Abstract
There is increasing awareness of the radiation dose delivered to patients using computed tomography (CT). It is important to properly manage the radiation dose when performing CT colonography (CTC) for colorectal cancer screening since the test may be repeated several times over the lifetime of the individual. There must be a balance of the overall benefit of screening CTC versus any theoretical risk of radiation. Technically there must also be a balance of radiation dose with image quality. Efforts continue to lower the radiation dose as much as possible while maintaining diagnostic accuracy for CTC in conjunction with overall national efforts by professional organizations, providers of medical imaging services, and equipment manufacturers. This article reviews the strategies that may be used to reduce the radiation dose for CTC including practical methods, modifications of specific CT parameters, and the use of new iterative reconstruction techniques.
Similar content being viewed by others
Introduction
Clinical use of computed tomography (CT) scans initially occurred in the 1970s, and since then significant technological evolution has helped propel the widespread usage of CT for medical imaging. When CT is employed as a screening test, there is a focus on balancing the benefit of early cancer detection and the theoretical risk of screening-induced malignancy. The theoretical risks associated with patient exposure to radiation from medical imaging have become a major topic of debate. Controversy exists regarding the linear, no-threshold model for estimating health effects from radiation since it assumes that any radiation dose, no matter how small, may be carcinogenic. According to this model, detrimental health effects are also thought to occur in direct proportion to the dose received. However, although high doses of radiation above 50–100 millisieverts (mSv) have been shown to induce cancer, the risks of low radiation dose tests such as CT colonography (CTC) have not been definitively demonstrated or may not even exist. The position statement of the Health Physics Society [1] was updated in 2010 and recommends against quantitative estimation of health risks below an individual dose of 50 mSv in 1 year or a lifetime dose of 100 mSv above that received from natural sources. Similarly, in 2011, the American Association of Physicists in Medicine [2] policy update stated that predictions of hypothetical cancer incidence and deaths in patient populations exposed to such low doses (of 50–100 mSv) are highly speculative and should be discouraged.
Screening CTC is currently recommended to be repeated every 5 years according to the joint guidelines of the American Cancer Society, the US Multi-Society Task Force, and the American College of Radiology [3•]. In practicing the ALARA (as low as reasonably achievable) approach for radiation dose minimization, significant reduction in dose is now obtainable. Employing the dose reduction strategies for CTC outlined in this article, the effective radiation dose of CTC approximates 3 mSv or lower, which is similar to or less than the annual natural background radiation dose in the US (Table 1) [1, 4•, 5].
Easily instituted practical tips are provided to help decrease radiation dose for CTC including proper patient positioning and assuring that patients are adequately prepared in order to avoid additional repeat scanning. Currently available techniques to decrease the radiation dose include lowering the tube current or tube voltage as well as the use of automatic tube current modulation and an iterative reconstruction technique.
Background
A commonly employed technique to reduce CT radiation dose is tube current reduction. This has been applied successfully to CTC in prior studies [6, 7]. Cohnen et al. [6] performed CTC in 137 patients using 10 mA in the supine position only, resulting in an effective dose of approximately 1 mSv. After mathematic noise reduction, 82 % of polyps larger than 5 mm were detected. Similarly, Iannaccone et al. [7] evaluated 88 patients undergoing CTC with 10 mA and found that CTC compared favorably with colonoscopy. Sensitivities for detection of polyps 6 mm in diameter or larger were 86 and 84 % for CTC and colonoscopy, respectively. More recently, tube current reduction has been combined with the iterative reconstruction technique. Flicek et al. [4•] performed CTC using standard 50 mA in the supine position and a lowered tube current of 25 mA combined with a 40 % adaptive statistical iterative reconstruction (ASIR) technique in the prone position. Results showed a dose reduction for CTC of 50 % below standard technique without significantly affecting image quality when ASIR is used.
Substantial dose reduction can be achieved by lowering the tube voltage for CTC. Chang et al. [8•] evaluated the effect of decreasing tube voltage from 120 to 100 kVp (peak kilovoltage) for CTC. A 20 % decrease in the volumetric CT dose index (CTDIvol) and 16 % decrease in the dose-length product (DLP) were demonstrated, but only a minimal decrease in three-dimensional (3D) image quality. Lowering the tube voltage was also found to increase the attenuation of tagged fluid by an average of 92 HU. This should be helpful for CTC when tagging is employed since increasing tagged fluid attenuation can improve the conspicuity of submerged polyps. Note is made that the low kVp technique may not be appropriate in large patients since there is significant attenuation of the photon beam resulting in noisy images that may be non-diagnostic.
