Abstract
Introduction
Although relevant for precision pharmacovigilance, there are conflicting data on whether former preterm birth is associated with QTc-Bazett prolongation in later life.
Methods
To explore QTc-Bazett interval differences between former preterm and/or extremely low birth weight (ELBW) cases and term-born controls in adolescence and young adulthood, we analyzed pooled individual data after a structured search on published cohorts. To test the absence of a QTc-Bazett difference, a non-inferiority approach was applied (one-sided, upper limit of the 95% confidence interval [CI] mean QTc-Bazett difference, 5 and 10 ms). We also investigated the impact of characteristics, either perinatal or at assessment, on QTc-Bazett in the full dataset (cases and controls). Data were reported as median and range.
Results
The pooled dataset contained 164 former preterm and/or ELBW (cases) and 140 controls born full-term from three studies. The median QTc-Bazett intervals were 409 (335–490) and 410 (318–480) ms in cases and controls. The mean QTc-Bazett difference was 1 ms, with an upper 95% CI of 6 ms (p > 0.05 and p < 0.01 for 5 and 10 ms, respectively). In the full dataset, females had a significantly longer QTc-Bazett than males (415 vs. 401 ms; p < 0.0001).
Conclusions
QTc-Bazett intervals are not significantly different between former preterm and/or ELBW cases and term-born controls, and we rejected a potential prolongation > 10 ms in cases. When prescribing QTc-prolonging drugs, pharmacovigilance practices in this subpopulation should be similar to the general public (NCT05243537).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There are conflicting data on whether former preterm birth is associated with a prolonged QTc-Bazett interval in later life. We therefore analyzed a pooled dataset of published case-control studies. |
The pooled dataset contained 164 very preterm or extremely low birth weight (ELBW, < 1 kg) cases and 140 term-born controls from three studies. The mean QTc-Bazett intervals were not significantly different between former preterm subjects and/or ELBW and term-born controls (409 vs. 410 ms). A potential QTc-Bazett prolongation > 10 ms in cases was rejected. |
Consequently, when prescribing QTc-prolonging drugs, pharmacovigilance practices in this subpopulation should be similar to those applied in the general public. |
1 Introduction
Preterm birth is the primary cause of neonatal mortality [1]. Cardiovascular issues affect preterm infants during neonatal life and afterwards. Elevated blood pressure, changes in heart structure and function, or impaired vascular growth are consequences of preterm birth [2,3,4]. Former preterm subjects still have a higher overall mortality risk in infancy, childhood, and even early adulthood, including sudden death [5]. Despite these findings, the association between preterm birth and cardiac conduction or repolarization abnormalities in later life has been investigated less often, and associations with established cardiovascular risk factors are poorly explored [4, 5]. Such abnormalities may provide a mechanistic explanation for the higher mortality and may facilitate precision screening and prevention, including pharmacovigilance [4,5,6].
Bassareo et al. (Italy) reported that a heart rate-corrected QT time according to the Bazett formula (QTc-Bazett) in former extremely low birth weight (ELBW) infants in young adulthood (mean age 23 years) was at the upper limit of the normal range and correlated with gestational age. Relevant for precision pharmacovigilance, Bassareo et al. observed a significant difference in mean QTc-Bazett time (417 vs. 369.9 ms) between former ELBW cases and controls [7]. On the contrary, neither Gervais et al. (Canada) nor Salaets et al. (Belgium) confirmed these differences in former preterm subjects in young adulthood and late childhood to adolescence, respectively [8, 9]. More clarity on the presence or absence of a difference in QTc-Bazett is relevant for precision pharmacovigilance, as certain QTc-prolonging drugs, such as antipsychotics or attention deficit and hyperactivity disorder (ADHD) drugs, are more commonly prescribed in former premature infants [10, 11].
Therefore, the primary aim of this study was to explore potential differences in QTc-Bazett intervals between former preterm and/or ELBW cases and term-born healthy controls by pooling individual data as published. On a second level, we explored the impact of covariates on the QTc-Bazett intervals in cases and controls.
2 Methods
2.1 Ethics, Study Registration, and Data Handling
The Ethics Committee Research of University Hospitals Leuven approved the study protocol (7 January 2022; S66020) and the study was registered at ClinicalTrials.gov (NCT05243537). When not available, individual data extracted from figures or tables in the source document using a web-based, valid extraction program (WebPlotDigitizer) was our second option, be that this commonly results in a more restricted dataset [12].
