Abstract
The evaluation of errors in use with different inhaler devices is challenging to quantify as there are a number of definitions of critical and non-critical errors with respect to inhaler use; in addition, performance characteristics of the device, such as airflow resistance, can also influence effective use in the real-world setting. Repeated observations and checking/correcting inhaler use are essential to optimise clinical effectiveness of inhaled therapy in patients. Breezhaler® is a single unit-dose dry powder inhaler used in chronic obstructive pulmonary disease and in asthma (budesonide) that has low airflow resistance, making it easier for patients of varying disease severities to achieve the inhalation flow rate required for lung deposition of treatment. Similar to Breezhaler®, the Aerolizer® is a single unit-dose dry powder inhaler used in asthma management with low airflow resistance. Studies have shown relatively low rates of critical errors with Breezhaler® and Aerolizer®, with similarities in the critical errors reported; these data on critical errors together with similarities in the usability of Breezhaler® and Aerolizer® further support the functional similarity between the two devices in both asthma and chronic obstructive pulmonary disease. Breezhaler® also has patient-feedback features, including use of a transparent drug capsule that can be checked after inhalation to see it is empty. The low resistance of the dose-confirming Breezhaler® results in less inspiratory effort being required by patients for its effective use, which allows the device to be used effectively across a wide age range of patients and disease severities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Evaluation of use errors with inhalers is challenging because of differences in the definitions of critical and non-critical errors, plus performance characteristics of an inhaler can influence clinical effectiveness. |
Breezhaler® is a single unit-dose dry powder inhaler that has relatively low rates of critical errors. |
Breezhaler® has low airflow resistance, making it easier for patients across a wide age range and disease severities to achieve the inhalation flow rate required for effective drug deposition in the lungs. |
1 Introduction
While inhalation is the delivery route of choice for many drug formulations used in the treatment of lung diseases such as chronic obstructive pulmonary disease (COPD), asthma and cystic fibrosis, incorrect use of the inhalation devices can lead to poor symptom control and even disease worsening [1]. Correct use of the various inhaler devices results in high bronchial concentrations of treatments while keeping systemic bioavailability to a minimum [2]. However, in 2005, Fink and Ruben reported that 28–68% of patients did not use their pressurised metered-dose inhaler (pMDI) or dry powder inhaler (DPI) well enough to provide clinical benefit from their prescribed medication; they also reported that 39–67% of healthcare workers failed to describe the critical steps for inhaler use to their patients [3].
In asthma, despite available therapies, many patients remain uncontrolled with poor inhaler technique identified as a key contributing factor [4]. A recent study has reported that incorrect inhaler handling was present in nearly 70% of patients with asthma [5]. For the majority of inhaler devices, with the exception of the recent development of digital ‘smart inhaler’ devices, patients are unable to ascertain whether they have inhaled the drug dose correctly [6]. In reality, it is likely that patients believe that they are using the devices correctly but are, in fact, using them incorrectly; this can result in reduced drug delivery and effectiveness, leading to reduced adherence and lung function, increased symptoms and risk of hospitalisation, and reduced quality of life.
There are a number of different types of errors that can occur with inhaler use, and the type of error can be specific to the inhaler device or type of device. Identification of critical errors, specific to the inhaler device, may help improve patient outcomes [4]. Furthermore, a recent study of inhaler use in patients with COPD found that ease of use (self-explaining) should be considered when prescribing inhalers for the first time [7], and that this should be accompanied by training and repeated counselling to increase correct inhaler use [8,9,10]. Counselling has also been shown to improve pMDI inhaler technique in adolescents with asthma [11]. In addition, performance characteristics of the device, such as airflow resistance, can also influence effective use in the real-world setting. This review evaluates the types of errors that can occur with inhaler device use, how the Breezhaler® compares with other devices in terms of inhalation errors and the impact that device airflow resistance can have on effective use.
2 Types and Clinical Impact of Errors
Although there are a number of definitions of errors and critical errors with respect to inhaler use, in this review, we largely restrict our appraisal to those studies using the most common definition of the term, namely incorrect inhaler technique(s) that leads to low or no deposition of medication in the airways and lungs [12,13,14,15,16,17,18,19,20,21,22,23,24]. Whilst important, the possibilities of overdosing when using an inhaler will not be considered in this review, it will focus on the errors and critical errors that result in the active drug not reaching the airways to the extent required to have a clinical effect.
