Abstract
Background
Ischemic stroke is a major cause of disability and death worldwide. A narrow therapeutic window profoundly constrained the utilization of alteplase.
Objectives
To investigate therapeutic effects and safety of intravenous recombinant human prourokinase (rhPro-UK) in patients with acute ischemic stroke (AIS) in the 4.5–6 h therapeutic time windows.
Methods
We conducted a phase IIa, randomized, and open-label multicenter clinical trial. Between 4.5 and 6 h after the onset of AIS, patients were randomly administrated to receive intravenous rhPro-UK at a 50 mg or 35 mg dose. The primary endpoint was excellent functional outcome defined as modified Rankin scale (mRS) score of 1 or less at 90 days. The secondary outcome was the treatment response, which was based on an at least 4-point improvement from baseline National Institutes of Health stroke scale (NIHSS) score at 24 h after drug administration. Safety endpoints included death, symptomatic intracerebral hemorrhage (sICH), and other serious adverse events.
Results
We enrolled 80 patients in the 4.5–6 h therapeutic time windows at 17 medical centers in China from December 2016 to November 2017. A total of 39 patients were treated with 50 mg rhPro-UK, and 39 were treated with 35 mg rhPro-UK. Compared with the baseline, the NIHSS score at 24 h and days 7, 14, 30, and 90 was decreased significantly among patients treated with either rhPro-UK 50 mg or 35 mg. The mean reduction in the NIHSS from baseline to 90 days after the onset was 3.56 and 5.79 in the rhPro-UK 50 mg group and the rhPro-UK 35 mg group, respectively. The rates of functional independence at 90 days of rhPro-UK 50 mg and 35 mg were 61.54% and 69.23%, respectively (P = 0.475), and the proportion of patients with functional response to treatment at 24 h were 28.21% and 33.33% (P = 0.624). No sICH occurred in the two groups, and death occurred in only one patient in the rhPro-UK 50 mg group. There was no significant difference in mortality at 90 days and the rate of other serious adverse events between two groups.
Conclusion
In the 4.5–6 h time window, more than 60% of patients at either dose of rhPro-UK (50 mg or 35 mg) achieved functional independence at 90 days without increased mortality and sICH risk. Thus, intravenous rhPro-UK was effective and safe for patients with AIS within 4.5–6 h after stroke onset. While no significant differences were identified between different dosages of rhPro-UK regarding clinical outcomes, it is a logical step to further test the safety and efficacy of the low dose of rhPro-UK in a well-powered phase III study.
Trial Registration
http://www.chictr.org.cn. Identifier: ChiCTR1800016519. Date of registration: 6 June 2018.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this phase II, multicenter, open-label trial, the safety and efficacy of two different doses of recombinant pro urokinase (rhPro-UK) in acute ischemic stroke patients within 4.5–6h from onset were evaluated. |
Conclusions related to efficacy were limited because of the study design, but no significant differences were identified between different dosages of rhPro-UK (50 mg and 35 mg) regarding clinical outcomes in the 4.5–6 h time window. |
1 Introduction
Ischemic stroke is a major cause of disability and death worldwide. Intravenous (IV) recombination tissue plasminogen activator (rt-PA) is the standard care for acute ischemic stroke (AIS) within 4.5 h from symptom onset [1]. However, a narrow therapeutic window and hemorrhagic complications have profoundly constrained the utilization of rt-PA. With an increasing awareness of the importance of acute stroke care, endovascular treatment (EVT) has been a significant advancement for management of patients with stroke related to large vessel occlusions [2]. However, the required infrastructure and human expertise again limited EVT to a small amount of stroke patients [3]. Accordingly, there is an urgent need for effective thrombolytic drug treatment.
