Abstract
Extracellular vesicles (EVs) are a promising drug delivery vehicle candidate because of their natural origin and intrinsic function of transporting various molecules between different cells. Several advantages of the EV delivery platform include enhanced permeability and retention effect, efficient interaction with recipient cells, the ability to traverse biological barriers, high biocompatibility, high biodegradability, and low immunogenicity. Furthermore, EV membranes share approximately similar structures and contents to the cell membrane, which allows surface modification of EVs, an approach to enable specific targeting. Enhanced drug accumulation in intended sites and reduced adverse effects of chemotherapeutic drugs are the most prominent effects of targeted drug delivery. In order to improve the targeting ability of EVs, chemical modification and genetic engineering are the most adopted methods to date. Diverse chemical methods are employed to decorate EV surfaces with various ligands such as aptamers, carbohydrates, peptides, vitamins, and antibodies. In this review, we introduce the biogenesis, content, and cellular pathway of natural EVs and further discuss the genetic modification of EVs, and its challenges. Furthermore, we provide a comprehensive deliberation on the various chemical modification methods for improved drug delivery, which are directly related to increasing the therapeutic index.
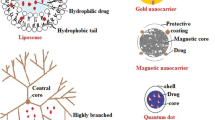
Graphical Abstract




Similar content being viewed by others
References
Kesharwani P, Taurin S, Greish K, editors. Theory and applications of nonparenteral nanomedicines. Amsterdam: Elsevier; 2020.
Wang Q, et al. Delivery of therapeutic agents by nanoparticles made of grapefruit-derived lipids. Nat Commun. 2013;4(1):1–13. https://doi.org/10.1038/ncomms2886.
Gupta AK, Gupta M. Synthesis and surface engineering of iron oxide nanoparticles for biomedical applications. Biomaterials. 2005;26(18):3995–4021. https://doi.org/10.1016/j.biomaterials.2004.10.012.
Liu F, et al. Towards site-specific nanoparticles for drug delivery application: preparation, characterization and release performance. Chem Pap. 2017;71(12):2385–94. https://doi.org/10.1007/s11696-017-0233-5.
He X, et al. A novel peptide probe for imaging and targeted delivery of liposomal doxorubicin to lung tumor. Mol Pharm. 2011;8(2):430–8. https://doi.org/10.1021/mp100266g.
Mitchell MJ, et al. Engineering precision nanoparticles for drug delivery. Nat Rev Drug Discovery. 2021;20(2):101–24. https://doi.org/10.1038/s41573-020-0090-8.
Andriyanov AV, et al. Therapeutic efficacy of combined PEGylated liposomal doxorubicin and radiofrequency ablation: comparing single and combined therapy in young and old mice. J Control Release. 2017;257:2–9. https://doi.org/10.1016/j.jconrel.2017.02.018.
Maier MA, et al. Biodegradable lipids enabling rapidly eliminated lipid nanoparticles for systemic delivery of RNAi therapeutics. Mol Ther. 2013;21(8):1570–8. https://doi.org/10.1038/mt.2013.124.
Torchilin VP. Recent advances with liposomes as pharmaceutical carriers. Nat Rev Drug Discovery. 2005;4(2):145–60. https://doi.org/10.1038/nrd1632.
Dolatabadi JEN, Omidi Y. Solid lipid-based nanocarriers as efficient targeted drug and gene delivery systems. TrAC Trends Anal Chem. 2016;77:100–8. https://doi.org/10.1016/j.trac.2015.12.016.
Fenton OS, et al. Advances in biomaterials for drug delivery. Adv Mater. 2018;30(29):1705328. https://doi.org/10.1002/adma.201705328.
Gomes-da-Silva LC, et al. Lipid-based nanoparticles for siRNA delivery in cancer therapy: paradigms and challenges. Acc Chem Res. 2012;45(7):1163–71. https://doi.org/10.1021/ar300048p.
Pardridge WM. Transport of small molecules through the blood-brain barrier: biology and methodology. Adv Drug Deliv Rev. 1995;15(1–3):5–36. https://doi.org/10.1016/0169-409X(95)00003-P.
Kim MS, et al. Development of exosome-encapsulated paclitaxel to overcome MDR in cancer cells. Nanomed Nanotechnol Biol Med. 2016;12(3):655–64. https://doi.org/10.1016/j.nano.2015.10.012.
Kim WJ, Kim SW. Efficient siRNA delivery with non-viral polymeric vehicles. Pharm Res. 2009;26(3):657–66. https://doi.org/10.1007/s11095-008-9774-1.
Simons M, Raposo G. Exosomes–vesicular carriers for intercellular communication. Curr Opin Cell Biol. 2009;21(4):575–81. https://doi.org/10.1007/s00441-012-1428-2.
Wei H, et al. A nanodrug consisting of doxorubicin and exosome derived from mesenchymal stem cells for osteosarcoma treatment in vitro. Int J Nanomed. 2019;14:8603. https://doi.org/10.2147/IJN.S218988.
Sedykh SE, et al. Milk exosomes: isolation, biochemistry, morphology, and perspectives of use. Extracell Vesicles Import Hum Health. 2020. https://doi.org/10.5772/intechopen.85416.
