Abstract
Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the gastrointestinal (GI) tract that is subdivided into Crohn’s disease (CD) and ulcerative colitis (UC). CD is characterized by involvement of the entire GI tract, while UC mainly affects the distal GI tract. Moreover, both CD and UC can present with extraintestinal manifestations (EIMs) of the disease affecting multiple organ systems including the hepatobiliary tract, kidney, bones, eyes, joints, and skin. These complications can cause significant morbidity and negatively impact the quality of life for IBD patients. Although the pathogenesis of EIMs is not clearly elucidated, it is postulated that the diseased GI mucosa similarly stimulates excess immune responses at the extraintestinal sites. Cutaneous EIMs occur in up to 15% of patients with IBD, often predating their IBD diagnosis. They are categorized into (1) specific, (2) reactive, (3) associated, and (4) treatment-induced. Here, we review the epidemiological, clinical, diagnostic, and histologic features of the most commonly described cutaneous EIMs of IBD along with their respective treatment options.



Similar content being viewed by others
References
McDowell CFU, Haseeb M. Inflammatory Bowel Disease. [Updated 2021 Aug 31]. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing, https://www.ncbi.nlm.nih.gov/books/NBK470312/.
Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12(4):205–17.
Windsor JW, Kaplan GG. Evolving epidemiology of IBD. Curr Gastroenterol Rep. 2019;21(8):40.
Aniwan S, Harmsen WS, Tremaine WJ, Loftus EV. Incidence of inflammatory bowel disease by race and ethnicity in a population-based inception cohort from 1970 through 2010. Therap Adv Gastroenterol. 2019;12:1756284819827692.
Sonnenberg A, McCarty DJ, Jacobsen SJ. Geographic variation of inflammatory bowel disease within the United States. Gastroenterology. 1991;100(1):143–9.
Calkins BM, Lilienfeld AM, Garland CF, Mendeloff AI. Trends in incidence rates of ulcerative colitis and Crohn’s disease. Dig Dis Sci. 1984;29(10):913–20.
Roth MP, Petersen GM, McElree C, Feldman E, Rotter JI. Geographic origins of Jewish patients with inflammatory bowel disease. Gastroenterology. 1989;97(4):900–4.
StatPearls. 2021.
van Wijk F, Cheroutre H. Mucosal T cells in gut homeostasis and inflammation. Expert Rev Clin Immunol. 2010;6(4):559–66.
Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448(7152):427–34.
Das KM, Vecchi M, Sakamaki S. A shared and unique epitope(s) on human colon, skin, and biliary epithelium detected by a monoclonal antibody. Gastroenterology. 1990;98(2):464–9.
Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(8):1982–92.
Levine JS, Burakoff R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol (NY). 2011;7(4):235–41.
Vavricka SR, Rogler G, Gantenbein C, Spoerri M, Prinz Vavricka M, Navarini AA, et al. Chronological order of appearance of extraintestinal manifestations relative to the time of IBD diagnosis in the Swiss inflammatory bowel disease cohort. Inflamm Bowel Dis. 2015;21(8):1794–800.
Huang BL, Chandra S, Shih DQ. Skin manifestations of inflammatory bowel disease. Front Physiol. 2012;3:13.
Panackel C, John J, Krishnadas D, Vinayakumar KR. Metastatic Crohn’s disease of external genitalia. Indian J Dermatol. 2008;53(3):146–8.
Lauritano D, Boccalari E, Di Stasio D, Della Vella F, Carinci F, Lucchese A, et al. Prevalence of oral lesions and correlation with intestinal symptoms of inflammatory bowel disease: a systematic review. Diagnostics (Basel). 2019;9(3):77.
Laube R, Liu K, Schifter M, Yang JL, Suen MK, Leong RW. Oral and upper gastrointestinal Crohn’s disease. J Gastroenterol Hepatol. 2018;33(2):355–64.
Grave B, McCullough M, Wiesenfeld D. Orofacial granulomatosis—a 20-year review. Oral Dis. 2009;15(1):46–51.
Lazzerini M, Bramuzzo M, Ventura A. Association between orofacial granulomatosis and Crohn’s disease in children: systematic review. World J Gastroenterol. 2014;20(23):7497–504.
