Abstract
The developmental and epileptic encephalopathies encompass a group of rare syndromes characterised by severe drug-resistant epilepsy with onset in childhood and significant neurodevelopmental comorbidities. The latter include intellectual disability, developmental delay, behavioural problems including attention-deficit hyperactivity disorder and autism spectrum disorder, psychiatric problems including anxiety and depression, speech impairment and sleep problems. Classical examples of developmental and epileptic encephalopathies include Dravet syndrome, Lennox–Gastaut syndrome and tuberous sclerosis complex. The mainstay of treatment is with multiple anti-seizure medications (ASMs); however, the ASMs themselves can be associated with psychobehavioural adverse events, and effects (negative or positive) on cognition and sleep. We have performed a targeted literature review of ASMs commonly used in the treatment of developmental and epileptic encephalopathies to discuss the latest evidence on their effects on behaviour, mood, cognition, sedation and sleep. The ASMs include valproate (VPA), clobazam, topiramate (TPM), cannabidiol (CBD), fenfluramine (FFA), levetiracetam (LEV), brivaracetam (BRV), zonisamide (ZNS), perampanel (PER), ethosuximide, stiripentol, lamotrigine (LTG), rufinamide, vigabatrin, lacosamide (LCM) and everolimus. Bromide, felbamate and other sodium channel ASMs are discussed briefly. Overall, the current evidence suggest that LEV, PER and to a lesser extent BRV are associated with psychobehavioural adverse events including aggressiveness and irritability; TPM and to a lesser extent ZNS are associated with language impairment and cognitive dulling/memory problems. Patients with a history of behavioural and psychiatric comorbidities may be more at risk of developing psychobehavioural adverse events. Topiramate and ZNS may be associated with negative effects in some aspects of cognition; CBD, FFA, LEV, BRV and LTG may have some positive effects, while the remaining ASMs do not appear to have a detrimental effect. All the ASMs are associated with sedation to a certain extent, which is pronounced during uptitration. Cannabidiol, PER and pregabalin may be associated with improvements in sleep, LTG is associated with insomnia, while VPA, TPM, LEV, ZNS and LCM do not appear to have detrimental effects. There was variability in the extent of evidence for each ASM: for many first-generation and some second-generation ASMs, there is scant documented evidence; however, their extensive use suggests favourable tolerability and safety (e.g. VPA); second-generation and some third-generation ASMs tend to have the most robust evidence documented over several years of use (TPM, LEV, PER, ZNS, BRV), while evidence is still being generated for newer ASMs such as CBD and FFA. Finally, we discuss how a variety of factors can affect mood, behaviour and cognition, and untangling the associations between the effects of the underlying syndrome and those of the ASMs can be challenging. In particular, there is enormous heterogeneity in cognitive, behavioural and developmental impairments that is complex and can change naturally over time; there is a lack of standardised instruments for evaluating these outcomes in developmental and epileptic encephalopathies, with a reliance on subjective evaluations by proxy (caregivers); and treatment regimes are complex involving multiple ASMs as well as other drugs.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Patients with developmental and epileptic encephalopathies have significant neurodevelopmental comorbidities including cognitive, behavioural, psychiatric and sleep impairments. |
Some anti-seizure medications have side effects that may contribute to these impairments, including levetiracetam and perampanel (aggressiveness and irritability), topiramate and zonisamide (language and memory problems) and lamotrigine (insomnia). |
Cannabidiol, fenfluramine, levetiracetam, brivaracetam and lamotrigine may have positive effects on some aspects of cognition. |
1 Introduction
The developmental and epileptic encephalopathies (DEEs) encompass a group of rare syndromes characterised by severe epilepsy with onset in childhood and neurodevelopmental impairment [1]. Individuals with DEEs experience frequent severe seizures, often numerous times a day; the seizures can be of many different semiologies and they tend to be refractory to currently available anti-seizure medications (ASMs). Dravet syndrome (DS), Lennox–Gastaut syndrome (LGS) and tuberous sclerosis complex (TSC) are classical examples of DEEs in which advances in the understanding of the underlying aetiology have translated through to the clinic with new drug approvals in recent years (Table 1) [2,3,4,5].
Neurodevelopmental impairment is common in these syndromes, affecting cognition, communication, attention, behaviour and sleep (Fig. 1; Table 1). The underlying aetiology of the syndrome can be a cause of the neurodevelopmental impairment, while seizures themselves can also have an adverse impact (Fig. 2) [6]. A vicious cycle can also emerge whereby sleep disorders, which can be exacerbated by nocturnal seizures as well as cogitative/behavioural problems, can in turn further affect the cognitive/behavioural problems [7]. Sleep problems may also cause neuroinflammation and neurodegeneration, further intensifying seizures [8]. These comorbidities can have profound effects on the quality of life (QoL) of patients and their families [9,10,11,12,13], and therefore their importance has been growing in recent decades, with more recent clinical trials and observational studies including specific evaluations of these outcomes.
Factors affecting cognition, behaviour, mood and sleep disturbances. The underlying aetiology can result in damage to the brain, including during critical periods of development, and the seizures themselves may exacerbate damage to the brain leading to further cognitive impairments [6]. Patient characteristics (e.g. age of onset, genetics) and anti-seizure medications (ASMs) can also have an effect. The comorbidities and the factors contributing to them are all tightly inter-linked
In addition to the pathogenesis of the syndrome, the very treatments used to alleviate seizures in patients with DEEs—the ASMs themselves—can be associated with various psychobehavioural adverse events (PBAEs) (Fig. 2). In addition, some ASMs can have negative effects on cognition and sleep in some patients, while others can be neutral or are associated with positive effects. Psychobehavioural adverse events encompass a range of behavioural adverse events (AEs) including irritability, aggression, tantrum/outbursts, hyperactivity and emotional lability/mood changes and a range of psychiatric AEs including depression, psychosis, anxiety and suicidal ideation. Adverse events, including PBAEs in epilepsy patients, are associated with decreased patient QoL [10] and increased healthcare resources and costs [14].
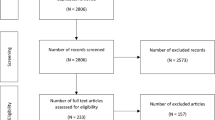
We have conducted a narrative review of the effects of ASMs on PBAEs, cognition, sedation and sleep, with a focus on ASMs used to treat DEEs/drug-resistant epilepsy (DRE), particularly DS, LGS and TSC, either as approved therapies (bold text in Table 1) or off-label (unbold text in Table 1), as specified in recent treatment guidance/reviews for DS [3, 15,16,17], LGS [18,19,20,21] and TSC [2, 22,23,24,25,26]. Studies of particular interest were those that included patients with DEE/DREs, especially studies whose main objective was to assess these specific outcomes, pooled safety analyses and meta-analyses (as rarer events may only become evident with such analyses), and data from real-world studies (as regulatory clinical trials can often exclude people with suicidal ideation and psychosis) [27, 28]. To identify the studies, PubMed was searched in March 2022 using a range of MeSH terms encompassing cognition, behaviour, psychiatric and sleep for each ASM. Furthermore, regulatory documents, including the Summary of Product Characteristics (SmPC) for the European Union (EU) and the US prescribing information (PI), were identified. In particular, this review includes data on recently approved ASMs such as CBD and FFA, and the potential of preventative treatment in TSC, as well as the most up-to-date data on other ASMs.
The following sections are divided into those ASMs used in the treatment of at least two of the three DEEs, followed by those used predominantly for DS alone, LGS and then TSC (Table 1). Finally, we briefly discuss ASMs that are less commonly used including bromide, felbamate and the other sodium channel blockers carbamazepine, eslicarbazepine acetate, oxcarbazepine and phenytoin, and the GABA agonists gabapentin and pregabalin. Of note, all the ASMs are associated with somnolence/sedation to some extent, which are usually pronounced during uptitration. However, because of differences in study designs and populations, it is not possible to make comparisons between the ASMs. In addition, most ASMs have a precautionary warning for an increased risk of suicidal behaviour and ideation; however, suicidal outcomes are not a specific focus of this review; a recent meta-analysis of placebo-controlled randomised controlled trials (RCTs) of newer ASMs reporting suicide outcomes (ESL, PER, BRV, CBD and CNB) found no evidence of an increased risk of suicide attempt or ideation overall or for any individual drug compared to placebo [29]; however, patients should still be monitored.
2 ASMs Used in the Treatment of More Than One of the Syndromes: DS, LGS and TSC
2.1 Valproate (VPA)
Valproate has a broad indication for the treatment of focal and generalised seizures, or other epileptic syndromes [30, 31], and is the mainstay first-line treatment for many DEEs including DS and LGS. While VPA has been used for many decades, there is a lack of evidence of efficacy and safety from RCTs, with the main evidence from expert opinion (Table 1) and a few small observational studies in patients with DS [32], LGS [33] and TSC [34]. It is generally accepted that VPA rarely controls seizures as monotherapy in patients with DEEs [35], and it is usually used in combination with other escalation ASMs (Table 1). Its multiple mechanisms of action include the modulation of the inhibitory neurotransmitter GABA and voltage-gated sodium channels, and as a histone deacetylase inhibitor [30, 31]. While generally a well-tolerated treatment (Table 2), VPA is associated with major congenital malformations mandating the use of effective contraception in women of childbearing age, and also rare cases of hepatic failure (see Table 3).
As per the SmPC and the PI, VPA is associated with a range of psychiatric and behavioural disorders including confusion, aggression, agitation and disturbance in attention, chiefly in the paediatric population [30, 31]. However, in general, VPA appears to have a good PBAE profile, with observational studies in adults and children with epilepsy (~ 80% with DRE in both adult and paediatric populations) showing it had a significantly lower rate of PBAEs compared with the average across 18 ASMs in adults [36] and a low/moderate rate in children [37] (Table S1 of the Electronic Supplementary Material [ESM]). Of note, VPA is also licensed as a mood stabiliser [30, 31].
Reports on the effects of VPA on sleep have been conflicting, with positive, neutral and negative effects on various aspects of sleep observed across seven small studies in patients with various epilepsy conditions [38]. Further to this, VPA-associated cases of nocturnal enuresis have been reported, with studies suggesting a link to sleep architecture problems [39, 40]. Overall, the effects of VPA on sleep need to be addressed in larger dedicated studies in DEEs, although the prevalent use of this ASM suggests that problems are likely to be minimal.
There is a paucity of studies on the effects of VPA on PBAEs, cognition and sleep in patients with DRE. However, the available evidence of this extensively used ASM suggests minimal effects across these outcomes. Although VPA has been used extensively, it does have several limitations, including a lack of gold-standard evidence from RCTs, a range of AEs and a propensity for adverse drug interactions (Table 2), and therefore it has been suggested that newer ASMs could replace VPA in the future [41]. Because of the significant teratogenic effects of VPA that increase the risk of malformations and neurodevelopmental disorders (e.g. autism spectrum disorder [ASD]), VPA is already heavily restricted in women of childbearing age across all indications, to be used only when there are no other options available, and when pregnancy prevention measures are followed [42]. Further to these concerns, recent evidence suggests VPA may cause congenital impairments with an epigenetic inheritance that have the potential to be transgenerational [43,44,45].
2.2 Clobazam (CLB)
Clobazam is a 1,5-benzodiazepine that is indicated as an adjunctive therapy in epilepsy in the EU and for seizures associated with LGS in the USA [46, 47]. Its efficacy and safety have been evaluated in RCTs in patients with LGS [48,49,50], and in small observational studies in patients with DS [32] and TSC [51], although it has been extensively used in patients with DREs for decades. In the EU, CLB is also indicated for the short-term treatment of severe anxiety [46]. Benzodiazepines, including CLB, mediate their effects through the GABA-A receptor. Clobazam has lower sedative effects than the 1,4-benzodiazepine clonazepam, owing to it being structurally distinct with a lower affinity for GABA-A subunits that are involved in sedation. As with other benzodiazepines, CLB has a warning for physical and psychological dependence, although real-world studies suggest this is rare in patients with epilepsy, with one study estimating that patients with epilepsy had a 99.4% chance of being free of drug dependency over a 5-year treatment for CLB and 98.5% for clonazepam [52]. Overall, CLB has a good tolerability and safety profile (Table 2) [46, 47].
Psychobehavioural AEs have been reported in real-world studies evaluating CLB in children with DREs, with a frequency of 2.2–7.7% across studies [53,54,55]. A post-hoc analysis evaluating aggression and behaviour in patients enrolled in the phase III RCT in patients with LGS reported the occurrence of aggression-related AEs in 23/146 (15.8%) CLB-treated patients versus 4/48 (8.3%) placebo-treated patients [56]. There was no difference in the frequency of aggression-related AEs in those with and without a history of aggressive behaviour. No significant differences between CLB and placebo were observed for the behaviour domains of the Child Behavior Checklist (CBCL) [56]. This is in line with a previous study in children with newly diagnosed epilepsy that showed no differences between CLB (n = 24) and standard monotherapy (phenytoin or carbamazepine; n = 17) across a range of neuropsychological measures (intelligence, memory, attention, psychomotor speed and impulsivity) obtained at 6 weeks or 12 months [57]. However, in a study of 115 children with DREs, 72% reported an improvement in at least one aspect of neurologic function after initiating CLB, particularly alertness, attention span, mood, balance and appetite, while 26% reported a worsening [58]. A more recent (2019), albeit small pilot study, in ten children with LGS treated with CLB observed statistically significant improvements from baseline to week 10 in cognition, behaviour and overall QoL assessed using the Quality of Life in Childhood Epilepsy questionnaire [59]. No studies specifically analysing the effects of CLB on sleep parameters were identified, although benzodiazepines are a treatment option for chronic insomnia in adults [60].
Overall, CLB has a generally good tolerability profile; however, PBAEs have been reported in a proportion of patients with DREs, although there is also some evidence that CLB may be associated with improvements in some aspects of cognition and behaviour. There is a lack of studies on sleep; however, its properties as a benzodiazepine can aid in falling asleep, while somnolence or sedation is a frequently reported AE.
2.3 Topiramate (TPM)
Topiramate is indicated as an adjunctive therapy in patients with LGS, as well as for focal seizures or primary generalised tonic-clonic seizures [61, 62]. The efficacy and safety of TPM have been evaluated in RCTs in patients with LGS [63], with evidence being limited to observational studies in patients with DS [32, 64, 65] and TSC [34]. A Cochrane analysis identified 12 trials evaluating add‐on TPM for DREs (Table S1 of the ESM) [66]. This second-generation ASM modulates voltage-dependent sodium channels, enhances GABA inhibition and antagonises the AMPA/kainate subtype of glutamate receptors [61, 62].
While generally well tolerated, the SmPC and PI contain a warning for PBAEs (Table 2); in the regulatory RCTs (which used a rapid titration schedule), PBAEs were more common in adults than children, and occurred more frequently at higher doses [61, 62]. In the Cochrane analysis of trials evaluating add‐on TPM for DREs, PBAEs associated with TPM were concentration difficulties and ‘thinking abnormally’; however, the majority of the studies were in adults [66] (Table S1 of the ESM). Although rare, co-administration with VPA may increase the risk of hyperammonaemia that may present as encephalopathy (with associated neurocognitive and behavioural changes) or sedation (Table 2) [61, 62].
Negative effects on language abilities and memory are particular concerns of TPM, worse than for many other ASMs [67,68,69,70,71,72,73]. For example, in 84 adults with DRE, TPM showed significantly worse scores compared with LTG for verbal fluency, verbal digit, nonverbal working memory and visual Corsi block spans, with a trend for worse scores for verbal working memory, verbal comprehension, mental rotation, visual anticipation speed and planning ability [69]. The effects appear to be dose related; they are common at high doses but can occur even at low doses in some patients [69, 73,74,75].
Several observational studies in patients with DREs show that PBAEs and cognitive AEs are frequently reported in these real-world situations. In 36 children with DS, AEs included behavioural disorders (agitation or aggression in 14%]), fatigue (11%), insomnia (11%) and impairment of language (5.6%) [65]. In 45 children with LGS, AEs included drowsiness (8.9%), cognitive dulling (8.9%), transient dysarthric speech (4.4%), hyperexcitability (4.4%) and nervousness (2.2%) [76]. In a large study of children with various DREs, behaviour disturbances/aggressiveness was reported in 14/227 (6.2%), attention or concentration difficulty in 11 (4.8%) and acute psychosis in six (2.6%) [65]. Another study in 98 children with DREs reported that cognitive dulling was a particular problem, leading to discontinuation in 31% of patients [77].
Studies specifically evaluating the effect of TPM on PBAEs and cognition in epilepsy patients with cognitive comorbidities have suggested that TPM is associated with worsening of cognition (including cognitive speed, verbal memory, verbal fluency and flexibility) and behaviour in a significant proportion of patients [70, 78]. A post-marketing study of TPM in 596 adults with epilepsy found that having a past psychiatric history was not only a predictor of having PBAEs (including irritability, aggression and depression) but also of cognitive AEs [79]. In contrast to the above studies, a study of 64 adults with DRE and a learning disability found that mean caregiver scores for behaviour, alertness and sleep improved with TPM use [80].
The effect of TPM on sleep has not been extensively studied; however, data from three studies in adults with epilepsy suggest that TPM is not associated with sleep problems, including excessive daytime sleepiness, subjective sleep quality and insomnia [80,81,82]. Overall, TPM is associated with a range of PBAEs and cognitive deficits including behavioural disorders and cognitive dulling. Speech disorders are particularly common, occurring even at lower doses in some patients. Clinicians should also be aware of the increased risk of hyperammonaemic encephalopathy with VPA.
2.4 Highly Purified Cannabidiol (CBD)
Cannabidiol is a third-generation ASM approved as an adjunctive therapy for seizures associated with LGS, DS (in conjunction with CLB in the EU) and TSC [83, 84]. The approvals were based on evidence from RCTs in patients with LGS [85, 86], DS [87, 88] and TSC [89]. Cannabidiol is also being evaluated for the treatment of anxiety disorders, depression, attention-deficit hyperactivity disorder and ASD [90, 91]. Cannabidiol has multiple mechanisms of action that are distinct from other ASMs including modulating intracellular calcium via G protein-coupled receptor 55 and extracellular calcium influx via transient receptor potential vanilloid type 1 channels, and inhibiting adenosine cellular uptake [92].
