% CI 0.51–13.6] and 0.4% for both tamoxifen and placebo, with a p-value of 1.0, respectively) over a follow-up period of 6–10 years [45, 67]. Although the first mentioned study was in women receiving HRT [45], which might have influenced the VTE incidence because HRT leads to a higher VTE risk itself [68], the absolute incidence for VTE is very low. These findings support the idea that a reduction in the tamoxifen dose may lead to a lower incidence of VTE than standard tamoxifen dosing, although this has not been directly investigated.
3.2 Dose of Tamoxifen and Clinical Efficacy
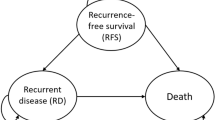
Thus far, no RCT investigating the efficacy between a standard tamoxifen dose of 20 mg and lower doses of tamoxifen in the adjuvant setting has been conducted and is highly unlikely to be conducted given the impressively large number of patients needed, together with the long duration of follow-up that is required. Consequently, direct evidence elucidating the clinical efficacy of lower tamoxifen doses in the adjuvant setting is lacking. To answer the question whether lower doses of tamoxifen still have antitumor efficacy, a search was conducted for articles that evaluated lower doses of tamoxifen versus a standard dose or placebo using derived measures of tamoxifen efficacy in the adjuvant setting. First, the efficacy of low-dose tamoxifen in preventing the development of breast cancer (primary and secondary chemoprevention) will be discussed. Second, two derived measures of tamoxifen efficacy are discussed: (1) the effect of tamoxifen on mammographic density; and (2) the effect of tamoxifen on the proliferation marker Ki67. An overview of the results of low-dose tamoxifen on the different clinical efficacy derivatives can be found in Table 3.
3.2.1 Low-Dose Tamoxifen in Preventing Breast Cancer Development
A standard dose of tamoxifen is known to be effective in not only preventing breast cancer recurrence after invasive breast cancer but also in primary and secondary prevention, i.e. preventing (new) primary breast cancers in patients with high breast cancer risk or a history of breast carcinoma in situ, such as DCIS [36]. For example, in women with DCIS, tamoxifen 20 mg reduces the risk of developing invasive breast cancer by 36% [36]. These findings have resulted in ASCO and NCCN guidelines to consider a daily dose of tamoxifen 20 mg for women with high risk for breast cancer, DCIS or LCIS to prevent breast cancer development [34, 35]. Aiming to increase the compliance for the primary and secondary prevention indication, studies with low-dose tamoxifen for this patient group were performed. Six prevention studies (three observational and three randomized) examined the clinical efficacy of low-dose tamoxifen in terms of preventing the development of breast cancer [38, 45, 48, 59, 60, 69].
In three large observational studies, low-dose tamoxifen (5 mg/day, 10 mg every other day, or 20 mg per week) for 2–5 years was compared with no tamoxifen (not placebo-controlled) in women who underwent surgery for DCIS [59, 60, 69]. They found approximately 30% reduction in breast cancer risk in women taking low-dose tamoxifen (independent of dose) compared with women who did not use tamoxifen [59, 60, 69]. In subanalysis, the significant breast cancer risk reduction of low-dose tamoxifen disappeared in women below 50 years of age [59]. The same trend was seen for premenopausal women [60].
Three randomized, placebo-controlled trials were conducted in healthy women using HRT [45] and women with carcinoma in situ [38, 48], comparing tamoxifen 5 mg daily with placebo for 2–5 years. In two studies, only a numerical (but not statistical) lower incidence of invasive breast cancer or DCIS in tamoxifen-treated patients could be found [45, 48]. One study had a small sample size of only 60 patients per treatment group [48] and the other study enrolled a significantly lower number of women than estimated (n = 1884 instead of 4500) due to challenges in recruitment and an earlier-than-expected cessation of inclusion, also leading to a lack of power [45]. In the third study (n = 500), taking tamoxifen for 3 years halved the incidence of breast cancer [38, 67]. Consistent with the observational studies, the efficacy of low-dose tamoxifen was more pronounced in postmenopausal women than in premenopausal women [67].
Taken together, these data provide evidence for the efficacy of low doses of tamoxifen in the primary and secondary prevention settings, mainly in postmenopausal women. It is however not entirely clear whether the efficacy in preventing the development of primary breast cancer can simply be translated into efficacy in preventing breast cancer recurrences in the adjuvant setting. Furthermore, no direct comparisons were made with tamoxifen 20 mg daily.
3.2.2 Lowering Mammographic Density as a Derived Measure of Tamoxifen Efficacy
Mammographic density is based on the distribution between stromal, epithelial and fat cells, where women with high mammographic density have relatively more stromal and epithelial cells and less adipocytes [70]. Several studies have shown that high breast tissue density, as assessed by mammography, is associated with an increased risk for developing breast cancer in both pre- and postmenopausal women compared with low breast density [70,71,72,73]. Although it is not completely understood why higher mammographic density is associated with higher breast cancer risk, it is hypothesized that a combination of higher cell proliferation of stromal and epithelial cells and genetic damage to these proliferating cells in dense breast tissue increases the risk of breast cancer [74].
