Abstract
Purpose
We aimed to explore possible contributors to discrepancies between randomized controlled trials (RCTs) and real-world observational studies (OS) in cardiovascular benefits of sodium-glucose cotransporter 2 (SGLT2) inhibitors in type 2 diabetes (T2D) patients.
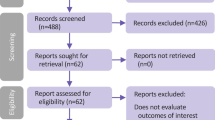
Methods
We searched PubMed and EMBASE to identify meta-analyses of RCTs and OS on cardiovascular effects of SGLT2 inhibitors in T2D patients. Cardiovascular outcomes included major adverse cardiovascular events (MACE), myocardial infarction (MI), stroke, cardiovascular mortality (CVM), all-cause mortality (ACM), hospitalization for heart failure (HHF), and atrial fibrillation (AF). We examined the summary relative risk (RR) and 95% confidence interval (CI) for each endpoint from meta-analyses of RCTs.
Results
We identified and included 15 eligible meta-analyses, 13 for RCTs and 2 for OS, with moderately strong evidence. The results revealed a significant discrepancy between RCTs and OS for MI (RR, 95% CI 1.05, 0.82–1.38; I = 91.5% versus odds ratio (OR), 95% CI 0.77, 0.73–0.81; I = 15.0%), stroke (RR, 95% CI 0.99, 0.76–1.29; I = 93.4% versus OR, 95% CI 0.75, 0.72–0.78; I = 23.0%), and AF (RR, 95% CI 0.72, 0.62–0.85; I = 0.0% versus OR, 95% CI 0.92, 0.83–1.02; I = 0.0%).
Conclusion
OS presented significant benefits of SGLT2 inhibitors both on primary and secondary preventions of MACE, MI, stroke, ACM, CVM, and HHF; RCTs did not. Given the spectrum of T2D patient characteristics and the strength of overall evidence, our review underscored the importance of constant integration of all available information and critical interpretation of all inconsistencies to optimize evidence-based diabetes care.


Similar content being viewed by others
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SGLT2 :
-
Sodium-glucose cotransporter 2
- T2D :
-
Type 2 diabetes
- FDA :
-
Food and Drug Administration
- CVD :
-
Cardiovascular disease
- RCTs :
-
Randomized clinical trials
- RWE :
-
Real-world evidence
- OS :
-
Observational studies
- CV :
-
Cardiovascular
- PRISMA :
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- CI :
-
Confidence interval
- MACE :
-
Major adverse cardiovascular events
- MI :
-
Myocardial infarction
- ACM :
-
All-cause mortality
- CVM :
-
CV-specific mortality
- HHF :
-
Hospitalization for heart failure
- AF :
-
Atrial fibrillation
- RR :
-
Relative risk
- AMSTAR :
-
A MeaSurement Tool to Assess systematic Reviews
- GRADE :
-
Grading of Recommendations, Assessment, Development and Evaluation
- OR :
-
Odds ratio
References
Marx N, Davies MJ, Grant PJ, Mathieu C, Petrie JR, Cosentino F et al (2021) Guideline recommendations and the positioning of newer drugs in type 2 diabetes care. Lancet Diabetes Endocrinol 9(1):46–52
Poole RM, Dungo RT (2014) Ipragliflozin: first global approval. Drugs 74(5):611–617
Markham A, Elkinson S (2014) Luseogliflozin: first global approval. Drugs 74(8):945–950
Poole RM, Prossler JE (2014) Tofogliflozin: first global approval. Drugs 74(8):939–944
Bragg F, Holmes MV, Iona A, Guo Y, Du H, Chen Y et al (2017) Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA 317(3):280–289
Gregg EW, Cheng YJ, Srinivasan M, Lin J, Geiss LS, Albright AL et al (2018) Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: an epidemiological analysis of linked national survey and vital statistics data. Lancet 391(10138):2430–2440
Cherney DZI, Udell JA (2016) Use of sodium glucose cotransporter 2 inhibitors in the hands of cardiologists with great power comes great responsibility. Circulation 134(24):1915–1917
Ioannidis JP, Haidich AB, Pappa M, Pantazis N, Kokori SI, Tektonidou MG et al (2001) Comparison of evidence of treatment effects in randomized and nonrandomized studies. JAMA 286(7):821–830
Monti S, Grosso V, Todoerti M, Caporali R (2018) Randomized controlled trials and real-world data: differences and similarities to untangle literature data. Rheumatology 57:54–58
Rothwell PM (2005) External validity of randomised controlled trials: “To whom do the results of this trial apply?”. Lancet 365(9453):12.
