Abstract
Background and Objective
Vitamin D insufficiency is common in several pediatric diseases including obesity and asthma. Little data exist describing the pharmacokinetics of oral vitamin D in children or the optimal dosing to achieve therapeutic 25(OH)D targets. Describe the pharmacokinetics of oral Vitamin D in children with asthma.
Methods
This was a multi-center, randomized, open-label, oral supplementation study to describe the pharmacokinetics of vitamin D in children aged 6–17 years who have asthma and were overweight/obese. Participants had a serum 25(OH)D concentration between 10 and < 30 ng/mL at baseline. In Part 1 of the study, we assessed four 16-week dosing regimens for their ability to achieve 25(OH)D concentrations ≥ 40 ng/mL. Using serial serum 25(OH)D sampling over 28 weeks, we created a population pharmacokinetic model and performed dosing simulations to achieve 25(OH)D concentrations ≥ 40 ng/mL. In Part 2, the optimal regimen chosen from Part 1 was compared (2:1) to a standard-of-care control dose (600 international units [IU] daily) over 16 weeks. A final population pharmacokinetic model using both parts was developed to perform dosing simulations and determine important co-variates in the pharmacokinetics of vitamin D.
Results
Based on empiric and simulation data, the daily dose of 8000 IU and a loading dose of 50,000 IU were chosen; this regimen raised 25(OH)D concentrations above 40 ng/mL in the majority of participants while avoiding concentrations > 100 ng/mL. A 50,000-IU loading dose led to faster achievement of 25(OH)D therapeutic concentrations (≥ 40 ng/mL). The estimated median (5th–95th percentiles) apparent clearance of vitamin D from the final population pharmacokinetic model was 0.181 (0.155–0.206) L/h. The body mass index z-score was a significant covariate on apparent clearance and was associated with a significantly decreased median half-life in 25(OH)D (body mass index z-score 1.00–1.99: 97.7 days, body mass index z-score 2.00–2.99: 65.9 days, body mass index z-score ≥ 3.00: 39.1 days, p < 0.001).
Conclusions
Obesity impacts vitamin D clearance and the half-life, but serum concentrations > 40 ng/mL can be reached in most children using a loading dose of 50,000 IU followed by a daily dose of 8000 IU.
Clinical Trial Registration
ClinicalTrials.gov identifier number NCT03686150
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Among children aged 6–17 years who are overweight/obese and have asthma with a baseline 25(OH)D concentration from between 10 and 29.9 ng/mL, the oral vitamin D dosing regimen of a 50,000-IU loading dose followed by once-daily 8000 IU over 16 weeks reliably achieved 25(OH)D concentrations above 40 ng/mL without exceeding 100 ng/mL. |
Body mass index was a significant covariate of vitamin D pharmacokinetics; a progressively increasing body mass index was associated with a reduced 25(OH)D half-life. |
Children with severe obesity (z-scores >3) may need higher daily dosing to achieve serum 25(OH)D concentrations above 40 ng/mL. |
1 Introduction
Low serum vitamin D concentrations [25(OH)D] are highly prevalent in obesity [1] and asthma [2]. Asthma is one of the most common chronic illnesses in childhood; the disease burden of uncontrolled asthma in children includes missed school days, parental work absence, limitation of activities of daily living, emergency department visits, and hospitalizations [3]. Low vitamin D concentrations are associated with higher rates of asthma exacerbations [2, 4], and decreased lung function [5]. Similarly, obesity is a burgeoning problem throughout the USA [6]. Patients with asthma who are overweight or obese tend to have increased asthma symptoms [7,8,9]. The 25(OH)D serum concentration that is optimal for asthma is not known; although it has been proposed that concentrations above 40 ng/mL are particularly beneficial [10, 11] owing to enhanced anti-infective and anti-inflammatory activity [12, 13]. For children with asthma and overweight/obesity to attain serum 25(OH)D concentrations above 40 ng/mL, the optimal dosing regimen of oral vitamin D is unknown. However, it is likely that higher doses are needed given the large volume of distribution for lipophilic molecules that exists with obesity. Defining vitamin D pharmacokinetics in children with overweight/obesity is a critical first step in evaluating the role of vitamin D as a potential low-cost, readily available asthma therapy.
Studies of vitamin D supplementation in adults with overweight/obesity have demonstrated decreased bioavailability [14], which was attributed to increased serum 25(OH)D deposition in body fat [15,16,17]. Studies are lacking that describe the pharmacokinetics of vitamin D supplementation in children with overweight/obesity. The Vitamin D Oral Replacement in Asthma (VDORA) pharmacokinetic (PK) study intends to fill this gap by describing key PK parameters and identifying the appropriate dose of oral vitamin D needed to raise 25(OH)D concentrations above 40 ng/mL in children with overweight/obesity and asthma. The primary paper including clinical outcomes will be presented separately. Here, we present the pharmacokinetics of vitamin D in this randomized clinical trial of oral vitamin D supplementation in children with overweight/obesity and asthma.
