Abstract
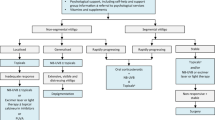
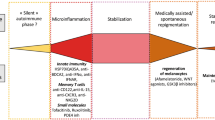
Vitiligo is a chronic autoimmune disease characterized by loss of pigment of the skin, affecting 0.5–2% of the population worldwide. It can have a significant impact on patients’ quality of life. In recent years, there has been significant progress in our understanding of the pathogenesis of vitiligo. It is believed that vitiligo develops due to a complex combination of genetics, oxidative stress, inflammation, and environmental triggers. Conventional treatments include camouflage, topical corticosteroids, topical calcineurin inhibitors, oral corticosteroids, phototherapy, and surgical procedures, with the treatment regimen dependent on the patient’s preferences and characteristics. With increased understanding of the importance of the Janus kinase (JAK)/signal transducer and activator of transcription (STAT) pathway in the pathogenesis of vitiligo, treatment has expanded to include the first US FDA-approved cream to repigment patients with vitiligo. This review summarizes our understanding of the major mechanisms involved in the pathogenesis of vitiligo and its most common available treatments.

Similar content being viewed by others
References
Krüger C, Schallreuter KU. A review of the worldwide prevalence of vitiligo in children/adolescents and adults. Int J Dermatol. 2012;51(10):1206–12. https://doi.org/10.1111/j.1365-4632.2011.05377.x.
Taïeb A, Picardo M. Clinical practice Vitiligo. N Engl J Med. 2009;360(2):160–9. https://doi.org/10.1056/NEJMcp0804388.
Alikhan A, Felsten LM, Daly M, Petronic-Rosic V. Vitiligo: a comprehensive overview Part I. Introduction, epidemiology, quality of life, diagnosis, differential diagnosis, associations, histopathology, etiology, and work-up. J Am Acad Dermatol. 2011;65(3):473–91. https://doi.org/10.1016/j.jaad.2010.11.061.
Sehgal VN, Srivastava G. Vitiligo: compendium of clinico-epidemiological features. Indian J Dermatol Venereol Leprol. 2007;73(3):149–56. https://doi.org/10.4103/0378-6323.32708.
Silverberg JI, Silverberg NB. Association between vitiligo extent and distribution and quality-of-life impairment. JAMA Dermatol. 2013;149(2):159–64. https://doi.org/10.1001/jamadermatol.2013.927.
Ezzedine K, Sheth V, Rodrigues M, Eleftheriadou V, Harris JE, Hamzavi IH, Pandya AG, Vitiligo Working Group. Vitiligo is not a cosmetic disease. J Am Acad Dermatol. 2015;73(5):883–5. https://doi.org/10.1016/j.jaad.2015.07.039.
Ezzedine K, Grimes PE, Meurant JM, Seneschal J, Léauté-Labrèze C, Ballanger F, Jouary T, Taïeb C, Taïeb A. Living with vitiligo: results from a national survey indicate differences between skin phototypes. Br J Dermatol. 2015;173(2):607–9. https://doi.org/10.1111/bjd.13839.
Osinubi O, Grainge MJ, Hong L, Ahmed A, Batchelor JM, Grindlay D, Thompson AR, Ratib S. The prevalence of psychological comorbidity in people with vitiligo: a systematic review and meta-analysis. Br J Dermatol. 2018;178(4):863–78. https://doi.org/10.1111/bjd.16049.
Hamidizadeh N, Ranjbar S, Ghanizadeh A, Parvizi MM, Jafari P, Handjani F. Evaluating prevalence of depression, anxiety and hopelessness in patients with Vitiligo on an Iranian population. Health Qual Life Outcomes. 2020;18(1):20. https://doi.org/10.1186/s12955-020-1278-7.
Bae JM, Kim JE, Lee RW, Ju HJ, Han JH, Lee JH, Woo YR, Lee JH, Bang CH, Park CJ, Ezzedine K, Kim M. Beyond quality of life: a call for patients’ own willingness to pay in chronic skin disease to assess psychosocial burden—a multicenter, cross-sectional, prospective survey. J Am Acad Dermatol. 2021;85(5):1321–4. https://doi.org/10.1016/j.jaad.2020.09.088.
Ezzedine K, Lim HW, Suzuki T, Katayama I, Hamzavi I, Lan CC, Goh BK, Anbar T. Vitiligo Global Issue Consensus Conference Panelists. Revised classification/nomenclature of vitiligo and related issues: the Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma Res. 2012;25(3):E1–13. https://doi.org/10.1111/j.1755-148X.2012.00997.x.
Taïeb A, Picardo M, VETF Members. The definition and assessment of vitiligo: a consensus report of the Vitiligo European Task Force. Pigment Cell Res. 2007;20(1):27–35. https://doi.org/10.1111/j.1600-0749.2006.00355.x.
Gawkrodger DJ, Ormerod AD, Shaw L, Mauri-Sole I, Whitton ME, Watts MJ, Anstey AV, Ingham J, Young K, Therapy Guidelines and Audit Subcommittee, British Association of Dermatologists; Clinical Standards Department, Royal College of Physicians of London; Cochrane Skin Group. Vitiligo Society Guideline for the diagnosis and management of vitiligo. Br J Dermatol. 2008;159(5):1051–76. https://doi.org/10.1111/j.1365-2133.2008.08881.x.
Taieb A, Alomar A, Böhm M, Dell’anna ML, De Pase A, Eleftheriadou V, Ezzedine K, Gauthier Y, Gawkrodger DJ, Jouary T, Leone G, Moretti S, Nieuweboer-Krobotova L, Olsson MJ, Parsad D, Passeron T, Tanew A, van der Veen W, van Geel N, Whitton M, Wolkerstorfer A, Picardo M, Vitiligo European Task Force (VETF); European Academy of Dermatology and Venereology (EADV); Union Europeenne des MedecinsSpecialistes (UEMS). Guidelines for the management of vitiligo: the European Dermatology Forum consensus. Br J Dermatol. 2013;168(1):5–19. https://doi.org/10.1111/j.1365-2133.2012.11197.x.
Oiso N, Suzuki T, Wataya-Kaneda M, Tanemura A, Tanioka M, Fujimoto T, Fukai K, Kawakami T, Tsukamoto K, Yamaguchi Y, Sano S, Mitsuhashi Y, Nishigori C, Morita A, Nakagawa H, Mizoguchi M, Katayama I. Guidelines for the diagnosis and treatment of vitiligo in Japan. J Dermatol. 2013;40(5):344–54. https://doi.org/10.1111/1346-8138.12099.
Esmat SM, El-Tawdy AM, Hafez GA, Zeid OA, Abdel Halim DM, Saleh MA, Leheta TM, Elmofty M. Acral lesions of vitiligo: why are they resistant to photochemotherapy? J Eur Acad Dermatol Venereol. 2012;26(9):1097–104. https://doi.org/10.1111/j.1468-3083.2011.04215.x.
Gawkrodger DJ, Ormerod AD, Shaw L, Mauri-Sole I, Whitton ME, Watts MJ, Anstey AV, Ingham J, Young K. Vitiligo: concise evidence based guidelines on diagnosis and management. Postgrad Med J. 2010;86(1018):466–71. https://doi.org/10.1136/pgmj.2009.093278.
Whitton ME, Pinart M, Batchelor J, Lushey C, Leonardi-Bee J, González U. Interventions for vitiligo. Cochrane Database Syst Rev. 2010;1: CD003263. https://doi.org/10.1002/14651858.CD003263.pub4.
Whitton ME, Pinart M, Batchelor J, Leonardi-Bee J, González U, Jiyad Z, Eleftheriadou V, Ezzedine K. Interventions for vitiligo. Cochrane Database Syst Rev. 2015;2: CD003263. https://doi.org/10.1002/14651858.CD003263.pub5.
Whitton M, Pinart M, Batchelor JM, Leonardi-Bee J, Gonzalez U, Jiyad Z, Eleftheriadou V, Ezzedine K. Evidence-based management of vitiligo: summary of a Cochrane systematic review. Br J Dermatol. 2016;174(5):962–9. https://doi.org/10.1111/bjd.14356.
Picardo M, Dell’Anna ML, Ezzedine K, Hamzavi I, Harris JE, Parsad D, Taieb A. Vitiligo. Nat Rev Dis Primers. 2015;1:15011. https://doi.org/10.1038/nrdp.2015.11.
Spritz RA, Andersen GH. Genetics of Vitiligo. Dermatol Clin. 2017;35(2):245–55. https://doi.org/10.1016/j.det.2016.11.013.
Spritz RA. Modern vitiligo genetics sheds new light on an ancient disease. J Dermatol. 2013;40(5):310–8. https://doi.org/10.1111/1346-8138.12147.
Spritz RA. Shared genetic relationships underlying generalized vitiligo and autoimmune thyroid disease. Thyroid. 2010;20(7):745–54. https://doi.org/10.1089/thy.2010.1643.
Czajkowski R, Męcińska-Jundziłł K. Current aspects of vitiligo genetics. Postepy Dermatol Alergol. 2014;31(4):247–55. https://doi.org/10.5114/pdia.2014.43497.
Jin Y, Mailloux CM, Gowan K, Riccardi SL, LaBerge G, Bennett DC, Fain PR, Spritz RA. NALP1 in vitiligo-associated multiple autoimmune disease. N Engl J Med. 2007;356(12):1216–25. https://doi.org/10.1056/NEJMoa061592.
Jin Y, Birlea SA, Fain PR, Gowan K, Riccardi SL, Holland PJ, Mailloux CM, Sufit AJ, Hutton SM, Amadi-Myers A, Bennett DC, Wallace MR, McCormack WT, Kemp EH, Gawkrodger DJ, Weetman AP, Picardo M, Leone G, Taïeb A, Jouary T, Ezzedine K, van Geel N, Lambert J, Overbeck A, Spritz RA. Variant of TYR and autoimmunity susceptibility loci in generalized vitiligo. N Engl J Med. 2010;362(18):1686–97. https://doi.org/10.1056/NEJMoa0908547.
Jin Y, Andersen G, Yorgov D, Ferrara TM, Ben S, Brownson KM, Holland PJ, Birlea SA, Siebert J, Hartmann A, Lienert A, van Geel N, Lambert J, Luiten RM, Wolkerstorfer A, Wietze van der Veen JP, Bennett DC, Taïeb A, Ezzedine K, Kemp EH, Gawkrodger DJ, Weetman AP, Kõks S, Prans E, Kingo K, Karelson M, Wallace MR, McCormack WT, Overbeck A, Moretti S, Colucci R, Picardo M, Silverberg NB, Olsson M, Valle Y, Korobko I, Böhm M, Lim HW, Hamzavi I, Zhou L, Mi QS, Fain PR, Santorico SA, Spritz RA. Genome-wide association studies of autoimmune vitiligo identify 23 new risk loci and highlight key pathways and regulatory variants. Nat Genet. 2016;48(11):1418–24. https://doi.org/10.1038/ng.3680.
Jin Y, Birlea SA, Fain PR, Mailloux CM, Riccardi SL, Gowan K, Holland PJ, Bennett DC, Wallace MR, McCormack WT, Kemp EH, Gawkrodger DJ, Weetman AP, Picardo M, Leone G, Taïeb A, Jouary T, Ezzedine K, van Geel N, Lambert J, Overbeck A, Spritz RA. Common variants in FOXP1 are associated with generalized vitiligo. Nat Genet. 2010;42(7):576–8. https://doi.org/10.1038/ng.602.
Jin Y, Birlea SA, Fain PR, Ferrara TM, Ben S, Riccardi SL, Cole JB, Gowan K, Holland PJ, Bennett DC, Luiten RM, Wolkerstorfer A, van der Veen JP, Hartmann A, Eichner S, Schuler G, van Geel N, Lambert J, Kemp EH, Gawkrodger DJ, Weetman AP, Taïeb A, Jouary T, Ezzedine K, Wallace MR, McCormack WT, Picardo M, Leone G, Overbeck A, Silverberg NB, Spritz RA. Genome-wide association analyses identify 13 new susceptibility loci for generalized vitiligo. Nat Genet. 2012;44(6):676–80. https://doi.org/10.1038/ng.2272.