Cannabidiol is a generally well-tolerated treatment (Table 2) [83, 84, 93]. In the regulatory trials, sleep disturbances (insomnia/sleep disorder/poor quality sleep) occurred in 5–11% of patients with CBD versus 4% for placebo [83]. Somnolence and sedation are more common in patients taking concomitant CLB owing to a bi-directional drug–drug interaction that increases the plasma concentrations of the major metabolites of CBD (7-OH-CBD) and CLB (norclobazam [N-desmethyl-clobazam]); dose reductions of CLB are recommended if somnolence/sedation is observed [83, 84]. In-line with this, a recent meta-analysis of CBD trials across multiple therapy areas noted that CBD was only associated with somnolence and sedation in childhood epilepsy trials, most likely owing to interactions with other ASMs such as CLB and VPA [94]. A small study in children with DRE (n = 35, including DS, LGS and other genetic epilepsy syndromes) found that of 13 patients with abnormal sleep architecture at baseline, sleep improved in 11 (84.6%) patients [95].
Regarding cognition, no cases of significant cognitive decline from baseline were observed in 39 children with DRE assessed using standardised neuropsychological tests on memory, executive functions and attention completed by the patient or caregiver [96]. The vast majority (>89%) of the individual test results showed stable or improved outcomes from baseline, and a significant improvement in measures of selective attention and behaviour were observed. In line with this, in a phase II expanded access program study evaluating the long-term treatment of children with DRE, improvements were recorded for sleep (sleep duration, daytime sleepiness and nocturnal arousals), irritability, hyperactivity, cognition in QoL, behavioural function and general health (n = 28, assessed using the Children’s Sleep Habit Questionnaire [CSHQ], Aberrant Behavior Checklist [ABC] or the Quality of Life in Childhood Epilepsy questionnaire) [97]. Similar to studies in children, a study of 27 adults with DRE reported that cognitive testing (assessed using the NIH Toolbox Cognition Battery) was below average at baseline, but importantly it did not decline further during CBD treatment (1-year follow-up) [98]. Although CBD has only recently been approved (2018–21 across indications and regions), there is now a growing body of evidence beyond the clinical trial programme that CBD may have associated benefits (improvements or stabilisation) for sleep, cognition and behavioural outcomes, albeit from small studies.
2.5 Fenfluramine (FFA)
Fenfluramine, a third-generation ASM, is approved in the EU and USA as an add-on treatment for seizures associated with DS [99, 100]. In the USA, it is also recently approved for LGS, and is currently undergoing regulatory review for this indication in the EU. Pivotal RCTs have been conducted in patients with DS [101, 102] and with LGS [103]. Uniquely among ASMs, FFA has agonistic activity at multiple serotonin receptors and acts as a positive modulator of the sigma-1 receptor, and it is hypothesised the two mechanisms together may help to restore the balance between inhibitory GABA signalling and excitatory glutamatergic signalling [104].
Fenfluramine is generally well tolerated (Table 2) [100, 105, 106]. Psychobehavioural AEs occurred infrequently in pivotal trials, most commonly abnormal behaviour in 0–9% across the FFA doses versus 0% in a combined placebo group, and irritability in 0–9% in FFA-treated patients versus 2% with placebo [99]. Of 78 patients with DS treated with FFA in a compassionate use programme in Germany, an increase in behavioural problems was reported in five (6%) patients and aggressive behaviour in three (4%) and two discontinued because of PBAEs [107]. Across the entire European compassionate use programme (n = 149 patients with DS), PBAEs were reported in 13 (9%) patients, sleep disturbances in six (4%) and somnolence in 24 (16%) [108].
A post-hoc analysis of data from a pivotal RCT and open-label extension (with a ≥ 1 year follow-up) in children and young adults with DS found that responders (a ≥ 50% reduction in monthly convulsive seizure frequency) showed improved everyday executive function assessed using the Behavior Rating Inventory of Executive Function (BRIEF2), which measures factors such as behaviour (e.g. impulsivity), emotion (e.g. emotional outbursts) and cognitive regulation (e.g. attention, memory, planning/organising); in particular, the ≥ 50% monthly convulsive seizure frequency reduction group was significantly more likely to achieve clinically meaningful improvements in emotional regulation (p = 0.002) and cognitive regulation (p = 0.001) than the < 50% monthly convulsive seizure frequency reduction group [109]. Initial data presented at conferences also show that FFA is associated with improvements in executive function in preschool children with DS [110] and in patients with LGS [111]. Importantly, in a real-world study, caregivers of patients with DS treated with FFA reported improvements in patient QoL associated with enhanced cognitive function, alertness and academic performance [112]. Fenfluramine has only recently been approved in patients with DS, and evidence of its effects on cognition and sleep is still being garnered; however, initial data suggest FFA has a positive effect on executive function, which may be mediated through sigma-1 receptors [113, 114].
2.6 Levetiracetam (LEV)
Levetiracetam is a second-generation ASM indicated for the treatment of focal seizures (with or without secondary generalisation in the EU), myoclonic seizures in patients with juvenile myoclonic epilepsy and primary generalised tonic-clonic seizures in patients with idiopathic generalised epilepsy [115, 116]. Retrospective observational studies have provided evidence of the efficacy and safety of LEV in patients with DS [32, 117], LGS [118] and TSC [119], while there is RCT evidence from 14 studies in patients with DREs (Table S1 of the ESM) [120]. Levetiracetam may act through multiple targets, including binding to the synaptic vesicle protein 2A (SV2A), a membrane glycoprotein that is present in synaptic vesicles of neurons and endocrine cells [121].
The tolerability profile of LEV is generally favourable [122] (Table 2), and it is frequently used in patients with DEEs [115]. However, the SmPC and PI for LEV contain a warning for PBAEs including psychotic symptoms, suicidal ideation, irritability and aggressive behaviours [115, 116]. Furthermore, a number of pooled analyses and meta-analyses of RCTs and observational studies have confirmed the association with PBAEs, particularly hostility, aggression, irritability, nervousness and anxiety [120, 123,124,125,126,127,128], with a higher rate of PBAEs compared with many other ASMs (Table S1 of the ESM) [36, 37, 127], which can lead to treatment discontinuations in a small proportion of patients [126, 127] (Table S1 of the ESM).
Psychobehavioural AEs appear to be more common in paediatric patients and adolescents than in adults across the pivotal regulatory RCTs (Table 2) [116, 129]. Indeed, the latest Cochrane meta-analysis of placebo-controlled RCTs of LEV as add‐on therapy for DREs reported that the increased risks of PBAEs compared to placebo were minimal in adults but significant in children [120] (Table S1 of the ESM). Levetiracetam was not significantly associated with an increased risk of any individual PBAE alone (Table S1 of the ESM).
Levetiracetam does not appear to have a significant detrimental effect on cognition, and it may even have some benefits on certain aspects [130,131,132]. For example, in one RCT in children and adolescents with DRE and an IQ ≥ 65, no differences were found between LEV and placebo in memory and attention [133], while in the long-term open-label extension study, cognitive functioning (Leiter-R Score) was stable and behavioural and emotional functioning (CBCL) showed slight improvements from baseline to week 48 [134]. In another RCT in children and adolescents with DRE, a worsening of the mean CBCL Aggressive Behavior score was reported in the LEV group but not placebo, whereas the CBCL Activities Competence score worsened in the placebo group but not the LEV group [135]. There is a lack of dedicated studies examining sleep disorders with LEV [38]; however, Thelengana et al. observed sleep-related AEs in only one of 66 patients with adult epilepsy (1.6%) treated with LEV and cases of hypersomnolence were rare [136].
Overall, while generally a tolerable treatment option, PBAEs may be the biggest drawback of LEV, leading to discontinuation in a proportion of adults and children. However, LEV may have neutral effects on sleep and neutral/positive effects on cognition. Sedation might occur during uptitration, but will usually resolve after a few weeks.
2.7 Brivaracetam (BRV)
Brivaracetam is a third-generation ASM that is indicated as adjunctive therapy in the treatment of focal seizures (with or without secondary generalisation in the EU) [137, 138]. A Cochrane analysis identified six trials evaluating add‐on BRV for DREs (Table S1 of the ESM) [139], while BRV has also been analysed in a large number of observational studies in patients with DEEs/DREs [140,141,142,143,144,145,146,147,148]. Brivaracetam is an analogue of LEV that has 15–30 times greater affinity for SV2A and higher brain permeability compared with LEV [149]. Brivaracetam has a good tolerability profile similar to, or perhaps better than, LEV [150, 151]. The most frequently reported AEs in regulatory trials were somnolence and dizziness (Table 2).
Similar to LEV, the SmPC and PI for BRV warns of behavioural reactions including psychotic symptoms, irritability, depression, aggressive behaviour, anxiety, and suicidal behaviour and ideation [137, 138]. In a pooled analysis of the clinical trial programme for adjunct BRV in patients aged ≥ 16 years, overall psychiatric disorder-related AEs were reported in 11.3% of patients treated with BRV versus 8.2% with placebo, behavioural disorder-related AEs in 4.0% versus 2.5%, irritability in 2.7% versus 1.5%, while anger, aggression and agitation were each reported infrequently (≤ 1% of BRV-treated patients) [152]. Psychosis-related AEs were also rare [152]. Two meta-analyses of BRV placebo-controlled RCTs in adults with DREs have both found that BRV was significantly associated with irritability but not for other PBAEs including insomnia, depression and anxiety [153, 154]
As with LEV, PBAEs appear to occur more common in children. In the regulatory, open-label, uncontrolled, long-term studies, behavioural disorders were reported in 24.8% of paediatric patients compared with 15.1% of adults, suicidal ideation in 4.7% of paediatric patients compared with 2.4% of adults and psychomotor hyperactivity was reported in 4.7% of paediatric patients [137]. In both adult and paediatric patients, most of the PBAEs were not serious, were of mild or moderate intensity and did not lead to study discontinuation [137].
The efficacy and tolerability of BRV have also been analysed in a number of real-world observational studies. Across five observational studies in paediatric patients, with most or all patients having DRE (n = 23–66), PBAEs were reported in 3–31% of patients, primarily irritability and aggressiveness [140,141,142,143,144], while discontinuations because of PBAEs were infrequent (0–6%) [141,142,143,144]. Similarly in studies exclusively [145, 146] or predominantly in adults with DREs [147, 148] (n = 44–1029), PBAEs included irritability/agitation (6–9% across studies [145, 146, 148], aggression (2–7% [145, 146, 148]), mood changes (2.3% [145]) and memory disturbances (4.7% [146]), and discontinuations because of PBAEs were reported in 4–11% of patients [146, 147]. While one study reported that tolerability in general was not influenced by having a history of learning disability or psychiatric comorbidity [146], other studies have suggested that having pre-existing psychiatric or behavioural comorbidities is a risk factor for the associated PBAEs [155, 156]. Of note, switching from LEV to BRV may have a favourable effect on PBAEs in a proportion of patients (33.3–83.0% across observation studies [Table S1 of the ESM]) [127].
Brivaracetam may benefit some aspects of cognition, with one study in 43 patients with epilepsy showing a significant improvement in attention and executive functions and a trend towards improved reaction times, and stabilised verbal memory performance [157]. No studies were identified that specifically analysed the effect of BRV on sleep disorders, although somnolence is a commonly reported AE, which usually resolves after few weeks.
There is a lack of head-to-head RCTs precluding a direct comparison of the rate of PBAEs in LEV-treated and BRV-treated patients. However, the evidence suggests that BRV has a fairly neutral PBAE profile (except for irritability and aggressiveness), and it may be a valid alternative in patients who have discontinued LEV because of PBAEs. The fact that BRV has enhanced activity at SV2A compared with LEV, but a similar or better psychobehavioural tolerability profile, suggests that SV2A may not be the mechanism responsible for the occurrence of PBAEs [158].
2.8 Zonisamide (ZNS)
Zonisamide, a synthetic sulfonamide, is indicated for the treatment of focal seizures as adjunctive therapy from ≥ 6 years of age in the EU and in adults in the USA [159, 160]. Zonisamide has been evaluated in patients with DREs [161,162,163], and in a multicentre open-label study in patients with LGS [164]. There is also some evidence of use in clinical practice in patients with DS, albeit in a limited capacity [165, 166]. A Cochrane analysis identified eight RCTs in patients with DREs (Table S1 of the ESM) [162]. Zonisamide is a carbonic anhydrase inhibitor, and although its exact mechanism of action is unknown, it includes inhibition of voltage-dependent sodium and a reduction in voltage-sensitive T-type calcium channels [131, 160]. It also allosterically binds to the GABA-benzodiazepine receptor and has been found to facilitate both dopaminergic and serotonergic neurotransmission [160]. Evidence from 20 years of clinical studies in Japan, confirmed by four placebo-controlled trials in Europe and the USA, shows ZNS is a well-tolerated ASM, although sulfonamides including ZNS are known to cause serious skin reactions, including rash and allergic reactions (Table 2). In addition, the SmPC and PI warn of an association with cognitive/neuropsychiatric AEs, the most common being agitation and irritability (Table 2) [159, 160]. In comparative real-world studies, ZNS was significantly associated with a higher rate of PBAEs and discontinuations because of PBAEs in adults and children (the majority with DRE), especially depressed mood (Table S1 of the ESM) [36, 37].
Zonisamide may be associated with negative cognitive and mood effects [159]. For example, a retrospective study that included 28 patients with epilepsy reported ZNS-associated negative effects on executive function (EpiTrack) that was reversed upon withdrawal; verbal memory and QoL measurements were not affected [167]. Zonisamide may also elicit detrimental effects on language ability, especially at high doses [130]. A study in patients with epilepsy evaluating the long-term effects of ZNS found negative cognitive (memory and concentration), mood (anxiety and depression) and language effects may persist even after a year of treatment; the deficits were especially prevalent at high doses but also occurred in a small proportion of patients at low doses [168]. In a study of 87 adult patients with DRE and intellectual disability, PBAEs including sedation (38%), language impairment (19%) and challenging behaviour (10%) were among the most commonly reported AEs [169]. Mania, psychosis and suicidal ideation were also associated with the use of ZNS in a study of 24 patients with DRE; however, psychiatric AEs were not severe and only one patient (4.3%) discontinued the study because of a psychiatric AE (major depressive disorder) [170]. This is reflected in another study where only 1.2% of 167 adults with DRE reported severe psychiatric AEs [171]. In relation to sleep, a small study (n = 13 patients with focal seizures) of ZNS showed no negative effects on measurements that assessed nocturnal sleep and daytime somnolence [172].
Overall, ZNS may be associated with negative cognitive and mood effects, although only limited data are available especially in children, meaning concrete conclusions are difficult to make [38, 130, 132]. However, ZNS appears to be well tolerated in both children and adults if appropriately dosed.
2.9 Perampanel (PER)
Perampanel is indicated for focal seizures and primary generalised tonic-clonic seizures [173, 174]. Perampanel has been evaluated in observational studies in cohorts of patients with DEEs that included LGS, DS and TSC [175,176,177,178,179,180,181,182], while other studies have been performed exclusively in patients with LGS [183, 184] and DS [185]. Perampanel was being evaluated in a phase III RCT; however, the study was terminated by the sponsor because of challenges with recruitment that were exacerbated because of the coronavirus disease 2019 pandemic (NCT02834793). Perampanel is a non-competitive antagonist of the AMPA glutamate receptor on post-synaptic neurons; however, the exact mechanism responsible for its anti-epileptic effects are not known [174]. While PER is considered generally well tolerated, there are warnings for serious PBAEs including aggression, hostility, irritability and anger, especially at higher doses [173, 174] (Table 2). In addition, homicidal ideation and threats have also been reported, although in < 1% of patients in the regulatory clinical trials [173, 174].
In an observational study of 62 children and adolescents with DRE, the most frequently reported AEs included irritability (11.3%) with aggressiveness (4.8%), and reduced vigilance or fatigue (11.3%), while insomnia was reported in 3.2% of patients [180]. A meta-analysis of observational studies in adults with epilepsy have confirmed PER-related behavioural effects, with weighted mean incidences of 12.3% (range 1.4–33.7%) for irritability, 2.0% (range 1.5–7.7%) for anger and 4.4% (range 1.0–24.5%) for aggressiveness (Table S1 of the ESM). A large pooled analysis of 44 retrospective and prospective studies from 17 countries encompassing 4617 patients with epilepsy treated with PER reported behavioural disorders in 5.4% of patients across studies and psychiatric AEs in 21%, leading to discontinuation in 3.1% for irritability, 2.8% for behavioural disorders and 1.1% for mood disturbance [186]. There were no reported cases of homicidal ideation. Psychiatric AEs were significantly associated with having a history of psychiatric comorbidity, while overall tolerability was better when a slow titration was used [186]. Although it has been suggested that PBAEs may be affected by dose [132, 187], other studies have reported the occurrence of PBAEs over a wide range of doses [188]. In addition, PER-associated aggressive behaviour may be more frequent in adolescents than adults [189, 190]. Of note, aggressive behaviour has been reported to occur months or even years after initiating PER [191]. As well as aggression, PER may also be associated with an increased risk of depression [187, 192].
Other studies in patients with DRE have noted that PER can have variable effects on behaviour and cognition, including some positive changes. For example, in a retrospective study of 135 adult patients with epilepsy (the majority with DRE with one or more psychiatric and behavioural comorbidity), 23.7% had aggravated behavioural and psychiatric AEs, while 16.3% showed symptom improvements [193]. In adult patients with LGS treated with PER, 32% had significant adverse behavioural changes; however, improvements were noted in 5.6%, including “feelings of wellness, calm and better contact” [184]. In a study of 13 children with LGS, AEs included decreased activity/social interaction (n = 3) and behaviour disturbance with agitation (n = 2), while improvements in behaviour and cognitive functioning were experienced by 52.8% of patients, particularly with language abilities [183]. This is reflected in another study of children with DRE, in which cognitive performance was slightly improved and no major changes in behaviour, attention or executive functions were seen [194].