Padmavathi B, Sharma S, Astekar M, Rajan Y, Sowmya G. Oral Crohn’s disease. J Oral Maxillofac Pathol. 2014;18(Suppl 1):S139–42.
Chi AC, Neville BW, Krayer JW, Gonsalves WC. Oral manifestations of systemic disease. Am Fam Physician. 2010;82(11):1381–8.
Lankarani KB, Sivandzadeh GR, Hassanpour S. Oral manifestation in inflammatory bowel disease: a review. World J Gastroenterol. 2013;19(46):8571–9.
Zbar AP, Ben-Horin S, Beer-Gabel M, Eliakim R. Oral Crohn’s disease: is it a separable disease from orofacial granulomatosis? A review. J Crohns Colitis. 2012;6(2):135–42.
Kim SK, Lee ES. Orofacial granulomatosis associated with Crohn’s disease. Ann Dermatol. 2010;22(2):203–5.
Rice SA, Woo PN, El-Omar E, Keenan RA, Ormerod AD. Topical tacrolimus 0.1% ointment for treatment of cutaneous Crohn’s disease. BMC Res Notes. 2013;6:19.
Dupuy A, Cosnes J, Revuz J, Delchier JC, Gendre JP, Cosnes A. Oral Crohn disease: clinical characteristics and long-term follow-up of 9 cases. Arch Dermatol. 1999;135(4):439–42.
Sakuntabhai A, MacLeod RI, Lawrence CM. Intralesional steroid injection after nerve block anesthesia in the treatment of orofacial granulomatosis. Arch Dermatol. 1993;129(4):477–80.
Fedele S, Fung PP, Bamashmous N, Petrie A, Porter S. Long-term effectiveness of intralesional triamcinolone acetonide therapy in orofacial granulomatosis: an observational cohort study. Br J Dermatol. 2014;170(4):794–801.
Campbell HE, Escudier MP, Patel P, Challacombe SJ, Sanderson JD, Lomer MC. Review article: cinnamon- and benzoate-free diet as a primary treatment for orofacial granulomatosis. Aliment Pharmacol Ther. 2011;34(7):687–701.
Espinoza I, Navarrete J, Benedetto J, Borzutzky A, Roessler P, Ortega-Pinto A. Orofacial granulomatosis and diet therapy: a review of the literature and two clinical cases. An Bras Dermatol. 2018;93(1):80–5.
Marzano AV, Borghi A, Stadnicki A, Crosti C, Cugno M. Cutaneous manifestations in patients with inflammatory bowel diseases: pathophysiology, clinical features, and therapy. Inflamm Bowel Dis. 2014;20(1):213–27.
Quezada S, Turner PL, Alexiev B, Daly B, Cross R. Severe refractory orofacial Crohn’s disease: report of a case. Dig Dis Sci. 2009;54(10):2290–5.
Williams DR, Coller JA, Corman ML, Nugent FW, Veidenheimer MC. Anal complications in Crohn’s disease. Dis Colon Rectum. 1981;24(1):22–4.
Sangwan YP, Schoetz DJ, Murray JJ, Roberts PL, Coller JA. Perianal Crohn’s disease. Results of local surgical treatment. Dis Colon Rectum. 1996;39(5):529–35.
Singh B, McC Mortensen NJ, Jewell DP, George B. Perianal Crohn’s disease. Br J Surg. 2004;91(7):801–14.
Safar B, Sands D. Perianal Crohn’s disease. Clin Colon Rectal Surg. 2007;20(4):282–93.
Danese S, Semeraro S, Papa A, Roberto I, Scaldaferri F, Fedeli G, et al. Extraintestinal manifestations in inflammatory bowel disease. World J Gastroenterol. 2005;11(46):7227–36.
Schwartz DA, Tagarro I, Carmen Díez M, Sandborn WJ. Prevalence of fistulizing Crohn’s disease in the United States: estimate from a systematic literature review attempt and population-based database analysis. Inflamm Bowel Dis. 2019;25(11):1773–9.
Sandborn WJ, Fazio VW, Feagan BG, Hanauer SB, Committee AGACP. AGA technical review on perianal Crohn’s disease. Gastroenterology. 2003;125(5):1508–30.
Egal A, London J, Lidove O, Atienza P, Etienney I. Anorectal manifestations in systemic diseases. Rev Med Interne. 2019;40(11):729–32.
