Abstract
Background
The Psoriasis Symptom Inventory (PSI) is a patient-reported outcome measure designed to assess psoriasis signs and symptoms.
Objectives
The aim was to assess the usefulness of the PSI in enhancing patient care in the clinical setting.
Methods
Eight dermatology clinics in six countries enrolled adults representing the full spectrum of psoriasis severity who regularly received care at the clinic. Patients were administered the eight-item PSI (score range 0–32; higher scores indicate greater severity) while waiting for the physician; the physician conducted a static physician global assessment (sPGA) and estimated psoriasis-affected body surface area (BSA) at the same visit. Physicians completed a brief questionnaire after each patient visit, and were interviewed about the PSI after all patients were seen.
Results
The clinics enrolled 278 patients; mean [standard deviation (SD)] psoriasis-affected BSA was 7.6% (11.4). Based on BSA, 47.8% had mild psoriasis, 29.1% had moderate psoriasis, and 23.0% had severe psoriasis. Based on sPGA, 18.7% were clear/almost clear, 67.3% were mild/moderate, and 14.0% were severe/very severe. The mean (SD) PSI total score was 12.2 (8.3). Physicians spent a mean (SD) 4.9 (4.8) min discussing PSI findings with their patients (range 0–20 min). Key benefits of PSI discussions included the following: new information regarding symptom location and severity for physicians; prompting of quality-of-life discussions; better understanding of patient treatment priorities; change in treatment regimens to target specific symptoms or areas; and improvement of patient–physician relationship.
Conclusions
The PSI was useful for treated and untreated patients to enhance patient–physician communication, and influenced treatment decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The Psoriasis Symptom Inventory (PSI) is a validated patient-reported outcome instrument that was designed to quantify the patient’s perception of psoriasis signs and symptoms. |
Use of the PSI in real-world dermatology clinics elicited meaningful discussions of psoriasis signs and symptoms between physicians and patients (treated and untreated and across a wide range of disease severity), improved patient perception of the treating physician, and influenced treatment decisions. |
The PSI is a validated assessment tool that allows standardized objective evaluation of a patient’s perception of psoriasis signs and symptoms, and importantly, improves disease-specific communications between physician and patient. |
1 Introduction
Psoriasis is a chronic, immune-mediated, hyperproliferative skin disease characterized by erythematous, scaly plaques [1]. Globally, an estimated 100–125 million people suffer from psoriasis [2, 3]. This disease has significant negative impacts on health-related quality of life, most notably on emotional and social domains [4,5,6]. In a recent National Psoriasis Foundation survey of 5604 patients with psoriasis, 94% reported that psoriasis was a significant problem in daily life [5]. More than 80% reported feelings of self-consciousness, anger or frustration, helplessness, and embarrassment due to psoriasis [5]. Understanding the impact of psoriasis and the patient’s perception of psoriasis is important for developing a patient-centered approach to psoriasis treatment.
The Psoriasis Symptom Inventory (PSI) is a patient-reported outcome (PRO) measure that was designed to assess the patient’s perception of psoriasis signs and symptoms [7]. The PSI is an eight-item questionnaire that assesses signs and symptoms of itch, redness, scaling, burning, stinging, cracking, flaking, and pain. The severity of each item/sign or symptom is scored on a scale of 0 (“not at all”) to 4 (“very severe”); the eight items are summed for a total score (range 0–32). The PSI is valid, reproducible, and responsive to change [8, 9], and can demonstrate improvements in symptoms with treatment [10]. Two versions with different recall periods were developed and validated: a 24-h recall period and a 7-day recall period [8, 11]. The PSI has undergone cultural/linguistic validation with a wide variety of languages using standard PRO translation methodology (including all languages used in this study) [12, 13].
