Abstract
Improved repigmentation of generalized vitiligo in skin types IV–VI has been reported in clinical response to combined therapy with apremilast and narrowband (NB)-UVB; however, tissue responses to combined therapy versus NB-UVB monotherapy have not been elucidated. We compared the change from baseline in cellular and molecular markers in vitiligo skin after combined therapy versus NB-UVB monotherapy. We assessed lesional and nonlesional skin samples from enrolled subjects and evaluated for immune infiltrates, inflammatory, and melanogenesis-related markers which were compared across different treatment groups. Combined therapy resulted in significant reduction of CD8+T cells and CD11c+ dendritic cells, downregulation of PDE4B and Th17-related markers, and upregulation of melanogenesis markers. This study was limited to small sample size, skin types IV–VI, and high dropout rate. Our molecular findings support the clinical analysis that apremilast may potentiate NB-UVB in repigmentation of generalized vitiligo in skin types IV–VI.




Similar content being viewed by others
References
Taïeb A, Picardo M (2007) The definition and assessment of vitiligo: a consensus report of the Vitiligo European Task Force. Pigment Cell Res 20(1):27–35
Conic RZ, Tamashunas NL, Damiani G, Fabbrocini G, Cantelli M, Bergfeld WF (2020) Comorbidities in pediatric alopecia areata. J Eur Acad Dermatol Venereol 34(12):2898–2901
Malerba M, Damiani G, Radaeli A, Ragnoli B, Olivini A, Calzavara-Pinton PG (2015) Narrowband ultraviolet B phototherapy in psoriasis reduces proinflammatory cytokine levels and improves vitiligo and neutrophilic asthma. Br J Dermatol 173(6):1544–1545
Mineiro Dos Santos Garrett NF, Carvalho da Costa AC, Barros Ferreira E, Damiani G, Diniz Dos Reis PE, Inocêncio Vasques C. Prevalence of dermatological toxicities in patients with melanoma undergoing immunotherapy: Systematic review and meta-analysis. PLoS One. 2021;16(8):e0255716.
Ciccarese G, Drago F, Boldrin S, Pattaro M, Parodi A (2022) Sudden onset of vitiligo after COVID-19 vaccine. Dermatol Ther. 35(1):e15196
Kotobuki Y, Tanemura A, Yang L, Itoi S, Wataya-Kaneda M, Murota H et al (2012) Dysregulation of melanocyte function by Th17-related cytokines: significance of Th17 cell infiltration in autoimmune vitiligo vulgaris. Pigment Cell Melanoma Res 25(2):219–230
Antonelli A, Ferrari SM, Fallahi P (2015) The role of the Th1 chemokine CXCL10 in vitiligo. Ann Transl Med 3(Suppl 1):S16
Sushama S, Dixit N, Gautam RK, Arora P, Khurana A, Anubhuti A (2019) Cytokine profile (IL-2, IL-6, IL-17, IL-22, and TNF-α) in vitiligo-New insight into pathogenesis of disease. J Cosmet Dermatol 18(1):337–341
Wang CQ, Cruz-Inigo AE, Fuentes-Duculan J, Moussai D, Gulati N, Sullivan-Whalen M et al (2011) Th17 cells and activated dendritic cells are increased in vitiligo lesions. PLoS One. 6(4):e18907
Zhou L, Shi YL, Li K, Hamzavi I, Gao TW, Huggins RH et al (2015) Increased circulating Th17 cells and elevated serum levels of TGF-beta and IL-21 are correlated with human non-segmental vitiligo development. Pigment Cell Melanoma Res 28(3):324–329
Richmond JM, Bangari DS, Essien KI, Currimbhoy SD, Groom JR, Pandya AG et al (2017) Keratinocyte-derived chemokines orchestrate T-Cell positioning in the epidermis during vitiligo and may serve as biomarkers of disease. J Invest Dermatol 137(2):350–358
Harris JE, Harris TH, Weninger W, Wherry EJ, Hunter CA, Turka LA (2012) A mouse model of vitiligo with focused epidermal depigmentation requires IFN-γ for autoreactive CD8+ T-cell accumulation in the skin. J Invest Dermatol. 132(7):1869–76
Khemis A, Fontas E, Moulin S, Montaudié H, Lacour JP, Passeron T (2020) Apremilast in combination with narrowband UVB in the treatment of vitiligo: a 52-week monocentric prospective randomized placebo-controlled study. J Invest Dermatol 140(8):1533–7.e2