In the large National CTC Trial by The American College of Radiology Imaging Network (ACRIN), CTC was performed in 2,531 asymptomatic patients using a protocol consisting of 50 mA and 120 kVp, which was a relatively lower dose compared to older techniques where 100–150 mA was employed [9•]. The per-patient sensitivity and specificity for large adenomas and cancers were 90 and 86 %, respectively. Another screening CTC trial evaluating the low-dose technique was performed in 307 asymptomatic, average-risk screening patients [10]. The average effective dose to patients was 4.5 mSv with high per-polyp sensitivity and specificity for detection of polyps 6 mm or larger of 91 and 93 %, respectively, and for polyps 9 mm or larger of 91 and 98 %, respectively.
Favorable results were found for CTC in a study by Berrington de González et al. [11•] determining the benefit-to-risk ratio comparing the potential lives saved using screening CTC to the potential deaths caused by fatal cancers induced by radiation from the test. Radiation dose levels from the ACRIN National CT Colonography Study were used for modeling and assumed that CTC screening is performed every 5 years between the ages 50 and 80. Additionally potential radiation risk due to the imaging workup of extracolonic findings was also included in the analysis. All three microsimulation models for colorectal cancer development that were employed demonstrated a large benefit-to-risk ratio in favor of screening CTC, ranging from 24:1 to 35:1. These results are similar to findings reported by Brenner and Georgsson [12] who determined that the benefit-to-risk ratio for CTC was high and that induced cancers were rare even when taking into consideration the controversial linear no-threshold model. It was found that the potential lifetime cancer risk for one CTC exam at age 50 was low at 0.14 %. At age 70 this risk decreased to 0.07 %. Using optimized low-dose CTC protocols, these values could be further lowered by factors of 5 or 10.
Radiation Dose Metrics
Modern CT scanners display two metrics that are often used to estimate the radiation dose. Although these metrics do not measure the dose the patient absorbs, they quantify the radiation dose to which a patient is exposed. The CTDIvol is reported in units of milligray (mGy) and represents the dose within the scanned volume from a particular scan protocol for a standardized phantom [13]. It is a measure of scanner output and not a direct measure of patient dose. The DLP is reported in units of mGy centimeter (mGy cm) and represents the CTDIvol multiplied by the scan length. This allows calculation of the applied radiation dose to a scanned volume and extends the CTDIvol from a single rotation to the entire scanned volume [14].
CTDIvol and DLP are displayed on the consoles of all modern CT scanners after the technologist has performed the localizer scans, but before the start of the CTC scan series. They are then displayed again following scan completion, although if automated tube current modulation has been employed, the end values for CTDIvol and DLP may be different from those initially displayed. Standard CTC examinations include scans in the supine and prone positions. Therefore, a CTC dose report should include the CTDIvol and DLP from each of these two series (Fig. 1). The sum of the DLP from each series should then be converted to an estimated effective dose, which is reported in mSv. This is accomplished by multiplying the total DLP by a conversion factor (k), which is determined by the size of the patient and the region of the body scanned. A conversion factor of 0.015 is multiplied by the total DLP to obtain the effective dose for CTC [15]. When dose reduction techniques have been applied such as decreasing the tube current from 50 mA in the supine position to 25 mA in the prone position, the effective dose of CTC approximates 3 mSv or less [4•]. A Sub-mSv effective dose for CTC can be obtained using more aggressive reduction of the tube current combined with other described strategies.
Practical Methods of Radiation Dose Reduction
There are several practical methods that can help reduce the overall radiation dose without changing CTC protocols or CT scanner options. Ideal patient positioning within the CT gantry improves image quality and allows for optimum use of automatic dose modulation. Positioning a patient too high or too low relative to the center of the CT gantry can result in an inaccurate estimation of the amount of radiation dose needed. A study evaluating the impact of suboptimal centering on the patient dose and image noise found that for a 64-slice CT scanner with a 2.2-cm miscentering below the isocenter on scout scans, there was on average an increase of 23 % in patient dose and an increase of 7 % in image noise [16]. Optimal positioning is typically achieved by use of laser guides that the technologist uses to place the patient in the isocenter of the scanner gantry in both the superior-inferior and lateral directions. The use of automatic patient-centering software to more precisely center patients off of a localizer over the specific body range being scanned has been shown to be capable of reducing the surface dose by up to 30 % [17].