Panés J, Rimola J. Perianal fistulizing Crohn’s disease: pathogenesis, diagnosis and therapy. Nat Rev Gastroenterol Hepatol. 2017;14(11):652–64.
Bataille F, Klebl F, Rümmele P, Schroeder J, Farkas S, Wild PJ, et al. Morphological characterisation of Crohn’s disease fistulae. Gut. 2004;53(9):1314–21.
de Zoeten EF, Pasternak BA, Mattei P, Kramer RE, Kader HA. Diagnosis and treatment of perianal Crohn disease: NASPGHAN clinical report and consensus statement. J Pediatr Gastroenterol Nutr. 2013;57(3):401–12.
Ickrath F, Stoevesandt J, Schulmeyer L, Glatzel C, Goebeler M, Kerstan A. Metastatic Crohn’s disease: an underestimated entity. J Dtsch Dermatol Ges. 2021;19(7):973–82.
Shields BE, Richardson C, Arkin L, Kornik R. Vulvar Crohn disease: diagnostic challenges and approach to therapy. Int J Womens Dermatol. 2020;6(5):390–4.
Abboud ME, Frasure SE. Vulvar inflammation as a manifestation of Crohn’s disease. World J Emerg Med. 2017;8(4):305–7.
Bhoyrul B, Lyon C. Crohn’s disease of the vulva: a prospective study. J Gastroenterol Hepatol. 2018;33(12):1969–74.
Barret M, de Parades V, Battistella M, Sokol H, Lemarchand N, Marteau P. Crohn’s disease of the vulva. J Crohns Colitis. 2014;8(7):563–70.
Batra J, Goraya SK, Grewal S, Singh A. Metastatic Crohn’s disease of the vulva: a rare presentation. Indian Dermatol Online J. 2020;11(3):416–8.
Granese R, Calagna G, Morabito G, Carriero C, Perino A, Tonni G, et al. Vulvar involvement in pediatric Crohn’s disease: a systematic review. Arch Gynecol Obstet. 2018;297(1):3–11.
Loftus EV. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004;126(6):1504–17.
Siroy A, Wasman J. Metastatic Crohn disease: a rare cutaneous entity. Arch Pathol Lab Med. 2012;136(3):329–32.
Burgdorf W. Cutaneous manifestations of Crohn’s disease. J Am Acad Dermatol. 1981;5(6):689–95.
Aberumand B, Howard J. Metastatic Crohn’s disease: an approach to an uncommon but important cutaneous disorder. Biomed Res Int. 2017;2017:8192150.
Laftah Z, Bailey C, Zaheri S, Setterfield J, Fuller LC, Lewis F. Vulval Crohn’s disease: a clinical study of 22 patients. J Crohns Colitis. 2015;9(4):318–25.
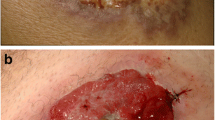
Chakiri R, Baybay H, Hatimi AE, Gallouj S, Harmouch T, Mernissi FZ. Clinical and histological patterns and treatment of pyoderma gangrenosum. Pan Afr Med J. 2020;36:59.
Keyal U, Liu Y, Bhatta AK. Dermatologic manifestations of inflammatory bowel disease: a review. Discov Med. 2018;25(139):225–33.
States V, O’Brien S, Rai JP, Roberts HL, Paas M, Feagins K, et al. Pyoderma gangrenosum in inflammatory bowel disease: a systematic review and meta-analysis. Dig Dis Sci. 2020;65(9):2675–85.
Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal manifestations and complications in inflammatory bowel diseases. World J Gastroenterol. 2006;12(30):4819–31.
Xia FD, Liu K, Lockwood S, Butler D, Tsiaras WG, Joyce C, et al. Risk of developing pyoderma gangrenosum after procedures in patients with a known history of pyoderma gangrenosum—a retrospective analysis. J Am Acad Dermatol. 2018;78(2):310-4.e1.
Powell FC, Su WP, Perry HO. Pyoderma gangrenosum: classification and management. J Am Acad Dermatol. 1996;34(3):395–409 (quiz 10–12).
Brooklyn T, Dunnill G, Probert C. Diagnosis and treatment of pyoderma gangrenosum. BMJ. 2006;333(7560):181–4.