Regarding sleep, a cross-sectional study of adults observed insomnia was less prevalent in patients who received PER than those who did not [195]. Clinically significant insomnia scores also differed between the two groups when using a stepwise linear regression model, although no difference was found with a univariate analysis [195]. Studies identified in a systematic literature review (SLR) suggest PER has neutral effects or even improves several aspects of sleep such as reducing daytime sleepiness, and improving total sleep time, sleep latency, sleep efficiency, sleep maintenance index and wake time after sleep onset [38].
In conclusion, behavioural changes are among the most frequent PER-related AEs. Aggressive behaviour is common and may be more typical in adolescent populations. Despite serious warnings, PER can be a well-tolerated treatment if used with caution at the appropriate dose, and it may be associated with improvements in several sleep parameters.
2.10 Ethosuximide (ESM)
Ethosuximide is a first-generation ASM indicated for the control of absence seizures (petit mal) epilepsy, as well as for myoclonic seizures [196, 197]. In an RCT, ESM was found to be more effective in patients with childhood absence epilepsy than LTG, and to have a better tolerability profile (fewer adverse effects on attention) than VPA [198, 199], and as such it is the recommended first-line therapy for childhood absence epilepsy [200]. For DS, ESM is recommended in recent guidelines as a third-line treatment option but for absence seizures only [5, 15, 17]. Ethosuximide acts by depression of the motor cortex and reducing T-type currents on calcium channels, thought to prevent synchronised firing, primarily in thalamocortical neurons [130, 196, 201]. Ethosuximide-related side effects include severe skin reactions such as SCARs and drug reaction with eosinophilia and systemic symptoms, but is generally well tolerated (Table 2) [196, 197]. Psychiatric disorders including withdrawal, anxiety and sleep disturbances were reported to be uncommon in the SmPC (Table 2) [196].
There is very limited information about the cognitive or behavioural effects of ESM, even though it has been used clinically for over 60 years [201]. However, two studies have suggested ESM may be associated with attentional dysfunction, although to a lower or similar extent to some other ASMs [198, 199, 202]. The first study comparing initial monotherapy of different ASMs in 453 children with absence epilepsy found that ESM had significantly less adverse attentional effects compared with VPA, as measured by the Conners Continuous Performance Test criteria, observed both at 16–20 weeks and after 1 year, while there was no difference in attentional dysfunction between ESM and LTG [198, 199]. Another study of ESM monotherapy in 61 children with absence seizures showed that, compared with controls, the children had significantly lower scores for verbal, performance and full-scale IQ, perceptual organisation, motor integration and motor coordination, and multiple domains related to attentional functions, although it was suggested that ESM itself caused only mild effects for some parameters, with the seizures and the underlying aetiology also being contributing factors [202].
There is limited literature available for ESM directly related to sleep parameters [38]; however, sleep-related AEs including sleep disturbances and night terrors are known to occur with ESM [196, 197]. In conclusion, although evidence of ESM-related PBAEs, cognition or sleep changes are limited, mild attentional effects and other reactions have been reported.
3 Additional ASMs Used in the Treatment of DS
3.1 Stiripentol (STP)
Stiripentol is indicated as an adjunctive therapy for seizures in patients with DS (in conjunction with CLB in the USA and VPA and CLB in the EU) [203, 204]. Stiripentol acts by enhancing the inhibitory neurotransmitter GABA. It was approved in the EU in 2007 and in the USA in 2018 based on the evidence from a pivotal RCT in children with DS [205]. Stiripentol is generally well tolerated, although it is associated with some PBAEs including agitation and aggression, as well as insomnia (Table 2) [165, 203, 206]. Of note, an interaction with CLB leads to increased plasma concentrations of CLB and its metabolite N-desmethyl-clobazam that may increase CLB-related AEs; somnolence and sedation are particularly prevalent with STP and CLB, which may be alleviated by reductions in the dose of CLB [203, 204].
There are limited studies evaluating PBAEs and the effects on cognition and sleep with STP. A prospective observational open-label study that followed patients with DS (age 11 months to 22 years at initiation) from 2003 to 2015 reported drowsiness/sedation in 14/41 (34%) patients, behavioural change in nine (22%) and insomnia in four (10%) [207]. A long-term open-label study in Japan reported somnolence in 19/24 (79.2%) patients with DS, agitation in two (8.3%) patients and initial insomnia in two (8.3%) [208]. Another long-term study of patients with DS who initiated STP in childhood and continued into adulthood reported that intellectual disability present in childhood continued to decline into adulthood [209]. Overall, there do not appear to be either concerns or benefits with regard to PBAEs, cognition or sleep with STP, although somnolence and sedation are common side effects requiring dose reductions of CLB.
4 Additional ASMs Used in the Treatment of LGS
4.1 Lamotrigine (LTG)
Lamotrigine is a second-generation, sodium-channel-blocking ASM. It is indicated as adjunctive treatment for seizures associated with LGS, as well as focal and generalised tonic-clonic seizures in general [210, 211]. The approval in patients with LGS was based on RCT evidence in patients with LGS [212]. In addition, a recent Cochrane analysis identified 14 trials encompassing 1806 participants with DREs (Table S1 of the ESM) [213]. Slow titration of LTG is required at initiation to reduce the risk of serious, potentially fatal, rashes, including Stevens–Johnson syndrome and toxic epidermal necrolysis, and titration should be even slower in combination with VPA. Otherwise, LTG has a good tolerability and safety profile (Table 2) [210, 211].
Psychobehavioural AEs reported in the regulatory trials include insomnia, depression, anxiety and emotional lability, reported in ≤ 6% of adult patients [210, 211]. In studies comparing the rate of PBAEs across 18 ASMs in adults [36] and in children [37] with epilepsy (mainly with DRE), LTG, one of the most frequently used ASMs, had one of the lowest rates of PBAEs and discontinuations because of PBAEs (Table S1 of the ESM). The good PBAE profile of LTG is in line with other studies [131, 214, 215], including the recent Cochrane systematic reviews of LTG studies in drug-resistant focal seizures and drug-resistant generalised tonic-clonic seizures where no PBAEs were among the most frequently reported (Table S1 of the ESM) [213, 216]. Of note, LTG also acts as a mood stabiliser and is indicated for depression in patients with bipolar disorder [210, 211].
Many studies have reported that LTG has a neutral or positive effect on cognition and behaviour [217,218,219,220,221,222,223,224,225,226,227,228,229]. McKee et al. reported improvements from baseline in social functioning in nearly half of their patients with DRE and mental retardation (n = 95), with significant improvements in mean scores for lethargy and habilitation [227], while other studies have reported significant improvements in measures of mood/depression in patients with DREs [225, 230]. This is in line with several studies reporting anecdotal improvements in cognition and behaviour, including increased alertness, responsiveness and social interactions [217, 219, 231]. However, it should be noted that negative effects on aspects of behaviour have been noted in patients treated with LTG [225, 226, 232]. For example, in a small study of seven patients with epilepsy with mental retardation (including five with LGS), positive effects were noted in four patients, including reduced irritability and hyperactivity, improved speech and social interactions; however, negative effects were observed in three patients including increased temper tantrums, hyperactivity, irritability and poor cooperation [232].
Insomnia/sleep disturbances has been reported as a dose-dependent AE in a number of studies including in patients with LGS [231, 233, 234], although other studies have shown no major effect on sleep parameters including nocturnal sleep or daytime somnolence [235, 236]. Overall, LTG is predominantly a favourable ASM in terms of PBAEs, cognition and behaviour, although it may be related to insomnia.
4.2 Rufinamide (RUF)
Rufinamide was approved as adjunctive therapy for the treatment of seizures associated with LGS in the EU and the USA in 2007 and 2008, respectively [237, 238] with evidence in patients with LGS garnered from RCTs [239,240,241]. Furthermore, a Cochrane analysis identified six studies in patients with DREs (Table S1 of the ESM) [242]. This triazole derivative is thought to act by prolonging the inactive state of voltage-gated sodium channels, although the exact mechanisms are unknown [237, 238]. Rufinamide is a well-tolerated ASM (Table 2) [237, 238, 242, 243]. Somnolence and anxiety were the only psychiatric disorders “commonly” experienced by patients in the regulatory trials. Psychobehavioural AEs have not been notable in RUF clinical trials and observational studies [239, 242,243,244,245,246,247].
In one of the pivotal RCTs in LGS paediatric patients (aged ≥ 1 to < 4 years; n = 25 in the RUF group vs 12 in the placebo group), no statistically significant differences were observed between groups for mean CBCL total problems score assessed every 24 weeks up to 106 weeks [239]. Similarly, an observational multicentre prospective study of 16 patients with LGS (aged 7–58 years) found no statistically significant differences from baseline in behaviour (CBCL), intellectual functioning (LEITER-R) and adaptive functions (Vineland Adaptive Behavior Scale) after 12 months of treatment with RUF [246]. No studies specifically examining sleep parameters were identified. Overall, RUF does not negatively impact patients in terms of PBAEs, cognition and behaviour.
5 Additional ASMs Used in the Treatment of TSC
5.1 Vigabatrin (VGB)
Vigabatrin is indicated as an adjunct therapy for refractory focal seizures and as monotherapy for infantile spasms (IS) [248, 249]. The efficacy and safety of VGB for IS in patients with TSC was evaluated in an RCT, and it has also been evaluated in retrospective observational studies for IS and focal seizures in patients with TSC [250,251,252,253]. In patients with DREs, VGB has been evaluated in 11 RCTs as per a recent Cochrane analysis (Table S1 of the ESM) [254]. Vigabatrin, a structural analogue of GABA, was rationally designed to bind irreversibly to the enzyme responsible for the breakdown of GABA (GABA-transaminase), thus increasing GABA levels in the brain [248, 249]. A significant drawback of VGB is its frequent association with visual field defects, reported to occur in up to a third of patients, with a range in severity from mild to irreversible vision loss [248, 249]. As such VGB is not commonly used for DREs in general, and is primarily used for IS in patients with TSC. Other AEs include sedation, drowsiness, fatigue and impaired concentration, with excitation or agitation being frequent in children (Table 2). In addition to concerns regarding visual field defects, VGB has a relatively poor PBAE profile in patients with focal seizures, associated with depression and to a lesser extent psychosis (Table S1 of the ESM) [254, 255]. Of note, some observational studies have reported high discontinuation rates with VGB because of PBAEs (6–22% across studies) [256,257,258,259,260].
Three trials have evaluated cognitive outcomes in patients with focal seizures [261,262,263,264,265,266]; one trial reported small dose-dependent negative effects in cognitive performance from the Digit Cancellation Test, but otherwise VBG showed little impact on an extensive range of cognitive tests across the studies [261, 263]. However, improved cognitive and behavioural outcomes, including developmental quotient, autistic behaviour and verbal level, was observed in patients with TSC with infantile spasms treated with VGB, but not in patients with focal seizures [267]. No studies specifically evaluating the effects of VGB on sleep parameters, above and beyond the AEs, were identified in this review.
Studies have shown that early control of seizures benefits cognitive/behavioural outcomes in TSC [250, 268]. Vigabatrin has been at the forefront of preventative treatment in TSC: the EPISTOP trial evaluated conventional VGB treatment (after the first electrographic or clinical seizure; n = 29) versus preventive treatment (when epileptiform electroencephalogram activity was detected before the first seizure; n = 25) [269]. Preventative treatment significantly reduced the risk of clinical seizures; however, the neurodevelopment benefits were less clear because of the low occurrence of deficits in both groups: none of the patients across groups had a severe learning disability at 2 years of age, and while fewer patients had a neurodevelopmental delay at age 2 years with preventative treatment, the difference was not statistically significant (33% vs 50%). The authors hypothesised that the lack of a difference between groups may have been due to the small number of patients, short follow-up duration and/or the rigorous treatment strategies employed at an early stage in both groups (median age was similar across groups, and all children were aged less than 10 weeks at enrolment), or conversely that the window of opportunity may already have passed in some patients.
Overall, VGB may be associated with some PBAEs such as depression and psychosis. Vigabatrin treatment may have some positive effects on cognition and behaviour in patients with IS, but does not seem to have an effect in patients with focal seizures. The effects of early treatment (before seizure onset) on neurodevelopmental outcomes are thus far inconclusive.
5.2 Everolimus (EVE)
Everolimus, an oral protein kinase inhibitor of the mTOR signalling, is a targeted therapy indicated for the treatment of refractory seizures and subependymal giant cell astrocytoma associated with TSC [270, 271]. The EXIST-3 RCT evaluated the efficacy and safety of EVE for controlling focal seizures associated with TSC [272]. Everolimus has immunosuppressive effects and therefore patients may be at increased risk of infections, but it generally has a good tolerability profile (Table 2) [270, 271]. Psychiatric disorders including insomnia, aggression and irritability are reported to be common (≥ 1/100 to < 1/10) [270]. In a real-world study involving 134 patients with TSC treated with EVE, stomatitis was the most frequently reported AE, while EVE was not associated with PBAEs [273].
Two RCTs that specifically evaluated the effects of EVE on TSC-associated neuropsychiatric disorders in children with TSC aged ≥ 6 years failed to find any significant benefits of EVE compared to placebo over a range of cognitive/behavioural outcomes [274, 275]. The first study, conducted in children and young adults with TSC aged 6–21 years, found no significant difference in patients treated with EVE (n = 32) versus placebo (n = 15) for most of the neuropsychological measures (memory, attention, executive function, behaviour), although there were some trends towards improvements in parental ratings of behaviour, social skills in older children/young adults and depressed mood in younger children [274]. In line with those results, the other RCT, which evaluated EVE (n = 15) versus placebo (n = 17) in children aged 4–17 years with TSC and intellectual impairment (IQ < 80, learning disability, special schooling or autism), without intractable seizures, there was also no benefit of EVE compared to placebo for measures of IQ, autism, visual and fine motor skills, memory and executive functioning [275]. Similarly, no improvements were observed for behavioural and emotional problems at home and at school, social functioning, communication skills, executive functioning, sleep, QoL or sensory processing, as assessed using parent and teacher questionnaires. In contrast, a small study of six patients with TSC aged 7.5–23 years demonstrated improvements in behaviour and cognition in some patients: improvement in inattention and concentration occurred in three patients, improvements in social interactions, speech and verbal responses were experienced in three out of four patients with ASD, while aggression and irritability decreased in one patient but increased in another [276]. Furthermore, Kadish et al. reported a modest increase in absolute values of developmental age for development and adaptive functioning, suggesting that although EVE may not reverse TSC-associated neuropsychiatric disorders, it may help to narrow the gap in developmental delay [277]. Studies have begun to assess EVE in younger children and infants; however, no consistent improvements in neurodevelopment have been observed in this age group [278, 279].
The existing data suggest that EVE may be associated with some PBAEs including aggression and irritability. Some behavioural improvements in patients with TSC have been reported in observational studies, but RCTs demonstrated no improvements compared with placebo across a comprehensive set of cognitive and behavioural measures in children aged ≥ 6 years.
5.3 Lacosamide (LCM)
Lacosamide is indicated as monotherapy and adjunctive therapy for focal seizures [280, 281]. The efficacy and tolerability of LCM in patients with LGS were reported in an observational study [282], while a Cochrane analysis identified five trials in patients with DREs (Table S1 of the ESM) [283]. Although the mechanism of action is not fully understood, LCM works selectively to increase slow inactivation in voltage-gated sodium channels, which in turn causes inhibition of repetitive neuronal firing involved in seizures [284].
Lacosamide is considered an effective and well tolerated treatment (Table 2), with a PBAE and cognitive profile that is similar to placebo, as evidenced from a pooled analysis of RCTs evaluating LCM in adults with epilepsy [285]. A recent SLR found overwhelming evidence from 251 studies that the effects of LCM on cognitive and mood were negligible [286]. In line with this, another SLR conducted to assess the impact of LCM on mood in adult patients with epilepsy found that studies either reported a neutral or positive effect, including positive effects on depressive and anxiety symptoms [287]. A SLR in patients with DRE [288], and another specifically in patients with LGS [289], have noted that LCM can be associated with adverse mood and behavioural changes; however, AEs rarely led to discontinuations [288]. Of note, studies have suggested that LCM is effective and tolerable, with good retention rates in patients with epilepsy and intellectual disability [290, 291]; a slower titration in the first 3 months of initiating LCM has been recommended to reduce PBAEs [290]. Finally, the available evidence suggests that LCM improves or has no effect on sleep, with a low incidence of daytime sleepiness [38].
Current evidence suggests LCM-related AEs are generally mild and well tolerated, with minimal detrimental effects on cognition, sleep and PBAEs, while it may even improve some psychiatric symptoms in patients.
6 Less Frequently Used ASMs
6.1 Bromide
Bromide is the oldest ASM and is used to treat severe epilepsy in children, notably myoclonic seizures or DS [292]. Bromide increases noradrenaline and serotonin release and acts primarily through GABAergic inhibition via hyperpolarisation of postsynaptic membranes [293]. Bromide is not widely used because of historical concerns regarding psychiatric toxicities (bromism) that can cause somnolence, psychosis and hallucinations, and in severe cases coma, paralysis or even death [293]. However, at lower doses used in patients with DS, studies in Germany and Japan (where it is more widely used) have shown it be efficacious and tolerable with drowsiness, loss of weight and loss of appetite being the most commonly reported AEs [294,295,296,297,298]. A 1994 paper reported that only a minority of patients experienced deterioration of cognition following bromide treatment, while some even reported improvements [299]. However, there are no studies specifically investigating effects on cognition or behaviour in patients receiving bromide. In conclusion, bromide is not widely used because of the potential for serious side effects, and although studies suggest PBAEs are not prevalent in patients with DS, data are limited.