2 Methods
2.1 Ethics Approval and Consent
The University of Arkansas for Medical Sciences Institutional Review Board served as the institutional review board of record for this multi-site study. Informed consent and assent were obtained from the participants and their parents or legally authorized representatives (caregiver) prior to any research-related procedures. The Clinical Trials website (https://clinicaltrials.gov) study number was NCT03686150.
2.2 Study Design and Population
The trial design of the VDORA study, a multi-center, randomized, open-label PK study, has been previously described [17]. Briefly, VDORA was conducted in two parts: Part 1 was a PK analysis to inform optimal dosing to test in Part 2. Part 2 was a 16-week study to confirm the success of the chosen dosing regimen to achieve a serum concentration of 25(OH)D ≥ 40 ng/mL. Both parts included children aged between 6 and 17 at enrollment. Inclusion criteria also included the following: body mass index (BMI) ≥ 85% for age and sex; physician-diagnosed asthma; and a baseline serum 25(OH)D concentration between 10 ng/mL and < 30 ng/mL. Exclusion criteria included the following: taking supplemental vitamin D > 1000 international units (IU) per day; plans to move out of the study area; another child in the household enrolled in the study; and medical issues that in the opinion of the investigator put the participant at risk or would affect the results of the study.
2.2.1 Study Design
Part 1 Participants were randomized (1:1:1:1) into one of four 16-week vitamin D3 dosing cohorts: Cohort A received a single 50,000-IU loading dose plus a 6000-IU daily dose; Cohort B received a single 50,000-IU loading dose plus a 10,000-IU daily dose; Cohort C received no loading dose but a 6000-IU daily dose; and Cohort D received no loading dose but a 600-IU ‘standard-of-care’ daily dose. After four participants in each dosing cohort (16 total participants) completed PK sampling at week 20, an interim analysis was performed to determine the recommended dose for use in Part 2 of the study. Criteria for selection for Part 2 included achieving a 25(OH)D concentration > 40 ng/mL at week 16 in the majority of participants, while minimizing the number of participants with 25(OH)D concentrations exceeding 100 ng/mL.
Part 2 Based on the results of the Part 1 interim analysis, an optimal regimen was chosen to be given through week 16 (Cohort E). This optimal regimen was compared to a standard-of-care dose of 600 IU daily (Cohort F). Participants in Part 2 were randomized in a 2:1 ratio (i.e., two allotments of the optimal regimen to one allotment of a 600-IU comparator). The randomization used a stratified block scheme, based on age (6–11 vs 12–17 years) and age-adjusted and sex-adjusted BMI percentiles (overweight [85th–94th] vs obese [≥ 95th%]).
2.3 Blood Draw and Sample Preparation
In both Part 1 and Part 2, serum 25(OH)D was evaluated at baseline and at pre-determined times during the dosing phase (week 1, between week 1 and week 3 [optional], weeks 4, 8, 12, and 16) and during follow-up (weeks 20, 24, and 28) to assess elimination kinetics. Blood samples were collected by venipuncture or the finger stick method (venipuncture only at baseline and week 16 when cytokines were collected). Blood samples for determination of serum 25(OH)D were analyzed by Quest Labs using a validated immunoassay.
2.4 Pharmacokinetic and Statistical Analysis
Available demographic and clinical data were summarized within each dosing cohort using standard summary statistics (e.g., mean, median, range) for continuous variables or counts and percentages for categorical variables. Pharmacokinetic calculations were conducted on Part 1 and Part 2 individually and combined.
2.4.1 Part 1
An interim population PK (popPK) analysis using 25(OH)D concentrations measured from serum samples collected after oral administration of vitamin D3 was performed using the software for nonlinear mixed-effects modeling (NONMEM, version 7.4) and the first order conditional estimation method with interaction. One-compartment and two-compartment structural models were evaluated. Both linear and nonlinear absorption and elimination kinetics implemented using Michaelis–Menten kinetics were tested. A multivariable covariate screen was performed for potential associations with PK parameters. The following potential covariates were screened: total body weight, fat-free mass, normal fat mass, lean body mass, age, body mass index (BMI), BMI percentile, obese (BMI ≥ 95th percentile), morbidly obese (BMI ≥ 99th percentile), season, ethnicity, race, and sex. During the model building process, potential covariates that reduced the objective function value by more than 3.84 (p < ~ 0.05 for 1 degree of freedom) were planned for inclusion in the subsequent multivariable analysis. A forward inclusion approach with backwards elimination was planned for the multivariable step, and a reduction in the objective function value of 7.88 (p < ~ 0.005 for 1 degree of freedom) was required for retention of a covariate in the final model. Empirical Bayesian estimates (EBEs) of individual participant PK parameters were generated from the final model using the post-hoc subroutine and were summarized by age group (6–<12 years and ≥ 12 years) and weight group (overweight, obese, and morbidly obese). The Wilcoxon rank-sum test was performed to compare the distribution of EBE PK parameters between age groups and between weight groups.