Recombinant human prourokinase (rhPro-UK), one of the novel thrombolytics, preferentially activates plasminogen on the fibrin surface and induces fibrin-selective clot lysis. With the advantages of a greater efficacy and less adverse reactions than other thrombolytics, thrombolytic therapy with rhPro-UK has showed a promising curative effect and good safety profile in acute myocardial infarction (AMI) patients [4], which has been approved by National Medical Products Administration (NMPA) for AMI. The Prolyse in Acute Cerebral Thromboembolism (PROACT) trial showed that intra-arterial (IA) local recombinant pro-urokinase infusion within 6 h of onset was superior to control drug treatment in recanalization in AIS patients with middle cerebral artery (MCA) occlusions [5].
In our previous study, compared with rt-PA, both the low (35 mg) and high (50 mg) dose of IV rhPro-UK appeared to be safe with possible efficacy in AIS patients within 4.5 h of symptoms onset [6]. However, proof of benefits and safety of IV rhPro-UK treatment for AIS patients in the 4.5–6 h window remains lacking. The aims of this study were to investigate the efficacy and safety of IV rhPro-UK treatment in Chinese patients with AIS at 4.5–6 h therapeutic time windows after the onset of symptoms.
2 Methods
2.1 Study Design and Participants
We conducted this phase IIa, randomized, open-label multicenter clinical trial including 17 study sites in China. The clinical trial was accepted by NMPA (No. 2016L05323) and was approved by the institutional review boards of the participating centers. Xuanwu Hospital, Capital Medical University had the primary responsibility for leading the study. The study was conducted in accordance with the principles of the Declaration of Helsinki. The written consent was obtained from all patients prior to their enrollment. The trial is registered with chictr.org.cn, number ChiCTR1800016519.
2.2 Study Participants
Patients eligible for the trial were aged 18–80 years old with a diagnosis of AIS with neurological deficits on the National Institutes of Health Stroke Scale (NIHSS) scores of 4–25 points, who received treatment within 4.5–6 h after symptom onset. A cerebral computed tomographic (CT) scan was required before randomization to exclude patients who had an intracranial hemorrhage (ICH) or major ischemic infarction. Patients with contraindications for stroke thrombolysis were not eligible for the study. Exclusion criteria included transient ischemic attack (TIA), a stroke or myocardial infarction episode within the previous 3 months, history of ICH, active visceral hemorrhage or high hemorrhagic risk, taking anticoagulants, severe uncontrolled hypertension, and blood glucose less than 2.7 mmol/L or over 22.2 mmol/L, etc. Detailed clinical, CT, and laboratory inclusion and exclusion criteria are described in Supplementary Table 1.
2.3 Randomization and Masking
Eligible patients within 4.5–6 h after onset were randomly administrated in a 1:1 ratio to receive IV rhPro-UK at 50 mg (group A) or rhPro-UK at 35 mg (group B). A central randomization system was used for all participating centers, and the randomization was carried out online, in a centralized way, with filling out the electronic case report form. Randomization was performed by the neurologist who visited the patient. This was an open-label trial and did not involve masking of treatment or outcomes.
2.4 Study Procedures
rhPro-UK (batch no. 20160701) was obtained from Tasly Biopharmaceuticals Co., Ltd. (Shanghai, China). For rhPro-UK 50 mg group, patients were administered a bolus of 20 mg within 3 min followed by a 30-min infusion. For rhPro-UK 35 mg group, a bolus of 15 mg was administered within 3 min followed by a 30-min infusion. No antiplatelet agents were permitted within 24 h after administration of the investigational drug, and no anticoagulants were permitted at any time in this study. All other treatments were guided by the standard of care of thrombolysis in AIS. The assessment schedule was summarized in Supplementary Table 2.
Assessments were made at the time of enrollment, at 2, 6 and 24 h after drug administration, and on days 7, 14, 30, and 90 after drug treatment. In addition, clinical condition of patients (e.g., blood pressure, oxygenation, and heart rate) was closely monitored for the first 24 h after treatment. Initial assessments included a physical examination, CT, and the quantification of any neurologic deficit with the use of the NIHSS and the level of global disability with the application of the modified Rankin scale (mRS). During the follow-up period, patients were assessed with the NIHSS and mRS on days 7, 14, 30, and 90.