6.2 Felbamate (FLB)
Felbamate is indicated in the USA for the treatment of patients with LGS [300], but is not licenced in the EU because of safety concerns surrounding the risk of fatal aplastic anaemia and hepatic failure. However, it is available is some European countries based on national regulations. Felbamate was assessed by the Felbamate Study Group in an RCT in patients with LGS [301]. Felbamate is thought to work mainly through blockage of sodium channels and inhibition of glutamate neurotransmission via NMDA receptors [130, 201]. Typical AEs related to FLB include anorexia, vomiting, insomnia and nausea in both children and adults [300]. Somnolence and headache are also considered common, as well as dizziness in adults [300]. Psychobehavioural AE data with FLB in DREs are limited; however, in a study of 20 children with LGS who had been taking FLB for 1–22 months (median = 3.5 months), parents reported significant improvements for social, intellectual and motor functioning, attention and concentration, alertness, initiative, variability in performance and memory [302]. Because of serious side effects, 17 children discontinued the treatment. In a placebo-controlled study of 30 patients with refractory epilepsy, half the patients had deterioration of psychiatric conditions alongside stimulant effects, while the other half showed a slight psychiatric improvement [303]. In terms of sleep, it has been reported the FLB either worsens or has no effect on sleep [303]. Overall, data on the effects of FLB on PBAEs, cognition and sleep are too limited to make any conclusions.
6.3 Sodium Channel Blockers and GABA Agonists
Other sodium channel blocker ASMs include carbamazepine, eslicarbazepine acetate, oxcarbazepine and phenytoin. In general, they all have a similar AE profile to LTG and LCM, with a minimal impact on PBAEs, while the effects on sleep vary based on different sedating effects (Table S1 of the ESM). The recently approved cenobamate acts on voltage-gated sodium channels and the GABAergic system; however, experience in children or DEEs is not yet sufficient to make recommendations [304]. Likewise, the GABA agonists gabapentin and pregabalin have a benign PBAE profile, and pregabalin may have a positive impact on sleep maintenance [305]; however, both drugs have to be used with caution in DEEs as they can exacerbate seizures, especially in DS and in genetic generalised epilepsies.
7 Discussion
Deciphering the effects of ASMs on cognition, behaviour, psychiatric symptoms and sleep is challenging and complex. The causes of these comorbidities associated with DEEs are multi-factorial (Fig. 2) [6], the specific manifestations are highly individual and can naturally evolve over time, and cognition, behaviour, psychiatric symptoms and sleep impairments may all be inter-linked [7, 306]. While it is clear that ASMs themselves are associated with various PBAEs (which improve upon dose reductions or discontinuation), the overall complex nature of behaviour, cognition and sleep tends to mean that studies analysing the effects of ASMs on these comorbidities have heterogenous results, and conclusions can be difficult to make. Indeed, many questions remain that could help us better interpret the evidence and help improve patient outcomes. These relate to (1) the tailoring of treatments to specific individuals based on their risk of developing PBAEs, i.e. what are the effects of age/sex/age of onset/severity of seizures/seizure type/ having a history of the comorbidity/specific genotypes? (2) The practical details of using ASMs, i.e. what are the effects of different doses and titration schedules, and the effects of polypharmacy and interactions between particular combinations of ASMs and other drugs? (3) Understanding the mechanisms of the effects of ASMs, e.g. are positive/negative effects due the underlying mechanisms of the ASMs themselves, or through their improvements/lack of improvements in seizures, or are both inherently connected? (4) What are the genetic factors involved in adverse drug reactions?
Studies are trying to elicit the answers to these questions. For example, the area of pharmacogenomics is growing with the aim of personalising therapies based on an individual’s genetic profile with regard to variants that affect response and AEs [307]. With this in mind, the HLA-A*11:01 allele has been identified as possibly being associated with LEV-induced psychiatric AEs [308]. Furthermore, several studies documented herein suggest that having a history of psychiatric or behavioural problems is a predictor of PBAEs [36, 37]. In addition, experiencing PBAEs with one ASM may increase the risk of having PBAEs with another ASM [309]. Regarding polypharmacy, AEs may increase with an increasing number of concomitant ASMs [310, 311], and studies suggest that increased drug load may be related to some poorer cognitive outcomes including impaired memory [312, 313] and executive functions [306].
In addition to the underlying aetiology of the disease, evidence suggests that seizures themselves can exacerbate the neurodevelopmental comorbidities in DEEs; early age of seizure onset and occurrence of (severe) seizures (e.g. status epilepticus in DS and infantile spasms in TSC) have been associated with negative impacts on neurodevelopment outcomes in patients with DS, TSC and other DEEs [314,315,316,317,318,319,320]. In this respect, effects on psychobehavioural and cognitive outcomes may reflect the ASM’s efficacy on seizures, i.e. a lack of neurodevelopmental deterioration may be because of good seizure control, while conversely, adverse effects could be due to poor seizure control. However, positive effects of ASMs that lead to actual improvements in psychobehavioural and cognitive outcomes may be more complex and challenging, requiring early/preventative treatment and/or therapies that target the underlying molecular mechanisms. Regarding the former, the use of preventative treatment before seizures begin is being evaluated in TSC, although no conclusions with regard to TSC-associated neuropsychiatric disorders have been made thus far. Regarding targeted therapies, there is preliminary evidence that some ASMs may have a mode of action that could more directly improve aspects of cognition. For example, FFA acts as a positive modulator of the sigma-1 receptor, a protein that has been implicated in multiple cognitive disorders [104, 321]. In addition, CBD appears to have potential as a treatment for mental health and cognitive and behavioural disorders [90, 91], suggesting it may have mechanisms of action independent of seizure activity. Additionally, of note, a phenomenon denoted “forced normalisation” exists whereby patients experience psychiatric disturbances, but when seizure control or epileptiform electroencephalogram patterns are improved, usually triggered by successful ASM treatment or epilepsy surgery [322, 323]. The pathophysiology of this condition is still unclear, but it further shows the complex interplay between disease aetiology, drug effect and seizures [322, 323].
Developmental and epileptic encephalopathies are complex syndromes; however, treatment often primarily focuses on seizure control, and there is a need for improvements in the identification and treatment of the developmental, behavioural and psychiatric comorbidities (including treatment-related exacerbations) [12, 15, 324, 325]. The management of DEEs requires a rational, holistic and multi-disciplinary approach tailored to the unique circumstances of the individual patient and their evolving symptoms throughout all stages of childhood, adolescence and adulthood, including a smooth transition from paediatric to adult care [12, 15, 324, 325]. Indeed, the comorbidities can be the predominant burden in older children and adults when seizures decrease [320, 326, 327]. As part of this approach, clinicians should also actively screen for treatment-related AEs affecting these comorbidities and adjust treatment accordingly. This is particularly pertinent when considering the substantial impact that these comorbidities have on the QoL of patients with DEEs and their family caregivers [9,10,11,12,13, 312, 328]. Furthermore, comorbidities contribute to the heavy economic burden that DEEs impose on healthcare systems, families and society [329,330,331,332].
Additional novel treatments that target the underlying pathogenesis of both seizures and the neurodevelopment comorbidities would also be welcome. In this respect, soticlestat, which has a novel mechanism of action as an inhibitor of cholesterol 24-hydroxylase, is in clinical development as adjunctive therapy in children with DS or LGS [333]. To date, soticlestat has been found to be well tolerated and was associated with significant reductions in seizure frequency in patients with DS and LGS [333].
8 Conclusions
As evidenced here, there is a growing literature base on the effects of ASMs on PBAEs, cognition and sleep; however, there are still many limitations: RCTs may exclude relevant populations, while observational studies lack a placebo arm and are often small. Furthermore, evaluations often rely on caregivers’ perspectives, which are inherently subjective, and, among a plethora of options for examining behaviour and cognition, there is a lack of standardised measurements for DEEs. There is also variability in the extent of evidence for each ASM: for first-generation, and some second-generation ASMs, there is scant documented evidence; however, the extensive use of VPA and CLB suggests favourable tolerability and safety. Second-generation and some third-generation ASMs tend to have the most robust evidence documented over several years of use, while evidence is still being generated for newer ASMs such as CBD and FFA.
Despite some clinical challenges and limitations in the evidence base, trends on the effects of ASMs on cognition, behaviour, psychiatric symptoms and sleep have become apparent over time. Overall, the current evidence suggests that LEV and PER and to a lesser extent BRV are associated with PBAEs including aggressiveness and irritability; TPM and to a lesser extent ZNS are associated with language impairment and cognitive dulling/memory problems. Topiramate and ZNS may be associated with negative effects in some aspects of cognition, while CBD, FFA, LEV, BRV and LTG may have some positive effects. Cannabidiol, PER and pregabalin may be associated with improvements in sleep, and LTG may be associated with insomnia. Finally, all the ASMs are associated with sedation to a certain extent.
References
Raga S, Specchio N, Rheims S, et al. Developmental and epileptic encephalopathies: recognition and approaches to care. Epileptic Disord. 2021;23(1):40–52. https://doi.org/10.1684/epd.2021.1244.
Schubert-Bast S, Strzelczyk A. Review of the treatment options for epilepsy in tuberous sclerosis complex: towards precision medicine. Ther Adv Neurol Disord. 2021;14:17562864211031100. https://doi.org/10.1177/17562864211031100.
Strzelczyk A, Schubert-Bast S. Therapeutic advances in Dravet syndrome: a targeted literature review. Expert Rev Neurother. 2020;20(10):1065–79. https://doi.org/10.1080/14737175.2020.1801423.
Strzelczyk A, Schubert-Bast S. Expanding the treatment landscape for Lennox-Gastaut syndrome: current and future strategies. CNS Drugs. 2021;35(1):61–83. https://doi.org/10.1007/s40263-020-00784-8.
Strzelczyk A, Schubert-Bast S. A practical guide to the treatment of Dravet syndrome with anti-seizure medication. CNS Drugs. 2022;36(3):217–37. https://doi.org/10.1007/s40263-022-00898-1.
Berg AT. Epilepsy, cognition, and behavior: the clinical picture. Epilepsia. 2011;52 Suppl. 1(Suppl. 1):7–12. https://doi.org/10.1111/j.1528-1167.2010.02905.x.
Gibbon FM, Maccormac E, Gringras P. Sleep and epilepsy: unfortunate bedfellows. Arch Dis Child. 2019;104(2):189–92. https://doi.org/10.1136/archdischild-2017-313421.
Bonilla-Jaime H, Zeleke H, Rojas A, et al. Sleep disruption worsens seizures: neuroinflammation as a potential mechanistic link. Int J Mol Sci. 2021;22(22):12531. https://doi.org/10.3390/ijms222212531.
Silva B, Moniz E, Barahona-Corrêa B. 2 Psychiatric comorbidity and quality of life in drug-resistant epilepsy. J Neurol Neurosurg Psychiatry. 2017;88(8):A13. https://doi.org/10.1136/jnnp-2017-BNPA.26.
Welton JM, Walker C, Riney K, et al. Quality of life and its association with comorbidities and adverse events from antiepileptic medications: online survey of patients with epilepsy in Australia. Epilepsy Behav. 2020;104: 106856. https://doi.org/10.1016/j.yebeh.2019.106856.
Lagae L, Brambilla I, Mingorance A, et al. Quality of life and comorbidities associated with Dravet syndrome severity: a multinational cohort survey. Dev Med Child Neurol. 2018;60(1):63–72. https://doi.org/10.1111/dmcn.13591.
Marchese F, Cappelletti S, Filippini M, et al. Comorbidities in Dravet syndrome and Lennox-Gastaut syndrome. SN Compr Clin Med. 2021;3(10):2167–79. https://doi.org/10.1007/s42399-021-00989-y.
Sinoo C, de Lange IM, Westers P, et al. Behavior problems and health-related quality of life in Dravet syndrome. Epilepsy Behav. 2019;90:217–27. https://doi.org/10.1016/j.yebeh.2018.11.029.
de Kinderen RJ, Evers SM, Rinkens R, et al. Side-effects of antiepileptic drugs: the economic burden. Seizure. 2014;23(3):184–90. https://doi.org/10.1016/j.seizure.2013.11.009.
Cardenal-Muñoz E, Auvin S, Villanueva V, et al. Guidance on Dravet syndrome from infant to adult care: road map for treatment planning in Europe. Epilepsia Open. 2022;7(1):11–26. https://doi.org/10.1002/epi4.12569.
Knupp KG, Wirrell EC. Treatment strategies for Dravet syndrome. CNS Drugs. 2018;32(4):335–50. https://doi.org/10.1007/s40263-018-0511-y.
Andrade DM, Berg AT, Hood V, et al. Dravet syndrome: a quick transition guide for the adult neurologist. Epilepsy Res. 2021;177: 106743. https://doi.org/10.1016/j.eplepsyres.2021.106743.
Montouris G, Aboumatar S, Burdette D, et al. Expert opinion: proposed diagnostic and treatment algorithms for Lennox-Gastaut syndrome in adult patients. Epilepsy Behav. 2020;110: 107146. https://doi.org/10.1016/j.yebeh.2020.107146.
Cross JH, Auvin S, Falip M, et al. Expert opinion on the management of Lennox-Gastaut syndrome: treatment algorithms and practical considerations. Front Neurol. 2017;8:505. https://doi.org/10.3389/fneur.2017.00505.
Riva A, Coppola A, Bonaventura CD, et al. An Italian consensus on the management of Lennox-Gastaut syndrome. Seizure. 2022;101:134–40. https://doi.org/10.1016/j.seizure.2022.07.004.
Verrotti A, Striano P, Iapadre G, et al. The pharmacological management of Lennox-Gastaut syndrome and critical literature review. Seizure. 2018;63:17–25. https://doi.org/10.1016/j.seizure.2018.10.016.
Northrup H, Aronow ME, Bebin EM, et al. Updated international tuberous sclerosis complex diagnostic criteria and surveillance and management recommendations. Pediatr Neurol. 2021;123:50–66. https://doi.org/10.1016/j.pediatrneurol.2021.07.011.
Canevini MP, Kotulska-Jozwiak K, Curatolo P, et al. Current concepts on epilepsy management in tuberous sclerosis complex. Am J Med Genet C Semin Med Genet. 2018;178(3):299–308. https://doi.org/10.1002/ajmg.c.31652.
Curatolo P, Nabbout R, Lagae L, et al. Management of epilepsy associated with tuberous sclerosis complex: updated clinical recommendations. Eur J Paediatr Neurol. 2018;22(5):738–48. https://doi.org/10.1016/j.ejpn.2018.05.006.
van der Poest CE, Jansen FE, Braun KPJ, et al. Update on drug management of refractory epilepsy in tuberous sclerosis complex. Pediatr Drugs. 2020;22(1):73–84. https://doi.org/10.1007/s40272-019-00376-0.
Nabbout R, Kuchenbuch M, Chiron C, et al. Pharmacotherapy for seizures in tuberous sclerosis complex. CNS Drugs. 2021;35(9):965–83. https://doi.org/10.1007/s40263-021-00835-8.
Munger Clary HM, Croxton RD, Allan J, et al. Who is willing to participate in research? A screening model for an anxiety and depression trial in the epilepsy clinic. Epilepsy Behav. 2020;104(Pt A): 106907. https://doi.org/10.1016/j.yebeh.2020.106907.
Steinhoff BJ, Staack AM, Hillenbrand BC. Randomized controlled antiepileptic drug trials miss almost all patients with ongoing seizures. Epilepsy Behav. 2017;66:45–8. https://doi.org/10.1016/j.yebeh.2016.10.025.
Klein P, Devinsky O, French J, et al. Suicidality risk of newer antiseizure medications: a meta-analysis. JAMA Neurol. 2021;78(9):1118–27. https://doi.org/10.1001/jamaneurol.2021.2480.
Depakene (valproic acid). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/018081s065_018082s048lbl.pdf. Accessed 29 Aug 2022.
Epilim (sodium valproate). Summary of product characteristics. https://www.medicines.org.uk/emc/product/1446/smpc#gref. Accessed 29 Aug 2022.
Dressler A, Trimmel-Schwahofer P, Reithofer E, et al. Efficacy and tolerability of the ketogenic diet in Dravet syndrome: comparison with various standard antiepileptic drug regimen. Epilepsy Res. 2015;109:81–9. https://doi.org/10.1016/j.eplepsyres.2014.10.014.
Covanis A, Gupta AK, Jeavons PM. Sodium valproate: monotherapy and polytherapy. Epilepsia. 1982;23(6):693–720. https://doi.org/10.1111/j.1528-1157.1982.tb05085.x.
Overwater IE, Bindels-de Heus K, Rietman AB, et al. Epilepsy in children with tuberous sclerosis complex: chance of remission and response to antiepileptic drugs. Epilepsia. 2015;56(8):1239–45. https://doi.org/10.1111/epi.13050.
Wirrell EC, Laux L, Donner E, et al. Optimizing the diagnosis and management of Dravet syndrome: recommendations from a North American consensus panel. Pediatr Neurol. 2017;68:18-34.e3. https://doi.org/10.1016/j.pediatrneurol.2017.01.025.
Chen B, Choi H, Hirsch LJ, et al. Psychiatric and behavioral side effects of antiepileptic drugs in adults with epilepsy. Epilepsy Behav. 2017;76:24–31. https://doi.org/10.1016/j.yebeh.2017.08.039.
Chen B, Detyniecki K, Choi H, et al. Psychiatric and behavioral side effects of anti-epileptic drugs in adolescents and children with epilepsy. Eur J Paediatr Neurol. 2017;21(3):441–9. https://doi.org/10.1016/j.ejpn.2017.02.003.
Liguori C, Toledo M, Kothare S. Effects of anti-seizure medications on sleep architecture and daytime sleepiness in patients with epilepsy: a literature review. Sleep Med Rev. 2021;60: 101559. https://doi.org/10.1016/j.smrv.2021.101559.
Esmael A, Elsherief M, Abdelsalam M, et al. Sleep architecture in valproate-induced nocturnal enuresis in primary school and preschool children. J Child Neurol. 2020;35(14):975–82. https://doi.org/10.1177/0883073820944051.
Ozan K, Coskun Y, Bora CK, et al. Valproic acid-induced nocturnal enuresis in pediatric patients. Niger J Clin Pract. 2019;22(1):108–12. https://doi.org/10.4103/njcp.njcp_120_18.
Balagura G, Iapadre G, Verrotti A, et al. Moving beyond sodium valproate: choosing the right anti-epileptic drug in children. Expert Opin Pharmacother. 2019;20(12):1449–56. https://doi.org/10.1080/14656566.2019.1617850.