It should be mentioned that in a recent review [12] an error was defined as critical if it had an impact on the effectiveness of the drug. A systematic review conducted to define ‘critical’ errors and their impact on health outcomes in asthma and COPD reported that out of 36 studies giving specific examples of ‘critical’ errors, 32 included a definition of ‘critical’ inhaler errors but the definition varied between studies [25]. In most cases, studies did not provide information on the origin of their definition of a critical error; however, where this information was provided, definitions were commonly taken from previous studies, rather than being formulated by the study researchers [25]. The most common definition was an action affecting the lung deposition of an inhaled drug, resulting in little or no medicine being inhaled or reaching the lungs (n = 27; 14 definitions stated a critical error “would” affect inhalation and drug delivery; 13 others said a critical error “could” affect these). Four articles defined a critical error in terms of effectiveness (i.e. an error that would make aerosol therapy useless), and one publication used a combined definition of deposition and effectiveness (i.e. an error that compromised the potential benefit of the treatment, such as impeding drug deposition or the delivery of an insufficient dose) [25]. This non-consensus between the authors of published studies in the categorisation of critical vs non-critical errors has affected attempts to compare studies and collectively understand the impact of inhaler errors in daily clinical practice [25], which indicates a need for a consensus in defining critical and non-critical errors. It is possible that different definitions between groups/studies in what constitutes a critical error could contribute to different conclusions, even with the same inhaler device type [25]. Overall, the difference between the definitions used can be explained by the fact that the demonstration of inhaler use is only a ‘snapshot’ of reality (i.e. it occurs at a single time point); observation and checking of correct device usage has to be repeated regularly (and any errors corrected) to have a clinical impact for the patient.
The role that errors and critical errors play in asthma treatment outcomes was reported recently in the CritiKal study, which investigated the association between specific inhaler errors and asthma outcomes [4]. The CritiKal study found associations between specific inhaler errors and poorer asthma outcomes, including an increased likelihood of having uncontrolled symptoms and increased exacerbation rates. The study aimed to identify critical inhaler errors, with ‘critical’ meaning those errors related to poor disease outcomes. The analysis utilised data from the iHarp Asthma Review Service and was undertaken between 2011 and 2014 using data from Australia and seven European countries; details from over 5000 patients including data on demographic characteristics were included. The devices tested were Turbuhaler®, Diskus® and pMDI, and errors associated with uncontrolled asthma and an increased risk of exacerbations were: insufficient inspiratory effort; did not breathe out to empty lungs before inhalation; dose compromised after preparation because of shaking or tipping (DPIs only); not sealing lips around the mouthpiece; not removing cap/sliding cover open; head in incorrect position; no breath-hold (or hold breath for less than 3 seconds); actuation did not correspond with inhalation (pMDI only); exhaled into device before inhalation; did not actuate (pMDI only) or did not inhale through mouth [4].
3 Breezhaler® Inhaler
Breezhaler® is a single unit-dose dry powder inhaler (Fig. 1a); in COPD, the device is used to deliver the long-acting β2-agonist indacaterol, the long-acting muscarinic antagonist glycopyrronium, and the combination of indacaterol and glycopyrronium. The combination of indacaterol and the inhaled corticosteroid mometasone furoate (QMF149) and the combination of indacaterol/glycopyrronium/mometasone furoate, both delivered via Breezhaler®, have recently been approved for once-daily treatment of asthma in Europe, Japan and Canada [26,27,28]. In asthma, Breezhaler® is also used to deliver the inhaled corticosteroid budesonide.
In addition to correct handling and inhalation, different inhaler designs and formulation differences can lead to remarkable differences in dispersion efficiency and lung delivery [29]. Breezhaler® has low airflow resistance (compared with Handihaler®), making it easier for patients of varying disease severity to achieve the inhalation flow rate required for lung deposition of treatment [30]. High-resistance devices require greater effort by the patient to achieve inspiratory flows adequate to ensure fine particle dose delivery [31], and some patients with significant pulmonary disease struggle to generate these flows [32, 33].