In some patients, it may be necessary to perform a third scan, usually in the decubitus position, to better distend a poorly distended or collapsed colonic segment. This additional scan can add substantially to the total radiation exposure. Optimizing colonic distention on routine supine and prone views is therefore critical to reduce the necessity of additional positions. An automatic carbon dioxide insufflator, when used properly, has been shown to optimize distention more than hand insufflation [18]. Routine evacuation in between positions can help prevent “fluid blocks,” which may prevent adequate insufflation [5]. In the situation where additional scans are required, at the least, limiting the coverage to the colonic area of interest should be considered. Furthermore, for screening CTC examinations, when coverage for the scan volume is being determined, the included area should be limited to the top of the colon and need not be extended to the diaphragm unless necessary as for routine CT abdomen protocols. Coverage should include the superior aspect of the highest colonic flexure to the level of the anus. Radiation dose reduction can also be achieved with the use of dynamic Z-axis collimation, which can limit unnecessary radiation due to over-scanning at the superior and inferior margins of the scan volume [5, 19]. This increase in dose with multidetector CT is related to the need to scan a slightly larger volume (i.e., over-scanning) in order to interpolate data to reconstruct the first and last slice.
Modification of image viewing at the workstation can help to offset the resulting noisier images. The use of thicker reconstructions can be helpful for evaluating extracolonic findings or soft tissue structures on lower dose, noisier images. Technologists can be instructed to automatically send thicker reconstructions to a viewing workstation or the reader can create thicker slices at the 3D workstation. The use of relatively wider window settings and noise reduction filters applied at the post-processing level can also be useful to decrease image noise at the workstation [5]. Selective patient shielding of more radiation-sensitive tissues during CT is available but not widely used at this time because of the increase in noise and artifacts that accompany the modest reduction in organ dose [20].
Tube Current Reduction
Tube current is one of the main CT parameters that can be adjusted to reduce the radiation dose. A decrease in the dose can be achieved with a proportional decrease in mA given the direct linear relationship. As mA is decreased, however, image noise is increased by a factor of 1/(square root of mA). A larger amount of noise can be acceptable with CTC since we are focusing predominantly on the inherent high contrast between intraluminal air and the soft tissue density of the colon mucosal boundary. However, the the visualization of extracolonic findings can be compromised with decreasing dose, although images can be reconstructed to thicker slices if the level of noise renders the image uninterpretable. This can be performed by either routine reconstructions using thicker slices or thick slab maximum intensity projections [5]. With excessive dose reduction and the resultant concurrent increase in image noise, however, the 3D endoluminal images may be degraded by an increase in colon wall “nodularity” [5]. This image degradation on the 3D images can also impact the performance of CAD in polyp detection. Studies have shown that CTC examinations using extra low tube currents can still maintain interpretable imaging quality for the detection of polyps, even with tube currents as low as 10 mA [7, 21]. A more recent study found dose reductions of 40 and 70 % could be achieved for overweight and normal patients, respectively, by the use of a body mass index-adjusted dose reduction approach with tube current [22].
Automatic Dose Modulation
A more judicious method of reducing radiation dose rather than simply reducing tube current for an entire scan relies on the modulation of tube current tailored to each projection around a patient’s body. Attenuation of the rotating CT X-ray beam varies significantly depending on slice location in the craniocaudal axis of the patient. For example, X-ray attenuation is lower in gas-filled portions of the body such as the lung bases and higher in the pelvis where there are more osseous structures to penetrate. Similarly, as the human torso is generally wider in the lateral dimension than the AP dimension with lateral projections contributing most of the perceived noise to an image, tube current can be significantly reduced in AP projections compared to lateral projections without impact on image quality [23, 24]. As such, tube current can also be dynamically varied in the angular plane. Both methods combined result in an X-Y-Z axis or 3D automatic dose modulation, also known as automatic exposure control, the approach now taken by most current CT vendors and known by several trade names such as Smart mA, CARE Dose, D-DOM/Z-DOM, and SureExposure. These approaches typically predict the amount of dose modulation to utilize throughout a scan on the attenuation information gleaned from the initial AP and lateral CT scout images. Each vendor takes a slightly different approach to titrating how much dose modulation to utilize, often based upon the amount of image noise the interpreting radiologist is willing to tolerate for each exam type. For CTC in particular, the amount of allowable image noise, and thus the potential dose savings that can be realized using automatic dose modulation, can be much higher than in most other CT exams.