Degremont A, Kerbrat S, Balusson F, et al. Prescribing trends for valproate among pregnant women. Neurology. 2022;98(21): e2163. https://doi.org/10.1212/WNL.0000000000200260.
Choi CS, Gonzales EL, Kim KC, et al. The transgenerational inheritance of autism-like phenotypes in mice exposed to valproic acid during pregnancy. Sci Rep. 2016;6(1):36250. https://doi.org/10.1038/srep36250.
Martin M, Hill C, Bewley S, et al. Transgenerational adverse effects of valproate? A patient report from 90 affected families. Birth Defects Res. 2022;114(1):13–6. https://doi.org/10.1002/bdr2.1967.
Tartaglione AM, Cipriani C, Chiarotti F, et al. Early behavioral alterations and increased expression of endogenous retroviruses are inherited across generations in mice prenatally exposed to valproic acid. Mol Neurobiol. 2019;56(5):3736–50. https://doi.org/10.1007/s12035-018-1328-x.
Frisium (clobazam). Summary of product characteristics. https://www.medicines.org.uk/emc/product/1574/smpc#gref. Accessed 29 Aug 2022.
ONFI (clobazam). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/203993s005lbl.pdf. Accessed 29 Aug 2022.
Ng YT, Conry JA, Drummond R, et al. Randomized, phase III study results of clobazam in Lennox-Gastaut syndrome. Neurology. 2011;77(15):1473–81. https://doi.org/10.1212/WNL.0b013e318232de76.
Conry JA, Ng YT, Kernitsky L, et al. Stable dosages of clobazam for Lennox-Gastaut syndrome are associated with sustained drop-seizure and total-seizure improvements over 3 years. Epilepsia. 2014;55(4):558–67. https://doi.org/10.1111/epi.12561.
Conry JA, Ng YT, Paolicchi JM, et al. Clobazam in the treatment of Lennox-Gastaut syndrome. Epilepsia. 2009;50(5):1158–66. https://doi.org/10.1111/j.1528-1167.2008.01935.x.
Jennesson M, van Eeghen AM, Caruso PA, et al. Clobazam therapy of refractory epilepsy in tuberous sclerosis complex. Epilepsy Res. 2013;104(3):269–74. https://doi.org/10.1016/j.eplepsyres.2012.10.010.
Brodie MJ, Chung S, Wade A, et al. Clobazam and clonazepam use in epilepsy: results from a UK database incident user cohort study. Epilepsy Res. 2016;123:68–74. https://doi.org/10.1016/j.eplepsyres.2016.04.003.
Klehm J, Thome-Souza S, Sánchez Fernández I, et al. Clobazam: effect on frequency of seizures and safety profile in different subgroups of children with epilepsy. Pediatr Neurol. 2014;51(1):60–6. https://doi.org/10.1016/j.pediatrneurol.2014.01.025.
Lee EH, Yum MS, Choi HW, et al. Long-term use of clobazam in Lennox-Gastaut syndrome: experience in a single tertiary epilepsy center. Clin Neuropharmacol. 2013;36(1):4–7. https://doi.org/10.1097/WNF.0b013e3182770730.
Montenegro MA, Arif H, Nahm EA, et al. Efficacy of clobazam as add-on therapy for refractory epilepsy: experience at a US epilepsy center. Clin Neuropharmacol. 2008;31(6):333–8. https://doi.org/10.1097/WNF.0b013e31815cd960.
Paolicchi JM, Ross G, Lee D, et al. Clobazam and aggression-related adverse events in pediatric patients with Lennox-Gastaut syndrome. Pediatr Neurol. 2015;53(4):338–42. https://doi.org/10.1016/j.pediatrneurol.2015.06.021.
Bawden HN, Camfield CS, Camfield PR, et al. The cognitive and behavioural effects of clobazam and standard monotherapy are comparable. Canadian Study Group for Childhood Epilepsy. Epilepsy Res. 1999;33(2–3):133–43. https://doi.org/10.1016/s0920-1211(98)00088-6.
Munn R, Farrell K. Open study of clobazam in refractory epilepsy. Pediatr Neurol. 1993;9(6):465–9. https://doi.org/10.1016/0887-8994(93)90026-9.
Weinstock A, Agarwal N, Farooq O, et al. Evaluation of the effects of clobazam on seizure control and quality of life in children with Lennox-Gastaut syndrome: a pilot study. J Child Neurol. 2019;34(8):432–9. https://doi.org/10.1177/0883073819836534.
Dujardin S, Pijpers A, Pevernagie D. Prescription drugs used in insomnia. Sleep Med Clin. 2018;13(2):169–82. https://doi.org/10.1016/j.jsmc.2018.03.001.
Topamax (topiramate). Summary of product characteristics. https://www.medicines.org.uk/emc/product/1442/smpc#gref. Accessed 29 Aug 2022.
Topamax (topiramate). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020505s057_020844s048lbl.pdf. Accessed 29 Aug 2022.
Sachdeo RC, Glauser TA, Ritter F, et al. A double-blind, randomized trial of topiramate in Lennox-Gastaut syndrome. Topiramate YL Study Group. Neurology. 1999;52(9):1882–7. https://doi.org/10.1212/wnl.52.9.1882.
Nieto-Barrera M, Candau R, Nieto-Jimenez M, et al. Topiramate in the treatment of severe myoclonic epilepsy in infancy. Seizure. 2000;9(8):590–4. https://doi.org/10.1053/seiz.2000.0466.
Kröll-Seger J, Portilla P, Dulac O, et al. Topiramate in the treatment of highly refractory patients with Dravet syndrome. Neuropediatrics. 2006;37(6):325–9. https://doi.org/10.1055/s-2007-964867.
Bresnahan R, Hounsome J, Jette N, et al. Topiramate add-on therapy for drug-resistant focal epilepsy. Cochrane Database Syst Rev. 2019;10(10):CD001417. https://doi.org/10.1002/14651858.CD001417.pub4.
Buckley A, Fitzgerald M, Hoerold D, et al. Effects of the anticonvulsant topiramate on language abilities in people with epilepsy: a cross-sectional study. Ir J Psychol Med. 2010;27(4):179–83. https://doi.org/10.1017/s0790966700001488.
Kim SJ, Kim MY, Choi YM, et al. Effects of topiramate on language functions in newly diagnosed pediatric epileptic patients. Pediatr Neurol. 2014;51(3):324–9. https://doi.org/10.1016/j.pediatrneurol.2014.05.033.
Kockelmann E, Elger CE, Helmstaedter C. Cognitive profile of topiramate as compared with lamotrigine in epilepsy patients on antiepileptic drug polytherapy: relationships to blood serum levels and comedication. Epilepsy Behav. 2004;5(5):716–21. https://doi.org/10.1016/j.yebeh.2004.06.017.
Brandt C, Lahr D, May TW. Cognitive adverse events of topiramate in patients with epilepsy and intellectual disability. Epilepsy Behav. 2015;45:261–4. https://doi.org/10.1016/j.yebeh.2014.12.043.
Donegan S, Dixon P, Hemming K, et al. A systematic review of placebo-controlled trials of topiramate: How useful is a multiple-indications review for evaluating the adverse events of an antiepileptic drug? Epilepsia. 2015;56(12):1910–20. https://doi.org/10.1111/epi.13209.
Witt JA, Elger CE, Helmstaedter C. Impaired verbal fluency under topiramate: evidence for synergistic negative effects of epilepsy, topiramate, and polytherapy. Eur J Neurol. 2013;20(1):130–7. https://doi.org/10.1111/j.1468-1331.2012.03814.x.
Kim S-Y, Lee H-W, Jung D-K, et al. Cognitive effects of low-dose topiramate compared with oxcarbazepine in epilepsy patients. J Clin Neurol. 2006;2(2):126–33. https://doi.org/10.3988/jcn.2006.2.2.126.
Lee HW, Jung DK, Suh CK, et al. Cognitive effects of low-dose topiramate monotherapy in epilepsy patients: a 1-year follow-up. Epilepsy Behav. 2006;8(4):736–41. https://doi.org/10.1016/j.yebeh.2006.03.006.
Loring DW, Williamson DJ, Meador KJ, et al. Topiramate dose effects on cognition: a randomized double-blind study. Neurology. 2011;76(2):131–7. https://doi.org/10.1212/WNL.0b013e318206ca02.
Coppola G, Caliendo G, Veggiotti P, et al. Topiramate as add-on drug in children, adolescents and young adults with Lennox-Gastaut syndrome: an Italian multicentric study. Epilepsy Res. 2002;51(1–2):147–53. https://doi.org/10.1016/s0920-1211(02)00103-1.
Dooley JM, Camfield PR, Smith E, et al. Topiramate in intractable childhood onset epilepsy: a cautionary note. Can J Neurol Sci. 1999;26(4):271–3. https://doi.org/10.1017/s0317167100000366.
Coppola G, Verrotti A, Resicato G, et al. Topiramate in children and adolescents with epilepsy and mental retardation: a prospective study on behavior and cognitive effects. Epilepsy Behav. 2008;12(2):253–6. https://doi.org/10.1016/j.yebeh.2007.09.001.
Kanner AM, Wuu J, Faught E, et al. A past psychiatric history may be a risk factor for topiramate-related psychiatric and cognitive adverse events. Epilepsy Behav. 2003;4(5):548–52. https://doi.org/10.1016/j.yebeh.2003.07.007.
Kelly K, Stephen LJ, Sills GJ, et al. Topiramate in patients with learning disability and refractory epilepsy. Epilepsia. 2002;43(4):399–402. https://doi.org/10.1046/j.1528-1157.2002.47401.x.
Bonanni E, Galli R, Maestri M, et al. Daytime sleepiness in epilepsy patients receiving topiramate monotherapy. Epilepsia. 2004;45(4):333–7. https://doi.org/10.1111/j.0013-9580.2004.47803.x.
Shen Y, Zhang M, Wang Y, et al. Subjective sleep disturbance in Chinese adults with epilepsy: Associations with affective symptoms. Epilepsy Res. 2017;135:150–7. https://doi.org/10.1016/j.eplepsyres.2017.06.014.
Epidiolex. Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/210365s005s006s007lbl.pdf. Accessed 29 Aug 2022.
Epidyolex. Summary of product characteristics. https://www.medicines.org.uk/emc/product/10781#gref. Accessed 29 Aug 2022.
Thiele EA, Marsh ED, French JA, et al. Cannabidiol in patients with seizures associated with Lennox-Gastaut syndrome (GWPCARE4): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391(10125):1085–96. https://doi.org/10.1016/s0140-6736(18)30136-3.
Devinsky O, Patel AD, Cross JH, et al. Effect of cannabidiol on drop seizures in the Lennox-Gastaut syndrome. N Engl J Med. 2018;378(20):1888–97. https://doi.org/10.1056/NEJMoa1714631.
Devinsky O, Patel AD, Thiele EA, et al. Randomized, dose-ranging safety trial of cannabidiol in Dravet syndrome. Neurology. 2018;90(14):e1204–11. https://doi.org/10.1212/wnl.0000000000005254.
Miller I, Scheffer IE, Gunning B, et al. Dose-ranging effect of adjunctive oral cannabidiol vs placebo on convulsive seizure frequency in Dravet syndrome: a randomized clinical trial. JAMA Neurol. 2020;77(5):613–21. https://doi.org/10.1001/jamaneurol.2020.0073.
Thiele EA, Bebin EM, Bhathal H, et al. Add-on cannabidiol treatment for drug-resistant seizures in tuberous sclerosis complex: a placebo-controlled randomized clinical trial. JAMA Neurol. 2021;78(3):285–92. https://doi.org/10.1001/jamaneurol.2020.4607.
Black N, Stockings E, Campbell G, et al. Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(12):995–1010. https://doi.org/10.1016/s2215-0366(19)30401-8.
Berger M, Li E, Rice S, et al. Cannabidiol for treatment-resistant anxiety disorders in young people: an open-label trial. J Clin Psychiatry. 2022. https://doi.org/10.4088/JCP.21m14130.
Gray RA, Whalley BJ. The proposed mechanisms of action of CBD in epilepsy. Epileptic Disord. 2020;22(S1):10–5. https://doi.org/10.1684/epd.2020.1135.
Lattanzi S, Brigo F, Trinka E, et al. Efficacy and safety of cannabidiol in epilepsy: a systematic review and meta-analysis. Drugs. 2018;78(17):1791–804. https://doi.org/10.1007/s40265-018-0992-5.
Chesney E, Oliver D, Green A, et al. Adverse effects of cannabidiol: a systematic review and meta-analysis of randomized clinical trials. Neuropsychopharmacology. 2020;45(11):1799–806. https://doi.org/10.1038/s41386-020-0667-2.
Klotz KA, Grob D, Schönberger J, et al. Effect of cannabidiol on interictal epileptiform activity and sleep architecture in children with intractable epilepsy: a prospective open-label study. CNS Drugs. 2021;35(11):1207–15. https://doi.org/10.1007/s40263-021-00867-0.
Metternich B, Wagner K, Geiger MJ, et al. Cognitive and behavioral effects of cannabidiol in patients with treatment-resistant epilepsy. Epilepsy Behav. 2021;114(Pt A): 107558. https://doi.org/10.1016/j.yebeh.2020.107558.
Anderson CL, Evans V, Gorham L, et al. Seizure frequency, quality of life, behavior, cognition, and sleep in pediatric patients enrolled in a prospective, open-label clinical study with cannabidiol. Epilepsy Behav. 2021;124: 108325. https://doi.org/10.1016/j.yebeh.2021.108325.
Martin RC, Gaston TE, Thompson M, et al. Cognitive functioning following long-term cannabidiol use in adults with treatment-resistant epilepsy. Epilepsy Behav. 2019;97:105–10. https://doi.org/10.1016/j.yebeh.2019.04.044.
Fintepla. Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/212102s003lbl.pdf. Accessed Apr 2022.
Fintepla. Summary of product characteristics. https://www.medicines.org.uk/emc/product/11998/smpc#gref. Accessed 29 Aug 2022.
Lagae L, Sullivan J, Knupp K, et al. Fenfluramine hydrochloride for the treatment of seizures in Dravet syndrome: a randomised, double-blind, placebo-controlled trial. Lancet. 2019;394(10216):2243–54. https://doi.org/10.1016/s0140-6736(19)32500-0.
Nabbout R, Mistry A, Zuberi S, et al. Fenfluramine for treatment-resistant seizures in patients with Dravet syndrome receiving stiripentol-inclusive regimens: a randomized clinical trial. JAMA Neurol. 2020;77(3):300–8. https://doi.org/10.1001/jamaneurol.2019.4113.
Knupp KG, Scheffer IE, Ceulemans B, et al. Efficacy and safety of fenfluramine for the treatment of seizures associated with Lennox-Gastaut syndrome: a randomized clinical trial. JAMA Neurol. 2022;79(6):554–64. https://doi.org/10.1001/jamaneurol.2022.0829.
Martin P, Reeder T, Sourbron J, et al. An emerging role for sigma-1 receptors in the treatment of developmental and epileptic encephalopathies. Int J Mol Sci. 2021;22(16):8416. https://doi.org/10.3390/ijms22168416.
Sharawat IK, Panda PK, Kasinathan A, et al. Efficacy and tolerability of fenfluramine in patients with Dravet syndrome: a systematic review and meta-analysis. Seizure. 2021;85:119–26. https://doi.org/10.1016/j.seizure.2020.12.016.
Zhang L, Li W, Wang C. Efficacy and safety of fenfluramine in patients with Dravet syndrome: a meta-analysis. Acta Neurol Scand. 2021;143(4):339–48. https://doi.org/10.1111/ane.13387.
Strzelczyk A, Pringsheim M, Mayer T, et al. Efficacy, tolerability, and retention of fenfluramine for the treatment of seizures in patients with Dravet syndrome: compassionate use program in Germany. Epilepsia. 2021;62(10):2518–27. https://doi.org/10.1111/epi.17034.
Guerrini R, Specchio N, Aledo-Serrano Á, et al. An examination of the efficacy and safety of fenfluramine in adults, children, and adolescents with Dravet syndrome in a real-world practice setting: a report from the Fenfluramine European Early Access Program. Epilepsia Open. 2022. https://doi.org/10.1002/epi4.12624.10.1002/epi4.12624.
Bishop KI, Isquith PK, Gioia GA, et al. Improved everyday executive functioning following profound reduction in seizure frequency with fenfluramine: analysis from a phase 3 long-term extension study in children/young adults with Dravet syndrome. Epilepsy Behav. 2021;121(Pt A): 108024. https://doi.org/10.1016/j.yebeh.2021.108024.
Bishop KI, Isquith PK, Gioia GA, et al. Fintepla (fenfluramine) treatment improves everyday executive functioning in preschool children with Dravet syndrome: analysis from 2 pooled phase 3 clinical trials. Abstract 2.413 at American Epilepsy Society; 2021.
Bishop KI, Isquith PK, Gioia GA, et al. Fenfluramine treatment improves everyday executive functioning in patients with Lennox-Gastaut syndrome: analysis from a phase 3 clinical Trial. Neuropediatrics. 2021;52:S1–S53. https://doi.org/10.1055/s-0041-1739606.
Jensen MP, Gammaitoni AR, Galer BS, et al. Fenfluramine treatment for dravet syndrome: real-world benefits on quality of life from the caregiver perspective. Epilepsy Res. 2022;185: 106976. https://doi.org/10.1016/j.eplepsyres.2022.106976.
Martin P, de Witte PAM, Maurice T, et al. Fenfluramine acts as a positive modulator of sigma-1 receptors. Epilepsy Behav. 2020;105: 106989. https://doi.org/10.1016/j.yebeh.2020.106989.
Martin P, Maurice T, Gammaitoni A, et al. Fenfluramine modulates the anti-amnesic effects induced by sigma-1 receptor agonists and neuro(active)steroids in vivo. Epilepsy Behav. 2022;127: 108526. https://doi.org/10.1016/j.yebeh.2021.108526.
Keppra. Summary of product characteristics. https://www.medicines.org.uk/emc/product/2293/smpc#gref. Accessed 29 Aug 2022.
Keppra. Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021035s099,021505s038lbl.pdf. Accessed 29 Aug 2022.