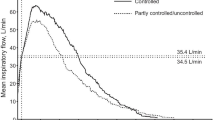
Altman et al. [34] acknowledge that different types of DPI have their own intrinsic resistance, which affects the required inspiratory effort for effective inhalation of the drug from the device. The pressure differential within the DPI created by the patient’s inspiratory manoeuvre drives the speed of airflow, which is dependent on the inhaler’s intrinsic airflow resistance. Those inhalers with low airflow resistance allow patients to inhale with reduced effort [34]. In the study comparing peak inspiratory flow (PIF) achieved by patients with moderate-to-severe COPD who inhaled through Breezhaler®, Handihaler® or Ellipta® inhalers, patients achieved inhalation with the lowest inspiratory effort and produced the highest average PIF reading through the Breezhaler® compared with the other two inhalers; this was irrespective of the severity of COPD, patient age or sex [34]. As can be seen in Fig. 2, the internal resistance of the Breezhaler® device is lower than those of the Diskus®, Turbuhaler® and Handihaler®, allowing a greater flow rate to be achieved with less inspiratory effort [32, 35,36,37,38], which may be beneficial in elderly patients and patients with moderate-to-severe respiratory disease who have difficulty generating the necessary inspiratory flow to achieve an efficient drug delivery from DPIs [32, 33].
Van der Palen et al. [39] noted that patients find low-resistance DPIs more acceptable than high-resistance devices. In elderly patients, irrespective of whether they have COPD, there is a reduced or compromised ability to produce inspiratory flow through DPIs [32]. Bearing this in mind, Molimard and D’Andrea [35] noted that low-resistance DPIs are relatively insensitive to variations in PIF, meaning that the low airflow resistance associated with Breezhaler® would benefit this group of patients and overall can be expected to elicit consistent drug delivery to the lungs.
Similar to Breezhaler®, the Aerolizer® device is a DPI used for single-dose delivery of powder formulations contained in a capsule for inhalation (Fig. 1b). The Aerolizer® is used in the management of asthma and COPD, it has a low airflow resistance and Haidl et al. [1] set values for a requisite minimum flow rate at 40 L/min and an optimum PIF rate at 65 L/min. Two studies by Boshra et al. [40, 41] demonstrated the effectiveness of salbutamol delivered via the Aerolizer® device at a flow rate of >40 L/min and suggested that patients achieving flow rates of >30 L/min should inhale twice through the device to ensure full dose delivery. For both devices, the geometry of the capsule rotation housing and the air inlets are similar to allow similar powder disaggregation even at low flow rates. It is notable that the incidence of critical errors when using Aerolizer® were similar both in patients with asthma and patients with COPD [42, 43] (Table 1).
The similar intrinsic resistance values and inspiratory flow rates associated with the Aerolizer® and Breezhaler® devices [37], together with similarities in geometry and their operational designs, enables potential extrapolation of critical errors with Breezhaler® in COPD to Breezhaler® in asthma and of critical errors reported with Aerolizer® in asthma to Breezhaler® in asthma, although caution is needed when doing this because of intra- and inter-inhaler variability in the emitted dose. It should be noted that the use/handling of the two devices is different, thus each device requires separate instructions on use.
4 Device Handling Errors
In a review intended as a policy document, the Inhaler Error Steering Committee [17] concluded that outcomes for COPD and asthma control are less than optimal and are inferior to those noted in clinical trials, with a major factor contributing to this being inadequate inhaler technique. In reality, multiple errors are made during inhaler use by patients in the community, reducing benefits seen in clinical trials [13]. The findings of this study and other studies on device handling errors imply that there is a requirement for continuing education of both prescribers and patients in the correct use of these devices to promote improvement in the efficacy of treatment [2, 13]. A large observational study involving 3811 primary care patients receiving inhaled medication either via a pMDI or via one of four DPIs (Aerolizer®, Autohaler®, Diskus® or Turbuhaler®) found that the most common errors made by patients are independent of the device being used and fall into categories that include failure to breathe out prior to actuating the device (28.9%) and not holding the breath for a few seconds after inhaling (28.3%) [2]. That said, 76% of patients made at least one error with a pMDI compared with 49–55% with DPIs (Table 2). Critical errors (defined as those that could significantly affect drug disposition to the lungs) were made only by 11–12% of patients treated with Aerolizer®, Autohaler® or Diskus® compared with 28% and 32% of patients treated with pMDI and Turbuhaler®, respectively (Table 2).