2.2 Search Strategy
Two authors (JV, MVP) conducted a search for relevant articles using PubMed Advanced to retrieve case-control cohorts in November 2021. Following internal discussion, it was agreed to use ‘(long) QT’ and ‘preterm’ as search terms. Based on the aims of this study, papers had to report on QTc data in such cohorts after neonatal stay, and had to report on more than one specific covariate. Retained papers were checked for potential additional relevant references or citations (electronic supplementary material [ESM] Table S1).
2.3 Quality Assessment
Quality assessment was performed in the retained articles, applying the Scottish Intercollegiate Guidelines Network (SIGN) methodology checklist for case-control studies [13]. The SIGN questionnaire contains 15 questions rating aspects on internal validity (selection of subjects, assessment, confounding, statistical analysis) and overall assessment. When the majority of criteria are met and results are unlikely to be changed by further research, this is classified as high quality (++); when most criteria are met, with some flaws in the study with an associated risk of bias, and conclusions may change in the light of further studies, this is classified as acceptable (+); and when most criteria were not met or significant flaws related to key aspects of the study design, so that conclusions are likely to change in the light of further studies, this is classified as low quality [13]. This effort was made to provide transparency on the quality (risk of bias) of the studies retained. Two authors (JV, MVP) individually completed the SIGN questionnaire. In the event of discrepancy for a given question, a third author (KA) also assessed the paper to find consensus.
2.4 Primary Outcome
QTc-Bazett obtained at rest was chosen as the primary outcome measure. The Bazett formula (QTc-Bazett = QT/√RR) was used for heart rate correction.
2.5 Statistical Analysis
Descriptive statistics are presented as median (range) for continuous variables, or frequency (%) for categorical variables. For the comparison of QTc-Bazett intervals between preterm and/or ELBW cases and term-born controls, a non-inferiority approach was followed. This approach aims to test the null hypothesis that the mean QTc-Bazett is prolonged in cases, compared with controls, by a clinically relevant margin. For the primary analysis, a non-inferiority margin of 5 ms was considered, based on the US Food and Drug Administration (FDA) and European Medicines Agency (EMA) paired study guidelines as the most stringent criteria for positive control effects [14, 15]. In a post hoc analysis (after publication of the protocol on the ClinicalTrials.gov website), we also considered 10 ms as another non-inferiority margin because a 10 ms margin better reflects the clinically relevant margin, as the International Conference on Harmonisation (ICH) E14 guidelines define a negative ‘thorough QT/QTc study’ as the one in which the upper bound of the 95% one-sided confidence interval (CI) for the largest time-matched mean effect of the drug on the QTc interval excludes 10 ms [15].
The analysis was performed by estimating the upper limit of a one-sided 95% CI around the difference in means (cases to controls) using a pooled variance t-test, and non-inferiority was demonstrated if the upper limit falls below the non-inferiority margin.
Comparative statistical analyses were used (Spearman’s rank, Mann–Whitney U, or t-test) to explore associations of QTc-Bazett measurements to characteristics, either perinatal or at assessment.
Analyses were performed using SAS® software (version 9.4, SAS System for Windows; SAS Institute, Inc., Cary, NC, USA) or MedCalc® (version 20.111; MeldCalc Software Ltd, Ostend, Belgium). A p-value < 0.05 was considered to be statistically significant.
3 Results
3.1 Search Results
Based on the search strategy described, a limited number of papers were retrieved (25 for ‘long QT and preterm’), of which we retained three articles [7,8,9]. Twenty-two papers were not retained because they were reviews (n = 2), case reports or clinical observations on congenital long QT (either maternal, fetal, or neonatal; n = 13), drug-related observations during neonatal care (cisapride, 4; erythromycin, 1; serotonin reuptake inhibitors, 1), or related to car seating in former preterm subjects (n = 1) (ESM Table S1). Further efforts (‘QT and preterm’), references, or citation tracking (snowball and citation search) did not provide additional documents.
3.2 Quality Assessment
Using the SIGN approach, two papers (Salaets et al. [9] and Gervais et al. [8]) were classified as ‘high quality’. The study by Bassareo et al. did not meet these criteria due to uncertainties on the representation of the population (marked difference in sex distribution, with 20/24 females in both cases and controls) and on the blinding procedures, and was hence classified as having ‘low quality’ [7]. The final consensus assessment is provided in ESM Table S2.