Spritz RA. The genetics of generalized vitiligo: autoimmune pathways and an inverse relationship with malignant melanoma. Genome Med. 2010;2(10):78. https://doi.org/10.1186/gm199.
Birlea SA, Jin Y, Bennett DC, Herbstman DM, Wallace MR, McCormack WT, Kemp EH, Gawkrodger DJ, Weetman AP, Picardo M, Leone G, Taïeb A, Jouary T, Ezzedine K, van Geel N, Lambert J, Overbeck A, Fain PR, Spritz RA. Comprehensive association analysis of candidate genes for generalized vitiligo supports XBP1, FOXP3, and TSLP. J Investig Dermatol. 2011;131(2):371–81. https://doi.org/10.1038/jid.2010.337.
Spritz RA. Six decades of vitiligo genetics: genome-wide studies provide insights into autoimmune pathogenesis. J Investig Dermatol. 2012;132(2):268–73. https://doi.org/10.1038/jid.2011.321.
Alkhateeb A, Fain PR, Thody A, Bennett DC, Spritz RA. Epidemiology of vitiligo and associated autoimmune diseases in Caucasian probands and their families. Pigment Cell Res. 2003;16(3):208–14. https://doi.org/10.1034/j.1600-0749.2003.00032.x.
Millington GW, Levell NJ. Vitiligo: the historical curse of depigmentation. Int J Dermatol. 2007;46(9):990–5. https://doi.org/10.1111/j.1365-4632.2007.03195.x.
Nath SK, Majumder PP, Nordlund JJ. Genetic epidemiology of vitiligo: multilocus recessivity cross-validated. Am J Hum Genet. 1994;55(5):981–90.
Dell’Anna ML, Maresca V, Briganti S, Camera E, Falchi M, Picardo M. Mitochondrial impairment in peripheral blood mononuclear cells during the active phase of vitiligo. J Investig Dermatol. 2001;117(4):908–13. https://doi.org/10.1046/j.0022-202x.2001.01459.x.
Maresca V, Roccella M, Roccella F, Camera E, Del Porto G, Passi S, Grammatico P, Picardo M. Increased sensitivity to peroxidative agents as a possible pathogenic factor of melanocyte damage in vitiligo. J Investig Dermatol. 1997;109(3):310–3. https://doi.org/10.1111/1523-1747.ep12335801.
Jimbow K, Chen H, Park JS, Thomas PD. Increased sensitivity of melanocytes to oxidative stress and abnormal expression of tyrosinase-related protein in vitiligo. Br J Dermatol. 2001;144(1):55–65. https://doi.org/10.1046/j.1365-2133.2001.03952.x.
Speeckaert R, Dugardin J, Lambert J, Lapeere H, Verhaeghe E, Speeckaert MM, van Geel N. Critical appraisal of the oxidative stress pathway in vitiligo: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2018;32(7):1089–98. https://doi.org/10.1111/jdv.14792.
Richmond JM, Frisoli ML, Harris JE. Innate immune mechanisms in vitiligo: danger from within. Curr Opin Immunol. 2013;25(6):676–82. https://doi.org/10.1016/j.coi.2013.10.010.
Dell’Anna ML, Urbanelli S, Mastrofrancesco A, Camera E, Iacovelli P, Leone G, Manini P, D’Ischia M, Picardo M. Alterations of mitochondria in peripheral blood mononuclear cells of vitiligo patients. Pigment Cell Res. 2003;16(5):553–9. https://doi.org/10.1034/j.1600-0749.2003.00087.x.
Kang P, Zhang W, Chen X, Yi X, Song P, Chang Y, Zhang S, Gao T, Li C, Li S. TRPM2 mediates mitochondria-dependent apoptosis of melanocytes under oxidative stress. Free Radic Biol Med. 2018;126:259–68. https://doi.org/10.1016/j.freeradbiomed.2018.08.022.
Dell’Anna ML, Ottaviani M, Bellei B, Albanesi V, Cossarizza A, Rossi L, Picardo M. Membrane lipid defects are responsible for the generation of reactive oxygen species in peripheral blood mononuclear cells from vitiligo patients. J Cell Physiol. 2010;223(1):187–93. https://doi.org/10.1002/jcp.22027.
Denat L, Kadekaro AL, Marrot L, Leachman SA, Abdel-Malek ZA. Melanocytes as instigators and victims of oxidative stress. J Investig Dermatol. 2014;134(6):1512–8. https://doi.org/10.1038/jid.2014.65.
Zhong J, Rao X, Xu JF, Yang P, Wang CY. The role of endoplasmic reticulum stress in autoimmune-mediated beta-cell destruction in type 1 diabetes. Exp Diabetes Res. 2012;2012: 238980. https://doi.org/10.1155/2012/238980.
Bergqvist C, Ezzedine K. Vitiligo: a focus on pathogenesis and its therapeutic implications. J Dermatol. 2021;48(3):252–70. https://doi.org/10.1111/1346-8138.15743.
Meyskens FL Jr, Farmer P, Fruehauf JP. Redox regulation in human melanocytes and melanoma. Pigment Cell Res. 2001;14(3):148–54. https://doi.org/10.1034/j.1600-0749.2001.140303.x.
Puri N, Mojamdar M, Ramaiah A. In vitro growth characteristics of melanocytes obtained from adult normal and vitiligo subjects. J Investig Dermatol. 1987;88(4):434–8. https://doi.org/10.1111/1523-1747.ep12469795.
Puri N, Mojamdar M, Ramaiah A. Growth defects of melanocytes in culture from vitiligo subjects are spontaneously corrected in vivo in repigmenting subjects and can be partially corrected by the addition of fibroblast-derived growth factors in vitro. Arch Dermatol Res. 1989;281(3):178–84. https://doi.org/10.1007/BF00456389.
Ogg GS, Rod Dunbar P, Romero P, Chen JL, Cerundolo V. High frequency of skin-homing melanocyte-specific cytotoxic T lymphocytes in autoimmune vitiligo. J Exp Med. 1998;188(6):1203–8. https://doi.org/10.1084/jem.188.6.1203.
Wańkowicz-Kalińska A, van den Wijngaard RM, Tigges BJ, Westerhof W, Ogg GS, Cerundolo V, Storkus WJ, Das PK. Immunopolarization of CD4+ and CD8+ T cells to Type-1-like is associated with melanocyte loss in human vitiligo. Lab Investig. 2003;83(5):683–95. https://doi.org/10.1097/01.lab.0000069521.42488.1b.
van den Boorn JG, Konijnenberg D, Dellemijn TA, van der Veen JP, Bos JD, Melief CJ, Vyth-Dreese FA, Luiten RM. Autoimmune destruction of skin melanocytes by perilesional T cells from vitiligo patients. J Investig Dermatol. 2009;129(9):2220–32. https://doi.org/10.1038/jid.2009.32.
Harris JE, Harris TH, Weninger W, Wherry EJ, Hunter CA, Turka LA. A mouse model of vitiligo with focused epidermal depigmentation requires IFN-γ for autoreactive CD8+ T-cell accumulation in the skin. J Investig Dermatol. 2012;132(7):1869–76. https://doi.org/10.1038/jid.2011.463.
Bertolotti A, Boniface K, Vergier B, Mossalayi D, Taieb A, Ezzedine K, Seneschal J. Type I interferon signature in the initiation of the immune response in vitiligo. Pigment Cell Melanoma Res. 2014;27(3):398–407. https://doi.org/10.1111/pcmr.12219.
Yang L, Wei Y, Sun Y, Shi W, Yang J, Zhu L, Li M. Interferon-gamma inhibits melanogenesis and induces apoptosis in melanocytes: a pivotal role of CD8+ cytotoxic T lymphocytes in vitiligo. Acta Derm Venereol. 2015;95(6):664–70. https://doi.org/10.2340/00015555-2080.
Rashighi M, Agarwal P, Richmond JM, Harris TH, Dresser K, Su MW, Zhou Y, Deng A, Hunter CA, Luster AD, Harris JE. CXCL10 is critical for the progression and maintenance of depigmentation in a mouse model of vitiligo. Sci Transl Med. 2014;6(223): 223ra23. https://doi.org/10.1126/scitranslmed.3007811.
Rashighi M, Harris JE. Interfering with the IFN-γ/CXCL10 pathway to develop new targeted treatments for vitiligo. Ann Transl Med. 2015;3(21):343. https://doi.org/10.3978/j.issn.2305-5839.2015.11.36.
Wang XX, Wang QQ, Wu JQ, Jiang M, Chen L, Zhang CF, Xiang LH. Increased expression of CXCR3 and its ligands in patients with vitiligo and CXCL10 as a potential clinical marker for vitiligo. Br J Dermatol. 2016;174(6):1318–26. https://doi.org/10.1111/bjd.14416.
Abdallah M, El-Mofty M, Anbar T, Rasheed H, Esmat S, Al-Tawdy A, Fawzy MM, Abdel-Halim D, Hegazy R, Gawdat H, Bassiouny D, Ibrahim MA, Sany I, El-Bassiouny M, Khalil M, Abdel-Aziz A, El Maadawi ZM, Mostafa WZ, Egyptian Vitiligo Group. CXCL-10 and Interleukin-6 are reliable serum markers for vitiligo activity: a multicenter cross-sectional study. Pigment Cell Melanoma Res. 2018;31(2):330–6. https://doi.org/10.1111/pcmr.12667.
Riding RL, Harris JE. The role of memory CD8+ T cells in vitiligo. J Immunol. 2019;203(1):11–9. https://doi.org/10.4049/jimmunol.1900027.
Tokura Y, Phadungsaksawasdi P, Kurihara K, Fujiyama T, Honda T. Pathophysiology of skin resident memory T cells. Front Immunol. 2021;11: 618897. https://doi.org/10.3389/fimmu.2020.618897.
Boniface K, Jacquemin C, Darrigade AS, Dessarthe B, Martins C, Boukhedouni N, Vernisse C, Grasseau A, Thiolat D, Rambert J, Lucchese F, Bertolotti A, Ezzedine K, Taieb A, Seneschal J. Vitiligo skin is imprinted with resident memory CD8 T cells expressing CXCR3. J Investig Dermatol. 2018;138(2):355–64. https://doi.org/10.1016/j.jid.2017.08.038.
Cheuk S, Schlums H, GallaisSérézal I, Martini E, Chiang SC, Marquardt N, Gibbs A, Detlofsson E, Introini A, Forkel M, Höög C, Tjernlund A, Michaëlsson J, Folkersen L, Mjösberg J, Blomqvist L, Ehrström M, Ståhle M, Bryceson YT, Eidsmo L. CD49a expression defines tissue-resident CD8+ T cells poised for cytotoxic function in human skin. Immunity. 2017;46(2):287–300. https://doi.org/10.1016/j.immuni.2017.01.009.
Atwa MA, Ali SMM, Youssef N, Mahmoud Marie RE. Elevated serum level of interleukin-15 in vitiligo patients and its correlation with disease severity but not activity. J Cosmet Dermatol. 2021;20(8):2640–4. https://doi.org/10.1111/jocd.13908.
Frączek A, Owczarczyk-Saczonek A, Placek W. The role of TRM cells in the pathogenesis of vitiligo—a review of the current state-of-the-art. Int J Mol Sci. 2020;21(10):3552. https://doi.org/10.3390/ijms21103552.
Richmond JM, Strassner JP, Zapata L Jr, Garg M, Riding RL, Refat MA, Fan X, Azzolino V, Tovar-Garza A, Tsurushita N, Pandya AG, Tso JY, Harris JE. Antibody blockade of IL-15 signaling has the potential to durably reverse vitiligo. Sci Transl Med. 2018;10(450): eaam7710. https://doi.org/10.1126/scitranslmed.aam7710.
Azzolino V, Zapata L Jr, Garg M, Gjoni M, Riding RL, Strassner JP, Richmond JM, Harris JE. Jak inhibitors reverse vitiligo in mice but do not deplete skin resident memory T cells. J Investig Dermatol. 2021;141(1):182-184.e1. https://doi.org/10.1016/j.jid.2020.04.027.