Wu M, et al. Isolation of exosomes from whole blood by integrating acoustics and microfluidics. Proc Natl Acad Sci. 2017;114(40):10584–9. https://doi.org/10.1073/pnas.1709210114.
He L, et al. A highly efficient method for isolating urinary exosomes. Int J Mol Med. 2019;43(1):83–90. https://doi.org/10.3892/ijmm.2018.3944.
Bai R, et al. Induction of immune-related gene expression by seminal exosomes in the porcine endometrium. Biochem Biophys Res Commun. 2018;495(1):1094–101. https://doi.org/10.1016/J.BBRC.2017.11.100.
Zlotogorski-Hurvitz A, et al. Human saliva-derived exosomes: comparing methods of isolation. J Histochem Cytochem. 2015;63(3):181–9. https://doi.org/10.1369/0022155414564219.
Asea A, et al. Heat shock protein-containing exosomes in mid-trimester amniotic fluids. J Reprod Immunol. 2008;79(1):12–7. https://doi.org/10.1016/j.jri.2008.06.001.
Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200(4):373–83. https://doi.org/10.1083/jcb.201211138.
Théry C, et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7(1):1535750. https://doi.org/10.1080/20013078.2018.1535750.
Johnstone R. Maturation of reticulocytes: formation of exosomes as a mechanism for shedding membrane proteins. Biochem Cell Biol. 1992;70(3–4):179–90. https://doi.org/10.1139/o92-028.
Mathivanan S, Simpson RJ. ExoCarta: A compendium of exosomal proteins and RNA. Proteomics. 2009;9(21):4997–5000. https://doi.org/10.1002/pmic.200900351.
Valadi H, et al. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9(6):654–9. https://doi.org/10.1038/ncb1596.
Llorente A, et al. Molecular lipidomics of exosomes released by PC-3 prostate cancer cells. Biochimica et Biophysica Acta (BBA)-Molecular and Cell Biology of Lipids. 2013;1831(7):1302–9. https://doi.org/10.1016/j.bbalip.2013.04.011.
Blanco E, Shen H, Ferrari M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat Biotechnol. 2015;33(9):941–51. https://doi.org/10.1038/nbt.3330.
Lu M, et al. Comparison of exosome-mimicking liposomes with conventional liposomes for intracellular delivery of siRNA. Int J Pharm. 2018;550(1–2):100–13. https://doi.org/10.1016/j.ijpharm.2018.08.040.
Haney MJ, et al. Exosomes as drug delivery vehicles for Parkinson’s disease therapy. J Control Release. 2015;207:18–30. https://doi.org/10.1016/j.jconrel.2015.03.033.
El-Andaloussi S, et al. Exosome-mediated delivery of siRNA in vitro and in vivo. Nat Protoc. 2012;7(12):2112–26. https://doi.org/10.1038/nprot.2012.131.
Sun D, et al. A novel nanoparticle drug delivery system: the anti-inflammatory activity of curcumin is enhanced when encapsulated in exosomes. Mol Ther. 2010;18(9):1606–14. https://doi.org/10.1038/mt.2010.105.
Somiya M, Yoshioka Y, Ochiya T. Biocompatibility of highly purified bovine milk-derived extracellular vesicles. J Extracell Vesicles. 2018;7(1):1440132. https://doi.org/10.1080/20013078.2018.1440132.
Kumar S, et al. Cloaked exosomes: biocompatible, durable, and degradable encapsulation. Small. 2018;14(34):1802052. https://doi.org/10.1002/smll.201802052.
Lv L-H, et al. Anticancer drugs cause release of exosomes with heat shock proteins from human hepatocellular carcinoma cells that elicit effective natural killer cell antitumor responses in vitro. J Biol Chem. 2012;287(19):15874–85. https://doi.org/10.1074/jbc.M112.340588.
Shyong Y-J, Chang K-C, Lin F-H. Calcium phosphate particles stimulate exosome secretion from phagocytes for the enhancement of drug delivery. Colloids Surf B. 2018;171:391–7. https://doi.org/10.1016/j.colsurfb.2018.07.037.
Panigrahi GK, et al. Hypoxia-induced exosome secretion promotes survival of African-American and Caucasian prostate cancer cells. Sci Rep. 2018;8(1):1–13. https://doi.org/10.1038/s41598-018-22068-4.
Chinnappan M, et al. Exosomes as drug delivery vehicle and contributor of resistance to anticancer drugs. Cancer Lett. 2020;486:18–28. https://doi.org/10.1016/j.canlet.2020.05.004.
Lai CP, et al. Dynamic biodistribution of extracellular vesicles in vivo using a multimodal imaging reporter. ACS Nano. 2014;8(1):483–94. https://doi.org/10.1021/nn404945r.
Wiklander OP, et al. Extracellular vesicle in vivo biodistribution is determined by cell source, route of administration and targeting. J Extracell Vesicles. 2015;4(1):26316. https://doi.org/10.3402/jev.v4.26316.
Das CK, et al. Exosome as a novel shuttle for delivery of therapeutics across biological barriers. Mol Pharm. 2018;16(1):24–40. https://doi.org/10.1021/acs.molpharmaceut.8b00901.
Gilligan KE, Dwyer RM. Engineering exosomes for cancer therapy. Int J Mol Sci. 2017;18(6):1122. https://doi.org/10.3390/ijms18061122.