3.3 Data Acquisition, Cohort and Study Characteristics
Reaching out to the corresponding authors resulted in data sharing and access to two of three cohorts (Salaets et al., 93 cases, 87 controls; Gervais et al., 47 cases, 53 controls) for the individual QTc-Bazett and related characteristics [7,8,9]. Despite repeated attempts, we failed to receive any response from the Bassareo et al. study team [7]; however, based on the figures provided in the paper by Bassareo et al., we were able to extract raw individual data on QTc-Bazett intervals and gestational age in the 24 cases. Based on the information in the public domain, we were unable to link this to either their birth weight or sex, and neither could we extract raw individual data in the 24 controls [12].
Gervais et al. characterized cases as born preterm (< 30 weeks gestational age). Controls were term-born with a birth weight >2500 g, and were matched for age (at assessment) and sex. Controls were either friends or siblings of the preterm cases or found through advertising. The mean age at assessment was 23.9 years [8]. Similarly, Salaets et al. defined cases as preterm-born children (gestational age of 23–33 weeks) born with a birth weight of ≤ 1000 g (ELBW). Controls were either term-born friends of the cases or were recruited from an elementary school nearby the research center (Hamont Achel, Belgium). The median age at assessment was 11 (8–14) years [9]. Bassareo et al. recruited former ELBW cases and controls as healthy, term-born subjects, matched for sex, age and body mass index (BMI). Furthermore, all subjects were contacted in alphabetical order from the records of the Neonatal Intensive Care Unit of the University of Cagliari. The mean age at assessment was 23.2 years [7].
In the Gervais cohort, continuous 12-lead ECG (GE Case Stress System V6.5 and 6.73, GE Medical Systems Information Technologies GmbH, Freiburg, Germany) was recorded at a speed of 25 mm/s. The ECG of participants at rest was manually analyzed. Tracings were scanned and measurements were performed using the magnifier and ruler function of Adobe Photoshop (version 19.1.6; Adobe Systems, San Jose, CA, USA) by two trained operators blinded to the exposure status, under the supervision of a staff cardiologist. Intraobserver correlation, assessed on a subset of 24 QTc measurements performed twice on separate days, was very good, with an intraclass correlation coefficient of 0.94. Three measurements were taken in lead DII or V5 on three QRS complexes, and averaged [8].
In the Salaets cohort, a 12-lead ECG was collected at rest after 30 min in the supine position by a trained assistant. As a quality control measure, research assistants received periodical training on skin preparation, electrode placement, and positioning of the participants. The Cardiax® device (RDSM Medical Devices, Hasselt, Belgium) was used for ECG acquisition and automatic determination of standard ECG parameters on the digital traces, thereby excluding observer-related bias. PR and QT intervals, QRS duration, and QRS were automatically measured to the nearest 1 ms (they were not calculated manually). Based on visual inspection of printouts, the quality of the ECGs used for analysis was assessed by one assessor, blinded for group allocation [9].
Although not explicitly mentioned, Bassareo et al. did not specify in which state the ECGs were taken, but we indirectly understood—based on an additional letter—that the Bassareo et al. data were also collected at rest [7, 16]. For additional details on the individual cohorts, including the equipment used and automatic versus manual measurements, we refer to the initial papers and related letters as published source documents [7,8,9, 16, 17].
After pooling, the final cohort was based on 164 ELBW and/or preterm cases and 140 healthy, term-born controls. Table 1 describes the characteristics (either perinatal or at assessment [ECG related or biochemical findings]) of the pooled study population. The heart rate at rest in the pooled dataset was 78 (48–161) and 72 (49–129) in the cases and controls, respectively (p > 0.05). Differences in clinical characteristics (shorter, lower weight, BMI) and blood pressure between cases and controls confirmed the previously reported differences in clinical characteristics [8, 9].
While there was no information on QT-prolonging medications in the Bassareo et al. cohort [7], asthma medicines (9 vs. 2 cases vs. controls), or psychiatry/ADHD (8 vs. 3) or any QTC-prolonging medicines (11 vs. 2) were more commonly used in former preterm-born adults in the Gervais cohort [8]. In the Salaets cohort, eight medicines in four ELBW cases and four controls were reported to be associated with QTc prolongation (inhaled formoterol [n = 2] or oral methylphenidate [n = 6]) [9]. For both cohorts, the impact of these drugs on the QTc interval was not significant, as reported in the individual papers [8, 9].