In the same study, critical errors for DPIs included blowing into the device before inhaling, lack of capsule insertion, lack of two-button press and release (Aerolizer®); not raising the lever to vertical position (Autohaler®); not sliding the lever as far as possible (Diskus®); and not holding inhaler upright for grip rotation and missing rotating grip clockwise then counter-clockwise until ‘click’ (Turbuhaler®) [2].
In a study of patient-related factors of asthma control, Molimard and Le Gros [14] noted that over 20% of patients were not using inhaler devices correctly, leading to a 0.84-point increase in the asthma control score. It was concluded that, among other factors, the incorrect usage of delivery devices exerts a significant negative effect on the control of asthma.
In a French study conducted by Girodet et al. [44], the use of DPIs in the management of COPD using four devices including Aerolizer® was assessed in terms of the frequency of critical errors. This is of interest because in this instance Aerolizer®, which shares technical characteristics with Breezhaler®, was being used to deliver medication suitable for COPD management rather than asthma management. This study bridges the gap between Aerolizer® and Breezhaler®, enabling possible extrapolation of findings in asthma studies to be viewed as similar to findings in COPD studies. The findings of the study indicated that the frequency of critical errors associated with Aerolizer® (11.5–14.9%) was lower than for those using Autohaler® (37.4%) or Diskus® (38.1%).
Chronic obstructive pulmonary disease studies have shown relatively low rates of critical errors with Breezhaler® [45] (Table 3), and the low frequency of critical errors reported for Aerolizer® in the COPD setting in the study by Girodet et al. [44] (Table 4) further supports the possibility of functional similarity between the two devices in both the COPD and the asthma treatment arena. Using Aerolizer® in patients with suboptimal asthma control, it was reported that 98% of patients treated with formoterol via Aerolizer® correctly performed all essential inhalation manoeuvres compared with 86% of patients treated with formoterol via Turbuhaler® [46]. While clinical efficacy was similar for formoterol delivered via the two devices, handling of Aerolizer® was easier than Turbuhaler® [46].
The results of a study evaluating the device handling errors with Breezhaler® in patients with asthma or COPD found similar errors reported in both patient populations [43] (Table 5), and these were similar to those reported with Aerolizer® in the two populations [42]. This is perhaps not unexpected as the two devices share many technical characteristics (e.g. both are single-dose capsule DPIs with low internal airflow resistance) and many of the learnings with Aerolizer® in asthma are expected to be applicable to Breezhaler®.
It is noteworthy that similarly to Aerolizer® [47], Breezhaler® has some patient feedback features: a ‘Hear–Feel–See’ mechanism aims to reassure patients that they have successfully inhaled the medication [35]. During inhalation, the capsule containing the dry powder formulation spins in the device chamber and produces a ‘whirring noise’, providing positive auditory feedback; a fraction of the lactose component of the drug formulation will deposit in the user’s mouth during inhalation, which the patient tastes, confirming that the drug has left the device; and after inhalation, the patient can visually check that the transparent capsule is empty. The instructions for use ask patients to repeat the inhalation step in case of remaining powder in the capsule, and the device type allows patients to make sure the full dose has been inhaled in a second inhalation if the first inhalation was not sufficient to allow delivery of the entire dose (although it should be noted that the two devices open in slightly difference ways: the Breezhaler® tilts on a hinge whereas the Aerolizer® rotates). Furthermore, these feedback features would apply irrespective of whether a patient had asthma or COPD. However, caution needs to be exercised when results from COPD are extrapolated to asthma as there are differences in the patient populations such as age and comorbidities, which might affect device usability. Yet, this is potentially valid for all devices not just Breezhaler®; therefore, the comparability between devices will probably remain similar.
5 Dose Delivery Considerations
In contrast to pMDIs, DPIs are breath actuated, with most devices relying on a rapid and powerful inhalation manoeuvre for drug delivery [25]. Such inhalation manoeuvres, involving a fast initial acceleration rate, are required to generate a turbulent force inside the inhaler, thus enabling a break-up of the drug formulation into particles [33]. All DPIs demonstrate flow-dependent dose emission [33]. Peak inspiratory flow is related to acceleration rate and variations in PIF values achieved when using different DPIs are linked to the severity of the obstruction and the airflow resistance of the device [33]. For the plethora of DPIs currently available, inspiratory flows between 30 and 90 L/minute are usually required for effective drug delivery to the lungs; however, if the minimum inspiratory flow specific to each of the devices is not achieved, the inhaled dose can be reduced considerably [3].
