Abstract
Background
Metformin and sodium-glucose cotransporter-2 (SGLT2) inhibitors have demonstrated cardiovascular benefits but their comparative effects on mortality in type 2 diabetes mellitus (T2DM) patients with cardiovascular disease (CVD) are unknown. Hence, we evaluated and compared lifetime benefits arising from metformin or SGLT2 inhibitors in T2DM patients with CVD.
Materials and Methods
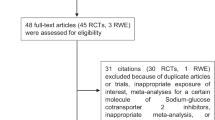
Studies published in the PubMed, EMBASE and CENTRAL databases before 28 October 2023 were retrieved. Treatment effects of metformin against US FDA-approved SGLT2 inhibitors in T2DM patients with CVD were evaluated and lifetime gains in event-free survival were estimated from our primary endpoints of all-cause and cardiovascular mortality. Risk ratios were derived to assess their impact on secondary outcomes such as major adverse cardiovascular events and hospitalizations for heart failure.
Results
Overall, 14 studies were included. Five studies published Kaplan–Meier curves for the primary outcome of all-cause mortality. Individual participant data were reconstructed from these Kaplan–Meier curves, from which we conducted our two-stage meta-analysis. Participants receiving metformin and SGLT2 inhibitors experienced a reduction in the risk for all-cause mortality as compared with those not taking metformin and placebo. However, participants receiving SGLT2 inhibitors had a higher all-cause mortality (hazard ratio 1.308, 95% confidence interval 1.103–1.550) versus metformin. Treatment with metformin was estimated to offer an additional 23.26 months of survival free from all-cause mortality versus 23.04 months with SGLT2 inhibitors.
Conclusions
In patients with T2DM and CVD, metformin and SGLT2 inhibitors were associated with substantially lower all-cause mortality rates and slightly longer life expectancies than in patients without. Metformin presented an advantage over SGLT2 inhibitors in reducing all-cause mortality.



Similar content being viewed by others
References
Sun H, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. https://doi.org/10.1016/j.diabres.2021.109119.
Stam-Slob MC, et al. Effect of type 2 diabetes on recurrent major cardiovascular events for patients with symptomatic vascular disease at different locations. Diabetes Care. 2015;38(8):1528–35. https://doi.org/10.2337/dc14-2900.
Shin H, et al. Trends in first-line glucose-lowering drug use in adults with type 2 diabetes in light of emerging evidence for SGLT-2i and GLP-1RA. Diabetes Care. 2021;44(8):1774–82. https://doi.org/10.2337/dc20-2926.
Moran GM, et al. Type 2 diabetes: summary of updated NICE guidance. BMJ. 2022;377:o775. https://doi.org/10.1136/bmj.o775.
American Diabetes Association Professional Practice Committee. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2022. Diabetes Care, 2022; 45(Suppl 1):S125-S143. doi:https://doi.org/10.2337/dc22-S009
Pernicova I, Korbonits M. Metformin–mode of action and clinical implications for diabetes and cancer. Nat Rev Endocrinol. 2014;10(3):143–56. https://doi.org/10.1038/nrendo.2013.256.
Holman RR, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89. https://doi.org/10.1056/NEJMoa0806470.
Vallon V. The mechanisms and therapeutic potential of SGLT2 inhibitors in diabetes mellitus. Annu Rev Med. 2015;66:255–70. https://doi.org/10.1146/annurev-med-051013-110046.
Han S, et al. Dapagliflozin, a selective SGLT2 inhibitor, improves glucose homeostasis in normal and diabetic rats. Diabetes. 2008;57(6):1723–9. https://doi.org/10.2337/db07-1472.
Zinman B, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28. https://doi.org/10.1056/NEJMoa1504720.
Neal B, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57. https://doi.org/10.1056/NEJMoa1611925.
Perkovic V, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306. https://doi.org/10.1056/NEJMoa1811744.
Wiviott SD, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2018;380(4):347–57. https://doi.org/10.1056/NEJMoa1812389.
McMurray JJV, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008. https://doi.org/10.1056/NEJMoa1911303.
Packer M, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383(15):1413–24. https://doi.org/10.1056/NEJMoa2022190.
Anker SD, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451–61. https://doi.org/10.1056/NEJMoa2107038.
van Walraven C. Should sodium-glucose cotransporter-2 inhibitors be first-line treatment for patients with type 2 diabetes? CMAJ. 2020;192(14):e375–6. https://doi.org/10.1503/cmaj.200426.
