Abstract
Meibomian gland dysfunction (MGD) can be characterized by terminal duct obstruction as well as associated changes in glandular secretion. The diagnosis of MGD and other MGD-related disorders is based on abnormal expressions of the anatomic and physiological compositions of the meibomian glands. Four basic clinical subtypes and a series of clinical tests can be performed to aid in the diagnosis of MGD. Future studies are necessary to document glandular atresia. Qualitative and quantative meibography should prove useful for glandular characterization of the extent of MGD and for objective evaluation of the effect of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meibomian gland dysfunction, as stated in the International Workshop on Meibomian Gland Dysfunction, is a chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction and/or qualitative/quantitative changes in the glandular secretion. It may result in alteration of the tear film, symptoms of eye irritation, clinically apparent inflammation, and ocular surface disease (OSD) [1••]. Diagnosis of MG dysfunction (MGD), as well as other MGD-related disorders is based on abnormal expressions of the anatomic and physiological compositions of the meibomian glands. The purpose of this article is to address the clinical diagnosis of MGD, as well as the applied tests that are used in making the diagnosis. This article is divided into three sections. Part I will discuss the four major clinical subtypes in patients suffering from MGD. Part II will elaborate on the major clinical ocular surface and lid margin signs found in patients suffering from MGD. Finally, part III will discuss how to make a clinical diagnosis within a specialized clinic. Here we will address all the clinical tests conducted, as well as the grading system that is used for grading severity.
Meibomian Gland Activity
The meibomian glands are located on the tarsal plates. In normal subjects, the meibomian orifices are disposed at regular intervals along the lid margins, just anterior to the mucocutaneous junction. Biomicroscopically, they are surrounded by a characteristic ring-shaped architecture, reflecting the concentric arrangement of orifice, mucosa, distal acini, fibers of the muscle of Riolan, and the connective tissue sheath of the glands [2–4]. This arrangement of the glands becomes less well circumscribed and orderly with aging. As MGD progresses, the glands’ structural arrangement also becomes more unorganized and atretic, with loss of the gland.
Meibomian glands secrete a lipid at lid temperature that is delivered to the skin of the lid margin as a clear fluid termed meibum [5]. There, it forms shallow reservoirs on both the upper and lower lid margins from which the tear film lipid layer (TFLL) is formed and replenished. The amount of meibum present in the normal lower lid reservoir can be measured by the meibometry technique and used to deduce the content of the total lid reservoir [6–8].
MGD can be an asymptomatic subclinical condition that is detected only by gland expression or meibography. The distribution of affected meibomian glands in MGD may be diffusely located in both the upper and lower lids or can present in a more localized region of the eyelids either nasally or temporally. Alternatively, it may be symptomatic accompanied by specific ocular surface clinical signs [9, 10]. MGD may be primary and not related to other local or systemic disease, or it may be secondary to several systemic disorders. The natural history of MGD is not yet known; however, it should be seen as a developmental but treatable disease in which treatment may prevent progression and irreversible ocular surface changes. The decision to treat is based on the diagnosis and severity of the disease process. The diagnosing of MGD may be straightforward; however, quantifying the degree and the severity of MGD as the basis for treatment is much more complex [1••].
The diagnosis of MGD can be arrived at by the demonstration of a single affected gland. However, clinically relevant disease most often includes multiple affected glands. Therefore, making the diagnosis demands both a qualitative and quantitative approach [11–13]. The clinical features of MGD may be intrinsic when they involve the meibomian glands alone and the lid tissues in their immediate area, or they may be extrinsic, where they affect neighboring lid structures [1••].
With the background that is presented, meibomian glands can be summarized as follows: The glands are under neural and hormonal control and secrete their oil into shallow reservoirs on the lid margins. Lipid secretion is intrinsic to the glands, and the meibum delivery is aided by the blink [14]. Not all glands are active at a given time, with the possible inference that each gland goes through a cycle of activity followed by a period of quiescence, when acinar stores are replenished. There is an uneven distribution of gland activity along the length of the lid, with the least distribution temporally and the greatest distribution nasally [15].
Clinical Subtypes in Patients with MGD
When diagnosing a patient with MGD, they can be classified into one of four major clinical subtypes [1••]. Characterization of these four subtypes requires an initial diagnosis of MGD, followed by the inclusion or exclusion of other OSDs. Diagnostic tests for each subtype will be explained in detail in section three. The four clinical subtypes include:
-
(1)
MGD alone (symptomatic and asymptomatic)
-
(2)
MGD associated with ocular surface damage
-
(3)
MGD-related evaporative dry eye
-
(4)
MGD associated with additional ocular surface disorders
MGD Alone, Symptomatic and Asymptomatic
Meibomian gland dysfunction has both subjective and objective features [16, 17]. Symptoms can be a large part in this complex disease. Some symptoms that characterize MGD can include personal habits related to the condition. These could be lid rubbing to relieve itching and irritation, lid redness and swelling in the absence of crusts or flakes, and the presence of sensory symptoms referable to the lid margins (itching, irritation, and soreness). Global features included ocular surface damage, tear instability, and tear hyperosmolarity. There are key clinical signs of MGD that a clinician should look for, such as: meibomian gland dropout, altered meibomian gland secretion, and changes in lid morphology such as lid margin vascularity of the area between the anterior and posterior edges of the lid.