Yamada T, Hasegawa S, Inoue Y, Date Y, Yamamoto N, Mizutani H, Nakata S, Matsunaga K, Akamatsu H. Wnt/β-catenin and kit signaling sequentially regulate melanocyte stem cell differentiation in UVB-induced epidermal pigmentation. J Investig Dermatol. 2013;133(12):2753–62. https://doi.org/10.1038/jid.2013.235.
Zhao SJ, Jia H, Xu XL, Bu WB, Zhang Q, Chen X, Ji J, Sun JF. Identification of the role of Wnt/β-catenin pathway through integrated analyses and in vivo experiments in vitiligo. Clin Cosmet Investig Dermatol. 2021;14:1089–103. https://doi.org/10.2147/CCID.S319061.
Regazzetti C, Joly F, Marty C, Rivier M, Mehul B, Reiniche P, Mounier C, Rival Y, Piwnica D, Cavalié M, Chignon-Sicard B, Ballotti R, Voegel J, Passeron T. Transcriptional analysis of vitiligo skin reveals the alteration of WNT pathway: a promising target for repigmenting vitiligo patients. J Investig Dermatol. 2015;135(12):3105–14.
Wagner RY, Luciani F, Cario-André M, Rubod A, Petit V, Benzekri L, Ezzedine K, Lepreux S, Steingrimsson E, Taieb A, Gauthier Y, Larue L, Delmas V. Altered E-cadherin levels and distribution in melanocytes precede clinical manifestations of vitiligo. J Investig Dermatol. 2015;135(7):1810–9. https://doi.org/10.1038/jid.2015.25.
Han X, Chang L, Qiu Z, Lin M, Wang Y, Liu D, Diao Q, Zhong JL, Xu W. Micro-injury induces hair regeneration and vitiligo repigmentation through Wnt/β-catenin pathway. Stem Cells Dev. 2022;31(5–6):111–8. https://doi.org/10.1089/scd.2021.0276.
Tedeschi A, Dall’Oglio F, Micali G, Schwartz RA, Janniger CK. Corrective camouflage in pediatric dermatology. Cutis. 2007;79(2):110–2.
Ongenae K, Dierckxsens L, Brochez L, van Geel N, Naeyaert JM. Quality of life and stigmatization profile in a cohort of vitiligo patients and effect of the use of camouflage. Dermatology. 2005;210(4):279–85. https://doi.org/10.1159/000084751.
Tanioka M, Yamamoto Y, Kato M, Miyachi Y. Camouflage for patients with vitiligo vulgaris improved their quality of life. J Cosmet Dermatol. 2010;9(1):72–5. https://doi.org/10.1111/j.1473-2165.2010.00479.x.
Bassiouny D, Hegazy R, Esmat S, Gawdat HI, Ahmed Ezzat M, Tawfik HA, Hegazy AA, Ibrahim S. Cosmetic camouflage as an adjuvant to vitiligo therapies: effect on quality of life. J Cosmet Dermatol. 2021;20(1):159–65. https://doi.org/10.1111/jocd.13459.
Morales-Sánchez MA, Laguna-Meraz JP, Peralta-Pedrero ML, Jurado-Santa CF. Effect of cosmetic camouflage in adults with vitiligo. Actas Dermosifiliogr. 2022;113(3):316–8. https://doi.org/10.1016/j.ad.2020.04.018(English, Spanish).
Li M, Wang F, Ding X, Xu Q, Du J. Evaluation of the potential interference of camouflage on the treatment of vitiligo: an observer-blinded self-controlled study. Dermatol Ther. 2021;34(1): e14545. https://doi.org/10.1111/dth.14545.
Fesq H, Brockow K, Strom K, Mempel M, Ring J, Abeck D. Dihydroxyacetone in a new formulation: a powerful therapeutic option in vitiligo. Dermatology. 2001;203(3):241–3. https://doi.org/10.1159/000051757.
Suga Y, Ikejima A, Matsuba S, Ogawa H. Medical pearl: DHA application for camouflaging segmental vitiligo and piebald lesions. J Am Acad Dermatol. 2002;47(3):436–8. https://doi.org/10.1067/mjd.2002.119670.
Rajatanavin N, Suwanachote S, Kulkollakarn S. Dihydroxyacetone: a safe camouflaging option in vitiligo. Int J Dermatol. 2008;47(4):402–6. https://doi.org/10.1111/j.1365-4632.2008.03356.x.
Steuer AB, Zampella JG. Camouflaging vitiligo using a spray tan. Dermatol Online J. 2020;26(7): 13030/qt63j996qx.
Hsu S. Camouflaging vitiligo with dihydroxyacetone. Dermatol Online J. 2008;14(8):23.
Speeckaert R, van Geel N. Vitiligo: an update on pathophysiology and treatment options. Am J Clin Dermatol. 2017;18(6):733–44. https://doi.org/10.1007/s40257-017-0298-5.
Njoo MD, Spuls PI, Bos JD, Westerhof W, Bossuyt PM. Nonsurgical repigmentation therapies in vitiligo Meta-analysis of the literature. Arch Dermatol. 1998;134(12):1532–40. https://doi.org/10.1001/archderm.134.12.1532.
Coondoo A, Phiske M, Verma S, Lahiri K. Side-effects of topical steroids: a long overdue revisit. Indian Dermatol Online J. 2014;5(4):416–25. https://doi.org/10.4103/2229-5178.142483.
Kwinter J, Pelletier J, Khambalia A, Pope E. High-potency steroid use in children with vitiligo: a retrospective study. J Am Acad Dermatol. 2007;56(2):236–41.
Arora CJ, Rafiq M, Shumack S, Gupta M. The efficacy and safety of tacrolimus as mono- and adjunctive therapy for vitiligo: a systematic review of randomised clinical trials. Australas J Dermatol. 2020;61(1):e1–9. https://doi.org/10.1111/ajd.13096.
Lepe V, Moncada B, Castanedo-Cazares JP, Torres-Alvarez MB, Ortiz CA, Torres-Rubalcava AB. A double-blind randomized trial of 0.1% tacrolimus vs 0.05% clobetasol for the treatment of childhood vitiligo. Arch Dermatol. 2003;139(5):581–5. https://doi.org/10.1001/archderm.139.5.581.
Coskun B, Saral Y, Turgut D. Topical 0.05% clobetasol propionate versus 1% pimecrolimus ointment in vitiligo. Eur J Dermatol. 2005;15(2):88–91.
Mumtaz H, Anis S, Akhtar A, Rubab M, Zafar A, Niazi N, Bahadur H, Talpur AS, Shafiq MA, Fatima T. Efficacy of tacrolimus versus clobetasol in the treatment of vitiligo. Cureus. 2020;12(12): e11985. https://doi.org/10.7759/cureus.11985.
Ho N, Pope E, Weinstein M, Greenberg S, Webster C, Krafchik BR. A double-blind, randomized, placebo-controlled trial of topical tacrolimus 0.1% vs. clobetasol propionate 0.05% in childhood vitiligo. Br J Dermatol. 2011;165(3):626–32. https://doi.org/10.1111/j.1365-2133.2011.10351.x.
Chang HC, Hsu YP, Huang YC. The effectiveness of topical calcineurin inhibitors compared with topical corticosteroids in the treatment of vitiligo: a systematic review and meta-analysis. J Am Acad Dermatol. 2020;82(1):243–5. https://doi.org/10.1016/j.jaad.2019.07.108.
Saleh R, Ahmed AA, M Abd-Elmagid W. Efficacy of topical tacrolimus 003% monotherapy in the treatment of non-segmental vitiligo: a randomized, controlled trial. J Cosmet Dermatol. 2021;20(12):3943–52. https://doi.org/10.1111/jocd.14041.
Lee JH, Kwon HS, Jung HM, Lee H, Kim GM, Yim HW, Bae JM. Treatment outcomes of topical calcineurin inhibitor therapy for patients with vitiligo: a systematic review and meta-analysis. JAMA Dermatol. 2019;155(8):929–38. https://doi.org/10.1001/jamadermatol.2019.0696.
Seneschal J, Duplaine A, Maillard H, Passeron T, Andreu N, Lassalle R, Favary C, Droitcourt C, Taïeb A, Ezzedine K. Efficacy and safety of tacrolimus 0.1% for the treatment of facial vitiligo: a multicenter randomized, double-blinded vehicle-controlled study. J Investig Dermatol. 2021;141(7):1728–34. https://doi.org/10.1016/j.jid.2020.12.028.
Cavalié M, Ezzedine K, Fontas E, Montaudié H, Castela E, Bahadoran P, Taïeb A, Lacour JP, Passeron T. Maintenance therapy of adult vitiligo with 0.1% tacrolimus ointment: a randomized, double blind, placebo-controlled study. J Investig Dermatol. 2015;135(4):970–4. https://doi.org/10.1038/jid.2014.527.
Shim WH, Suh SW, Jwa SW, Song M, Kim HS, Ko HC, Kim BS, Kim MB. A pilot study of 1% pimecrolimus cream for the treatment of childhood segmental vitiligo. Ann Dermatol. 2013;25(2):168–72. https://doi.org/10.5021/ad.2013.25.2.168.
Hu W, Xu Y, Ma Y, Lei J, Lin F, Xu AE. Efficacy of the topical calcineurin inhibitors tacrolimus and pimecrolimus in the treatment of vitiligo in infants under 2 years of age: a randomized open-label pilot study. Clin Drug Investig. 2019;39(12):1233–8. https://doi.org/10.1007/s40261-019-00845-x.
Hu W, Lin F, Lei J, Xu AE. Impacts of exposure to topical calcineurin inhibitors on metabolism in vitiligo infants. Pediatr Res. 2022. https://doi.org/10.1038/s41390-022-02133-5.
Ju HJ, Han JH, Kim MS, Lee SH, Shin JW, Choi M, Jeong KH, Han TY, Choi CW, Lee HJ, Oh SH, Lee SH, Kim DH, Shin J, Lee JH, Kim SS, Kang HY, Chang SE, Kim JS, Lee DY, Choi GS, Suh DH, Chan Kim Y, Park CJ, Kim KH, Lee AY, Chan Park K, Lee MH, Bae JM, Korean Society for Vitiligo and the Korean Society for Photomedicine. The long-term risk of lymphoma and skin cancer did not increase after topical calcineurin inhibitor use and phototherapy in a cohort of 25,694 patients with vitiligo. J Am Acad Dermatol. 2021;84(6):1619–27. https://doi.org/10.1016/j.jaad.2021.01.067.
Mosher DB, Parrish JA, Fitzpatrick TB. Monobenzylether of hydroquinone. A retrospective study of treatment of 18 vitiligo patients and a review of the literature. Br J Dermatol. 1977;97(6):669–79. https://doi.org/10.1111/j.1365-2133.1977.tb14275.x.
Njoo MD, Vodegel RM, Westerhof W. Depigmentation therapy in vitiligo universalis with topical 4-methoxyphenol and the Q-switched ruby laser. J Am Acad Dermatol. 2000;42(5 Pt 1):760–9. https://doi.org/10.1067/mjd.2000.103813.
Rordam OM, Lenouvel EW, Maalo M. Successful treatment of extensive vitiligo with monobenzone. J Clin Aesthet Dermatol. 2012;5(12):36–9.
Tan ES, Sarkany R. Topical monobenzyl ether of hydroquinone is an effective and safe treatment for depigmentation of extensive vitiligo in the medium term: a retrospective cohort study of 53 cases. Br J Dermatol. 2015;172(6):1662–4. https://doi.org/10.1111/bjd.13642.
Oakley AM. Rapid repigmentation after depigmentation therapy: vitiligo treated with monobenzyl ether of hydroquinone. Australas J Dermatol. 1996;37(2):96–8. https://doi.org/10.1111/j.1440-0960.1996.tb01014.x.
Nofal A, Fawzy MM, Alakad R. The use of trichloroacetic acid as a depigmenting therapy in universal vitiligo. J Dtsch Dermatol Ges. 2021;19(2):241–6. https://doi.org/10.1111/ddg.14316.