In a previous study, it was demonstrated that PSI scores were responsive to clinical changes as assessed by the Psoriasis Area and Severity Index (PASI); therefore, PSI score may be useful in monitoring psoriasis severity in the clinic [9]. In a partnership between the International Psoriasis Council (IPC) and Amgen (the developer of the PSI), we tested the utility of the PSI in eight dermatology clinics in six countries that treat and manage patients with psoriasis. In addition to administering the PSI to their regular patients, the physicians at the clinics also filled out a brief questionnaire on each patient interaction, and were subsequently interviewed to discuss their impressions on the use of the PSI. The objective of the study was to assess the usefulness of the PSI in enhancing patient care in the clinical setting.
2 Patients and Methods
2.1 Study Design
This was a noninterventional, international, multicenter, cross-sectional study of the clinical usefulness of physicians’ use of the PSI with their patients with plaque psoriasis. Eight global clinical practice sites were selected by the IPC to participate in the study, including three sites in the USA (Farmington, CT; St. Louis, MO; and Salt Lake City, UT) and one site each in the UK (Manchester), the Netherlands (Nijmegen), Brazil (Porto Alegre), Chile (Santiago), and Canada (Quebec City). Study sites regularly treated patients with mild to severe psoriasis. All study sites obtained institutional review board (IRB) approval. All patients provided written informed consent prior to initiation of study-specific procedures.
At a regularly scheduled clinic visit, potentially eligible patients were identified and contacted by clinic staff, completed screening and enrollment, and were administered the paper 7-day recall version of the PSI. Patients were also asked about how much they were currently bothered by psoriasis symptoms, the severity of their current symptoms, the worst severity of their symptoms ever and before treatment, and the location(s) and severity of current psoriasis lesions. During the visit, the physician documented the patient’s psoriasis-affected body surface area (BSA) and static physician global assessment (sPGA) score [14], and used the patient’s information on the PSI to support discussions about the patient’s psoriasis signs and symptoms. After the visit, the physician completed a one-page survey about the visit. After enrollment was closed at each site (upon enrollment of ~ 35 patients), the participating physicians completed a 20–30-min qualitative telephone interview.
2.2 Patients
To be eligible, patients were adults (≥ 18 years of age), had physician-confirmed diagnosis of mild to severe plaque psoriasis, and were able to complete the PSI and discuss their symptoms with their physician. Patients who had any clinically relevant condition, were receiving treatment that could interfere with the patient’s ability to focus their responses on psoriasis symptoms, or were enrolled in a psoriasis investigational drug study were excluded. Enrollment was monitored to assure a distribution of ~ 40% mild psoriasis (affected BSA 0–4%), ~ 40% moderate psoriasis (BSA 5–9%), and ~ 20% severe psoriasis (BSA ≥ 10%), and that ~ 50% of the population was treatment naïve as well as balanced for demographic characteristics of sex and age.
2.3 Study Outcomes
The primary outcome was the physician experiences on the usefulness of the PSI based on physician surveys and interviews. The physician survey included questions about the length of time spent discussing the PSI, if other psoriasis symptoms were discussed, if any new information was obtained from the discussion, if the PSI data enhanced the discussion or interaction with the patient, any benefits that the PSI provided toward patient care, and if the PSI was useful to have during the visit. The qualitative interview was based on a structured interview guide, which used open-ended, exploratory questions by trained interviewers. Physician interviews were audio recorded, transcribed, and summarized. The transcripts were used to extract key quotations and summary statements against specific questions discussed during the interview process.
3 Results
3.1 Patients
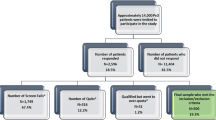
Across the eight study sites, 278 patients were enrolled in the study. The mean [standard deviation (SD)] age was 47.5 (14.0) years; 57.9% of the patients were male (Table 1). Additional demographic information is shown in Supplemental Table S1. Based on affected BSA, 47.8% of patients had mild psoriasis (range 40.0–67.5% across all sites), 29.1% had moderate psoriasis (range 12.5–40.0%), and 23.0% had severe psoriasis (range 17.5–42.9%). Across all patients, 18.7% had an sPGA score 0–1 (clear–almost clear) (range 2.9–28.6% across all sites), 67.3% had an sPGA score 2–3 (mild–moderate) (range 42.9–91.4%), and 14.0% had an sPGA score 4–5 (severe–very severe) (range 0–37.1%). Forty-nine patients (17.6%) were treatment-naïve or receiving no treatment for their psoriasis.