CT was performed before treatment and at 24 h after treatment. Additional CT studies were performed at the discretion of the investigators. The investigators reassessed safety data on intercurrent events and adjudicated whether each death or score change indicating neurologic deterioration was likely due to ICH, other brain injury and disease, or neither of these causes.
2.5 Outcomes Assessment
The primary efficacy endpoint was the degree of disability at day 90 (3-month visit), as assessed by the mRS score, dichotomized as a favorable outcome (score of 0 or 1) or an unfavorable outcome (score of 2–6). The secondary efficacy endpoint was the early neurologic improvement (defined as a reduction of at least 4-point on the NIHSS score at 24 h), the NIHSS scores measured at different assessment time points, and the recurrence of AIS within 7 days after the treatment.
Safety endpoints included overall mortality at day 90; symptomatic intracranial hemorrhage (sICH), which was defined as subarachnoid hemorrhage associated with clinical symptoms and symptomatic intracerebral hemorrhage adjudicated as parenchymal hematoma type 2 within 36 h after treatment, combined with a deterioration of at least 4 points from baseline in the NIHSS score [7]; and any intracranial hemorrhage, and other serious adverse events (SAE).
2.6 Statistical Analysis
Efficacy endpoints were assessed in the intention-to-treat population, which included all treated patients, whether or not they completed the whole study. Missing data on mRS score or NIHSS score were replaced with the Last Observation Carried Forward principle. The frequency and proportion of each mRS value was calculated, and the method of χ2 test was used for categorical variables (the proportion of subjects with 0–1 score and > 1 score) to test differences between groups, and Fisher’s exact test was used in the case of small sample size. For NIHSS score, descriptive methods were used to characterize the measured value and the value changed from baseline. T test was used to compare the value of NIHSS at each visit point. The analysis of covariance (ANCOVA) model with baseline as covariant and treatment as fix effect was used to compare the NIHSS score changed from baseline between the groups.
3 Results
From December 2016 to November 2017, we enrolled 80 patients in the 4.5–6 h therapeutic time windows at 17 centers in China. Two patients were excluded owing to withdrawal by the enrolling physician before treatment because of an error in assessing patient eligibility. A total of 39 patients were assigned to receive 50 mg of rhPro-UK and 39 were assigned to receive 35 mg of rhPro-UK (Fig. 1). The baseline demographic and clinical characteristics of the patients are listed in Table 1. The rhPro-UK 50 mg group had a lower frequency of heart disease as compared with the rhPro-UK 35 mg group (10.26% versus 33.33%, P = 0.014). The summary of prior “heart diseases” was presented in Supplementary Table 3. Besides the history of “heart disease”, there were no significant differences between groups at baseline.
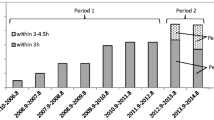
For the primary endpoint, the rates of functional independence at 3 months of rhPro-UK 50 mg- and 35 mg-treated patients were 61.54% and 69.23%, respectively (P = 0.475, Table 2). The overall distribution of scores on the mRS was shown in Fig. 2.
Compared with the baseline, the NIHSS score at 24 h and days 7, 14, 30, and 90 was decreased significantly among patients treated with either rhPro-UK 50 mg or 35 mg (Table 2, Fig. 3). The mean reduction in the NIHSS from baseline to 90 days after the onset was 3.56 and 5.79 in the rhPro-UK 50 mg group and the rhPro-UK 35 mg group, respectively. By 90 days, 66.67% of the patients in the rhPro-UK 50 mg group and 82.05% of those in the rhPro-UK 35 mg group had achieved a mRS score of 0–2 (P = 0.120). A total of 11 patients (28.21%) in the rhPro-UK 50 mg group and 13 patients (33.33%) in the rhPro-UK 35 mg group achieved major neurological improvement at 24 h. No ischemic stroke relapsed within 7 days among patients in both groups. The rate of early neurologic improvement at 24 h and the recurrence of AIS within 7 days did not differ significantly with either rhPro-UK dose. The reduction of NIHSS score at days 7, 14, 30, and 90 from baseline in the rhPro-UK 35 mg group was more than that in the rhPro-UK 50 mg group (Table 2, Fig. 3).