Zanini M, Machado Filho CD. Depigmentation therapy for generalized vitiligo with topical 88% phenol solution. An Bras Dermatol. 2005;80(4):415–6.
Mahmood F, Beach RA. Can it make me white again? A case report of 88% phenol as a depigmenting agent in vitiligo. SAGE Open Med Case Rep. 2021;9: 2050313X21993307. https://doi.org/10.1177/2050313X21993307.
Kim YJ, Chung BS, Choi KC. Depigmentation therapy with Q-switched ruby laser after tanning in vitiligo universalis. Dermatol Surg. 2001;27(11):969–70. https://doi.org/10.1046/j.1524-4725.2001.01101.x.
Komen L, Zwertbroek L, Burger SJ, van der Veen JP, de Rie MA, Wolkerstorfer A. Q-switched laser depigmentation in vitiligo, most effective in active disease. Br J Dermatol. 2013;169(6):1246–51. https://doi.org/10.1111/bjd.12571.
Majid I, Imran S. Depigmentation therapy with Q-switched Nd:YAG laser in universal vitiligo. J Cutan Aesthet Surg. 2013;6(2):93–6. https://doi.org/10.4103/0974-2077.112670.
Rao J, Fitzpatrick RE. Use of the Q-switched 755-nm alexandrite laser to treat recalcitrant pigment after depigmentation therapy for vitiligo. Dermatol Surg. 2004;30(7):1043–5. https://doi.org/10.1111/j.1524-4725.2004.30313.x.
Radmanesh M. Depigmentation of the normally pigmented patches in universal vitiligo patients by cryotherapy. J Eur Acad Dermatol Venereol. 2000;14(3):149–52. https://doi.org/10.1046/j.1468-3083.2000.00038.x.
van Geel N, Depaepe L, Speeckaert R. Laser (755 nm) and cryotherapy as depigmentation treatments for vitiligo: a comparative study. J Eur Acad Dermatol Venereol. 2015;29(6):1121–7. https://doi.org/10.1111/jdv.12762.
Kavuossi H. Induction of depigmentation in a universal vitiligo patient with combination of cryotherapy and phenol. J Pak Assoc Dermatol. 2009;19:112–4.
Di Nuzzo S, Masotti A. Depigmentation therapy in vitiligo universalis with cryotherapy and 4-hydroxyanisole. Clin Exp Dermatol. 2010;35(2):215–6. https://doi.org/10.1111/j.1365-2230.2009.03412.x.
AlGhamdi KM, Kumar A. Depigmentation therapies for normal skin in vitiligo universalis. J Eur Acad Dermatol Venereol. 2011;25(7):749–57. https://doi.org/10.1111/j.1468-3083.2010.03876.x.
Kim SM, Lee HS, Hann SK. The efficacy of low-dose oral corticosteroids in the treatment of vitiligo patients. Int J Dermatol. 1999;38(7):546–50. https://doi.org/10.1046/j.1365-4362.1999.00623.x.
Imamura S, Tagami H. Treatment of vitiligo with oral corticosteroids. Dermatologica. 1976;153(3):179–85. https://doi.org/10.1159/000251114.
Rice JB, White AG, Scarpati LM, Wan G, Nelson WW. Long-term systemic corticosteroid exposure: a systematic literature review. Clin Ther. 2017;39(11):2216–29. https://doi.org/10.1016/j.clinthera.2017.09.011.
Pasricha JS, Khaitan BK. Oral mini-pulse therapy with betamethasone in vitiligo patients having extensive or fast-spreading disease. Int J Dermatol. 1993;32(10):753–7. https://doi.org/10.1111/j.1365-4362.1993.tb02754.x.
Radakovic-Fijan S, Fürnsinn-Friedl AM, Hönigsmann H, Tanew A. Oral dexamethasone pulse treatment for vitiligo. J Am Acad Dermatol. 2001;44(5):814–7. https://doi.org/10.1067/mjd.2001.113475.
Banerjee K, Barbhuiya JN, Ghosh AP, Dey SK, Karmakar PR. The efficacy of low-dose oral corticosteroids in the treatment of vitiligo patient. Indian J Dermatol Venereol Leprol. 2003;69(2):135–7.
Kanwar AJ, Mahajan R, Parsad D. Low-dose oral mini-pulse dexamethasone therapy in progressive unstable vitiligo. J Cutan Med Surg. 2013;17(4):259–68. https://doi.org/10.2310/7750.2013.12053.
Chavez-Alvarez S, Herz-Ruelas M, Raygoza-Cortez AK, Suro-Santos Y, Ocampo-Candiani J, Alvarez-Villalobos NA, Villarreal-Martinez A. Oral mini-pulse therapy in vitiligo: a systematic review. Int J Dermatol. 2021;60(7):868–76. https://doi.org/10.1111/ijd.15464.
Koh MJ, Mok ZR, Chong WS. Phototherapy for the treatment of vitiligo in Asian children. Pediatr Dermatol. 2015;32(2):192–7. https://doi.org/10.1111/pde.12506.
Seccombe E, Wynne MD, Clancy C, Godfrey KM, Fityan A. A retrospective review of phototherapy in children, at a tertiary paediatric dermatology unit. Photodermatol Photoimmunol Photomed. 2021;37(1):34–8. https://doi.org/10.1111/phpp.12604.
Lopes C, Trevisani VF, Melnik T. Efficacy and safety of 308-nm monochromatic excimer lamp versus other phototherapy devices for vitiligo: a systematic review with meta-analysis. Am J Clin Dermatol. 2016;17(1):23–32. https://doi.org/10.1007/s40257-015-0164-2.
Bae JM, Jung HM, Hong BY, Lee JH, Choi WJ, Lee JH, Kim GM. Phototherapy for vitiligo: a systematic review and meta-analysis. JAMA Dermatol. 2017;153(7):666–74. https://doi.org/10.1001/jamadermatol.2017.0002.
Brazzelli V, Antoninetti M, Palazzini S, Barbagallo T, De Silvestri A, Borroni G. Critical evaluation of the variants influencing the clinical response of vitiligo: study of 60 cases treated with ultraviolet B narrow-band phototherapy. J Eur Acad Dermatol Venereol. 2007;21(10):1369–74. https://doi.org/10.1111/j.1468-3083.2007.02278.x.
Anbar TS, Westerhof W, Abdel-Rahman AT, El-Khayyat MA. Evaluation of the effects of NB-UVB in both segmental and non-segmental vitiligo affecting different body sites. Photodermatol Photoimmunol Photomed. 2006;22(3):157–63. https://doi.org/10.1111/j.1600-0781.2006.00222.x.
Abdulla SJ, Desgroseilliers JP. Treatment of vitiligo with narrow-band ultraviolet B: advantages and disadvantages. J Cutan Med Surg. 2008;12(4):174–9. https://doi.org/10.2310/7750.2008.07054.
Khojah HMJ, Alharbi AG, Alshaeri AA, Alahmadi YM, Elbadawy HM. Impact of narrow-band ultraviolet B radiation therapy on the quality of life of patients with vitiligo. J Taibah Univ Med Sci. 2021;16(6):843–8. https://doi.org/10.1016/j.jtumed.2021.04.012.
Agarwal K, Podder I, Kassir M, Vojvodic A, Schwartz RA, Wollina U, Valle Y, Lotti T, Rokni GR, Grabbe S, Goldust M. Therapeutic options in vitiligo with special emphasis on immunomodulators: a comprehensive update with review of literature. Dermatol Ther. 2020;33(2): e13215. https://doi.org/10.1111/dth.13215.
Ashraf AZ, Azurdia RM, Cohen SN. The effectiveness of home-based phototherapy for vitiligo: a systematic review of randomised controlled trials. Photodermatol Photoimmunol Photomed. 2021. https://doi.org/10.1111/phpp.12766.
Sonthalia S. Topical Band-pass Filter Cream (TBFC)-assisted home-based NB-UVB: a must-know Alternative to artificial phototherapy. J Cosmet Dermatol. 2021;20(7):2141–7. https://doi.org/10.1111/jocd.14215.
Leone G, Iacovelli P, Paro Vidolin A, Picardo M. Monochromatic excimer light 308 nm in the treatment of vitiligo: a pilot study. J Eur Acad Dermatol Venereol. 2003;17(5):531–7. https://doi.org/10.1046/j.1468-3083.2003.00818.x.
Cheng YP, Chiu HY, Jee SH, Tsai TF. Excimer light photototherapy of segmental and non-segmental vitiligo: experience in Taiwan. Photodermatol Photoimmunol Photomed. 2012;28(1):6–11. https://doi.org/10.1111/j.1600-0781.2011.00628.x.
Abdel Latif AA, Ibrahim SM. Monochromatic excimer light versus combination of topical steroid with vitamin D3 analogue in the treatment of nonsegmental vitiligo: a randomized blinded comparative study. Dermatol Ther. 2015;28(6):383–9. https://doi.org/10.1111/dth.12289.
Sun Y, Wu Y, Xiao B, Li L, Li L, Chen HD, Gao XH. Treatment of 308-nm excimer laser on vitiligo: a systemic review of randomized controlled trials. J Dermatolog Treat. 2015;26(4):347–53. https://doi.org/10.3109/09546634.2014.991268.
Tran AK, Vaidya S. Treatment of refractory vitiligo with the 308-nm excimer lamp—an Australian prospective analysis of clinical efficacy and safety. Australas J Dermatol. 2020;61(3):289–91. https://doi.org/10.1111/ajd.13259.
Spencer JM, Nossa R, Ajmeri J. Treatment of vitiligo with the 308-nm excimer laser: a pilot study. J Am Acad Dermatol. 2002;46(5):727–31. https://doi.org/10.1067/mjd.2002.121357.
Taneja A, Trehan M, Taylor CR. 308-nm excimer laser for the treatment of localized vitiligo. Int J Dermatol. 2003;42(8):658–62. https://doi.org/10.1046/j.1365-4362.2003.01997.x.
Choi KH, Park JH, Ro YS. Treatment of Vitiligo with 308-nm xenon-chloride excimer laser: therapeutic efficacy of different initial doses according to treatment areas. J Dermatol. 2004;31(4):284–92. https://doi.org/10.1111/j.1346-8138.2004.tb00674.x.
Esposito M, Soda R, Costanzo A, Chimenti S. Treatment of vitiligo with the 308 nm excimer laser. Clin Exp Dermatol. 2004;29(2):133–7. https://doi.org/10.1111/j.1365-2230.2004.01477.x.
Hadi SM, Spencer JM, Lebwohl M. The use of the 308-nm excimer laser for the treatment of vitiligo. Dermatol Surg. 2004;30(7):983–6. https://doi.org/10.1111/j.1524-4725.2004.30302.x.
Hadi S, Tinio P, Al-Ghaithi K, Al-Qari H, Al-Helalat M, Lebwohl M, Spencer J. Treatment of vitiligo using the 308-nm excimer laser. Photomed Laser Surg. 2006;24(3):354–7. https://doi.org/10.1089/pho.2006.24.354.
Hofer A, Hassan AS, Legat FJ, Kerl H, Wolf P. The efficacy of excimer laser (308 nm) for vitiligo at different body sites. J Eur Acad Dermatol Venereol. 2006;20(5):558–64. https://doi.org/10.1111/j.1468-3083.2006.01547.x.
Chimento SM, Newland M, Ricotti C, Nistico S, Romanelli P. A pilot study to determine the safety and efficacy of monochromatic excimer light in the treatment of vitiligo. J Drugs Dermatol. 2008;7(3):258–63.
Cho S, Zheng Z, Park YK, Roh MR. The 308-nm excimer laser: a promising device for the treatment of childhood vitiligo. Photodermatol Photoimmunol Photomed. 2011;27(1):24–9. https://doi.org/10.1111/j.1600-0781.2010.00558.x.
Greve B, Raulin C, Fischer E. Excimer-Laser bei Vitiligo—Kritische Wertung eigener retrospektiver Behandlungsergebnisse und Literaturübersicht [Excimer laser treatment of vitiligo—critical retrospective assessment of own results and literature overview]. J Dtsch Dermatol Ges. 2006;4(1):32–40. https://doi.org/10.1111/j.1610-0387.2006.05879.x(German).