The mean (SD) PSI total score for all patients was 12.2 (8.3). Mean PSI item scores differed by study site, but all were within the range of SDs from the US validation study (Fig. 1) [8]. PSI total scores also differed by study site (range 10.3–14.9); study sites with a greater percentage of patients who had severe disease reported higher mean PSI total scores. The mean (SD) PSI total scores by study site were 12.6 (8.4) for CT, USA; 10.6 (7.9) for MO, USA; 13.3 (8.8) for UT, USA; 11.7 (9.2) for the UK; 10.5 (7.5) for the Netherlands; 14.9 (8.1) for Brazil; 12.9 (9.1) for Chile; and 10.3 (6.8) for Canada. Based on PSI total score categories, 107 patients (38.5%) had no/mild symptoms (PSI total score 0–8), 89 (32.0%) had moderate symptoms (PSI total score 9–16), 57 (20.5%) had severe symptoms (PSI total score 17–24), and 25 (9.0%) had very severe symptoms (PSI total score 25–32).
Mean PSI item scores by study site. Mean item scores are shown for study sites in Brazil (yellow), Canada (green), Chile (red), the Netherlands (gray), the UK (orange), the US sites (data from 3 sites pooled; blue), and the US study used to validate the PSI [8] (bold hashed line). Upper and lower dashed lines represent SDs for the US validation study. PSI Psoriasis Symptom Inventory, SD standard deviation
3.2 Physician Surveys
The PSI was considered to be a useful tool during the clinic visit for three-quarters of the participating patients. Overall, physicians spent a mean (SD) of 4.9 (4.8) min discussing the PSI with their patients (range 0–20 min). The amount of time spent discussing the PSI varied based on PSI total score category (none/mild, moderate, severe, and very severe) and treatment status (treated and treatment naïve). The mean (SD) time for treated patients was 3.4 (3.8) min for patients with none/mild symptoms, 5.1 (4.4) min for patients with moderate symptoms, 5.8 (6.6) min for patients with severe symptoms, and 6.7 (5.5) min for patients with very severe symptoms. The mean (SD) time for treatment-naïve patients was 6.1 (5.1) min for patients with none/mild symptoms, 4.5 (4.6) min for patients with moderate symptoms, 4.9 (4.7) min for patients with severe symptoms, and 7.8 (7.3) min for patients with very severe symptoms.
In the surveys, physicians noted that symptoms not usually discussed in routine visits were discussed in the context of the PSI, and patients were encouraged to discuss new information (Table 2). In some cases, physicians noted that the use of the PSI appeared to improve the patient–physician relationship.
3.3 Physician Interviews
In qualitative interviews, all eight physicians endorsed the PSI as an aid in patient–physician interactions regarding psoriasis disease management (Table 3). The PSI was determined to be useful for many reasons. There was a low time burden (less than 5 min) to discuss the information. The physicians obtained a better understanding of the patient-specific experiences related to psoriasis and often re-examined patient priorities for treatment. Over time, the PSI could be used to document progress in treatment satisfaction. The physicians also noted several benefits for patients with the use of the PSI. The instrument provided the patients with the ability to rate their symptoms in writing (which puts less pressure on the patient), the symptoms were provided in the instrument, and patients were less likely to underreport symptoms in the time-sensitive context of a clinic visit. Patients were able to address sensitive issues such as genital symptoms. Patients also discussed quality-of-life aspects as they related to their psoriasis signs and symptoms, and some patients were able to use PSI symptom ratings to alert the physician to their distress from their psoriasis signs and symptoms when they had been previously unable to do so verbally. Physicians, who generally focused on lesion size, were frequently directed to a specific lesion location when a sign or symptom was rated as severe by the patient. The PSI appeared to be particularly useful in driving communication with patients with low verbal aptitude. Physicians noted that the PSI discussions affected some treatment decisions. For example, one physician added topical therapy for specific lesions in patients who were receiving biologic therapies, and one physician opted for more aggressive regimens when the PSI score was high in patients with low affected BSA.