Although historically PIF has been viewed as the parameter exerting the greatest influence on the performance of dose delivery, a recent study has indicated that flow acceleration, or airflow ramp-up, also contributes to variations in dose delivery to the lungs using DPIs. Ung and Chan [48] examined the effect of airflow ramp-up, or flow acceleration, on dose delivery performance and in doing so compared seven different DPIs: Simoon™ (engineered particles), Podhaler® (engineered particles), Breezhaler® (lactose carrier blend), Diskus® (lactose carrier blend), Handihaler® (lactose carrier blend), Flexhaler® (soft agglomerates) and Twisthaler® (soft agglomerates). Measurement of drug dose delivered and aerosol emission kinetics was undertaken using photometry to ascertain the degree of fluidisation of bulk powder and clearance of the aerosol from each of the seven inhalers under investigation. These were in vitro studies utilising the Alberta idealised mouth–throat model to determine aerosol dispersion quality, deagglomeration, and associated performance with respect to the aerosol reaching the lungs assessed by measurement of the total lung dose. The effect of flow ramp on the total lung dose was found to be relatively small for all investigated DPIs including Breezhaler®, except for Asmanex® and Twisthaler®. Thus, Breezhaler® appears to have the potential for a high level of consistency of lung delivery [48] across a wide range of flow rates [49]. High consistency of lung delivery from Breezhaler® was observed in a pharmacokinetic study by Vaidya et al. [50], which demonstrated lower variability in blood exposure to mometasone furoate following inhalation via Breezhaler® compared with exposure to mometasone furoate via Twisthaler®.
The Breezhaler® inhaler is a low-resistance device that achieves effective dose delivery in the form of a fine particulate fraction (the fraction of particles < 5 µm in diameter—the optimum size for bronchial and alveoli deposition, for a review, see [35]) at low flow rates; this is because with the Breezhaler®, powder ejected from the spinning capsule can undergo multiple collisions with the inhaler walls of the round-shaped rotation chamber, which provides an effective source of dispersion energy through inertial impaction. Colthorpe et al. [51] showed that delivery of a fine particulate fraction of glycopyrronium via Breezhaler® was higher and achieved more consistent intrathoracic deposition, regardless of age or severity of disease in COPD, than tiotropium delivery via Handihaler®. This implies that the Breezhaler® device is ideal for use by patients with a broad range of disease severities [35, 51].
A biophysical model has demonstrated a high level of consistency in lung delivery of the combination of indacaterol/glycopyrronium delivered via Breezhaler® at inspiratory flows between 30 and 90 L/min [49]. Again, this finding provides support for use of the Breezhaler® device by patients across various ages and lung disease severities.
6 Conclusions
Overall, the evaluation of errors in use with the different inhaler devices is challenging to quantify as a result of differences in the definitions of critical and non-critical errors and limitations in our understanding of their use in the real world. Repeated training and counselling on correct inhaler use are essential to optimise clinical effectiveness of inhaled therapy in patients. The relatively low rates of critical errors with Breezhaler® and Aerolizer®, with similarities in the critical errors reported, together with similarities in the usability support the functional similarity between the two devices in both asthma and COPD. The low resistance of the dose-confirming Breezhaler® results in an inspiratory effort that patients over a wide range of ages, disease severities and indications can easily achieve.
References
Haidl P, Heindl S, Siemon K, Bernacka M, Cloes RM. Inhalation device requirements for patients’ inhalation maneuvers. Respir Med. 2016;118:65–75.
Molimard M, Raherison C, Lignot S, Depont F, Abouelfath A, Moore N. Assessment of handling of inhaler devices in real life: an observational study in 3811 patients in primary care. J Aerosol Med. 2003;16:249–54.
Fink JB, Rubin BK. Problems with inhaler use: a call for improved clinician and patient education. Respir Care. 2005;50:1360–74.
Price DB, Roman-Rodriguez M, McQueen RB, Bosnic-Anticevich S, Carter V, Gruffydd-Jones K, et al. Inhaler errors in the CRITIKAL study: type, frequency, and association with asthma outcomes. J Allergy Clin Immunol Pract. 2017;5(1071–81):e9.