Tian T, et al. Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials. 2018;150:137–49.
Pan B-T, Johnstone RM. Fate of the transferrin receptor during maturation of sheep reticulocytes in vitro: selective externalization of the receptor. Cell. 1983;33(3):967–78. https://doi.org/10.1016/0092-8674(83)90040-5.
Harding C, Stahl P. Transferrin recycling in reticulocytes: pH and iron are important determinants of ligand binding and processing. Biochem Biophys Res Commun. 1983;113(2):650–8. https://doi.org/10.1016/0006-291X(83)91776-X.
Johnstone RM, et al. Vesicle formation during reticulocyte maturation. Association of plasma membrane activities with released vesicles (exosomes). J Biol Chem. 1987;262(19):9412–20. https://doi.org/10.1016/S0021-9258(18)48095-7.
Pan B-T, et al. Electron microscopic evidence for externalization of the transferrin receptor in vesicular form in sheep reticulocytes. J Cell Biol. 1985;101(3):942–8. https://doi.org/10.1083/jcb.101.3.942.
Johnstone R, et al. Exosome formation during maturation of mammalian and avian reticulocytes: evidence that exosome release is a major route for externalization of obsolete membrane proteins. J Cell Physiol. 1991;147(1):27–36. https://doi.org/10.1002/jcp.1041470105.
Raposo G, et al. B lymphocytes secrete antigen-presenting vesicles. J Exp Med. 1996;183(3):1161–72. https://doi.org/10.1084/jem.183.3.1161.
Zitvogel L, et al. Eradication of established murine tumors using a novel cell-free vaccine: dendritic cell derived exosomes. Nat Med. 1998;4(5):594–600. https://doi.org/10.1038/nm0598-594.
Crawford N. The presence of contractile proteins in platelet microparticles isolated from human and animal platelet-free plasma. Br J Haematol. 1971;21(1):53–69. https://doi.org/10.1111/j.1365-2141.1971.tb03416.x.
Fourcade O, et al. Secretory phospholipase A2 generates the novel lipid mediator lysophosphatidic acid in membrane microvesicles shed from activated cells. Cell. 1995;80(6):919–27. https://doi.org/10.1016/0092-8674(95)90295-3.
Théry C, et al. Proteomic analysis of dendritic cell-derived exosomes: a secreted subcellular compartment distinct from apoptotic vesicles. J Immunol. 2001;166(12):7309–18. https://doi.org/10.4049/jimmunol.166.12.7309.
Gawrisch K, et al. The rate of lateral diffusion of phospholipids in erythrocyte microvesicles. Biochimica et Biophysica Acta (BBA)-Biomembranes. 1986;856(3):443–7. https://doi.org/10.1016/0005-2736(86)90135-5.
Subra C, et al. Exosome lipidomics unravels lipid sorting at the level of multivesicular bodies. Biochimie. 2007;89(2):205–12. https://doi.org/10.1016/j.biochi.2006.10.014.
Ratajczak J, et al. Embryonic stem cell-derived microvesicles reprogram hematopoietic progenitors: evidence for horizontal transfer of mRNA and protein delivery. Leukemia. 2006;20(5):847–56. https://doi.org/10.1038/sj.leu.2404132.
Skog J, et al. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat Cell Biol. 2008;10(12):1470–6. https://doi.org/10.1038/ncb1800.
Luo X, et al. High-performance chemical isotope labeling liquid chromatography mass spectrometry for exosome metabolomics. Anal Chem. 2018;90(14):8314–9. https://doi.org/10.1021/acs.analchem.8b01726.
Van Niel G, et al. Exosomes: a common pathway for a specialized function. J Biochem. 2006;140(1):13–21. https://doi.org/10.1093/jb/mvj128.
Caponnetto F, et al. The miRNA content of exosomes released from the glioma microenvironment can affect malignant progression. Biomedicines. 2020;8(12):564. https://doi.org/10.3390/biomedicines8120564.
Trajkovic K, et al. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science. 2008;319(5867):1244–7. https://doi.org/10.1126/science.1153124.
Wei X, et al. Surface phosphatidylserine is responsible for the internalization on microvesicles derived from hypoxia-induced human bone marrow mesenchymal stem cells into human endothelial cells. PLoS ONE. 2016;11(1): e0147360. https://doi.org/10.1371/journal.pone.0147360.
Sobo-Vujanovic A, Munich S, Vujanovic NL. Dendritic-cell exosomes cross-present Toll-like receptor-ligands and activate bystander dendritic cells. Cell Immunol. 2014;289(1–2):119–27. https://doi.org/10.1016/j.cellimm.2014.03.016.
Montecalvo A, et al. Mechanism of transfer of functional microRNAs between mouse dendritic cells via exosomes. Blood J Am Soc Hematol. 2012;119(3):756–66. https://doi.org/10.1182/blood-2011-02-338004.
Escrevente C, et al. Interaction and uptake of exosomes by ovarian cancer cells. BMC Cancer. 2011;11(1):1–10. https://doi.org/10.1186/1471-2407-11-108.
Eguchi S, et al. Cardiomyocytes capture stem cell-derived, anti-apoptotic microRNA-214 via clathrin-mediated endocytosis in acute myocardial infarction. J Biol Chem. 2019;294(31):11665–74. https://doi.org/10.3390/cells11223664.