Striano P, Coppola A, Pezzella M, et al. An open-label trial of levetiracetam in severe myoclonic epilepsy of infancy. Neurology. 2007;69(3):250–4. https://doi.org/10.1212/01.wnl.0000265222.24102.db.
Kim HJ, Kim SH, Kang H-C, et al. Adjunctive levetiracetam treatment in pediatric Lennox-Gastaut syndrome. Pediatr Neurol. 2014;51(4):527–31. https://doi.org/10.1016/j.pediatrneurol.2014.06.004.
Collins JJ, Tudor C, Leonard JM, et al. Levetiracetam as adjunctive antiepileptic therapy for patients with tuberous sclerosis complex: a retrospective open-label trial. J Child Neurol. 2006;21(1):53–7. https://doi.org/10.1177/08830738060210011201.
Mbizvo GK, Chandrasekar B, Nevitt SJ, et al. Levetiracetam add-on for drug-resistant focal epilepsy. Cochrane Database Syst Rev. 2020;6(6):CD001901. https://doi.org/10.1002/14651858.CD001901.pub3.
Lynch BA, Lambeng N, Nocka K, et al. The synaptic vesicle protein SV2A is the binding site for the antiepileptic drug levetiracetam. Proc Natl Acad Sci U S A. 2004;101(26):9861–6. https://doi.org/10.1073/pnas.0308208101.
Zaccara G, Giovannelli F, Giorgi FS, et al. Tolerability of new antiepileptic drugs: a network meta-analysis. Eur J Clin Pharmacol. 2017;73(7):811–7. https://doi.org/10.1007/s00228-017-2245-z.
Cao Y, He X, Zhao L, et al. Efficacy and safety of Levetiracetam as adjunctive treatment in children with focal onset seizures: a systematic review and meta-analysis. Epilepsy Res. 2019;153:40–8. https://doi.org/10.1016/j.eplepsyres.2019.04.001.
Chen D, Bian H, Zhang L. A meta-analysis of levetiracetam for randomized placebo-controlled trials in patients with refractory epilepsy. Neuropsychiatr Dis Treat. 2019;15:905–17. https://doi.org/10.2147/ndt.S188111.
Egunsola O, Choonara I, Sammons HM. Safety of levetiracetam in paediatrics: a systematic review. PLoS ONE. 2016;11(3): e0149686. https://doi.org/10.1371/journal.pone.0149686.
Halma E, de Louw AJ, Klinkenberg S, et al. Behavioral side-effects of levetiracetam in children with epilepsy: a systematic review. Seizure. 2014;23(9):685–91. https://doi.org/10.1016/j.seizure.2014.06.004.
Steinhoff BJ, Klein P, Klitgaard H, et al. Behavioral adverse events with brivaracetam, levetiracetam, perampanel, and topiramate: a systematic review. Epilepsy Behav. 2021;118: 107939. https://doi.org/10.1016/j.yebeh.2021.107939.
Verrotti A, Prezioso G, Di Sabatino F, et al. The adverse event profile of levetiracetam: a meta-analysis on children and adults. Seizure. 2015;31:49–55. https://doi.org/10.1016/j.seizure.2015.07.004.
Harden C. Safety profile of levetiracetam. Epilepsia. 2001;42(s4):36–9. https://doi.org/10.1111/j.1528-1167.2001.00008.x.
Besag FMC, Vasey MJ. Neurocognitive effects of antiseizure medications in children and adolescents with epilepsy. Pediatr Drugs. 2021;23(3):253–86. https://doi.org/10.1007/s40272-021-00448-0.
Moavero R, Santarone ME, Galasso C, et al. Cognitive and behavioral effects of new antiepileptic drugs in pediatric epilepsy. Brain Dev. 2017;39(6):464–9. https://doi.org/10.1016/j.braindev.2017.01.006.
Ulate-Campos A, Fernández IS. Cognitive and behavioral comorbidities: an unwanted effect of antiepileptic drugs in children. Semin Pediatr Neurol. 2017;24(4):320–30. https://doi.org/10.1016/j.spen.2017.10.011.
Levisohn PM, Mintz M, Hunter SJ, et al. Neurocognitive effects of adjunctive levetiracetam in children with partial-onset seizures: a randomized, double-blind, placebo-controlled, noninferiority trial. Epilepsia. 2009;50(11):2377–89. https://doi.org/10.1111/j.1528-1167.2009.02197.x.
Schiemann-Delgado J, Yang H, Loge Cde L, et al. A long-term open-label extension study assessing cognition and behavior, tolerability, safety, and efficacy of adjunctive levetiracetam in children aged 4 to 16 years with partial-onset seizures. J Child Neurol. 2012;27(1):80–9. https://doi.org/10.1177/0883073811417183.
de la Loge C, Hunter SJ, Schiemann J, et al. Assessment of behavioral and emotional functioning using standardized instruments in children and adolescents with partial-onset seizures treated with adjunctive levetiracetam in a randomized, placebo-controlled trial. Epilepsy Behav. 2010;18(3):291–8. https://doi.org/10.1016/j.yebeh.2010.04.017.
Thelengana A, Shukla G, Srivastava A, et al. Cognitive, behavioural and sleep-related adverse effects on introduction of levetiracetam versus oxcarbazepine for epilepsy. Epilepsy Res. 2019;150:58–65. https://doi.org/10.1016/j.eplepsyres.2019.01.004.
Briviact (brivaracetam). Summary of product characteristics. https://www.ema.europa.eu/en/medicines/human/EPAR/briviact-italy-nubriveo. Accessed 29 Aug 2022.
Briviact (brivaracetam). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/205836s009,205837s007,205838s006lbl.pdf. Accessed 29 Aug 2022.
Bresnahan R, Panebianco M, Marson AG. Brivaracetam add-on therapy for drug-resistant epilepsy. Cochrane Database Syst Rev. 2019;3(3):CD011501. https://doi.org/10.1002/14651858.CD011501.pub2.
Ferragut Ferretjans F, Soto Insuga V, Bernardino Cuesta B, et al. Efficacy of brivaracetam in children with epilepsy. Epilepsy Res. 2021;177: 106757. https://doi.org/10.1016/j.eplepsyres.2021.106757.
McGuire S, Silva G, Lal D, et al. Safety and efficacy of brivaracetam in pediatric refractory epilepsy: a single-center clinical experience. J Child Neurol. 2020;35(2):102–5. https://doi.org/10.1177/0883073819879276.
Nissenkorn A, Tzadok M, Bar-Yosef O, et al. Treatment with brivaracetam in children: the experience of a pediatric epilepsy center. Epilepsy Behav. 2019;101(Pt A): 106541. https://doi.org/10.1016/j.yebeh.2019.106541.
Schubert-Bast S, Willems LM, Kurlemann G, et al. Postmarketing experience with brivaracetam in the treatment of focal epilepsy in children and adolescents. Epilepsy Behav. 2018;89:89–93. https://doi.org/10.1016/j.yebeh.2018.10.018.
Visa-Reñé N, Raspall-Chaure M, Paredes-Carmona F, et al. Clinical experience with brivaracetam in a series of 46 children. Epilepsy Behav. 2020;107: 107067. https://doi.org/10.1016/j.yebeh.2020.107067.
Lattanzi S, Canafoglia L, Canevini MP, et al. Adjunctive brivaracetam in focal epilepsy: real-world evidence from the BRIVAracetam add-on First Italian netwoRk STudy (BRIVAFIRST). CNS Drugs. 2021;35(12):1289–301. https://doi.org/10.1007/s40263-021-00856-3.
Villanueva V, López-González FJ, Mauri JA, et al. BRIVA-LIFE-A multicenter retrospective study of the long-term use of brivaracetam in clinical practice. Acta Neurol Scand. 2019;139(4):360–8. https://doi.org/10.1111/ane.13059.
Strzelczyk A, Zaveta C, von Podewils F, et al. Long-term efficacy, tolerability, and retention of brivaracetam in epilepsy treatment: a longitudinal multicenter study with up to 5 years of follow-up. Epilepsia. 2021;62(12):2994–3004. https://doi.org/10.1111/epi.17087.
Willems LM, Bertsche A, Bösebeck F, et al. Efficacy, retention, and tolerability of brivaracetam in patients with epileptic encephalopathies: a multicenter cohort study from Germany. Front Neurol. 2018;9:569. https://doi.org/10.3389/fneur.2018.00569.
Feyissa AM. Brivaracetam in the treatment of epilepsy: a review of clinical trial data. Neuropsychiatr Dis Treat. 2019;15:2587–600. https://doi.org/10.2147/ndt.S143548.
Hirsch M, Hintz M, Specht A, et al. Tolerability, efficacy and retention rate of Brivaracetam in patients previously treated with levetiracetam: a monocenter retrospective outcome analysis. Seizure. 2018;61:98–103. https://doi.org/10.1016/j.seizure.2018.07.017.
Zhang L, Li S, Li H, et al. Levetiracetam vs. brivaracetam for adults with refractory focal seizures: a meta-analysis and indirect comparison. Seizure. 2016;39:28–33. https://doi.org/10.1016/j.seizure.2016.05.004.
Brandt C, Klein P, Badalamenti V, et al. Safety and tolerability of adjunctive brivaracetam in epilepsy: In-depth pooled analysis. Epilepsy Behav. 2020;103(Pt A): 106864. https://doi.org/10.1016/j.yebeh.2019.106864.
Lattanzi S, Cagnetti C, Foschi N, et al. Brivaracetam add-on for refractory focal epilepsy: a systematic review and meta-analysis. Neurology. 2016;86(14):1344–52. https://doi.org/10.1212/wnl.0000000000002545.
Ma J, Huang S, You C. Adjunctive brivaracetam for patients with refractory partial seizures: a meta-analysis of randomized placebo-controlled trials. Epilepsy Res. 2015;114:59–65. https://doi.org/10.1016/j.eplepsyres.2015.04.017.
Foo EC, Geldard J, Peacey C, et al. Adjunctive brivaracetam in focal and generalized epilepsies: a single-center open-label prospective study in patients with psychiatric comorbidities and intellectual disability. Epilepsy Behav. 2019;99: 106505. https://doi.org/10.1016/j.yebeh.2019.106505.
Andres E, Kerling F, Hamer H, et al. Behavioural changes in patients with intellectual disability treated with brivaracetam. Acta Neurol Scand. 2018;138(3):195–202. https://doi.org/10.1111/ane.12943.
Witt JA, Elger CE, Helmstaedter C. Short-term and longer-term effects of brivaracetam on cognition and behavior in a naturalistic clinical setting: preliminary data. Seizure. 2018;62:49–54. https://doi.org/10.1016/j.seizure.2018.09.016.
Hansen CC, Ljung H, Brodtkorb E, et al. Mechanisms underlying aggressive behavior induced by antiepileptic drugs: focus on topiramate, levetiracetam, and perampanel. Behav Neurol. 2018. https://doi.org/10.1155/2018/2064027.
Zonegran. Summary of product characteristics. https://www.medicines.org.uk/emc/product/72/smpc#gref. Accessed 29 Aug 2022.
Zonegran (zonisamide). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2006/020789s019lbl.pdf. Accessed 29 Aug 2022.
Lee YJ, Kang HC, Seo JH, et al. Efficacy and tolerability of adjunctive therapy with zonisamide in childhood intractable epilepsy. Brain Dev. 2010;32(3):208–12. https://doi.org/10.1016/j.braindev.2009.02.003.
Brigo F, Lattanzi S, Igwe SC, et al. Zonisamide add-on therapy for focal epilepsy. Cochrane Database Syst Rev. 2020;7(7):CD001416. https://doi.org/10.1002/14651858.CD001416.pub5.
Brodie MJ. Zonisamide as adjunctive therapy for refractory partial seizures. Epilepsy Res. 2006;68(Suppl. 2):S11–6. https://doi.org/10.1016/j.eplepsyres.2005.11.005.
You SJ, Kang HC, Kim HD, et al. Clinical efficacy of zonisamide in Lennox-Gastaut syndrome: Korean multicentric experience. Brain Dev. 2008;30(4):287–90. https://doi.org/10.1016/j.braindev.2007.09.004.
Schubert-Bast S, Wolff M, Wiemer-Kruel A, et al. Seizure management and prescription patterns of anticonvulsants in Dravet syndrome: a multicenter cohort study from Germany and review of literature. Epilepsy Behav. 2019;98(Pt A):88–95. https://doi.org/10.1016/j.yebeh.2019.06.021.
Shi XY, Tomonoh Y, Wang WZ, et al. Efficacy of antiepileptic drugs for the treatment of Dravet syndrome with different genotypes. Brain Dev. 2016;38(1):40–6. https://doi.org/10.1016/j.braindev.2015.06.008.
Meschede C, Witt JA, Brömling S, et al. Changes in cognition after introduction or withdrawal of zonisamide versus topiramate in epilepsy patients: a retrospective study using Bayes statistics. Epilepsia. 2020;61(7):1481–90. https://doi.org/10.1111/epi.16576.
Park SP, Hwang YH, Lee HW, et al. Long-term cognitive and mood effects of zonisamide monotherapy in epilepsy patients. Epilepsy Behav. 2008;12(1):102–8. https://doi.org/10.1016/j.yebeh.2007.08.002.
Eck K, Rauch C, Kerling F, et al. Long-term effects of zonisamide in adult patients with intellectual disability. Acta Neurol Scand. 2021;144(3):275–82. https://doi.org/10.1111/ane.13443.
Cavanna AE, Seri S. Psychiatric adverse effects of zonisamide in patients with epilepsy and mental disorder comorbidities. Epilepsy Behav. 2013;29(2):281–4. https://doi.org/10.1016/j.yebeh.2013.08.024.
Leppik IE, Willmore LJ, Homan RW, et al. Efficacy and safety of zonisamide: results of a multicenter study. Epilepsy Res. 1993;14(2):165–73. https://doi.org/10.1016/0920-1211(93)90021-x.
Romigi A, Izzi F, Placidi F, et al. Effects of zonisamide as add-on therapy on sleep-wake cycle in focal epilepsy: a polysomnographic study. Epilepsy Behav. 2013;26(2):170–4. https://doi.org/10.1016/j.yebeh.2012.11.049.
Fycompa (perampanel). https://www.medicines.org.uk/emc/medicine/26951#gref. Accessed 29 Aug 2022.
FYCOMPA (perampanel). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/202834s011lbl.pdf. Accessed 29 Aug 2022.
Alonso-Singer P, Aguilar-Amat Prior MJ, Oliva-Navarro J, et al. Perampanel as adjuvant treatment in epileptic encephalopathies: a multicenter study in routine clinical practice. Epilepsy Behav. 2022;134: 108836. https://doi.org/10.1016/j.yebeh.2022.108836.
Huber B, Schmid G. A two-year retrospective evaluation of perampanel in patients with highly drug-resistant epilepsy and cognitive impairment. Epilepsy Behav. 2017;66:74–9. https://doi.org/10.1016/j.yebeh.2016.10.020.
Chang FM, Fan PC, Weng WC, et al. The efficacy of perampanel in young children with drug-resistant epilepsy. Seizure. 2020;75:82–6. https://doi.org/10.1016/j.seizure.2019.12.024.
Qu R, Dai Y, Qu X, et al. Use of perampanel in children with refractory epilepsy of genetic aetiology. Epileptic Disord. 2022;24(4):687–95. https://doi.org/10.1684/epd.2022.1443.
Heyman E, Lahat E, Levin N, et al. Tolerability and efficacy of perampanel in children with refractory epilepsy. Dev Med Child Neurol. 2017;59(4):441–4. https://doi.org/10.1111/dmcn.13362.
De Liso P, Vigevano F, Specchio N, et al. Effectiveness and tolerability of perampanel in children and adolescents with refractory epilepsies: an Italian observational multicenter study. Epilepsy Res. 2016;127:93–100. https://doi.org/10.1016/j.eplepsyres.2016.08.021.
Lin KL, Lin JJ, Chou ML, et al. Efficacy and tolerability of perampanel in children and adolescents with pharmacoresistant epilepsy: the first real-world evaluation in Asian pediatric neurology clinics. Epilepsy Behav. 2018;85:188–94. https://doi.org/10.1016/j.yebeh.2018.06.033.
Biró A, Stephani U, Tarallo T, et al. Effectiveness and tolerability of perampanel in children and adolescents with refractory epilepsies: first experiences. Neuropediatrics. 2015;46(2):110–6. https://doi.org/10.1055/s-0035-1546276.
Auvin S, Dozieres B, Ilea A, et al. Use of perampanel in children and adolescents with Lennox-Gastaut syndrome. Epilepsy Behav. 2017;74:59–63. https://doi.org/10.1016/j.yebeh.2017.05.036.
Crespel A, Tang NPL, Macorig G, et al. Open-label, uncontrolled retrospective study of perampanel in adults with Lennox-Gastaut syndrome. Seizure. 2020;75:66–9. https://doi.org/10.1016/j.seizure.2019.12.012.
Yoshitomi S, Takahashi Y, Yamaguchi T, et al. Efficacy and tolerability of perampanel in pediatric patients with Dravet syndrome. Epilepsy Res. 2019;154:34–8. https://doi.org/10.1016/j.eplepsyres.2019.02.014.
Villanueva V, D’Souza W, Goji H, et al. PERMIT study: a global pooled analysis study of the effectiveness and tolerability of perampanel in routine clinical practice. J Neurol. 2021. https://doi.org/10.1007/s00415-021-10751-y.
Lee SA, Jeon JY, Kim HW. Effect of perampanel on aggression in patients with refractory focal epilepsy: a 6-month longitudinal study. Epilepsy Behav. 2020;102: 106658. https://doi.org/10.1016/j.yebeh.2019.106658.
Andres E, Kerling F, Hamer H, et al. Behavioural changes in patients with intellectual disability treated with perampanel. Acta Neurol Scand. 2017;136(6):645–53. https://doi.org/10.1111/ane.12781.
Dozières-Puyravel B, Auvin S. An evidence-based review on the use of perampanel for the treatment of focal-onset seizures in pediatric patients. Neuropsychiatr Dis Treat. 2019;15:2789–98. https://doi.org/10.2147/ndt.S178405.