Although MGD is a symptomatic disorder, it does go through an asymptomatic preclinical stage, when its presence may be missed by the clinician. When MGD is at this stage, it may be more readily diagnosed by meibomian gland expression [9, 10, 18–20]. This is shown through the demonstration of an altered quality of expressed secretions and/or decreased or absent expression. As the disease progresses, MGD most often becomes symptomatic, and additional lid margin signs such as vascular changes may be detected with the slit lamp. With these associated findings, MGD-related “posterior blepharitis” is said to be present. Since it is often stated that signs and symptoms do not correlate in dry eye and OSD, it is imperative to treat both positive symptoms when signs are absent. Moreover, when there are no solicited symptoms but positive spectrum of MGD-related signs, it is in our opinion important to treat and treat aggressively.
MGD with Associated Ocular Surface Damage
There are a variety of disorders affecting the conjunctiva, cornea, and the lids that may be grouped together in the category of OSD [21]. These include lid and conjunctival disorders, including ocular rosacea, lagophthalmus, senile entropion or ectropion, Stevens-Johnson syndrome, conjunctival chalasis, and pterygia, respectively. These disorders are also responsible for aqueous-deficient and evaporative dry eye. A certain overlap has been noticed among them. A disorder in one category can be associated with a disorder in another category [22]. OSDs may cause severe damage to the surface. Various reasons have been proposed for such damage, including the release of inflammatory mediators into the tear film and the mechanisms of evaporative dry eye [1••]. Damage to the ocular surface may be quantified by grading the staining of the cornea and conjunctiva through the use of a lissamine green stain.
MGD-Related Evaporative Dry Eye
In MGD the amount of meibum delivered to the lid’s lipid reservoir is reduced. This can result in meibomian gland obstruction, gland atrophy, and malpositioned orifices, causing the ductal portions of the gland to be stretched and narrowed.
Several mechanisms may often be at work when these multiple forms of MGD occur together. As MGD progresses, the amount of meibum in the reservoir, or its distribution along the lid margins, is insufficient to maintain the normal TFLL. Abnormal meibum composition could also contribute to this disturbance.
Abnormalities of the TFLL include abnormal or slow-spreading oil patterns, vertical interferometry patterns that relate to reduced TFLL stability. All of these abnormalities are accompanied by an increased evaporative water loss. It is noted that spreading of the TFLL is altered in the higher degrees of aqueous-deficient dry eye. This spreading has also been attributed to thinning of the aqueous layer of the tear film. In a recent publication, it was suggested that this effect gives rise to a functional TFLL deficiency and a consequent increased evaporative water loss [23–26]. Therefore, it is proposed that a functional evaporative dry eye may also occur in the presence of aqueous-deficient dry eye.
MGD Associated with Additional Ocular Surface Disorders
It has been reported in the literature that there may be an association of MGD with other ocular and systemic disorders. These include contact lens intolerance, meibomian keratoconjunctivitis, as well as some particular skin conditions [27••]. McCulley and Sciallis [28, 29] described a condition of tear film instability, ocular inflammation, and ocular surface damage in a group of patients with chronic blepharitis, which they called MKC. In the conducted study, patients exhibited both anterior and posterior blepharitis and some form of associated skin disorder. Signs of obstructive MGD were associated with conjunctival injection and superficial punctate keratitis, preferentially affecting the lower interpalpebral globe and cornea. In all cases, MKC was associated with some form of skin disease, such as seborrhea sicca, acne rosacea, or seborrheic dermatitis, on its own or in combination with atopy [1••].
MGD is very frequently associated with contact lens intolerance [27••]. There are several clinical reports of an association between MGD, allergic conjunctivitis, and giant papillary conjunctivitis [30••]. Mathers and Billborough found significantly more gland dropout and greater viscosity of expressed secretions in contact lens wearers with GPC than without GPC, whereas Martin et al. [31–33] found that the severity of GPC correlated with the severity of the MGD in a consecutive series of GPC patients.
