Abstract
Sweet's syndrome (the eponym for acute febrile neutrophilic dermatosis) is characterized by a constellation of clinical symptoms, physical features, and pathologic findings which include fever, neutrophilia, tender erythematous skin lesions (papules, nodules, and plaques), and a diffuse infiltrate consisting predominantly of mature neutrophils that are typically located in the upper dermis. Several hundreds cases of Sweet's syndrome have been published. Sweet's syndrome presents in three clinical settings: classical (or idiopathic), malignancy-associated, and drug-induced. Classical Sweet's syndrome (CSS) usually presents in women between the age of 30 to 50 years, it is often preceded by an upper respiratory tract infection and may be associated with inflammatory bowel disease and pregnancy. Approximately one-third of patients with CSS experience recurrence of the dermatosis. The malignancy-associated Sweet's syndrome (MASS) can occur as a paraneoplastic syndrome in patients with an established cancer or individuals whose Sweet's syndrome-related hematologic dyscrasia or solid tumor was previously undiscovered; MASS is most commonly related to acute myelogenous leukemia. The dermatosis can precede, follow, or appear concurrent with the diagnosis of the patient's cancer. Hence, MASS can be the cutaneous harbinger of either an undiagnosed visceral malignancy in a previously cancer-free individual or an unsuspected cancer recurrence in an oncology patient. Drug-induced Sweet's syndrome (DISS) most commonly occurs in patients who have been treated with granulocyte-colony stimulating factor, however, other medications may also be associated with DISS. The pathogenesis of Sweet's syndrome may be multifactorial and still remains to be definitively established. Clinical and laboratory evidence suggests that cytokines have an etiologic role. Systemic corticosteroids are the therapeutic gold standard for Sweet's syndrome. After initiation of treatment with systemic corticosteroids, there is a prompt response consisting of dramatic improvement of both the dermatosis-related symptoms and skin lesions. Topical application of high potency corticosteroids or intralesional corticosteroids may be efficacious for treating localized lesions. Other first-line oral systemic agents are potassium iodide and colchicine. Second-line oral systemic agents include indomethacin, clofazimine, cyclosporine, and dapsone. The symptoms and lesions of Sweet's syndrome may resolved spontaneously, without any therapeutic intervention; however, recurrence may follow either spontaneous remission or therapy-induced clinical resolution.
Similar content being viewed by others
Disease name and synonyms
Sweet's syndrome
Acute febrile neutrophilic dermatosis
Gomm-Button disease
Introduction
The syndrome was originally described by Dr. Robert Douglas Sweet in the August-September 1964 issue of the British Journal of Dermatology as an "acute febrile neutrophilic dermatosis" [1–10]. This seminal paper summarizes the cardinal features of "a distinctive and fairly severe illness" that he had encountered in eight women during the 15-year period from 1949 to 1964. In his disease defining report, Dr. Sweet commented that "the condition was known in my department as the Gomm-Button disease, a title some may still prefer to that which heads this paper;" this nomenclature was "in eponymous honor of the first two patients" with the disease in Dr. Sweet's department [8]. Subsequently, Dr. Sweet recommended that the name of the condition remain descriptive; however, in spite of his suggestion, 'Sweet's syndrome' has become the established eponym for this acute febrile neutrophilic dermatosis [1–10]. Several hundreds of reports of Sweet's syndrome patients have since been published [11–435].
Definition and diagnostic criteria
Sweet's syndrome can present in several clinical settings: classical (or idiopathic) Sweet's syndrome, malignancy-associated Sweet's syndrome, and drug-induced Sweet's syndrome.
Classical Sweet's syndrome
Classical Sweet's syndrome is characterized by a constellation of clinical symptoms, physical features, and pathologic findings which include pyrexia, elevated neutrophil count, tender erythematous skin lesions (papules, nodules, and plaques), and a diffuse infiltrate consisting predominantly of mature neutrophils typically located in the upper dermis. The symptoms and clinical manifestations typically respond promptly after initiation of systemic corticosteroid therapy (Figures 1 and 2).
Sweet's syndrome skin lesions in a woman with classical Sweet's syndrome. Cutaneous lesions of classical Sweet's syndrome on the left hand, left proximal arm and left shoulder in a 48-year-old woman with pyrexia, neutropenia, and a recent respiratory tract infection. (From [10] Cohen PR, Almeida L, Kurzrock R: Acute febrile neutrophilic dermatosis. Am Fam Physician 1989;39(3):199–204. Copyright 1989, Reprinted with permission from Academy of American Family Physicians, Leewood, Kansas.)
(a, b, and c). Tender, red Sweet's syndrome lesions in a woman with the classical form of the dermatosis. A closer view of the Sweet's syndrome lesions from the woman in Figure 1. The skin lesions improved rapidly after corticosteroid therapy was initiated. There is an erythematous plaque, 5 cm in diameter, with a pseudovesicular appearance on the left shoulder of the patient (a). A nodular lesion, 1 cm in diameter, is present on the lateral left arm (b). Painful, erythematous, pseudovesicular plaques of acute febrile neutrophilic dermatosis are present on the left hand (c). (From [10] Cohen PR, Almeida L, Kurzrock R: Acute febrile neutrophilic dermatosis. Am Fam Physician 1989;39(3):199–204. Copyright 1989, Reprinted with permission from Academy of American Family Physicians, Leewood, Kansas.)
The diagnostic criteria for classical Sweet's syndrome were originally proposed by Su and Liu [11] in 1986. They were modified by von den Driesch [12] in 1994 (Table 1) [13, 14]. Additional cases of Sweet's syndrome continue to appear in the medical literature since Sweet's original paper [1–435].
Malignancy-associated Sweet's syndrome
Shapiro et al [24] reported the first patient with solid tumor-associated Sweet's syndrome, a 58-year-old man with testicular carcinoma, in 1971. However, prior to Dr. Sweet's 1964 publication, Costello et al [29] described a 16-year-old girl with acute myelogenous leukemia and recurrent cutaneous lesions of variable morphologies in 1955. Retrospectively, several authors have acknowledged that Costello et al's patient represents the first report of malignancy-associated Sweet's syndrome. It was not until 18 years later, in 1973, that Matta and Kurban [25] reported two women whose biopsy-confirmed Sweet's syndrome lesions were the presenting manifestation of their previously unsuspected acute leukemia.
Malignancy-associated Sweet's syndrome was initially included as a subset of classical Sweet's syndrome. However, since many of the cases of Sweet's syndrome are cancer-related, several authors have chosen to distinguish between the classical form and the malignancy-associated form of this condition. The onset of Sweet's syndrome can precede, follow, or appear concurrent with the diagnosis of the patient's neoplasm. Indeed, the dermatosis can be the cutaneous harbinger of either an undiagnosed visceral malignancy in a previously cancer-free individual or an unsuspected cancer recurrence in an oncology patient.
Drug-induced Sweet's syndrome
Su and Liu [11] reported the first patient with drug-induced Sweet's syndrome in 1986; the associated medication was trimethoprim-sulfamethoxazole. A decade later, criteria for drug-induced Sweet's syndrome were established by Walker and Cohen [13]. The most frequently implicated drug is granulocyte-colony stimulating factor. However, several other medications – albiet less often – have been observed to promote the development of Sweet's syndrome.
Diagnostic criteria for drug-induced Sweet's syndrome were presented by Walker and Cohen [13] in 1996 (Table 1).
Epidemiology
The distribution of Sweet's syndrome cases is worldwide and there is no racial predilection (Table 2) [1, 2, 12, 13, 15–20, 30, 31].
Classical or idiopathic Sweet's syndrome predominantly affects in women. It may be associated with infection (upper respiratory tract or gastrointestinal tract), inflammatory bowel disease, or pregnancy [13, 15]. Recurrence of the dermatosis is noted in approximately one-third of individuals.
The initial episode of classical Sweet's syndrome most frequently occurs between the ages of 30 to 60 years. However, classical Sweet's syndrome has been reported in children (as young as 7 weeks of age) and younger adults [32–48]. Brothers who developed the dermatosis at 10 and 15 days of age are the youngest Sweet's syndrome patients reported [46].
Malignancy-associated Sweet's syndrome has been published as descriptions of individual oncology patients with Sweet's syndrome, observations from small series of Sweet's syndrome patients with cancer, and retrospective reviews in which the features from multiple Sweet's syndrome patients (some with malignancy) are summarized. In 1993, Cohen and Kurzrock [15] reviewed and combined the data from 15 studies of patients with Sweet's syndrome studies (each containing between ten to 48 individuals) in order to more accurately define the incidence of malignancy-associated Sweet's syndrome. They found that 21 percent of the patients with Sweet's syndrome (96 of 448 individuals) had either a hematologic malignancy or a solid tumor.
Several investigators consider it appropriate to distinguish malignancy-associated Sweet's syndrome from the classical form of this disease. Malignancy-associated Sweet's syndrome occurs as frequently in men as in women. Also, it is less often preceded by an upper respiratory tract infection. In addition, the onset or recurrence of many of the cases of malignancy-associated Sweet's syndrome is temporally associated with the discovery or relapse of cancer. Specifically, in these individuals, either the new discovery of an unsuspected neoplasm in a patient in whom cancer has not previously been diagnosed or the recurrence of malignancy in a patient with a previously established cancer is temporally associated with the appearance of the dermatosis [15, 49–60].
Malignancy-associated Sweet's syndrome is most often associated with acute myelogenous leukemia [61, 62]. However, in patients with hematologic disorders, Sweet's syndrome can occur in one or more of the following forms: a paraneoplastic syndrome, a drug-induced dermatosis, or a condition whose skin lesions concurrently demonstrate leukemia cutis. Carcinomas of the genitourinary organs, breast, and gastrointestinal tract are the most frequently occurring cancers in Sweet's syndrome patients with dermatosis-related solid tumors [1, 2, 63–66].
Drug-induced Sweet's syndrome
Several medications have been associated with the subsequent development of drug-induced Sweet's syndrome (Table 3) [1, 2, 11, 13, 17, 39, 41, 67–124, 398, 401, 404, 417, 426, 435] (Figure 3). However, the drug-induced variant of the dermatosis has most frequently been observed in patients following the administration of granulocyte-colony stimulating factor. Recurrence of the dermatosis is often noted when the patient is rechallenged with the associated drug. However, once the causative agent has been discontinued, the disease manifestations frequently improve.
(a, b, and c). Drug-induced Sweet's syndrome with photodistributed skin lesions. Photodistributed drug-induced Sweet's syndrome in a 50-year-old woman with trimethoprim-sulfamethoxazole-associated acute febrile neutrophilic dermatosis. Distant (a) and closer (b) views of Sweet's syndrome lesions located on the sun-exposed areas of the arms, hands, and upper chest are shown. The biopsy specimen (c) shows a confluent neutrophilic infiltrate in the reticular dermis and edema in the papillary dermis (hematoxylin and eosin, × 50). (From [13] Walker DC, Cohen PR: Trimethoprim-sulfamethoxazole-associated acute febrile neutrophilic dermatosis: case report and review of drug-induced Sweet's syndrome. J Am Acad Dermatol 1996;34:918–923. Copyright 1996, Reprinted with permission from the American Academy of Dermatology, Inc, Elsevier Ltd, Oxford, United Kingdom.)
Clinical description
Symptoms
Sweet's syndrome patients may appear dramatically ill. Fever is the most frequent symptom. Indeed, the skin eruption of Sweet's syndrome is usually accompanied by fever and leukocytosis. However, the cutaneous manifestations of the disease may be preceded by several days to weeks of fever. Alternatively, pyrexia can be concurrently present throughout the entire episode of the dermatosis. Also, in some patients with biopsy-confirmed malignancy-associated Sweet's syndrome, fever may be absent. Other Sweet's syndrome-associated symptoms, such as arthralgia, general malaise, headache, and myalgia may also be present [1, 2, 23].
Skin lesions
Skin lesions of Sweet's syndrome are typically tender. They appear as painful, red or purple-red, papules or nodules. Larger lesions may develop into plaques (Figures 1 and 2). The eruption is often distributed asymetrically. It presents as either a single lesion or multiple lesions. The most frequent lesion locations are the upper extremities, face, and neck (Figure 4) [1, 10].
(a and b). Recurrent Sweet's syndrome in a man with antiphospholipid syndrome. A 65-year-old white man with a 7-year history of recurrent Sweet's syndrome and antiphospholipid syndrome (initially manifested by multiple pulmonary emboli and subsequently managed with chronic coumadin therapy). Painful, red, biopsy-confirmed, pseudovesicular nodules and plaques of Sweet's syndrome are present on the posterior neck (a), chest, and upper arm (b). Although the Sweet's syndrome skin lesions resolved after the initiation of oral prednisone (60 mg/day), they recurred when the dose of the drug was subsequently tapered; potassium iodide, colchicine, dapsone, antimalarials, azathioprine, methotrexate, retinoids, and nonsteroidal anti-inflammatory agents were not effective as corticosteroid-sparing agents. (From [1] Cohen PR, Kurzrock R: Sweet's syndrome revisited: a review of disease concepts. Int J Dermatol 2003;42:761–778. Copyright 2003, Reprinted with permission from the International Society of Dermatology, Blackwell Publishing, Oxford, United Kingdom.)
The Sweet's syndrome lesions have a transparent, vesicle-like appearance because of the pronounced edema in the upper dermis; some lesions are morphologically similar to bullae [401, 419]. Central clearing may lead to annular or arcuate patterns in latter stages. In patients with malignancy-associated Sweet's syndrome, the lesions may appear bullous, become ulcerated, and/or mimic the morphologic features of pyoderma gangrenosum [133, 134, 401].
The individual Sweet's syndrome lesions enlarge and may coalesce to form irregular, sharply border plaques over a period of days to weeks. Subsequently, either spontaneously or after treatment, the lesions usually resolve without scarring. In one-third to two-thirds of patients, lesions associated with recurrent episodes of Sweet's syndrome occur [1, 2, 135, 136].
Skin hypersensitivity, also referred to as cutaneous pathergy, is a Sweet's syndrome-associated feature characterized by dermatosis-associated skin lesions appearing at sites of cutaneous trauma [1, 2, 410, 432]. These include the sites where procedures such as biopsies [20], intravenous catheter placement [20, 400], vaccination [419], and venipuncture have been performed [12, 17, 20, 37, 137, 138]. Sweet's syndrome lesions have also been observed at the locations of cat scratches and insect bites [20], areas that have received radiation therapy (Figure 5) [23, 139–141], and places that have been contacted by sensitizing antigens [137, 142]. Lesions have also been photodistributed (Figures 3a and 3b) or localized to the site of a prior phototoxic reaction (sunburn) in some Sweet's syndrome patients [13, 20, 98, 143–145]. Occasionally, Sweet's syndrome lesions have appeared on the arm affected by postmastectomy lymphedema [100, 146, 414].
(a and b). Radiotherapy-related Sweet's syndrome skin lesions in a woman with malignancy-associated Sweet's syndrome. Radiotherapy associated-exacerbated Sweet's syndrome in a patient with chronic lymphocytic leukemia and cutaneous squamous cell carcinoma. This biopsy-confirmed culture-negative, erythematous-based hemorrhagic, and vesicular-appearing Sweet's syndrome lesion extends from the dorsal (a) to the palmar (b) surface of the radial side of the right index finger and involves the skin between the metacarpal-phalangeal joint and the proximal interphalangeal joint of a 77-year-old woman. She has a prior medical history of hypothyroidism for which she receives daily Synthroid. Twenty-four months earlier, she had been diagnosed with chronic lymphocytic leukemia, which is adequately being managed with 2 mg of Myleran each day; her current white blood cell count of 51,800 cells/mm3 consists of 79% neutrophils, 15% bands, and 2% lymphocytes. More recently (3 months previously), a biopsy confirmed (at both initial microscopic evaluation and subsequent consultation pathology review) cutaneous squamous cell carcinoma involving the left index finger. She was started on an oral antibiotic (ciprofloxaxin), and radiotherapy (in fractionated doses over a period of 3 weeks) to the left index finger tumor was performed; during this treatment, a clinically similar-appearing lesion whose "presentation was suspicious for squamous cell carcinoma" began to develop on her right index finger. Based only on the lesion's morphologic characteristics, a single treatment with radiotherapy was also given; promptly thereafter, the right index finger lesion rapidly increased in size. Within a week, the lesion on the right index finger (as shown in a and b) had grown to a 4- × 4-cm pseudovesicular nodule that nearly involved the entire circumference of the digit and she was referred to the dermatology clinic. The lesion was painful and her leukocyte count was markedly elevated; however, she was (and had been) afebrile. Lesional biopsies for microscopic and culture evaluation were performed. Because the diagnosis of Sweet's syndrome was suspected, daily oral corticosteroid therapy with 60 mg prednisone was started. Oral cephalexin (250 mg 4 times each day for 7 days) and topical 2% mupirocin ointment (3 times each day) were also given. After a week of therapy, the lesion was greatly improved: it was no longer tender and it had decreased in size. Subsequently, the lesion completely resolved. The dose of prednisone was tapered during the next 5 weeks and then discontinued. (From [23] Cohen PR, Kurzrock R: Sweet's syndrome: a neutrophilic dermatosis classically associated with acute onset and fever. Clin Dermatol 2000;18:265–282. Copyright 2000, Reprinted with permission from Elsevier Ltd, Oxford, United Kingdom.)
In addition to pseudovesicular papules, plaques, and nodules, Sweet's syndrome can appear as a pustular dermatosis [147]. The lesions appear as either erythematous-based pustules or tiny pustules on the tops of red papules. This clinical variant of Sweet's syndrome probably also includes the "pustular eruption of ulcerative colitis" that has previously been described in some of the patients with this inflammatory bowel disease [1, 148].
When the clinical lesions of the dermatosis are predominantly restricted to the dorsal hands, this localized, pustular variant of Sweet's syndrome has been referred to as either "neutrophilic dermatosis of the dorsal hands" or "pustular vasculitis of the dorsal hands" [3, 149–154, 401, 402, 408, 420, 427]. The morphology and response to treatment of the dermatosis-associated lesions reported as neutrophilic dermatosis of the dorsal hands are similar to those of Sweet's syndrome. The lesions rapidly resolve after systemic corticosteroids and/or dapsone therapy is initiated. Resolution of lesions has also been observed spontaneously [420] or following therapy with either topical corticosteroids [401], systemic colchicine [401], or systemic indomethacin [427]. In addition, concurrent lesions were located on either their oral mucosa, arm, leg, back, and/or face of several patients with this form of the disease [3, 155–163, 401, 420].
Subcutaneous Sweet's syndrome is characterized by skin lesions which usually present as erythematous, tender dermal nodules on the extremities [4, 8, 12, 17, 99, 119, 164–185, 397]. The lesions often mimic erythema nodosum when they are located on the legs [170]. Even in a patient whose Sweet's syndrome has previously been biopsy-confirmed, tissue evaluation of one or more new dermal nodules may be necessary to establish the correct diagnosis since Sweet's syndrome can present concurrently (Figures 6 and 7) [21, 125, 187–189] or sequentially [170] with erythema nodosum [1, 2, 4, 17, 21, 187, 190, 403].