Al-Otaibi SR, Zadeh VB, Al-Abdulrazzaq AH, Tarrab SM, Al-Owaidi HA, Mahrous R, Kadyan RS, Najem NM. Using a 308-nm excimer laser to treat vitiligo in Asians. Acta Dermatovenerol Alp Pannonica Adriat. 2009;18(1):13–9.
Zhang XY, He YL, Dong J, Xu JZ, Wang J. Clinical efficacy of a 308 nm excimer laser in the treatment of vitiligo. Photodermatol Photoimmunol Photomed. 2010;26(3):138–42. https://doi.org/10.1111/j.1600-0781.2010.00509.x.
Noborio R, Nakamura M, Yoshida M, Nakamura R, Oshima R, Kubo R, Kato H, Morita A. Monotherapy for vitiligo using a 308-nm xenon-chloride excimer laser: colorimetric assessment of factors that influence treatment efficacy. J Dermatol. 2012;39(12):1102–3. https://doi.org/10.1111/j.1346-8138.2012.01633.x.
Fa Y, Lin Y, Chi XJ, Shi WH, Wang JL, Guo X, Geng JH, Liu HX, Zhang FR. Treatment of vitiligo with 308-nm excimer laser: our experience from a 2-year follow-up of 979 Chinese patients. J Eur Acad Dermatol Venereol. 2017;31(2):337–40. https://doi.org/10.1111/jdv.13917.
Do JE, Shin JY, Kim DY, Hann SK, Oh SH. The effect of 308 nm excimer laser on segmental vitiligo: a retrospective study of 80 patients with segmental vitiligo. Photodermatol Photoimmunol Photomed. 2011;27(3):147–51. https://doi.org/10.1111/j.1600-0781.2011.00587.x.
Majid I, Imran S. Excimer light therapy in childhood segmental vitiligo: early treatment gives better results. Dermatol Ther. 2020;33(3): e13408. https://doi.org/10.1111/dth.13408.
Sethi S, Silverberg N. Short and long-term outcomes of 308-nm laser for pediatric vitiligo. J Drugs Dermatol. 2022;21(7):773–5. https://doi.org/10.36849/JDD.6895.
Tabassum H, Majid I, Imran S. Is targeted UVB as effective as excimer light phototherapy in treatment of vitiligo? Dermatol Ther. 2021;34(5): e15058. https://doi.org/10.1111/dth.15058.
Poolsuwan P, Churee C, Pattamadilok B. Comparative efficacy between localized 308-nm excimer light and targeted 311-nm narrowband ultraviolet B phototherapy in vitiligo: a randomized, single-blind comparison study. Photodermatol Photoimmunol Photomed. 2021;37(2):123–30. https://doi.org/10.1111/phpp.12619.
Yadav D, Khandpur S, Bhari N. Targeted phototherapy with excimer light is not efficacious in the management of residual vitiligo patches following whole-body narrowband ultraviolet B light therapy: results of a retrospective case series. Indian J Dermatol Venereol Leprol. 2022;88(2):249–51. https://doi.org/10.25259/IJDVL_8_2020.
Hofer A, Hassan AS, Legat FJ, Kerl H, Wolf P. Optimal weekly frequency of 308-nm excimer laser treatment in vitiligo patients. Br J Dermatol. 2005;152(5):981–5. https://doi.org/10.1111/j.1365-2133.2004.06321.x.
Shen Z, Gao TW, Chen L, Yang L, Wang YC, Sun LC, Li CY, Xiao Y, Liu YF. Optimal frequency of treatment with the 308-nm excimer laser for vitiligo on the face and neck. Photomed Laser Surg. 2007;25(5):418–27. https://doi.org/10.1089/pho.2007.2086.
Ayob S, Cockayne SE, Gawkrodger DJ. Once weekly targeted excimer light produced modest repigmentation of vitiligo over a 20-week period. J Eur Acad Dermatol Venereol. 2018;32(8):e307–8. https://doi.org/10.1111/jdv.14853.
Xiang L. Once-weekly treatment of vitiligo with monochromatic excimer light 308 nm in Chinese patients. J Eur Acad Dermatol Venereol. 2008;22(7):899–900. https://doi.org/10.1111/j.1468-3083.2007.02518.x.
Al-Shobaili HA. Correlation of clinical efficacy and psychosocial impact on vitiligo patients by excimer laser treatment. Ann Saudi Med. 2014;34(2):115–21. https://doi.org/10.5144/0256-4947.2014.115.
Al-Shobaili HA. Treatment of vitiligo patients by excimer laser improves patients’ quality of life. J Cutan Med Surg. 2015;19(1):50–6. https://doi.org/10.2310/7750.2014.14002.
Bae JM, Eun SH, Oh SH, Shin JH, Kang HY, Kim KH, Lee SC, Choi CW. The 308-nm excimer laser treatment does not increase the risk of skin cancer in patients with vitiligo: a population-based retrospective cohort study. Pigment Cell Melanoma Res. 2019;32(5):714–8. https://doi.org/10.1111/pcmr.12781.
Sung JM, Bae JM, Kang HY. Comparison of cyclic and continuous 308-nm excimer laser treatments for vitiligo: a randomized controlled noninferiority trial. J Am Acad Dermatol. 2018;78(3):605-607.e1. https://doi.org/10.1016/j.jaad.2017.09.048.
Shenoi SD, Prabhu S, Indian Association of Dermatologists, Venereologists and Leprologists. Photochemotherapy (PUVA) in psoriasis and vitiligo. Indian J Dermatol Venereol Leprol. 2014;80(6):497–504. https://doi.org/10.4103/0378-6323.144143.
Wildfang IL, Jacobsen FK, Thestrup-Pedersen K. PUVA treatment of vitiligo: a retrospective study of 59 patients. Acta Derm Venereol. 1992;72(4):305–6.
Chuan MT, Tsai YJ, Wu MC. Effectiveness of psoralen photochemotherapy for vitiligo. J Formos Med Assoc. 1999;98(5):335–40.
Sahin S, Hindioğlu U, Karaduman A. PUVA treatment of vitiligo: a retrospective study of Turkish patients. Int J Dermatol. 1999;38(7):542–5. https://doi.org/10.1046/j.1365-4362.1999.00654.x.
Tallab T, Joharji H, Bahamdan K, Karkashan E, Mourad M, Ibrahim K. Response of vitiligo to PUVA therapy in Saudi patients. Int J Dermatol. 2005;44(7):556–8. https://doi.org/10.1111/j.1365-4632.2004.02014.x.
Anbar TS, El-Sawy AE, Attia SK, Barakat MT, Moftah NH, El-Ammawy TS, Abdel-Rahman AT, El-Tonsy MH. Effect of PUVA therapy on melanocytes and keratinocytes in non-segmental vitiligo: histopathological, immuno-histochemical and ultrastructural study. Photodermatol Photoimmunol Photomed. 2012;28(1):17–25. https://doi.org/10.1111/j.1600-0781.2011.00631.x.
Wu CS, Lan CC, Wang LF, Chen GS, Wu CS, Yu HS. Effects of psoralen plus ultraviolet A irradiation on cultured epidermal cells in vitro and patients with vitiligo in vivo. Br J Dermatol. 2007;156(1):122–9. https://doi.org/10.1111/j.1365-2133.2006.07584.x.
Kwok YK, Anstey AV, Hawk JL. Psoralen photochemotherapy (PUVA) is only moderately effective in widespread vitiligo: a 10-year retrospective study. Clin Exp Dermatol. 2002;27(2):104–10. https://doi.org/10.1046/j.1365-2230.2002.00984.x.
Yones SS, Palmer RA, Garibaldinos TM, Hawk JL. Randomized double-blind trial of treatment of vitiligo: efficacy of psoralen-UV-A therapy vs Narrowband-UV-B therapy. Arch Dermatol. 2007;143(5):578–84. https://doi.org/10.1001/archderm.143.5.578.
El-Mofty M, Mostafa WZ, Bosseila M, Youssef R, Esmat S, El Ramly A, Fawzi M, Mahgoub D, Nagui N, Mashaly HM, El-Fangary M, Fathy M. A large scale analytical study on efficacy of different photo(chemo)therapeutic modalities in the treatment of psoriasis, vitiligo and mycosis fungoides. Dermatol Ther. 2010;23(4):428–34. https://doi.org/10.1111/j.1529-8019.2010.01345.x.
Bhatnagar A, Kanwar AJ, Parsad D, De D. Psoralen and ultraviolet A and narrow-band ultraviolet B in inducing stability in vitiligo, assessed by vitiligo disease activity score: an open prospective comparative study. J Eur Acad Dermatol Venereol. 2007;21(10):1381–5. https://doi.org/10.1111/j.1468-3083.2007.02283.x.
Sakhiya J, Sakhiya D, Virmani N, Gajjar T, Kaklotar J, Khambhati R, Daruwala F, Dudhatra N. A retrospective study of 3,000 Indian patients with vitiligo treated with phototherapy or topical monotherapy. J Clin Aesthet Dermatol. 2021;14(2):46–9.
Liu YY, Zhou JF, Zhen Y, Cui Y, Song Y, Yao L, Li SS. Clinical efficacy analysis of 110 cases of childhood vitiligo with non-surgical combined therapy. J Dermatolog Treat. 2022. https://doi.org/10.1080/09546634.2022.2104443.
Roy P, Saha SK, Paul PC, Reza AK, Nandi AK, Sultana S, Saha S, Akhter SM, Khatun S, Habibunnahar M. Effectiveness of topical corticosteroid, topical calcineurin inhibitors and combination of them in the treatment of vitiligo. Mymensingh Med J. 2016;25(4):620–7.
Dang YP, Li Q, Shi F, Yuan XY, Liu W. Effect of topical calcineurin inhibitors as monotherapy or combined with phototherapy for vitiligo treatment: a meta-analysis. Dermatol Ther. 2016;29(2):126–33. https://doi.org/10.1111/dth.12295.
Chang HC, Sung CW. Efficacy of combination therapy of narrowband-ultraviolet B phototherapy or excimer laser with topical tacrolimus for vitiligo: an updated systematic review and meta-analysis. Photodermatol Photoimmunol Photomed. 2021;37(1):74–7. https://doi.org/10.1111/phpp.12593.
Li R, Qiao M, Wang X, Zhao X, Sun Q. Effect of narrow band ultraviolet B phototherapy as monotherapy or combination therapy for vitiligo: a meta-analysis. Photodermatol Photoimmunol Photomed. 2017;33(1):22–31. https://doi.org/10.1111/phpp.12277.
Nordal EJ, Guleng GE, Rönnevig JR. Treatment of vitiligo with narrowband-UVB (TL01) combined with tacrolimus ointment (0.1%) vs. placebo ointment, a randomized right/left double-blind comparative study. J Eur Acad Dermatol Venereol. 2011;25(12):1440–3. https://doi.org/10.1111/j.1468-3083.2011.04002.x.
Bae JM, Hong BY, Lee JH, Lee JH, Kim GM. The efficacy of 308-nm excimer laser/light (EL) and topical agent combination therapy versus EL monotherapy for vitiligo: a systematic review and meta-analysis of randomized controlled trials (RCTs). J Am Acad Dermatol. 2016;74(5):907–15. https://doi.org/10.1016/j.jaad.2015.11.044.
Iraji F, Asilian A, Talebzadeh Z, Saber M, Mokhtari F, Siadat A, Hosseini SM. Microneedling in combination with topical pimecrolimus 1% versus topical pimecrolimus 1% for the treatment of refractory stable vitiligo: a randomized clinical trial. Dermatol Res Pract. 2021;2021:5652140. https://doi.org/10.1155/2021/5652140.
Hu M, Liao K, Lei W, Zhang R, Tu C. The addition of topical calcipotriol to phototherapy enhance the efficacy of treatment in patients with vitiligo: a systematic review and meta-analysis. Int Immunopharmacol. 2021;98: 107910. https://doi.org/10.1016/j.intimp.2021.107910.