Diagnosis and Quantification of MGD Within a Specialized Ocular Surface Clinic
Clinical Tests
In the attempt to distinguish particular disorders from within another member of their larger group, diagnostic tests must differentiate not only between that particular disease and the unaffected normal state, but also between that condition and other members of the larger group of OSDs. In order to do this, there is a suitable sequence of tests to perform within a specialized ocular surface clinic for both symptomatic and asymptomatic patients with OSD. This test sequence also permits a diagnosis of symptomatic MGD, with or without ocular surface involvement. For example, lissamine green staining of the cornea and with or without aqueous dry eye based on Schirmer’s strip testing can be helpful in discerning lissamine green stain based on inflammation and less on desiccation. Grading approaches have been used to differentiate mild from severe disease and is particularly helpful to monitor relative disease states and treatment responses especially when signs and symptoms are not correlating. When the signs and symptoms do not correlate, it is imperative to document many objective signs reflecting OSD to help the clinician determine severity and progression of the disease when applying the various focused treatment regimens that are recommended.
Additionally, baseline measurements are particularly useful to help the clinician for stratification purposes in clinical trials. Moreover, when such trials are extended as in natural history studies or where meibomian gland damage occurs as an adverse event, they may provide a record of change over time. The graded scores for each test can be used to monitor the disease during treatment or may demonstrate the dynamic variation of the patient’s disease process and their response to the variety of current and future ocular surface treatment options. The diagnostic tests are as follows:
Tear Osmolarity
Tear film osmolarity indicates the balance of inputs and outputs of the lacrimal system. The osmolarity of a sample can be determined by sampling, as well as using methods that measure the colligative properties of the tears [34, 35]. The Tear Lab system is used in our clinic as a measurement for tear osmolarity in each patient. With increasing rates of evaporation from aqueous deficient dry eye, the concentration of the tear film increases as well. Tear osmolarity is graded within the ranges of mOsmls/l: normal (275–300), mild (303–310), moderate (320–335), and severe (350+).
Schirmer’s Tear Strip
The basal tear test or Schirmer’s 1 may not be a direct test of MGD; however, it is useful in the differentiation of aqueous-deficient dry eye and evaporative dry eye, both of which may occur concurrently. The basal test is done with topical anesthesia, while the Schirmer’s 1 is performed without anesthesia, reflecting the patient's reflex tear capacity. Both tests are currently used, and it is important to use the same method during each surface examination to be able to compare consecutive examinations. A drop of anesthetic, proparacaine, is placed in each of the patient's eyes to avoid discomfort from the strips. A cotton swab is used to gently blot any residual tears in the cul de sac before the strips are placed on the patient’s eyes for 5 min. The arbitrary value for dryness is set at ≤10 mm/5 min [21, 36]. While there may be a wide intrasubject, temporal, and visit-to-visit variation, repeatable scores <5 and >25 mm in basal tear measurement scores are particularly helpful in defining the extreme spectrum of aqueous production as related to lacrimal gland and accessory gland failure. Those values in between these extremes are helpful and reflect an interim stage of the disease state and only a snapshot of its possible progression.
Lissamine Green
Ocular surface damage may be quantified by grading staining of the cornea and conjunctiva by using the vital dye, lissamine green staining [37–40]. Ocular surface damage is encountered in association with MGD. Various etiologies have been proposed for such damage, including the release of inflammatory mediators into the tear film and the desiccation mechanism of evaporative dry eye. Once lissamine green has been applied, the grading is divided into three zones, the corneal and two temporal and nasal conjunctival zones. The spots present in each zone are graded on a scale of 0-3, with 0 being no staining and 3 being a large amount of lissaming green staining.
Tear Film Breakup Time
Tear film stability is measured by a test of fluorescein breakup time. This is the time to initial breakup of the tear film after a blink. It has been proposed that fluorescein breakup can be caused by quenching of fluorescence related to the increase in fluorescein concentration caused by evaporation. The classic and usual method to determine breakup time utilizes fluorescein to stain the tear film. The fluorescein is applied as a drop in the patient’s eye. After instillation, the patient is asked to blink several times and to move the eyes, to mix the fluorescein in the tears. Observation is with the slit lamp; a cobalt blue filter is slowly moved from side to side to cover the entire cornea. The patient is instructed to blink naturally and then, once homogeneous tear film fluorescence has been confirmed, to keep the eyes open while looking straight ahead. The time from upstroke of the last blink to the first tear film break or dry spot formation is recorded as the fluorescein breakup time measurement [41–43].
Ocular Surface Exam
Abnormal test results provide partial evidence of the presence of dry eye, but does not specify whether it is aqueous deficient or evaporative. Quantification of MGD is based on grading the meibum quality and expressibility, and the appearance of the glands and lid margins with direct observation or imaging adds to the assessment of the state of the ocular surface. Once the previous tests have been discussed, an ocular surface exam is performed. MGD and associated lid margin characteristics can be further assessed as follows.