3.4 Comparison of the QTc-Bazett Interval Between Cases and Controls
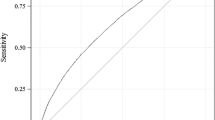
In the analysis of the pooled individual QTc-Bazett observations, there was no statistical difference between cases and controls upon superiority testing (cases to controls: 409 vs. 410 ms; p > 0.05) (Table 1, Fig. 1). For QTc-Bazett, we observed a mean difference between cases and controls of 1 ms (95% upper CI limit 6 ms). This means that the upper limit does not fall below the initially set non-inferiority margin of 5 ms (p > 0.05). However, the upper limit does fall below the clinically relevant non-inferiority margin of 10 ms (p < 0.01, post hoc analysis).
3.5 Covariate Analysis of QTc-Bazett in the Pooled Dataset of Cases and Controls
In the covariate analysis, we did not observe any significant association between QTc-Bazett and birth weight or gestational age (perinatal characteristics). The same holds true for age, height, weight, BMI, systolic and diastolic blood pressure (clinical characteristics at assessment), or sodium, potassium or calcium (biochemical findings). The mean QTc-Bazett was significantly higher in female subjects compared with male subjects (415 vs. 401 ms; p < 0.0001). There was also a significant correlation (Spearman’s rank 0.151; p < 0.05) between QTc-Bazett and phosphate level.
4 Discussion
In an effort to pool individual data of published cohorts, we observed no significant differences in the QTc-Bazett time interval between former ELBW and/or preterm-born cases and term-born controls in late childhood, adolescence, and young adulthood. Applying a one-sided non-inferiority approach, a difference of > 10 ms (but not > 5 ms) in former ELBW and/or preterm subjects was hereby excluded. The absence of a significant correlation between QTc-Bazett and birth weight or gestational age in the covariate analysis provides further support for the absence of a relevant QTc-Bazett prolongation in former ELBW and/or preterm subjects. At assessment, sex (female to male, 415 to 401 ms) was a strong covariate, while phosphate levels were a weak (Spearman 0.151, p < 0.05) covariate of the QTc-Bazett time interval. Both can be expected, as it is generally known that both sex and electrolytes, including calcium/phosphate balance, have been reported as significant covariates of the QTc-Bazett time interval, as also reflected in the FDA guidance and EMA guidelines [14, 15, 18]. Although evidence is inconsistent, a higher BMI in adults was associated with a longer QTc-Bazett in some studies [19, 20]. In the current pooled dataset, this was not the case.
Our main motivation was driven by targeted or precision pharmacovigilance, as certain QT-prolonging drugs, such as antipsychotics or drugs used to treat ADHD, are more commonly prescribed in former preterm subjects [10, 11]. As these drugs are associated with prolongation of the QTc-Bazett interval, the absence of any a priori prolongation in former ELBW and/or preterm subjects matters. In essence, these findings support the statement that pharmacovigilance procedures in this subpopulation should be similar to the general public, and that additional precautions or precision pharmacovigilance on this topic are obsolete. Obviously, there are limitations to our study and reporting.
First, we only had partial access (cases only, and individual QTc-Bazett values only linked gestational age, not birth weight) to the first case-control study (24 cases and 24 controls) [7], and assessed the quality of this case-control study to be poorer compared with the two other cohorts [8, 9]. Despite these limitations, we decided to retain these data in cases in the pooled analysis as the Bassareo et al. cohort was the only study that reported on a prolonged QTc-Bazett time interval in former ELBW cases [7]. Our approach also limited the use of other QTc formulae, despite the FDA recommendations to explore different formulae, because the best correction factor remains controversial, and the problems with Bazett QTc correction in pediatric screening for prolonged QTc [14, 21].