Liu X, Yao Z, Wang Y, Chai L, Zhou X. Vitamin D analogs combined with different types of phototherapy in the treatment of vitiligo: a systematic review of randomized trials and within-patient studies. Int Immunopharmacol. 2022;109: 108789. https://doi.org/10.1016/j.intimp.2022.108789.
Juntongjin P, Sangganjanavanich P. Efficacy of the combined excimer light and topical calcipotriol for acral vitiligo: a randomized double-blind comparative study. Dermatol Ther. 2021;34(2): e14886. https://doi.org/10.1111/dth.14886.
Batchelor JM, Thomas KS, Akram P, Azad J, Bewley A, Chalmers JR, Cheung ST, Duley L, Eleftheriadou V, Ellis R, Ferguson A, Goulding JM, Haines RH, Hamad H, Ingram JR, Laguda B, Leighton P, Levell N, Makrygeorgou A, Meakin GD, Millington A, Ogboli M, Rajasekaran A, Ravenscroft JC, Rogers A, Sach TH, Santer M, Stainforth J, Tan W, Wahie S, White J, Whitton ME, Williams HC, Wright A, Montgomery AA. Home-based narrowband UVB, topical corticosteroid or combination for children and adults with vitiligo: HI-Light Vitiligo three-arm RCT. Health Technol Assess. 2020;24(64):1–128. https://doi.org/10.3310/hta24640.
El Mofty M, Essmat S, Youssef R, Sobeih S, Mahgoub D, Ossama S, Saad A, El Tawdy A, Mashaly HM, Saney I, Helal R, Shaker O. The role of systemic steroids and phototherapy in the treatment of stable vitiligo: a randomized controlled trial. Dermatol Ther. 2016;29(6):406–12. https://doi.org/10.1111/dth.12384.
Esmat SM, El-Mofty M, Rasheed H, Mostafa WZ, Anbar TS, Abdallah M, Bassiouny D, Abdel-Halim D, Hegazy R, Eid AA, Nassar A, Abdel-Aziz RT, Fawzy MM, Gawdat HI, El Hawary M, Sany I, Shalaby S, Ragab N, Abdel-Gaber RM, Tawfik YM, El-Bassiouny M, El-Husseiny R, Attia MS, Farid C, Genedy RM, Mogawer RM. Efficacy of narrow band UVB with or without OMP in stabilization of vitiligo activity in skin photo-types (III-V): a double-blind, randomized, placebo-controlled, prospective, multicenter study. Photodermatol Photoimmunol Photomed. 2022;38(3):277–87. https://doi.org/10.1111/phpp.12749.
Tovar-Garza A, Hinojosa JA, Hynan LS, Pandya AG. Addition of oral minipulse dexamethasone to narrowband ultraviolet B phototherapy and topical steroids helps arrest disease activity in patients with vitiligo. Br J Dermatol. 2019;180(1):193–4. https://doi.org/10.1111/bjd.17150(Erratum in: Br J Dermatol. 2020;182(5):1318).
Lee J, Chu H, Lee H, Kim M, Kim DS, Oh SH. A Retrospective study of methylprednisolone mini-pulse therapy combined with narrow-band UVB in non-segmental vitiligo. Dermatology. 2016;232(2):224–9. https://doi.org/10.1159/000439563.
Mulekar SV, Isedeh P. Surgical interventions for vitiligo: an evidence-based review. Br J Dermatol. 2013;169(Suppl 3):57–66. https://doi.org/10.1111/bjd.12532.
Rodrigues M, Ezzedine K, Hamzavi I, Pandya AG, Harris JE, Vitiligo Working Group. Current and emerging treatments for vitiligo. J Am Acad Dermatol. 2017;77(1):17–29. https://doi.org/10.1016/j.jaad.2016.11.010.
Ju HJ, Bae JM, Lee RW, Kim SH, Parsad D, Pourang A, Hamzavi I, Shourick J, Ezzedine K. Surgical interventions for patients with vitiligo: a systematic review and meta-analysis. JAMA Dermatol. 2021;157(3):307–16. https://doi.org/10.1001/jamadermatol.2020.5756.
Mohammad TF, Hamzavi IH. Surgical therapies for vitiligo. Dermatol Clin. 2017;35(2):193–203. https://doi.org/10.1016/j.det.2016.11.009.
Feetham HJ, Chan JL, Pandya AG. Characterization of clinical response in patients with vitiligo undergoing autologous epidermal punch grafting. Dermatol Surg. 2012;38(1):14–9. https://doi.org/10.1111/j.1524-4725.2011.02171.x.
Fongers A, Wolkerstorfer A, Nieuweboer-Krobotova L, Krawczyk P, Tóth GG, van der Veen JP. Long-term results of 2-mm punch grafting in patients with vitiligo vulgaris and segmental vitiligo: effect of disease activity. Br J Dermatol. 2009;161(5):1105–11. https://doi.org/10.1111/j.1365-2133.2009.09367.x.
Bae JM, Lee JH, Kwon HS, Kim J, Kim DS. Motorized 0.8-mm micropunch grafting for refractory vitiligo: a retrospective study of 230 cases. J Am Acad Dermatol. 2018;79(4):720-727.e1. https://doi.org/10.1016/j.jaad.2018.06.016.
Kim JC, Kim DC, Kang HY, Kim DS. Treatment outcomes and prognostic factors of motorized 0.5-mm micropunch grafting with a skin-seeding technique for 83 cases of vitiligo in children. J Am Acad Dermatol. 2022. https://doi.org/10.1016/j.jaad.2022.07.021.
Ragab M, El Zagh O, Farid C. Transverse needling after autologous mini-punch grafts improves repigmentation in stable non-segmental vitiligo. Clin Cosmet Investig Dermatol. 2021;14:827–35. https://doi.org/10.2147/CCID.S315407.
McCrary MR, Gibbs DC, Alharthi M, Krueger LD. Utilization of our toolkit: a systematic review and meta-analysis of surgical therapies in vitiligo treatment. Dermatol Surg. 2022;48(8):815–21. https://doi.org/10.1097/DSS.0000000000003503.
Nanda S, Relhan V, Grover C, Reddy BS. Suction blister epidermal grafting for management of eyelid vitiligo: special considerations. Dermatol Surg. 2006;32(3):387–91. https://doi.org/10.1111/j.1524-4725.2006.32078.x.
Gupta S, Goel A, Kanwar AJ, Kumar B. Autologous melanocyte transfer via epidermal grafts for lip vitiligo. Int J Dermatol. 2006;45(6):747–50. https://doi.org/10.1111/j.1365-4632.2006.02694.x.
Kar BR, Raj C. Suction blister epidermal grafting for vitiligo involving angles of lip: experience of 112 patients. J Cutan Aesthet Surg. 2018;11(1):13–9. https://doi.org/10.4103/JCAS.JCAS_111_15.
Kumar A, Mohanty S, Sahni K, Kumar R, Gupta S. Extracted hair follicle outer root sheath cell suspension for pigment cell restoration in vitiligo. J Cutan Aesthet Surg. 2013;6(2):121–5. https://doi.org/10.4103/0974-2077.112679.
Mohanty S, Kumar A, Dhawan J, Sreenivas V, Gupta S. Noncultured extracted hair follicle outer root sheath cell suspension for transplantation in vitiligo. Br J Dermatol. 2011;164(6):1241–6. https://doi.org/10.1111/j.1365-2133.2011.10234.x.
Chen YF, Yang PY, Hu DN, Kuo FS, Hung CS, Hung CM. Treatment of vitiligo by transplantation of cultured pure melanocyte suspension: analysis of 120 cases. J Am Acad Dermatol. 2004;51(1):68–74. https://doi.org/10.1016/j.jaad.2003.12.013.
Hong WS, Hu DN, Qian GP, McCormick SA, Xu AE. Treatment of vitiligo in children and adolescents by autologous cultured pure melanocytes transplantation with comparison of efficacy to results in adults. J Eur Acad Dermatol Venereol. 2011;25(5):538–43. https://doi.org/10.1111/j.1468-3083.2010.03824.x.
Lommerts JE, Uitentuis SE, Bekkenk MW, de Rie MA, Wolkerstorfer A. The role of phototherapy in the surgical treatment of vitiligo: a systematic review. J Eur Acad Dermatol Venereol. 2018;32(9):1427–35. https://doi.org/10.1111/jdv.14950.
Hesseler MJ, Shyam N. Platelet-rich plasma and its utility in medical dermatology: a systematic review. J Am Acad Dermatol. 2019;81(3):834–46. https://doi.org/10.1016/j.jaad.2019.04.037.
Rekik M, Mseddi M, Kammoun N, Sellami K, Turki H. Efficacy of autologous platelet-rich plasma in the treatment of vitiligo: a 10-patient prospective study. J Cosmet Dermatol. 2022. https://doi.org/10.1111/jocd.15050.
Afify AA, Zuelfakkar NM, Eshafi MA. Fractional CO2 laser, platelet rich plasma and narrow band ultraviolet B in the treatment of Vitiligo (a randomized clinical trial). Lasers Med Sci. 2021;36(7):1479–86. https://doi.org/10.1007/s10103-020-03195-9.
Chen J, Wan Y, Lin Y, Jiang H. Current art of combination therapy with autologous platelet-rich plasma for stable vitiligo: a meta-analysis. Int Wound J. 2021;18(3):251–60. https://doi.org/10.1111/iwj.13524.
Deng Y, Li J, Yang G. 308-nm excimer laser plus platelet-rich plasma for treatment of stable vitiligo: a prospective, randomized case-control study. Clin Cosmet Investig Dermatol. 2020;13:461–7. https://doi.org/10.2147/CCID.S260434.
Khattab FM, Abdelbary E, Fawzi M. Evaluation of combined excimer laser and platelet-rich plasma for the treatment of nonsegmental vitiligo: a prospective comparative study. J Cosmet Dermatol. 2020;19(4):869–77. https://doi.org/10.1111/jocd.13103.
Kadry M, Tawfik A, Abdallah N, Badawi A, Shokeir H. Platelet-rich plasma versus combined fractional carbon dioxide laser with platelet-rich plasma in the treatment of vitiligo: a comparative study. Clin Cosmet Investig Dermatol. 2018;11:551–9. https://doi.org/10.2147/CCID.S178817.
Abdelghani R, Ahmed NA, Darwish HM. Combined treatment with fractional carbon dioxide laser, autologous platelet-rich plasma, and narrow band ultraviolet B for vitiligo in different body sites: a prospective, randomized comparative trial. J Cosmet Dermatol. 2018;17(3):365–72. https://doi.org/10.1111/jocd.12397.
Raizada A, Panda M, Singh BS, Kar BR. Fractional carbon dioxide laser versus fractional carbon dioxide laser with autologous intralesional platelet-rich plasma in the treatment of stable, non-segmental vitiligo: a randomized comparative study. J Cutan Aesthet Surg. 2021;14(1):55–63. https://doi.org/10.4103/JCAS.JCAS_188_19.
Mercuri SR, Di Nicola MR, Brianti P, Bianchi VG, Paolino G. Pilot study on the use of the “monocyte-rich” platelet-rich plasma in combination with 1927 nm fractional and 308 nm excimer lasers for the treatment of vitiligo. Medicina (Kaunas). 2021;57(9):904. https://doi.org/10.3390/medicina57090904.
Salem SAM, Fezeaa TA, El Khazragy N, Soltan MY. Effect of platelet-rich plasma on the outcome of mini-punch grafting procedure in localized stable vitiligo: clinical evaluation and relation to lesional basic fibroblast growth factor. Dermatol Ther. 2021;34(2): e14738. https://doi.org/10.1111/dth.14738.
Ibrahim ZA, El-Ashmawy AA, El-Tatawy RA, Sallam FA. The effect of platelet-rich plasma on the outcome of short-term narrowband-ultraviolet B phototherapy in the treatment of vitiligo: a pilot study. J Cosmet Dermatol. 2016;15(2):108–16. https://doi.org/10.1111/jocd.12194.