Delenclos M, et al. Investigation of endocytic pathways for the internalization of exosome-associated oligomeric alpha-synuclein. Front Neurosci. 2017;11:172. https://doi.org/10.3389/fnins.2017.00172.
Nanbo A, et al. Exosomes derived from Epstein-Barr virus-infected cells are internalized via caveola-dependent endocytosis and promote phenotypic modulation in target cells. J Virol. 2013;87(18):10334–47. https://doi.org/10.1128/JVI.01310-13.
Feng D, et al. Cellular internalization of exosomes occurs through phagocytosis. Traffic. 2010;11(5):675–87. https://doi.org/10.1111/j.1600-0854.2010.01041.x.
Kamerkar S, et al. Exosomes facilitate therapeutic targeting of oncogenic KRAS in pancreatic cancer. Nature. 2017;546(7659):498–503. https://doi.org/10.1038/nature22341.
Komuro H, et al. Engineering extracellular vesicles to target pancreatic tissue in vivo. Nanotheranostics. 2021;5(4):378. https://doi.org/10.7150/ntno.54879.
Li S, et al. Engineering macrophage-derived exosomes for targeted chemotherapy of triple-negative breast cancer. Nanoscale. 2020;12(19):10854–62. https://doi.org/10.1016/j.nano.2017.09.011.
Alvarez-Erviti L, et al. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29(4):341–5. https://doi.org/10.1038/nbt.1807.
Ohno S-I, et al. Systemically injected exosomes targeted to EGFR deliver antitumor microRNA to breast cancer cells. Mol Ther. 2013;21(1):185–91. https://doi.org/10.1038/mt.2012.180.
Longatti A, et al. High affinity single-chain variable fragments are specific and versatile targeting motifs for extracellular vesicles. Nanoscale. 2018;10(29):14230–44. https://doi.org/10.1039/C8NR03970D.
Liang G, et al. Engineered exosome-mediated delivery of functionally active miR-26a and its enhanced suppression effect in HepG2 cells. Int J Nanomed. 2018;13:585. https://doi.org/10.2147/IJN.S154458.
Cheng Q, et al. Expanding the toolbox of exosome-based modulators of cell functions. Biomaterials. 2021;277: 121129. https://doi.org/10.1016/j.biomaterials.2021.121129.
Tian Y, et al. A doxorubicin delivery platform using engineered natural membrane vesicle exosomes for targeted tumor therapy. Biomaterials. 2014;35(7):2383–90. https://doi.org/10.1016/j.biomaterials.2013.11.083.
Bai J, et al. Engineered targeting tLyp-1 exosomes as gene therapy vectors for efficient delivery of siRNA into lung cancer cells. Asian J Pharm Sci. 2020;15(4):461–71. https://doi.org/10.1016/j.ajps.2019.04.002.
Yu Y, et al. Genetically engineered exosomes display RVG peptide and selectively enrich a neprilysin variant: a potential formulation for the treatment of Alzheimer’s disease. J Drug Target. 2021;29(10):1128–38. https://doi.org/10.1080/1061186X.2021.1929257.
Tomanin R, Scarpa M. Why do we need new gene therapy viral vectors? Characteristics, limitations and future perspectives of viral vector transduction. Curr Gene Ther. 2004;4(4):357–72. https://doi.org/10.2174/1566523043346011.
Gomari H, Moghadam MF, Soleimani M. Targeted cancer therapy using engineered exosome as a natural drug delivery vehicle. Onco Targets Ther. 2018;11:5753. https://doi.org/10.2147/OTT.S173110.
Jang SC, et al. Bioinspired exosome-mimetic nanovesicles for targeted delivery of chemotherapeutics to malignant tumors. ACS Nano. 2013;7(9):7698–710. https://doi.org/10.1021/nn402232g.
Jo W, et al. Large-scale generation of cell-derived nanovesicles. Nanoscale. 2014;6(20):12056–64. https://doi.org/10.1039/C4NR02391A.
Severic M, et al. Genetically-engineered anti-PSMA exosome mimetics targeting advanced prostate cancer in vitro and in vivo. J Control Release. 2021;330:101–10. https://doi.org/10.1016/j.jconrel.2020.12.017.
Wang C, et al. Engineering a HEK-293T exosome-based delivery platform for efficient tumor-targeting chemotherapy/internal irradiation combination therapy. J Nanobiotechnol. 2022;20(1):247. https://doi.org/10.1186/s12951-022-01462-1.
Mentkowski KI, Lang JK. Exosomes engineered to express a cardiomyocyte binding peptide demonstrate improved cardiac retention in vivo. Sci Rep. 2019;9(1):1–13. https://doi.org/10.1038/s41598-019-46407-1.
Liang G, et al. Engineered exosomes for targeted co-delivery of miR-21 inhibitor and chemotherapeutics to reverse drug resistance in colon cancer. J Nanobiotechnol. 2020;18(1):1–15. https://doi.org/10.1186/s12951-019-0563-2.
Liang Y, et al. Chondrocyte-targeted microRNA delivery by engineered exosomes toward a cell-free osteoarthritis therapy. ACS Appl Mater Interfaces. 2020;12(33):36938–47. https://doi.org/10.1021/acsami.0c10458.