A standard dose of tamoxifen 20 mg daily can significantly reduce mammographic density compared with placebo after 1 year of treatment [75]. Interestingly, in the preventive setting, a reduction in mammographic density of ≥10% after 1 year of tamoxifen 20 mg daily led to a reduction in breast cancer risk of 63% compared with a group of women who received placebo [76]. This reduction in breast cancer risk was not seen in women treated with tamoxifen who experienced a <10% reduction in mammographic density. Similar results were found in the adjuvant setting. Breast cancer patients with a 20% reduction in mammographic density after an average of 1 year of standard-dose tamoxifen had a 50% reduction in the risk for breast cancer-specific death compared with patients taking tamoxifen with no reduction in mammographic density [77].
Low doses of tamoxifen (5 mg daily) also led to a significant reduction in mammographic density after 6–12 months in women with a high baseline mammographic density [40], HRT for menopausal symptoms [44], history of chest radiation [50], or carcinoma in situ [48] compared with placebo (or ultra-low-dose tamoxifen) [40, 44, 48, 50], and a non-inferior reduction compared with the standard dose of tamoxifen [40]. Notably, the breast density reduction was predominantly seen in premenopausal women [40, 48].
3.2.3 Ki67 Changes in Response to Endocrine Therapy
Tamoxifen slows the proliferation of breast cancer cells by inhibiting the cell cycle from the G1-phase to the S-phase [78]. To express the degree of proliferation in cancer cells, Ki67 staining is often used. Ki67 is a nuclear marker expressed in all phases of the cell cycle other than the G0-phase, is absent in nuclei of resting cells, and is expressed in proliferating cells [79, 80]. Ki67 is a well-known prognostic marker in primary breast cancer [79, 81]. More interestingly, changes in Ki67 expression in cancer cells in response to standard endocrine therapy have shown to be strong predictive markers for efficacy of endocrine therapy [81, 82].
Nearly 20 years ago, Dowsett et al. were the first to demonstrate that only 2 weeks of endocrine therapy (tamoxifen or aromatase inhibitors) before surgery could lead to a decrease in proliferation (expressed as a Ki67 decrease) of ER-positive breast cancer cells, and that this phenomenon might be predictive of recurrence-free survival [83]. In the POETIC study, a large, randomized, phase III study, it was confirmed that the effect of 2 weeks of preoperative aromatase inhibitors on ER-positive breast cancer cell proliferation was a strong predictor of time-to-recurrence and therefore could be used as a surrogate endpoint for the long-term efficacy of endocrine therapy [81]. These investigators came to the conclusion that there is efficacy of the endocrine therapy if the Ki67 falls below 10% after 2 weeks of treatment. If the value is already below 10% before the start of treatment, no reliable conclusion can be drawn as to whether or not the endocrine therapy is effective. Since then, this surrogate endpoint has been widely used in preoperative endocrine therapy studies (both tamoxifen and aromatase inhibitors) to answer important clinically relevant research questions, of which the ADAPT study is a perfect example [84, 85]. In that study, breast cancer patients who had an adequate decrease in Ki67 after a short duration of neoadjuvant endocrine therapy were spared adjuvant chemotherapy [84]. In contrast, in the ongoing POETIC-A trial, breast cancer patients who did not have an adequate response in Ki67 after neoadjuvant endocrine therapy are offered additional adjuvant abemaciclib (ClinicalTrials.gov NCT04584853) [84].
The ability of low doses of tamoxifen to suppress the proliferation of ER-positive breast cancer, as a measure of efficacy, has been investigated in three studies, with somewhat conflicting results [42, 86, 87]. In the first study, three groups of patients (40 patients per group) with ER-positive breast cancer were randomized to treatment with tamoxifen 1, 5 or 20 mg compared with non-randomized breast cancer patients who were not treated preoperatively. After 4 weeks of tamoxifen treatment, Ki67 decreased similarly in all three treated groups (i.e. no dose response relation) and the decrease was significantly lower than in the untreated patient group. This suggests that treatment with a lower dose of tamoxifen also shows antitumor activity. Furthermore, no evidence of an association between change in Ki67 expression and concentrations of tamoxifen or 4-hydroxy-tamoxifen in serum could be found [88]. Unfortunately, no endoxifen levels were measured. In a second smaller study, these results were confirmed [42]. Eighteen ER-positive breast cancer patients were treated with tamoxifen 10 mg daily for 2 weeks and showed a significant reduction in Ki67, from a mean expression index of 25% to a mean expression of 10%, while in the control group who did not receive tamoxifen, no significant reduction in Ki67 was seen [86]. In the third study, these results could not be confirmed for ultra-low dose tamoxifen. In that study, premenopausal patients with invasive breast cancer (n = 125) were randomized between an ultra-low dose tamoxifen 10 mg/week or placebo for 6 weeks before surgery [87]. No significant decrease in Ki67 expression was seen after preoperative treatment with ultra-low-dose tamoxifen among these premenopausal patients.
4 Discussion
Our review shows that low-dose tamoxifen demonstrates a clinically relevant, better toxicity profile than standard-dose tamoxifen, and that there is strong indirect evidence that lower doses of tamoxifen also possess antitumor efficacy. This is important because it could allow dose reduction in those patients who experience bothersome adverse effects from tamoxifen at a standard dose of 20 mg daily. However, in the absence of randomized trials in the adjuvant setting, the challenge is to select the right patients with invasive breast cancer for whom dose reduction can potentially be used.