Zaccardi F, et al. First-line treatment for type 2 diabetes: is it too early to abandon metformin? Lancet. 2020;396(10264):1705–7. https://doi.org/10.1016/s0140-6736(20)32523-x.
Cosentino F, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). Eur Heart J. 2019;41(2):255–323. https://doi.org/10.1093/eurheartj/ehz486.
Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700.
Guyot P, et al. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12(1):9. https://doi.org/10.1186/1471-2288-12-9.
Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81(3):515–26. https://doi.org/10.1093/biomet/81.3.515.
Haddaway NR, et al. PRISMA2020: an R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev. 2022;18(2): e1230. https://doi.org/10.1002/cl2.1230.
Cefalu WT, et al. Dapagliflozin’s effects on glycemia and cardiovascular risk factors in high-risk patients with type 2 diabetes: a 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. Diabetes Care. 2015;38(7):1218–27. https://doi.org/10.2337/dc14-0315.
Retwiński A, et al. The influence of metformin and the presence of type 2 diabetes mellitus on mortality and hospitalisation in patients with heart failure. Kardiol Pol. 2018;76(9):1336–43. https://doi.org/10.5603/KP.a2018.0127.
Abualsuod A, et al. The effect of metformin use on left ventricular ejection fraction and mortality post-myocardial infarction. Cardiovasc Drugs Ther. 2015;29(3):265–75. https://doi.org/10.1007/s10557-015-6601-x.
Mahaffey KW, et al. Canagliflozin for primary and secondary prevention of cardiovascular events: results from the CANVAS Program (Canagliflozin Cardiovascular Assessment Study). Circulation. 2018;137(4):323–34. https://doi.org/10.1161/CIRCULATIONAHA.117.032038.
Roussel R, et al. Metformin use and mortality among patients with diabetes and atherothrombosis. Arch Intern Med. 2010;170(21):1892. https://doi.org/10.1001/archinternmed.2010.409.
Shah DD, Fonarow GC, Horwich TB. Metformin therapy and outcomes in patients with advanced systolic heart failure and diabetes. J Card Fail. 2010;16(3):200–6. https://doi.org/10.1016/j.cardfail.2009.10.022.
Cannon CP, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020;383(15):1425–35. https://doi.org/10.1056/NEJMoa2004967.
Hong J, et al. Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease. Diabetes Care. 2013;36(5):1304–11. https://doi.org/10.2337/dc12-0719.
Park S, et al. Association of sodium-glucose cotransporter 2 inhibitors with post-discharge outcomes in patients with acute heart failure with type 2 diabetes: a cohort study. Cardiovasc Diabetol. 2023;22(1):191. https://doi.org/10.1186/s12933-023-01896-3.
Chen T-H, et al. Sodium-glucose cotransporter 2 inhibitor versus metformin as first-line therapy in patients with type 2 diabetes mellitus: a multi-institution database study. Cardiovasc Diabetol. 2020;19(1):189. https://doi.org/10.1186/s12933-020-01169-3.
Shin H, et al. Cardiovascular outcomes in patients initiating first-line treatment of type 2 diabetes with sodium-glucose cotransporter-2 inhibitors versus metformin: a cohort study. Ann Intern Med. 2022;175(7):927–37. https://doi.org/10.7326/m21-4012.
Inzucchi SE, et al. Are the cardiovascular and kidney benefits of empagliflozin influenced by baseline glucose-lowering therapy? Diabetes Obes Metab. 2020;22(4):631–9. https://doi.org/10.1111/dom.13938.
Chew NWS, et al. The global burden of metabolic disease: Data from 2000 to 2019. Cell Metab. 2023;35(3):414-428.e3. https://doi.org/10.1016/j.cmet.2023.02.003.
Guembe MJ, et al. Risk for cardiovascular disease associated with metabolic syndrome and its components: a 13-year prospective study in the RIVANA cohort. Cardiovasc Diabetol. 2020;19(1):195. https://doi.org/10.1186/s12933-020-01166-6.
Mottillo S, et al. The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–32. https://doi.org/10.1016/j.jacc.2010.05.034.
Khan J, et al. Mechanisms of ageing: growth hormone, dietary restriction, and metformin. Lancet Diabetes Endocrinol. 2023;11(4):261–81. https://doi.org/10.1016/s2213-8587(23)00001-3.