Román-Rodríguez M, Metting E, Gacía-Pardo M, Kocks J, van der Molen T. Wrong inhalation technique is associated to poor asthma clinical outcomes. Is there room for improvement? Curr Opin Pulm Med. 2019;25:18–26.
Molimard M, Giorgi-Vigo K. How can we improve patient use of inhaler devices in COPD? Eur Respir J. 2011;38(Suppl. 55):p3978.
Harb HS, Laz NI, Rabea H, Abdelrahim MEA. First-time handling of different inhalers by chronic obstructive lung disease patients. Exp Lung Res. 2020;46:258–691.
Harb HS, Laz NI, Rabea H, Abdelrahim ME. Prevalence and predictors of suboptimal peak inspiratory flow rate in COPD patients. Eur J Pharm Sci. 2020;147:105298.
Laube BL, Janssens HM, de Jongh FHC, Devadason SG, Dhand R, Diot P, et al. What the pulmonary specialist should know about the new inhalation therapies. Eur Respir J. 2011;37:1308–31.
Nicola M, Elberry AA, Sayed OM, Hussein RR, Abdelrahim ME. Effect of DPI’s training-device on inhalation technique and clinical efficacy in asthmatics. Beni Suef Univ J Basic Appl Sci. 2018;7:178–83.
Elgendy MO, Abdelrahim ME, Eldin RS. Potential benefit of repeated dry powder inhaler’s inhalation technique counseling on asthmatic patients. Pulm Ther. 2015;1:91–101.
Kocks JWH, Chrystyn H, van der Palen J, Thomas M, Yates L, Landis SH, et al. Systematic review of association between critical errors in inhalation and health outcomes in asthma and COPD. NPJ Prim Care Respir Med. 2018;28:43.
Molimard M. How to achieve good compliance and adherence with inhalation therapy. Curr Med Res Opin. 2005;21(Suppl. 4):S33–7.
Molimard M, Le Gros V. Impact of patient-related factors on asthma control. J Asthma. 2008;45:109–13.
Lavorini F, Magnan A, Dubus JC, Voshaar T, Corbetta L, Broeders M, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med. 2008;102:593–604.
Schulte M, Osseiran K, Betz R, Wencker M, Brand P, Meyer T, et al. Handling of and preferences for available dry powder inhaler systems by patients with asthma and COPD. J Aerosol Med Pulm Drug Deliv. 2008;21:321–8.
Inhaler Error Steering Committee, Price D, Bosnic-Anticevich S, Briggs A, Chrystyn H, Rand C, et al. Inhaler competence in asthma: common errors, barriers to use and recommended solutions. Respir Med. 2013;107:37–46.
van der Palen J, van der Valk P, Goosens M, Groothuis-Oudshoorn K, Brusse-Keizer M. A randomised cross-over trial investigating the ease of use and preference of two dry powder inhalers in patients with asthma or chronic obstructive pulmonary disease. Expert Opin Drug Deliv. 2013;10:1171–8.
van der Palen J, Thomas M, Chrystyn H, Sharma RK, van der Valk PD, Goosens M, et al. A randomised open-label cross-over study of inhaler errors, preference and time to achieve correct inhaler use in patients with COPD or asthma: comparison of ELLIPTA with other inhaler devices. NPJ Prim Care Respir Med. 2016;26:16079.
Voshaar T, Spinola M, Linnane P, Campanini A, Lock D, Lafratta A, et al. Comparing usability of NEXThaler® with other inhaled corticosteroid/long-acting beta2-agonist fixed combination dry powder inhalers in asthma patients. J Aerosol Med Pulm Drug Deliv. 2014;27:363–70.
Al Ammari M, Sultana K, Yunus F, Al Ghobain M, Al Halwan SM. A cross-sectional observational study to assess inhaler technique in Saudi hospitalized patients with asthma and chronic obstructive pulmonary disease. Saudi Med J. 2016;37:570–4.
Freitas Ferreira E, Pascoal A, Silva P, Lourenço O, Valente S, Valente MJ, et al. Inhaler training and asthma knowledge are associated with a higher proportion of patients with correct inhaler technique in young but not in elderly asthmatic patients. J Asthma. 2020;57:556–66.
Janezic A, Locatelli I, Kos M. Inhalation technique and asthma outcomes with different corticosteroid-containing inhaler devices. J Asthma. 2020;57:654–62.
Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J. 2002;19:246–51.
Usmani OS, Lavorini F, Marshall J, Dunlop WCN, Heron L, Farrington E, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19:10.
van Zyl-Smit RN, Krüll M, Gessner C, Gon Y, Noga O, Richard A, et al. Once-daily mometasone plus indacaterol versus mometasone or twice-daily fluticasone plus salmeterol in patients with inadequately controlled asthma (PALLADIUM): a randomised, duble-blind, triple-dummy, controlled phase 3 study. Lancet Respir Med. 2020;8:987–99. https://doi.org/10.1016/S2213-2600(20)30178-8.
Kerstjens HAM, Maspero J, Chapman KR, van Zyl-Smit RN, Hosoe M, Tanase AM, et al. Once-daily, single-inhaler mometasone-indacaterol-glycopyrronium versus mometasone-indacaterol or twice-daily fluticasone-salmeterol in patients with inadequately controlled asthma (IRIDIUM): a randomised, double-blind, controlled phase 3 study. Lancet Respir Med. 2020;8:1000–2. https://doi.org/10.1016/S2213-2600(20)30190-9.
Price D, Kornmann O, Mucsi J, Kato M, Bandelli L, Sen B, et al. Efficacy and safety of once-daily low-dose indacaterol/mometasone via Breezhaler® in symptomatic adult and adolescent patients with inadequately controlled asthma: phase III randomised QUARTZ study findings. Respir Med. 2020;161:105809. https://doi.org/10.1016/j.rmed.2019.105809.
Dolovich M. New propellant-free technologies under investigation. J Aerosol Med. 1999;12(Suppl. 1):S9-17.
Chapman K, Fogarty CM, Peckitt C, Lassen C, Jadayel D, Dederichs J, et al. Delivery characteristics and patients’ handling of two single-dose dry-powder inhalers used in COPD. Int J COPD. 2011;6:353–63.
Labiris NR, Dolovich MB. Pulmonary drug delivery. Part II: the role of inhalant delivery devices and drug formulation in the therapeutic effectiveness of aerolized medications. Br J Clin Pharmacol. 2003;56:600–12.
Janssens W, Van den Brande P, Hardeman E, De Langhe E, Philps T, Troosters T, et al. Inspiratory flow rates at different levels of resistance in elderly COPD patients. Eur Respir J. 2008;31:78–83.
Al-Showair RA, Tarsin WY, Assi KH, Pearson SB, Chrystyn H. Can all patients with COPD use the correct inhalation flow with all inhalers and does training help? Respir Med. 2007;101:2395–401.
Altman P, Wehbe L, Dederichs J, Guerin T, Ament B, Moronta MC, et al. Comparison of peak inspiratory flow rate via the Breezhaler®, Ellipta® and HandiHaler® dry powder inhalers in patients with moderate to very severe COPD: a randomized cross-over trial. BMC Pulm Med. 2018;18:100.
Molimard M, D’Andrea P. Once-daily glycopyrronium via the Breezhaler® device for the treatment of COPD: pharmacological and clinical profile. Expert Rev Clin Pharmacol. 2013;6:503–17.
Pavkov R, Mueller S, Fiebich K, Singh D, Stowasser F, Pignatelli G, et al. Characteristics of a capsule based dry powder inhaler for the delivery of indacaterol. Curr Med Res Opin. 2010;26:2527–33.
Tarsin W, Assi KH, Chrystyn H. In-vitro intra- and inter-inhaler flow rate-dependent dosage emission from a combination of budesonide and eformoterol in a dry powder inhaler. J Aerosol Med. 2004;17:25–32.
Chodosh S, Flanders JS, Kesten S, Serby CW, Hochrainer D, Witek TJ Jr. Effective delivery of particles with the HandiHaler dry powder inhalation system over a range of chronic obstructive pulmonary disease severity. J Aerosol Med. 2001;14:309–15.
Van Der Palen J, Eijsvogel MM, Kuipers BF, Schipper M, Vermue NA. Comparison of the Diskus inhaler and the Handihaler regarding preference and ease of use. J Aerosol Med. 2007;20:38–44.