The ultimate goal of reducing the tamoxifen dose in cases of severe adverse effects is to increase the adherence to tamoxifen and thus improve the prognosis for breast cancer patients. Unfortunately, there were no studies in patients with breast cancer that have examined whether lowering the adverse effects by reducing the tamoxifen dose also led to an increase in adherence. This has been investigated in prevention studies with tamoxifen in women at high risk of developing breast cancer. Patients preferred low-dose tamoxifen over standard-dose tamoxifen in the preventive setting [89, 90]. Furthermore, adherence rates were numerically higher for low-dose tamoxifen (93.3% vs. 85%), although this did not meet statistical significance [89]. Adherence between placebo and low-dose tamoxifen was equal in several prevention studies [38, 45, 49, 50]; however, treatment compliance among study populations within prevention studies tends to be lower than in the adjuvant setting, with adherence rates often falling below 50% [91]. This can be partly attributed to adverse effects, but might also be influenced by lower intrinsic motivation of patients to use medication for primary or secondary prevention. Consequently, the findings from such studies may possess limited generalizability to the adjuvant setting.
A first evidence that lower doses of tamoxifen also have an antitumor effect comes from preventive studies that showed that low doses of tamoxifen compared with placebo also prevent the development of breast cancer. This evidence led to including tamoxifen 5 mg daily as an alternative option (compared with tamoxifen 20 mg daily) for patients with high breast cancer risk, DCIS, or other breast carcinoma in situ, in the ASCO and NCCN guidelines [34, 35]. The effect of low-dose tamoxifen in primary prevention was mainly observed in postmenopausal women. The explanation of menopausal status as a possible effect-modifier must likely be sought in the working mechanism of tamoxifen, i.e. competitive inhibition of the ER with estradiol. In the studies that also included premenopausal women, these women did not receive gonadotropin hormone-releasing hormone (GnRH) agonists next to the tamoxifen treatment, and thus estradiol levels were much higher compared with the postmenopausal women. Moreover, in contrast with postmenopausal women, estradiol levels increase with tamoxifen use in premenopausal women [92]. The elevated estradiol levels might compete with the relatively low endoxifen levels for the ER. This could therefore explain the smaller preventive effect of low-dose tamoxifen in premenopausal women. Indeed, in one of the RCTs, the effect of low-dose tamoxifen on breast cancer prevention also seemed more pronounced in women with lower than median, compared with higher than median, estradiol levels [67, 93].
A second indirect indication that lower doses of tamoxifen have an antitumor effect comes from studies that looked at a decrease in mammographic density, which has been shown to be predictive of reducing the risk of breast cancer recurrence [76, 77]. Although low-dose tamoxifen also reduces breast density, this was found to be mainly the case in premenopausal women. Although this seems in contrast with the efficacy of low-dose tamoxifen in primary prevention studies, the absence of an effect in postmenopausal women is probably caused by the much lower mammographic density at baseline found in postmenopausal women compared with premenopausal women [94]. Unfortunately, for now, mammographic density reduction does not seem to be practical to use as an individual test for tamoxifen efficacy because of the long duration of tamoxifen treatment (6–12 months) that is needed to influence the density of the breast. One small study (n = 42) showed significant mammographic density reduction after 3 months of tamoxifen, but more research to confirm this timing is needed [95]. Moreover, no clear limits of adequate or inadequate mammographic density reduction are known.
The results of the functional test used to determine the efficacy of endocrine treatments by measuring Ki67 after low-dose tamoxifen is probably the most compelling evidence for efficacy of low-dose tamoxifen for invasive breast cancer. Two studies showed this convincingly, although a third study was seemingly in contrast with these findings [87]. Seemingly, since three explanations could be given for these findings. First, a tamoxifen dose of 10 mg/week might be too low to be effective. A subanalysis of patients with a normal CYP2D6 enzymatic function (in contrast to poor or intermediate metabolizers) further supports this theory [87]. In this analysis, in normal CYP2D6 metabolizers, Ki67 did show a significant reduction after administration of tamoxifen 10 mg weekly, likely because patients with a normal CYP2D6 function reach higher endoxifen levels than poor or intermediate metabolizers. Second, the post-treatment breast cancer samples on which the Ki67 was measured were derived from resection material (core cuts). An additional analyses of the POETIC trial showed that in patients who underwent a core biopsy and a resection after a short duration of endocrine therapy preoperatively, the decrease in Ki67 found on core biopsies was not seen on the resection sample [96]. Although further research is needed to clarify these findings, it could have played a role in this study. Finally, as previously mentioned, treating premenopausal patients with low-dose tamoxifen without a GnRH agonist could result in inefficacy of tamoxifen due to the loss of competition with high plasma estradiol levels for the ER.
How can the findings described in this review be applied in the clinical setting for patients with bothersome adverse effects from standard doses of tamoxifen? One approach could be a dose reduction of tamoxifen based on endoxifen levels. For this approach, the precise threshold value for endoxifen, the most active metabolite of tamoxifen, must be known. Previous studies have shown different lower limits ranging between 10 and 16 nM [22,23,24]. Based on linear kinetics, it can be predicted that halving the tamoxifen dose approximately halves the level of endoxifen. If a conservative lower limit for endoxifen of 16 nM is used, a dose reduction can only be safely achieved in patients with an endoxifen level of 32 nM or higher with the standard tamoxifen dose. This seems to be the case for only 30% of patients using tamoxifen at a standard dose of 20 mg [97] (Fig. 2). Although the minimal effective concentration of endoxifen is likely much lower, there is still too little evidence to recommend a safe dose reduction based on a much lower threshold of endoxifen. In addition, the efficacy of tamoxifen is not only dependent on the dose but also on factors such as tamoxifen resistance mechanisms and, importantly, the expression of ER- and PR receptors on the breast tumor cells. Tamoxifen dose reduction based on endoxifen levels alone therefore appears to be an approach that is too limiting, as patient and tumor characteristics are not taken into account enough.