4 Discussion
In this study of the use of the PSI in the setting of routine clinical practice, we made three key observations. First, physicians received new information about their patients’ perceptions of psoriasis symptoms. For example, patients who appeared to the physician to have mild disease overall sometimes rated specific symptoms as very severe or noted symptoms in problem areas. Second, the PSI information helped with making decisions about care. In some instances, topical therapies were added to problem areas, and in some instances, systemic therapy was initiated. Third, the burden of the instrument was low for the patient and for the physician. Patients completed the instrument while waiting to see the physician, and the physicians required only 5 min on average during the visit to review the results.
Physicians and patients use different measures to estimate psoriasis severity in both clinical trials and in clinical practice. In psoriasis clinical trials, the PASI is the most commonly used measure of psoriasis severity and the Dermatology Life Quality Index (DLQI) is the most common measure of patient-reported health-related quality of life [15]. In clinical practice, physicians focus on elements of the PASI (e.g., size and appearance of lesions), whereas patients tend to focus on the location of lesions and impact of the disease on their lives. The correlation between improvements in psoriasis lesions (as measured by PASI) and improvements in quality of life (as measured by DLQI) varies, with some studies showing weak correlations [16, 17].
A recent study of patients enrolled in the Swedish psoriasis registry (PsoReg) showed that the decision to initiate systemic therapy was more strongly associated with the patient’s PASI score than with DLQI results [18]. While this approach is appropriate for most patients, patients with a low affected BSA who rated their disease as moderate to severe (~ 30% of patients in a recent survey [19]) represent a patient population that is likely to be undertreated. Patients with a single severe symptom (such as itch [20, 21]) or with lesions in certain areas (such as visible areas [22]) may report poor quality of life and yet have a low PASI score. A recent survey of dermatologists showed that the level of treatment satisfaction for approximately one in five patients was misaligned with the physician’s level of satisfaction with treatment [23]. These patients reported a poorer quality of life and more severe symptoms than the patients who were aligned with their physicians. Patients are reliable in the assessment of their disease severity [19, 24, 25]. These observations support a growing call for better communication between physicians and patients to achieve optimal treatment regimens, which improve quality of life [6, 26,27,28]. In particular, it has been suggested that physicians need to carefully evaluate the impacts of signs and symptoms on patients [19].
Differences in PSI item and total scores were noted between geographic regions, although statistically all values were within the SDs for item and total scores recorded in the validation study. For five of the eight PSI item scores, Latin American sites (Brazil and Chile) had the highest mean scores, which may reveal a significant cultural difference. While we do not know the specific reasons for these differences, ethnic and racial differences may potentially impact the perception and effects of psoriasis symptoms. Additionally, quality of life and standards of living vary geographically, which may impact perception of disease severity based on the geographic location of the patient. Cultural and geographic differences in the patient–physician relationship may also exist, and the PSI could potentially normalize these differences cross-culturally. Further studies in larger real-world populations are needed to understand these differences.
Differences were also seen in the time spent discussing the PSI based on PSI total scores. In both treated and treatment-naïve patients, the time spent discussing the PSI was longer in patients who had rated their symptoms as more severe on the PSI compared to patients with no/mild symptoms. Physicians may therefore consider the PSI score as an indication of the amount of time that may be required for a particular patient visit. Overall, the investigators responded that patients with severe psoriasis required more time during the clinical evaluation to discuss symptom scores. For example, among the treated group, a mean (SD) of 5.8 (6.6) min was spent on patients with severe symptoms, and among the treatment-naïve group, 4.9 (4.7) min was spent on patients with severe symptoms, and 7.8 (7.3) min was spent on patients with very severe symptoms. Notably, for patients with high PSI scores, a higher proportion of physicians noted that the PSI discussions assisted with decision on care and were useful to have during the visit (data not shown). The PSI may therefore be particularly useful for patients with severe/very severe disease.