A The mean (± SE) NIHSS scores at different time points in the rhPro-UK 50 mg group. B The mean (± SE) NIHSS scores at different time points in the rhPro-UK 35 mg group. C The mean (± SE) changes of NIHSS scores from baseline of the intention-to-treat population at different time points. *Statistically significant P value. SE standard error
For the safety outcome, no sICH occurred, and death due to any cause occurred in only one patient in the rhPro-UK 50mg group. A list of adverse events, including causes of death, and serious adverse events are provided in Table 2.
After adjustment for the baseline variables of status with respect to age, hypertension, diabetes, hyperlipidemia, prior heart disease, and prior stroke, the original statistical conclusions are not changed (Table 3).
4 Discussion
Our trial showed no significant difference between different dosages of rhPro-UK regarding clinical outcomes in the 4.5–6 h therapeutic time window. Without an increase in SAEs and sICH risk, the proportion of patients with slight or no neurological disability at 90 days exceeded 60% with rhPro-UK treatment at either dose. Thus, IV rhPro-UK was effective and safe for AIS patients within 4.5–6 h after stroke onset.
To date, rapid administration of rt-PA to well-selected patients remains the only pharmacotherapy approved by the Food and Drug Administration for early treatment of AIS [8]. However, only about 5–20% of patients received rt-PA treatment in clinical settings [9]. Hacke et al. [10] demonstrated that the proportion of patients with full recovery decreased with increased time gap between stroke onset and treatment initiation. Beyond 4.5 h, there was increased mortality with no significant clinical benefit.
In the third international stroke trial (IST-3) [11], AIS patients treated within 6 h of onset were enrolled, and 37% of patients in the rt-PA group versus 35% in the control group were alive and independent at 6 months. Based on Virtual International Stroke Trials Archive (VISTA) dataset, Fulton et al. [12] found that usage of simple clinical variables and plain CT alone failed to identify a population in whom the alteplase effect would be safe and effective with treatment initiation between 4.5 and 6 h. A meta-analysis of nine randomized controlled trials (RCTs), of which six RCTs could randomized patients beyond 4.5 h and up to 6 h after symptom onset, showed no evidence of significant benefit of alteplase compared with placebo after 4.5 h of stroke onset or when last seen well [13]. According to the European Stroke Organization, AIS patients of 4.5–9 h duration (known onset time), without advanced imaging, were recommended no IV thrombolysis [14]. Thus, other thrombolytic drugs with equal or superior efficacy and safety are urgently needed for AIS exceeding 4.5 h.
As a specific plasminogen activator that mainly acts on fibrin at the thrombus site, prourokinase (Pro-UK) does not form covalent complexes with protease inhibitors in plasma. Minimal deactivation by circulating inhibitors and clot-specific plasminogen activation are two advantages of Pro-UK [15]. In contrast to rt-PA, Pro-UK induces minimal (< 5%) or no re-thrombosis and exerts no procoagulant effect in blood.
In a rat model with thromboembolic stroke, Hao [16] found that intravenous infusion of Pro-UK in the acute-early stage (1.5 h after embolism) reduced the neurological deficits and decreased the lesion and infarct volume, without increasing the ICH as compared with urokinase and rt-PA. In the 4.5 h or 6 h time windows, the use of Pro-UK thrombolysis was slightly better than rt-PA without hemorrhage. In a rabbit model with cerebral ischemia at 3, 4.5, and 6 h therapeutic time windows, IV Pro-UK improved recanalization with reduced risk of cerebral hemorrhage, exerting therapeutic effects within a 6 h time frame [17].