Practical advice for patients receiving treatment. Patients with ER-positive breast cancer who were treated with adjuvant tamoxifen reached steady-state levels of endoxifen after 3 months of treatment. From then on, the endoxifen concentration should be measured at least once. When a patient does not experience (bothersome) adverse effects, the standard dose of tamoxifen 20 mg can be continued if the endoxifen concentration is ≥16 nM. In case a patient experiences bothersome adverse effects, for some patients tamoxifen dose reduction can be considered using the conservative endoxifen threshold of 16 nM. AI aromatase inhibitor, ER+ estrogen receptor-positive. Figure created with Biorender
The use of a functional endocrine sensitivity test could be the fitting solution for individualized tamoxifen dosing in the future. The difference in Ki67 percentage before and after short exposure of tamoxifen treatment preoperatively could serve as an endocrine sensitivity test used on an individual base. This approach incorporates all individual patient and tumor characteristics and could be performed preoperatively without postponing breast cancer treatment. After all, after 2–3 weeks of preoperative treatment, often corresponding to the waiting time until surgery, this test already leads to a result. Since endoxifen only reaches steady-state after 12 weeks, the endoxifen levels reached after 2–3 weeks will be specifically low and therefore useful for tamoxifen dose reduction in the case of adverse effects, when tamoxifen will be administered in the adjuvant setting. Although promising, there are still some challenges that need to be resolved before this test for tamoxifen sensitivity can be routinely used in clinical practice. These include the Ki67 staining on breast cancer cells causing high intra- and intervariability in inexperienced hands, and the fact that demonstration of the inefficacy of tamoxifen at a certain dose has not yet demonstrated the efficacy of a somewhat higher dose. This is likely the reason why, at the moment, this test is mainly used within innovative trials.
5 Conclusions
Our review shows that low-dose tamoxifen has an improved toxicity profile compared with standard-dose tamoxifen. In the primary and secondary chemoprevention settings, low-dose tamoxifen has already proven its clinical efficacy. Although there is growing evidence that a lower dose of tamoxifen may also have antitumor efficacy against ER-positive breast cancers, this cannot yet be translated into a generally accepted lower dose of tamoxifen at which efficacy is guaranteed in the adjuvant setting. Nevertheless, in one-third of patients with unacceptable adverse effects after receiving standard doses of tamoxifen, a dose reduction of tamoxifen can be performed based on endoxifen levels (Fig. 2). For the remaining patients, further development of the functional test based on the Ki67 changes on ER-positive breast cancer after a short preoperatively treatment with tamoxifen is likely of great value.
References
Early Breast Cancer Trialists’ Collaborative Group. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378(9793):771–84.
Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687–717.
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(8):1194–220.
Burstein HJ, Lacchetti C, Anderson H, Buchholz TA, Davidson NE, Gelmon KA, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol. 2019;37(5):423–38.
Gnant M, Fitzal F, Rinnerthaler G, Steger GG, Greil-Ressler S, Balic M, et al. Duration of adjuvant aromatase-inhibitor therapy in postmenopausal breast cancer. N Engl J Med. 2021;385(5):395–405.
Jordan VC. 50th anniversary of the first clinical trial with ICI 46,474 (tamoxifen): then what happened? Endocr Relat Cancer. 2021;28(1):R11–30.
Martinkovich S, Shah D, Planey SL, Arnott JA. Selective estrogen receptor modulators: tissue specificity and clinical utility. Clin Interv Aging. 2014;9:1437–52.
Stearns V, Ullmer L, López JF, Smith Y, Isaacs C, Hayes D. Hot flushes. Lancet. 2002;360(9348):1851–61.
Land SR, Wickerham DL, Costantino JP, Ritter MW, Vogel VG, Lee M, et al. Patient-reported symptoms and quality of life during treatment with tamoxifen or raloxifene for breast cancer prevention. The NSABP study of tamoxifen and raloxifene (STAR) P-2 trial. JAMA. 2006;295(23):2742–51.
Swerdlow AJ, Jones ME, British Tamoxifen Second Cancer Study G. Tamoxifen treatment for breast cancer and risk of endometrial cancer: a case-control study. J Natl Cancer Inst. 2005;97(5):375–84.
Cuzick J, Powles T, Veronesi U, Forbes J, Edwards R, Ashley S, et al. Overview of the main outcomes in breast-cancer prevention trials. Lancet. 2003;361(9354):296–300.
Buijs SM, van Dorst DCH, Kruip MJHA, van den Akker RFP, Cheung KL, Porrazzo R, et al. The interplay between tamoxifen and endoxifen plasma concentrations and coagulation parameters in patients with primary breast cancer. Biomed Pharmacother. 2024;170: 115969.
Boehm DU, Lebrecht A, Eckhardt T, Albrich S, Schmidt M, Siggelkow W, et al. Quality of life and adjuvant tamoxifen treatment in breast cancer patients. Eur J Cancer Care. 2009;18(5):500–6.