(a and b). Clinical presentation of concurrent Sweet's syndrome and erythema nodosum. A 30-year-old woman had been receiving an oral contraceptive (0.3 mg norgestrel with 0.3 mg ethinyl estradiol) and an appetite suppressant (105 mg phendimetrazine tartrate) during the 5 months before these dermatoses appeared. An episode of recurrent herpes labialis involving her right upper lip also began 2 days prior to the onset of her skin lesions. Tender, erythematous plaques of biopsy-confirmed Sweet's syndrome are shown on the dorsal right hand and wrist; the suture indicates the biopsy site (a). A tender, erythematous nodule of biopsy confirmed erythema nodosum – which morphologically mimiced subcutaneous Sweet's syndrome – is shown on her right pretibial region (b). (From [21] Cohen PR, Holder WR, Rapini RP: Concurrent Sweet's syndrome and erythema nodosum: a report, world literature review and mechanism of pathogenesis. J Rheumatol 1992;5:814–820. Copyright 1992, Reprinted with permission from the Journal of Rheumatology, Toronto, Ontario.)
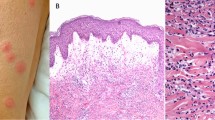
(a and b). Histopathology of a Sweet's syndrome lesion from a patient with concurrent erythema nodosum. Skin biopsy from one of the Sweet's syndrome plaques on the right dorsal wrist of a woman with concurrent biopsy-confirmed Sweet's sydrome and biopsy-confirmed erythema nodosum. The characteristic histopathologic features of Sweet's syndrome are observed at low (a) and higher (b) magnification: papillary dermal edema, swollen endothelial cells, and a diffuse infiltrate of predominantly neutrophils with leukocytoclasia. There is no evidence of vasculitis (hematoxylin and eosin, × 25 (a), × 100 (b)). (From [21] Cohen PR, Holder WR, Rapini RP: Concurrent Sweet's syndrome and erythema nodosum: a report, world literature review and mechanism of pathogenesis. J Rheumatol 1992;5:814–820. Copyright 1992, Reprinted with permission from the Journal of Rheumatology, Toronto, Ontario.)
Extracutaneous manifestations
Bones, central nervous system, ears, eyes, kidneys, intestines, liver, heart, lung, mouth, muscles, and spleen can be the sites of extracutaneous manifestations of Sweet's syndrome (Table 4) [12, 16, 17, 20, 25, 26, 32, 33, 44, 73, 75, 88, 101, 117, 138, 139, 165, 202, 203, 205, 212–257, 421, 423, 434]. In addition, dermatosis-related sterile osteomyelitis has been reported in children.
Ocular manifestations may be the presenting feature of Sweet's syndrome. The incidence of ocular involvement (such as conjunctivitis) is variable in classical Sweet's syndrome. However, ocular lesions of Sweet's syndrome are uncommon in the malignancy-associated and drug-induced forms of the dermatosis.
Mucosal involvement of the mouth, appearing as oral ulcers, is uncommon in patients with classical Sweet's syndrome. However, dermatosis-related oral lesions occurs more frequently in Sweet's syndrome patients with hematologic disorders [23, 26, 102, 117, 203, 252]. Similar to extracutaneous manifestations of Sweet's syndrome occurring at other sites, the dermatosis-related oral ulcers typically resolve after initiation of treatment with systemic corticosteroids [1, 2].
Included diseases
Several conditions – including other neutrophilic dermatoses and leukemia cutis – have been observed to occur either before, concurrent with, or following the diagnosis of Sweet's syndrome in patients with this dermatosis. Therefore, it is reasonable to conclude that the occurrence of Sweet's syndrome in these individuals may be etiologically to the development of some of these conditions.
Associated diseases
A bona fide association between Sweet's syndrome probably exists with the following conditions: cancer (including both hematologic malignancies and solid tumors) (Figure 8), infections (predominantly of the upper respiratory tract and the gastrointestinal tract), inflammatory bowel disease (including both Crohn's disease and ulcerative colitis), medications (granulocyte-colony stimulating factor is the most commonly reported drug) and pregnancy (Table 5). There are also several conditions for which the association with Sweet's syndrome is possibly bona fide (Table 6). In addition, the validity of the association between Sweet's syndrome and many of the conditions that have been observed in patients with the dermatosis remains to be established (Table 7) (Figure 9); indeed, the detection of that condition in an individual with Sweet's syndrome may merely represent a coincidental occurrence [1, 2, 5, 11–20, 30, 36–43, 69–126, 158–161, 164, 166, 186–190, 195, 214, 231, 236, 259–339, 401, 404, 407, 409–411, 413, 415, 417–419, 421, 424, 425, 431, 433].
(a and b). Malignancy-associated Sweet's syndrome in a woman with dermatosis-related laryngeal carcinoma. Solid tumor-associated Sweet's syndrome in a 69-year-old woman in whom a workup after the appearance of Sweet's syndrome lesions revealed an unsuspected recurrent squamous cell carcinoma of the larynx. A tender, erythematous-based, vesicular-appearing nodule of Sweet's syndrome with central ulceration and crust located proximally on the dorsum of the right second digit is shown (a). The histologic features of the Sweet's syndrome lesion revealed a neutrophilic dermatosis; the papillary dermis was edematous and contained a dense infiltrate of neutrophils (b) (hematoxylin and eosin, × 50). (From [362] Cohen PR, Holder WR, Tucker SB, Kono S, Kurzrock R: Sweet's syndrome in patients with solid tumors. Cancer 1993;72:2723–2731. Copyright 1993, Reprinted with permission from John Wiley & Sons, Inc., Hoboken, New Jersey.)
(a and b). Recurrent, oral corticosteroid-responsive, Sweet's syndrome lesions. A 46-year-old Indian woman with oral corticosteroid-responsive, tender erythematous, biopsy-confirmed plaques of recurrent Sweet's syndrome on the posterior neck (a) and right arm (b). Her laboratory evaluation was significant for the elevation of the erythrocyte sedimentation rate, liver function tests [serum glutamic-oxaloacetic transaminase (SGOT), serum glutamic-pyruvic transaminase (SGPT), and lactate dehydrogenase (LDH)], cytomegalovirus immunoglobulin G (IgG) antibody (consistent with previous exposure), hepatitis A IgG antibody (consistent with previous infection), and Epstein-Barr virus capsid IgG antibody (consistent with recent or past infection). (From [1] Cohen PR, Kurzrock R: Sweet's syndrome revisited: a review of disease concepts. Int J Dermatol 2003;42:761–778. Copyright 2003, Reprinted with permission from the International Society of Dermatology, Blackwell Publishing, Oxford, United Kingdom.)
Associated neutrophilic dermatoses
Neutrophilic dermatoses of the skin and mucosa demonstrate a unifying characteristic. They all have an inflammatory infiltrate that consists of mature polymorphonuclear leukocytes. Although many of these conditions exhibit similar clinical and pathologic features, the location of the neutrophilic infiltrate may permit differentiation of these dermatoses [6, 120, 416]. Erythema elevatum diutinum [340], neutrophilic eccrine hidradenitis [6], pyoderma gangrenosum [231, 269, 341, 342, 401], subcorneal pustular dermatosis [6], and vasculitis [3, 192, 210, 231] are other neutrophilic dermatoses that have been observed to occur in patients with Sweet's syndrome. The onset of Sweet's syndrome may appear prior to, concurrent with, or following the detection of the additional neutrophilic dermatoses.
Associated leukemia cutis
Sweet's syndrome may occur in three settings in patients with hematologic disorders, such as leukemia: (1) a paraneoplastic syndrome heralding either the initial discovery of an unsuspected malignancy or the recurrence of a previously treated cancer; (2) a drug-induced dermatosis subsequent to the patient being treated with either all-trans retinoic acid, bortezomib, granulocyte-colony stimulating factor, or imatinib mesylate; or (3) a dermatosis in which the skin lesions concurrently demonstrate leukemia cutis [1]. In the latter setting, the individual skin lesions are characterized by the coincident presence of abnormal neutrophils (leukemia cutis) and mature polymorphonuclear leukocytes (Sweet's syndrome) [1, 70, 71, 93, 109, 165, 205–211, 401, 417, 425]. The most frequent hematologic malignancies associated with this unique presentation of Sweet's syndrome are acute myelocytic leukemia and acute promyelocytic leukemia. Other hematologic disorders that have been associated with concurrent Sweet's syndrome and leukemia cutis are chronic myelogenous leukemia, myelogenous leukemia (not otherwise specified), and myelodysplastic syndrome [109].
Several hypotheses have been suggested to explain concurrent Sweet's syndrome and leukemia cutis in the same lesion. One theory is that the circulating immature myeloid precursor cells are innocent bystanders that have been recruited to the skin as the result of an inflammatory oncotactic phenomenon stimulated by the Sweet's syndrome lesions ("secondary" leukemia cutis) [165, 206, 207]. Alternatively, the leukemic cells within the skin may constitute the bonified incipient presence of a specific leukemic infiltrate ("primary" leukemia cutis) [207]. Finally, in patients with "primary" leukemia cutis who have been treated with this granulocyte-colony stimulating factor, it is possible that the atypical cells of leukemia cutis developed into mature neutrophils of Sweet's syndrome as a result of granulocyte-colony stimulating factor therapy-induced differentiation of the sequestered leukemia cells [205].
Pathological description
The diagnostic criteria for Sweet's syndrome includes a diffuse infiltrate of mature neutrophils. In addition to the dense polymorphonuclear cell infiltrate in the upper dermis, edema are characteristically present (Figures 8b and 3c). Fragmented neutrophil nuclei (referred to as karyorrhexis or leukocytoclasia), swollen endothelial cells, and dilated small blood vessels may also be present (Figure 7). The overlying epidermis is normal and changes of "primary" leukocytoclastic vasculitis (such as fibrin deposition or neutrophils within the vessel walls) are usually absent [1, 2, 23, 167, 168].
Since the initial description of 'acute febrile neutrophilic dermatosis' by Dr. Sweet, the spectrum of pathologic changes described in cutaneous lesions of Sweet's syndrome has expanded. There is variability regarding the composition of the inflammatory infiltrate and its depth within the skin. Although the neutrophilic infiltrate is traditionally found in the dermis, it can also be present in either the overlying epidermis or the underlying adipose tissue. Also, in patients with hematologic malignancy-associated Sweet's syndrome, concurrent leukemia cutis may be present in the dermatosis-related skin lesions [3, 191].
The predominant cells that comprise the infiltrate in the dermis of cutaneous Sweet's syndrome lesions are mature neutrophils. However, eosinophils have been observed within the dermal infiltrate in the Sweet's syndrome skin lesions of some patients with either the classical [11, 167, 168, 195, 202–204, 212] or the drug-induced [84, 107, 110, 111] dermatosis. Occasionally, lymphocytes or histiocytes may also be present in the inflammatory infiltrate [11, 104, 167, 168, 198–200, 425].
A unique clinicopathologic subset of 11 Sweet's syndrome patients has recently been characterized [200, 425]. The patients either presented with or subsequently developed myelodysplastic syndrome; four of the patients also developed relapsing polychondritis [5, 409, 425]. Initially, the diagnosis of Sweet's syndrome was based on clinical features. Surprisingly, the Sweet's syndrome lesions from the early episodes of the dermatosis in these individuals showed a dense mononuclear cell infiltrate consisting predominantly of lymphocytes; histiocytes and atypical mononuclear cells were also present. However, 24 to 96 months later, sequential biopsies of lesion from recurrent episodes in these patients revealed neutrophilic dermal infiltrates typical of Sweet's syndrome [425].
Abnormal or immature myeloid cells have been observed in Sweet's syndrome lesions. For example, abnormal neutrophils (leukemia cutis) – in addition to mature neutrophils – comprise the dermal infiltrate in some Sweet's syndrome patients with hematologic disorders [1, 70, 71, 93, 109, 165, 205–211, 401, 417]. Recently, a "histiocytoid" pathologic variant of Sweet's syndrome has been described; it is characterized by an infiltrate mainly composed of immature myeloid cells which have been misinterpreted as histiocytes (macrophages) [201].
The inflammatory infiltrate in Sweet's syndrome is usually located in the papillary and upper reticular dermis. However, neutrophils can also be present in the epidermis [17, 197] or adipose tissue. For example, exocytosis of neutrophils into the overlying epidermis has been observed as either neutrophilic spongiotic vesicles [194] or subcorneal pustules [12, 80, 167, 195, 196]. The condition is referred to as "subcutaneous Sweet's syndrome" when the neutrophils are located either entirely or only partially in the subcutaneous fat [4, 8, 12, 17, 99, 119, 164–184, 397, 399, 417].
Subcutaneous Sweet's syndrome can involve either the adipose tissue alone or both the dermis and the subcutaneous fat [1, 4, 401]. Within the subcutaneous fat, the neutrophilic infiltrate is present in the lobules 166,167,171-173,399,401,417], the septae [167, 397], or both [167, 174–177]. The presence of subcutaneous neutrophilic inflammation in Sweet's syndrome lesions may be a more common finding in patients with either an associated hematologic dyscrasia [99, 165, 170, 174, 177, 178, 183, 184, 401, 417] or solid tumor [397, 399].
Cutaneous lesions of subcutaneous Sweet's syndrome typically present as tender erythematous subepidermal nodules on the extremities. They are morphologically similar in appearance to erythema nodosum [431]. Therefore, a biopsy of one or more new nodules may be necessary to establish the correct diagnosis – even in a patient with histology – confirmed Sweet's syndrome – since Sweet's syndrome can develop concurrently or sequentially with erythema nodosum [21, 405].
The neutrophils are typically located in the papillary and upper reticular dermis as a dense and diffusely distributed infiltrate in Sweet's syndrome lesions. However, in some Sweet's syndrome lesions, the neutrophils have been observed to be perivascular and exhibiting pathologic changes consistent with leukocytoclastic vasculitis [192, 193, 396, 401, 410, 428]. In these lesions of Sweet's syndrome, the vascular changes are considered to be those of a "secondary" leukocytoclastic vasculitis occurring as an epiphenomenon and not representative of a "primary" vasculitis [3]. However, some authors have introduced an alternative hypothesis: that Sweet's syndrome be regarded as a variant of leukocytoclastic vasculitis [428].
Pathologic findings of Sweet's syndrome can also occur in extracutaneous sites. They often present as sterile neutrophilic inflammation in the involved organ. These changes have been described in the bones, intestines, liver, aorta, lungs, and muscles of patients with Sweet's syndrome.
Etiology
The pathogenesis of Sweet's syndrome remains to be definitively determined. Indeed, it may be multifactorial and many etiologies – not necessarily mutually exclusive – have been postulated. The accompanying fever and peripheral leukocytosis suggest a septic process. Since most patients with classic Sweet's syndrome have a febrile upper respiratory tract infection or tonsillitis that precedes their skin lesions by 1 to 3 weeks, a bacterial infection may have a causative role. Also, the manifestations of Sweet's syndrome improve with systemic antibiotics in some of the patients with dermatosis-associated culture-confirmed and serology-confirmed Yersinia enterolitica intestinal infection [2, 77, 125–127].
A hypersensitivity reaction to an eliciting bacterial, viral, or tumor antigen may promote the development of Sweet's syndrome. This concept is suggested by the appearance, histopathology and course of the Sweet's syndrome skin lesions. This hypothesis is also supported by the prompt response of both the symptoms and the lesions to corticosteroids [2, 127].
Circulating autoantibodies, cytokines, dermal dendrocytes, human leukocyte antigen serotypes, immune complexes, and leukotactic mechanisms have all been postulated to contribute to the pathogenesis of Sweet's syndrome. However, complement does not appear to be essential to the disease process. Antibodies to neutrophilic cytoplasmic antigens have been demonstrated in some Sweet's syndrome patients. Yet, their role in the pathogenesis of this dermatosis has not been established and they are likely to represent an epiphenomenon [2].
The effects of cytokines – either directly or indirectly or both – have an etiologic role in the development of Sweet's syndrome symptoms and lesions [2, 21–23]. Granulocyte-colony stimulating factor, granulocyte macrophage colony stimulating factor, interferon-gamma, interleukin-1, interleukin-3, interleukin-6, and interleukin-8 are potential cytokine candidates [2, 13, 21, 23, 44, 128–132, 397, 398]. Recently, a healthy woman donor for peripheral blood stem cell harvest was observed to develop granulocyte-colony stimulating factor-induced Sweet's syndrome which appeared four days after commencing granulocyte-colony stimulating factor at a dose of 10 micrograms per kilogram per day [398].
Tumor-associated production of granulocyte-colony stimulating factor may be involved in the development of Sweet's syndrome in patients with dermatosis-related malignancies. Production of granulocyte-colony stimulating factor and marked leukocytosis have been demonstrated by various malignant tumors. Immunohistiochemical studies showed staining for granulocyte-colony stimulating factor in the tumor cells and surrounding matrix of an intrahepatic cholangiocarcinoma which had been resected from a woman whose Sweet's syndrome was associated with this cancer. Although the level of serum granuocyte-colony stimulating factor was not abnormally elevated, the detection of granulocyte-colony stimulating factor in the tumor suggests the possiblity that tumors capable of producing granulocyte-colony stimulating factor might cause Sweet's syndrome in these oncology patients [397].
Another example supporting the role of cytokines in the pathogenesis of Sweet's syndrome is a patient with myelodysplastic syndrome-associated (non-granulocyte-colony stimulating factor-induced) Sweet's syndrome in whom elevated serum levels of granulocyte-colony stimulating factor and interleukin-6 were detected [128]. Also, in an infant with classical Sweet's syndrome, detectable levels of intra-articular synovial fluid granulocyte macrophage-colony stimulating factor were observed [44]. A recent study comparing patients with active and inactive Sweet's syndrome demonstrated significantly higher levels of serum granulocyte-colony stimulating factor in individuals whose dermatosis was active than in patients whose Sweet's syndrome was inactive [129].
Immunohistochemical evaluation of the epidermis of Sweet's syndrome lesions suggests the importance of interleukins as a potential cytokine mediator in Sweet's syndrome. Significantly elevated levels of helper T-cell type 1 cytokines (interleukin-2 and interferon-gamma) and normal levels of a helper T-cell type 2 cytokine (interleukin-4) were observed in the immunohistochemical studies of Sweet's syndrome patients' serum [130]. Decreased epidermal staining for interleukin-1 and interleukin-6 were noted in other immunohistochemical studies; the investigators postulated that these findings were due to the release of these cytokines into the dermis [131]. In summary, granulocyte-colony stimulating factor, granulocyte macrophage colony stimulating factor, interferon-gamma, interleukin-1, interleukin-3, interleukin-6, and interleukin-8 are potential cytokine candidates in the pathogenesis of Sweet's syndrome [2, 13, 21–23, 44, 128–132].
The possibility that Sweet's syndrome, when associated with neutrophil monoclonality, represents a form of indolent, localized cutaneous neutrophilic dyscrasia has recently been postulated. An X-inactivation assay to detect clonal restriction of neutrophils, based on the human androgen receptor (HUMARA) gene, was performed on Sweet's syndrome skin biopsy specimens from four patients with acute myelogenous leukemia and two patients without underlying hematologic dyscrasia when the biopsies were obtained. Clonal restriction of the neutrophil infiltrate was found in two of the patients with acute myelogenous leukemia; the other two patients were homozygous for the HUMARA gene, precluding analysis. Both control patients had clonal restricted infiltrates within their skin lesions; subsequent investigation revealed unexplained neutropenia with a bone marrow biopsy interpreted as being within normal limits and no further features to suggest a definitive myeloproliferative disorder. These findings demonstrated that clonality of the neutrophilic infiltrate in Sweet's syndrome skin lesions is not exclusively restricted to patients with an established myeloproliferative disease. The significance of the clonal neutrophilic infiltrate in Sweet's syndrome patients without an underlying myeloid dysplasia remains to be determined; however, the investigators speculated that it may have some implications regarding the pathogenesis of sterile neutrophilic infiltrates [429].