Jockenhöfer F, Wollina U, Salva KA, Benson S, Dissemond J. The PARACELSUS score: a novel diagnostic tool for pyoderma gangrenosum. Br J Dermatol. 2019;180(3):615–20.
Harbord M, Annese V, Vavricka SR, Allez M, Barreiro-de Acosta M, Boberg KM, et al. The first European evidence-based consensus on extra-intestinal manifestations in inflammatory bowel disease. J Crohns Colitis. 2016;10(3):239–54.
Greuter T, Navarini A, Vavricka SR. Skin manifestations of inflammatory bowel disease. Clin Rev Allergy Immunol. 2017;53(3):413–27.
Maverakis E, Marzano AV, Le ST, Callen JP, Brüggen MC, Guenova E, et al. Pyoderma gangrenosum. Nat Rev Dis Primers. 2020;6(1):81.
Marzano AV, Fanoni D, Antiga E, Quaglino P, Caproni M, Crosti C, et al. Expression of cytokines, chemokines and other effector molecules in two prototypic autoinflammatory skin diseases, pyoderma gangrenosum and Sweet’s syndrome. Clin Exp Immunol. 2014;178(1):48–56.
Braswell SF, Kostopoulos TC, Ortega-Loayza AG. Pathophysiology of pyoderma gangrenosum (PG): an updated review. J Am Acad Dermatol. 2015;73(4):691–8.
Prajapati V, Man J, Brassard A. Pyoderma gangrenosum: common pitfalls in management and a stepwise, evidence-based, therapeutic approach. J Cutan Med Surg. 2009;13(Suppl 1):S2-11.
Hughes AP, Jackson JM, Callen JP. Clinical features and treatment of peristomal pyoderma gangrenosum. JAMA. 2000;284(12):1546–8.
Jolles S, Niclasse S, Benson E. Combination oral and topical tacrolimus in therapy-resistant pyoderma gangrenosum. Br J Dermatol. 1999;140(3):564–5.
Marzano AV, Trevisan V, Lazzari R, Crosti C. Pyoderma gangrenosum: study of 21 patients and proposal of a “clinicotherapeutic” classification. J Dermatol Treat. 2011;22(5):254–60.
Brooklyn TN, Dunnill MG, Shetty A, Bowden JJ, Williams JD, Griffiths CE, et al. Infliximab for the treatment of pyoderma gangrenosum: a randomised, double blind, placebo controlled trial. Gut. 2006;55(4):505–9.
Hubbard VG, Friedmann AC, Goldsmith P. Systemic pyoderma gangrenosum responding to infliximab and adalimumab. Br J Dermatol. 2005;152(5):1059–61.
Alkhouri N, Hupertz V, Mahajan L. Adalimumab treatment for peristomal pyoderma gangrenosum associated with Crohn’s disease. Inflamm Bowel Dis. 2009;15(6):803–6.
Vidal D, Puig L, Gilaberte M, Alomar A. Review of 26 cases of classical pyoderma gangrenosum: clinical and therapeutic features. J Dermatol Treat. 2004;15(3):146–52.
Nousari HC, Lynch W, Anhalt GJ, Petri M. The effectiveness of mycophenolate mofetil in refractory pyoderma gangrenosum. Arch Dermatol. 1998;134(12):1509–11.
von den Driesch P. Pyoderma gangrenosum: a report of 44 cases with follow-up. Br J Dermatol. 1997;137(6):1000–5.
Sardar P, Guha P, Das NK, Gharami RC, Majumdar S, Banerjee D, et al. Ulcerative pyoderma gangrenosum in mixed connective tissue disorder: a rare association and role of azathioprine in the management. Indian J Dermatol. 2011;56(5):600–2.
Din RS, Tsiaras WG, Li DG, Mostaghimi A. Efficacy of systemic dapsone treatment for pyoderma gangrenosum: a retrospective review. J Drugs Dermatol. 2018;17(10):1058–60.
Cohen PR. Sweet’s syndrome—a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:34.
Cohen PR, Kurzrock R. Sweet’s syndrome revisited: a review of disease concepts. Int J Dermatol. 2003;42(10):761–78.
von den Driesch P. Sweet’s syndrome (acute febrile neutrophilic dermatosis). J Am Acad Dermatol. 1994;31(4):535–56 (quiz 57–60).