Yin L, Adotama P, Svigos K, Gutierrez D, Lo SK. Platelet-rich plasma, a promising adjunctive treatment for vitiligo: a case report. JAAD Case Rep. 2020;6(12):1320–2. https://doi.org/10.1016/j.jdcr.2020.09.021.
Parambath N, Sharma VK, Parihar AS, Sahni K, Gupta S. Use of platelet-rich plasma to suspend noncultured epidermal cell suspension improves repigmentation after autologous transplantation in stable vitiligo: a double-blind randomized controlled trial. Int J Dermatol. 2019;58(4):472–6. https://doi.org/10.1111/ijd.14286.
Albalat W, Elsayed M, Salem A, Ehab R, Fawzy M. Non-cultured epidermal cells suspended in either platelet-rich plasma or ringer lactate for stable vitiligo: a prospective comparative study. J Cosmet Dermatol. 2022;21(7):3102–9. https://doi.org/10.1111/jocd.14576.
De Cuyper C. Permanent makeup: indications and complications. Clin Dermatol. 2008;26(1):30–4. https://doi.org/10.1016/j.clindermatol.2007.10.009.
Halder RM, Pham HN, Breadon JY, Johnson BA. Micropigmentation for the treatment of vitiligo. J Dermatol Surg Oncol. 1989;15(10):1092–8. https://doi.org/10.1111/j.1524-4725.1989.tb03129.x.
Mahajan BB, Garg G, Gupta RR. Evaluation of cosmetic tattooing in localised stable vitiligo. J Dermatol. 2002;29(11):726–30. https://doi.org/10.1111/j.1346-8138.2002.tb00210.x.
Eun SH, Lee HN, Kim SH, et al. Micropigmentation for acral vitiligo: an open-label pilot study of 12 patients. Korean J Dermatol. 2020;58:20–5.
Singh AK, Karki D. Micropigmentation: tattooing for the treatment of lip vitiligo. J Plast Reconstr Aesthet Surg. 2010;63(6):988–91. https://doi.org/10.1016/j.bjps.2009.03.013.
Francis A, Criton S, Shojan A, Philip R. Micropigmentation in vitiligo of lateral lower lip. J Cutan Aesthet Surg. 2013;6(4):236–7. https://doi.org/10.4103/0974-2077.123416.
Ju HJ, Eun SH, Lee HN, Lee JH, Kim GM, Bae JM. Micropigmentation for vitiligo on light to moderately colored skin: updated evidence from a clinical and animal study. J Dermatol. 2020;47(5):464–9. https://doi.org/10.1111/1346-8138.15282.
Singh H, Kumaran MS, Bains A, Parsad D. A Randomized comparative study of oral corticosteroid minipulse and low-dose oral methotrexate in the treatment of unstable vitiligo. Dermatology. 2015;231(3):286–90. https://doi.org/10.1159/000433424.
Garza-Mayers AC, Kroshinsky D. Low-dose methotrexate for vitiligo. J Drugs Dermatol. 2017;16(7):705–6.
Ugurer E, Altunay IK, Erdem Y, Ozkur E, Tuncel D. Undesirable repigmentation in vitiligo patient receiving methotrexate therapy for the treatment of psoriasis: treatment or side effect? Dermatol Online J. 2022. https://doi.org/10.5070/D328157067.
Abdelmaksoud A, Dave DD, Lotti T, Vestita M. Topical methotrexate 1% gel for treatment of vitiligo: a case report and review of the literature. Dermatol Ther. 2019;32(5): e13013. https://doi.org/10.1111/dth.13013.
Song X, Xu A, Pan W, Wallin B, Kivlin R, Lu S, Cao C, Bi Z, Wan Y. Minocycline protects melanocytes against H2O2-induced cell death via JNK and p38 MAPK pathways. Int J Mol Med. 2008;22(1):9–16.
Parsad D, Kanwar A. Oral minocycline in the treatment of vitiligo: a preliminary study. Dermatol Ther. 2010;23(3):305–7. https://doi.org/10.1111/j.1529-8019.2010.01328.x.
Singh A, Kanwar AJ, Parsad D, Mahajan R. Randomized controlled study to evaluate the effectiveness of dexamethasone oral minipulse therapy versus oral minocycline in patients with active vitiligo vulgaris. Indian J Dermatol Venereol Leprol. 2014;80(1):29–35. https://doi.org/10.4103/0378-6323.125479.
Siadat AH, Zeinali N, Iraji F, Abtahi-Naeini B, Nilforoushzadeh MA, Jamshidi K, Khosravani P. Narrow-band ultraviolet B versus oral minocycline in treatment of unstable vitiligo: a prospective comparative trial. Dermatol Res Pract. 2014;2014: 240856. https://doi.org/10.1155/2014/240856.
Charoenpongpun N, Kamanamool N, Udompataikul M, Khunkhet S, Kanokrungsee S. A pilot study of combined oral minocycline and narrowband UVB phototherapy in vitiligo: a randomized, double-blind, placebo-controlled trial. Dermatol Ther. 2022;35(8): e15596. https://doi.org/10.1111/dth.15596.
Radmanesh M, Saedi K. The efficacy of combined PUVA and low-dose azathioprine for early and enhanced repigmentation in vitiligo patients. J Dermatolog Treat. 2006;17(3):151–3. https://doi.org/10.1080/09546630600791442.
Patra S, Khaitan BK, Sharma VK, Khanna N. A randomized comparative study of the effect of betamethasone oral mini-pulse therapy versus oral azathioprine in progressive nonsegmental vitiligo. J Am Acad Dermatol. 2021;85(3):728–9. https://doi.org/10.1016/j.jaad.2019.03.025.
Khondker L, Khan SI. Efficacy of levamisole for the treatment of slow spreading vitiligo. Mymensingh Med J. 2013;22(4):761–6.
Agarwal S, Ramam M, Sharma VK, Khandpur S, Pal H, Pandey RM. A randomized placebo-controlled double-blind study of levamisole in the treatment of limited and slowly spreading vitiligo. Br J Dermatol. 2005;153(1):163–6. https://doi.org/10.1111/j.1365-2133.2005.06556.x.
Pasricha JS, Khera V. Effect of prolonged treatment with levamisole on vitiligo with limited and slow-spreading disease. Int J Dermatol. 1994;33(8):584–7. https://doi.org/10.1111/j.1365-4362.1994.tb02903.x.
Majid I, Imran S, Batool S. Apremilast is effective in controlling the progression of adult vitiligo: a case series. Dermatol Ther. 2019;32(4): e12923. https://doi.org/10.1111/dth.12923.
Khemis A, Fontas E, Moulin S, Montaudié H, Lacour JP, Passeron T. Apremilast in combination with narrowband UVB in the treatment of vitiligo: a 52-week monocentric prospective randomized placebo-controlled study. J Investig Dermatol. 2020;140(8):1533-1537.e2. https://doi.org/10.1016/j.jid.2019.11.031.
Kim HJ, Singer GK, Del Duca E, Abittan BJ, Chima MA, Kimmel G, Bares J, Gagliotti M, Genece J, Chu J, Wilding G, Pavel AB, Guttman-Yassky E, Lebwohl MG. Combination of apremilast and narrowband ultraviolet B light in the treatment of generalized vitiligo in skin phototypes IV to VI: a randomized split-body pilot study. J Am Acad Dermatol. 2021;85(6):1657–60. https://doi.org/10.1016/j.jaad.2020.12.073.
Kim HJ, Del Duca E, Pavel AB, Singer GK, Abittan BJ, Chima MA, Kimmel G, Bares J, Baum D, Gagliotti M, Genece J, Chu J, Lebwohl MG, Guttman-Yassky E. Apremilast and narrowband ultraviolet B combination therapy suppresses Th17 axis and promotes melanogenesis in vitiligo skin: a randomized, split-body, pilot study in skin types IV–VI. Arch Dermatol Res. 2022. https://doi.org/10.1007/s00403-022-02343-1.
Dell’Anna ML, Mastrofrancesco A, Sala R, Venturini M, Ottaviani M, Vidolin AP, Leone G, Calzavara PG, Westerhof W, Picardo M. Antioxidants and narrow band-UVB in the treatment of vitiligo: a double-blind placebo controlled trial. Clin Exp Dermatol. 2007;32(6):631–6. https://doi.org/10.1111/j.1365-2230.2007.02514.x.
Jung HM, Jung YS, Lee JH, Kim GM, Bae JM. Antioxidant supplements in combination with phototherapy for vitiligo: a systematic review and metaanalysis of randomized controlled trials. J Am Acad Dermatol. 2021;85(2):506–8. https://doi.org/10.1016/j.jaad.2018.10.010.
Parsad D, Pandhi R, Juneja A. Effectiveness of oral Ginkgo biloba in treating limited, slowly spreading vitiligo. Clin Exp Dermatol. 2003;28(3):285–7. https://doi.org/10.1046/j.1365-2230.2003.01207.x.
Szczurko O, Shear N, Taddio A, Boon H. Ginkgo biloba for the treatment of vitilgo vulgaris: an open label pilot clinical trial. BMC Complement Altern Med. 2011;11:21. https://doi.org/10.1186/1472-6882-11-21.
Gonzalez S, Gilaberte Y, Philips N. Mechanistic insights in the use of a Polypodium leucotomos extract as an oral and topical photoprotective agent. Photochem Photobiol Sci. 2010;9(4):559–63. https://doi.org/10.1039/b9pp00156e.
Reyes E, Jaén P, de las Heras E, Carrión F, Alvarez-Mon M, de Eusebio E, Alvare M, Cuevas J, González S, Villarrubia VG. Systemic immunomodulatory effects of Polypodium leucotomos as an adjuvant to PUVA therapy in generalized vitiligo: a pilot study. J Dermatol Sci. 2006;41(3):213–6. https://doi.org/10.1016/j.jdermsci.2005.12.006.
Pacifico A, Damiani G, Iacovelli P, Conic RRZ, Young Dermatologists Italian Network (YDIN), Gonzalez S, Morrone A. NB-UVB plus oral Polypodium leucotomos extract display higher efficacy than NB-UVB alone in patients with vitiligo. Dermatol Ther. 2021;34(2): e14776. https://doi.org/10.1111/dth.14776.
Middelkamp-Hup MA, Bos JD, Rius-Diaz F, Gonzalez S, Westerhof W. Treatment of vitiligo vulgaris with narrow-band UVB and oral Polypodium leucotomos extract: a randomized double-blind placebo-controlled study. J Eur Acad Dermatol Venereol. 2007;21(7):942–50. https://doi.org/10.1111/j.1468-3083.2006.02132.x.
Phan K, Phan S, Shumack S, Gupta M. Repigmentation in vitiligo using janus kinase (JAK) inhibitors with phototherapy: systematic review and meta-analysis. J Dermatolog Treat. 2022;33(1):173–7. https://doi.org/10.1080/09546634.2020.1735615.
Rosmarin D, Passeron T, Pandya AG, Grimes P, Harris JE, Desai SR, Lebwohl M, Ruer-Mulard M, Seneschal J, Wolkerstorfer A, Kornacki D, Sun K, Butler K, Ezzedine K. Efficacy and safety of ruxolitinib cream monotherapy for the treatment of vitiligo: results from two 52-week phase 3 studies. Presented at the American Academy of Dermatology Annual Meeting, 25–29 March 2022, Boston.
Rosmarin D, Passeron T, Pandya AG, Grimes P, Harris JE, Desai SR, Lebwohl M, Ruer-Mulard M, Seneschal J, Wolkerstorfer A, Kornacki D, Sun K, Butler K, Ezzedine K, TRuE-V Study Group. Two phase 3, randomized, controlled trials of ruxolitinib cream for vitiligo. N Engl J Med. 2022;387(16):1445–55. https://doi.org/10.1056/NEJMoa2118828.
Rosmarin D, Pandya AG, Lebwohl M, Grimes P, Hamzavi I, Gottlieb AB, Butler K, Kuo F, Sun K, Ji T, Howell MD, Harris JE. Ruxolitinib cream for treatment of vitiligo: a randomised, controlled, phase 2 trial. Lancet. 2020;396(10244):110–20. https://doi.org/10.1016/S0140-6736(20)30609-7.