Diagnostic methods
Lesional skin biopsy
A lesional skin biopsy for routine histopathologic evaluation is a useful procedure to confirm a clinically suspected diagnosis of Sweet's syndrome. Pathologic features of Sweet's syndrome, such as the diffuse inflammatory infiltrate of neutrophils in the dermis, subcutaneous fat, or both can also be observed in cutaneous lesions caused by an infectious agent. Therefore, it may also be prudent to also submit lesional tissue for bacterial, fungal, mycobacterial, and possibly viral cultures [1, 2].
Laboratory evaluation
The most consistent laboratory abnormalties in patients with Sweet's syndrome are peripheral leukocytosis with neutrophilia and an elevated erythrocyte sedimentation rate [23]. However, an elevated white blood cell count is not always observed in all patients with biopsy-confirmed Sweet's syndrome [26]. For example, some of the patients with malignancy-associated Sweet's syndrome may have either anemia, neutropenia, and/or abnormal platelet counts.
Extracutaneous manifestations of Sweet's syndrome may result in other laboratory abnormalities. Abnormalites may be found on brain SPECTs, computerized axial tomography, electroencephalograms, magnetic resonance imaging and cerebrospinal fluid analysis in patients with central nervous system involvement. Urinalysis abnormalities (hematuria and proteinuria) may be observed in patients with dermatosis-related kidney involvement. Hepatic serum enzyme elevation may be present in patients with Sweet's syndrome-associated liver involvment. Pleural effusions and corticosteroid-responsive culture-negative infiltrates may be present on chest roentgenograms in patients with Sweet's syndrome who have extracutaneous manifestations that involve their lungs [2, 343].
Laboratory evaluation should include a complete blood cell count with leukocyte differential and platelet count. Evaluation of acute phase reactants (such as the erythrocyte sedimentation rate or C-reactive protein), serum chemistries (evaluating hepatic function and renal function) and a urinalysis should also be performed. It may also be reasonable to perform a serologic evaluation for antistreptolysin-O antibody, rheumatoid factor, and thyroid function since streptococcal infection, rheumatoid arthritis, and thyroid disease have been observed to have either a probably or possible bona fide association with the dermatosis [1, 2].
Recommendations for the initial malignancy workup in newly diagnosed Sweet's syndrome patients without a prior cancer were proposed by Cohen and Kurzrock [15] in 1993. Their recommendations were based upon the neoplasms that had concurrently or subsequently been discovered in previously cancer-free Sweet's syndrome patients and the age-related recommendations by the American Cancer Society for the early detection of cancer in asymptomatic persons [406]. They recommended: (1) a detailed medical history; (2) a complete physical examination, including: (a) examination of the thyroid, lymph nodes, oral cavity, and skin; (b) digital rectal examination; (c) breast, ovary, and pelvic examination in women; and (d) prostate and testicle examination in men; (3) laboratory evaluation: (a) carcinoembryonic antigen level; (b) complete blood cell count with leukocyte differential and platelet count; (c) pap test in women; (c) serum chemistries; (d) stool guaiac slide test; (e) urinalysis; and (f) urine culture; and (4) other screening tests: (a) chest roentgenograms; (b) endometrial tissue sampling in either menopausal women or women with a history of abnormal uterine bleeding, estrogen therapy, failure to ovulate, infertility, or obesity; and (c) sigmoidoscopy in patients over 50 years of age. They also suggested that it was reasonable to check a complete blood cell count with leukocyte differential and platelet count every 6 to 12 months since the intial appearance of dermatosis-related skin lesions preceded the diagnosis of a Sweet's syndrome-associated hematologic malignancy by as long as 11 years [2, 15].
Differential diagnosis
Clinical differential diagnosis
There are several mucocutaneous and systemic disorders whose dermatologic manifestations can morpholocally mimic those of Sweet's sydrome. These disorders consist of not only cutaneous conditions and systemic diseases, but also infectious and inflammatory disorders, neoplastic conditions, reactive erythemas, and vasculitis (Figure 10). The clinical differential diagnosis of Sweet's syndrome is listed in Table 8[2, 15, 23, 148, 165, 194, 202, 220, 344, 345, 400, 412, 422].
(a and b). Sweet's syndrome with lesions distributed in a sporotrichoid pattern. A 53-year-old Hispanic woman presented to the emergency room with a recent episode of a "sore throat," fever, and a 2-day history of a swollen, tender left wrist accompanied by erythema that was beginning to extend proximally; a bacterial cellulitis was clinically suspected and she was started on oral antibiotics: double-strength trimethoprim-sulfamethoxazole twice daily and 400 mg of ofloxacin twice daily. She was initially seen in the dermatology clinic 9 days later; she was still febrile and her original lesion had developed into a painful larger pseudovesicular nodule on the radial side of her left wrist. In addition, distal (a) and closer (b) views show a smaller red dermal nodule (between arrows) that appeared on her left arm proximal to the original lesion. The clinical differential diagnosis included infections whose lesions demonstrated a sporotrichoid pattern (sporotrichosis and atypical mycobacterial infection) and Sweet's syndrome. Biopsies for microscopic and culture evaluation were performed. In addition to her antibiotics, the patient was started on oral saturated solution of potassium iodide (3 drops 3 times each day and increased by 1 drop each day to a final dose of 10 drops 3 times each day). The hematoxylin and eosin-stained sections from her biopsy showed a neutrophilic dermatosis; the bacterial, mycobacterial, and fungal cultures were negative for organisms. Within a few days after initiating treatment with potassium iodide, her symptoms resolved and her skin lesions began to improve. (From [23] Cohen PR, Kurzrock R: Sweet's syndrome: a neutrophilic dermatosis classically associated with acute onset and fever. Clin Dermatol 2000;18:265–282. Copyright 2000, Reprinted with permission from Elsevier Ltd, Oxford, United Kingdom.)
Histologic differential diagnosis
The histologic differential diagnosis of Sweet's syndrome includes conditions microscopically characterized by either neutrophilic dermatosis or neutrophilic panniculitis (Table 9) [2–4, 6, 12, 193, 346–353]. Neutrophilic dermatoses include abscess or cellulitis, bowel (intestinal) bypass syndrome, erythema elevatum diutinum, granuloma faciale, halogenoderma, leukocytoclastic vasculitis, neutrophilic eccrine hidradenitis, pyoderma gangrenosum, and rheumatoid neutrophilic dermatitis. Culture of lesional tissue for bacteria, fungi, and mycobacteria should be considered to rule out infection since the pathologic changes associated with Sweet's syndrome are similar to those observed in an abscess or cellulitis [23].
Leukemia cutis can occur concurrently with Sweet's syndrome. It can also mimic the dermal changes of Sweet's syndrome. However, in contrast to the mature polymorphonuclear neutrophils found in Sweet's syndrome, the dermal infiltrate in leukemia cutis consists of malignant immature leukocytes [354].
Subcutaneous Sweet's syndrome lesions may have pathologic changes in the adipose tissue that can be found in either the lobules, the septae, or both. Hence, the adipose tissue changes of subcutaneous Sweet's syndrome are similar to those of other conditions characterized by a neutrophilic lobular and/or septal panniculitis. Therefore, alpha 1-antitrypsin deficiency, factitial panniculitis, infection, leukocytoclastic vasculitis, pancreatitis, and rheumatoid arthritis should be considered and ruled out [2, 4].
Management
Sweet's syndrome lesions, if untreated, can remain for weeks to months. However, without any therapeutic intervention, the dermatosis-related symptoms and cutaneous lesions eventually resolved in some patients with classical Sweet's syndrome [10]. Cure or remission of the dermatosis-related cancer in patients with malignancy-associated Sweet's syndrome is occasionally followed by resolution of the individual's Sweet's syndrome. And, in patients with drug-induced Sweet's syndrome, spontaneous improvement and subsequent clearing of the syndrome occurs after stopping the associated medication. Surgical intervention has also occasionally promoted resolution of the patient's Sweet's syndrome when the dermatosis was associated with therapy amendable tonsillitis, solid tumors, or renal failure.
Topical or intralesional corticosteroids
Topical or intralesional corticosteroids can be used to treat patients who have a small number of localized Sweet's syndrome lesions as either monotherapy or concurrently with another therapy [1, 2, 7]. High potency topical corticosteroids (such as 0.05% clobetasol propionate) in either a cream base, an ointment base, a gel base, or a foam base can be applied to the lesions [13, 19–21, 30, 234, 362–365]. Individual lesions have improved following a single injection or multiple intralesional treatments with triamcinolone acetonide when used at a dose ranging from 3 mg/ml to 10 mg/ml [362, 366, 367].
First-line systemic agents
Systemic corticosteroids are the therapeutic mainstay for Sweet's syndrome. Other first-line systemic treatments for Sweet's syndrome are potassium iodide and colchicine (Table 10) [10, 12, 17, 20, 23, 30, 49, 70, 143, 184, 198, 203, 221, 223, 231, 240, 245, 250, 259, 261, 281, 284, 294, 296, 329, 359–363, 368–384, 397, 410].
Corticosteroids
Systemic corticosteroids are the "gold standard" of therapy for Sweet's syndrome [7, 8, 10, 12, 16, 17, 19, 20, 23, 36, 49, 50, 70, 184, 223, 233, 240, 250, 284, 358–361]. Dermatosis-associated symptoms improve promptly after treatment has been started and the cutaneous lesions resolve subsequently. Systemic corticosteroid therapy often begins with 1 mg/kg/day of prednisone as a single oral morning dose. Usually, the dose can be tapered to 10 mg/day within 4 to 6 weeks. However, some patients may require treatment for 2 to 3 months.
Intravenous corticosteroid therapy may be necessary in those Sweet's syndrome patients whose dermatosis has been refractory to other treatments [400]. Daily pulse intravenous methylprednisolone sodium succinate (at a dose of up to 1000 mg/day) over 1 or more hours for 3 to 5 days can be given. Upon conclusion of the course of intravenous treatment, either a tapering oral dose of corticosteroid or another immunosuppressant agent usually follows.
Potassium iodide
Horio et al [143] originally described the dramatic improvement in patients with Sweet's syndrome who were treated with potassium iodide in 1980. He confirmed his earlier observations with a larger study in 1983 [368]. Subsequently, several other investigators have also observed similar improvement when using potassium iodide to treat patients with Sweet's syndrome. Vasculitis and hypothyroidism are potential drug-induced side effects of potassium iodide [385].
After the initiation of potassium iodide therapy, symptoms of the dermatosis typically resolve within 1 to 2 days and skin lesions subside within 3 to 5 days. Potassium iodide, when available as a 300 mg enteric-coated tablet, can be administered orally 3 times each day (for a total daily dose of 900 mg). Alternatively, when the drug is available as a saturated solution (1 gram/ml of water) of potassium iodide (SSKI, which is also referred to as Lugol's solution), it is initially given at a dose of 3 drops 3 times each day. When a "standard" medicine dropper (which dispenses 20 drops per ml) is used, 1 drop equals 0.05 ml (or 50 mg when the concentration of potassium iodide is 1000 mg/ml). Therefore, the initial dose is 9 drops per day which equals 450 mg of potassium iodide per day. The dose is increased by 1drop 3 times each day, typically to a final dose between 21 drops per day (1050 mg) to 30 drops per day (1500 mg).
Colchicine
The efficacy of colchicine for Sweet's syndrome was initially reported by Suehisa and Tagami [373] in 1981. Two years later, in 1983, Suehisa et al [375] reported 3 additional patients with Sweet's syndrome who were successfully treated with colchicine. Colchicine may cause gastrointestinal symptoms such as diarrhea, abdominal pain, nausea and vomiting. These potential adverse effects from colchicine may improve after lowering the daily dose of the drug [2].
Several larger studies have subsequently confirmed that colchicine is an effective agent for the successful management of patients with Sweet's syndrome. For example, Maillard et al [329] presented 20 patients with Sweet's syndrome of whom 90% (18 individual) responded to colchicine therapy: fever resolved within 2 to 3 days, skin lesions attenuated within 2 to 5 days, arthralgia disappeared within 2 to 4 days, and leukocytosis normalized within 8 to 14 days. Similar to earlier studies, the starting dose of colchicine was 0.5 mg orally 3 times each day (for a total daily dose of 1.5 mg); treatment ranged from 10 to 21 days (mean = 15 days).
Second-line systemic agents
Second-line agents for treating Sweet's syndrome include indomethacin, clofazimine, cyclosporin, and dapsone (Table 11) [1, 12, 17, 20, 30, 203, 221, 231, 245, 259, 261, 284, 294, 296, 372, 378–384, 421]. All of these agents have been used as monotherapy either in the initial management of the patient or after first-line therapies have failed. In addition, cyclosporine and dapsone have been used in combination therapy either with other drugs or as a corticosteroid-sparing agent [1, 2, 7, 303, 421].
Indomethacin and clofazimine
Indomethacin and clofazimine have each been described in individual case reports and a single larger study to be effective for the management of patients with Sweet's syndome. In 1997, Jeanfils et al [261] reported the therapeutic efficacy for 17 of the 18 patients with Sweet's syndrome who received indomethacin as first-line monotherapy: an oral daily dose of 150 mg for 7 days and then 100 mg per day for 14 days. Von den Driesch [12] reported "almost complete remission" in 6 patients who were treated with clofazimine. The patients had chronic and relapsing Sweet's syndrome and had previously been unsuccessfully treated with methylprednisolone; they received an oral daily dose of 200 mg of clofazimine for 4 weeks and then 100 mg per day for 4 more weeks. None of the 6 patients required systemic treatment of their Sweet's syndrome after the clofazimine was discontinued.
Cyclosporin and dapsone
Cyclosporin and dapsone have been used either as monotherapy or in combination with other agents. The initial oral dose of cyclosporin ranged from 2 mg/kg/day [380] to 10 mg/kg/day [12, 381]; for the patient who was receiving 10 mg/kg/day, the dose was reduced by 2 mg/kg/day every 2 days and discontinued on day 21 [12, 381]. The initial oral dose of dapsone ranged from 100 mg per day to 200 mg per day [17, 20, 30, 203, 221, 245, 284, 372, 382–384, 421].
Other systemic agents
There are individual case reports of patients with Sweet's syndrome whose dermatosis has improved after receiving systemic therapy with antibiotics [7]. For example, these include individuals whose lesions have become secondarily impetiginized with Staphylococcus aureus; their dermatosis-related skin lesions often partially improve after treatment with an antimicrobial agent to which the bacterial strain is susceptible [23]. The symptoms and lesion of Sweet's syndrome also resolved in other patients with inflammatory bowel disease (treated with metronidazole) [267, 387], and persons with dermatosis-related Yersinia [125, 126] or Chlamydia [306, 307] infection (treated with either doxycycline [125, 389], minocycline [30, 126], or tetracycline [306, 307, 388]). Resolution of Sweet's syndrome has also been observed following treatment with other antibiotics such as ciprofloxacin, metronidazole, penicillin, or pyrimethamine and sulfonamide; some of these patients also had Sweet's syndrome-associated infections caused by either group D Salmonella [401], Salmonella typhimurium, Streptococcus, Helicobacter pylori, or Toxoplasma.
Other systemic drugs have also been effective for the treatment of Sweet's syndrome. These observations have predominantly been described in case reports. The agents include cytotoxic chemotherapies and antimetabolites (chlorambucil and cyclophosphamide) [30, 39, 148, 200, 251, 360, 390], immunoglobulin [303], interferon alpha [202, 366], etretinate [361], and tumor necrosis factors antagonists (etanercept [392], infliximab [264, 265, 278, 266], and thalidomide [5, 393, 425]). Pentoxifylline was postulated to be of therapeutic benefit for treating Sweet's syndrome [394, 395]; however, it was not found to be efficacious when used as monotherapy [1, 2, 7, 295, 362].
Prognosis
Clinical course
In some patients with classical Sweet's syndrome, the symptoms and lesions of Sweet's syndrome eventually resolved without any therapeutic intervention. However, the lesions may persist for weeks to months [10, 23, 254, 355]. Successful management of the cancer occasionally results in clearing of the related dermatosis in patients with malignancy-associated Sweet's syndrome [13, 15, 23]. Similarly, spontaneous improvement and subsequent resolution of the syndrome typically follows discontinuation of the associated medication in patients with drug-induced Sweet's syndrome [13, 15, 23]. In some of the Sweet's syndrome patients who had dermatosis-associated tonsillitis, solid tumors, or renal failure, surgical intervention resulted in the resolution of the dermatosis [1, 2, 19, 315, 356, 357].
Sweet's syndrome may recur following either spontaneous remission or therapy-induced clinical resolution [10]. The duration of remission is variable between recurrent episodes of the dermatosis. In cancer patients, Sweet's syndrome recurrences are more common. Indeed, the reappearance of dermatosis-associated symptoms and lesions in an oncology patient may represent a paraneoplastic syndrome which is signaling the return of the previously treated malignancy [1, 2, 15, 135].
Complications
Patients with Sweet's syndrome can develop complications which are either directly related to the mucocutaneous lesions or indirectly related to the Sweet's syndrome-associated conditions or both. Antimicrobial therapy may be necessary if the skin lesions may become secondarily infected. Reappearance of the dermatosis may herald the unsuspected discovery that the cancer has recurred in patients with malignancy-associated Sweet's syndrome. Disease-specific treatment may be warranted for the systemic manifestations of Sweet's syndrome-related conditions such as inflammatory bowel disease, sarcoidosis and thyroid diseases.
Abbreviations
- kg:
-
kilogram
- mg:
-
milligrams
- ml:
-
milliliter
- SSKI:
-
saturated solution of potassium iodide
References
Cohen PR, Kurzrock R: Sweet's syndrome revisited: a review of disease concepts. Int J Dermatol. 2003, 42: 761-778. 10.1046/j.1365-4362.2003.01891.x.
Cohen PR: Sweet's syndrome. Orphanet Encyclopedia. 2003, (accessed 25 July 2007)., [http://www.orpha.net/data/patho/GB/uk-Sweet.pdf]
Cohen PR: Skin lesions of Sweet syndrome and its dorsal hand variant contain vasculitis: an oxymoron or an epiphenomenon?. Arch Dermatol. 2002, 138: 400-403. 10.1001/archderm.138.3.400.
Cohen PR: Subcutaneous Sweet's syndrome: a variant of acute febrile neutrophilic dermatosis that is included in the histologic differential diagnosis of neutrophilic panniculitis. J Am Acad Dermatol. 2005, 52: 927-928. 10.1016/j.jaad.2005.03.001.
Cohen PR: Sweet's syndrome and relapsing polychondritis:is their appearance in the same patient a coincidental occurrence or a bonified association of these conditions?. Int J Dermatol. 2004, 43: 772-777. 10.1111/j.1365-4632.2004.02197.x.
Cohen PR: Neutrophilic dermatoses occurring in oncology patients. Int J Dermatol. 2007, 46 (1): 106-111. 10.1111/j.1365-4632.2006.02605.x.
Cohen PR, Kurzrock R: Sweet's syndrome: a review of current treatment options. Am J Clin Dermatol. 2002, 3: 117-131. 10.2165/00128071-200203020-00005.
Sweet RD: An acute febrile neutrophilic dermatosis. Br J Dermatol. 1964, 76: 349-356. 10.1111/j.1365-2133.1964.tb14541.x.
Sweet RD: Acute febrile neutrophilic dermatosis – 1978. Br J Dermatol. 1979, 100: 93-99. 10.1111/j.1365-2133.1979.tb03573.x.
Cohen PR, Almeida L, Kurzrock R: Acute febrile neutrophilic dermatosis. Am Fam Physician. 1989, 39: 199-204.
Su WPD, Liu HNH: Diagnostic criteria for Sweet's syndrome. Cutis. 1986, 37: 167-174.
von den Driesch P: Sweet's syndrome (acute febrile neutrophilic dermatosis). J Am Acad Dermatol. 1994, 31: 535-556.