Ali M, Duerksen DR. Ulcerative colitis and Sweet’s syndrome: a case report and review of the literature. Can J Gastroenterol. 2008;22(3):296–8.
Cohen PR, Kurzrock R. Sweet’s syndrome: a review of current treatment options. Am J Clin Dermatol. 2002;3(2):117–31.
Suehisa S, Tagami H. Treatment of acute febrile neutrophilic dermatosis (Sweet’s syndrome) with colchicine. Br J Dermatol. 1981;105(4):483.
Amouri M, Masmoudi A, Ammar M, Boudaya S, Khabir A, Boudawara T, et al. Sweet’s syndrome: a retrospective study of 90 cases from a tertiary care center. Int J Dermatol. 2016;55(9):1033–9.
el Sherif AI, Bharija SC, Belhaj MS, Singh G. Dapsone in Sweet syndrome. Int J Dermatol. 1990;29(10):737.
Bourke JF, Berth-Jones J, Graham-Brown RA. Sweet’s syndrome responding to cyclosporin. Br J Dermatol. 1992;127(1):36–8.
Seminario-Vidal L, Guerrero C, Sami N. Refractory Sweet’s syndrome successfully treated with rituximab. JAAD Case Rep. 2015;1(3):123–5.
Agarwal A, Barrow W, Selim MA, Nicholas MW. Refractory subcutaneous Sweet syndrome treated with adalimumab. JAMA Dermatol. 2016;152(7):842–4.
Schmidt E, Kasperkiewicz M, Joly P. Pemphigus. Lancet. 2019;394(10201):882–94.
Svecova D. Pemphigus vulgaris: a clinical study of 44 cases over a 20-year period. Int J Dermatol. 2015;54(10):1138–44.
Chmurova N, Svecova D. Pemphigus vulgaris: a 11-year review. Bratisl Lek Listy. 2009;110(8):500–3.
Kridin K, Zelber-Sagi S, Comaneshter D, Batat E, Cohen AD. Pemphigus and hematologic malignancies: a population-based study of 11,859 patients. J Am Acad Dermatol. 2018;78(6):1084-9.e1.
Kridin K. Pemphigus group: overview, epidemiology, mortality, and comorbidities. Immunol Res. 2018;66(2):255–70.
Heelan K, Mahar AL, Walsh S, Shear NH. Pemphigus and associated comorbidities: a cross-sectional study. Clin Exp Dermatol. 2015;40(6):593–9.
Seo JW, Park J, Lee J, Kim MY, Choi HJ, Jeong HJ, et al. A case of pemphigus vulgaris associated with ulcerative colitis. Intest Res. 2018;16(1):147–50.
Kacar S, Sezgin O, Sahin T. Pemphigus vulgaris and ulcerative colitis. Am J Gastroenterol. 2002;97(2):507–8.
Prendiville JS, Israel DM, Wood WS, Dimmick JE. Oral pemphigus vulgaris associated with inflammatory bowel disease and herpetic gingivostomatitis in an 11-year-old girl. Pediatr Dermatol. 1994;11(2):145–50.
Kridin K, Zelber-Sagi S, Comaneshter D, Cohen AD. Ulcerative colitis associated with pemphigus: a population-based large-scale study. Scand J Gastroenterol. 2017;52(12):1360–4.
Takizawa H, Watanabe S, Takahashi M, Asakura H. Pemphigus vulgaris with asymptomatic pseudomembranous colitis. Am J Gastroenterol. 1996;91(8):1654–5.
Leshem YA, Hodak E, David M, Anhalt GJ, Mimouni D. Successful treatment of pemphigus with biweekly 1-g infusions of rituximab: a retrospective study of 47 patients. J Am Acad Dermatol. 2013;68(3):404–11.
Anandan V, Jameela WA, Sowmiya R, Kumar MMS, Lavanya P. Rituximab: a magic bullet for pemphigus. J Clin Diagn Res. 2017;11(4):WC01–6.
Lunardon L, Tsai KJ, Propert KJ, Fett N, Stanley JR, Werth VP, et al. Adjuvant rituximab therapy of pemphigus: a single-center experience with 31 patients. Arch Dermatol. 2012;148(9):1031–6.