There were some limitations to this study. Both the physicians and the patients were aware that the PSI was administered as part of a clinical survey, which could have introduced a bias towards favorable impressions of the instrument. The generalizability of the PSI usefulness may be restricted because the data were collected in referral centers focused on the treatment of psoriasis. An instrument that adds a 5-min discussion to a clinic visit could be construed as too burdensome for some physicians or patients. Some patients’ symptoms may be deliberately overestimated to increase the likelihood of obtaining systemic (primarily biologic) treatments; this may be driven by access to health care in some countries. Psoriatic arthritis, a common comorbidity in patients with psoriasis, is not addressed in the PSI, which assesses skin symptoms but not joint symptoms. The study did not address conversations about psoriatic arthritis in the physician surveys or interviews. Finally, although the overall sample size was large, the sample sizes of individual regions were too small to allow regional comparisons.
A strength of the study was the relatively large patient population that was recruited across several countries. Patients represented a wide range of disease severity and treatments, and the population was reasonably balanced among treatment-naïve and treatment-experienced patients and across genders. The global distribution of study sites allows for external validity of the instrument. The use of the PSI provides opportunities for working in the virtual environment. Patient-reported severity is condensed to a single-digit assessment. Importantly, the instrument can be used to document a treatment response.
5 Conclusion
In conclusion, the PSI has the potential to improve dermatologic practice by providing a comprehensive tool to assess psoriasis symptoms. In this study, physicians endorsed the usefulness of the PSI to discuss symptoms and symptom impacts in routine clinic visits. The discussions informed treatment decisions and enhanced physician–patient relationships. Despite the greater amount of time spent discussing the PSI in patients with more severe disease, physicians treating those patients reported an influence of the PSI discussion on treatment decisions. The PSI may improve communication between physicians and patients and provide an option for quality monitoring.
References
Weigle N, McBane S. Psoriasis. Am Fam Physician. 2013;87:626–33.
World Health Organization. Global report on psoriasis [WWW document]. http://apps.who.int/iris/bitstream/10665/204417/1/9789241565189_eng.pdf. Accessed 13 June 2019.
International Federation of Psoriasis Associations. Our cause: psoriasis [WWW document]. https://ifpa-pso.com/our-cause/. Accessed 13 June 2019.
Pariser D, Schenkel B, Carter C, et al. A multicenter, non-interventional study to evaluate patient-reported experiences of living with psoriasis. J Dermatolog Treat. 2016;27:19–26.
Armstrong AW, Schupp C, Wu J, et al. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003-2011. PLoS One. 2012;7:e52935.
Bhosle MJ, Kulkarni A, Feldman SR, et al. Quality of life in patients with psoriasis. Health Qual Life Outcomes. 2006;4:35.
Martin ML, McCarrier KP, Chiou CF, et al. Early development and qualitative evidence of content validity for the Psoriasis Symptom Inventory (PSI), a patient-reported outcome measure of psoriasis symptom severity. J Dermatolog Treat. 2013;24:255–60.
Bushnell DM, Martin ML, McCarrier K, et al. Validation of the Psoriasis Symptom Inventory (PSI), a patient-reported outcome measure to assess psoriasis symptom severity. J Dermatolog Treat. 2013;24:356–60.
Revicki DA, Jin Y, Wilson HD, et al. Reliability and validity of the Psoriasis Symptom Inventory in patients with moderate-to-severe psoriasis. J Dermatolog Treat. 2014;25:8–14.
Gordon KB, Kimball AB, Chau D, et al. Impact of brodalumab treatment on psoriasis symptoms and health-related quality of life: use of a novel patient-reported outcome measure, the Psoriasis Symptom Inventory. Br J Dermatol. 2014;170:705–15.
Viswanathan HN, Mutebi A, Milmont CE, et al. Measurement properties of the Psoriasis Symptom Inventory electronic daily diary in patients with moderate to severe plaque psoriasis. Value Health. 2017;20:1174–9.
Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005;8:94–104.