Using the final PK model and individual EBEs of PK parameters for the Part 1 study participants, serum concentration–time profiles of 25(OH)D were simulated for each participant. A 16-week treatment course was simulated for each of the following dosing regimens: (1) single 50,000-IU loading dose and 10,000-IU daily dose; (2) single 50,000-IU loading dose and 9000 IU daily dose; (3) single 50,000-IU loading dose and 8000-IU daily dose; (4) single 50,000-IU loading dose and 5000-IU daily dose; (5) 8000-IU daily dose; and (6) 600-IU daily dose. The percentage of simulation subjects (the Part 1 study participants included in the PK model) with serum 25(OH)D ≥ 40 ng/mL, serum 25(OH)D >100 ng/mL, and serum 25(OH)D > 150 ng/mL at 16 weeks was calculated for each dosing regimen. The best dosing regimen was determined as the one resulting in serum 25(OH)D ≥ 40 ng/mL at 16 weeks in a majority (i.e., 75%) of subjects and serum 25(OH)D > 100 ng/mL in a minimum number of subjects. In addition, a 52-week treatment course was simulated for regimen 1 and regimen 3 above. The percentage of simulation subjects with serum 25(OH)D ≥40 ng/mL, serum 25(OH)D >100 ng/mL, and serum 25(OH)D >150 ng/mL at 52 weeks were calculated for regimen 1 and regimen 3.
The comparability analysis of PK model-predicted 25(OH)D concentrations (using the popPK model derived from Part 1) was compared to observed 25(OH)D concentrations in VDORA Part 2. The overall bias and imprecision of predicted plasma concentrations was assessed through calculation of the median percentage prediction error (MPPE) and median absolute percentage prediction error (MAPE), respectively, according to the following equations:
where CONCplasma_OBS is the observed plasma concentration and CONCplasma_PRED is the predicted plasma concentration based on the PK model from VDORA Part 1. The MPPE and MAPE values less than 15% were considered acceptable.
2.4.2 Combined Model Development: Part 2
A popPK model was refitted employing PK data combined from Parts 1 and 2. A two-compartment popPK model with linear absorption and elimination kinetics was employed as the base model. The refitted model was guided by goodness-of-fit plots, plausibility of parameter estimates, and reductions in inter-individual variability (IIV) for structural and residual error parameters, as well as objective function and shrinkage values. Model output was processed using software Stata (Version 13.1; Statacorp LLC, College Station, TX, USA), and the Xpose, ggplot2, and lattice packages in the software R. Inter-individual variability and shrinkage were calculated using Eqs. 3 and 4, respectively. Inter-individual variability was not retained on a given parameter if shrinkage was >40%.
where Pij denotes the estimate of parameter j in the ith individual, θPop,j is the population value for parameter j, and ηij denotes the deviation from the average population value for parameter j in the ith individual. The random variable η is assumed to be normally distributed with a mean zero and variance ω2.
where \({\text{SD}}(\eta_{j}\)) is the standard deviation of the jth ETA overall number of subjects and \(\omega j,j\) is the population variance of the jth random effect.
Covariate evaluation was performed using both visual and statistical approaches to examine the relationship between PK Pmodel parameters and demographic factors and co-administered medications, as applicable. Weight status including BMI, BMI z-score, and BMI percentile were evaluated using both fixed and estimated exponents. Similar to Part 1, a standard forward inclusion-backward elimination approach was used to include covariates in the popPK model. Additional categorical weight-related covariates were evaluated on the allometric scaling relationship (obese or morbidly obese) evaluated on a univariate and multivariate analysis. To judge inclusion of covariates in the PK model, an objective function value drop of 3.84, corresponding to a p-value of 0.05 and 1 degree of freedom, was used for the forward inclusion, and 10.83 (p = 0.001) was used for the backward elimination step. A popPK model was refitted employing combined PK data from Parts 1 and 2 of the VDORA study.