Kasperkiewicz M, Shimanovich I, Meier M, Schumacher N, Westermann L, Kramer J, et al. Treatment of severe pemphigus with a combination of immunoadsorption, rituximab, pulsed dexamethasone and azathioprine/mycophenolate mofetil: a pilot study of 23 patients. Br J Dermatol. 2012;166(1):154–60.
Antonelli E, Bassotti G, Tramontana M, Hansel K, Stingeni L, Ardizzone S, et al. Dermatological manifestations in inflammatory bowel diseases. J Clin Med. 2021;10(2):364.
Thrash B, Patel M, Shah KR, Boland CR, Menter A. Cutaneous manifestations of gastrointestinal disease: part II. J Am Acad Dermatol. 2013;68(2):211.e1-233.e1 (quiz 44–6).
Hagen JW, Swoger JM, Grandinetti LM. Cutaneous manifestations of Crohn disease. Dermatol Clin. 2015;33(3):417–31.
Roth N, Biedermann L, Fournier N, Butter M, Vavricka SR, Navarini AA, et al. Occurrence of skin manifestations in patients of the Swiss inflammatory bowel disease cohort study. PLoS ONE. 2019;14(1):e0210436.
Cui RZ, Bruce AJ, Rogers RS. Recurrent aphthous stomatitis. Clin Dermatol. 2016;34(4):475–81.
Scully C, Porter S. Oral mucosal disease: recurrent aphthous stomatitis. Br J Oral Maxillofac Surg. 2008;46(3):198–206.
Vavricka SR, Gubler M, Gantenbein C, Spoerri M, Froehlich F, Seibold F, et al. Anti-TNF treatment for extraintestinal manifestations of inflammatory bowel disease in the Swiss IBD cohort study. Inflamm Bowel Dis. 2017;23(7):1174–81.
Greenstein AJ, Janowitz HD, Sachar DB. The extra-intestinal complications of Crohn’s disease and ulcerative colitis: a study of 700 patients. Medicine (Baltimore). 1976;55(5):401–12.
Greuter T, Vavricka SR. Extraintestinal manifestations in inflammatory bowel disease—epidemiology, genetics, and pathogenesis. Expert Rev Gastroenterol Hepatol. 2019;13(4):307–17.
Karmiris K, Avgerinos A, Tavernaraki A, Zeglinas C, Karatzas P, Koukouratos T, et al. Prevalence and characteristics of extra-intestinal manifestations in a large cohort of Greek patients with inflammatory bowel disease. J Crohns Colitis. 2016;10(4):429–36.
Trost LB, McDonnell JK. Important cutaneous manifestations of inflammatory bowel disease. Postgrad Med J. 2005;81(959):580–5.
Timani S, Mutasim DF. Skin manifestations of inflammatory bowel disease. Clin Dermatol. 2008;26(3):265–73.
Apgar JT. Newer aspects of inflammatory bowel disease and its cutaneous manifestations: a selective review. Semin Dermatol. 1991;10(3):138–47.
Requena L, Requena C. Erythema nodosum. Dermatol Online J. 2002;8(1):4.
Blake T, Manahan M, Rodins K. Erythema nodosum—a review of an uncommon panniculitis. Dermatol Online J. 2014;20(4):22376.
Ubogy Z, Persellin RH. Suppression of erythema nodosum by indomethacin. Acta Derm Venereol. 1982;62(3):265–6.
Lehman CW. Control of chronic erythema nodosum with naproxen. Cutis. 1980;26(1):66–7.
Horio T, Danno K, Okamoto H, Miyachi Y, Imamura S. Potassium iodide in erythema nodosum and other erythematous dermatoses. J Am Acad Dermatol. 1983;9(1):77–81.
Elizaga FV. Erythema nodosum and indomethacin. Ann Intern Med. 1982;96(3):383.
Alloway JA, Franks LK. Hydroxychloroquine in the treatment of chronic erythema nodosum. Br J Dermatol. 1995;132(4):661–2.
Gilchrist H, Patterson JW. Erythema nodosum and erythema induratum (nodular vasculitis): diagnosis and management. Dermatol Ther. 2010;23(4):320–7.
Reddy H, Shipman AR, Wojnarowska F. Epidermolysis bullosa acquisita and inflammatory bowel disease: a review of the literature. Clin Exp Dermatol. 2013;38(3):225–9 (quiz 9–30).