Wild D, Eremenco S, Mear I, et al. Multinational trials-recommendations on the translations required, approaches to using the same language in different countries, and the approaches to support pooling the data: the ISPOR Patient-Reported Outcomes Translation and Linguistic Validation Good Research Practices Task Force report. Value Health. 2009;12:430–40.
Pascoe VL, Enamandram M, Corey KC, et al. Using the Physician Global Assessment in a clinical setting to measure and track patient outcomes. JAMA Dermatol. 2015;151:375–81.
Garduno J, Bhosle MJ, Balkrishnan R, et al. Measures used in specifying psoriasis lesion(s), global disease and quality of life: a systematic review. J Dermatolog Treat. 2007;18:223–42.
Schafer I, Hacker J, Rustenbach SJ, et al. Concordance of the Psoriasis Area and Severity Index (PASI) and patient-reported outcomes in psoriasis treatment. Eur J Dermatol. 2010;20:62–7.
Griffiths CE, Sterry W, Brock F, et al. Pattern of response in patients with moderate-to-severe psoriasis treated with etanercept. Br J Dermatol. 2015;172:230–8.
Hagg D, Sundstrom A, Eriksson M, et al. Decision for biological treatment in real life is more strongly associated with the Psoriasis Area and Severity Index (PASI) than with the Dermatology Life Quality Index (DLQI). J Eur Acad Dermatol Venereol. 2015;29:452–6.
Korman NJ, Zhao Y, Li Y, et al. Clinical symptoms and self-reported disease severity among patients with psoriasis - Implications for psoriasis management. J Dermatolog Treat. 2015;26:514–9.
Globe D, Bayliss MS, Harrison DJ. The impact of itch symptoms in psoriasis: results from physician interviews and patient focus groups. Health Qual Life Outcomes. 2009;7:62.
Zhu B, Edson-Heredia E, Guo J, et al. Itching is a significant problem and a mediator between disease severity and quality of life for patients with psoriasis: results from a randomized controlled trial. Br J Dermatol. 2014;171:1215–9.
Heydendael VM, de Borgie CA, Spuls PI, et al. The burden of psoriasis is not determined by disease severity only. J Investig Dermatol Symp Proc. 2004;9:131–5.
Korman NJ, Zhao Y, Pike J, et al. Satisfaction with current psoriasis treatment: misalignment between physician and patient perceptions. Dermatol Online J. 2016;22. Retrieved from https://escholarship.org/uc/item/7405k1nn.
Feldman SR, Fleischer AB Jr, Reboussin DM, et al. The self-administered psoriasis area and severity index is valid and reliable. J Investig Dermatol. 1996;106:183–6.
Sampogna F, Sera F, Mazzotti E, et al. Performance of the self-administered psoriasis area and severity index in evaluating clinical and sociodemographic subgroups of patients with psoriasis. Arch Dermatol. 2003;139:353–8.
Nash AS, McAteer H, Schofield J, et al. Psoriasis today: experiences of healthcare and impact on quality of life in a major UK cohort. Prim Health Care Res Dev. 2015;16:415–23.
Strohal R, Prinz JC, Girolomoni G, et al. A patient-centred approach to biological treatment decision making for psoriasis: an expert consensus. J Eur Acad Dermatol Venereol. 2015;29:2390–8.
Gonzalez JM, Johnson FR, McAteer H, et al. Comparing preferences for outcomes of psoriasis treatments among patients and dermatologists in the U.K.: results from a discrete-choice experiment. Br J Dermatol. 2017;176:777–85.
Acknowledgements
Dikran Toroser (Amgen Inc.) and Julia R. Gage (on behalf of Amgen Inc.) provided medical writing support. This research was supported by a grant from Amgen, and R.B. Warren is supported by the NIHR Manchester Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Immunex, a wholly owned subsidiary of Amgen Inc.