Walker DC, Cohen PR: Trimethoprim-sulfamethoxazole-associated acute febrile neutrophilic dermatosis: case report and review of drug-induced Sweet's syndrome. J Am Acad Dermatol. 1996, 34: 918-923. 10.1016/S0190-9622(96)90080-8.
Cohen PR, Kurzrock R: Diagnosing the Sweet syndrome. Ann Intern Med. 1989, 110: 573-574.
Cohen PR, Kurzrock R: Sweet's syndrome and cancer. Clin Dermatol. 1993, 11: 149-157. 10.1016/0738-081X(93)90112-P.
Kemmett D, Hunter JAA: Sweet's syndrome: a clinicopathologic review of twenty-nine cases. J Am Acad Dermatol. 1990, 23: 503-507.
Sitjas D, Cuatrecasas M, De Moragas JM: Acute febrile neutrophilic dermatosis (Sweet's syndrome). Int J Dermatol. 1993, 32: 261-268. 10.1111/j.1365-4362.1993.tb04265.x.
Hommel L, Harms M, Saurat JH: The incidence of Sweet's syndrome in Geneva. A retrospective study of 29 cases. Dermatology. 1993, 187: 303-305.
Chan H-L, Lee Y-S, Kuo T-T: Sweet's syndrome: clinicopathologic study of eleven cases. Int J Dermatol. 1994, 33: 425-432. 10.1111/j.1365-4362.1994.tb04045.x.
Fett DL, Gibson LE, Su WPD: Sweet's syndrome: systemic signs and symptoms and associated disorders. Mayo Clin Proc. 1995, 70: 234-240.
Cohen PR, Holder WR, Rapini RP: Concurrent Sweet's syndrome and erythema nodosum: a report, world literature review and mechanism of pathogenesis. J Rheumatol. 1992, 19: 814-820.
Cohen PR, Kurzrock R: The pathogenesis of Sweet's syndrome. J Am Acad Dermatol. 1991, 25: 734-
Cohen PR, Kurzrock R: Sweet's syndrome: a neutrophilic dermatosis classically associated with acute onset and fever. Clin Dermatol. 2000, 18: 265-282. 10.1016/S0738-081X(99)00129-7.
Shapiro L, Baraf CS, Richheimer LL: Sweet's syndrome (acute febrile neutrophilic dermatosis): report of a case. Arch Dermatol. 1971, 103: 81-84. 10.1001/archderm.103.1.81.
Matta M, Kurban AK: Sweet's syndrome: systemic association. Cutis. 1973, 12: 561-565.
Cohen PR, Talpaz M, Kurzrock R: Malignancy-associated Sweet's syndrome: Review of the world literature. J Clin Oncol. 1988, 6: 1887-1897.
Greer KE, Cooper PH: Sweet's syndrome (acute febrile neutrophilic dermatosis). Clin Rheum Dis. 1982, 8: 427-441.
Callen JP: Acute febrile neutrophilic dermatosis (Sweet's syndrome) and the related conditions of "bowel bypass: syndrome and bullous pyoderma gangrenosum. Dermatol Clin. 1985, 3: 153-163.
Costello MJ, Canizares O, Montague M, Buncke CM: Cutaneous manifestations of myelogenous leukemia. Arch Dermatol. 1955, 71: 605-614.
Bourke JF, Keohane S, Long CC, Kemmett D, Davies M, Zaki I, Graham-Brown RAC: Sweet's syndrome and malignancy in the U.K. Br J Dermatol. 1997, 137: 609-613. 10.1111/j.1365-2133.1997.tb03796.x.
Fitzgerald RL, McBurney EI, Nesbitt LT: Sweet's syndrome. Int J Dermatol. 1996, 35: 9-15.
Majeed HA, Kalaawi M, Mohanty D, Teebi AS, Tunjekar MF, Al-Gharbawy F, Majeed SA, Al-Gazzar AH: Congenital dyserythropoietic anemia and chronic recurrent multifocal osteomyelitis in three related children and the association with Sweet's syndrome in two siblings. J Pediatr. 1989, 115: 730-734. 10.1016/S0022-3476(89)80650-X.
Dunn TR, Saperstein HW, Biederman A, Kaplan RP: Sweet' syndrome in a neonate with aseptic meningitis. Pediatr Dermatol. 1992, 9: 288-292.
Boatman BW, Taylor RC, Klein LE: Sweet's syndrome in children. South Med J. 1994, 87: 193-196. 10.1097/00007611-199402000-00009.
Hassouna L, Nabulsi-Khalil M, Mroueh SM, Zaynoun ST, Kibbi A-G: Multiple erythematous tender papules and nodules in an 11-month-old boy: Sweet's syndrome (acute febrile neutrophilic dermatosis). Arch Dermatol. 1996, 132: 1507-1512. 10.1001/archderm.132.12.1507.
Baron F, Sybert VP, Andrews RG: Cutaneous and extracutaneous neutrophilic infiltrates (Sweet's syndrome) in three patients with Fanconi anemia. J Pediatr. 1989, 115: 726-729. 10.1016/S0022-3476(89)80649-3.
Sedel D, Huguet P, Lebbe C, Donadieu J, Odievre M, Labrune PH: Sweet syndrome as the presenting manifestation of chronic granulomatous disease in an infant. Pediatr Dermatol. 1994, 11: 237-240.
Kibbi AG, Zaynoun ST, Kurban AK, Najjar SS: Acute febrileneutrophilic dermatosis (Sweet's syndrome): case report and review of the literature. Pediatr Dermatol. 1985, 3: 40-44.
Shimizu T, Yoshida I, Eguchi H, Takahashi K, Inada H, Ando A, Kato H: Sweet syndrome in a child with aplastic anemia receiving recombinant granulocyte colony-stimulating factor. J Pediatr Hematol Oncol. 1996, 18: 282-284. 10.1097/00043426-199608000-00009.
Schneider DT, Schuppe H-C, Schwamborn D, Koerholz D, Lehmann P, Goebel U: Acute febrile neutrophilic dermatosis (Sweet's syndrome) as initial presentation in a child with acute myelogenous leukemia. Med Pediatr Oncol. 1998, 31: 178-181. 10.1002/(SICI)1096-911X(199809)31:3<178::AID-MPO12>3.0.CO;2-T.
Garty BZ, Levy I, Nitzan M, Barak Y: Sweet syndrome associated with G-CSF treatment in a child with glycogen storage disease type Ib. Pediatrics. 1996, 97: 401-403.
Hwang ST, Williams ML, McCalmont TH, Frieden IJ: Sweet's syndrome leading to acquired cutis laxa (Marshall's syndrome) in an infant with alpha1-antitrypsin deficiency. Arch Dermatol. 1995, 131: 1175-1177. 10.1001/archderm.131.10.1175.
Lipp KE, Shenefelt PD, Nelson RP, Messina JL, Fenske NA: Persistent Sweet's syndrome occurring in a child with a primary immunodeficiency. J Am Acad Dermatol. 1999, 40: 838-841. 10.1053/jd.1999.v40.a95650.
Tuerlinckx D, Bodart E, Despontin K, Boutsen Y, Godding V, Ninane J: Sweet's syndrome with arthritis in a 8-month-old boy. J Rheumatol. 1999, 26: 440-442.
Herron MD, Coffin CM, Vanderhooft SL: Sweet syndrome in two children. Pediatr Dermatol. 2005, 22: 525-529. 10.1111/j.1525-1470.2005.00132.x.
Parsapour K, Reep MD, Gohar K, Shah V, Church A, Shwayder TA: Familial Sweet's syndrome in 2 brothers, both seen in the first 2 weeks of life. J Am Acad Dermatol. 2003, 49: 132-138. 10.1067/mjd.2003.328.
Prasad PV, Ambujam S, Priya K, Padma K, Rehana T: Sweet's syndrome in an infant – report of a rare case. Int J Dermatol. 2002, 41: 928-930. 10.1046/j.1365-4362.2002.01681_1.x.
Kourtis AP: Sweet syndrome in infants. Clin Pediatr (Phila). 2002, 41: 175-177.
Cohen PR, Kurzrock R: Chronic myelogenous leukemia and Sweet syndrome. Am J Hematol. 1989, 32: 134-137. 10.1002/ajh.2830320211.
Cohen PR: Acral erythema: a clinical review. Cutis. 1993, 20: 15-20.
Cohen PR: Cutaneous paraneoplastic syndromes. Am Fam Physician. 1994, 50: 1273-1282.
Kurzrock R, Cohen PR: Mucocutaneous paraneoplastic manifestationsof hematologic malignancies. Am J Med. 1995, 99: 207-216. 10.1016/S0002-9343(99)80141-7.
Kurzrock R, Cohen PR: Cutaneous paraneoplastic syndromes in solid tumors. Am J Med. 1995, 99: 662-671. 10.1016/S0002-9343(99)80254-X.
Cohen PR: Cutaneous manifestations of internal malignancy. Current Practice of Medicine. (Section V, Dermatology). Edited by: Callen JP (Dermatology section editor); [Series editor Bone RC]. 1996, Philadelphia, PA: Current Medicine, Inc, 2 (V): 19.1-19.3.
Cohen PR, Kurzrock R: Paraneoplastic syndromes of the skin. Current Diagnosis 9. Edited by: Conn RB, Borer WZ, Snyder JW. 1997, Philadelphia: W.B. Saunders Company, 1199-1206.
Cohen PR, Kurzrock R: Mucocutaneous paraneoplastic syndromes. Seminars in Oncology. 1997, 24: 334-359.
Cohen PR: Cutaneous paraneoplastic syndromes associated with lung cancer. Mayo Clin Proc. 1993, 68: 620-621.
Cohen PR: Cutaneous paraneoplastic syndromes and genodermatoses with malignant potential. Acta Derm Venereol Stockh). 1974, 74: 229-230.
Cohen PR, Kurzrock R: Mucocutaneous paraneoplastic manifestations of hematologic malignancies. The reply. Am J Med. 1996, 101: 231-233.
Cohen PR, Kurzrock R: Paraneoplastic Sweet's syndrome. Emergency Med. 1994, 26: 37-38.
Haverstock C, Libecco JF, Sadeghi P, Maytin E: Tender erythematous plaques in a woman with acute myelogenous leukemia. Arch Dermatol. 2006, 142: 235-240. 10.1001/archderm.142.2.235-b.
Disel U, Paydas S, Yavuz S, Tuncer I, Alpay R: Bilateral ear Sweet's syndrome in a case with relapse acute myeloblastic leukemia. Leuk Res. 2006, 30: 364-10.1016/j.leukres.2005.08.003.
Sudhakar MK, Kallarakkal JT, Damodharan J, Sahib K, Mahajan A, Kannan R: Sweet's syndrome preceding carcinoma of the adrenal cortex. J Indian Med Assoc. 2005, 103: 433-435.
Hussein K, Nanda A, Al-Sabah H, Alsaleh QA: Sweet's syndrome (acute febrile neutrophilic dermatosis) associated with adenocarcinoma of prostate and transitional cell carcinoma of urinary bladder. J Eur Acad Dermatol Venereol. 2005, 19: 597-599. 10.1111/j.1468-3083.2005.01207.x.
Culp L, Crowder S, Hatch S: A rare association of Sweet's syndorme with cervical cancer. Gynecol Oncol. 2004, 95: 396-399. 10.1016/j.ygyno.2004.06.050.
Dereure O, Ebrard-Charra S, Guillon F, Baldet P, Guilhou JJ: Sweet's syndrome associated with pheochromocytoma. Dermatology. 2004, 208: 175-10.1159/000076499.
Saez M, Garcia-Bustinduy M, Noda A, Dorta S, Escoda M, Fagundo E, Rodriguez F, Guimera F, Sanchez R, Garcia-Montelongo R: Drug-induced Sweet's syndrome. J Eur Acad Dermatol Venereol. 2004, 18: 233-10.1111/j.1468-3083.2004.00866.x.
Stenzel W, Frosch PJ, Schwarz M: Sweet's syndrome associated with acute benign encephalitis. A drug induced etiology. J Neurol. 2003, 250: 770-771. 10.1007/s00415-003-1092-2.
Del Giudice P, Vandenbos F, Perrin C, Bernard E, Marq L, Dellamonica P: Sweet's syndrome following abacavir therapy. J Am Acad Dermatol. 2004, 51: 474-475. 10.1016/j.jaad.2003.09.033.
Cox NH, O'Brien HAW: Sweet's syndrome associated with trans-retinoic acid treatment in acute promyelocytic leukemia. Clin Exp Dermatol. 1994, 19: 51-52. 10.1111/j.1365-2230.1994.tb01115.x.
Piette WW, Trapp JF, O'Donnell MJ, Argenyi Z, Talbot EA, Burns CP: Acute neutrophlic dermatosis with myeloblastic infiltrate in a leukemia patient receiving all-trans-retinoic acid therapy. J Am Acad Dermatol. 1994, 30: 293-297.
Tomas JF, Escudero A, Fernandez-Ranada J: All-trans retinoic acid treatment and Sweet syndrome. Leukemia. 1994, 8: 1596-
Christ E, Linka A, Jacky E, Speich R, Marincek B, Schaffner A: Sweet's syndrome involving the musculoskeletal system during treatment of promyelocytic leukemia with all-trans retinoic acid. Leukemia. 1996, 10: 731-734.
Al-Saad K, Khanani MF, Naqvi A, Krafchik B, Grant R, Pappo A: Sweet syndrome developing during treatment with all-trans retinoic acid in a child with acute myelogenous leukemia. J Pediatr Hematol Oncol. 2004, 26: 197-199. 10.1097/00043426-200403000-00011.
Melinkeri SR, Gupta RK, Dabadghao S: A Sweet-like syndrome manifesting as gingival hyperplasia and myositis without cutaneous involvement. Ann Hematol. 2002, 81: 397-398. 10.1007/s00277-002-0470-7.
Astudillo L, Loche F, Reynish W, Rigal-Huguet F, Lamant L, Pris J: Sweet's syndrome associated with retinoic acid syndrome in a patient with promyelocytic leukemia. Ann Hematol. 2002, 81: 111-114. 10.1007/s00277-001-0416-5.
Park CJ, Bae YD, Choi JY, Heo PS, Lee KS, Park YS, Lee JA: Sweet's syndrome during the treatment of acute promyelocytic leukemia with all-trans retinoic acid. Korean J Intern Med. 2001, 16: 218-221.
Van Regenmortel N, Van de Voorde K, De Raeve H, Rombouts S, Van deVelde A, Lambert J, Schroyens W: Bortezomib-induced Sweet's syndrome. Haematologica. 2005, 90: ECR43-
Knoops L, Jacquemain A, Tennstedt D, Theate I, Ferrant A, van den Neste E: Bortezomib-induced Sweet syndrome. Br J Haematol. 2005, 131: 142-10.1111/j.1365-2141.2005.05636.x.
Fye KH, Crowley E, Berger TG, LeBoit PE, Connolly MK: Celecoxib-induced Sweet's syndrome. J Am Acad Dermatol. 2001, 45: 300-302. 10.1067/mjd.2001.114587.
Gyorfy A, Kovacs T, Szegedi I, Olah E, Kiss C: Sweet's syndrome associated with 13-cis-retinoic acid (isotretinoin) therapy. Med Pediatr Oncol. 2003, 40: 135-136. 10.1002/mpo.10089.
Sconfeldt-Lecuona C, Connemann BJ: Sweet's syndrome and polyserositis with clozapine. Am J Psychiatry. 2002, 159: 1947-10.1176/appi.ajp.159.11.1947.
Saez M, Garcia-Bustinduy M, Noda A, Guimera F, Dorta S, Escoda M, Fagundo E, Sanchez R, Martin-Herrera A, Garcia Montelongo R: Sweet's syndrome induced by oral contraceptive. Dermatology. 2002, 204: 84-10.1159/000051820.
Tefany FJ, Georgouras K: A neutrophilic reaction of Sweet's syndrome type associated with the oral contraceptive. Australas J Dermatol. 1991, 32: 55-59. 10.1111/j.1440-0960.1991.tb00684.x.
Hamill M, Bowling J, Vega-Lopez F: Sweet's syndrome and a Mirena intrauterine system. J Fam Plann Reprod Health Care. 2004, 30: 115-116. 10.1783/147118904322995519.
Guimera FJ, Garcia-Bustinduy M, Noda A, Saez M, Dorta S, Sanchez R, Martin-Herrera A, Garcia-Montelongo R: Diazepam-associated Sweet's syndrome. Int J Dermatol. 2000, 39: 795-798. 10.1046/j.1365-4362.2000.00051.x.
Ginarte M, Garcia-Doval I, Toribio J: Sweet's syndrome: a study of 16 cases. Med Clin Barc. 1997, 109: 588-591.
Govindarajan G, Bashir Z, Kuppuswamy S, Brooks C: Sweet syndrome associated with furosemide. South Med J. 2005, 98: 570-572. 10.1097/01.SMJ.0000157530.63614.9B.
Paydas S, Berksoy S, Seyrek E, Soylu M, Gonlusen G, Acar A, Tuncer I: Sweet's syndrome associated with G-CSF. Br J Haematol. 1993, 85: 191-192.
Park JW, Mehrotra B, Barnett BO, Baron AD, Venook AP: The Sweet syndrome during therapy with granulocyte-colony stimulating factor. Ann Intern Med. 1992, 116: 996-998.
Peters MS, Argenyi Z, Cerio R, Finan M, Gagne E, Scott G: Friday evening slide symposium. J Cutan Pathol. 1993, 20: 465-478. 10.1111/j.1600-0560.1993.tb00673.x.
Morioka N, Otsuka F, Nogita T, Igisu K, Urabe A, Ishibashi Y: Neutrophilic dermatosis with myelodysplastic syndrome: nuclear segmentation anomalies of neutrophils in the skin lesion and in peripheral blood. J Am Acad Dermatol. 1990, 23: 247-249.
Van Kamp H, Van den Berg E, Timens W, Kraaijenbrink RA, Halie MR, Daenen SM: Sweet's syndrome in myeloid malignancy: a report of two cases. Br J Haematol. 1994, 86: 415-417.
Asnis LA, Gaspar AA: Cutaneous reactions to recombinant cytokine therapy. J Am Acad Dermatol. 1995, 33: 393-410. 10.1016/0190-9622(95)91382-3.
Jain KK: Sweet's syndrome associated with granulocyte colony-stimulating factor. Cutis. 1966, 57: 107-110.
Prevost-Blank PL, Shwayder TA: Sweet's syndrome secondary to granulocyte colony-stimulating factor. J Am Acad Dermatol. 1996, 35: 995-997. 10.1016/S0190-9622(96)90132-2.
Richard MA, Grob JJ, Laurans R, Hesse S, Brunet P, Stoppa AM, Bonerandi JJ, Berland Y, Maraninchi D: Sweet's syndrome induced by granulocyte colony-stimulating factor in a woman with congenital neutropenia. J Am Acad Dermatol. 1996, 35: 629-631. 10.1016/S0190-9622(96)90693-3.
Berger TG, Dhar A, McCalmont TH: Neutrophilic dermatoses in HIV infection. J Am Acad Dermatol. 1994, 31: 1045-1047.
Fukutoku M, Shimizu S, Ogawa Y, Takeshita S, Masaki Y, Arai T, Hirose Y, Sugal S, Konda S, Takiguchi T: Sweet's syndrome during therapy with granulocyte colony-stimulating factor in a patient with aplastic anaemia. Br J Haematol. 1994, 86: 645-648.