Boshra MS, Almeldien AG, Eldin RS, Elberry AA, Abdelwahab NS, Salem MN, et al. Inhaled salbutamol from aerolizer and diskus at different inhalation flows, inhalation volume and number of inhalations in both healthy subjects and COPD patients. Exp Lung Res. 2019;45:84–91.
Boshra MS, Almeldien AG, Salah Eldin R, Elberry AA, Abdelwahab NS, Nabil Salem M, et al. Total emitted dose of salbutamol sulphate at different inhalation flows and inhalation volumes through different types of dry powder inhalers. Exp Lung Res. 2018;44:211–6.
Ocakli B, Ozmen I, Tuncay EA, Gungor S, Altinoz H, Adiguzel N, et al. A comparative analysis of errors in inhaler technique among COPD versus asthma patients. Int J Chron Obstruct Pulmon Dis. 2018;13:2941–7.
Takaku Y, Kurashima K, Ohta C, Ishiguro T, Kagiyama N, Yanagisawa T, et al. How many instructions are required to correct inhalation errors in patients with asthma and chronic obstructive pulmonary disease? Respir Med. 2017;123:110–5.
Girodet PO, Raherison C, Abouelfath A, Lignot S, Depont F, Moore N, et al. Real-life use of inhaler devices for chronic obstructive pulmonary disease in primary care. Therapie. 2003;58:499–504.
Molimard M, Raherison C, Lignot S, Balestra A, Lamarque S, Chartier A, et al. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: real-life assessment of 2935 patients. Eur Respir J. 2017;49:1601794. https://doi.org/10.1183/13993003.01794-2016.
Eliraz A, Ramirez-Rivera A, Ferranti P, Holzer R, García JM, Turcotte C, et al. Similar efficacy following four weeks treatment of asthmatics with formoterol 12 micrograms b.d. delivered by two different dry powder inhalers: differences in inhaler handling. Int J Clin Pract. 2001;55:164–70.
Molimard M, Till D, Stenglein S, Singh D, Krummen M. Inhalation devices for long-acting beta2-agonists: efficiency and ease of use of dry powder formoterol inhalers for use by patients with asthma and COPD. Curr Med Res Opin. 2007;23:2405–13.
Ung KT, Chan HK. Effects of ramp-up of inspired airflow on in vitro aerosol dose delivery performance for certain dry powder inhalers. Eur J Pharm Sci. 2016;84:46–54.
Dolovich MB, Kuttler A, Dimke TJ, Usmani OS. Biophysical model to predict lung delivery from a dual bronchodilator dry-powder inhaler. Int J Pharm X. 2019;1:100018.
Vaidya S, Khindri S, Robinson J, Smith T, Magnusson B, Kaiser G, et al. Pharmacokinetics (PK) of single doses of mometasone furoate (MF) delivered via the Breezhaler® (BH) and Twisthaler® (TH) devices in healthy subjects. Eur Respir J. 2012;40:P2145.
Colthorpe P, Voshaar T, Kieckbusch T, Cuoghi E, Jauernig J. Delivery characteristics of a low-resistance dry-powder inhaler used to deliver the long-acting muscarinic antagonist glycopyrronium. J Drug Assess. 2013;2:11–6.
Acknowledgements
Medical writing and editorial support for this manuscript was provided by Ian Wright of Novartis Ireland Ltd, funded by Novartis Pharma AG (Basel, Switzerland) in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This review was supported by Novartis Pharma AG, Basel, Switzerland.
Conflict of interest
Mathieu Molimard is a full-time employee at the University of Bordeaux and the University Hospital of Bordeaux; he has also received fees for consultancy and participation in advisory boards for GSK, Novartis Pharma and Boehringer Ingelheim. Ioannis Kottakis, Juergen Jauernig, Sonja Lederhilger and Ivan Nikolaev are full-time employees with Novartis Pharma AG, Basel, Switzerland.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
MM: conceptualisation, reviewing, editing and visualisation. IK: conceptualisation, reviewing and editing. JJ: conceptualisation, reviewing and editing. SL: conceptualisation, reviewing and editing. IN: conceptualisation, original draft preparation, reviewing, editing and visualisation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Molimard, M., Kottakis, I., Jauernig, J. et al. Performance Characteristics of Breezhaler® and Aerolizer® in the Real-World Setting. Clin Drug Investig 41, 415–424 (2021). https://doi.org/10.1007/s40261-021-01021-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-021-01021-w