Owusu C, Buist DSM, Field TS, Lash TL, Thwin SS, Geiger AM, et al. Predictors of tamoxifen discontinuation among older women with estrogen receptor-positive breast cancer. J Clin Oncol. 2008;26(4):549–55.
Lailler G, Memoli V, Le Bihan BC, Ben Diane M-K, Lauzier S, Mancini J, et al. Five-year adjuvant endocrine therapy adherence trajectories among women with breast cancer: a nationwide french study using administrative data. Clin Breast Cancer. 2021;21(4):e415–26.
Murphy CC, Bartholomew LK, Carpentier MY, Bluethmann SM, Vernon SW. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat. 2012;134(2):459–78.
Bosco-Lévy P, Jové J, Robinson P, Moore N, Fourrier-Réglat A, Bezin J. Persistence to 5-year hormonal breast cancer therapy: a French national population-based study. Br J Cancer. 2016;115(8):912–9.
Mulder TAM, de With M, Del Re M, Danesi R, Mathijssen RHJ, van Schaik RHN. Clinical CYP2D6 genotyping to personalize adjuvant tamoxifen treatment in ER-positive breast cancer patients: current status of a controversy. Cancers (Basel). 2021;13(4):771.
Stearns V, Johnson MD, Rae JM, Morocho A, Novielli A, Bhargava P, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758–64.
Coezy E, Borgna JL, Rochefort H. Tamoxifen and metabolites in MCF7 cells: correlation between binding to estrogen receptor and inhibition of cell growth. Cancer Res. 1982;42(1):317–23.
Mürdter TE, Schroth W, Bacchus-Gerybadze L, Winter S, Heinkele G, Simon W, et al. Activity levels of tamoxifen metabolites at the estrogen receptor and the impact of genetic polymorphisms of phase I and II enzymes on their concentration levels in plasma. Clin Pharmacol Ther. 2011;89(5):708–17.
Helland T, Henne N, Bifulco E, Naume B, Borgen E, Kristensen VN, et al. Serum concentrations of active tamoxifen metabolites predict long-term survival in adjuvantly treated breast cancer patients. Breast Cancer Res. 2017;19(1):125.
Madlensky L, Natarajan L, Tchu S, Pu M, Mortimer J, Flatt SW, et al. Tamoxifen metabolite concentrations, CYP2D6 genotype, and breast cancer outcomes. Clin Pharmacol Ther. 2011;89(5):718–25.
Saladores P, Mürdter T, Eccles D, Chowbay B, Zgheib NK, Winter S, et al. Tamoxifen metabolism predicts drug concentrations and outcome in premenopausal patients with early breast cancer. Pharmacogenomics J. 2015;15(1):84–94.
Groenland SL, van Eerden RAG, Westerdijk K, Meertens M, Koolen SLW, Moes D, et al. Therapeutic drug monitoring based precision dosing of oral targeted therapies in oncology: a prospective multicentre study. Ann Oncol. 2022;33(10):1071–82.
Groenland SL, Verheijen RB, Joerger M, Mathijssen RHJ, Sparreboom A, Beijnen JH, et al. Precision dosing of targeted therapies is ready for prime time. Clin Cancer Res. 2021;27(24):6644–52.
Neven P, Jongen L, Lintermans A, Van Asten K, Blomme C, Lambrechts D, et al. Tamoxifen metabolism and efficacy in breast cancer: a prospective multicenter trial. Clin Cancer Res. 2018;24(10):2312–8.
Sanchez-Spitman A, Dezentjé V, Swen J, Moes DJAR, Böhringer S, Batman E, et al. Tamoxifen pharmacogenetics and metabolism: results from the prospective CYPTAM study. J Clin Oncol. 2019;37(8):636–46.
Braal CL, Beijnen JH, Koolen SLW, Oomen-de Hoop E, Steeghs N, Jager A, et al. Relevance of endoxifen concentrations: absence of evidence is not evidence of absence. J Clin Oncol. 2019;37(22):1980–1.
Jager NG, Koornstra RH, Vincent AD, van Schaik RH, Huitema AD, Korse TM, et al. Hot flashes are not predictive for serum concentrations of tamoxifen and its metabolites. BMC Cancer. 2013;13:612.
Peyrade F, Frenay M, Etienne MC, Ruch F, Guillemare C, François E, et al. Age-related difference in tamoxifen disposition. Clin Pharmacol Ther. 1996;59(4):401–10.
Gallicchio L, Lord G, Tkaczuk K, Danton M, Lewis LM, Lim CK, et al. Association of Tamoxifen (TAM) and TAM metabolite concentrations with self-reported side effects of TAM in women with breast cancer. Breast Cancer Res Treat. 2004;85(1):89–97.
Lorizio W, Wu AHB, Beattie MS, Rugo H, Tchu S, Kerlikowske K, et al. Clinical and biomarker predictors of side effects from tamoxifen. Breast Cancer Res Treat. 2012;132(3):1107–18.
Gradishar WJ, Anderson BO, Balassanian R, Blair SL, Burstein HJ, Cyr A, et al. Breast cancer, version 4.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2018;16(3):310–20.