Petit T, Frances C, Marinho E, Herson S, Chosidow O: Lymphoedema-area-restricted Sweet syndrome during G-CSF treatment. Lancet. 1996, 347: 690-10.1016/S0140-6736(96)91241-6.
Paydas S, Sahin B, Zorludemir S: Sweet's syndrome accompanying leukaemia: seven cases and review of the literature. Leuk Res. 2000, 24: 83-86. 10.1016/S0145-2126(99)00140-X.
Arbetter KR, Hubbard KW, Markovic SN, Gibson LE, Phyliky RL: Case of granulocytic colony-stimulating factor-induced Sweet's syndrome. Am J Hematol. 1999, 61: 126-129. 10.1002/(SICI)1096-8652(199906)61:2<126::AID-AJH9>3.0.CO;2-8.
White JM, Mufti GJ, Salisbury JR, du Vivier AWP: Cutaneous manifestations of granulocyte colony-stimulating factor. Clin Exp Dermatol. 2006, 31: 206-207. 10.1111/j.1365-2230.2005.01996.x.
Abecassis S, Ingen-Housz-Oro S, Cavelier-Balloy B, Arnulf B, Bachelez H, Dubertret L: Particular histological features of a case of Sweet's syndrome induced by G-CSF. Ann Dermatol Venereol. 2004, 131: 369-372.
Bayer-Garner IB, Cottler-Fox M, Smoller BR: Sweet syndrome in multiple myeloma: a series of six cases. J Cutan Pathol. 2003, 30: 261-264. 10.1046/j.0303-6987.2002.029.x.
Kumar G, Bernstein JM, Waibel JS, Baumann MA: Sweet's syndrome associated with sargramostim (granulocyte-macrophage colony stimulating factor) treatment. Am J Hematol. 2004, 76: 283-285. 10.1002/ajh.20112.
Gilmour E, Chalmers RJG, Rowlands DJ: Drug-induced Sweet's syndrome (acute febrile neutrophilic dermatosis) associated with hydralazine. Br J Dermatol. 1995, 133: 490-491. 10.1111/j.1365-2133.1995.tb02686.x.
Ayirookuzhi SJ, Ma L, Ramshesh P, Mills G: Imatinib-induced Sweet syndrome in a patient with chronic myeloid leukemia. Arch Dermatol. 2005, 141: 368-370. 10.1001/archderm.141.3.368.
Liu D, Seiter K, Mathews T, Madahar CJ, Ahmed T: Sweet's syndrome with CML cell infiltration of the skin in a patient with chronic-phase CML while taking imatinib mesylate. Leuk Res. 2004, 28: S61-S63. 10.1016/S0145-2126(03)00257-1.
Mensing H, Kowalzick L: Acute febrile neutrophilic dermatosis (Sweet's syndrome) caused by minocycline. Dermatologica. 1991, 182: 43-46.
Thibault M-J, Billick RC, Srolovitz H: Minocycline-induced Sweet's syndrome. J Am Acad Dermatol. 1992, 27: 801-804.
Khan Durani B, Jappe U: Drug-induced Sweet's syndrome in acne caused by different tetracyclines: case report and review of the literature. Br J Dermatol. 2002, 147: 558-562. 10.1046/j.1365-2133.2002.04817.x.
Retief CR, Malkinson FD: Nitrofurantoin-associated Sweet's syndrome. Cutis. 1999, 63: 177-179.
Aguiar-Bujanda D, Aguiar-Morales J, Bohn-Sarmiento U: Sweet's syndrome associated with norfloxacin in a prostate cancer patient. QJM. 2004, 97: 55-56. 10.1093/qjmed/hch011.
Ozdemir D, Korkmaz U, Sahin I, Sencan I, Kavak A, Kucukbayrak A, Selma C: Ofloxacin induced Sweet's syndrome in a patient with Crohn's disease. J Infect. 2006, 52: e155-e157. 10.1016/j.jinf.2005.08.002.
Draper BK, Robbins JR, Stricklin GP: Bullous Sweet's syndrome in congenital neutropenia: association with pegfilgrastim. J Am Acad Dermatol. 2005, 52: 901-905. 10.1016/j.jaad.2004.12.028.
Miller RM, Darben TA, Nedwich J, Savige J: Propylthiouracil-induced antineutrophil cytoplasmic antibodies in a patient with Graves' disease and a neutrophilic dermatosis. Br J Dermatol. 1999, 141: 931-955. 10.1046/j.1365-2133.1999.03186.x.
Choi HS, Kim HJ, Lee TH, Lee SH, Lee TW, Ihm CG, Kim MJ: Quinupristin/dalfopristin-induced Sweet's syndrome. Korean J Intern Med. 2003, 18: 187-190.
Choi JW, Chung KY: Sweet's syndrome with systemic lupus erythematosus and herpes zoster. Br J Dermatol. 1999, 140: 1174-1175.
Mecca P, Tobin E, Andrew Carlson J: Photo-distributed neutrophilic drug eruption and adult respiratory distress syndrome associated with antidepressant therapy. J Cutan Pathol. 2004, 31: 189-194. 10.1111/j.0303-6987.2004.00155.x.
Keefe M, Wakeel RA, Kerr REI: Sweet's syndrome, plantar pustulosis, and vulvar pustules. Clin Exp Dermatol. 1988, 13: 344-346. 10.1111/j.1365-2230.1988.tb00720.x.
Cobb MW: Furosemide-induced eruption simulating Sweet's syndrome. J Am Acad Dermatol. 1989, 21: 339-343.
Ramsey-Goldman R, Franz T, Solano FX, Medsger TA: Hydralazine-induced lupus and Sweet's syndrome. Report and review of the literature. J Rheumatol. 1990, 17: 682-684.
Sequiera W, Polinsky RB, Alrenga DP: Neutrophilic dermatosis (Sweet's syndrome). Association with a hydralazine-induced lupus syndrome. Am J Med. 1986, 81: 558-560. 10.1016/0002-9343(86)90316-5.
Elsner P, Hartmann AA, Lechner W: Sweet's syndrome associated with Yersinia enterocolitica infection. Dermatologica. 1986, 173: 85-89.
Escallier F, Gaudard S, Courtois JM, Dalac S, Collet E, Lambert D: Sweet's syndrome and Yersinia enterocolitica infection. Ann Dermatol Venereol. 1990, 117: 858-860.
Honigsmann H, Cohen PR, Wolff K: Acute febrile neutrophilic dermatosis (Sweet's syndrome). (Chapter 94). Fitzpatrick's Dermatology in General Medicine. Edited by: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, Fitzpatrick TB. 2003, New York: McGraw-Hill Health Professions Division, 949-955. 6
Reuss-Borst MA, Pawelec G, Saal JG, Horny HP, Muller CA, Waller HD: Sweet's syndrome associated with myelodysplasia: possible role of cytokines in the pathogenesis of the disease. Br J Haematol. 1993, 84: 356-358.
Kawakami T, Ohashi S, Kawa Y, Takahama H, Ito M, Soma Y, Mizoguchi M: Elevated serum granulocyte colony-stimulating factor levels in patients with active phase of Sweet syndrome and patients with activeBehcet disease: implication in neutrophil apoptosis dysfunction. Arch Dermatol. 2004, 140: 570-574. 10.1001/archderm.140.5.570.
Giasuddin ASM, El-Orfi AHAM, Ziu MM, El-Barnaw NY: Sweet's syndrome: is the pathogenesis mediated by helper T cell type 1 cytokines?. J Am Acad Dermatol. 1998, 39: 940-943. 10.1016/S0190-9622(98)70266-X.
Bourke JF, Jones JL, Fletcher A, Graham-Brown RAC: An immunohistochemical study of the dermal infiltrate and epidermal staining for interleukins 1 in 12 cases of Sweet's syndrome. Br J Dermatol. 1996, 134: 705-709. 10.1046/j.1365-2133.1996.81843.x.
Reuss-Borst MA, Muller CA, Waller HD: The possible role of G-CSF in the pathogenesis of Sweet's syndrome. Leuk Lymphoma. 1994, 15: 261-264.
Bielsa S, Baradad M, Marti RM, Casanova JM: Sweet's syndrome with bullous lesions. Actas Dermosifiliogr. 2005, 96: 315-316.
Voelter-Mahlknecht S, Bauer J, Metzler G, Fierlbeck G, Rassner G: Bullous variant of Sweet's syndrome. Int J Dermatol. 2005, 44: 946-947. 10.1111/j.1365-4632.2004.02287.x.
Cohen PR, Kurzrock R: Sweet's syndrome and malignancy. Am J Med. 1987, 82: 1220-1226. 10.1016/0002-9343(87)90229-4.
Honigsmann H, Cohen PR, Wolff K: Acute febrile neutrophilic dermatosis (Sweet's syndrome) (Chapter 93). Fitzpatrick's Dermatology in General Medicine. Edited by: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, Fitzpatrick TB. 1999, New York, McGraw-Hill Health Professions Division, 1117-1123. 5
Delmonte S, Brusati C, Parodi A, Rebora A: Leukemia-related Sweet's syndrome elicited by pathergy to arnica. Dermatology. 1998, 197: 195-196.
Astudillo L, Sailler L, Launay F, Josse AG, Lamant L, Couret B, Arlet-Suau E: Pulmonary involvement in Sweet's syndrome: a case report and review of the literature. Int J Dermatol. 2006, 45: 677-680. 10.1111/j.1365-4632.2006.02585.x.
van der Meij EH, Epstein JB, Hay J, Ho V, Lerner K: Sweet's syndrome in a patient with oral cancer associated with radiotherapy. Eur J Cancer B Oral Oncol. 1996, 32B: 133-136. 10.1016/0964-1955(95)00070-4.
Dawe SA, Phillips R, Porter W, Francis NA, Bunker CB: Sweet's syndrome as a complication of radiotherapy for squamous carcinoma of the pharynx. Br J Dermatol. 2003, 149: 884-10.1046/j.1365-2133.2003.05541.x.
Vergara G, Vargas-Machuca I, Pastor MA, Farina MC, Martin L, Requena L: Localization of Sweet's syndrome in radiation-induced locus minoris resistentae. J Am Acad Dermatol. 2003, 49: 907-909. 10.1016/S0190-9622(03)01832-2.
Greer JM, Rosen T, Tschen JA: Sweet's syndrome with an exogenous cause. Cutis. 1993, 51: 112-114.
Horio T, Imamura S, Danno K, Furukawa F, Ofuji S: Treatment of acute febrile neutrophilic dermatosis (Sweet's syndrome) with potassium iodide. Dermatologica. 1980, 160: 341-347.
Belhadjali H, Marguery MC, Lamant L, Giordano-Labadie F, Bazex J: Photosensitivity in Sweet's syndrome: two cases that were photoinduced and photoaggravated. Br J Dermatol. 2003, 149: 675-677. 10.1046/j.1365-2133.2003.05487.x.
Bessis D, Dereure O, Peyron JL, Augias D, Guilhou JJ: Photoinduced Sweet syndrome. Arch Dermatol. 2001, 137: 1106-1108.
Demitsu T, Tadaki T: Atypical neutrophilic dermatosis on the upper extremity affected by postmastectomy lymphedema: report of 2 cases. Dermatologica. 1991, 183: 230-233.
Sommer S, Wilkinson SM, Merchant WJ, Goulden V: Sweet's syndrome presenting as palmoplantar pustulosis. J Am Acad Dermatol. 2000, 42: 332-334. 10.1016/S0190-9622(00)90105-1.
Sarkany RPE, Burrows NP, Grant JW, Pye RJ, Norris PG: The pustular eruption of ulcerative colitis: a variant of Sweet's syndrome. Br J Dermatol. 1998, 138: 365-366. 10.1046/j.1365-2133.1998.02099.x.
Jorizzo JL, Solomon AR, Zanolli MD, Leshin B: Neutrophilic vascular reactions. J Am Acad Dermatol. 1988, 19: 983-1005.
Strutton G, Weedon D, Robertson I: Pustular vasculitis of the hands. J Am Acad Dermatol. 1995, 32: 192-198. 10.1016/0190-9622(95)90125-6.
Galaria NA, Junkins-Hopkins JM, Kligman D, James WD: Neutrophilic dermatosis of the dorsal hands: pustular vasculitis revisited. J Am Acad Dermatol. 2000, 43: 870-874. 10.1067/mjd.2000.109286.
DiCaudo DJ, Connolly SM: Neutrophilic dermatosis (pustular vasculitis) of the dorsal hands: a report of seven cases and review of the literature. Arch Dermatol. 2002, 138: 361-365. 10.1001/archderm.138.3.361.
Curco N, Pagerols X, Tarroch X, Vives P: Pustular vasculitis of the hands. Report of two men. Dermatology. 1998, 196: 346-347. 10.1159/000017911.
Hall AP, Goudge RJ, Ireton HJ, Burrell LM: Pustular vasculits of the hands. Australas J Dermatol. 1999, 40: 204-207. 10.1046/j.1440-0960.1999.00362.x.
Walling HW, Snipes CJ, Gerami P, Piette WW: The relationship between neutrophilic dermatosis of the dorsal hands and sweet syndrome: report of 9 cases and comparison to atypical pyoderma gangrenosum. Arch Dermatol. 2006, 142: 57-63. 10.1001/archderm.142.1.57.
Boye T, Terrier JP, Guennoc B, Fournier B, Carsuzaa F: Neutrophilic dermatosis of the hands. A localized subset of Sweet's syndrome: 3 cases. Ann Dermatol Venereol. 2005, 132: 883-885.
Larsen HK, Danielsen AG, Krustrup D, Weismann K: Neutrophilic dermatosis of the dorsal hands. J Eur Acad Dermatol Venereol. 2005, 19: 634-637. 10.1111/j.1468-3083.2005.01241.x.
Aydin F, Senturk N, Yildiz L, Canturk M, Turanli A: Neutrophilic dermatosis of the dorsal hands in a farmer. J Eur Acad Dermatol Venereol. 2004, 18: 716-717. 10.1111/j.1468-3083.2004.01059.x.
Weenig RH, Bruce AJ, McEvoy MT, Gibson LE, Davis MD: Neutrophilic dermatosis of the hands: four new cases and review of the literature. Int J Dermatol. 2004, 43: 95-102. 10.1111/j.1365-4632.2004.01845.x.
Stransky L, Broshtilova V: Neutrophilic dermatosis of the dorsal hands elicited by thermal injury. Contact Dermatitis. 2003, 49: 42-10.1111/j.0105-1873.2003.0120a.x.
Baz K, Yaziei AC, Kaya TI, Ikizoglu G, Ulubas B, Apa DD, Cinel L: Neutrophilic dermatosis of the hands (localized Sweet's syndrome) in association with chronic hepatitis C and sarcoidosis. Clin Exp Dermatol. 2003, 28: 377-379. 10.1046/j.1365-2230.2003.01299.x.
Ayoub N, Tomb R: Neutrophilic dermatosis of the dorsal hands: a variant of erythema elevatum diutinum?. Arch Dermatol. 2003, 139: 102-10.1001/archderm.139.1.102.
James WD: Newer neutrophilic dermatoses. Arch Dermatol. 2003, 139: 101-102. 10.1001/archderm.139.1.101.
Marie I, Boyer A, Heron F, Joly P, Levesque H, Thomine E, Courtois H: Focal aseptic osteitis underlying neutrophilic dermatosis. Br J Dermatol. 1998, 139: 744-745. 10.1046/j.1365-2133.1998.02482.x.
Morgan KW, Callen JP: Sweet's syndrome in acute myelogenous leukemia presenting as periorbital cellulitis with an infiltrate of leukemic cells. J Am Acad Dermatol. 2001, 45: 590-595. 10.1067/mjd.2001.119032.
Florez A, Sanchez-Aguilar D, Roson E, Prieto A, Van den Eyden A, Toribio J: Sweet's syndrome associated with Salmonella enteritidis infection. Clin Exp Dermatol. 1999, 24: 237-242. 10.1046/j.1365-2230.1999.00465.x.
Jordaan HF: Acute febrile neutrophilic dermatosis. A histopathological study of 37 patients and a review of the literature. Am J Dermatopathol. 1989, 11: 99-111.
Going JJ, Going SM, Myskow MW, Beveridge GW: Sweet's syndrome: histological and immunohistochemical study of 15 cases. J Clin Pathol. 1987, 40: 175-179. 10.1136/jcp.40.2.175.
Honigsmann H, Wolff K: Acute febrile neutrophilic dermatosis (Sweet's syndrome). Major Problems in Dermatology, Vasculitis. Edited by: Wolff K, Winkelmann FK. [Consulting editor, Rook A]. 1980, London: Lloyd-Luke, 10: 307.
Suzuki Y, Kuroda K, Kojima T, Fujita M, Iseki T, Shinkai H: Unusual cutaneous manifestations of myelodysplastic syndrome. Br J Dermatol. 1995, 133: 483-486. 10.1111/j.1365-2133.1995.tb02684.x.
Cooper PH, Frierson HF, Greer KE: Subcutaneous neutrophilic infiltrates in acute febrile neutrophilic dermatosis. Arch Dermatol. 1983, 119: 610-611. 10.1001/archderm.119.7.610.
Cullity J, Maguire B, Gebauer K: Sweet's panniculitis. Australas J Dermatol. 1991, 32: 61-64. 10.1111/j.1440-0960.1991.tb00063.x.
Vignon-Pennamen M-D, Wallach D: Cutaneous manifestations of neutrophilic disease. A study of seven cases. Dermatologica. 1991, 183: 255-264.
Matsumura Y, Tanabe H, Wada Y, Ohta K, Okamoto H, Imamura S: Neutrophilic panniculitis associated with myelodysplastic syndromes. Br J Dermatol. 1997, 136: 142-144. 10.1111/j.1365-2133.1997.tb08775.x.
Sutra-Loubet C, Carlotti A, Guillemette J, Wallach D: Panniculite neutrophilique (P151 at the Journees Dermatologiques de Paris, December 6–9, 2000). Ann Dermatol Venereol (Paris). 2000, 127: 4S176-4S177.
Sutra-Loubet C, Carlotti A, Guillemette J, Wallach D: Neutrophilic lobular panniculitis. J Am Acad Dermatol. 2004, 50: 280-285. 10.1016/j.jaad.2003.10.006.
Hasegawa M, Sato S, Nakada M, Nitta H, Shirasaki H, Kasahara K, Takehara K: Sweet's syndrome associated with granulocyte colony-stimulating factor. Eur J Dermatol. 1998, 8: 503-505.
Cho K-H, Han K-H, Kim S-W, Youn S-W, Youn J-I, Kim B-K: Neutrophilic dermatoses associated with myeloid malignancies. Clin Exp Dermatol. 1997, 22: 269-273. 10.1111/j.1365-2230.1997.tb01093.x.
Leibowitz MR, Rippey JJ, Bezwoda WR, Carman HA: Unusual aspects of febrile neutrophilic dermatosis (Sweet's syndrome). Case reports. S Afr Med J. 1982, 62: 375-378.
Chmel J, Armstrong D: Sweet's syndrome. South Med J. 1978, 71: 1350-1352.
Evans S, Evans CC: Acute febrile neutrophilic dermatosis – two cases. Dermatologica. 1971, 143: 153-159.
Rahav G, Moses A, Michaeli J: Acute febrile neutrophilic dermatosis (Sweet's syndrome). Cutis. 1989, 44: 157-159.
Cooper PH, Innes DJ, Greer KE: Acute febrile neutrophilic dermatosis (Sweet's syndrome) and myeloproliferative disorders. Cancer. 1983, 51: 1518-1526. 10.1002/1097-0142(19830415)51:8<1518::AID-CNCR2820510827>3.0.CO;2-U.