Continuous covariates were normalized to the population median value as described in Eq. 5, whereas for categorical covariates, a relationship as shown in Eq. 6 was used.
where PARij denotes the estimate of parameter j in the ith individual, θPop,j is the population value for parameter j, \({cov}_{i}\) denotes the individual covariate value, \({cov}_{m}\) is the population median covariate value, \({\theta }_{cov}\) is a parameter that represents the covariate effect, and CATEGORICAL is a dichotomous categorical variable that can take on the value of zero or one for each level of a categorical predictor.
Covariates for which there was >50% missing data were not evaluated in the model. All continuous covariates were imputed after stopping the dosing period. The imputation was performed using the last covariate recorded value. Missing values for categorical covariates were not imputed.
The following diagnostic plots were generated: individual predictions (IPRED) and population predictions (PRED) versus observed data; conditional weighted residuals versus PRED and time; and individual weighted residuals versus IPRED. The precision of popPK parameters was evaluated using non-parametric bootstrapping to generate the 95% confidence intervals of parameter estimates. Visual predictive checks were performed for the final model by generating 1000 Monte Carlo simulation replicates per timepoint and simulated results were compared with those observed in the study. The following diagnostic plots were generated among others: IPRED and PRED versus observed data; conditional weighted residuals versus PRED and time; and individual weighted residuals versus IPRED.
Precision of popPK parameters was evaluated using non-parametric bootstrapping to generate the 95% confidence intervals of parameter estimates. Visual predictive checks were performed for the final model by generating 1000 Monte Carlo simulation replicates per timepoint and simulated results were compared with those observed in the study.
3 Results
3.1 Participant Characteristics of the PK study
Part 1 baseline characteristics were generally similar across the dosing cohorts including baseline BMI, BMI percentile, age, race/ethnicity, and baseline serum 25(OH)D concentrations. Table 1 also shows that these baseline characteristics were generally similar among Part 1 and Part 2 participants.
3.2 Part 1 PK Model Development and Simulations
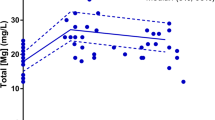
Part 1 of the VDORA study evaluated the population pharmacokinetics of 25(OH)D using 227 serum concentrations among 44 pediatric participants, including participants who were overweight (N = 9), obese (N = 11), and morbidly obese (N = 24). The median (range) number of samples collected per participant was 5 (1–9). Part 1 25(OH)D serum concentrations during the 16-week treatment period and the 12-week follow-up period for each dosing cohort are shown in Fig. 1.
Different PK structural models were evaluated. Based on model selection criteria, a two-compartment model with linear absorption and linear elimination kinetics fit the data best. A constant endogenous input rate to the central compartment for 25(OH)D was included in the model. A parameter (BASE) was used to describe the baseline 25(OH)D concentration in the model. Scatter plots of physiologically plausible covariates versus ETA_CL and ETA_BASE, the individual deviation from the population typical value for apparent clearance (CL/F) and BASE, respectively, were used to determine which covariates would be assessed for inclusion in the final model. A summary table of the covariate model building process is shown in Table 1 of the Electronic Supplementary Material (ESM). The final popPK model did not identify any significant covariates. Parameter estimates for the final PK model are shown in Table 2.
Simulated 25(OH)D serum concentration–time profiles after a 16-week treatment in simulation participants using the final Part 1 PK model and individual EBE PK parameters are shown in Fig. 2. Notably, the precision of dosing simulations was limited, especially with large IIV on CL/F, the main parameter affecting plasma concentrations at steady state. The percentages of simulation participants with serum 25(OH)D ≥ 40 ng/mL, ≥ 100 ng/mL, and ≥ 150 ng/mL at 16 weeks are shown in Table 3. A single 50,000-IU loading dose and an 8000-IU daily dose resulted in serum 25(OH)D ≥ 40 ng/mL at 16 weeks in a majority of subjects (82%) and serum 25(OH)D > 100 ng/mL in 0% of subjects. Higher maintenance doses (9000 IU daily or 10,000 IU daily) increased the percentage of subjects with serum 25(OH)D ≥ 40 ng/mL at 16 weeks (93% and 98%, respectively), but also resulted in a small portion of subjects with serum 25(OH)D > 100 ng/mL (2% and 7%, respectively).
Serum 25(OH)D concentration–time profiles during 52 weeks of treatment in simulation participants using the final PK model and individual EBE PK parameters are shown in Fig. 3. A single 50,000-IU loading dose plus 10,000 IU daily for 52 weeks resulted in serum 25(OH)D ≥40 ng/mL, > 100 ng/mL, and >150 ng/mL in 98%, 48%, and 7% respectively; while the same loading dose plus a reduction to 8000 IU daily for 52 weeks resulted in serum 25(OH)D ≥40 ng/mL, > 100 ng/mL, and > 150 ng/mL of 98%, 27%, and 0% respectively. Results from Part 1 of the study led the study team to select a loading dose of 50,000 IU followed by a daily dose of 8000 IU to be confirmed in Part 2. Omitting the loading dose resulted in similar exposures at week 16 but resulted in concentrations below the PK target earlier in the study period.