Visvanathan K, Fabian CJ, Bantug E, Brewster AM, Davidson NE, DeCensi A, et al. Use of endocrine therapy for breast cancer risk reduction: ASCO clinical practice guideline update. J Clin Oncol. 2019;37(33):3152–65.
Allred DC, Anderson SJ, Paik S, Wickerham DL, Nagtegaal ID, Swain SM, et al. Adjuvant tamoxifen reduces subsequent breast cancer in women with estrogen receptor-positive ductal carcinoma in situ: a study based on NSABP protocol B-24. J Clin Oncol. 2012;30(12):1268–73.
Landis-Piwowar KR, Iyer NR. Cancer chemoprevention: current state of the art. Cancer Growth Metastasis. 2014;7:19–25.
DeCensi A, Puntoni M, Guerrieri-Gonzaga A, Caviglia S, Avino F, Cortesi L, et al. Randomized placebo controlled trial of low-dose tamoxifen to prevent local and contralateral recurrence in breast intraepithelial neoplasia. J Clin Oncol. 2019;37(19):1629–37.
de Vries Schultink AHM, Dolro TPC, Madlensky L, Pierce JP, Beijnen JH, Huitema ADR. Prospective evaluation of Therapeutic Drug Monitoring of endoxifen: feasibility of observational and randomized trials. Available online at: www.page-meeting.org/?abstract=9150. 2019.
Eriksson M, Eklund M, Borgquist S, Hellgren R, Margolin S, Thoren L, et al. Low-dose tamoxifen for mammographic density reduction: a randomized controlled trial. J Clin Oncol. 2021;39(17):1899–908.
Hammarström M, Gabrielson M, Crippa A, Discacciati A, Eklund M, Lundholm C, et al. Side effects of low-dose tamoxifen: results from a six-armed randomised controlled trial in healthy women. Br J Cancer. 2023;129(1):61–71.
Decensi A, Robertson C, Viale G, Pigatto F, Johansson H, Kisanga ER, et al. A randomized trial of low-dose tamoxifen on breast cancer proliferation and blood estrogenic biomarkers. J Natl Cancer Inst. 2003;95(11):779–90.
Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women. The women’s health initiative randomized trial. JAMA. 2003;289(24):3243–53.
Decensi A, Gandini S, Serrano D, Cazzaniga M, Pizzamiglio M, Maffini F, et al. Randomized dose-ranging trial of tamoxifen at low doses in hormone replacement therapy users. J Clin Oncol. 2007;25(27):4201–9.
DeCensi A, Bonanni B, Maisonneuve P, Serrano D, Omodei U, Varricchio C, et al. A phase-III prevention trial of low-dose tamoxifen in postmenopausal hormone replacement therapy users: the HOT study. Ann Oncol. 2013;24(11):2753–60.
Pruthi S, Heisey RE, Bevers TB. Chemoprevention for breast cancer. Ann Surg Oncol. 2015;22(10):3230–5.
Buttiron Webber T, Marra D, Puntoni M, Giuliano S, Briata IM, Cevasco I, et al. Patient- versus physician-reported outcomes in a low-dose tamoxifen trial in noninvasive breast cancer. Breast J. 2021;27(11):817–23.
Decensi A, Robertson C, Guerrieri-Gonzaga A, Serrano D, Cazzaniga M, Mora S, et al. Randomized double-blind 2 X 2 trial of low-dose tamoxifen and fenretinide for breast cancer prevention in high-risk premenopausal women. J Clin Oncol. 2009;27(23):3749–56.
Serrano D, Gandini S, Guerrieri-Gonzaga A, Feroce I, Johansson H, Macis D, et al. Quality of life in a randomized breast cancer prevention trial of low-dose tamoxifen and fenretinide in premenopausal women. Cancer Prev Res. 2018;11(12):811–8.
Bhatia S, Palomares MR, Hageman L, Chen Y, Landier W, Smith K, et al. A randomized Phase IIb study of low-dose tamoxifen in chest-irradiated cancer survivors at risk for breast cancer. Clin Cancer Res. 2021;27(4):967–75.
Lee CI, Fox P, Balakrishnar B, Balleine RL, Gao B, Provan P, et al. Tamoxifen-induced severe hot flashes and endoxifen levels: is dose reduction a safe and effective strategy? Breast. 2019;46:52–7.
Buijs SM, Hoop EO, Braal CL, van Rosmalen MM, Drooger JC, van Rossum-Schornagel QC, et al. The impact of endoxifen-guided tamoxifen dose reductions on endocrine side-effects in patients with primary breast cancer. ESMO Open. 2023;8(1): 100786.
Fallowfield LJ, Leaity SK, Howell A, Benson S, Cella D. Assessment of quality of life in women undergoing hormonal therapy for breast cancer: validation of an endocrine symptom subscale for the FACT-B. Breast Cancer Res Treat. 1999;55(2):189–99.
Fisher B, Costantino JP, Redmond CK, Fisher ER, Wickerham DL, Cronin WM. Endometrial cancer in tamoxifen-treated breast cancer patients: findings from the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-14. J Natl Cancer Inst. 1994;86(7):527–37.
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381(9869):805–16.
Bernstein L, Deapen D, Cerhan JR, Schwartz SM, Liff J, McGann-Maloney E, et al. Tamoxifen therapy for breast cancer and endometrial cancer risk. J Natl Cancer Inst. 1999;91(19):1654–62.