Cheng Q, et al. Reprogramming exosomes as nanoscale controllers of cellular immunity. J Am Chem Soc. 2018;140(48):16413–7. https://doi.org/10.1021/jacs.8b10047.
Bose RJ, et al. Engineered cell-derived vesicles displaying targeting peptide and functionalized with nanocarriers for therapeutic microRNA delivery to triple-negative breast cancer in mice. Adv Healthcare Mater. 2022;11(5):2101387. https://doi.org/10.1002/adhm.202270026.
Komuro H, et al. Design and evaluation of engineered extracellular vesicle (EV)-based targeting for EGFR-overexpressing tumor cells using monobody display. Bioengineering. 2022;9(2):56. https://doi.org/10.3390/bioengineering9020056.
Mai J, et al. αvβ3-targeted sEVs for efficient intracellular delivery of proteins using MFG-E8. BMC Biotechnol. 2022;22(1):1–10. https://doi.org/10.1186/s12896-022-00745-7.
Limoni SK, et al. Engineered exosomes for targeted transfer of siRNA to HER2 positive breast cancer cells. Appl Biochem Biotechnol. 2019;187(1):352–64. https://doi.org/10.1007/s12010-018-2813-4.
Bellavia D, et al. Interleukin 3-receptor targeted exosomes inhibit in vitro and in vivo Chronic Myelogenous Leukemia cell growth. Theranostics. 2017;7(5):1333. https://doi.org/10.7150/thno.17092.
Mahati S, et al. Delivery of miR-26a using an exosomes-based nanosystem inhibited proliferation of hepatocellular carcinoma. Front Mol Biosci. 2021. https://doi.org/10.3389/fmolb.2021.738219.
Kim G, et al. Engineering exosomes for pulmonary delivery of peptides and drugs to inflammatory lung cells by inhalation. J Control Release. 2021;330:684–95. https://doi.org/10.1016/j.jconrel.2020.12.053.
Huang L, et al. Engineered exosomes as an in situ DC-primed vaccine to boost antitumor immunity in breast cancer. Mol Cancer. 2022;21(1):1–19. https://doi.org/10.1186/s12943-022-01515-x.
Zhai Y, et al. High-efficiency brain-targeted intranasal delivery of BDNF mediated by engineered exosomes to promote remyelination. Biomater Sci. 2022;10(19):5707–18. https://doi.org/10.1039/d2bm00518b.
Gečys D, et al. Internalisation of RGD-engineered extracellular vesicles by glioblastoma cells. Biology. 2022;11(10):1483. https://doi.org/10.3390/biology11101483.
Kooijmans SA, et al. Modulation of tissue tropism and biological activity of exosomes and other extracellular vesicles: new nanotools for cancer treatment. Pharmacol Res. 2016;111:487–500. https://doi.org/10.1016/j.phrs.2016.07.006.
Smyth T, et al. Surface functionalization of exosomes using click chemistry. Bioconjug Chem. 2014;25(10):1777–84. https://doi.org/10.1021/bc500291r.
Komuro H, et al. Advances of engineered extracellular vesicles-based therapeutics strategy. Sci Technol Adv Mater. 2022. https://doi.org/10.1080/14686996.2022.2133342.
Song S, et al. In situ one-step fluorescence labeling strategy of exosomes via bioorthogonal click chemistry for real-time exosome tracking in vitro and in vivo. Bioconjug Chem. 2020;31(5):1562–74. https://doi.org/10.1021/acs.bioconjchem.0c00216.
Armstrong JP, Holme MN, Stevens MM. Re-engineering extracellular vesicles as smart nanoscale therapeutics. ACS Nano. 2017;11(1):69–83. https://doi.org/10.1021/acsnano.6b07607.
Fan Y, et al. Responsive dual-targeting exosome as a drug carrier for combination cancer immunotherapy. Research. 2021. https://doi.org/10.34133/2021/9862876.
Kooijmans SA, et al. Recombinant phosphatidylserine-binding nanobodies for targeting of extracellular vesicles to tumor cells: a plug-and-play approach. Nanoscale. 2018;10(5):2413–26. https://doi.org/10.1039/c7nr06966a.
Si Y, et al. Targeted exosomes for drug delivery: biomanufacturing, surface tagging, and validation. Biotechnol J. 2020;15(1):1900163. https://doi.org/10.1002/biot.201900163.
Kooijmans S, et al. PEGylated and targeted extracellular vesicles display enhanced cell specificity and circulation time. J Control Release. 2016;224:77–85. https://doi.org/10.1016/j.jconrel.2016.01.009.
Guo L, et al. Surface-modified engineered exosomes attenuated cerebral ischemia/reperfusion injury by targeting the delivery of quercetin towards impaired neurons. J Nanobiotechnol. 2021;19(1):1–15. https://doi.org/10.1186/s12951-021-00879-4.
Ye Z, et al. Methotrexate-loaded extracellular vesicles functionalized with therapeutic and targeted peptides for the treatment of glioblastoma multiforme. ACS Appl Mater Interfaces. 2018;10(15):12341–50. https://doi.org/10.1021/acsami.7b18135.