3.3 Part 2 Combined PK Model Development
3.3.1 Part 2 Concentrations of 25(OH)D
A total of 63 participants were enrolled and randomized to one of two Part 2 dosing groups: (1) single 50,000-IU loading dose and an 8000-IU daily dose or (2) no loading dose and a 600-IU daily dose regimen. Baseline characteristics for Part 2 participants are shown in Table 1. Part 2 25(OH)D serum concentrations during the 16-week treatment period and the 12-week follow-up period for the two dosing cohorts are shown in Fig. 4.
A total of 848 25(OH)D serum concentrations from 109 combined participants (46 from Part 1 and 63 from Part 2) were collected after administration of vitamin D and were included to perform the popPK analysis. A comparability analysis was conducted on PK model-predicted 25(OH)D concentrations from Part 1 compared to observed 25(OH)D concentrations in Part 2. The overall bias and imprecision of predicted plasma concentrations expressed in terms of MPPE and MAPE were − 1.67% and 8.17%, respectively (Table 2 of the ESM).
A covariate analysis identified weight as a significant covariate. After evaluating allometric scaling of weight on CL/F and apparent volume of distribution (V/F) and subsequent evaluation of the BMI Z-score as a covariate, BMI Z-score inclusion on CL/F and V/F showed improved parameter precision and was retained in the final model. The covariate analysis identified weight as a significant covariate on CL/F and V/F, and the BMI Z-score as a significant covariate on CL/F and V/F. The BMI Z-score improved parameter precision compared to weight and was included in the final model. After including the BMI z-score in the popPK analysis, the IIV (expressed as % coefficient of variation) on CL/F was reduced from 63 to 59% and intercompartmental clearance (Q)/bioavailability (F) (Q/F) reduced substantially from 120% to 104%, and BASE reduced from 30 to 29%. The equation for the final PK model was:
where ZBMIi denotes the BMI z-score of an individual participant, CL, Vc, and Q are the population estimates for a median BMI z-score of 2.36, and CLi, Vci, and Qi are the estimates for an individual participant. Refer to Table 3 of the ESM for a summary of the combined covariate model-building process for 25(OH)D.
The final popPK parameter estimates for the final model, and comparison with parameter estimates between Part 1 and Part 2, are shown in Table 4. In the final popPK model, the elimination half-life of 25(OH)D was calculated after implementing the BMI Z-score. Morbidly obese subjects showed lower half-lives (p < 0.001), compared with overweight and obese subjects (Table 5). Refer to Figs. 2–4 of the ESM for further details on the model evaluation including diagnostic plots and visual predictive check. Overall, the final popPK model characterized the data well with no evidence of model misspecification. The majority of observed concentrations fell within the 90% prediction interval.
4 Discussion
This multi-center, randomized, 16-week, open-label study evaluated the PK parameters and optimal dosing of oral vitamin D in vitamin D-insufficient or deficient children who are overweight or obese and have asthma. We found that the dosing regimen of a 50,000-IU single oral loading dose plus once-daily oral dosing of 8000 IU was successful in achieving 25(OH)D concentrations > 40 ng/mL in most patients, with important variability and changes in the half-life associated with BMI z-scores. While this study focused on children with asthma and overweight/obesity, a better understanding of vitamin D pharmacokinetics in children with overweight/obesity will be clinically useful for many pediatric disorders.
25(OH)D is the major circulating form of vitamin D and is commonly used to measure vitamin D status [18]. Previous studies have indicated that a 25(OH)D serum concentration above 40 ng/mL may improve asthma control [12, 13, 19, 20]. The upper bound of normal serum 25(OH)D is typically 100 ng/mL in most laboratories, and toxicity is unlikely to occur at concentrations < 150 ng/mL [21, 22]. However, optimal dosing to achieve a concentration of 25(OH)D ≥ 40 ng/mL is not known in children who are overweight or obese.