Second, in our initial study protocol (ClinicalTrials.gov NCT05243537), we defined non-inferiority using an upper limit of 5 ms, based on our initial understanding of the FDA guidance and the EMA paired guidelines on the paired study design [14, 15]. However, this is a very stringent criterion that we did not meet. A post hoc power analysis based on our pooled data distribution determined that we would need a very large sample size of 1160 subjects to document the absence of a difference 5 ms in a non-inferiority study (with a power of 80% and a significance level of 5%). Regulatory guidance indeed considers a 5 ms increase in QT/QTc to be of clinical relevance in drug trials and sets this as the threshold for a ‘thorough QT/QTc study’, but does not recommend a non-inferiority approach using 5 ms as the maximal upper limit of the 95% CI. In order to exclude a relevant increase in QT/QTc as reliable and feasible, regulatory authorities define a negative ‘thorough QT/QTc study’ as one in which the upper bound of the 95% one-sided CI for the largest time-matched mean effect of the drug on the QTc interval excludes 10 ms. This 10 ms criterion is very reasonable as a clinical target, as also recently suggested [3]. Thus, our post hoc analysis, using a cut-off of 10 ms—to show non-inferiority of the former preterm-born subjects to controls with regard to QTc-Bazett—is in line with regulatory guidance and excludes this 10 ms cut-off.
Finally, most participants included in our study design had a Caucasian background and all were recruited in Italy, Canada, and Belgium. Although research on inter-ethnic differences in baseline QTc intervals is limited, the available data suggest that there is no relevant difference in QTc time intervals related to ethnicity, while the FDA guidance and EMA guideline also state that it is not expected that clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs would be affected by ethnic factors [14, 15].
5 Conclusions
There was no significant difference in the QTc-Bazett interval between preterm and/or ELBW cases and term-born controls at late childhood/adolescence and young adulthood, and a potential prolongation in QTc-Bazett interval of > 10 ms was rejected. When prescribing QTc-prolonging drugs, pharmacovigilance practices in this subpopulation should be similar to the general public.
References
World Health Organization. Data platform. Maternal, Newborn, Child and Adolescent Health and Ageing. https://platform.who.int/data/maternal-newborn-child-adolescent-ageing/maternal-and-newborn-data/maternal-and-newborn---mortality-causes-of-death. Accessed 4 June 2023.
Nuyt AM, Lavoie JC, Mohamed I, Paquette K, et al. Adult consequence of extremely preterm birth: cardiovascular and metabolic diseases. Risk factors, mechanisms, and prevention avenues. Clin Perinatol. 2017;44:315–32.
Kumar VHS. Cardiovascular morbidities in adults born preterm: getting to the heart of the matter! Children. 2022;9:1843.
Flahault A, Paquette K, Fernandes RO, et al. Increased incidence by lack of association between cardiovascular risk factors in adults born preterm. Hypertension. 2020;75:796–805.
Crump C. Adult mortality after preterm birth-time to translate findings into clinical practice. JAMA Netw Open. 2021;4: e2033361.
Malik M. Conundrum of clinical QTc monitoring. Drug Saf. 2022;45:1011–4.
Bassareo PP, Fanos V, Puddu M, et al. Significant QT interval prolongation and long QT in young adult ex-preterm newborns with extremely low birth weight. J Matern Fetal Neonatal Med. 2011;24:1115–8.
Gervais AS, Flahault A, Chan T, et al. Electrocardiographic features at rest and during exercise in young adults born preterm below 30 weeks of gestation. Pediatr Res. 2020;88:305–11.
Salaets T, Raaijmakers A, Zhang ZY, et al. QTc intervals are not prolonged in former ELBW infants at pre-adolescent age. Pediatr Res. 2022;92:848–52.
Bachmann CS, Risnes K, Bjørngaard JH, et al. Relative age and psychotropic drug use in preterm and term-born children and young adults. Pediatrics. 2022;150: e2022057085.
Bachmann CS, Risnes K, Bjørngaard JH, et al. Psychotropic drugs in adolescence and young adulthood. JAMA Netw Open. 2021;4: e2114420.
Rohatgi A. WebPlotDigitizer Web based tool to extract data from plots, images and maps. https://automeris.io/WebPlotDigitizer. Accessed 4 June 2023.
Healthcare Improvement Scotland. The Scottish Intercollegiate Guidelines Network (SIGN). https://www.sign.ac.uk/what-we-do/methodology/checklists. Accessed 4 June 2023.
United States, Food and Drug Administration. Guidance for Industry; E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs. 2005. https://www.fda.gov/files/drugs/published/E14-Clinical-Evaluation-of-QT-QTc-Interval-Prolongation-and-Proarrhythmic-Potential-for-Non-Antiarrhythmic-Drugs.pdf. Accessed 4 June 2023.