Runowicz CD, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Ford LG, et al. Gynecologic conditions in participants in the NSABP breast cancer prevention study of tamoxifen and raloxifene (STAR). Am J Obstet Gynaecol. 2011;205(6):535.
Cohen I, Bernheim J, Azaria R, Tepper R, Sharony R, Beyth Y. Malignant endometrial polyps in postmenopausal breast cancer tamoxifen-treated patients. Gynecol Oncol. 1999;75(1):136–41.
Guerrieri-Gonzaga A, Sestak I, Lazzeroni M, Serrano D, Rotmensz N, Cazzaniga M, et al. Benefit of low-dose tamoxifen in a large observational cohort of high risk ER positive breast DCIS. Int J Cancer. 2016;139(9):2127–34.
Guerrieri-Gonzaga A, Lazzeroni M, Botteri E, Serrano D, Rotmensz N, Varricchio MC, et al. Effect of low-dose tamoxifen after surgical excision of ductal intraepithelial neoplasia: results of a large retrospective monoinstitutional cohort study. Ann Oncol. 2013;24(7):1859–66.
Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90(18):1371–88.
Cuzick J, Forbes JF, Sestak I, Cawthorn S, Hamed H, Holli K, et al. Long-term results of tamoxifen prophylaxis for breast cancer–96-month follow-up of the randomized IBIS-I trial. J Natl Cancer Inst. 2007;99(4):272–82.
Saphner T, Tormey DC, Gray R. Venous and arterial thrombosis in patients who received adjuvant therapy for breast cancer. J Clin Oncol. 1991;9(2):286–94.
Deitcher SR, Gomes MP. The risk of venous thromboembolic disease associated with adjuvant hormone therapy for breast carcinoma: a systematic review. Cancer. 2004;101(3):439–49.
Amir E, Seruga B, Niraula S, Carlsson L, Ocaña A. Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis. J Natl Cancer Inst. 2011;103(17):1299–309.
Hernandez RK, Sørensen HT, Pedersen L, Jacobsen J, Lash TL. Tamoxifen treatment and risk of deep venous thrombosis and pulmonary embolism: a Danish population-based cohort study. Cancer. 2009;115(19):4442–9.
Lazzeroni M, Puntoni M, Guerrieri-Gonzaga A, Serrano D, Boni L, Buttiron Webber T, et al. Randomized placebo controlled trial of low-dose tamoxifen to prevent recurrence in breast noninvasive neoplasia: a 10-year follow-up of TAM-01 study. J Clin Oncol. 2023;41(17):3116–21.
Eisenberger A, Westhoff C. Hormone replacement therapy and venous thromboembolism. J Steroid Biochem Mol Biol. 2014;142:76–82.
Guerrieri-Gonzaga A, Botteri E, Rotmensz N, Bassi F, Lntra M, Serrano D, et al. Ductal intraepithelial neoplasia: Postsurgical outcome for 1,267 women cared for in one single institution over 10 years. Oncologist. 2009;14(3):201–12.
Nazari SS, Mukherjee P. An overview of mammographic density and its association with breast cancer. Breast Cancer. 2018;25(3):259–67.
Boyd NF, Byng JW, Jong RA, Fishell EK, Little LE, Miller AB, et al. Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst. 1995;87(9):670–5.
McCormack VA, dos Santos SI. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev. 2006;15(6):1159–69.
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356(3):227–36.
Martin LJ, Boyd NF. Mammographic density. Potential mechanisms of breast cancer risk associated with mammographic density: hypotheses based on epidemiological evidence. Breast Cancer Res. 2008;10(1):201.
Cuzick J, Warwick J, Pinney E, Warren RM, Duffy SW. Tamoxifen and breast density in women at increased risk of breast cancer. J Natl Cancer Inst. 2004;96(8):621–8.
Cuzick J, Warwick J, Pinney E, Duffy SW, Cawthorn S, Howell A, et al. Tamoxifen-induced reduction in mammographic density and breast cancer risk reduction: a nested case-control study. J Natl Cancer Inst. 2011;103(9):744–52.
Li J, Humphreys K, Eriksson L, Edgren G, Czene K, Hall P. Mammographic density reduction is a prognostic marker of response to adjuvant tamoxifen therapy in postmenopausal patients with breast cancer. J Clin Oncol. 2013;31(18):2249–56.
Osborne CK. Tamoxifen in the treatment of breast cancer. N Engl J Med. 1998;339(22):1609–18.
Nielsen TO, Leung SCY, Rimm DL, Dodson A, Acs B, Badve S, et al. Assessment of Ki67 in breast cancer: updated recommendations from the international Ki67 in breast cancer working group. J Natl Cancer Inst. 2020;113(7):808–19.
Uxa S, Castillo-Binder P, Kohler R, Stangner K, Müller GA, Engeland K. Ki-67 gene expression. Cell Death Differ. 2021;28(12):3357–70.
Smith I, Robertson J, Kilburn L, Wilcox M, Evans A, Holcombe C, et al. Long-term outcome and prognostic value of Ki67 after perioperative endocrine therapy in postmenopausal women with hormone-sensitive early breast cancer (POETIC): an open-label, multicentre, parallel-group, randomised, phase 3 trial. Lancet Oncol. 2020;21(11):1443–54.