Vitamin D, a hormone, can be obtained by dietary supplementation, but it is also produced endogenously in humans following sunlight exposure. Bile salts must be present in the body for the enteral absorption of exogenous vitamin D. Once vitamin D enters the circulation, most of it becomes stored in body fat. Vitamin D is converted to its active form in two steps: first, it is converted to 25(OH)D in the liver; then it is further metabolized in the kidneys to the active form 1,25(OH)2D [23]. Vitamin D is mainly eliminated through biliary excretion. The relationship between vitamin D dose and serum 25(OH)D concentration was reported to be nonlinear in studies using a meta-analysis of data collected after a wide range of vitamin D dosing [18, 23]. Bioavailability of the active form of vitamin D is impacted by several factors including sunlight exposure, nutrition, vitamin D metabolism gene polymorphisms, and albumin and vitamin D binding protein levels [24, 25]. Other researchers have shown that obesity is associated with lower vitamin D bioavailability in male adults.[14, 15] These obesity-related differences in bioavailability are present with both oral supplementation and ultraviolet light treatment [14]; this suggests that lower bioavailability in obesity is related to vitamin D deposition in a larger body fat compartment.
Very few studies have published pediatric PK results involving vitamin D following oral supplementation. In one study involving vitamin D supplementation, Lewis and colleagues gave otherwise healthy children 4000 IU daily, which yielded a median 25(OH)D increase of 30.45 ng/mL after 12 weeks [26]. Forno and colleagues gave children with asthma 4000 IU daily (without a loading dose) for 48 weeks, which yielded mean 25(OH)D concentrations at 16, 32, and 48 weeks of 57.2 ng/mL, 53.8 ng/mL, and 49.4 ng/mL, respectively.[27]
Principles of drug development recommend phase II trials to determine the optimal dose of a drug prior to larger pivotal efficacy trials [28, 29]. Little to no data exist describing the PK parameters and optimal dosing of oral vitamin D in children with obesity. The popPK model developed in Part 1 of this study recommended a target vitamin D dosage regimen that included a single 50,000-IU dose followed by daily oral doses of 8000 IU. In Part 2, 79% of the subjects assigned to the 50,000-IU regimen achieved the 25(OH)D concentration target (≥ 40 ng/mL), in contrast to zero subjects who received the standard-of-care regimen (no loading dose followed by a 600-IU daily dose). Of the participants who achieved the 25(OH)D target, 6% had concentrations > 100 ng/mL and no participant exceeded 150 ng/mL at week 16. After evaluating the PK model initially developed in Part 1 to the data from Part 2, significant bias and imprecision were not detected. The MPPE and MAPE values were below 15%, which was considered acceptable.
We found that the degree of obesity had a significant effect on the pharmacokinetics of 25(OH)D. The average 25(OH)D concentrations decreased with progressively higher BMI z-scores, suggesting that children with severe obesity (BMI z-scores > 3) may need higher dosing to achieve 25(OH)D concentrations ≥ 40 ng/mL. Specifically, the mean population-predicted 25(OH)D concentration in this subgroup was 33.7 ng/mL, below the ideal target of 40 ng/mL. As the BMI z-score was included as a covariate, the PK model in this study could be used to conduct dosing simulations for individual patients to derive more precise dosing; however, the results may not be reliable in populations different from the study population (e.g., children who are not overweight/obese).
During PK model development, both weight and the BMI z-score were important covariates on weight and volume of distribution. We found that the 25(OH)D half-life decreased with an increasing BMI z-score. However, because we used fixed exponents to characterize the effect of the BMI z-score on clearance and volume of distribution, our estimated half-lives may not be precisely estimated. Estimates of half-lives for 25(OH)D vary widely in the literature, from 14 to 21 days up to 111 days [18], consistent with the range observed in our study (46–117 days). Notably, 25(OH)D has widely variable pharmacokinetics and is difficult to estimate because of potential differences in endogenous production and sunlight exposure, exogenous dietary intake, and adherence to vitamin D supplementation, all of which could impact our PK parameter estimates. Additionally, vitamin D binding protein has been reported to be lower in obese versus non-obese patients, which could alter the amount of free drug available for clearance and potentially the half-life [30].
No major discrepancies were detected between the popPK models developed in Part 1 and after combining Part 1 and Part 2 PK data. However, there were some differences in the volume of the peripheral compartment going from 724 to 169 L, which could be owing to the better characterization of the distribution phase after obtaining high 25(OH)D concentration sample points and the consequent increment in IIV related to inter-compartmental clearance (% coefficient of variation: 121%). Reassuringly, the bootstrap analysis did not detect any inconsistencies in the popPK parameters. After including weight in the popPK analysis, the IIV (expressed as % coefficient of variation) on Q/F reduced substantially from 120 to 96%, clearance from 63 to 61%, and BASE from 30 to 29%. This suggests that weight is an important covariate for vitamin D pharmacokinetics.