-
(1)
Quantification of meibum expressibility and quality (VOT)
-
(2)
Quantification of lid margin changes (zone A and Marx’s line)
-
(3)
Chalasis
-
(4)
Meibography: quantification of gland morphology and gland dropout
Vascularity, Obstruction, Turbidity (VOT), Zone A and Conjunctivalchalasis
Vascularity
One aspect that is overlooked when conducting an ocular surface examination is the vascularity of the lower lid margin. Vascularity is graded in a range from 1 to 4. It ranges from an occasional telangiectasia, or multiple neovascular vessels, mild to a moderate number of vessels, to a florid, excessive number of vessels. The vascularity reflects the degree of chronic inflammation from the lid margin that could result from MGD or another inflammatory nidus originating from the ocular surface. It has been noted that children tend to be less vascular than adults [1••]. The increase from adolescence may be caused by aging, hormonal, and environmental factors, i.e., computer usage. In addition, increases in vascularitiy may represent a secondary immune response to offending ocular surface irritants from MGD.
Obstruction
Whether a specific meibomian gland is functional and capable of providing secretion is determined by observing the quantity and quality of secretion expressed from that gland. Since it is not possible to observe the flow of secretion from an individual gland during blinking, assessment requires expressing the meibomian gland with a physical force applied to the outer surface of the eyelid [33, 44–58]. The orifice of the gland must be observed with adequate magnification during compression to detect the outflow of meibomian gland secretion. The description of the force applied has been limited to gentle or forceful. Strain gauge types of devices have been used to standardize the amount of force. Practically, a cotton swab can be used to apply an adequate constant tolerable pressure. Despite being variably subjective, it is graded on a scale of O-4. Zero is no obstruction, then slight obstruction, moderate obstruction, and 4+ is complete obstruction. During expression, it is important to note tenderness suggesting the localized tenderness may be due to increased internal lumen pressure due to partial to complete obstruction. If this is a prominent feature, reversal of partial or complete meibomian gland obstruction may be indicated.
Turbidity
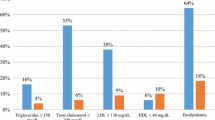
The secretory functions of the meibomian glands are assessed indirectly by compressing the tarsal plate locally in relation to individual groups of meibomian gland orifices. In normal lids, a dome of clear oil spills over the orifices with gentle compression. The quality of the expressed meibum secretion can be categorized in patients with MGD on a scale of 0-4. Zero represents clear meibum, while yellowish or globular meibum with or without epithelial debris, to more advanced moderately to severely cloudy and toothpaste-like debris representing grade 4 completes the spectrum. Moreover, reports of an association between patients with turbid oils and/or gland obstruction and high serum lipid levels have been reported by our group. When this is observed, patients are encouraged to obtain a serum cholesterol level and lipid profile before starting an omega 3 supplement, which alters absolute baseline levels.
Zone A
The avascular region approximately 0.5 mm posterior to the posterior lid margin arbitrarily called zone A is observed for the presence of telangiectasia or neovascularization with or without inflammation. These lid margin vascular alterations have been found to correlate with chronic ocular surface irritation, inflammation and suggest chronic ocular surface disease. They may be prominently present without any other ocular surface findings early in MGD and other ocular surface pathology. Observing zone A during an ocular surface exam is graded similarly to the vascularity noted on the anterior and central lid margin. A 0–4 grading is given where there can be no vessel involvement, occasional vessels, mild to moderate number of vessels, or 4+ representing a florid number of vessels. These lid margin changes may be more noticeable as one ages but can be seen more prominently when associated with contact lens wear and ocular allergies.
Conjunctivalchalasis
Conjunctivalchalasis is a common eye surface condition characterized by the presence of excess folds of the conjunctiva located between the globe of the eye and the eyelid margin. Most conjunctivochalasis is thought to be caused by both a gradual thinning and stretching of the conjunctiva that accompany age and a loss of adhesion between the conjunctiva and underlying sclera related to the dissolution of Tenon’s capsule. The resulting loose, excess conjunctiva may mechanically irritate the eye and disrupt the tear film and its outflow, leading to dry eye and excess tearing. A correlation may also exist between inflammation in the eye and conjunctivochalasis [59, 60], although it is unclear if this correlation is causal. Conjunctivochalasis may be associated with previous surgery, blepharitis, MGD, and aqueous tear deficiency and paradoxically epiphora.