Another factor particular to CTC is the effect fecal and fluid tagging agents such as barium and diatrizoate have on automatic dose modulation algorithms. While these hyperdense agents can theoretically increase the predicted tube current necessary to generate images for a particular level of image noise, previous studies have noted that their use did not in fact result in significant changes in radiation dose [25]. However, it was noted that at decreased dose, beam-hardening artifacts could reduce the measured attenuation of polyps submerged in tagged fluid.
While tube current modulation works well for the great majority of patients, results may be suboptimal for those at the very extremes of patient size (the very large and the very small) as larger patients may end up receiving higher tube currents and higher doses than necessary while smaller patients may end up receiving too low a dose and overly noisy images [26]. This can be prevented by setting a minimum and maximum mA range (for example, we use a minimum of 50 mA and a maximum of 450 mA).
An alternative approach to spatial tube current modulation is the variation in tube current based on X-ray tube direction relative to organs with higher sensitivity to radiation. For example, the tube current can be reduced anteriorly where radiosensitive organs such as the breast, thyroid, and ocular lens are closest to the skin surface accompanied by a compensatory increase posteriorly to result in a similar amount of image noise [27]. The use of bismuth shields over the breast, neck, or eyes to attenuate anterior X-rays accomplishes a similar goal although at a potential cost of streak artifacts in the underlying superficial soft tissues [28, 29]. However, the use of these techniques in the abdomen or pelvis may not result in as significant a reduction in patient dose as in the chest or head.
Tube Voltage Reduction
While there is a linear relationship between tube current and radiation dose, the relationship becomes more exponential with tube voltage. Dose theoretically decreases by a power of 2.6 with a reduction in kVp [30]. This makes kVp reduction a particularly powerful way to decrease the dose, although at the cost of an increase in image noise. Despite an increase in image noise, a reduction in kVp is analogous to imaging closer to the K-edge of iodine resulting in an increase in the attenuation of iodinated contrast agents including tagged fluid in CTC [8•, 31]. Thus, when considering contrast-to-noise ratios (CNRs), the increase in tagged fluid attenuation offsets the increase in image noise resulting in no net change in CNR, a result reached in several similar studies of CT angiography [8•]. This should serve to preserve the conspicuity of submerged polyps and improve the efficiency of fluid tagging.
The effects of kVp reduction become more pronounced as the patient body habitus increases, however, potentially resulting in images with inordinate image noise in larger individuals [32]. If automatic dose modulation is utilized, tube current may be automatically increased to counteract the increase in image noise leading to a reduction or even potential increase in the overall radiation dose. A variety of approaches can be employed to deal with this by tailoring kVp selection to patient size or weight, reserving tube voltage reduction for average size and smaller patients while maintaining or even increasing tube voltage for larger patients. The selection of kVp is automated on some scanners, while on others, a weight-based or size-based algorithm may be used.
While most of the above approaches come at a cost of an increase in image noise, iterative reconstruction promises to play a synergistic role in countering these effects by using alternative reconstruction algorithms to significantly reduce image noise and allow for even more aggressive reductions in radiation dose.
Iterative Reconstruction
Filtered back projection (FBP) has been the most commonly employed reconstruction algorithm for CT data since the first clinical use of CT scanners in the 1970s. FBP is a robust reconstruction tool that is relatively simple computationally and has the advantage of rapid image reconstruction. However, filters tend to enhance the noise of an image, and this is particularly problematic in very large patients and on lower dose images. With improved and faster computer technology, iterative reconstruction algorithms have been introduced for CT scanners that allow a reduction in radiation dose in conjunction with decreased noise levels.
Iterative reconstruction techniques employ mathematical models that may be raw-data-based iterations and/or image-based iterations. Various manufacturers have developed different versions of iterative reconstruction including Sinogram Affirmed Iterative Reconstruction by Siemens Healthcare, ASIR by General Electric Healthcare, adaptive iterative dose reduction 3D by Toshiba Medical Systems, and iDose by Phillips Healthcare. These algorithms can achieve up to 50 % dose reduction and are typically hybrid techniques that include a blend of iterative reconstruction data with FBP data [4•, 33]. Iterative Reconstruction in Image Space is a variation of iterative reconstruction by Siemens Healthcare that is based on image data only. Additional novel iterative reconstruction techniques are being released such as model-based iterative reconstruction (MBIR) by General Electric Healthcare, which is considered a pure iterative reconstruction algorithm that does not require blending with FBP and can achieve up to 80 % dose reduction. Significant computing power is still needed for MBIR, and reconstruction times are longer, taking approximately 20 min per case [14].