Mohammed I, et al. A critical review of the evidence that metformin is a putative anti-aging drug that enhances healthspan and extends lifespan. Front Endocrinol (Lausanne). 2021;12:718942. https://doi.org/10.3389/fendo.2021.718942.
Cardoso R, et al. SGLT2 inhibitors decrease cardiovascular death and heart failure hospitalizations in patients with heart failure: A systematic review and meta-analysis. eClinicalMedicine. 2021;2021:36. https://doi.org/10.1016/j.eclinm.2021.100933.
Griffin SJ, Leaver JK, Irving GJ. Impact of metformin on cardiovascular disease: a meta-analysis of randomised trials among people with type 2 diabetes. Diabetologia. 2017;60(9):1620–9. https://doi.org/10.1007/s00125-017-4337-9.
Han Y, et al. Effect of metformin on all-cause and cardiovascular mortality in patients with coronary artery diseases: a systematic review and an updated meta-analysis. Cardiovasc Diabetol. 2019;18(1):96. https://doi.org/10.1186/s12933-019-0900-7.
Singh AK, Singh R. Cardiovascular Outcomes with SGLT-2 inhibitors in patients with heart failure with or without type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Diabetes Metab Syndr. 2021;15(1):351–9. https://doi.org/10.1016/j.dsx.2021.01.006.
Wu JH, et al. Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, and major safety outcomes in adults with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2016;4(5):411–9. https://doi.org/10.1016/s2213-8587(16)00052-8.
de Boer IH, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and kidney disease: improving global outcomes (KDIGO). Diabetes Care. 2022;45(12):3075–90. https://doi.org/10.2337/dci22-0027.
Khunti K, et al. Re-examining the widespread policy of stopping sodium-glucose cotransporter-2 inhibitors during acute illness: A perspective based on the updated evidence. Diabetes Obes Metab. 2022;24(11):2071–80. https://doi.org/10.1111/dom.14805.
Shao SC, et al. Differences in outcomes of hospitalizations for heart failure after SGLT2 inhibitor treatment: effect modification by atherosclerotic cardiovascular disease. Cardiovasc Diabetol. 2021;20(1):213. https://doi.org/10.1186/s12933-021-01406-3.
Sarraju A, et al. Effects of canagliflozin on cardiovascular, renal, and safety outcomes in participants with type 2 diabetes and chronic kidney disease according to history of heart failure: results from the CREDENCE trial. Am Heart J. 2021;233:141–8. https://doi.org/10.1016/j.ahj.2020.12.008.
Solomon SD, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med. 2022;387(12):1089–98. https://doi.org/10.1056/NEJMoa2206286.
Jong CB, et al. Metformin was associated with lower all-cause mortality in type 2 diabetes with acute coronary syndrome: A Nationwide registry with propensity score-matched analysis. Int J Cardiol. 2019;291:152–7. https://doi.org/10.1016/j.ijcard.2019.03.021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Hon Jen Wong, Norman H. Lin, Yao Neng Teo, Nicholas L. Syn, Yao Hao Teo, and Ching-Hui Sia declare they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Funding
No sources of funding were used to assist in the preparation of this study.
Ethics approval
Not applicable.
Data availability statement
This manuscript makes use of publicly available data from published studies, hence no original data are available for sharing.
Code availability
Not applicable.
Author contributions
HJW, NHL, YNT, NLS, YHT and CHS were responsible for the conceptualization and design of the study. HJW, NHL and YNT formulated the search strategy. HJW and NHL conducted the screening for eligible studies, extracted the data and performed the risk-of-bias assessment. HJW and YNT reconstructed individual participant data. HJW, YNT and YHT performed the statistical analyses. HJW, NHL, YNT, NLS, YHT and CHS interpreted the data. HJW and NHL drafted the first manuscript. HJW, NHL, YNT, NLS, YHT and CHS critically reviewed and edited the manuscript. NLS, YHT and CHS supervised the study. All authors contributed to the article and approved the submitted version.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wong, H.J., Lin, N.H., Teo, Y.N. et al. Evaluation of the Lifetime Benefits of Metformin and SGLT2 Inhibitors in Type 2 Diabetes Mellitus Patients with Cardiovascular Disease: A Systematic Review and Two-Stage Meta-Analysis. Am J Cardiovasc Drugs (2024). https://doi.org/10.1007/s40256-024-00640-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s40256-024-00640-w