Koga H, Prost-Squarcioni C, Iwata H, Jonkman MF, Ludwig RJ, Bieber K. Epidermolysis bullosa acquisita: the 2019 update. Front Med (Lausanne). 2018;5:362.
Chen M, Kim GH, Prakash L, Woodley DT. Epidermolysis bullosa acquisita: autoimmunity to anchoring fibril collagen. Autoimmunity. 2012;45(1):91–101.
Gupta R, Woodley DT, Chen M. Epidermolysis bullosa acquisita. Clin Dermatol. 2012;30(1):60–9.
Chen M, O’Toole EA, Sanghavi J, Mahmud N, Kelleher D, Weir D, et al. The epidermolysis bullosa acquisita antigen (type VII collagen) is present in human colon and patients with Crohn’s disease have autoantibodies to type VII collagen. J Invest Dermatol. 2002;118(6):1059–64.
Ungureanu L, Cosgarea R, Alexandru Badea M, Florentina Vasilovici A, Cosgarea I, Corina ȘS. Cutaneous manifestations in inflammatory bowel disease (review). Exp Ther Med. 2020;20(1):31–7.
Vodegel RM, Jonkman MF, Pas HH, de Jong MC. U-serrated immunodeposition pattern differentiates type VII collagen targeting bullous diseases from other subepidermal bullous autoimmune diseases. Br J Dermatol. 2004;151(1):112–8.
Kim JH, Kim YH, Kim SC. Epidermolysis bullosa acquisita: a retrospective clinical analysis of 30 cases. Acta Derm Venereol. 2011;91(3):307–12.
Iranzo P, Herrero-González JE, Mascaró-Galy JM, Suárez-Fernández R, España A. Epidermolysis bullosa acquisita: a retrospective analysis of 12 patients evaluated in four tertiary hospitals in Spain. Br J Dermatol. 2014;171(5):1022–30.
Gürcan HM, Ahmed AR. Current concepts in the treatment of epidermolysis bullosa acquisita. Expert Opin Pharmacother. 2011;12(8):1259–68.
Iwata H, Vorobyev A, Koga H, Recke A, Zillikens D, Prost-Squarcioni C, et al. Meta-analysis of the clinical and immunopathological characteristics and treatment outcomes in epidermolysis bullosa acquisita patients. Orphanet J Rare Dis. 2018;13(1):153.
Cleynen I, Van Moerkercke W, Billiet T, Vandecandelaere P, Vande Casteele N, Breynaert C, et al. Characteristics of skin lesions associated with anti-tumor necrosis factor therapy in patients with inflammatory bowel disease: a cohort study. Ann Intern Med. 2016;164(1):10–22.
Fréling E, Baumann C, Cuny JF, Bigard MA, Schmutz JL, Barbaud A, et al. Cumulative incidence of, risk factors for, and outcome of dermatological complications of anti-TNF therapy in inflammatory bowel disease: a 14-year experience. Am J Gastroenterol. 2015;110(8):1186–96.
Rahier JF, Buche S, Peyrin-Biroulet L, Bouhnik Y, Duclos B, Louis E, et al. Severe skin lesions cause patients with inflammatory bowel disease to discontinue anti-tumor necrosis factor therapy. Clin Gastroenterol Hepatol. 2010;8(12):1048–55.
Fiorino G, Danese S, Pariente B, Allez M. Paradoxical immune-mediated inflammation in inflammatory bowel disease patients receiving anti-TNF-α agents. Autoimmun Rev. 2014;13(1):15–9.
Hu JZ, Billings SD, Yan D, Fernandez AP. Histologic comparison of tumor necrosis factor-α inhibitor-induced psoriasis and psoriasis vulgaris. J Am Acad Dermatol. 2020;83(1):71–7.
Brown G, Wang E, Leon A, Huynh M, Wehner M, Matro R, et al. Tumor necrosis factor-α inhibitor-induced psoriasis: systematic review of clinical features, histopathological findings, and management experience. J Am Acad Dermatol. 2017;76(2):334–41.
Collamer AN, Guerrero KT, Henning JS, Battafarano DF. Psoriatic skin lesions induced by tumor necrosis factor antagonist therapy: a literature review and potential mechanisms of action. Arthritis Rheum. 2008;59(7):996–1001.