Zhu Q, et al. Embryonic stem cells-derived exosomes endowed with targeting properties as chemotherapeutics delivery vehicles for glioblastoma therapy. Adv Sci. 2019;6(6):1801899. https://doi.org/10.1002/advs.201801899.
Huang X, et al. Engineered exosome as targeted lncRNA MEG3 delivery vehicles for osteosarcoma therapy. J Control Release. 2022;343:107–17. https://doi.org/10.1016/j.jconrel.2022.01.026.
Cao Y, et al. Engineered exosome-mediated near-infrared-II region V2C quantum dot delivery for nucleus-target low-temperature photothermal therapy. ACS Nano. 2019;13(2):1499–510. https://doi.org/10.1021/acsnano.8b07224.
Vandergriff A, et al. Targeting regenerative exosomes to myocardial infarction using cardiac homing peptide. Theranostics. 2018;8(7):1869. https://doi.org/10.7150/thno.20524.
Cheng H, et al. Chimeric peptide engineered exosomes for dual-stage light guided plasma membrane and nucleus targeted photodynamic therapy. Biomaterials. 2019;211:14–24. https://doi.org/10.1016/j.biomaterials.2019.05.004.
Cui G-H, et al. RVG-modified exosomes derived from mesenchymal stem cells rescue memory deficits by regulating inflammatory responses in a mouse model of Alzheimer’s disease. Immunity Ageing. 2019;16(1):1–12. https://doi.org/10.1186/s12979-019-0150-2.
Cui Y, et al. A bone-targeted engineered exosome platform delivering siRNA to treat osteoporosis. Bioactive Mater. 2022;10:207–21. https://doi.org/10.1016/j.bioactmat.2021.09.015.
Tian T, et al. Targeted delivery of neural progenitor cell-derived extracellular vesicles for anti-inflammation after cerebral ischemia. Theranostics. 2021;11(13):6507. https://doi.org/10.7150/thno.56367.
Liang S, Xu H, Ye B-C. Membrane-decorated exosomes for combination drug delivery and improved glioma therapy. Langmuir. 2021;38(1):299–308. https://doi.org/10.1021/acs.langmuir.1c02500.
Kanada M, et al. A dual-reporter platform for screening tumor-targeted extracellular vesicles. Pharmaceutics. 2022;14(3):475. https://doi.org/10.3390/pharmaceutics14030475.
Rong Y, et al. Engineered extracellular vesicles for delivery of siRNA promoting targeted repair of traumatic spinal cord injury. Bioactive Mater. 2023;23:328–42. https://doi.org/10.1016/j.bioactmat.2022.11.011.
Pullan J, et al. Modified bovine milk exosomes for doxorubicin delivery to triple-negative breast cancer cells. ACS Appl Bio Mater. 2022;5(5):2163–75. https://doi.org/10.1021/acsabm.2c00015.
Li D, et al. Hyaluronan decoration of milk exosomes directs tumor-specific delivery of doxorubicin. Carbohydr Res. 2020;493: 108032. https://doi.org/10.1016/j.carres.2020.108032.
Liu J, et al. Functional extracellular vesicles engineered with lipid-grafted hyaluronic acid effectively reverse cancer drug resistance. Biomaterials. 2019;223: 119475. https://doi.org/10.1016/j.biomaterials.2019.119475.
Choi ES, et al. Mannose-modified serum exosomes for the elevated uptake to murine dendritic cells and lymphatic accumulation. Macromol Biosci. 2019;19(7):1900042. https://doi.org/10.1002/mabi.201900042.
Yang X, et al. Eradicating intracellular MRSA via targeted delivery of lysostaphin and vancomycin with mannose-modified exosomes. J Control Release. 2021;329:454–67. https://doi.org/10.1016/j.jconrel.2020.11.045.
Tamura R, Uemoto S, Tabata Y. Augmented liver targeting of exosomes by surface modification with cationized pullulan. Acta Biomater. 2017;57:274–84. https://doi.org/10.1016/j.actbio.2017.05.013.
Zou J, et al. Aptamer-functionalized exosomes: elucidating the cellular uptake mechanism and the potential for cancer-targeted chemotherapy. Anal Chem. 2019;91(3):2425–30. https://doi.org/10.1021/acs.analchem.8b05204.
Pi F, et al. Nanoparticle orientation to control RNA loading and ligand display on extracellular vesicles for cancer regression. Nat Nanotechnol. 2018;13(1):82–9. https://doi.org/10.1038/s41565-017-0012-z.
Tran PH, et al. Aspirin-loaded nanoexosomes as cancer therapeutics. Int J Pharm. 2019;572: 118786. https://doi.org/10.1016/j.ijpharm.2019.118786.
Luo C, et al. Biomimetic carriers based on giant membrane vesicles for targeted drug delivery and photodynamic/photothermal synergistic therapy. ACS Appl Mater Interfaces. 2019;11(47):43811–9. https://doi.org/10.1021/acsami.9b11223.
Wang Y, et al. Nucleolin-targeted extracellular vesicles as a versatile platform for biologics delivery to breast cancer. Theranostics. 2017;7(5):1360. https://doi.org/10.7150/thno.16532.
Bagheri E, et al. Targeted doxorubicin-loaded mesenchymal stem cells-derived exosomes as a versatile platform for fighting against colorectal cancer. Life Sci. 2020;261: 118369. https://doi.org/10.1016/j.lfs.2020.118369.