The PROACT study demonstrated a partial or complete recanalization rate of initially occluded cerebral vessels of 57.7% with Pro-UK versus 15.4% in patients receiving placebo, substantially higher than the 34.4% observed with double-chain rt-PA given intravenously [5, 18]. In all, 40% of Pro-UK patients and 25% of control patients had a mRS of 2 or less at 90 days, despite sICH within 24 h occurring in 10% of Pro-UK patients and 2% of control patients [19]. Thus, IA local delivery Pro-UK within 6 h of the onset of AIS significantly improved recanalization efficacy and clinical outcome at 90 days, despite an increased risk of early sICH. Takano et al. [20] showed that both IA and IV Pro-UK significantly promoted reperfusion and decreased lesion in an embolic stroke model, indicating that IA and IV therapy with Pro-UK are equally effective in promoting reperfusion and inhibiting the development of focal ischemic injury. Takano et al. mentioned that, if the current IA efficacy trial of Pro-UK provides evidence that this novel thrombolytic agent improves clinical outcome when given to AIS patients within the first 6 h after onset, then it is likely that future assessment of Pro-UK treatment will occur.
Our previous study suggested that rhPro-UK intravenous thrombolysis therapy is effective for patients within 4.5 h after stroke onset [6]. In the present study, we compared the efficacy and safety between different doses of IV rhPro-UK for AIS in the 4.5–6 h time window. Without increased mortality and ICH risk, more than 60% of patients at either dose achieved functional independence at 90 days. The proportion of patients with favorable outcomes was similar to previous studies. In a meta-analysis of five randomized trials [21], the crude cumulative rates of disability-free (mRS 0–1) outcome at 3 months were tenecteplase 57.9% versus alteplase 55.4%, the crude summary sICH rates were tenecteplase 3% versus alteplase 3%, and the crude mortality rates at 3 months were tenecteplase 7.6% versus alteplase 8.1%.
There was a trend with rhPro-UK 35 mg toward an increase in the rate of patients with favorable outcome and a reduction in the mean NIHSS score compared with those in the rhPro-UK 50 mg group. There was a dose-response relationship for Pro-UK [22]. Efficacy increased from the lowest to the highest dose and increased as the time window shortened [17]. Meanwhile, some researchers found that conversion rate from single-chain Pro-UK to double-chain UK was not only related to the dosage, but also associated with the administration regimen [4]. When a 25% bolus was followed by a 60 min infusion, the conversion rates of 35 mg dosage and 50 mg dosage were 15.4% and 27.9%, respectively. When the administration regimen was changed to a 20 mg bolus first followed by a 30 min infusion, the conversion rate was significantly decreased. The conversion rate was only 14% for the 65 mg dosage, and 18.9% for the 85 mg dosage. The better trend in rhPro-UK 35 mg versus 50 mg groups might be related to the different conversion rates due to the administration regimen. This finding needs to be confirmed in future studies.
Our randomized study is limited by its small sample size. The potential benefit could be more obvious in a larger randomized cohort study. The treatment allocation was not blinded, and there was no control group. Despite taking several measures, such as selection of stroke centers with Good Clinical Practice (GCP) certification, conduction of uniform training for researchers, and regular supervision and inspection of centers, certain measure biases with the open design may not have been completely ruled out.
At the time when the trial was designed, there were no recognized safe and effective thrombolytic drugs approved for use within 4.5–6 h of onset in patients with ischemic stroke. As a phase II clinical trial for a new drug application with the primary objective of exploring the appropriate dose, only the safety and efficacy of intravenous rhPro-UK 35 mg and 50 mg were compared. In a subsequent phase III clinical trial, a randomized controlled design was used to further compare the rhPro-UK 35 mg dose group with the standard treatment. Furthermore, the optimal strategy and the influencing factors of curative effect need to be confirmed in further studies. Whether this strategy could be beneficial in improving long-term clinical outcomes needs to be clarified in larger studies. Finally, advanced imaging about perfusion lesions or vessel occlusion was not mandated. Information of reperfusion and recanalization on imaging was absent. However, the use of CT scans in the present study gives a wider applicability of this drug, as CT scans are widely available, even in smaller cities.