Meibography: Qualitative and Quantitative Measurements of the Meibomian Gland Morphology and Gland Loss
Meibomian gland dropout implies partial or total gland loss or atrophy and can be quantified by meibography [1••]. Meibography is an imaging technique that provides information on the morphological characteristics of meibomian glands (MGs) and is based on observation of the gland silhouette on retroillumination of the everted eyelid from the skin side [61–64]. We recently developed a noncontact infrared meibography system that allows for observation of MG structure with no discomfort to the patient [4]. Whereas conventional meibography is difficult to apply to the upper eyelid, noncontact meibography allows for observation of both the upper and lower eyelids [4]. More recently, Pult and Riede-Pult described a portable noncontact meibography system based on an infrared charge-coupled device (CCD) video camera [4], and we developed a mobile pen-shaped meibography device with an infrared light-emitting diode [65]. Instruments for noncontact meibography are now commercially available in several countries and include the BG-4 M for the slit lamp (Topcon, Tokyo, Japan), which is based on an infrared illumination system with an external infrared CCD camera; the Meibom Pen (Japan Focus Corp., Tokyo, Japan), which is a mobile pen-shaped meibography device; the Eye Top Topographer, Sirius Scheimpflug Camera, and Cobra Fundus Camera (CSO, Florence, Italy); and bon Optic Verttieb gmbH, Lübeck, Germany); and the Keratograph 5M (Oculus, Wetzlar, Germany). Such noncontact meibography systems have been shown to detect morphological changes such as dropout, shortening, dilation, and distortion of MGs in patients with MGD.
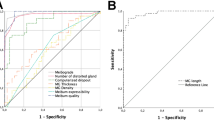
We have compared the results obtained with various MG examination techniques, including the lost area of MGs (meiboscore, see below) as determined by noncontact meibography as well as ocular symptoms, lid margin abnormalities, corneal staining, tear film breakup time, meibum grade, and Schirmer’s test findings between patients with obstructive MGD and normal control subjects. Receiver-operating characteristic (ROC) curves were constructed to determine the ability of each parameter to differentiate eyes with obstructive MGD from normal eyes. The area under the curve values indicated that the ocular symptom score had the highest diagnostic power as a single parameter, followed by the lid margin abnormality score, meiboscore, and tear film breakup time. On the basis of these findings, we recommend that physicians use the ocular symptom score, lid margin abnormality score, and meiboscore to diagnose MGD. Obstructive MGD should be suspected when any two of these three scores are abnormal, and it is highly likely when all three scores are abnormal. The ability to detect detailed changes of MGs with noninvasive meibography thus increases the likelihood of a correct diagnosis for patients with MGD and therefore allows for implementation of the most effective treatment as well as for evaluation of the effect of such treatment [66].
Equipment for Noncontact Meibography
The Topcon BG-4 meibography system comprises a slit lamp (BG-4M, Topcon) equipped with an infrared transmitting filter (IR-83; Hoya, Tokyo, Japan) and an infrared CCD video camera (XC-EI50; Sony, Tokyo, Japan) (Fig. 1). A transilluminating light probe is not required. Given that the infrared transmitting filter is included as one of the rotating filters of the slit lamp, meibography can be performed with the same slit lamp used for routine examinations.
Meiboscore
Partial or complete loss of MGs is scored for each eyelid from grade 0 (no loss) to grade 3 (lost area constituting more than two-thirds of the total gland area) (Fig. 2). Meiboscores for the upper and lower eyelids are summed to obtain a total score from 0 to 6 for each eye.
The grading of meibomian gland loss (Meibo-score). Partial or complete loss of MGs is scored for each eyelid from grade 0 to grade 3. Grade 0 means no loss of meibomian glands (a). Grade 1 means the lost area was less than 1/3 of total area (b). Grade 2 means the lost area was between 1/3 and 2/3 of total area (c). Grade 3 means the lost area was more than 2/3 of total area (d)
Development of software for automated quantitative analysis of the MG area
Several studies have described subjective grading of the area of MG loss [4, 61, 67]. A method for objective grading would be more useful, however, for evaluation of the subtle morphological changes of MGs. More recent studies have analyzed images of MGs with Image J software [4, 68–72]. With Image J, however, the user must manually define the gland region for each patient, and different examiners may draw the gland region differently, leading to interobserver variability. Koh et al. [73] described the automatic analysis of MG images with the use of original algorithms to identify the glands. They demonstrated a clear distinction between normal and abnormal glands based on both mean arc length and mean entropy for the upper eyelids. Their method provides such parameters as the central length of the detected MGs and the size of spaces between neighboring glands, which are not necessarily associated with MGD. In our newly developed method [74], the measurement area is automatically defined, and the contours of each MG in the upper and lower eyelids are analyzed. This approach is likely to be advantageous for detection of local and subtle changes of MGs because it specifies the outline of the gland itself and not the MG area (Fig. 3). We found that the ratio of the MG area to the total area decreased significantly as the meiboscore increased. Our results thus show a good correlation between subjective grading and objective measurements of the MG area [74].