Megarbane B, Bodemer C, Valensi F, Radford-Weiss I, Fraitag S, MacIntyre E, Bletry O, Varet B, Hermine O: Association of acute neutrophilic dermatosis and myelodysplastic syndrome with (6;9) chromosome translocation: a case report and review of the literature. Br J Dermatol. 2000, 143: 1322-1324. 10.1046/j.1365-2133.2000.03912.x.
Maalouf T, Angioi K, Ssi-Yan-Kai I, Vernerey F, Witz B, George J: Dacryoadenitis associated with subcutaneous Sweet's syndrome in a patient with acute myeloid leukemia. Orbit. 2005, 24: 55-57. 10.1080/01676830590903562.
Ben-Noun L: Sweet's syndrome associated with erythema nodosum. Aust Fam Physician. 1995, 24: 1867-1869.
Waltz KM, Long D, Marks JG, Billingsley EM: Sweet's syndrome and erythema nodosum: the simultaneous occurrence of 2 reactive dermatoses. Arch Dermatol. 1999, 135: 62-66. 10.1001/archderm.135.1.62.
Wilkinson SM, Heagerty AHM, English JSC: Acute febrile neutrophilic dermatosis in association with erythema nodosum and sarcoidosis. Clin Exp Dermatol. 1993, 18: 47-49. 10.1111/j.1365-2230.1993.tb00966.x.
Wasson S, Folzenlogen D: Concurrent occurrence of Sweet's syndrome and erythema nodosum: an overlap in the spectrum of reactive dermatoses. Clin Rheumatol. 2006, 25: 268-272. 10.1007/s10067-006-1171-8.
Ginarte M, Toribio J: Association of Sweet syndrome and erythema nodosum. Arch Dermatol. 2000, 136: 673-674. 10.1001/archderm.136.5.673-a.
Malone JC, Stone SP: Sweet syndrome: a disease in histologic evolution?. Arch Dermatol. 2005, 141: 893-895. 10.1001/archderm.141.7.893.
Malone JC, Stone SP, Wills-Frank LA, Fearneyhough PK, Lear SC, Goldsmith LJ, Hood AF, Callen JP: Vascular inflammation (vasculitis) in Sweet syndrome: a clinicopathologic study of 28 biopsy specimens from 21 patients. Arch Dermatol. 2002, 138: 345-349. 10.1001/archderm.138.3.345.
Von den Driesch P: Sweet's syndrome and vasculitis. J Am Acad Dermatol. 1996, 34: 539-10.1016/S0190-9622(96)90470-3.
Chiang C-T, Chan H-L, Kuo T-T, Wang P-N: Herpes zoster-like Sweet's syndrome in acute myelogenous leukemia. Int J Dermatol. 1997, 36: 717-718. 10.1046/j.1365-4362.1997.d01-786.x.
Fujimoto N, Tajima S, Ishibashi A, Ura-Ishikou A, Manaka I: Acute febrile neutrophilic dermatosis (Sweet's syndrome) in a patient with relapsing polychondritis. Br J Dermatol. 1998, 139: 930-931. 10.1046/j.1365-2133.1998.02536.x.
Wallach D: Neutrophilic disease. Rev Prat (Paris). 1999, 49: 356-358.
Greer KE, Pruitt JL, Bishop GF: Acute febrile neutrophilic dermatosis (Sweet syndrome). Arch Dermatol. 1975, 111: 1461-1463. 10.1001/archderm.111.11.1461.
Smith HR, Ashton RE, Beer TW, Theaker JM: Neutrophil-poor Sweet's syndrome with response to potassium iodide. Br J Dermatol. 1998, 139: 555-556. 10.1046/j.1365-2133.1998.02439.x.
Delabie J, De Wolf-Peeters C, Morren M, Marien K, Roskams T, Desmet V: Histiocytes in Sweet's syndrome. Br J Dermatol. 1991, 124: 348-353. 10.1111/j.1365-2133.1991.tb00595.x.
Evans AV, Sabroe RA, Liddle K, Russell-Jones R: Lymphocytic infiltrates as a presenting feature of Sweet's syndrome with myelodysplasia and response to cyclosphosphamide. Br J Dermatol. 2002, 146: 1087-1090. 10.1046/j.1365-2133.2002.04701.x.
Requena L, Kutzner H, Palmedo G, Pasual M, Fernandez-Herrera J, Fraga J, Garcia-Diez A, Sanchez Yus E: Histiocytoid Sweet syndrome: a dermal infiltration of immature neutrophilic granulocytes. Arch Dermatol. 2005, 141: 834-842. 10.1001/archderm.141.7.834.
Bianchi L, Masi M, Hagman JH, Piemonte P, Orlandi A: Systemic interferon-alpha treatment for idiopathic Sweet's syndrome. Clin Exp Dermatol. 1999, 24: 443-445. 10.1046/j.1365-2230.1999.00527.x.
Evans AV, Sabroe RA, Setterfield J, Greaves MW: Erythema elevatum diutinum/Sweet's syndrome overlap with gastrointestinal and oral involvement. Br J Dermatol. 1999, 141: 747-776. 10.1046/j.1365-2133.1999.03124.x.
Matsuda T, Abe Y, Arata J, Nagao Y: Acute febrile neutrophilic dermatosis (Sweet's syndrome) associated with extreme infiltration of eosinophils. J Dermatol (Tokyo). 1994, 21 (5): 341-346.
Magro CM, DeMoraes E, Burns F: Sweet's syndrome in the setting of CD34-positive acute myelogenous leukemia treated with granulocyte colony stimulating factor: evidence for a clonal neutrophilic dermatosis. J Cutan Pathol. 2001, 28: 90-96. 10.1034/j.1600-0560.2001.280205.x.
Urano Y, Miyaoka Y, Kosaka M, Kabe K, Uchida N, Arase S: Sweet's syndrome associated with chronic myelogenous leukemia: demonstration of leukemic cells within a skin lesion. J Am Acad Dermatol. 1999, 40: 275-279. 10.1016/S0190-9622(99)70206-9.
Tomasini C, Aloi F, Osella-Abate S, Dapavo P, Pippione M: Immature myeloid precursors in chronic neutrophilic dermatosis associated with myelodysplastic syndrome. Am J Dermatol. 2000, 22: 429-433. 10.1097/00000372-200010000-00008.
Deguchi M, Tsunoda T, Yuda F, Tagami H: Sweet's syndrome in acute myelogenous leukemia showing dermal infiltration of leukemic cells. Dermatology. 1997, 194: 182-184.
Wong T-Y, Suster S, Bouffard D, Flynn SD, Johnson RA, Barnhill RL, Mihm MC: Histologic spectrum of cutaneous involvement in patients with myelogenous leukemia including the neutrophilic dermatoses. Int J Dermatol. 1995, 34: 323-329. 10.1111/j.1365-4362.1995.tb03612.x.
del Pozo J, Martinez W, Manuel Pazos J, Yebra-Pimentel M, Garcia Silva J, Fonseca E: Concurrent Sweet's syndrome and leukemia cutis in patients with myeloid disorders. Int J Dermatol. 2005, 44: 677-680. 10.1111/j.1365-4632.2005.02037.x.
Vignon-Pennamen MD, Aractingi S: Sweet's syndrome and leukemia cutis: a common skin homing mechanism?. Dermatology. 2003, 206: 81-84. 10.1159/000068462.
Choonhakarn C, Chetchotisakd P, Jirarattanapochai K, Mootsikapun P: Sweet's syndrome associated with non-tuberculous mycobacterial infection: a report of five cases. Br J Dermatol. 1998, 139: 107-110. 10.1046/j.1365-2133.1998.02324.x.
Trentham DE, Masi AT, Bale GF: Arthritis with an inflammatory dermatosis resembling Sweet's syndrome: report of a unique case and review of the literature on arthritis associated with inflammatory dermatoses. Am J Med. 1976, 61: 424-432. 10.1016/0002-9343(76)90382-X.
Ytting H, Vind I, Bang D, Munkholm P: Sweet's syndrome – an extraintestinal manifestation in inflammatory bowel disease. Digestion. 2005, 72: 195-200. 10.1159/000088466.
Gosheger G, Hillmann A, Ozaki T, Buerger H, Winkelmann W: Sweet's syndrome associated with pigmented villonodular synovitis. Acta Orthop Belg. 2002, 68: 68-71.
Furukawa F, Toriyama R, Kawanishi T: Neutrophils in cerebrospinal fluid of a patient with acute febrile neutrophilic dermatosis (Sweet's syndrome). Int J Dermatol. 1992, 31: 670-671. 10.1111/j.1365-4362.1992.tb03996.x.
Chiba S: Sweet's syndrome with neurologic signs and psychiatric symptoms. Arch Neurol. 1983, 40: 829-
Druschky A, von den Driesch P, Anders M, Claus D, Neundorfer B: Sweet's syndrome (acute febrile neutrophilic dermatosis) affecting the central nervous system. J Neurol. 1996, 243: 556-557. 10.1007/BF00886881.
Martinez E, Fernandez A, Mayo J, Manrique P, Collazos J: Sweet's syndrome associated with cerebrospinal fluid neutrophilic pleocytosis. Int J Dermatol. 1995, 34: 73-74. 10.1111/j.1365-4362.1995.tb04389.x.
Noda K, Okuma Y, Fukae J, Fujishima K, Goto K, Sadamasa H, Yoshiike T, Mizuno Y: Sweet's syndrome associated with encephalitis. J Neurol Sci. 2001, 188: 95-97. 10.1016/S0022-510X(01)00541-X.
Pharis DB, Cerenko D, Caughman SW: Sweet's syndrome in a patient with idiopathic progressive bilateral sensorineural hearing loss. J Am Acad Dermatol. 2000, 42: 932-935. 10.1016/S0190-9622(00)90276-7.
Hisanaga K, Hosokawa M, Sato N, Mochizuki H, Itoyama Y, Iwasaki Y: "Neuro-sweet disease": benign recurrent encephalitis with neutrophilic dermatosis. Arch Neurol. 1999, 56: 1010-1013. 10.1001/archneur.56.8.1010.
Matthews PC, Willatts SM: Sweet's syndrome associated with systemic inflammatory response syndrome. Intensive Care Med. 1998, 24: 1106-1109. 10.1007/s001340050724.
Balass S, Duparc A, Zaid S, Bularca S, Modiano P: Aseptic meningitis during Sweet syndrome. Ann Dermatol Venereol. 2005, 132: 1003-1006.
Hisanaga K, Iwasaki Y, Itoyama Y, Neuro-Sweet Disease Study Group: Neuro-Sweet disease: clinical manifestations andcriteria for diagnosis. Neurology. 2005, 64: 1756-1761. 10.1212/01.WNL.0000161848.34159.B5.
Ramos Ramos JC, Sanz Moreno J, Oliveira Ramirez E, Garcia Rodriguez M: Aseptic meningitis and Sweets syndrome. Med Clin (Barc). 2003, 121: 437-10.1157/13052309.
Nobeyama Y, Kamide R: Sweet's syndrome with neurologicmanifestation: case report and literature review. Int J Dermatol. 2003, 42: 438-443. 10.1046/j.1365-4362.2003.01795.x.
Cano A, Ribes R, de la Riva A, Rubio FL, Sanchez C, Sancho JL: Idiopathic hypertrophic cranial pachymeningitis associated with Sweet's syndrome. Eur J Radiol. 2002, 44: 139-142. 10.1016/S0720-048X(02)00090-6.
Kato T, Kunikata N, Taira H, Kobayashi N, Tanji K, Endo M: Acute febrile neutrophilic dermatosis (Sweet's syndrome) with nodular episcleritis and polyneuropathy. Int J Dermatol. 2002, 41: 107-109. 10.1046/j.1365-4362.2002.01361_1.x.
Saliba WR, Goldstein LH, Habib GS, Elias MS: Sweet's syndrome affecting the external auditory canal and tympanic membrane. J Laryngol Otol. 2004, 118: 48-49. 10.1258/002221504322731637.
Wilson DM, John GR, Callen JP: Peripheral ulcerative keratitis – an extracutaneous neutrophilic disorder: report of a patient with rheumatoid arthritis, pustular vasculitis, pyoderma gangrenosum, and Sweet's syndrome with an excellent response to cyclosporine therapy. J Am Acad Dermatol. 1999, 40: 331-334. 10.1016/S0190-9622(99)70479-2.
Davies R: Limbal nodules in Sweet's syndrome. Aust N Z J Ophthalmol. 1992, 20: 263-265.
Cohen PR: Sweet's syndrome presenting as conjunctivitis. Arch Ophthalmol. 1993, 111: 587-588.
Chen TC, Goldstein DA, Tessler HH, Quinn JP, Bautista CM: Scleritis associated with acute febrile neutrophilic dermatosis (Sweet's syndrome). Br J Ophthalmol. 1998, 82: 328-329.
Nicolaides A, Packles MR, Schutzer PJ, Weinberg JM: Iritis associated with Sweet's syndrome. Clin Exp Dermatol. 2000, 25: 349-354. 10.1046/j.1365-2230.2000.00655-5.x.
Mazokopakis E, Kalikaki A, Stathopoulos E, Vrentzos G, Papadakis JA: Acute febrile neutrophilic dermatosis (Sweet's syndrome) with erythema nodosum and anterior scleritis. A case report. Int J Dermatol. 2005, 44: 1051-1053. 10.1111/j.1365-4632.2004.02278.x.
Sato M, Kawamura T, Hase S, Katsumata S, Oshika T: A case of bilateral retinal vasculitis associated with Sweet syndrome. Retina. 2005, 25: 800-802. 10.1097/00006982-200509000-00024.
Levy J, Schneck M, Erlich Y, Lifshitz T: Sweet's syndrome presenting as acute episcleritis. Can J Ophthalmol. 2005, 40: 90-92.
Anwar S, Hassan S, Fern AI, Douglas WS, Mann B: Bilateral periocular swelling in Sweet's syndrome. Eye. 2004, 18: 214-216. 10.1038/sj.eye.6700588.
Fain O, Mathieu E, Feton N, Sibony M, Sitbon M, Lejeune F, Thomas M: Intestinal involvement in Sweet's syndrome. J Am Acad Dermatol. 1996, 35: 989-990. 10.1016/S0190-9622(96)90128-0.
McDermott MB, Corbally MT, O'Marcaigh AS: Extracutaneous Sweet syndrome involving the gastrointestinal tract in a patient with Fanconi's anemia. J Pediatr Hematol Oncol. 2001, 23: 59-62. 10.1097/00043426-200101000-00015.
Zamora-Martinez E, Martin Moreno L, de Castro Torres A, Barat Cascante A: Sweet's syndrome. A study of 10 cases and review of the literature. Rev Clin Esp. 1990, 186: 264-269.
Shimizu K: Neutrophilic infiltration of the myocardium in a patient with myelodysplastic syndrome. Am J Hematol. 1998, 58: 337-338. 10.1002/(SICI)1096-8652(199808)58:4<337::AID-AJH16>3.0.CO;2-4.
Attias D, Laor R, Zuckermann E, Naschitz JE, Luria M, Misselevitch I, Boss JH: Acute neutrophilic myositis in Sweet's syndrome: late phase transformation into fibrosing myositis and panniculitis. Hum Pathol. 1995, 26: 688-690. 10.1016/0046-8177(95)90177-9.
Guia JM, Frias J, Castro FJ, Gracian M: Cardiovascular involvement in a boy with Sweet's syndrome. Pediatr Cardiol. 1999, 20: 295-297. 10.1007/s002469900468.
Muster AJ, Bharati S, Herman JJ, Esterly NB, Gonzales-Crussi F, Holbrook KA: Fatal cardiovascular disease and cutis laxa following acute febrile neutrophilic dermatosis. J Pediatr. 1983, 102: 243-248. 10.1016/S0022-3476(83)80529-0.
Dorenkamp M, Weikert U, Meyer R, Schwimmbeck PL, Morguet AJ: Heart failure in acute febrile neutrophilic dermatosis. Lancet. 2003, 362: 1374-10.1016/S0140-6736(03)14633-8.
Peters FPJ, Drent M, Verhaegh M, van Pampus ECM, Schouten HC: Myelodysplasia presenting with pulmonary manifestations associated with neutrophilic dermatosis. Ann Hematol. 1998, 77: 135-138. 10.1007/s002770050429.
Thurnheer R, Stammberger U, Hailemariam S, Russi EW: Bronchial manifestations of acute febrile neutrophilic dermatosis (Sweet's syndrome). Eur Respir J. 1998, 11: 978-980. 10.1183/09031936.98.11040978.
Cohen PR, Kurzrock R: Extracutaneous manifestations of Sweet's syndrome: steroid-responsive culture-negative pulmonary lesions. Am Rev Respir Dis. 1992, 146: 269-
Kumar A, Helwig K, Komar MJ: Sweet's syndrome in association with probable autoimmune hepatitis. J Clin Gastroenterol. 1999, 29: 349-350. 10.1097/00004836-199912000-00014.
Notani K, Kobayashi S, Kondoh K, Shindoh M, Ferguson MM, Fukuda H: A case of Sweet's syndrome (acute febrile neutrophilic dermatosis) with palatal ulceration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000, 89: 477-479. 10.1016/S1079-2104(00)70128-4.
Bamelis M, Boyden B, Sente F, Madoe V: Sweet's syndrome and acute myelogenous leukemia in a patient who presented with a sudden massive swelling of the tongue. Dermatology. 1995, 190: 335-337.
Brady RC, Morris J, Connelly BL, Boiko S: Sweet's syndrome as an initial manifestation of pediatric human immunodeficiency virus infection. Pediatrics. 1999, 104: 1142-1144. 10.1542/peds.104.5.1142.
Kim MK, Park JW, Park SH, Bang SM, Chung JG, Ahn JY, Baek HJ: Neutrophilic myositis without cutaneous involvement as the first manifestation of acute myeloid leukemia. Korean J InternMed. 2005, 20 (4): 346-348.
Rajeswari S, Rajendran CP, Madhavan R, Ramesh S: Sweet's syndrome with tendinitis. J Assoc Physicians India. 2005, 53: 718-730.
Brown AM, Davies MG, Hickling P: Recurrent tenosynovitis in Sweet's syndrome. Rheumatology (Oxford). 2002, 41: 1067-1069. 10.1093/rheumatology/41.9.1067.
Otheo E, Ros P, Vazquez JL, Carrillo R, Moreno R, Maldonado S, Martos I: Systemic inflammatory response syndrome associated with Sweet's syndrome. Pediatr Crit Care Med. 2002, 3: 190-193. 10.1097/00130478-200204000-00020.
Hoffman GS: Treatment of Sweet's syndrome (active febrile neutrophilic dermatosis) with indomethacin. J Rheumatol. 1977, 4: 201-206.
Darvay A: Sweet's syndrome preceding inflammatory bowel disease. Clin Exp Dermatol. 1996, 21: 175-10.1111/j.1365-2230.1996.tb00054.x.
Jeanfils S, Joly P, Young P, le Corvaisier-Pietro C, Thomine E, Lauret P: Indomethacin treatment of eighteen patients with Sweet's syndrome. J Am Acad Dermatol. 1997, 36: 436-439. 10.1016/S0190-9622(97)80222-8.
Burrows NP: Sweet's syndrome in association with Crohn's disease. Clin Exp Dermatol. 1995, 20: 279-281. 10.1111/j.1365-2230.1995.tb01324.x.
Vaz A, Kramer F, Kalish RA: Sweet's syndrome in association with Crohn's disease. Postgrad Med J. 2000, 76: 713-714. 10.1136/pmj.76.901.713.