5 Conclusions
In conclusion, this phase IIa, randomized, and open-label multicenter clinical study showed for the first time that IV rhPro-UK was effective and safe for patients with AIS within 4.5–6 h after stroke onset. Furthermore, this study provides critical data to plan a phase III multi-center clinical trial to further test the safety and efficacy of the 35 mg low dose of rhPro-UK.
References
Wang X, You S, Sato S, Yang J, Carcel C, Zheng D, et al. Current status of intravenous tissue plasminogen activator dosage for acute ischaemic stroke: an updated systematic review. Stroke Vasc Neurol. 2018;3:28–33. https://doi.org/10.1136/svn-2017-000112.
English JD, Yavagal DR, Gupta R, Janardhan V, Zaidat OO, Xavier AR, et al. Mechanical thrombectomy-ready comprehensive stroke center requirements and endovascular stroke systems of care: recommendations from the Endovascular Stroke Standards Committee of the Society of Vascular and Interventional Neurology (SVIN). Interv Neurol. 2016;4:138–50. https://doi.org/10.1159/000442715.
Adeoye O, Albright KC, Carr BG, Wolff C, Mullen MT, Abruzzo T, et al. Geographic access to acute stroke care in the United States. Stroke. 2014;45:3019–24. https://doi.org/10.1161/strokeaha.114.006293.
Prourokinase Clinical Trial Group. Multicenter phase III study of recombinant prourokinase for acute myocardial infarction with ST-segment evaluation. J Med Res. 2013;42:26–31 ((In Chinese)).
del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT Investigators. Prolyse in acute cerebral thromboembolism. Stroke. 1998;29:4–11.
Song H, Wang Y, Ma Q, Chen H, Liu B, Yang Y, et al. Efficacy and safety of recombinant human prourokinase in acute ischemic stroke: a phase iia randomized clinical trial. Transl Stroke Res. 2022. https://doi.org/10.1007/s12975-022-01012-9.
Wahlgren N, Ahmed N, Davalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007;369:275–82. https://doi.org/10.1016/s0140-6736(07)60149-4.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–110. https://doi.org/10.1161/str.0000000000000158.
Amiri H, Bluhmki E, Bendszus M, Eschenfelder CC, Donnan GA, Leys D, et al. European Cooperative Acute Stroke Study-4: extending the time for thrombolysis in emergency neurological deficits ECASS-4: ExTEND. Int J Stroke. 2016;11:260–7. https://doi.org/10.1177/1747493015620805.
Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363:768–74. https://doi.org/10.1016/s0140-6736(04)15692-4.
Sandercock P, Wardlaw JM, Lindley RI, Dennis M, Cohen G, Murray G, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 2012;379:2352–63. https://doi.org/10.1016/s0140-6736(12)60768-5.
Fulton RL, Lees KR, Bluhmki E, Biegert G, Albers GW, Davis SM, et al. Selection for delayed intravenous alteplase treatment based on a prognostic score. Int J Stroke. 2015;10:90–4. https://doi.org/10.1111/j.1747-4949.2012.00943.x.
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384:1929–35. https://doi.org/10.1016/s0140-6736(14)60584-5.
Berge E, Whiteley W, Audebert H, De Marchis GM, Fonseca AC, Padiglioni C, et al. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur Stroke J. 2021;6:I–XII. https://doi.org/10.1177/2396987321989865.
Liu JN, Liu JX, Liu Bf BF, Sun Z, Zuo JL, Zhang Px PX, et al. Prourokinase mutant that induces highly effective clot lysis without interfering with hemostasis. Circ Res. 2002;90:757–63.