Ettinger AB, LoPresti A, Yang H, et al. Psychiatric and behavioral adverse events in randomized clinical studies of the noncompetitive AMPA receptor antagonist perampanel. Epilepsia. 2015;56(8):1252–63. https://doi.org/10.1111/epi.13054.
Juhl S, Rubboli G. Add-on perampanel and aggressive behaviour in severe drug-resistant focal epilepsies. Funct Neurol. 2017;32(4):215–20.
Goji H, Kanemoto K. The effect of perampanel on aggression and depression in patients with epilepsy: a short-term prospective study. Seizure. 2019;67:1–4. https://doi.org/10.1016/j.seizure.2019.02.009.
Hasegawa N, Tohyama J. Positive and negative effects of perampanel treatment on psychiatric and behavioral symptoms in adult patients with epilepsy. Epilepsy Behav. 2021;117: 107515. https://doi.org/10.1016/j.yebeh.2020.107515.
Operto FF, Pastorino GMG, Mazza R, et al. Perampanel tolerability in children and adolescents with focal epilepsy: Effects on behavior and executive functions. Epilepsy Behav. 2020;103(Pt A): 106879. https://doi.org/10.1016/j.yebeh.2019.106879.
Lee SA, Jung M, Kim SJ, et al. Insomnia is less prevalent and less severe, independent of depressive symptoms, in patients with epilepsy treated with perampanel as an adjuvant. Epilepsy Behav. 2020;112: 107384. https://doi.org/10.1016/j.yebeh.2020.107384.
Ethosuximide (essential generics 250 mg capsules). Summary of product characteristics. https://www.medicines.org.uk/emc/product/12896/smpc#gref. Accessed 29 Aug 2022.
ZARONTIN- ethosuximide capsule. Prescribing information https://labeling.pfizer.com/ShowLabeling.aspx?id=610. Accessed 29 Aug 2022.
Glauser TA, Cnaan A, Shinnar S, et al. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy: initial monotherapy outcomes at 12 months. Epilepsia. 2013;54(1):141–55. https://doi.org/10.1111/epi.12028.
Glauser TA, Cnaan A, Shinnar S, et al. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy. N Engl J Med. 2010;362(9):790–9. https://doi.org/10.1056/NEJMoa0902014.
Kessler SK, McGinnis E. A practical guide to treatment of childhood absence epilepsy. Pediatr Drugs. 2019;21(1):15–24. https://doi.org/10.1007/s40272-019-00325-x.
Aldenkamp A, Besag F, Gobbi G, et al. Psychiatric and behavioural disorders in children with epilepsy (ILAE Task Force report): adverse cognitive and behavioural effects of antiepileptic drugs in children. Epileptic Disord. 2016. https://doi.org/10.1684/epd.2016.0817.
Dominique MIJ, van Veenendaal TM, Debeij-van Hall MH, et al. The cognitive profile of ethosuximide in children. Pediatr Drugs. 2016;18(5):379–85. https://doi.org/10.1007/s40272-016-0187-z.
Diacomit. Summary of product characteristics. https://www.medicines.org.uk/emc/product/10300/smpc. Accessed 22 Apr 2022.
Diacomit. Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/206709s000,207223s000lbl.pdf. Accessed 21 Mar 2022.
Chiron C, Tonnelier S, Rey E, et al. Stiripentol in childhood partial epilepsy: randomized placebo-controlled trial with enrichment and withdrawal design. J Child Neurol. 2006;21(6):496–502. https://doi.org/10.1177/08830738060210062101.
Aras LM, Isla J, Mingorance-Le MA. The European patient with Dravet syndrome: results from a parent-reported survey on antiepileptic drug use in the European population with Dravet syndrome. Epilepsy Behav. 2015;44:104–9. https://doi.org/10.1016/j.yebeh.2014.12.028.
Myers KA, Lightfoot P, Patil SG, et al. Stiripentol efficacy and safety in Dravet syndrome: a 12-year observational study. Dev Med Child Neurol. 2018;60(6):574–8. https://doi.org/10.1111/dmcn.13704.
Inoue Y, Ohtsuka Y. Long-term safety and efficacy of stiripentol for the treatment of Dravet syndrome: a multicenter, open-label study in Japan. Epilepsy Res. 2015;113:90–7. https://doi.org/10.1016/j.eplepsyres.2015.03.012.
Chiron C, Helias M, Kaminska A, et al. Do children with Dravet syndrome continue to benefit from stiripentol for long through adulthood? Epilepsia. 2018;59(9):1705–17. https://doi.org/10.1111/epi.14536.
Lamotrigine. Summary of product characteristics. https://www.medicines.org.uk/emc/product/6092/smpc#gref. Accessed 29 Aug 2022.
Lamictal (lamotrigine). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/020241s045s051lbl.pdf. Accessed 29 Aug 2022.
Motte J, Trevathan E, Arvidsson JF, et al. Lamotrigine for generalized seizures associated with the Lennox-Gastaut syndrome. Lamictal Lennox-Gastaut Study Group. N Engl J Med. 1997;337(25):1807–12. https://doi.org/10.1056/nejm199712183372504.
Panebianco M, Bresnahan R, Ramaratnam S, et al. Lamotrigine add-on therapy for drug-resistant focal epilepsy. Cochrane Database Syst Rev. 2020;3(3):CD001909. https://doi.org/10.1002/14651858.CD001909.pub3.
Meador KJ, Baker GA. Behavioral and cognitive effects of lamotrigine. J Child Neurol. 1997;12(Suppl. 1):S44–7. https://doi.org/10.1177/0883073897012001101.
Moavero R, Pisani LR, Pisani F, et al. Safety and tolerability profile of new antiepileptic drug treatment in children with epilepsy. Expert Opin Drug Saf. 2018;17(10):1015–28. https://doi.org/10.1080/14740338.2018.1518427.
Bresnahan R, Panebianco M, Marson AG. Lamotrigine add-on therapy for drug-resistant generalised tonic-clonic seizures. Cochrane Database Syst Rev. 2020;7(7):CD007783. https://doi.org/10.1002/14651858.CD007783.pub3.
Aldenkamp AP, Baker G. A systematic review of the effects of lamotrigine on cognitive function and quality of life. Epilepsy Behav. 2001;2(2):85–91. https://doi.org/10.1006/ebeh.2001.0168.
Blum D, Meador K, Biton V, et al. Cognitive effects of lamotrigine compared with topiramate in patients with epilepsy. Neurology. 2006;67(3):400–6. https://doi.org/10.1212/01.wnl.0000232737.72555.06.
Bootsma HP, Vos AM, Hulsman J, et al. Lamotrigine in clinical practice: long-term experience in patients with refractory epilepsy referred to a tertiary epilepsy center. Epilepsy Behav. 2008;12(2):262–8. https://doi.org/10.1016/j.yebeh.2007.10.004.
Crawford P, Brown S, Kerr M. A randomized open-label study of gabapentin and lamotrigine in adults with learning disability and resistant epilepsy. Seizure. 2001;10(2):107–15. https://doi.org/10.1053/seiz.2000.0474.
Eun SH, Eun BL, Lee JS, et al. Effects of lamotrigine on cognition and behavior compared to carbamazepine as monotherapy for children with partial epilepsy. Brain Dev. 2012;34(10):818–23. https://doi.org/10.1016/j.braindev.2012.03.006.
Helmstaedter C, Witt JA. The longer-term cognitive effects of adjunctive antiepileptic treatment with lacosamide in comparison with lamotrigine and topiramate in a naturalistic outpatient setting. Epilepsy Behav. 2013;26(2):182–7. https://doi.org/10.1016/j.yebeh.2012.11.052.
Lee SA, Kim MJ, Lee HW, et al. The effect of recurrent seizures on cognitive, behavioral, and quality-of-life outcomes after 12 months of monotherapy in adults with newly diagnosed or previously untreated partial epilepsy. Epilepsy Behav. 2015;53:202–8. https://doi.org/10.1016/j.yebeh.2015.10.020.
Lee SA, Lee HW, Heo K, et al. Cognitive and behavioral effects of lamotrigine and carbamazepine monotherapy in patients with newly diagnosed or untreated partial epilepsy. Seizure. 2011;20(1):49–54. https://doi.org/10.1016/j.seizure.2010.10.006.
Martinović Z, Buder N, Milovanović M, et al. Antiepileptic, behavioral, and antidepressant effects of adjuvant lamotrigine therapy in drug-resistant epilepsy. Vojnosanit Pregl. 2004;61(5):485–90. https://doi.org/10.2298/vsp0405485m.
McKee JR, Sunder TR, FineSmith R, et al. Lamotrigine as adjunctive therapy in patients with refractory epilepsy and mental retardation. Epilepsy Behav. 2003;4(4):386–94. https://doi.org/10.1016/s1525-5050(03)00117-3.
McKee JR, Sunder TR, Vuong A, et al. Adjunctive lamotrigine for refractory epilepsy in adolescents with mental retardation. J Child Neurol. 2006;21(5):372–9. https://doi.org/10.1177/08830738060210051401.
Pressler RM, Binnie CD, Coleshill SG, et al. Effect of lamotrigine on cognition in children with epilepsy. Neurology. 2006;66(10):1495–9. https://doi.org/10.1212/01.wnl.0000216273.94142.84.
Seo JG, Lee DI, Hwang YH, et al. Comparison of cognitive effects of lamotrigine and oxcarbazepine in epilepsy patients. J Clin Neurol. 2007;3(1):31–7. https://doi.org/10.3988/jcn.2007.3.1.31.
Cramer JA, Hammer AE, Kustra RP. Improved mood states with lamotrigine in patients with epilepsy. Epilepsy Behav. 2004;5(5):702–7. https://doi.org/10.1016/j.yebeh.2004.07.005.
Uvebrant P, Bauzienè R. Intractable epilepsy in children: the efficacy of lamotrigine treatment, including non-seizure-related benefits. Neuropediatrics. 1994;25(6):284–9. https://doi.org/10.1055/s-2008-1073041.
Ettinger AB, Weisbrot DM, Saracco J, et al. Positive and negative psychotropic effects of lamotrigine in patients with epilepsy and mental retardation. Epilepsia. 1998;39(8):874–7. https://doi.org/10.1111/j.1528-1157.1998.tb01183.x.
Donaldson JA, Glauser TA, Olberding LS. Lamotrigine adjunctive therapy in childhood epileptic encephalopathy (the Lennox Gastaut syndrome). Epilepsia. 1997;38(1):68–73. https://doi.org/10.1111/j.1528-1157.1997.tb01079.x.
Sadler M. Lamotrigine associated with insomnia. Epilepsia. 1999;40(3):322–5. https://doi.org/10.1111/j.1528-1157.1999.tb00712.x.
Placidi F, Marciani MG, Diomedi M, et al. Effects of lamotrigine on nocturnal sleep, daytime somnolence and cognitive functions in focal epilepsy. Acta Neurol Scand. 2000;102(2):81–6. https://doi.org/10.1034/j.1600-0404.2000.102002081.x.
Foldvary N, Perry M, Lee J, et al. The effects of lamotrigine on sleep in patients with epilepsy. Epilepsia. 2001;42(12):1569–73. https://doi.org/10.1046/j.1528-1157.2001.46100.x.
Inovelon (rufinamide). Summary of product characteristcs. https://www.ema.europa.eu/en/documents/product-information/inovelon-epar-product-information_en.pdf. Accessed 29 Aug 2022.
Banzel (rufinamide). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/021911s012lbl.pdf. Accessed 29 Aug 2022.
Arzimanoglou A, Ferreira J, Satlin A, et al. Evaluation of long-term safety, tolerability, and behavioral outcomes with adjunctive rufinamide in pediatric patients (≥ 1 to <4 years old) with Lennox-Gastaut syndrome: final results from randomized study 303. Eur J Paediatr Neurol. 2019;23(1):126–35. https://doi.org/10.1016/j.ejpn.2018.09.010.
Arzimanoglou A, Ferreira JA, Satlin A, et al. Safety and pharmacokinetic profile of rufinamide in pediatric patients aged less than 4 years with Lennox-Gastaut syndrome: An interim analysis from a multicenter, randomized, active-controlled, open-label study. Eur J Paediatr Neurol. 2016;20(3):393–402. https://doi.org/10.1016/j.ejpn.2015.12.015.
Glauser T, Kluger G, Sachdeo R, et al. Rufinamide for generalized seizures associated with Lennox-Gastaut syndrome. Neurology. 2008;70(21):1950–8. https://doi.org/10.1212/01.wnl.0000303813.95800.0d.
Panebianco M, Prabhakar H, Marson AG. Rufinamide add-on therapy for drug-resistant epilepsy. Cochrane Database Syst Rev. 2020;11(11):CD011772. https://doi.org/10.1002/14651858.CD011772.pub3.
Nikanorova M, Brandt C, Auvin S, et al. Real-world data on rufinamide treatment in patients with Lennox-Gastaut syndrome: results from a European noninterventional registry study. Epilepsy Behav. 2017;76:63–70. https://doi.org/10.1016/j.yebeh.2017.08.026.
Arzimanoglou A, Pringsheim M, Kluger GJ, et al. Safety and efficacy of rufinamide in children and adults with Lennox-Gastaut syndrome: a post hoc analysis from Study 022. Epilepsy Behav. 2021;124: 108275. https://doi.org/10.1016/j.yebeh.2021.108275.
Caraballo RH, Pociecha J, Reyes G, et al. Rufinamide as add-on therapy in children with epileptic encephalopathies other than Lennox-Gastaut syndrome: a study of 34 patients. Epilepsy Behav. 2020;108: 107074. https://doi.org/10.1016/j.yebeh.2020.107074.
Operto FF, Verrotti A, Marrelli A, et al. Cognitive, adaptive, and behavioral effects of adjunctive rufinamide in Lennox-Gastaut syndrome: a prospective observational clinical study. Epilepsy Behav. 2020;112: 107445. https://doi.org/10.1016/j.yebeh.2020.107445.
Thome-Souza S, Kadish NE, Ramgopal S, et al. Safety and retention rate of rufinamide in 300 patients: a single pediatric epilepsy center experience. Epilepsia. 2014;55(8):1235–44. https://doi.org/10.1111/epi.12689.
Sabril (vigabatrin). Summary of product characteristics. https://www.medicines.org.uk/emc/product/4279/smpc#gref. Accessed 29 Aug 2022.
Sabril (vigabatrin). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/020427s010s011s012,022006s011s012s013lbl.pdf. Accessed 29 Aug 2022.
Camposano SE, Major P, Halpern E, et al. Vigabatrin in the treatment of childhood epilepsy: a retrospective chart review of efficacy and safety profile. Epilepsia. 2008;49(7):1186–91. https://doi.org/10.1111/j.1528-1167.2008.01589.x.
Pellock JM, Faught E, Foroozan R, et al. Which children receive vigabatrin? Characteristics of pediatric patients enrolled in the mandatory FDA registry. Epilepsy Behav. 2016;60:174–80. https://doi.org/10.1016/j.yebeh.2016.03.030.
Friedman D, Bogner M, Parker-Menzer K, et al. Vigabatrin for partial-onset seizure treatment in patients with tuberous sclerosis complex. Epilepsy Behav. 2013;27(1):118–20. https://doi.org/10.1016/j.yebeh.2012.12.033.
van der Poest Clement EA, Sahin M, Peters JM. Vigabatrin for epileptic spasms and tonic seizures in tuberous sclerosis complex. J Child Neurol. 2018;33(8):519–24. https://doi.org/10.1177/0883073818768309.
Bresnahan R, Gianatsi M, Maguire MJ, et al. Vigabatrin add-on therapy for drug-resistant focal epilepsy. Cochrane Database Syst Rev. 2020;7(7):CD007302. https://doi.org/10.1002/14651858.CD007302.pub3.
Levinson DF, Devinsky O. Psychiatric adverse events during vigabatrin therapy. Neurology. 1999;53(7):1503–11. https://doi.org/10.1212/wnl.53.7.1503.
Aldenkamp AP, Vermeulen J, Mulder OG, et al. Gamma-vinyl GABA (vigabatrin) and mood disturbances. Epilepsia. 1994;35(5):999–1004. https://doi.org/10.1111/j.1528-1157.1994.tb02545.x.
Dam M, Betts T, Thomas L, et al. Vigabatrin and behaviour disturbances. Lancet. 1990;335(8689):605–6. https://doi.org/10.1016/0140-6736(90)90388-L.
Sander JW, Trevisol-Bittencourt PC, Hart YM, et al. Evaluation of vigabatrin as an add-on drug in the management of severe epilepsy. J Neurol Neurosurg Psychiatry. 1990;53(11):1008–10. https://doi.org/10.1136/jnnp.53.11.1008.
Wong IC. Retrospective study of vigabatrin and psychiatric behavioural disturbances. Epilepsy Res. 1995;21(3):227–30. https://doi.org/10.1016/0920-1211(95)00022-3.
Ring HA, Crellin R, Kirker S, et al. Vigabatrin and depression. J Neurol Neurosurg Psychiatry. 1993;56(8):925–8. https://doi.org/10.1136/jnnp.56.8.925.
Dean C, Mosier M, Penry K. Dose-Response Study of Vigabatrin as add-on therapy in patients with uncontrolled complex partial seizures. Epilepsia. 1999;40(1):74–82. https://doi.org/10.1111/j.1528-1157.1999.tb01991.x.
Dodrill CB, Arnett JL, Sommerville KW, et al. Evaluation of the effects of vigabatrin on cognitive abilities and quality of life in epilepsy. Neurology. 1993;43(12):2501–7. https://doi.org/10.1212/wnl.43.12.2501.
Dodrill CB, Arnett JL, Sommerville KW, et al. Effects of differing dosages of vigabatrin (Sabril) on cognitive abilities and quality of life in epilepsy. Epilepsia. 1995;36(2):164–73. https://doi.org/10.1111/j.1528-1157.1995.tb00976.x.
French JA, Mosier M, Walker S, et al. A double-blind, placebo-controlled study of vigabatrin three g/day in patients with uncontrolled complex partial seizures. Vigabatrin Protocol 024 Investigative Cohort. Neurology. 1996;46(1):54–61. https://doi.org/10.1212/wnl.46.1.54.