Rahier JF, Lion L, Dewit O, Lambert M: Regression of Sweet's syndrome associated with Crohn's disease after anti-tumor necrosis factor therapy. Acta Gastroenterol Belg. 2005, 68: 376-379.
Foster EN, Nguyen KK, Sheikh RA, Prindiville TP: Crohn's disease associated with Sweet's syndrome and Sjogren's syndrome treated with infliximab. Clin Dev Immunol. 2005, 12: 145-149. 10.1080/17402520500134254.
Vanbiervliet G, Anty R, Schneider S, Arab K, Rampal P, Hebuterne X: Sweet's syndrome and erythema nodosum associated with Crohn's disease treated by infliximab. Gastroenterol Clin Biol. 2002, 26: 295-297.
Rappaport A, Shaked M, Landau M, Dolev E: Sweet's syndrome in association with Crohn's disease: report of a case and review of the literature. Dis Colon Rectum. 2001, 44: 1526-1529. 10.1007/BF02234611.
Diaz-Peromingo JA, Garcia-Suarez F, Sanchez-Leira J, Saborido-Frojan J: Sweet's syndrome in a patient with acute ulcerative colitis: presentation of a case and review of the literature. Yale J Biol Med. 2001, 74: 165-168.
Salmon P, Rademaker M, Edwards L: A continuum of neutrophilic disease occurring in a patient with ulcerative colitis. Australas J Dermatol. 1998, 39: 116-118. 10.1111/j.1440-0960.1998.tb01262.x.
Satra KH, Zalka A, Cohen PR, Grossman ME: Sweet's syndrome and pregnancy. J Am Acad Dermatol. 1994, 30: 297-300.
Cohen PR: Pregnancy-associated Sweet's syndrome: world literature review. Obstet Gynecol Survey. 1993, 48: 584-587. 10.1097/00006254-199308000-00027.
Lee MS, Barnetson R, St C: Sweet's syndrome associated with Behcet's disease. Australas J Dermatol. 1996, 37: 99-101. 10.1111/j.1440-0960.1996.tb01015.x.
Quintana DC, de Mendarozqueta MGRZ, Arrazuria MAG, Oyon NS, Pueyo BA, Pena MVG, Carasa JCV: Concurrent Sweet's syndrome and Lofgren's syndrome. J Rheumatol. 1996, 23: 1995-1988.
Gillott TJ, Whallett AJ, Struthers GR, Ilchyshyn A: Concurrent Sweet's syndrome (acute febrile neutrophilic dermatosis), erythema nodosum, and sarcoidosis. Clin Exp Dermatol. 1996, 22 (1): 54-56.
Vaccaro M, Guarneri F, Guarneri C: Sweet's syndrome and erythema nodosum after Klebsiella pneumoniae cystitis. Acta Derm Venereol. 2003, 83: 290-291. 10.1080/00015550310016562.
Nishie W, Kimura T, Kanagawa M: Sweet's syndorme evolved from recurrent erythema nodosum in a patient with myelodysplastic syndrome. J Dermatol. 2002, 29: 91-95.
Astudillo L, Launay F, Lamant L, Sailler L, Bazex J, Couret B, Arlet-Suau E: Sweet's syndrome revealing relapsing polychondritis. Int J Dermatol. 2004, 43: 720-722. 10.1111/j.1365-4632.2004.02198.x.
Matzkies FG, Manger B, Schmitt-Haendle M: Severe septicaemia in a patient with polychondritis and Sweet's syndrome after initiation of treatment with infliximab. Ann Rheum Dis. 2003, 62: 81-82. 10.1136/ard.62.1.81.
Frances C, el Rassi RE, Laporte JL, Rybojad M, Papo T, Piette JC: Dermatologic manifestations of relapsing polychondritis. A study of 200 cases at a single center. Medicine (Baltimore). 2001, 80: 173-179. 10.1097/00005792-200105000-00003.
Le Gal FA, Roux ME, Vignon-Pennamen MD, Mouly F, Cordoliani F, Morel P, Rybojad M: Dermatoses neutrophiliques associees a une polychondrite atrophiante. 5 observations [Abstract]. Ann Dermatol Venereol (Paris). 1997, 124: S170-
Pouchot J, Bourgeots-Droin C, Vinceneu P, Barge J, Brun P, Granier F, Tremolieres F: Sweet's syndrome and mediastinal lymphadenopathy due to sarcoidosis: three cases of a new association. Arch Dermatol. 1993, 129: 1062-1064. 10.1001/archderm.129.8.1062.
Ganeshakrishnan KT, Ott GY, Barker A, Cobanoglu A: Sweet's sydrome and associated sarcoidosis – a rare clinical case. Thorac Cardiovasc Surgeon. 1997, 45: 247-248.
Saliba WR, Habib GS, Elias M: Sweet's syndrome and sarcoidosis. Eur J Intern Med. 2005, 16: 545-550. 10.1016/j.ejim.2005.06.017.
Goh CL, Alora M, Kohar Y: Sweet's syndrome in a skin clinic inSingapore: an epidemiology study. Ann Acad Med Singapore. 1996, 25: 222-227.
O'Brien TJ, Darling JA: Sweet's syndrome and hypothyroidism. Australas J Dermatol. 1994, 35: 91-92. 10.1111/j.1440-0960.1994.tb00906.x.
Nakayama H, Shimao S, Hamamoto T, Munemura C, Nakai A: Neutrophilic dermatosis of the face associated with aortitis syndrome and Hashimoto's thyroiditis. Acta Dermatol Venereol (Stockh). 1993, 73 (5): 380-381.
Granel F, Barbraud A, Schmutz J-L, DeMaistre E, Lecompte T: Anunexpected factor VIII inhibitor in a patient with Sweet's syndrome being treated with corticosteroids. Am J Med. 2000, 108: 434-435. 10.1016/S0002-9343(99)00252-1.
Campos LM, Castellanos AL, Afiune JY, Kiss MH, Silva CA: Takayasu's arteritis with aortic aneurysm associated with Sweet's syndrome in childhood. Ann Rheum Dis. 2005, 64: 168-169. 10.1136/ard.2003.006353.
Goette DK: Sweet's syndrome in subacute cutaneous lupus erythematosus. Arch Dermatol. 1985, 121: 789-791. 10.1001/archderm.121.6.789.
Hou TY, Chang DM, Gao HW, Chen CH, Chen HC, Lai JH: Sweet's syndrome as an initial presentation in systemic lupus erythemtosus: a case report and review of the literature. Lupus. 2005, 14: 399-402. 10.1191/0961203305lu2083cr.
del Pozo J, Martinez W, Carro E, Arevalo MP, Rodriguez-Lozano J, Fonseca E: A case of Sweet's syndrome and pemphigus vulgaris. J EurAcad Dermatol Venereol. 2004, 18: 745-746. 10.1111/j.1468-3083.2004.01056.x.
Reid PT, Alderdice J, Carson J, Sinnamon DG: Cryptogenic organizing pneumonia in association with Sweet's syndrome. Respir Med. 1996, 90: 57-59. 10.1016/S0954-6111(96)90246-2.
Chien SM, Jambrosic J, Mintz S: Pulmonary manifestations in Sweet's syndrome: first report of a case with bronchiolitis obliterans organizing pneumonia. Am J Med. 1991, 91: 553-554. 10.1016/0002-9343(91)90195-4.
Longo MI, Pico M, Bueno C, Lazara P, Serrano J, Lecona M, Carretero L, Alvarez E: Sweet's syndrome and bronchiolitis obliterans organizingpneumonia. Am J Med. 2001, 111: 80-81. 10.1016/S0002-9343(01)00789-6.
Cohen PR, Holder WR: Pentoxifylline for Sweet's syndrome. J Am Acad Dermatol. 1995, 32: 533-534. 10.1016/0190-9622(95)90109-4.
Antony F, Holden CA: Sweet's syndrome in association with generalized granuloma annulare in a patient with previous breastcarcinoma. Clin Exp Dermatol. 2001, 26: 668-670. 10.1046/j.1365-2230.2001.00914.x.
Jovanovic M, Polijacki M, Vujanovic L, Duran V: Acute febrile neutrophilic dermatosis (Sweet's syndrome) after influenza vaccination. J Am Acad Dermatol. 2005, 52: 367-369. 10.1016/j.jaad.2004.07.061.
Carpentier O, Piette F, Delaporte E: Sweet's syndrome after BCG vaccination. Acta Derm Venereol. 2002, 82: 221-10.1080/00015550260132604.
Lyon CC, Griffiths CEM: Chronic granulomatous disease and acute neutrophilic dermatosis. Clin Exp Dermatol. 1999, 24: 368-371. 10.1046/j.1365-2230.1999.00503.x.
Elliott SP, Mallory SB: Sweet syndrome: an unusual presentation of chronic granulomatous disease in a child. Pediatr Infect Dis J. 1999, 18: 568-570. 10.1097/00006454-199906000-00025.
Weiss RM, Schulz EJ: Complement deficiency in Sweet's syndrome. Br J Dermatol. 1989, 121: 413-415. 10.1111/j.1365-2133.1989.tb01441.x.
Hilliquin P, Marre JP, Cormier C, Renoux M, Menkes CJ, Puissant A: Sweet's syndrome in a human immunodeficiency virus-positive patient. Arthritis Rheum. 1992, 35: 484-486. 10.1002/art.1780350423.
Haliasos E, Soder B, Rubenstein DS, Henderson W, Morrell DS: Pediatric Sweet syndrome and immunodeficiency successfully treated with intravenous immunoglobulin. Pediatr Dermatol. 2005, 22: 530-535. 10.1111/j.1525-1470.2005.00133.x.
Halasz CL, Niedt GW, Kurtz CP, Scorpio DG, Bakken JS, Dumler JS: A case of Sweet syndrome associated with human granulocytic anaplasmosis. Arch Dermatol. 2005, 141: 887-889. 10.1001/archderm.141.7.887.
Bang B, Zachariae C: Capnocytophaga canimorsus sepsis causing Sweet's syndrome. Acta Dermatol Venereol (Stockh). 2001, 81: 73-74. 10.1080/000155501750208362.
Amichai B, Lazarov A, Cagnano M, Halevy S: Sweet's syndrome and chlamydial infection. Australas J Dermatol. 1993, 34: 31-33. 10.1111/j.1440-0960.1993.tb00845.x.
Amichai B, Lazarov A, Halevy S: Sweet's syndrome. J Am Acad Dermatol. 1995, 33: 144-145.
Rubegni P, Marano MR, DeAloe G, Pianigiani E, Bilenchi R, Fimiani M: Sweet's syndrome and Chlamydia pneumoniae infection. J Am Acad Dermatol. 2001, 44: 862-864. 10.1067/mjd.2001.112580.
DiCaudo DJ, Ortiz KJ, Mengden SJ, Lim KK: Sweet syndrome (acute febrile neutrophilic dermatosis) associated with pulmonary coccidioidomycosis. Arch Dermatol. 2005, 141: 881-884. 10.1001/archderm.141.7.881.
Paris O, Mahe A, Le Parc JM, Baglin C, Paolaggi JB, Auquier L: Acute polyarthritis associated with Sweet's syndrome. Presse Med. 1985, 14: 1599-1601.
Oskay T, Karademir A, Kutluay L: Sweet's syndrome associated with cytomegalovirus infection. Int J Dermatol. 2004, 43: 57-59. 10.1111/j.1365-4632.2004.01812.x.
Ruiz AI, Gonzalez A, Miranda A, Torrero V, Gutierrez C, Garcia M: Sweet's syndrome associated with francisella tularensis infection. Int J Dermatol. 2001, 40: 791-793. 10.1046/j.1365-4362.2001.01162.x.
Kurkcuoglu N, Aksoy F: Sweet's syndrome associated with Helicobacter pylori infection. J Am Acad Dermatol. 1997, 37: 123-124. 10.1016/S0190-9622(97)70225-1.
Tan E, Yosipovitch G, Giam Y-C, Tan SH: Bullous Sweet's syndrome associated with acute hepatitis B infection: a new association. Br J Dermatol. 2000, 143: 914-916. 10.1046/j.1365-2133.2000.03810.x.
Akovbyan V, Talanin N, Tukhvatullina Z: Sweet's syndome in patients with kidney and liver disorders. Cutis. 1992, 49: 448-450.
Theng TS, Chan YC, Leow YH, Tan SH: Sweet's syndrome associated with Mycobacterium chelonae and herpes simplex virus infections: a case report. Ann Acad Med Singapore. 2003, 32: 411-414.
Coskun U, Gunel N, Senol E, Ilter N, Dursun A, Tuzun D: A case of Sweet's syndrome developed after the treatment of herpes simplex infection in a metastatic breast cancer patient. J Cutan Pathol. 2002, 29: 301-304. 10.1034/j.1600-0560.2002.290508.x.
Hsiao G-H, Chiu H-C: Atypical mycobacterial cervical lymphadenitis associated with Sweet's syndrome. Acta Derm Venereol (Stockh). 1995, 75 (3): 237-239.
Itoh H, Shimasaki S, Nakashima A, Ohsato K, Tokikuni N, Kitajima C: Sweet's syndrome associated with subacute necrotizing lymphadenitis. Intern Med. 1992, 31: 686-689.
Mahaisavariya P, Chaiprasert A, Manonukul J, Khemngern S: Scrofuloderma and Sweet's syndrome. Int J Dermatol. 2002, 41: 28-31. 10.1046/j.1365-4362.2002.01362.x.
Chen HH, Hsiao CH, Chiu HC: Successive development of cutaneous polyarteritis nodosum, leucocytoclastic vasculitis and Sweet's syndrome in a patient with cervical lymphadenitis caused by Mycobacterium fortuitum. Br J Dermatol. 2004, 151: 1096-1100. 10.1111/j.1365-2133.2004.06201.x.
Tuchinda C, Puavilai S, Sathapatayavongs B, Sungkanuparph S, Vibhagool A, Jirasutus S, Rajatanavin N, Timpatanapong P: Sweet's syndrome: a reaction to non-tuberculous mycobacterial infections. J Med Assoc Thai. 2004, 87: 567-572.
Boivin S, Segard M, Piette F, Delaporte E: Sweet syndrome associated with Pasteurella multocida bronchitis. Arch Intern Med. 2000, 160: 1869-10.1001/archinte.160.12.1869.
Chowdhary V, Nityanand S, Prasad KN, Pandey R, Dabadghao S: Case report. Sweet's syndrome and Pneumocystis carinii pneumonia: two sequelae of low-dose cytosine arabinoside therapy in a patient with acute myeloid leukemia. Eur J Haematol. 2000, 65: 72-73. 10.1034/j.1600-0609.2000.9c177.x.
Zillikens D, Goldsstein RK, Elsner P, Hartmann AA, Burg G: Sweet's syndrome associated with Salmonella typhimurium infection. Acta Derm Venereol (Stockh). 1991, 71 (1): 77-79.
Abramovits W, Stevenson LC: Sweet's syndrome associated with Staphylococcus aureus. Int J Dermatol. 2004, 43: 938-941. 10.1111/j.1365-4632.2004.02000.x.
Gould KP, Jones JD, Callen JP: Sweet's syndorme in a patient with enterococcal subacute bacterial endocarditis. J Am Acad Dermatol. 2004, 50: 798-799. 10.1016/j.jaad.2003.05.003.
Delfino M, Suppa F, DeLuca F, Lembo G: Sweet's syndrome and toxoplasmosis: a coincidental association?. Dermatologica. 1985, 171: 102-105.
Maillard H, Leclech C, Peria P, Avenel-Audran M, Verret JL: Colchicine for Sweet's syndrome. A study of 20 cases. Br J Dermatol. 1999, 140: 565-566. 10.1046/j.1365-2133.1999.02747.x.
Singh RK: Acute febrile neutrophilic dermatosis following tuberculous infection. J Assoc Physicians India. 2002, 50: 1322-1323.
Stieler W, Schulte C: Localized Sweet syndrome in urethro-prostatitis caused by Ureaplasma. Hautarzt. 1988, 39: 658-661.
Lewis KG, Dill SW, Wilkel CS, Robinson-Bostom L: Mid-dermal elastolysis preceded by acute neutrophilic dermatosis. J Cutan Pathol. 2004, 31: 72-76. 10.1046/j.0303-6987.2004.0141.x.
Tal A: Sweet's syndrome. Mayo Clin Proc. 1995, 70: 605-606.
Saliba WR, Habib GS, Goldstein LH, Elias MS: Sweet's syndrome after pneumonectomy. Ann Thorac Surg. 2004, 78: 341-343. 10.1016/S0003-4975(03)01286-4.
Kyrmizakis DE, Drivas E, Kruger-Krasagakis S, Hajiioannou I, Karatzanis A, Velegrakis GA: Acute rhinosinusitis associated with Sweet's syndrome. J Otolaryngol. 2006, 35: 144-146.
Elinav H, Maly A, Ilan Y, Rubinow A, Naparstek Y, Amital H: The coexistence of Sweet's syndrome and Still's disease – is it merely a coincidence?. J Am Acad Dermatol. 2004, 50: S90-S92. 10.1016/S0190-9622(03)02796-8.
Roger M, Valence C, Bressieux JM, Bernard P, Fur A: Grover's disease associated with Waldenstrom's macroglobulinemia and neutrophilic dermatosis. Acta Derm Venereol (Stockh). 2000, 80 (2): 145-146.
Akovbyan VA, Tukhvatullina ZG, Persina IS: Sweet's syndrome. Vestn Dermatol Venereol. 1989, 11: 67-69.
Lack MD, Weingold DH: Localized neutrophilic dermatosis following welding burns. J Occup Environ Med. 2002, 44: 491-492. 10.1097/00043764-200206000-00006.
Evans AV, Sabroe RA, Setterfield J, Greaves MW: Erythema elevatum diutinum/Sweet's syndrome overlap with gastrointestinal and oral involvement. Br J Dermatol. 1999, 141: 766-767. 10.1046/j.1365-2133.1999.03140.x.
Caughman W, Stern R, Haynes H: Neutrophilic dermatosis of myeloproliferative disorders. J Am Acad Dermatol. 1983, 9: 751-758.
Lear JT, Byrne JPH: Bullous pyoderma gangrenosum, Sweet's syndrome and malignancy. Br J Dermatol. 1997, 136: 296-297. 10.1111/j.1365-2133.1997.tb08764.x.
Krug B, Sonet A, Pirson AS, Mahy N, Bosly A, Borght TV: FDG PET utility in paraneoplastic Sweet syndrome. Clin Nucl Med. 2004, 29: 91-92. 10.1097/01.rlu.0000109330.67331.86.
Ahn S-J, Choi J-H, Sung K-J, Moon K-C, Koh J-K: Sweet's syndrome presenting with lesions resembling eruptive xanthoma. Br J Dermatol. 2000, 143: 449-450. 10.1046/j.1365-2133.2000.03682.x.
Magro CM, Crowson AN: A distinctive vesiculopustular eruption associated with hepatobiliary disease. Int J Dermatol. 1997, 36: 837-844. 10.1046/j.1365-4362.1997.00010.x.
Cohen PR: Paraneoplastic dermatopathology: cutaneous paraneoplastic syndromes. Adv Dermatol. 1995, 11: 215-252.
Requena L, Sanchez Yus E: Part II. Mostly lobular panniculitis. J Am Acad Dermatol. 2001, 45: 325-362. 10.1067/mjd.2001.114735.
Weedon D: Panniculitis. Skin Pathology. Edited by: Weedon D. 1997, New York: Churchill Livingstone Inc, 441-456.