Hao CH, Ding WX, Sun Q, Li XX, Wang WT, Zhao ZY, et al. Effect of human recombinant prourokinase(rhpro-UK) on thromboembolic stroke in rats. Eur J Pharmacol. 2018;818:429–34. https://doi.org/10.1016/j.ejphar.2017.11.026.
Hao C, Ding W, Xu X, Sun Q, Li X, Wang W, et al. Effect of recombinant human prourokinase on thrombolysis in a rabbit model of thromboembolic stroke. Biomed Rep. 2018;8:77–84. https://doi.org/10.3892/br.2017.1013.
del Zoppo GJ, Poeck K, Pessin MS, Wolpert SM, Furlan AJ, Ferbert A, et al. Recombinant tissue plasminogen activator in acute thrombotic and embolic stroke. Ann Neurol. 1992;32:78–86. https://doi.org/10.1002/ana.410320113.
Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in acute cerebral thromboembolism. JAMA. 1999;282:2003–11.
Takano K, Carano RA, Tatlisumak T, Meiler M, Sotak CH, Kleinert HD, et al. Efficacy of intra-arterial and intravenous prourokinase in an embolic stroke model evaluated by diffusion-perfusion magnetic resonance imaging. Neurology. 1998;50:870–5.
Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischemic stroke: meta-analysis of 5 randomized trials. Stroke. 2019;50:2156–62. https://doi.org/10.1161/strokeaha.119.025080.
Weaver WD, Hartmann JR, Anderson JL, Reddy PS, Sobolski JC, Sasahara AA. New recombinant glycosylated prourokinase for treatment of patients with acute myocardial infarction. Prourokinase Study Group. J Am Coll Cardiol. 1994;24:1242–8.
Acknowledgements
We thank all the site research teams for their effort and time. We are also grateful to the patients who agreed to take part in the study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was sponsored by Tasly Biopharmaceutical Co., Ltd. And Tasly bio-pharmaceutical Co., Ltd, funded the open access fee.
Conflict of interest
Rui Liu reports being an employee of Tasly Biopharmaceuticals Co., Ltd. Haiqing Song, Yuan Wang, Qingfeng Ma, Huisheng Chen, Bo Liu, Yi Yang, Jianguo Zhu, Shigang Zhao, Xiaoping Jin, Yongqiu Li, Yanyong Wang, Runxiu Zhu, Liandong Zhao, Junyan Liu, Wuwei Feng, Xunming Ji, and Yuping Wang declare no other potential conflict of interest that might be relevant to this article.
Ethics approval
The study was approved by the Xuanwu Hospital Ethics Committee, Capital Medical University (Approval number [2018]010).
Consent to participate
All study participants or their legally authorized representative provided informed consent.
Consent for publication
Not applicable.
Availability of data and material
Data are available to researchers on request for the purpose of reproducing the results or replicating the procedure by directly contacting the corresponding author.
Code availability
Not applicable.
Author contributions
Drs. Song HQ and Wang Y contributed equally as co-first authors. Drs. Wang YP and Ji XM had full access to all the data in the study and were responsible for the integrity of the data and the accuracy of the data analysis. Drs. Song HQ, Ma QF, Ji XM, and Wang YP contributed to the study concept and design. All authors acquired, analyzed, and interpreted the data. Dr. Wang Y wrote the first draft the manuscript. Drs. Feng W, Ji XM, and Wang YP provided critical revision of the manuscript for important intellectual content. All authors provided administrative, technical, or material support, and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Song, H., Wang, Y., Ma, Q. et al. Thrombolysis with Recombinant Human Prourokinase 4.5–6 h After Acute Ischemic Stroke: A Phase IIa, Randomized, and Open-Label Multicenter Clinical Trial. CNS Drugs 38, 67–75 (2024). https://doi.org/10.1007/s40263-023-01051-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-023-01051-2