This PK study had limitations that should be considered. Our main endpoint for assessing response to oral supplementation was 25(OH)D concentrations. Though this endpoint is commonly accepted, there are other factors that affect free ‘bioavailable’ vitamin D that we did not collect including serum albumin and vitamin D binding protein levels. Additionally, we did not collect pharmacogenetics of vitamin D metabolism genes (e.g., GC, VDR), which in some reports have been influential in vitamin D action. Though we did include seasonality in PK models, which can affect endogenous vitamin D production, we did not include geographic latitude.
We speculate that for patients with BMI z-scores > 3, an additional 1–2 weekly loading doses may be considered if rapidly achieving the target of 25(OH)D ≥ 40 ng/mL is of key importance. It is important to note that our study treated participants for 16 weeks and then discontinued supplementation. Simulations showed that if daily treatment in the range of 8000 IU or higher is continued for up to a year, some participants are likely to reach 25(OH)D concentrations of 100–150 ng/mL or higher. For this reason, clinicians should use caution with long-term treatment and consider periodic 25(OH)D evaluations. More research is needed in the area of vitamin D supplementation and the optimal long-term regimen for children with obesity.
5 Conclusions
In this study, the majority of children (n = 32, 79%) receiving a single 50,000-IU loading dose of vitamin D plus 8000 IU daily achieved the target 25(OH)D concentration of 40 ng/mL. A popPK model was developed using all data. The BMI z-score was found to be an important covariate of vitamin D pharmacokinetics, and there was an apparent decrease in the 25(OH)D half-life with a progressively increased BMI z-score. Nevertheless, dosing simulations using the final PK model suggested that a single 50,000-IU loading dose plus 8000 IU daily is sufficient to achieve 25(OH)D concentrations (≥ 40 ng/mL) in the majority of children aged ≥ 6 years who are overweight or obese. However, children with severe obesity (z-scores > 3) may need optimized dosing to achieve 25(OH)D concentrations ≥ 40 ng/mL.
References
Turer CB, Lin H, Flores G. Prevalence of vitamin D deficiency among overweight and obese US children. Pediatrics. 2013;131(1):e152–61.
Brehm JM, Schuemann B, Fuhlbrigge AL, Hollis BW, Strunk RC, Zeiger RS, Childhood Asthma Management Program Research Group, et al. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J Allergy Clin Immunol. 2010;126(1):52-58.e55.
Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016;137(1):1–7.
Confino-Cohen R, Brufman I, Goldberg A, Feldman BS. Vitamin D, asthma prevalence and asthma exacerbations: a large adult population-based study. Allergy. 2014;69(12):1673–80.
Liu J, Dong YQ, Yin J, Yao J, Shen J, Sheng GJ, et al. Meta-analysis of vitamin D and lung function in patients with asthma. Respir Res. 2019;20(1):161.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14.
Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169–79.
Lang JE. Contribution of comorbidities to obesity-related asthma in children. Paediatr Respir Rev. 2021;37:22–9.
Reyes-Angel J, Kaviany P, Rastogi D, Forno E. Obesity-related asthma in children and adolescents. Lancet Child Adolesc Health. 2022;6(10):713–24.
Wolsk HM, Chawes BL, Litonjua AA, Hollis BW, Waage J, Stokholm J, et al. Prenatal vitamin D supplementation reduces risk of asthma/recurrent wheeze in early childhood: a combined analysis of two randomized controlled trials. PLoS ONE. 2017;12(10): e0186657.
Litonjua AA. Vitamin D and childhood asthma: causation and contribution to disease activity. Curr Opin Allergy Clin Immunol. 2019;19(2):126–31.
Weiss ST, Litonjua AA. Vitamin D dosing for infectious and immune disorders. Thorax. 2015;70(10):919–20.
Litonjua AA, Weiss ST. Vitamin D status through the first 10 years of life: a vital piece of the puzzle in asthma inception. J Allergy Clin Immunol. 2017;139(2):459–61.
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690–3.
Zhou JC, Zhu YM, Chen Z, Mo JL, Xie FZ, Wen YH, et al. Oral vitamin D supplementation has a lower bioavailability and reduces hypersecretion of parathyroid hormone and insulin resistance in obese Chinese males. Public Health Nutr. 2015;18(12):2211–9.
O’Sullivan BP, James L, Majure JM, Bickel S, Phan LT, Serrano Gonzalez M, et al. Obesity-related asthma in children: a role for vitamin D. Pediatr Pulmonol. 2021;56(2):354–61.
James L, O’Sullivan BP, Majure M, Lang J, Ounpraseuth S, Hornik C, et al. Protocol for the Vitamin D Oral Replacement in Asthma (VDORA) study. Contemp Clin Trials. 2022;120: 106861.
Mazahery H, von Hurst PR. Factors affecting 25-hydroxyvitamin D concentration in response to vitamin D supplementation. Nutrients. 2015;7(7):5111–42.