The quantitative analysis of meibomian gland area. a Original image. b The software compensated for the inhomogeneous illumination on the image by applying a top hat filter, and calculated the threshold value based on the average illumination level of the compensated image. Next, it specified the parts of the total analysis area that met the conditions of the threshold value after the area segmentation process. c After shading correction of the illumination of the whole image, the image was binarized so that the meibomian gland and non-meibomian gland areas could be easily separated by applying the Fourier transformation, γ correction, and gauss filter. d After the binarized meibomian glands were separated as independent closed curves, the software labeled each meibomian gland and calculated the area of the closed meibomian glands. Lastly, it calculated the ratio of the total meibomian gland area (closed cyan line) relative to the total analysis area (yellow) (Color figure online)
In conclusion, the relation of the MG area to the total analysis area can now be objectively analyzed with newly developed software. Such an approach should prove useful for characterization of the extent of MGD and for objective evaluation of the effect of treatment in patients with this condition [75].
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
•• Tomlinson A, Bron AJ, Korb DR, et al. The international workshop on meibomian gland dysfunction: report of the diagnosis subcommittee. 2011;2006–2039.
Foulks G, Bron AJ. A clinical description of meibomian gland dysfunction. Ocul Surf. 2003;1:107–26.
Kozak I, Bron AJ, Kucharova K, et al. Morphologic and volumetric studies of the meibomian glands in elderly human eyelids. Cornea. 2007;26:610–4.
Arita R, Itoh K, Inoue K, Amano S. Noncontact infrared meibography to document age-related changes of the Meibomian glands in a normal population. Ophthalmology. 2008;115:911–5.
Nicolaides N, Kaitaranta JK, Rawdah TN, Macy JI, Boswell FM 3rd, Smith RE. Meibomian gland studies: comparison of steer and human lipids. Invest Ophthalmol Vis Sci. 1981;20:522–36.
Chew CKS, Hykin PG, Jansweijer C, Dikstein S, Tiffany JM, Bron AJ. The casual level of meibomian lipids in humans. Curr Eye Res. 1993;12:255–9.
Yokoi N, Mossa F, Tiffany JM, Bron AJ. Assessment of meibomian gland function in dry eye using meibometry. Arch Ophthalmol. 1999;117:723–9.
Yokoi N, Bron AJ, Tiffany J, et al. Reflective meniscometry: a non-invasive method to measure tear meniscus curvature. Br J Ophthalmol. 1999;83:92–7.
Blackie CA, Korb DR. Recovery time of an optimally secreting meibomian gland. Cornea. 2009;28:293–7.
Blackie CA, Korb DR. The diurnal secretory characteristics in individual meibomian glands. Cornea. 2009;29:34–8.
Bron AJ, Tiffany JM. The evolution of lid margin changes in blepharitis. In: Lass JH, editor. Advances in corneal research: selected transactions of the World Congress on the Cornea IV. New York: Plenum; 1997. p. 3–18.
Obata H. Anatomy and histopathology of human meibomian gland. Cornea. 2002;21(7 Suppl):S70–4.
Matsumoto Y, Sato EA, Ibrahim OM, et al. The application of confocal microscopy to the diagnosis and evaluation of meibomian gland dysfunction. Mol Vis. 2008;14:1263–71.
McDonald JE. Surface phenomena of the tear film. Am J Ophthalmol. 1969;67:56–64.
Rolando M, Valente C, Barabino S. New test to quantify lipid layer behavior in healthy subjects and patients with keratoconjunctivitis sicca. Cornea. 2008;27(8):866–70.
Lemp MA. Report of the National Eye Institute/Industry Workshop on Clinical Trials in Dry Eyes. CLAO J. 1995;21:221–31.
DEWS. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop. Ocul Surf. 2007;5:75–92.
Korb DR, Henriquez AS. Meibomian gland dysfunction and contact lens intolerance. J Am Optom Assoc. 1980;51(3):243–51.
Korb DR, Blackie CA. Diagnostic versus therapeutic meibomian gland expression (abstract). Orlando: American Academy of Optometry annual meeting; 2009.
Goto E, Shimazaki J, Monden Y, et al. Low-concentration homogenized castor oil eye drops for noninflamed obstructive meibomian gland dysfunction. Ophthalmology. 2002;109(11):2030–5.
DEWS. Methodologies to diagnose and monitor dry eye disease: report of the diagnostic methodology subcommittee of the international dry eye workshop. Ocul Surf. 2007;5:108–52.
Behrens A, Doyle JJ, Stern L, et al. Dysfunctional tear syndrome: a Delphi approach to treatment recommendations. Cornea. 2006;25:900–7.