Dowsett M, Ebbs SR, Dixon JM, Skene A, Griffith C, Boeddinghaus I, et al. Biomarker changes during neoadjuvant anastrozole, tamoxifen, or the combination: influence of hormonal status and HER-2 in breast cancer—a study from the IMPACT trialists. J Clin Oncol. 2005;23(11):2477–92.
Dowsett M, Smith IE, Ebbs SR, Dixon JM, Skene A, Griffith C, et al. Short-term changes in Ki-67 during neoadjuvant treatment of primary breast cancer with anastrozole or tamoxifen alone or combined correlate with recurrence-free survival. Clin Cancer Res. 2005;11(2 Pt 2):951s-s958.
Nitz U, Gluz O, Kreipe HH, Christgen M, Kuemmel S, Baehner FL, et al. The run-in phase of the prospective WSG-ADAPT HR+/HER2- trial demonstrates the feasibility of a study design combining static and dynamic biomarker assessments for individualized therapy in early breast cancer. Therapeutic Adv Med Oncol. 2020;12:1758835920973130.
Harbeck N, Nitz UA, Christgen M, Kümmel S, Braun M, Schumacher C, et al. De-escalated neoadjuvant trastuzumab-emtansine with or without endocrine therapy versus trastuzumab with endocrine therapy in HR+/HER2+ early breast cancer: 5-year survival in the WSG-ADAPT-TP trial. J Clin Oncol. 2023;41(22):3796–804.
de Sousa JA, Facina G, da Silva BB, Gebrim LH. Effects of low-dose tamoxifen on breast cancer biomarkers Ki-67, estrogen and progesterone receptors. Int Seminars Surg Oncol. 2006. https://doi.org/10.1186/1477-7800-3-29.
Serrano D, Lazzeroni M, Gandini S, Macis D, Johansson H, Gjerde J, et al. A randomized phase II presurgical trial of weekly low-dose tamoxifen versus raloxifene versus placebo in premenopausal women with estrogen receptor-positive breast cancer. Breast Cancer Res. 2013. https://doi.org/10.1186/bcr3439.
Kisanga ER, Gjerde J, Guerrieri-Gonzaga A, Pigatto F, Pesci-Feltri A, Robertson C, et al. Tamoxifen and metabolite concentrations in serum and breast cancer tissue during three dose regimens in a randomized preoperative trial. Clin Cancer Res. 2004;10(7):2336–43.
Bychkovsky B, Laws A, Katlin F, Hans M, Knust Graichen M, Pace LE, et al. Initiation and tolerance of chemoprevention among women with high-risk breast lesions: the potential of low-dose tamoxifen. Breast Cancer Res Treat. 2022;193(2):417–27.
Patel R, Jin C, Tiersten A. Low-dose tamoxifen for breast cancer prevention in patients with ductal carcinoma in situ (DCIS) and atypical lesions: a real-world experience. J Clin Oncol. 2022;40(16): e12537.
Zhao H, Hei N, Wu Y, Chan W, Lei X, Cameron C, et al. Initiation of and adherence to tamoxifen and aromatase inhibitor therapy among elderly women with ductal carcinoma in situ. Cancer. 2017;123(6):940–7.
Ravdin PM, Fritz NF, Tormey DC, Jordan VC. Endocrine status of premenopausal node-positive breast cancer patients following adjuvant chemotherapy and long-term tamoxifen. Cancer Res. 1988;48(4):1026–9.
De Censi A, Puntoni M, Guerrieri-Gonzaga A, Caviglia S, Avino F, Cortesi L, et al. Effect modifiers in a randomized phase III trial of low-dose tamoxifen in breast preinvasive disease. J Clin Oncol. 2019;37(15):1500.
Burton A, Maskarinec G, Perez-Gomez B, Vachon C, Miao H, Lajous M, et al. Mammographic density and ageing: a collaborative pooled analysis of cross-sectional data from 22 countries worldwide. PLoS Med. 2017;14(6): e1002335.
Bäcklund M, Eriksson M, Hammarström M, Thoren L, Bergqvist J, Margolin S, et al. Time to mammographic density decrease after exposure to tamoxifen. Oncologist. 2022;27(7):e601–3.
Bliss JM. Polychemotherapy for early breast cancer: results from the international adjuvant breast cancer chemotherapy randomized trial. J Natl Cancer Inst. 2007;99(7):506–15.
Braal CL, Jager A, Oomen-de Hoop E, Westenberg JD, Lommen K, de Bruijn P, et al. Therapeutic drug monitoring of endoxifen for tamoxifen precision dosing: feasible in patients with hormone-sensitive breast cancer. Clin Pharmacokinet. 2022;61(4):527–37.
Acknowledgments
The authors wish to thank Elise Krabbendam, Christa Niehot and Wichor Bramer from the Erasmus MC Medical Library, Rotterdam, for developing and updating the search strategies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflicts of Interests
Sanne M. Buijs, Stijn L.W. Koolen, Ron H.J. Mathijssen, and Agnes Jager declare they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Author contributions
All authors were involved in conceptualization of the review. SB performed the literature review and wrote the first draft. All authors were involved in critical revision of the data and approval of the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Buijs, S.M., Koolen, S.L.W., Mathijssen, R.H.J. et al. Tamoxifen Dose De-Escalation: An Effective Strategy for Reducing Adverse Effects?. Drugs 84, 385–401 (2024). https://doi.org/10.1007/s40265-024-02010-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-024-02010-x