Wang XX, Wang QQ, Wu JQ, Jiang M, Chen L, Zhang CF et al (2016) Increased expression of CXCR3 and its ligands in patients with vitiligo and CXCL10 as a potential clinical marker for vitiligo. Br J Dermatol 174(6):1318–1326
Tulic MK, Cavazza E, Cheli Y, Jacquel A, Luci C, Cardot-Leccia N et al (2019) Innate lymphocyte-induced CXCR3B-mediated melanocyte apoptosis is a potential initiator of T-cell autoreactivity in vitiligo. Nat Commun 10(1):2178
Orihara K (2021) Skin and immune cells crosstalk via circadian regulations. Explor Immunol 1(4):285–294
Yu X, Rollins D, Ruhn KA, Stubblefield JJ, Green CB, Kashiwada M et al (2013) TH17 cell differentiation is regulated by the circadian clock. Science 342(6159):727–730
Guerra L, Dellambra E, Brescia S, Raskovic D (2010) Vitiligo: pathogenetic hypotheses and targets for current therapies. Curr Drug Metab 11(5):451–467
Njoo MD, Westerhof W, Bos JD, Bossuyt PM (1999) The development of guidelines for the treatment of vitiligo. Clinical epidemiology unit of the Istituto Dermopatico dell’Immacolata-Istituto di Recovero e Cura a Carattere Scientifico (IDI-IRCCS) and the archives of dermatology. Arch Dermatol. 135(12):1514–21
Kanwar AJ, Dogra S, Parsad D, Kumar B (2005) Narrow-band UVB for the treatment of vitiligo: an emerging effective and well-tolerated therapy. Int J Dermatol 44(1):57–60
Parsad D, Kanwar AJ, Kumar B (2006) Psoralen-ultraviolet A vs. narrow-band ultraviolet B phototherapy for the treatment of vitiligo. J Eur Acad Dermatol Venereol. 20(2):175–7
Li R, Qiao M, Wang X, Zhao X, Sun Q (2017) Effect of narrow band ultraviolet B phototherapy as monotherapy or combination therapy for vitiligo: a meta-analysis. Photodermatol Photoimmunol Photomed 33(1):22–31
Relke N, Gooderham M (2019) The use of janus kinase inhibitors in vitiligo: a review of the literature. J Cutan Med Surg 23(3):298–306
Liu LY, Strassner JP, Refat MA, Harris JE, King BA (2017) Repigmentation in vitiligo using the Janus kinase inhibitor tofacitinib may require concomitant light exposure. J Am Acad Dermatol 77(4):675–82.e1
Craiglow BG, King BA (2015) Tofacitinib citrate for the treatment of vitiligo: a pathogenesis-directed therapy. JAMA Dermatol 151(10):1110–1112
Schafer PH, Parton A, Gandhi AK, Capone L, Adams M, Wu L et al (2010) Apremilast, a cAMP phosphodiesterase-4 inhibitor, demonstrates anti-inflammatory activity in vitro and in a model of psoriasis. Br J Pharmacol 159(4):842–855
Gottlieb AB, Strober B, Krueger JG, Rohane P, Zeldis JB, Hu CC et al (2008) An open-label, single-arm pilot study in patients with severe plaque-type psoriasis treated with an oral anti-inflammatory agent, apremilast. Curr Med Res Opin 24(5):1529–1538
Kavanaugh A, Gladman DD, Edwards CJ, Schett G, Guerette B, Delev N et al (2019) Long-term experience with apremilast in patients with psoriatic arthritis: 5-year results from a PALACE 1–3 pooled analysis. Arthritis Res Ther 21(1):118
Hatemi G, Melikoglu M, Tunc R, Korkmaz C, Turgut Ozturk B, Mat C et al (2015) Apremilast for Behçet’s syndrome–a phase 2, placebo-controlled study. N Engl J Med 372(16):1510–1518
Perez-Aso M, Montesinos MC, Mediero A, Wilder T, Schafer PH, Cronstein B (2015) Apremilast, a novel phosphodiesterase 4 (PDE4) inhibitor, regulates inflammation through multiple cAMP downstream effectors. Arthritis Res Ther 17(1):249
Gottlieb AB, Matheson RT, Menter A, Leonardi CL, Day RM, Hu C et al (2013) Efficacy, tolerability, and pharmacodynamics of apremilast in recalcitrant plaque psoriasis: a phase II open-label study. J Drugs Dermatol 12(8):888–897
Schafer PH, Parton A, Capone L, Cedzik D, Brady H, Evans JF et al (2014) Apremilast is a selective PDE4 inhibitor with regulatory effects on innate immunity. Cell Signal 26(9):2016–2029
Khaled M, Levy C, Fisher DE (2010) Control of melanocyte differentiation by a MITF-PDE4D3 homeostatic circuit. Genes Dev 24(20):2276–2281