Goto E, Endo K, Suzuki A, et al. Tear evaporation dynamics in normal subjects and subjects with obstructive meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2003;44:533–9.
Yokoi N. Tear dynamics and dry eye. Nippon Ganka Gakkai Zasshi. 2004;108:275–6.
Yokoi N, Yamada H, Mizukusa Y, et al. Rheology of tear film lipid layer spread in normal and aqueous tear-deficient dry eyes. Invest Ophthalmol Vis Sci. 2008;49:5319–24.
Yokoi N, Komuro A. Non-invasive methods of assessing the tear film. Exp Eye Res. 2004;78(3):399–407.
•• Arita R, Itoh K, Inoue K, Kuchiba A, Yamaguchi T, Amano S. Contact lense wear is associated with decrease of meibomian glands. Ophthalmology. 2009;116(3):379–84.
McCulley JP, Sciallis GF. Meibomian keratoconjunctivitis. Am J Ophthalmol. 1977;84(6):788–93.
McCulley JP, Dougherty JM, Deneau DG. Classification of chronic blepharitis. Ophthalmology. 1982;89(10):1173–80.
•• Arita R, Itoh K, Maeda S, et al. Meibomian gland duct distortion in patients with perennial allergic conjunctivitis. Cornea. 2010;29(8):858–60.
Mathers WD, Billborough M. Meibomian gland function and giant papillary conjunctivitis. Am J Ophthalmol. 1992;114:188–92.
Martin NF, Rubinfeld RS, Malley JD, Manzitti JD. Giant papillary conjunctivitis and meibomian gland dysfunction blepharitis. CLAO J. 1992;18:165–9.
Ong BL, Larke JR. Meibomian gland dysfunction: some clinical, biochemical and physical observations. Ophthalmic Physiol Opt. 1990;10:144–8.
Tomlinson A, McCann LC, Pearce EI. Comparison of human tear film osmolarity measured by electrical impedance and freezing point depression techniques. Cornea. 2010;9:1036–41.
Tomlinson A, Khanal S, Ramaesh K, et al. Tear film osmolarity: determination of a referent for dry eye diagnosis. Invest Ophthalmol Vis Sci. 2006;47(10):4309–15.
Khanal S, Tomlinson A, McFadyen A, Diaper C, Ramaesh K. Dry eye diagnosis. Invest Ophthalmol Vis Sci. 2008;49:1407–14.
Marx E. Uber vitale Farbung des Auges und der Augenlieder. I. Uber Anatomie, Physiologie und Pathologie des Augenlidrandes under der Tranenpunkte. Graefes Arch Clin Exp Ophthalmol. 1924;114:465–82.
Marx E. Uber vitale Farbung des Auges und der Augenlieder. I. Uber Anatomie, Physiologie und Pathologie des Augenlidrandes under der Tranenpunkte. Graefes Arch Clin Exp Ophthalmol. 1926;116:114–25.
Doughty MJ, Naase T, Donald C, Hamilton L, Button NF. Visualization of “Marx’s line” along the marginal eyelid conjunctiva of human subjects with lissamine green dye. Ophthalmic Physiol Opt. 2004;24:1–7.
Hughes C, Hamilton L, Doughty MJ. A quantitative assessment of the location and width of Marx’s line along the marginal zone of the human eyelid. Optom Vis Sci. 2003;80:564–72.
Korb DR. Survey of preferred tests for diagnosis of the tear film and dry eye. Cornea. 2000;19:483–6.
Lemp MA, Hamill JR. Factors affecting tear film break-up in normal eyes. Arch Ophthalmol. 1973;89:103–5.
Norn MS. Desiccantion of the precorneal tear film. I. Corneal wetting time. Acta Ophthalmol (Copenh). 1969;47:865–80.
Craig JP, Blades K, Patel S. Tear lipid layer structure and stability following expression of the meibomian glands. Ophthalmic Physiol Opt. 1995;15:569–74.
Gifford SR. Meibomian glands in chronic blepharoconjunctivitis. Am J Ophthalmol. 1921;4:489–94.
Korb DR, Henriquez AS. Meibomian gland dysfunction and contact lens intolerance. J Am Optom Assoc. 1980;51:243–51.
Norn MS. Expressibility of meibomian secretion: relation to age, lipid precorneal film, scales, foam, hair and pigmentation. Acta Ophthalmol. 1987;65:137–42.
Hom MM, Silverman MW. Displacement technique and meibomian gland expression. J Am Optom Assoc. 1987;58:223–6.
Hom MM, Martinson JR, Knapp LL, et al. Prevalence of meibomian gland dysfunction. Optom Vis Sci. 1990;67:710–2.
Bron AJ, Benjamin L, Snibson GR. Meibomian gland disease: classification and grading of eyelid changes. Eye. 1991;5:395–411.