Conflict of interest
B. Strober serves as a consultant for AbbVie Inc., Almirall, S.A., Amgen Inc., AstraZeneca, Celgene Corp., Dermira, Inc., Janssen Global Services, LLC, LEO Pharma Inc., Eli Lilly & Co., GlaxoSmithKline, plc, Medac Pharma Inc., Menlo Therapeutics, Novartis AG, Pfizer Inc., UCB, Sun Pharma, and Ortho Dermatologics/Valeant Pharmaceuticals; is an investigator for AbbVie Inc., Boehringer Ingelheim, Celgene Corp., Eli Lilly & Co., Galderma S.A., Janssen Global Services, LLC, Merck & Co., Inc., and Sienna Biopharmaceuticals; serves as Scientific Director for the Corrona Psoriasis Registry; and has received grant support to the University of Connecticut Fellowship Program from AbbVie Inc. and Janssen Global Services, LLC. P.C.M. van de Kerkhof is a consultant for Abbott Laboratories, Almirall, S.A., Amgen Inc., Celgene Corp., Centocor, Eli Lilly & Co., Galderma S.A., Janssen-Cilag, LEO Pharma Inc., Mitsubishi Tanabe Pharma America, Inc., Novartis AG, Pfizer Inc., Koninklijke Philips N.V., and Sandoz International GmbH; and is an investigator for AbbVie Inc., Amgen Inc., Basilea Pharmaceutica Ltd., Eli Lilly & Co., Janssen-Cilag, LEO Pharma Inc., Koninklijke Philips N.V., and Pfizer Inc. K. Callis Duffin has received research grants from AbbVie Inc., Amgen Inc., Celgene Corp., Eli Lilly & Co., Janssen Global Services, LLC, Novartis AG, Pfizer Inc., Sienna Biopharmaceuticals, and Stiefel Laboratories, Inc.; and has received consulting fees from AbbVie Inc., Amgen Inc., Celgene Corp., Eli Lilly & Co., Janssen Global Services, LLC, Novartis AG, Pfizer Inc., Sienna Biopharmaceuticals, and Stiefel Laboratories, Inc. Y. Poulin has received research grants from Boehringer Ingelheim, Bristol-Myers Squibb, Celgene Corp., Eli Lilly & Co., Galderma S.A., GlaxoSmithKline plc, LEO Pharma Inc., MedImmune, Merck & Co., Inc., Novartis AG, Pfizer Inc., Regeneron, and UCB; and serves on speakers bureaus for AbbVie Inc., Amgen Inc., Eli Lilly & Co., Novartis AG, and Sanofi Genzyme. R.B. Warren has received research grants from AbbVie Inc., Almirall, S.A., Amgen Inc., Celgene Corp., Eli Lilly & Co., Janssen Global Services, LLC, LEO Pharma Inc., Novartis AG, Pfizer Inc., and UCB; and is a consultant for AbbVie Inc., Almirall, S.A., Amgen Inc., Boehringer Ingelheim, Celgene Corp., Eli Lilly & Co., Janssen Global Services, LLC, LEO Pharma Inc., Novartis AG, Pfizer Inc., Sanofi, XenoPort, Inc., and UCB. C. de La Cruz has received research grants from AbbVie Inc., Amgen Inc., Coherus Biosciences, Eli Lilly & Co., Genentech, Neovacs S.A., Novartis AG, and Pfizer Inc.; and is a consultant for AbbVie Inc., Janssen Global Services, LLC, Novartis AG, and Pfizer Inc. J. van der Walt has no conflicts to declare. B.S. Stolshek is an employee and shareholder of Amgen Inc. M.L. Martin is an employee of Health Research Associates, Inc., which received funding from Amgen Inc. to conduct this study. A.V.E. de Carvalho has received research grants from Amgen Inc. and serves on speakers bureaus for Janssen Global Services, LLC, Novartis AG, and Pfizer Inc.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Strober, B., van de Kerkhof, P.C.M., Callis Duffin, K. et al. Feasibility and Utility of the Psoriasis Symptom Inventory (PSI) in Clinical Care Settings: A Study from the International Psoriasis Council. Am J Clin Dermatol 20, 699–709 (2019). https://doi.org/10.1007/s40257-019-00458-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-019-00458-2