Collamer AN, Battafarano DF. Psoriatic skin lesions induced by tumor necrosis factor antagonist therapy: clinical features and possible immunopathogenesis. Semin Arthritis Rheum. 2010;40(3):233–40.
Li SJ, Perez-Chada LM, Merola JF. TNF inhibitor-induced psoriasis: proposed algorithm for treatment and management. J Psoriasis Psoriatic Arthritis. 2019;4(2):70–80.
Cullen G, Kroshinsky D, Cheifetz AS, Korzenik JR. Psoriasis associated with anti-tumour necrosis factor therapy in inflammatory bowel disease: a new series and a review of 120 cases from the literature. Aliment Pharmacol Ther. 2011;34(11–12):1318–27.
Andrisani G, Marzo M, Celleno L, Guidi L, Papa A, Gasbarrini A, et al. Development of psoriasis scalp with alopecia during treatment of Crohn’s disease with infliximab and rapid response to both diseases to ustekinumab. Eur Rev Med Pharmacol Sci. 2013;17(20):2831–6.
Ezzedine K, Visseaux L, Cadiot G, Brixi H, Bernard P, Reguiai Z. Ustekinumab for skin reactions associated with anti-tumor necrosis factor-α agents in patients with inflammatory bowel diseases: a single-center retrospective study. J Dermatol. 2019;46(4):322–7.
Tillack C, Ehmann LM, Friedrich M, Laubender RP, Papay P, Vogelsang H, et al. Anti-TNF antibody-induced psoriasiform skin lesions in patients with inflammatory bowel disease are characterised by interferon-γ-expressing Th1 cells and IL-17A/IL-22-expressing Th17 cells and respond to anti-IL-12/IL-23 antibody treatment. Gut. 2014;63(4):567–77.
Gregoriou S, Kazakos C, Christofidou E, Kontochristopoulos G, Vakis G, Rigopoulos D. Pustular psoriasis development after initial ustekinumab administration in chronic plaque psoriasis. Eur J Dermatol. 2011;21(1):104–5.
Adegbola SO, Pisani A, Sahnan K, Tozer P, Ellul P, Warusavitarne J. Medical and surgical management of perianal Crohn’s disease. Ann Gastroenterol. 2018;31(2):129–39.
Stringer EE, Nicholson TJ, Armstrong D. Efficacy of topical metronidazole (10 percent) in the treatment of anorectal Crohn’s disease. Dis Colon Rectum. 2005;48(5):970–4.
Hart AL, Plamondon S, Kamm MA. Topical tacrolimus in the treatment of perianal Crohn’s disease: exploratory randomized controlled trial. Inflamm Bowel Dis. 2007;13(3):245–53.
Hughes LE. Surgical pathology and management of anorectal Crohn’s disease. J R Soc Med. 1978;71(9):644–51.
Bouguen G, Trouilloud I, Siproudhis L, Oussalah A, Bigard MA, Bretagne JF, et al. Long-term outcome of non-fistulizing (ulcers, stricture) perianal Crohn’s disease in patients treated with infliximab. Aliment Pharmacol Ther. 2009;30(7):749–56.
Vogel JD, Johnson EK, Morris AM, Paquette IM, Saclarides TJ, Feingold DL, et al. Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis Colon Rectum. 2016;59(12):1117–33.
Thia KT, Mahadevan U, Feagan BG, Wong C, Cockeram A, Bitton A, et al. Ciprofloxacin or metronidazole for the treatment of perianal fistulas in patients with Crohn’s disease: a randomized, double-blind, placebo-controlled pilot study. Inflamm Bowel Dis. 2009;15(1):17–24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There is no funding for this manuscript.
Conflict of interest
The authors have no conflicts of interest to declare.
Ethics approval
Not applicable.
Consent to participate/publish
Not applicable.
Code availability
Not applicable.
Author contributions
All authors contributed to the manuscript conception and design. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by KP, DL, and AB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability
Our manuscript has no associated data.
Rights and permissions
About this article
Cite this article
Pagani, K., Lukac, D., Bhukhan, A. et al. Cutaneous Manifestations of Inflammatory Bowel Disease: A Basic Overview. Am J Clin Dermatol 23, 481–497 (2022). https://doi.org/10.1007/s40257-022-00689-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-022-00689-w