Li Z, et al. Non-small-cell lung cancer regression by siRNA delivered through exosomes that display EGFR RNA aptamer. Nucleic Acid Therap. 2021;31(5):364–74. https://doi.org/10.1089/nat.2021.0002.
Shamili FH, et al. Immunomodulatory properties of MSC-derived exosomes armed with high affinity aptamer toward mylein as a platform for reducing multiple sclerosis clinical score. J Control Release. 2019;299:149–64. https://doi.org/10.1016/j.jconrel.2019.02.032.
Huang H, et al. Edible and cation-free kiwi fruit derived vesicles mediated EGFR-targeted siRNA delivery to inhibit multidrug resistant lung cancer. J Nanobiotechnol. 2023;21(1):1–14. https://doi.org/10.1186/s12951-023-01766-w.
Zheng Z, et al. Folate-displaying exosome mediated cytosolic delivery of siRNA avoiding endosome trapping. J Control Release. 2019;311:43–9. https://doi.org/10.1016/j.jconrel.2019.08.021.
Yu M, et al. Targeted exosome-encapsulated erastin induced ferroptosis in triple negative breast cancer cells. Cancer Sci. 2019;110(10):3173–82. https://doi.org/10.1111/cas.14181.
Nguyen Cao TG, et al. Safe and targeted sonodynamic cancer therapy using biocompatible exosome-based nanosonosensitizers. ACS Appl Mater Interfaces. 2021;13(22):25575–88. https://doi.org/10.1021/acsami.0c22883.
Aqil F, et al. Milk exosomes-natural nanoparticles for siRNA delivery. Cancer Lett. 2019;449:186–95. https://doi.org/10.1016/j.canlet.2019.02.011.
Yan F, et al. Exosome-based biomimetic nanoparticles targeted to inflamed joints for enhanced treatment of rheumatoid arthritis. J Nanobiotechnol. 2020;18(1):1–15. https://doi.org/10.1186/s12951-020-00675-6.
Jiang L, et al. A post-insertion strategy for surface functionalization of bacterial and mammalian cell-derived extracellular vesicles. Biochimica et Biophysica Acta (BBA)-General Subjects. 2021;1865(4): 129763. https://doi.org/10.1016/j.bbagen.2020.129763.
Wang J, et al. Chemically edited exosomes with dual ligand purified by microfluidic device for active targeted drug delivery to tumor cells. ACS Appl Mater Interfaces. 2017;9(33):27441–52. https://doi.org/10.1021/acsami.7b06464.
Arslan FB, Atar KO, Calis S. Antibody-mediated drug delivery. Int J Pharm. 2021;596: 120268. https://doi.org/10.1016/j.ijpharm.2021.120268.
Shi C, et al. Novel drug delivery liposomes targeted with a fully human anti-VEGF165 monoclonal antibody show superior antitumor efficacy in vivo. Biomed Pharmacother. 2015;73:48–57. https://doi.org/10.1016/j.biopha.2015.05.008.
Lu L, et al. Antibody-modified liposomes for tumor-targeting delivery of timosaponin AIII. Int J Nanomed. 2018;13:1927. https://doi.org/10.2147/IJN.S153107.
Nejadmoghaddam M-R, et al. Antibody-drug conjugates: possibilities and challenges. Avicenna J Med Biotechnol. 2019;11(1):3.
Drake C. Combination immunotherapy approaches. Ann Oncol. 2012;23:41–6. https://doi.org/10.1093/annonc/mds262.
Dolk E, et al. Induced refolding of a temperature denatured llama heavy-chain antibody fragment by its antigen. PROTEINS Struct Funct Bioinform. 2005;59(3):555–64. https://doi.org/10.1002/prot.20378.
Wang AZ, et al. Biofunctionalized targeted nanoparticles for therapeutic applications. Expert Opin Biol Ther. 2008;8(8):1063–70. https://doi.org/10.1517/14712598.8.8.1063.
Salunkhe S, et al. Surface functionalization of exosomes for target-specific delivery and in vivo imaging & tracking: strategies and significance. J Control Release. 2020. https://doi.org/10.1016/j.jconrel.2020.07.042.
Dintzis HM. Assembly of the peptide chains of hemoglobin. Proc Natl Acad Sci. 1961;47(3):247–61. https://doi.org/10.1073/pnas.47.3.247.
Jia G, et al. NRP-1 targeted and cargo-loaded exosomes facilitate simultaneous imaging and therapy of glioma in vitro and in vivo. Biomaterials. 2018;178:302–16. https://doi.org/10.1016/j.biomaterials.2018.06.029.
Lee H, et al. pH-responsive hyaluronate-anchored extracellular vesicles to promote tumor-targeted drug delivery. Carbohyd Polym. 2018;202:323–33. https://doi.org/10.1016/j.carbpol.2018.08.141.
Saneja A, et al. CD44 targeted PLGA nanomedicines for cancer chemotherapy. Eur J Pharm Sci. 2018;121:47–58. https://doi.org/10.1016/j.ejps.2018.05.012.
Johannssen T, Lepenies B. Glycan-based cell targeting to modulate immune responses. Trends Biotechnol. 2017;35(4):334–46. https://doi.org/10.1016/j.tibtech.2016.10.002.