European Medicines Agency. ICH E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs—scientific guideline, 2020. https://www.ema.europa.eu/en/ich-e14-clinical-evaluation-qt-qtc-interval-prolongation-proarrhythmic-potential-non-antiarrhythmic. Accessed 4 Jun 2023.
Bassareo PP, Fanos V, Mercuro G. Young adults born preterm below 30 weeks of gestation and risk of QT tract prolongation. Pediatr Res. 2020;88:143.
Flahault A, Nuyt AM. Author’s response regarding manuscript entitled “Electrographic features at rest and during exercise in young adults born preterm below 30 weeks of gestation’ and subsequent correspondence. Pediatr Res. 2020;88:151–2.
Vink AS, Clur SA, Wilde AA, et al. Effect of age and gender on the QTc-interval in healthy individuals and patients with long-QT syndrome. Trends Cardiovasc Med. 2018;28:64–75.
Waheed S, Dawn B, Gupta K. Association of corrected QT interval with body mass index, and the impact of this association on mortality: results from the Third National Health and Nutrition Examination Survey. Obs Res Clin Pract. 2017;11:426–34.
Jayanthi R, Girijasivam SP, Gaur A. Association of blood pressure and BMI to corrected QT interval in young adults. Can J Physiol Pharmacol. 2021;99:894–9.
Andrsova I, Hnatkova K, Helanova K, et al. Problems with Bazett QTc correction in paediatric screening of prolonged QTc interval. BMC Pediatr. 2020;20:558.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
TS is supported by the Frans Van de Werf Fund for Clinical Cardiovascular Research for his research fellowship (2022 recipient), and V.Z.W. ‘De Kleine Hartjes’ and F.W.O. Vlaanderen. The PREMATCH study was supported by the Agency for Innovation by Science and Technology in Flanders (IWT) through the SAFE-PEDRUG project [IWT/SBO 130033]. KU Leuven Internal Funds (STG-18–00379) supported the Research Unit Hypertension and Cardiovascular Epidemiology, Department of Cardiovascular Sciences, Leuven. The research activities of AS are supported by the Clinical Research and Education Council of the University Hospitals, Leuven.
Conflict of interest
Jill Vanthienen, Marine Vassilev Petrov, Thuy Mai Luu, Anik Cloutier, Anke Raaijmakers, Jan A. Staessen, Zhenyu Zhang, Thomas Salaets, Annouschka Laenen, Anne Smits, Anne-Monique Nuyt, Adrien Flahault, and Karel Allegaert have no conflicts of interest to declare that are directly relevant to the contents of this study.
Ethics approval
The Ethics Committee Research (EC Research) of University Hospitals Leuven (UZ Leuven) approved the study protocol for the pooled analysis (7 January 2022; S66020). The Ethics Committee of CHU Sainte-Justine and the Université de Montréal also approved the study protocol for the pooled analysis (26 January 2022; reference number 2022-3773).
Consent to participate
All data pooled in this study have been previously published. These initial studies and sources were conducted following Ethics Committee approval at the individual institutes and following informed consent and, if applicable, assent.
Consent to publish
Not applicable.
Availability of data materials
The corresponding author can be contacted to share the raw data based on reasonable request and a study protocol. The individual study groups remain the sole owner and controller of their datasets.
Code availability
Not applicable.
Authors’ contributions
Conceptualization: AMN, AF, TML, AR, TS, KA. Funding acquisition: KA, JAS, AR. Data curation: KA, TML. Data acquisition and verification: AMN, AF, TML, AR, JAS, KA, AC, TS. Structured search and quality assessment: JV, MVP, KA. Statistics: AL, KA. Project administration: KA, TML. Writing original draft: JV, MVP, KA. Writing – reviewing and editing: AMN, AF, TML, AR, JAS, ZZ, TS, AL, KA, JV, MVP, AC, AS. All authors have read and approved the final version of the paper.
Additional information
Jill Vanthienen and Marine Vassilev Petrov are co-first authors; Adrien Flahault and Karel Allegaert are co-last authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Vanthienen, J., Petrov, M.V., Luu, T.M. et al. The QTc-Bazett Interval in Former Very Preterm Infants in Adolescence and Young Adulthood is Not Different from Term-Born Controls. Drug Saf 46, 897–904 (2023). https://doi.org/10.1007/s40264-023-01335-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-023-01335-y