D’Orazio JA, Nobuhisa T, Cui R, Arya M, Spry M, Wakamatsu K et al (2006) Topical drug rescue strategy and skin protection based on the role of Mc1r in UV-induced tanning. Nature 443(7109):340–344
Majid I, Imran S, Batool S (2019) Apremilast is effective in controlling the progression of adult vitiligo: A case series. Dermatol Ther. 32(4):e12923
Huff SB, Gottwald LD (2017) Repigmentation of Tenacious Vitiligo on Apremilast. Case Rep Dermatol Med 2017:2386234
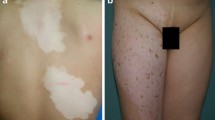
Kim HJ, Singer G, Abittan BJ, Chima MA, Kimmel G, Bares J et al (2021) Combination of apremilast and narrowband ultraviolet B light in the treatment of generalized vitiligo in skin phototypes IV to VI: A randomized split-body pilot study. J Am Acad Dermatol. 85(6):1657–1660
Saternus R, Pilz S, Gräber S, Kleber M, März W, Vogt T et al (2015) A closer look at evolution: Variants (SNPs) of genes involved in skin pigmentation, including EXOC2, TYR, TYRP1, and DCT, are associated with 25(OH)D serum concentration. Endocrinology 156(1):39–47
Seberg HE, Van Otterloo E, Cornell RA (2017) Beyond MITF: Multiple transcription factors directly regulate the cellular phenotype in melanocytes and melanoma. Pigment Cell Melanoma Res 30(5):454–466
Bianchi L, Del Duca E, Romanelli M, Saraceno R, Chimenti S, Chiricozzi A (2016) Pharmacodynamic assessment of apremilast for the treatment of moderate-to-severe plaque psoriasis. Expert Opin Drug Metab Toxicol 12(9):1121–1128
Alonso S, Izagirre N, Smith-Zubiaga I, Gardeazabal J, Díaz-Ramón JL, Díaz-Pérez JL et al (2008) Complex signatures of selection for the melanogenic loci TYR, TYRP1 and DCT in humans. BMC Evol Biol 8:74
Wehrle-Haller B (2003) The role of Kit-ligand in melanocyte development and epidermal homeostasis. Pigment Cell Res 16(3):287–296
Lim HW, Grimes PE, Agbai O, Hamzavi I, Henderson M, Haddican M et al (2015) Afamelanotide and narrowband UV-B phototherapy for the treatment of vitiligo: a randomized multicenter trial. JAMA Dermatol 151(1):42–50
Papp K, Reich K, Leonardi CL, Kircik L, Chimenti S, Langley RG et al (2015) Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: Results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol 73(1):37–49
Paul C, Cather J, Gooderham M, Poulin Y, Mrowietz U, Ferrandiz C et al (2015) Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol 173(6):1387–1399
Acknowledgements
This study received funding from Celgene Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Lebwohl has received research funds from Abbvie, Amgen, Arcutis, AstraZeneca, Boehringer Ingelheim, Celgene, Clinuvel, Corrona.Inc, Eli Lilly, Foundation for Research & Education in Dermatology, Incyte, Janssen Research & Development, Kadmon Corp, Leo Pharmaceuticals, MedImmune, Novartis, Ortho Dermatologics, Pfizer, Sciderm, UCB.Inc, and ViDac, and is a consultant for Allergan, Almirall, Arcutis, Boehringer Ingelheim, Bristol-Myers Squibb, Castle Biosciences, Leo Pharma, Menlo, Mitsubishi, Neuroderm, Pfizer, Promius/Dr. Reddy's Laboratories, Theravance, and Verrica. Dr. Guttman has received research funds from Abbvie, Celgene, Eli Lilly, Janssen, MedImmune/AstraZeneca, Novartis, Pfizer, Regeneron, Vitae, Glenmark, Galderma, Asana, Innovaderm, Dermira and UCB, and is also a consultant for Sanofi Aventis, Regeneron, Stiefel/GlaxoSmithKline, MedImmune, Celgene, Anacor, AnaptysBio, Dermira, Galderma, Glenmark, Novartis, Pfizer, Vitae, Leo Pharma, Abbvie, Eli Lilly, Kyowa, Mitsubishi Tanabe, Asana Biosciences, and Promius. Other authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H.J., Del Duca, E., Pavel, A.B. et al. Apremilast and narrowband ultraviolet B combination therapy suppresses Th17 axis and promotes melanogenesis in vitiligo skin: a randomized, split-body, pilot study in skin types IV–VI. Arch Dermatol Res 315, 215–221 (2023). https://doi.org/10.1007/s00403-022-02343-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-022-02343-1