Sawchik J, Hamdani J, Vanhaeverbeek M (2018) Randomized clinical trials and observational studies in the assessment of drug safety. Rev Epidemiol Sante 66(3):217–225
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J et al (2009) AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 62(10):1013–1020
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S et al (2004) Grading quality of evidence and strength of recommendations. Bmj-Brit Med J 328(7454):1490
Ghosh-Swaby OR, Goodman SG, Leiter LA, Cheng A, Connelly KA, Fitchett D et al (2020) Glucose-lowering drugs or strategies, atherosclerotic cardiovascular events, and heart failure in people with or at risk of type 2 diabetes: an updated systematic review and meta-analysis of randomised cardiovascular outcome trials. Lancet Diabetes Endocrinol 8(5):418–435
Guo M, Ding J, Li J, Wang J, Zhang T, Liu C et al (2018) SGLT2 inhibitors and risk of stroke in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab 20(8):1977–1982
Li WJ, Chen XQ, Xu LL, Li YQ, Luo BH (2020) SGLT2 inhibitors and atrial fibrillation in type 2 diabetes: a systematic review with meta-analysis of 16 randomized controlled trials. Cardiovasc Diabetol 19(1):130
Monami M, Dicembrini I, Mannucci E (2017) Effects of SGLT-2 inhibitors on mortality and cardiovascular events: a comprehensive meta-analysis of randomized controlled trials. Acta Diabetol 54(1):19–36
Radholm K, Wu JH, Wong MG, Foote C, Fulcher G, Mahaffey KW et al (2018) Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular disease, death and safety outcomes in type 2 diabetes - a systematic review. Diabetes Res Clin Pract 140:118–128
Saad M, Mahmoud AN, Elgendy IY, Abuzaid A, Barakat AF, Elgendy AY et al (2017) Cardiovascular outcomes with sodium-glucose cotransporter-2 inhibitors in patients with type II diabetes mellitus: a meta-analysis of placebo-controlled randomized trials. Int J Cardiol 228:352–358
Toyama T, Neuen BL, Jun M, Ohkuma T, Neal B, Jardine MJ et al (2019) Effect of SGLT2 inhibitors on cardiovascular, renal and safety outcomes in patients with type 2 diabetes mellitus and chronic kidney disease: a systematic review and meta-analysis. Diabetes Obes Metab 21(5):1237–1250
Usman MS, Siddiqi TJ, Memon MM, Khan MS, Rawasia WF, Ayub MT et al (2018) Sodium-glucose co-transporter 2 inhibitors and cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol 25(5):495–502
Wu JH, Foote C, Blomster J, Toyama T, Perkovic V, Sundstrom J et al (2016) Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, and major safety outcomes in adults with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 4(5):411–419
Zhang A, Luo X, Meng H, Kang J, Qin G, Chen Y et al (2020) Sodium glucose cotransporter 2 inhibitors reduce the risk of heart failure hospitalization in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Front Endocrinol (Lausanne) 11:604250
Arnott C, Li Q, Kang A, Neuen BL, Bompoint S, Lam CSP et al (2020) Sodium-glucose cotransporter 2 inhibition for the prevention of cardiovascular events in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. J Am Heart Assoc 9(3):e014908
Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP et al (2019) SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 393(10166):31–39
Lu Y, Li F, Fan Y, Yang Y, Chen M, Xi J (2021) Effect of SGLT-2 inhibitors on cardiovascular outcomes in heart failure patients: a meta-analysis of randomized controlled trials. Eur J Intern Med 87:20–28
Li CX, Liang S, Gao L, Liu H (2021) Cardiovascular outcomes associated with SGLT-2 inhibitors versus other glucose-lowering drugs in patients with type 2 diabetes: a real-world systematic review and meta-analysis. PLoS ONE 16(2):e0244689
Singh AK, Singh R (2019) Heart failure hospitalization with SGLT-2 inhibitors: a systematic review and meta-analysis of randomized controlled and observational studies. Expert Rev Clin Pharmacol 12(4):299–308
Einarson TR, Acs A, Ludwig C, Panton UH (2018) Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovas Dia 17
Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U et al (2020) Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med 383(15):1425–1435
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377(7):644–657
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A et al (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380(4):347–357
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373(22):2117–2128
Nordon C, Karcher H, Groenwold RH, Ankarfeldt MZ, Pichler F, Chevrou-Severac H et al (2016) The “efficacy-effectiveness gap”: historical background and current conceptualization. Value Health 19(1):75–81
Author information
Authors and Affiliations
Contributions
Seo, BJ has collected and analyzed/interpreted the data and drafted the manuscript. Song, Y has made substantial contributions to the design of this study, interpreted the data, and substantively revised the manuscript with a wide range of clinical and epidemiologic expertise. Su, J has made some contributions to the study conception and data interpretation from cardiological perspectives and reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable, since this study is an umbrella review that used published data of meta-analyses. Thus, we did not collect deeply personal, sensitive, or confidential information from participants, but just used publicly accessible documents as evidence. Therefore, there was no need to seek an institutional ethics approval and gain any consent to participate before commencing this study.
Consent for publication
Not applicable, our manuscript does not contain data from any individual person.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Seo, B., Su, J. & Song, Y. Exploring heterogeneities of cardiovascular efficacy and effectiveness of SGLT2 inhibitors in patients with type 2 diabetes: an umbrella review of evidence from randomized clinical trials versus real-world observational studies. Eur J Clin Pharmacol 78, 1205–1216 (2022). https://doi.org/10.1007/s00228-022-03327-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03327-w