Harris JE, Pandya AG, Lebwohl M, Hamzavi IH, Grimes P, Gottlieb AB, Sofen HL, Moore AY, Wang M, Kornacki D, Butler K, Rosmarin D. Safety and efficacy of ruxolitinib cream for the treatment of vitiligo: 156-week data from a phase 2 study. Presented at the British Association of Dermatologists Annual Meeting, 5–7 July 2022, Glasgow.
Rosmarin D, Ezzedine K, Desai SR, Seneschal J, Kornacki D, Sun K, Butler K, Passeron T. Efficacy and safety of Ruxolitinib cream for the treatment of vitiligo by patient demographics and baseline clinical characteristics: pooled subgroup analysis from two randomized phase 3 studies. Presented at the American Academy of Dermatology Annual Meeting, 25–29 March 2022, Boston.
Rosmarin D, Seneschal J, Grimes P, Desai SR, Pandya AG, Kornacki D, Wang M, Butler K, Ezzedine K. Efficacy and safety of ruxolitinib cream in adolescent patients with vitiligo: pooled analyses of the 52-week TRuE-V phase 3 studies. Presented at the Society for Pediatric Dermatology Annual Meeting, 7–10 July 2022, Indianapolis.
Passeron T, Harris JE, Pandya AG, Seneschal J, Grimes P, Kornacki D, Wang M, Butler K, Ezzedine K, Rosmarin D. Effect of ruxolitinib cream on achievement of VASI50 by body region: week 52 pooled analysis of the TRuE-V phase 3 studies. Presented at the European Academy of Dermatology of Venereology (EADV) Congress, 7–10 September 2022, Milan.
Hamzavi I, Rosmarin D, Harris JE, Pandya AG, Lebwohl M, Gottlieb AB, Butler K, Kuo FI, Sun K, Grimes P. Efficacy of ruxolitinib cream in vitiligo by patient characteristics and affected body areas: descriptive subgroup analyses from a phase 2, randomized, double-blind trial. J Am Acad Dermatol. 2022;86(6):1398–401. https://doi.org/10.1016/j.jaad.2021.05.047.
Rosmarin D, Pandya AG, Grimes P, Lebwohl M, Gottlieb AB, Hamzavi IH, Butler K, Wei S, Rumberger B, Harris JE. Maintenance of repigmentation after discontinuation of ruxolitinib cream in patients with vitiligo. Presented at the European Society for Dermatological Research Annual Meeting, 22–25 September 2021, Virtual.
Nicolaidou E, Antoniou C, Stratigos AJ, Stefanaki C, Katsambas AD. Efficacy, predictors of response, and long-term follow-up in patients with vitiligo treated with narrowband UVB phototherapy. J Am Acad Dermatol. 2007;56(2):274–8. https://doi.org/10.1016/j.jaad.2006.09.004.
Joshipura D, Alomran A, Zancanaro P, Rosmarin D. Treatment of vitiligo with the topical Janus kinase inhibitor ruxolitinib: a 32-week open-label extension study with optional narrow-band ultraviolet B. J Am Acad Dermatol. 2018;78(6):1205-1207.e1. https://doi.org/10.1016/j.jaad.2018.02.023.
Olamiju B, Craiglow BG. Tofacitinib cream plus narrowband ultraviolet B phototherapy for segmental vitiligo in a child. Pediatr Dermatol. 2020;37(4):754–5. https://doi.org/10.1111/pde.14159.
Pandya AG, Harris JE, Lebwohl M, Hamzavi IH, Butler K, Kuo FI, Wei S, Rosmarin D. Addition of narrow-band UVB phototherapy to ruxolitinib cream in patients with vitiligo. J Investig Dermatol. 2022. https://doi.org/10.1016/j.jid.2022.05.1093.
Craiglow BG, King BA. Tofacitinib citrate for the treatment of vitiligo: a pathogenesis-directed therapy. JAMA Dermatol. 2015;151(10):1110–2. https://doi.org/10.1001/jamadermatol.2015.1520.
Vu M, Heyes C, Robertson SJ, Varigos GA, Ross G. Oral tofacitinib: a promising treatment in atopic dermatitis, alopecia areata and vitiligo. Clin Exp Dermatol. 2017;42(8):942–4. https://doi.org/10.1111/ced.13290.
Komnitski M, Komnitski A, Komnitski Junior A, Silva de Castro CC. Partial repigmentation of vitiligo with tofacitinib, without exposure to ultraviolet radiation. An Bras Dermatol. 2020;95(4):473–6. https://doi.org/10.1016/j.abd.2019.08.032.
Moore AY, Cepica T, Maberry S. Amelioration of unstable vitiligo and normalization of thryroglobulin antibodies with oral tofacitinib. JAAD Case Rep. 2022;23:64–6. https://doi.org/10.1016/j.jdcr.2022.02.025.
Dong J, Huang X, Ma LP, Qi F, Wang SN, Zhang ZQ, Wei SN, Gao L, Liu F. Baricitinib is effective in treating progressing vitiligo in vivo and in vitro. Dose Response. 2022;20(2): 15593258221105370. https://doi.org/10.1177/15593258221105370.
Mumford BP, Gibson A, Chong AH. Repigmentation of vitiligo with oral baricitinib. Australas J Dermatol. 2020;61(4):374–6. https://doi.org/10.1111/ajd.13348.
Harris JE, Rashighi M, Nguyen N, Jabbari A, Ulerio G, Clynes R, Christiano AM, Mackay-Wiggan J. Rapid skin repigmentation on oral ruxolitinib in a patient with coexistent vitiligo and alopecia areata (AA). J Am Acad Dermatol. 2016;74(2):370–1. https://doi.org/10.1016/j.jaad.2015.09.073.
Ezzedine, K, Peeva E, Yamaguchi Y, Cox LA, Banerjee A, Han G, Hamzavi I, Ganesan AK, Picardo M, Thaci D, Harris JE, Bae JM, Tsukamoto K, Sinclair R, Pandya AG, Sloan A, Yu D, Gandhi K, Vincent MS, King B. Efficacy and safety of the oral kanus kinase 3/TEC inhibitor ritlecitinib (PF-06651600) in adults with active non-segmental vitiligo: results from a phase 2b, randomized, dose-ranging study with an extension period. Presented at the European Academy of Dermatology and Venereology Congress, 29 September–2 October 2021.
Liu LY, Strassner JP, Refat MA, Harris JE, King BA. Repigmentation in vitiligo using the Janus kinase inhibitor tofacitinib may require concomitant light exposure. J Am Acad Dermatol. 2017;77(4):675-682.e1. https://doi.org/10.1016/j.jaad.2017.05.043.
Kim SR, Heaton H, Liu LY, King BA. Rapid repigmentation of vitiligo using tofacitinib plus low-dose, narrowband UV-B phototherapy. JAMA Dermatol. 2018;154(3):370–1. https://doi.org/10.1001/jamadermatol.2017.5778.
Gianfaldoni S, Tchernev G, Wollina U, Roccia MG, Fioranelli M, Lotti J, Rovesti M, Satolli F, Valle Y, Goren A, Tirant M, Situm M, Kovacevic M, França K, Lotti T. Micro-focused phototherapy associated to janus kinase inhibitor: a promising valid therapeutic option for patients with localized vitiligo. Open Access Maced J Med Sci. 2018;6(1):46–8. https://doi.org/10.3889/oamjms.2018.042.
Tajalli M, Kabir S, Vance TM, Qureshi AA. Effective use of oral tofacitinib and phototherapy in a patient with concomitant alopecia areata, vitiligo, and plaque and inverse psoriasis. Clin Case Rep. 2020;8(5):819–22. https://doi.org/10.1002/ccr3.2759.
Elmariah SB, Smith JS, Merola JF. JAK in the [black] box: a dermatology perspective on systemic JAK inhibitor safety. Am J Clin Dermatol. 2022;23(4):427–31. https://doi.org/10.1007/s40257-022-00701-3.
Yang BJ, Fan SR, Zhang XF, Cai JY, Ruan T, Xiang ZR, Ren J, Hao XJ, Chen DZ. Design, synthesis and structure-activity relationship optimization of phenanthridine derivatives as new anti-vitiligo compounds. Bioorg Chem. 2022;119: 105582. https://doi.org/10.1016/j.bioorg.2021.105582.
Zou DP, Chen YM, Zhang LZ, Yuan XH, Zhang YJ, Inggawati A, Kieu Nguyet PT, Gao TW, Chen J. SFRP5 inhibits melanin synthesis of melanocytes in vitiligo by suppressing the Wnt/β-catenin signaling. Genes Dis. 2020;8(5):677–88. https://doi.org/10.1016/j.gendis.2020.06.003.
Mosenson JA, Zloza A, Nieland JD, Garrett-Mayer E, Eby JM, Huelsmann EJ, Kumar P, Denman CJ, Lacek AT, Kohlhapp FJ, Alamiri A, Hughes T, Bines SD, Kaufman HL, Overbeck A, Mehrotra S, Hernandez C, Nishimura MI, Guevara-Patino JA, Le Poole IC. Mutant HSP70 reverses autoimmune depigmentation in vitiligo. Sci Transl Med. 2013;5(174): 174ra28. https://doi.org/10.1126/scitranslmed.3005127.
Prajapati K, Perez C, Rojas LBP, Burke B, Guevara-Patino JA. Functions of NKG2D in CD8+ T cells: an opportunity for immunotherapy. Cell Mol Immunol. 2018;15(5):470–9. https://doi.org/10.1038/cmi.2017.161.
Chatterjee S, Eby JM, Al-Khami AA, Soloshchenko M, Kang HK, Kaur N, Naga OS, Murali A, Nishimura MI, Caroline Le Poole I, Mehrotra S. A quantitative increase in regulatory T cells controls development of vitiligo. J Investig Dermatol. 2014;134(5):1285–94. https://doi.org/10.1038/jid.2013.540.
Tulic MK, Cavazza E, Cheli Y, Jacquel A, Luci C, Cardot-Leccia N, Hadhiri-Bzioueche H, Abbe P, Gesson M, Sormani L, Regazzetti C, Beranger GE, Lereverend C, Pons C, Khemis A, Ballotti R, Bertolotto C, Rocchi S, Passeron T. Innate lymphocyte-induced CXCR3B-mediated melanocyte apoptosis is a potential initiator of T-cell autoreactivity in vitiligo. Nat Commun. 2019;10(1):2178. https://doi.org/10.1038/s41467-019-09963-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kaitlynne N. Cunningham declares no conflicts of interest. David Rosmarin has received honoraria as a consultant for AbbVie, Abcuro, AltruBio, Arena, Boehringer-Ingelheim, Bristol Myers Squibb, Celgene, Concert, CSL Behring, Dermavant, Dermira, Incyte, Janssen, Kyowa Kirin, Lilly, Novartis, Pfizer, Regeneron, Revolo Biotherapeutics, Sanofi, Sun Pharmaceuticals, UCB, and VielaBio; has received research support from AbbVie, Amgen, Bristol Myers Squibb, Celgene, Dermira, Galderma, Incyte, Janssen, Lilly, Merck, Novartis, Pfizer, and Regeneron Pharmaceuticals Inc; and has served as a paid speaker for AbbVie, Amgen, Bristol Myers Squibb, Celgene, Incyte, Janssen, Lilly, Novartis, Pfizer, Regeneron Pharmaceuticals Inc., and Sanofi.
Funding
Not applicable.
Ethics approval
Not applicable.
Patient consent to participate/publish
Not applicable.
Data availability
Not applicable.
Code availability
Not applicable.
Author contributions
Kaitlynne N. Cunningham wrote the manuscript, completed the literature review, edited the manuscript, and read and approved the final version of the manuscript for publication. David Rosmarin supervised the work, critically reviewed and edited the manuscript, and read and approved the final version of the manuscript for publication.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cunningham, K.N., Rosmarin, D. Vitiligo Treatments: Review of Current Therapeutic Modalities and JAK Inhibitors. Am J Clin Dermatol 24, 165–186 (2023). https://doi.org/10.1007/s40257-022-00752-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-022-00752-6