Kanatani I, et al. Efficient gene transfer by pullulan–spermine occurs through both clathrin-and raft/caveolae-dependent mechanisms. J Control Release. 2006;116(1):75–82. https://doi.org/10.1016/j.jconrel.2006.09.001.
Jo J-I, et al. Liver targeting of plasmid DNA with a cationized pullulan for tumor suppression. J Nanosci Nanotechnol. 2006;6(9–10):2853–9. https://doi.org/10.1166/jnn.2006.466.
Zhou J, Rossi J. Aptamers as targeted therapeutics: current potential and challenges. Nat Rev Drug Discovery. 2017;16(3):181–202. https://doi.org/10.1038/nrd.2016.199.
Fang X, Tan W. Aptamers generated from cell-SELEX for molecular medicine: a chemical biology approach. Acc Chem Res. 2010;43(1):48–57. https://doi.org/10.1021/ar900101s.
Tan W, Fang X. Aptamers selected by cell-SELEX for theranostics. New York: Springer; 2015.
Xiong X, et al. DNA Aptamer-Mediated Cell Targeting. Angew Chem. 2013;125(5):1512–6. https://doi.org/10.1002/anie.201207063.
Liu H, et al. DNA-based micelles: synthesis, micellar properties and size-dependent cell permeability. Chem A Eur J. 2010;16(12):3791–7. https://doi.org/10.1002/chem.200901546.
Wan Y, et al. Aptamer-conjugated extracellular nanovesicles for targeted drug delivery. Can Res. 2018;78(3):798–808. https://doi.org/10.1158/0008-5472.CAN-17-2880.
Pi F. RNA Nanotechnology for Next Generation Targeted Drug Delivery. 2016. https://doi.org/10.13023/ETD.2016.432.
Lu J, et al. Targeted delivery of doxorubicin by folic acid-decorated dual functional nanocarrier. Mol Pharm. 2014;11(11):4164–78. https://doi.org/10.1021/mp500389v.
Perillo B, et al. ROS in cancer therapy: The bright side of the moon. Exp Mol Med. 2020;52(2):192–203. https://doi.org/10.1038/s12276-020-0384-2.
Wu S-K, et al. MR-guided focused ultrasound facilitates sonodynamic therapy with 5-aminolevulinic acid in a rat glioma model. Sci Rep. 2019;9(1):1–10. https://doi.org/10.1038/s41598-019-46832-2.
Pollalis D, et al. Intraocular RGD-Engineered Exosomes and Active Targeting of Choroidal Neovascularization (CNV). Cells. 2022;11(16):2573. https://doi.org/10.3390/cells11162573.
Kim MS, et al. Engineering macrophage-derived exosomes for targeted paclitaxel delivery to pulmonary metastases: in vitro and in vivo evaluations. Nanomed Nanotechnol Biol Med. 2018;14(1):195–204. https://doi.org/10.1016/j.nano.2017.09.011.
Whitford W, Guterstam P. Exosome manufacturing status. Future Med Chem. 2019;11(10):1225–36. https://doi.org/10.4155/fmc-2018-0417.
Munagala R, et al. Bovine milk-derived exosomes for drug delivery. Cancer Lett. 2016;371(1):48–61. https://doi.org/10.1016/j.canlet.2015.10.020.
Kalani A, et al. Curcumin-loaded embryonic stem cell exosomes restored neurovascular unit following ischemia-reperfusion injury. Int J Biochem Cell Biol. 2016;79:360–9. https://doi.org/10.1016/j.biocel.2016.09.002.
Zhang D, et al. Enrichment of selective miRNAs in exosomes and delivery of exosomal miRNAs in vitro and in vivo. Am J Physiol Lung Cell Mol Physiol. 2017;312(1):L110–21. https://doi.org/10.1152/ajplung.00423.2016.
Izco M, et al. Systemic exosomal delivery of shRNA minicircles prevents Parkinsonian pathology. Mol Ther. 2019;27(12):2111–22. https://doi.org/10.1016/j.ymthe.2019.08.010.
Hung ME, Leonard JN. Stabilization of exosome-targeting peptides via engineered glycosylation. J Biol Chem. 2015;290(13):8166–72. https://doi.org/10.1074/jbc.M114.621383.
Acknowledgements
The authors acknowledge support from Tarbiat Modares University and Shahid Beheshti University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was supported by the Iran National Science Foundation (INSF; Grant number 4003363) and Tarbiat Modares University.
Conflict of interest
Amir Hossein Mohammadi, Zeinab Ghazvinian, Fatemeh Bagheri, Masako Harada, and Kaveh Baghaei declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Further information is available from the first author and corresponding authors upon request.
Code availability
Not applicable.
Author contributions
AHM and FB conceptualized the manuscript; AHM and ZG wrote the manuscript; AHM designed all figures of the manuscript; and FB, KB, and MH revised the final version of the manuscript and supervised the project. All authors read and approved the final version of the manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mohammadi, A.H., Ghazvinian, Z., Bagheri, F. et al. Modification of Extracellular Vesicle Surfaces: An Approach for Targeted Drug Delivery. BioDrugs 37, 353–374 (2023). https://doi.org/10.1007/s40259-023-00595-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-023-00595-5