Gillham RA, Blacklaw J, McKee PJ, et al. Effect of vigabatrin on sedation and cognitive function in patients with refractory epilepsy. J Neurol Neurosurg Psychiatry. 1993;56(12):1271–5. https://doi.org/10.1136/jnnp.56.12.1271.
McKee PJ, Blacklaw J, Friel E, et al. Adjuvant vigabatrin in refractory epilepsy: a ceiling to effective dosage in individual patients? Epilepsia. 1993;34(5):937–43. https://doi.org/10.1111/j.1528-1157.1993.tb02115.x.
Jambaqué I, Chiron C, Dumas C, et al. Mental and behavioural outcome of infantile epilepsy treated by vigabatrin in tuberous sclerosis patients. Epilepsy Res. 2000;38(2–3):151. https://doi.org/10.1016/s0920-1211(99)00082-0.
Bombardieri R, Pinci M, Moavero R, et al. Early control of seizures improves long-term outcome in children with tuberous sclerosis complex. Eur J Paediatr Neurol. 2010;14(2):146–9. https://doi.org/10.1016/j.ejpn.2009.03.003.
Kotulska K, Kwiatkowski DJ, Curatolo P, et al. Prevention of epilepsy in infants with tuberous sclerosis complex in the EPISTOP trial. Ann Neurol. 2021;89(2):304–14. https://doi.org/10.1002/ana.25956.
Votubia®. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/votubia-epar-product-information_en.pdf. Accessed 29 Aug 2022.
Afinitor® /Afinitor Disperz® . Highlights of prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/022334s040,203985s013lbl.pdf. Accessed 29 Aug 2022.
French JA, Lawson JA, Yapici Z, et al. Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study. Lancet. 2016;388(10056):2153–63. https://doi.org/10.1016/S0140-6736(16)31419-2.
Willems LM, Rosenow F, Schubert-Bast S, et al. Efficacy, retention and tolerability of everolimus in patients with tuberous sclerosis complex: a survey-based study on patients’ perspectives. CNS Drugs. 2021;35(10):1107–22. https://doi.org/10.1007/s40263-021-00839-4.
Krueger DA, Sadhwani A, Byars AW, et al. Everolimus for treatment of tuberous sclerosis complex-associated neuropsychiatric disorders. Ann Clin Transl Neurol. 2017;4(12):877–87. https://doi.org/10.1002/acn3.494.
Overwater IE, Rietman AB, Mous SE, et al. A randomized controlled trial with everolimus for IQ and autism in tuberous sclerosis complex. Neurology. 2019;93(2):e200–9. https://doi.org/10.1212/wnl.0000000000007749.
Kilincaslan A, Kok BE, Tekturk P, et al. Beneficial effects of everolimus on autism and attention-deficit/hyperactivity disorder symptoms in a group of patients with tuberous sclerosis complex. J Child Adolesc Psychopharmacol. 2017;27(4):383–8. https://doi.org/10.1089/cap.2016.0100.
Kadish NE, Riedel C, Stephani U, et al. Developmental outcomes in children/adolescents and one adult with tuberous sclerosis complex (TSC) and refractory epilepsy treated with everolimus. Epilepsy Behav. 2020;111: 107182. https://doi.org/10.1016/j.yebeh.2020.107182.
Saffari A, Brösse I, Wiemer-Kruel A, et al. Safety and efficacy of mTOR inhibitor treatment in patients with tuberous sclerosis complex under 2 years of age: a multicenter retrospective study. Orphan J Rare Dis. 2019;14(1):96. https://doi.org/10.1186/s13023-019-1077-6.
Samueli S, Dressler A, Gröppel G, et al. Everolimus in infants with tuberous sclerosis complex-related West syndrome: first results from a single-center prospective observational study. Epilepsia. 2018;59(9):e142–6. https://doi.org/10.1111/epi.14529.
Vimpat (lacosamide). Summary of product characteristics. https://www.medicines.org.uk/emc/product/2278/smpc#gref. Accessed 29 Aug 2022.
VIMPAT (lacosamide). Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/022253s049,022254s039,022255s031lbl.pdf. Accessed 29 Aug 2022.
Geffrey AL, Belt OD, Paolini JL, et al. Lacosamide use in the treatment of refractory epilepsy in tuberous sclerosis complex. Epilepsy Res. 2015;112:72–5. https://doi.org/10.1016/j.eplepsyres.2015.02.008.
Babar RK, Bresnahan R, Gillespie CS, et al. Lacosamide add-on therapy for focal epilepsy. Cochrane Database Syst Rev. 2021;5(5):CD008841. https://doi.org/10.1002/14651858.CD008841.pub3.
Beydoun A, D’Souza J, Hebert D, et al. Lacosamide: pharmacology, mechanisms of action and pooled efficacy and safety data in partial-onset seizures. Expert Rev Neurother. 2009;9(1):33–42. https://doi.org/10.1586/14737175.9.1.33.
Biton V, Gil-Nagel A, Isojarvi J, et al. Safety and tolerability of lacosamide as adjunctive therapy for adults with partial-onset seizures: Analysis of data pooled from three randomized, double-blind, placebo-controlled clinical trials. Epilepsy Behav. 2015;52(Pt A):119–27. https://doi.org/10.1016/j.yebeh.2015.09.006.
Li KY, Huang LC, Chang YP, et al. The effects of lacosamide on cognitive function and psychiatric profiles in patients with epilepsy. Epilepsy Behav. 2020;113: 107580. https://doi.org/10.1016/j.yebeh.2020.107580.
Toniolo S, Di Lorenzo F, Bozzali M, et al. The impact of lacosamide on mood disorders in adult patients with epilepsy: a systematic review. Epilepsy Behav. 2020;111: 107179. https://doi.org/10.1016/j.yebeh.2020.107179.
Ortiz de la Rosa JS, Ladino LD, Rodríguez PJ, et al. Efficacy of lacosamide in children and adolescents with drug-resistant epilepsy and refractory status epilepticus: a systematic review. Seizure. 2018;56:34–40. https://doi.org/10.1016/j.seizure.2018.01.014.
Panda PK, Sharawat IK, Dawman L, et al. Efficacy and tolerability of lacosamide in Lennox-Gastaut syndrome: a systematic review and meta-analysis. J Neurosci Rural Pract. 2022;13(1):32–42. https://doi.org/10.1055/s-0041-1740580.
Allard J, Henley W, McLean B, et al. Lacosamide in the general population and in people with intellectual disability: similar responses? Seizure. 2020;76:161–6. https://doi.org/10.1016/j.seizure.2020.02.013.
Brenner J, Majoie HJM, van Beek S, et al. The retention of lacosamide in patients with epilepsy and intellectual disability in three specialised institutions. Seizure. 2017;52:123–30. https://doi.org/10.1016/j.seizure.2017.09.017.
Great Ormond Street Hospital (GOSH). Bromide for epilepsy 2020. https://www.gosh.nhs.uk/conditions-and-treatments/medicines-information/bromide-epilepsy/. Accessed 29 Aug 2022.
Bast T, Steinhoff BJ. Anticonvulsant agents: potassium bromide. In: Riederer P, Laux G, Mulsant B, Le W, Nagatsu T, editors. NeuroPsychopharmacotherapy. Cham: Springer International Publishing; 2020. p. 1–7. https://doi.org/10.1007/978-3-319-56015-1_304-1.
Ernst JP, Doose H, Baier WK. Bromides were effective in intractable epilepsy with generalized tonic-clonic seizures and onset in early childhood. Brain Dev. 1988;10(6):385–8. https://doi.org/10.1016/s0387-7604(88)80098-6.
Kodama K, Omata T, Watanabe Y, et al. Potassium bromide in the treatment of pediatric refractory epilepsy. J Child Neurol. 2019;34(10):582–5. https://doi.org/10.1177/0883073819847862.
Lotte J, Haberlandt E, Neubauer B, et al. Bromide in patients with SCN1A-mutations manifesting as Dravet syndrome. Neuropediatrics. 2012;43(1):17–21. https://doi.org/10.1055/s-0032-1307454.
Oguni H, Hayashi K, Oguni M, et al. Treatment of severe myoclonic epilepsy in infants with bromide and its borderline variant. Epilepsia. 1994;35(6):1140–5. https://doi.org/10.1111/j.1528-1157.1994.tb01780.x.
Steinhoff BJ, Kruse R. Bromide treatment of pharmaco-resistant epilepsies with generalized tonic-clonic seizures: a clinical study. Brain Dev. 1992;14(3):144–9. https://doi.org/10.1016/s0387-7604(12)80253-1.
Meador KJ. Cognitive side effects of antiepileptic drugs. Can J Neurol Sci. 1994;21(3):S12–6. https://doi.org/10.1017/s0317167100040762.
Felbatol (felbamate). Prescribing Information. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020189s022lbl.pdf. Accessed 29 Aug 2022.
Efficacy of felbamate in childhood epileptic encephalopathy (Lennox-Gastaut syndrome). N Engl J Med. 1993;328(1):29–33. doi: https://doi.org/10.1056/nejm199301073280105.
Gay PE, Mecham GF, Coskey JS, et al. Behavioral effects of felbamate in childhood epileptic encephalopathy (Lennox-Gastaut syndrome). Psychol Rep. 1995;77(3 Pt 2):1208. https://doi.org/10.2466/pr0.1995.77.3f.1208.
Ketter TA, Malow BA, Flamini R, et al. Felbamate monotherapy has stimulant-like effects in patients with epilepsy. Epilepsy Res. 1996;23(2):129–37. https://doi.org/10.1016/0920-1211(95)00089-5.
Strzelczyk A, Mann C, Willems LM, et al. Cenobamate for the treatment of focal epilepsies. Expert Opin Pharmacother. 2020;21(18):2215–23. https://doi.org/10.1080/14656566.2020.1803830.
Roth T, Arnold LM, Garcia-Borreguero D, et al. A review of the effects of pregabalin on sleep disturbance across multiple clinical conditions. Sleep Med Rev. 2014;18(3):261–71. https://doi.org/10.1016/j.smrv.2013.07.005.
Helmstaedter C, Witt JA, Hoppe C. Evaluating the mediating role of executive functions for antiepileptic drugs’ effects on IQ in children and adolescents with epilepsy. Epilepsy Behav. 2019;96:98–103. https://doi.org/10.1016/j.yebeh.2019.04.003.
Wolking S, Campbell C, Stapleton C, et al. Role of common genetic variants for drug-resistance to specific anti-seizure medications. Front Pharmacol. 2021;12: 688386. https://doi.org/10.3389/fphar.2021.688386.
Yang TW, Moon J, Kim TJ, et al. HLA-A*11:01 is associated with levetiracetam-induced psychiatric adverse events. PLoS ONE. 2018;13(7): e0200812. https://doi.org/10.1371/journal.pone.0200812.
Chen B, Choi H, Hirsch LJ, et al. Cross-sensitivity of psychiatric and behavioral side effects with antiepileptic drug use. Seizure. 2018;62:38–42. https://doi.org/10.1016/j.seizure.2018.09.014.
Alsfouk BAA, Brodie MJ, Walters M, et al. Tolerability of antiseizure medications in individuals with newly diagnosed epilepsy. JAMA Neurol. 2020;77(5):574–81. https://doi.org/10.1001/jamaneurol.2020.0032.
Ortinski P, Meador KJ. Cognitive side effects of antiepileptic drugs. Epilepsy Behav. 2004;5(Suppl. 1):S60–5. https://doi.org/10.1016/j.yebeh.2003.11.008.
Giménez DeGeorge E, Fullen C, Gess J, et al. Effects of age of onset and medication on cognitive performance and quality of life in patients with epilepsy. Epilepsy Behav. 2021;121(Pt A): 108008. https://doi.org/10.1016/j.yebeh.2021.108008.
Höller Y, Höhn C, Schwimmbeck F, et al. Effects of antiepileptic drug tapering on episodic memory as measured by virtual reality tests. Front Neurol. 2020;11:93. https://doi.org/10.3389/fneur.2020.00093.
De Ridder J, Lavanga M, Verhelle B, et al. Prediction of neurodevelopment in infants with tuberous sclerosis complex using early EEG characteristics. Front Neurol. 2020;11: 582891. https://doi.org/10.3389/fneur.2020.582891.
Capal JK, Bernardino-Cuesta B, Horn PS, et al. Influence of seizures on early development in tuberous sclerosis complex. Epilepsy Behav. 2017;70(Pt A):245–52. https://doi.org/10.1016/j.yebeh.2017.02.007.
Brunklaus A, Ellis R, Reavey E, et al. Prognostic, clinical and demographic features in SCN1A mutation-positive Dravet syndrome. Brain. 2012;135(Pt 8):2329–36. https://doi.org/10.1093/brain/aws151.
Nabbout R, Chemaly N, Chipaux M, et al. Encephalopathy in children with Dravet syndrome is not a pure consequence of epilepsy. Orphan J Rare Dis. 2013;8(1):176. https://doi.org/10.1186/1750-1172-8-176.
Jansen FE, Vincken KL, Algra A, et al. Cognitive impairment in tuberous sclerosis complex is a multifactorial condition. Neurology. 2008;70(12):916–23. https://doi.org/10.1212/01.wnl.0000280579.04974.c0.
Winterkorn EB, Pulsifer MB, Thiele EA. Cognitive prognosis of patients with tuberous sclerosis complex. Neurology. 2007;68(1):62–4. https://doi.org/10.1212/01.wnl.0000250330.44291.54.
Balagura G, Xian J, Riva A, et al. Epilepsy course and developmental trajectories in DEE. Neurol Genet. 2022;8(3): e676. https://doi.org/10.1212/NXG.0000000000000676.
Sałaciak K, Pytka K. Revisiting the sigma-1 receptor as a biological target to treat affective and cognitive disorders. Neurosci Biobehav Rev. 2022;132:1114–36. https://doi.org/10.1016/j.neubiorev.2021.10.037.
Yan Y, Wu JH, Peng XY, et al. Effects of antiseizure medications on alternative psychosis and strategies for their application. World J Psychiatry. 2022;12(4):580–7. https://doi.org/10.5498/wjp.v12.i4.580.
Calle-López Y, Ladino LD, Benjumea-Cuartas V, et al. Forced normalization: a systematic review. Epilepsia. 2019;60(8):1610–8. https://doi.org/10.1111/epi.16276.
Kerr M, Kluger G, Philip S. Evolution and management of Lennox-Gastaut syndrome through adolescence and into adulthood: are seizures always the primary issue? Epileptic Disord. 2011;13(Suppl. 1):S15-26. https://doi.org/10.1684/epd.2011.0409.
Samanta D. Management of Lennox-Gastaut syndrome beyond childhood: a comprehensive review. Epilepsy Behav. 2021;114(Pt A): 107612. https://doi.org/10.1016/j.yebeh.2020.107612.
Stamberger H, Crosiers D, Balagura G, et al. Natural history study of STXBP1-developmental and epileptic encephalopathy into adulthood. Neurology. 2022;99(3):e221–33. https://doi.org/10.1212/wnl.0000000000200715.
Selvarajah A, Zulfiqar-Ali Q, Marques P, et al. A systematic review of adults with Dravet syndrome. Seizure. 2021;87:39–45. https://doi.org/10.1016/j.seizure.2021.02.025.
Zöllner JP, Conradi N, Sauter M, et al. Quality of life and its predictors in adults with tuberous sclerosis complex (TSC): a multicentre cohort study from Germany. Neurol Res Pract. 2021;3:35. https://doi.org/10.1186/s42466-021-00130-3.
Sullivan J, Deighton AM, Vila MC, et al. The clinical, economic, and humanistic burden of Dravet syndrome: a systematic literature review. Epilepsy Behav. 2022;130:108661. https://doi.org/10.1016/j.yebeh.2022.108661.
Strzelczyk A, Kalski M, Bast T, et al. Burden-of-illness and cost-driving factors in Dravet syndrome patients and carers: a prospective, multicenter study from Germany. Eur J Paediatr Neurol. 2019;23(3):392–403. https://doi.org/10.1016/j.ejpn.2019.02.014.
Lagae L, Irwin J, Gibson E, et al. Caregiver impact and health service use in high and low severity Dravet syndrome: a multinational cohort study. Seizure. 2019;65:72–9. https://doi.org/10.1016/j.seizure.2018.12.018.
Strzelczyk A, Kurlemann G, Bast T, et al. Exploring the relationships between composite scores of disease severity seizure-freedom and quality of life in Dravet syndrome. Neurol Res Pract. 2022;4:22. https://doi.org/10.1186/s42466-022-00186-9.
Hahn CD, Jiang Y, Villanueva V, et al. A phase 2, randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of soticlestat as adjunctive therapy in pediatric patients with Dravet syndrome or Lennox-Gastaut syndrome (ELEKTRA). Epilepsia. 2022. https://doi.org/10.1111/epi.17367.
Acknowledgements
Medical writing assistance to identify and synthesise the data and to draft the first draft, under the direction of the authors, was provided by Amanda Prowse (Lochside Medical Communications Ltd). Graphics support was provided by Emma Melchor (Emma Melchor Illustration).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by Projekt DEAL. Medical writing assistance was funded by Zogenix GmbH (now a part of UCB).
Conflicts of interest/Competing interests
Adam Strzelczyk reports personal fees and grants from Angelini Pharma, Desitin Arzneimittel, Eisai, GW Pharmaceuticals companies, Marinus Pharmaceuticals, Precisis, UCB Pharma, UNEEG Medical and Zogenix. Susanne Schubert-Bast reports personal fees from Eisai, Desitin Pharma, GW Pharmaceuticals companies, LivaNova, UCB Pharma and Zogenix.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
Both authors reviewed the literature, drafted the manuscript, generated the figures and assume full responsibility for the final publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Strzelczyk, A., Schubert-Bast, S. Psychobehavioural and Cognitive Adverse Events of Anti-Seizure Medications for the Treatment of Developmental and Epileptic Encephalopathies. CNS Drugs 36, 1079–1111 (2022). https://doi.org/10.1007/s40263-022-00955-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00955-9