Driver PJ, Lemp MA. Meibomian gland dysfunction. Surv Ophthalmol. 1996;40:343–67.
Goto E, Monden Y, Takano Y, et al. Treatment of non-inflamed obstructive meibomian gland dysfunction by an infrared warm compression device. Br J Ophthalmol. 2002;86:1403–7.
Goto E, Shimazaki J, Monden Y, et al. Low-concentration homogenized castor oil eye drops for noninflamed obstructive meibomian gland dysfunction. Ophthalmology. 2002;109:2030–5.
Romero JM, Biser SA, Perry HD, et al. Conservative treatment of meibomian gland dysfunction. Eye Contact Lens. 2004;30:14–9.
Korb DR, Greiner JV. Increase in tear film lipid layer thickness following treatment of meibomian gland expression. In: Sullivan DA, Stern ME, Tsubota K, et al., editors. Lacrimal gland, tear film, and dry eye syndromes. New York: Plenum; 1994. p. 293–8.
Foulks GN. Blepharitis: lid margin disease and the ocular surface. In: Holland EJ, Mannis MJ, editors. Ocular surface disease: medical and surgical management. New York: Springer; 2002. p. 39–48.
Mastrota KM. The meibomian Mastrota paddle. Rosenberg: Cynacon/Ocusoft; 2002.
Mathers WD, Shields WJ, Sachdev MS, et al. Meibomian gland dysfunction in chronic blepharitis. Cornea. 1991;10(4):277–85.
Yamaguchi M, Kutsuna M, Uno T, et al. Marx line: fluorescein staining line on the inner lid as indicator of meibomian gland function. Am J Ophthalmol. 2006;141:669–75.
Hughes WL. Conjunctivochalasis. Am J Ophthalmol. 1942;25:48–51.
Nichols JJ, Berntsen DA, Mitchell GL, et al. An assessment of grading scales for meibography images. Cornea. 2005;24:382–8.
Mathers WD, Daley T, Verdick R. Video imaging of the meibomian gland. Arch Ophthalmol. 1994;112:448–9.
Robin JB, Jester JV, Nobe J, et al. In vivo transillumination biomicroscopy and photography of meibomian gland dysfunction. A clinical study. Ophthalmology. 1985;92:1423–6.
Yokoi N, Komuro A, Yamada H, et al. A newly developed video meibography system featuring a newly designed probe. Jpn J Ophthalmol. 2007;51:53–6.
PultH Riede-PultBH. Non-contact meibography: keep it simple but effective. Cont Lens Anterior Eye. 2012;35:77–80.
Arita R, Itoh K, Maeda S, et al. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology. 2009;116:2058–63.
Pflugfelder SC, Tseng SC, Sanabria O, et al. Evaluation of subjective assessments and objective diagnostic tests for diagnosing tear-film disorders known to cause ocular irritation. Cornea. 1998;17:38–56.
Pult H, Riede-Pult B. Comparison of subjective grading and objective assessment in meibography. Cont Lens Anterior Eye. 2013;36:22–7.
Pult H, Nichols JJ. A review of meibography. Optom Vis Sci. 2012;89:E760–9.
Srinivasan S, Menzies K, Sorbara L, et al. Infrared imaging of meibomian gland structure using a novel keratograph. Optom Vis Sci. 2012;89:788–94.
Pult H, Riede-Pult BH, Nichols JJ. Relation between upper and lower lids’ meibomian gland morphology, tear film, and dry eye. Optom Vis Sci. 2012;89:E310–5.
Ban Y, Shimazaki-Den S, Tsubota K, Shimazaki J. Morphological evaluation of meibomian glands using noncontact infrared meibography. Ocul Surf. 2013;11:47–53.
Koh YW, Celik T, Lee HK, et al. Detection of meibomian glands and classification of meibography images. J Biomed Opt. 2012;17:086008. doi:10.1117/1.JBO.17.8.086008.
Arita R, Suehiro J, Haraguchi T, Shirakawa R, Tokoro H, Amano S. Objective image analysis of the meibomian gland area. Br J Ophthalmol. 2013;. doi:10.1136/bjophthalmol-2012-303014.
Arita R, Suehiro J, Haraguchi T, et al. Topical diquafosol for patients with obstructive meibomian gland dysfunction. Br J Ophthalmol. 2013;97:725–9.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclosure
Richard Yee has reported no conflicts of interest. Dr. Arita has a patent 5281846 non-contact meibography licensed.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arita, R., Zavala, M. & Yee, R.W. MGD Diagnosis. Curr Ophthalmol Rep 2, 49–57 (2014). https://doi.org/10.1007/s40135-014-0041-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40135-014-0041-9