Hollams EM, Teo SM, Kusel M, Holt BJ, Holt KE, Inouye M, et al. Vitamin D over the first decade and susceptibility to childhood allergy and asthma. J Allergy Clin Immunol. 2017;139(2):472-81.e479.
Brehm JM, Schuemann B, Fuhlbrigge AL, Hollis BW, Strunk RC, Zeiger RS, et al. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J Allergy Clin Immunol. 2010;126(1):52-58.e55.
Holick MF. Vitamin D is not as toxic as was once thought: a historical and an up-to-date perspective. Mayo Clin Proc. 2015;90(5):561–4.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
Ocampo-Pelland AS, Gastonguay MR, French JF, Riggs MM. Model-based meta-analysis for development of a population-pharmacokinetic (PPK) model for vitamin D3 and its 25OHD3 metabolite using both individual and arm-level data. J Pharmacokinet Pharmacodyn. 2016;43(2):191–206.
Madden K, Feldman HA, Chun RF, Smith EM, Sullivan RM, Agan AA, et al. Critically ill children have low vitamin D-binding protein, influencing bioavailability of vitamin D. Ann Am Thorac Soc. 2015;12(11):1654–61.
Denburg MR, Kalkwarf HJ, de Boer IH, Hewison M, Shults J, Zemel BS, et al. Vitamin D bioavailability and catabolism in pediatric chronic kidney disease. Pediatr Nephrol. 2013;28(9):1843–53.
Lewis RD, Laing EM, Hill Gallant KM, Hall DB, McCabe GP, Hausman DB, et al. A randomized trial of vitamin D(3) supplementation in children: dose-response effects on vitamin D metabolites and calcium absorption. J Clin Endocrinol Metab. 2013;98(12):4816–25.
Forno E, Bacharier LB, Phipatanakul W, Guilbert TW, Cabana MD, Ross K, et al. Effect of vitamin D3 supplementation on severe asthma exacerbations in children with asthma and low vitamin D levels: the VDKA randomized clinical trial. JAMA. 2020;324(8):752–60.
EMA. ICH guideline E8 (R1): general considerations for clinical studies. Amsterdam, The Netherlands: European Medicines Agency; 2021.
Schmidt R. Dose-finding studies in clinical drug development. Eur J Clin Pharmacol. 1988;34(1):15–9.
Yousefzadeh P, Shapses SA, Wang X. Vitamin D binding protein impact on 25-hydroxyvitamin D levels under different physiologic and pathologic conditions. Int J Endocrinol. 2014;2014: 981581.
Acknowledgments
The authors acknowledge the dedication of the research coordinators and staff of the IDeA States Pediatric Clinical Trial Research Network. SJB receives support from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
U24 OD024957 (University of Arkansas Data Coordinating and Operations Center), UG1 OD024942 (University of Mississippi Medical Center), UG1 OD024943 (University of Kansas Medical Center), UG1 OD024944 (Alaska Native Tribal Health Consortium), UG1 OD024945 (Arkansas Children’s Research Institute), UG1 OD024946 (Dartmouth College), UG1 OD024947 (University of New Mexico Health Sciences Center), UG1 OD024948 (University of Hawaii at Manoa), UG1 OD030016 (West Virginia University), UG1 OD024950 (University of Oklahoma Health Sciences Center), UG1 OD024951 (Rhode Island Hospital), UG1 OD024952 (University of Montana), UG1 OD024953 (University of Nebraska Medical Center), UG1 OD024954 (University of Louisville), UG1 OD024955 (University of Vermont and State Agricultural College), UG1 OD024956 (University of South Carolina at Columbia), UG1 OD024958 (Nemours Alfred I. duPont Hospital for Children), UG1 OD024959 (Louisiana State University Pennington Biomedical Research Center), UG1 OD030019 (Avera Research Institute Center for Pediatric and Community Research), 5110575 (Duke University).
Conflicts of Interest/Competing Interests
Jason E. Lang reports consulting fees from AbbVie, Inc. unrelated to the current project. Saranya Venkatachalam, Jessica Snowden, Laura James, Scott Bickel, J. Marc Majure, Rodrigo Gonzalez Ramirez, Brian O’Sullivan, and Christoph P. Hornik have no conflicts of interest that are directly relevant to the content of this article. Stephen Balevic is a consultant for UCB and has received research funding from Purdu Pharma.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Authors’ Contributions
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lang, J.E., Ramirez, R.G., Balevic, S. et al. Pharmacokinetics of Oral Vitamin D in Children with Obesity and Asthma. Clin Pharmacokinet 62, 1567–1579 (2023). https://doi.org/10.1007/s40262-023-01285-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01285-9