Ackerman A, Chongchitnant N, Sanchez J, Guo Y, Bennin B, Randall M: Algorithmic method for diagnosis that employs pattern analysis. Histologic diagnosis of inflammatory skin diseases. An algorithmic method based on pattern analysis. Edited by: Ackermann AB. 1997, Baltimore: Williams & Wilkins, 145-167. 2
Tran T-AN, DuPree M, Carlson JA: Neutrophilic lobular (pustular) panniculitis associated with rheumatoid arthritis. A case report and review of the literature. Am J Dermatopathol. 1999, 21: 247-252. 10.1097/00000372-199906000-00007.
Anstey A, Wilkinson JD, Wojnarowska F, Kirk A, Gowers L: Pustular panniculitis in rheumatoid arthritis. J R Soc Med. 1991, 84: 307-308.
Kuniyuki S, Shindow K, Tanaka T: Pustular panniculitis in a patient with rheumatoid arthritis. Int J Dermatol. 1997, 36: 292-293.
Newton J, Wojnarowska FT: Pustular pannniculitis in rheumatoid arthritis. Br J Dermatol. 1988, 119: 97-98. 10.1111/j.1365-2133.1988.tb05446.x.
Cohen PR, Rapini RP, Beran M: Infiltrated blue-gray plaques in a patient with leukemia. Chloroma (granulocytic sarcoma). Arch Dermatol. 1987, 123: 251-254. 10.1001/archderm.123.2.251.
Tavadia SMB, Smith G, Herd RM, Zuk RJ: Sweet's syndrome associated with oral squamous cell carcinoma and exhibiting the Koebner phenomenon. Br J Dermatol. 1999, 141: 169-170. 10.1046/j.1365-2133.1999.02913.x.
Okamoto H, Kohno A, Tsuru N, Ikematsy , Ayabe T: Sweet's syndrome and thyroid cancer. Rincho Dermatol. 1988, 30: 1212-1213.
O'Connor Reina C, Garcia Iriarte MT, Rodriguez Diaz A, Gomez Angel D, Garcia Monge E, Sanchez Conejo-Mir J: Tonsil cancer and Sweet's syndrome. Otolaryngol Head Neck Surg. 1998, 119: 709-710. 10.1016/S0194-5998(98)70042-7.
Bello Lopez JL, Fonseca E, Manso F: Sweet's syndrome during the chronic phase of chronic myeloid leukemia. Acta Haematol. 1990, 84: 207-208.
Harary AM: Sweet's syndrome associated with rheumatoid arthritis. Arch Intern Med. 1983, 143: 1993-1995. 10.1001/archinte.143.10.1993.
Case JD, Smith SZ, Callen JP: The use of pulse methylprednisolone and chlorambucil in the treatment of Sweet's syndrome. Cutis. 1989, 44: 125-129.
Altomare G, Capella GL, Frigerio E: Sweet's syndrome in a patient with idiopathic myelofibrosis and thymoma-myasthenia gravis-immunodeficiencycomplex: efficacy of treatment with etretinate. Haematologica (Pavia). 1996, 81 (1): 54-58.
Cohen PR, Holder WR, Tucker SB, Kono S, Kurzrock R: Sweet syndrome in patients with solid tumors. Cancer. 1993, 72: 2723-2731. 10.1002/1097-0142(19931101)72:9<2723::AID-CNCR2820720933>3.0.CO;2-F.
Myatt AE, Baker DJ, Byfield DM: Sweet's syndrome: a report on the use of potassium iodide. Clin Exp Dermatol. 1987, 12: 345-349. 10.1111/j.1365-2230.1987.tb02506.x.
Fanti PA, Moise GM, Vuga S, LoBrutto ME: Sindrome di Sweet in paziente con carcinome a cellule chiare del rene. Chron Derm. 1984, 15: 175-179.
Nguyen KQ, Hurst CG, Pierson DL, Rodman OG: Sweet's syndrome and ovarian carcinoma. Cutis. 1983, 32: 152-154.
Brodkin RH, Schwartz RA: Sweet's syndrome with myelofibrosis and leukemia: partial response to interferon. Dermatology. 1995, 190: 160-163.
Bennion SD, Fitzpatrick JE, DiBella NJ: Sweet's syndrome in association with breast cancer. Cutis. 1987, 82: 1084-1085.
Horio T, Danno K, Okamoto H, Miyachi Y, Imamura S: Potassium iodide in erythema nodosum and other erythematous dermatoses. J Am Acad Dermatol. 1983, 9: 77-81.
Bruyn GAW, Missier ETA, Toonstra J, Bijlsma JWJ: Sweet's syndrome. Neth J Med. 1990, 36: 62-68.
Kannan R, Dutta TK, Garg BB, Venkatesqaran S, Ratnakar C: Sweet's syndrome in chronic myeloid leukaemia. Postgrad Med J. 1995, 71: 383-
Su WPD, Fett DL, Gibson LE, Pittelkow MR: Sweet syndrome: acute febrile neutrophilic dermatosis. Seminars Dermatol. 1995, 14: 173-178.
Schiff BL, Kern AB, Bercovitch L: Sweet's syndrome: report of two atypical cases. Postgrad Med. 1982, 71: 55-60.
Suehisa S, Tagami H: Treatment of acute februle neutrophilic dermatosis (Sweet's syndrome) with colchicine. Br J Dermatol. 1981, 105: 483-10.1111/j.1365-2133.1981.tb00785.x.
Sterling JB, Heymann WR: Potassium iodide in dermatology: a 19th century drug for the 21st century – uses, pharmacology, adverseeffects, and contraindictions. J Am Acad Dermatol. 2000, 43: 691-697. 10.1067/mjd.2000.107247.
Suehisa S, Tagami H, Inoue F, Matsumoto K, Yoshikuni K: Colchicine in the treatment of acute febrile neutrophilic dermatosis (Sweet's syndrome). Br J Dermatol. 1983, 180: 99-101. 10.1111/j.1365-2133.1983.tb04584.x.
Boudghene-Stambouli O, Merad-Boudia A: Dermatose aigue febrile neutrophilique. Aspect clinique, evolutif et therapeutique. A propos de 55 observations. Nouv Dermatol. 1996, 15: 702-706.
Ritter S, George R, Serwatka LM, Elston DM: Long-term suppression of chronic Sweet's syndrome with colchicine. J Am Acad Dermatol. 2002, 47: 323-324. 10.1067/mjd.2002.121028.
Hehlmann R, Ludershmidt C, Goebel FD, Henze K: Relapsing acute febrile neutrophilic dermatosis and essential thrombocythemia. Blut. 1984, 48: 297-305.
Saxe N, Gordon W: Acute febrile neutrophilic dermatosis (Sweet's syndrome): four case reports. S Afr Med. 1978, 53: 253-256.
Sharpe GR, Leggat HM: A case of Sweet's syndrome and myelodysplasia: response to cyclosporin. Br J Dermatol. 1992, 127: 538-539. 10.1111/j.1365-2133.1992.tb14856.x.
von den Driesch P, Steffan C, Zobe A, Hornstein OP: Sweet's syndrome – therapy with cyclosporin. Clin Exp Dermatol. 1994, 19: 274-277. 10.1111/j.1365-2230.1994.tb01187.x.
Aram H: Acute febrile neutrophilic dermatosis (Sweet's syndrome): response to dapsone. Arch Dermatol. 1984, 120: 245-247. 10.1001/archderm.120.2.245.
El Sherif AI, Bharija SC, Belhaj MS, Singh G: Dapsone in Sweet syndrome. Int J Dermatol. 1990, 29: 737-
Inomata N, Sasaki T, Nakajima H: Sweet's syndrome with gastric cancer. J Am Acad Dermatol. 1999, 41: 1033-1034.
Cohen PR, Kurzrock R: Treatment of Sweet's syndrome. Am J Med. 1990, 89: 396-10.1016/0002-9343(90)90362-H.
Spillman DH, Carabajal MG, Errecaborde MS, Mazzini MA: Acute febrile neutrophilic dermatosis (Sweet's syndrome) [Abstract]. Book of Abstracts. 18th World Congress of Dermatology. Dermatology: Progress and Perspectives. New York City, 147A-June 12–18; 1992
Banet DE, McClave SA, Callen JP: Oral metronidazole, an effective treatment for Sweet's syndrome in a patient with associated inflammatory bowel disease. J Rheumatol. 1994, 21: 1766-1768.
Joshi RK, Atukorala DN, Abanmi A, Al Khamis O, Haleem A: Successful treatment of Sweet's syndrome with doxycycline. Br J Dermatol. 1993, 128: 584-586. 10.1111/j.1365-2133.1993.tb00242.x.
Purdy MJ, Fairbrother GE: Case reports: acute febrile neutrophilic dermatosis of Sweet. Australas J Dermatol. 1971, 12: 172-177. 10.1111/j.1440-0960.1971.tb00006.x.
Unis ME, Hill GS: Sweet's syndrome associated with acute renal failure. Cutis. 1987, 40: 139-142.
Feliu E, Cervantes F, Ferrando J, Puig S, Mascaro JP, Rozman C: Neutrophilic pustulosis associated with chronic myeloid leukemia: a special form of Sweet's syndrome. Report of two cases. Acta Haematol. 1992, 88: 154-157.
Yamuauchi PS, Turner L, Lowe NJ, Gindi V, Jackson MJ: Treatment of recurrent Sweet's syndrome with coexisting rheumatoid arthritis with the tumor necrosis factor antagonist etanercept. J Am Acad Dermatol. 2006, 54: S122-S126. 10.1016/j.jaad.2005.11.1089.
Browning CE, Dixon JE, Malone JC, Callen JP: Thalidomide in the treatment of recalcitrant Sweet's syndrome associated with myelodysplasia. J Am Acad Dermatol. 2005, 53: S135-S138. 10.1016/j.jaad.2004.12.041.
Ely H: White blood cells as mediators of hyperviscosity-induced tissue damage in neutrophilic vascular reactions: therapy with pentoxifylline. J Am Acad Dermatol. 1989, 20: 677-680.
Ely H: Is pentoxifylline the drug of the decade?. J Am Acad Dermatol. 1994, 30: 639-642.
Ratzinger G, Burgdorf W, Zelger B: Sweet syndrome: vasculitis or not?. Br J Dermatol. 2006, 154: 1099-1101. 10.1111/j.1365-2133.2006.07508.x.
Shinojima Y, Toma Y, Terui T: Sweet syndrome associated with intrahepatic cholangiocarcinoma producing granulocyte colony-stimulating factor. Br J Dermatol. 2006, 154: 1103-1104. 10.1111/j.1365-2133.2006.07521.x.
Oiso N, Watanabe K, Kawada A: Granulocyte colony-stimulating factor-induced Sweet syndrome in a healthy donor. Br J Haematol. 2006, 135: 148-10.1111/j.1365-2141.2006.06222.x.
Teng JMC, Draper BK, Boyd AS: Sweet's panniculitis associated with metastatic breast cancer. J Am Acad Dermatol. 2007, 56: S61-S62. 10.1016/j.jaad.2006.05.023.
Khatri ML, Taha M: Sweet's syndrome associated with myelodysplastic syndrome presenting as periorbital cellulitis. Int J Dermatol. 2007, 46: 496-499. 10.1111/j.1365-4632.2006.03019.x.
Neoh CY, Tan AWH, Ng SK: Sweet's syndrome: a spectrum of unusual clinical presentations and associations. Br J Dermatol. 2007, 156: 480-485. 10.1111/j.1365-2133.2006.07677.x.
Laguna C, Vilata JJ, Martin B: Neutrophilic dermatosis of the dorsal hands. Actas Dermosifiliogr. 2007, 98: 102-104.
Kocabay G, Cagatay A, Karadeniz A: Sweet syndrome associated with erythema nodosum: are they different manifestations of the same disease?. South Med J. 2007, 100: 414-415.
Ammar D, Denguezli M, Ghariani N, Sriha B, Belajouza C, Nouira R: Sweet's syndrome complicating isotretinoin therapy in acne. Ann Dermatol Venereol. 2007, 134: 151-154.
Cohen PR: Sweet's syndrome and erythema nodosum. South Med J.
Smith RA, Cokkinides V, Eyre HJ: Cancer screening in the United States, 2007: a review of current guidelines, practices, and prospects. CA Cancer J Clin. 2007, 57: 90-104.
Xiao T, He CD, Gao XH, Chen HD: Sweet's syndrome associated with skin methicillin-resistant Staphylococcus epidermidis infection. J Dermatol. 2007, 34: 258-261. 10.1111/j.1346-8138.2007.00264.x.
Del Pozo J, Sacristan F, Martinez W, Paradela S, Fernandez-Jorge B, Fonseca E: Neutrophilic dermatosis of the hands: presentation of eight cases and review of the literature. J Dermatol. 2007, 34: 243-247. 10.1111/j.1346-8138.2007.00261.x.
Cohen PR: Granuloma annulare, relapsing polychondritis, sarcoidosis, and systemic lupus erythematosus: conditions whose dermatologic manifestations may occur as hematologic malignancy-associated mucocutaneous paraneoplastic syndromes. Int J Dermatol. 2006, 45: 70-80. 10.1111/j.1365-4632.2005.02667.x.
Masmoudi A, Chaaben H, Hamdouni K, Boudaya S, Bouassida S, Turki H, Zahaf A: Sweet syndrome. Presse Med. 2007, 36: 419-424.
Rjeibi I, Zeglaoui F, El Fekih N, Ezzine N, Fazaa B, Kamoun MR: Sweet's syndrome: report of 5 cases. Rev Med Liege. 2006, 61: 834-836.
Cohen PR, Honigsmann H, Kurzrock R: Acute febrile neutrophilic dermatosis (Sweet's syndrome) (Chapter 31). Fitzpatrick's Dermatology in General Medicine. Edited by: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, Fitzpatrick TB. New York, McGraw-Hill Health Professions Division, 7,
Cohen PR, Kurzrock R: Sarcoidosis and malignancy. Clin Dermatol. 2007, 25: 326-333. 10.1016/j.clindermatol.2007.03.010.
Garcia-Rio I, Perez-Gala S, Aragues M, Fernandez-Herrera J, Fraga J, Garcia-Diez A: Sweet's syndrome on the area of postmastectomy lymphoedema. J Eur Acad Dermatol Venereol. 2006, 20: 401-405. 10.1111/j.1468-3083.2006.01460.x.
Ginarte M, Toribio J: Sweet's syndrome and erythema nodosum: two neutrophilic dermatoses?. Clin Rheumatol. 2007, 26: 1215-1216. 10.1007/s10067-007-0564-7.
Wallach D, Vignon-Pennamen M-D: From acute febrile neutrophilic dermatosis to neutrophilic disease: forty years of clinical research. J Am Acad Dermatol. 2006, 55: 1066-1071. 10.1016/j.jaad.2006.07.016.
Jagdeo J, Campbell R, Long T, Muglia J, Telang G, Robinson-Bostom L: Sweet's syndrome-like neutrophilic lobular panniculitis associated with all-trans-retinoic acid chemotherapy in a patient with acute promyelocytic leukemia. J Am Acad Dermatol. 2007, 56: 690-693. 10.1016/j.jaad.2006.08.011.
Martinez W, del Pozo J, Pena C, Yebra-Pimentel MT, Almagro M, Rodriguez-Lozano J, Fonseca E: Sweet's syndrome in a woman with chronic dermatophytic infection. Int J Dermatol. 2006, 45: 1365-1368. 10.1111/j.1365-4632.2006.02890.x.
Tan AW, Tan H-H, Lim PL: Bullous Sweet's syndrome following influenza vaccination in a HIV-infected patient. Int J Dermatol. 2006, 45: 1254-1255. 10.1111/j.1365-4632.2006.03005.x.
Duquia RP, de Almeida HL, Vettorato G, Souza PRM, Schwartz J: Neutrophilic dermatosis of the dorsal of the hands: acral sweet syndrome?. Int J Dermatol. 2006, 45: 51-52. 10.1111/j.1365-4632.2005.02652.x.
Mahajan VK, Sharma NL, Sharma RC: Sweet's syndrome from an Indian perspective: a report of four cases and review of the literature. Int J Dermatol. 2006, 45: 702-708. 10.1111/j.1365-4632.2006.02622.x.
Anavekar NS, Williams R, Chong AH: Facial Sweet's syndrome mimicking rosacea fulminans. Australas J Dermatol. 2007, 48: 50-55. 10.1111/j.1440-0960.2007.00334.x.
Hisanaga K: Neuro-neutrophilic disease: neuro-Behcet disease and neuro-Sweet disease. Intern Med. 2007, 46: 153-154. 10.2169/internalmedicine.46.0175.
Bachmeyer C, Begon E, Blum L, Cerf I, Petitjean B, Vignon-Pennamen M-D, Pertuiset E: Overlapping neutrophilic dermatosis in a patient with SAPHO syndrome. Arch Dermatol. 2007, 143: 275-276. 10.1001/archderm.143.2.275.
Vignon-Pennamen M-D, Juillard C, Rybojad M, Wallach D, Daniel M-T, Morel P, Verola O, Janin A: Chronic recurrent lymphocytic Sweet's syndrome as a predictive marker of myelodysplasia: a report of 9 cases. Arch Dermatol. 2006, 142: 1170-1176. 10.1001/archderm.142.9.1170.
Hoverson AR, Davis MDP, Weenig RH, Wolanskyi AP: Neutrophilic dermatosis (Sweet syndrome) of the hands associated with lenalidomide. Arch Dermatol. 2006, 142: 1070-1071. 10.1001/archderm.142.8.1070-b.
Kaur MR, Bazza MA, Ryatt KS: Neutrophilic dermatosis of the dorsal hands treated with indomethacin. Br J Dermatol. 2006, 154: 1089-1090. 10.1111/j.1365-2133.2006.07491.x.
Ratzinger G, Burgdorf W, Zelger BG, Zelger B: Acute febrile neutrophilic dermatosis: a histopathologic study of 31 cases with review of literature. Am J Dermatopathol. 2007, 29: 125-133. 10.1097/01.dad.0000249887.59810.76.
Magro CM, Kiani B, Li Jingwei, Crowson AN: Clonality in the setting of Sweet's syndrome and pyoderma gangrenosum is not limited to underlying myeloproliferative disease. J Cutan Pathol. 2007, 34: 526-534. 10.1111/j.1600-0560.2006.00654.x.
Zamanian A, Ameri A: Acute febrile neutrophilic dermatosis (Sweet's syndrome): a study of 15 cases in Iran. Int J Dermatol. 2007, 46: 571-574. 10.1111/j.1365-4632.2005.02688.x.
Dinh H, Murugasu A, Gin D: Sweet's syndrome associated with cellulites. Australas J Dermatol. 2007, 48: 105-109. 10.1111/j.1440-0960.2007.00347.x.
Awan F, Hamadani M, Devine S: Paraneoplastic Sweet's syndrome and the pathergy phenomenon. Ann Hematol. 2007, 86: 613-614. 10.1007/s00277-007-0279-5.
Souissi A, Benmously R, Fenniche S, Zarrouk M, Marrek H, Debbiche A, Ayed MB, Mokhtar I: Sweet's syndrome: a propos of 8 cases. Tunis Med. 2007, 85: 49-53.
Bouw J, Kater AP, van Tongeren J, Schultz MJ: Upper-airway obstruction instigated by Sweet's syndrome. Med Sci Monit. 2007, 13: CS53-55.
Thompson DF, Montarella KE: Drug-induced Sweet's syndrome. Ann Pharmacother. 2007, 41: 802-811. 10.1345/aph.1H563.
Acknowledgements
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
PRC drafted the entire manuscript and gives his approval of the version to be published.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cohen, P.R. Sweet's syndrome – a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis 2, 34 (2007). https://doi.org/10.1186/1750-1172-2-34
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1750-1172-2-34