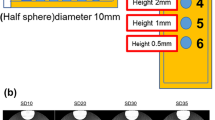
CTC images obtained using radiation dose-lowering techniques such as those acquired with an effective mA <50 may demonstrate decreased quality [4•]. Two-dimensional images can appear noisy, which can affect the appearance of both colonic and extracolonic findings. On 3D images the colonic surface may demonstrate nodularity and intraluminal artifacts. The application of iterative reconstruction can improve image quality by decreasing image noise on 2D images and by smoothing the wall on 3D endoluminal images (Fig. 2).
CT colonography using iterative reconstruction. Axial 2D (a–d) and 3D (e–h) images of a 7-mm polyp on a fold in the ascending colon (white arrows). Axial 2D supine (a, c at 100 mA) and axial prone (b, d at 50 mA) with 0 % ASIR (a, b) and 40 % ASIR (c, d). d Endoluminal displays of supine (e, g at 100 mA) and prone (f, h at 50 mA) with 0 % ASIR (e, f) and 40 % ASIR (g, h). Note that on the lower dose (50 mA) prone scans (f, h), there is subtle increased background nodularity
Conclusion
Various technical and practical strategies have been evaluated to decrease the radiation dose without compromising diagnostic image quality. The radiation dose should be kept as low as reasonably achievable (ALARA) while maintaining diagnostic image quality. Radiologists should be familiar with the various dose reduction options available to them and their particular scanner, while being mindful of the tradeoff with an increase in noise. Fortunately, CTC images can tolerate a higher level of noise than for routine abdominal CT examinations. Combined with noise reduction techniques, practical strategies for reducing noise at the post-processing level and at the PACS workstation allow for improvement in interpreting extracolonic findings on lower dose exams without compromising the detection of relevant colonic polyps.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Health Physics Society. Radiation risk in perspective. Position Statement of the Health Physics Society 2010. http://hps.org/documents/risk_ps010-2.pdf. Accessed 13 May 2013.
American Association of Physicists in Medicine. Position Statement on Radiation Risks from Medical Imaging Procedures 2011. http://aapm.org/org/policies/details.asp?id=318&type=PP. Accessed 13 May 2013.
• Levin B, Lieberman DA, McFarland B, et al.; American Cancer Society Colorectal Cancer Advisory Group; US Multi-Society Task Force; American College of Radiology Colon Cancer Committee. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008;58:130–60. This is a landmark joint guideline from multiple societies endorsing CT colonography as a valid screening test for colorectal cancer to be performed every 5 years.
• Flicek KT, Hara AK, Silva AC, Wu Q, Peter MB, Johnson CD. Reducing the radiation dose for CT colonography using adaptive statistical iterative reconstruction: a pilot study. Am J Roentgenol. 2010;195:126–31. This is the initial study performed demonstrating the successful application of the iterative reconstruction technique to CT colonography in both phantoms and patients resulting in significant radiation dose reduction.
Chang KJ, Yee J. Dose reduction methods for CT colonography. Abdom Imaging. 2013;38:224–32.
Cohnen M, Vogt C, Beck A, et al. Feasibility of MDCT colonography in ultra-low-dose technique in the detection of colorectal lesions: comparison with high-resolution video colonoscopy. Am J Roentgenol. 2004;183:1355–9.
Iannaccone R, Catalano C, Mangiapane F, et al. Colorectal polyps: detection with low-dose multidetector row helical CT colonography versus two sequential colonoscopies. Radiology. 2005;237:927–37.
• Chang KJ, Caovan DB, Grand DJ, et al. Reducing radiation dose at CT Colonography: decreasing tube voltage to 100 kVp. Radiology. 2013;266:791–800. This is the first study demonstrating the ability to significantly lower the radiation dose of CT colonography by decreasing kVp rather than mAs.
• Johnson CD, Chen MH, Toledano AY, et al. Accuracy of CT colonography for detection of large adenomas and cancers. N Engl J Med. 2008;359:1207–17. This is an important multicenter trial demonstrating that CT colonography has excellent sensitivity for 10 mm and larger polyps and cancer in a screening population.
Graser A, Stieber P, Nagel D, et al. Comparison of CT colonography, colonoscopy, sigmoidoscopy and fecal occult blood tests for the detection of advanced adenoma in an average risk population. Gut. 2009;58:241–8.
• Berrington de González A, Kim KP, Knudsen AB, et al. Radiation-related cancer risks from CT colonography screening: a risk-benefit analysis. Am J Roentgenol. 2011;196:816–23. This study addresses the concern regarding radiation risk related to screening CT colonography and showed that there was a very large benefit of colorectal cancers prevented using CTC compared to a very low risk of radiation-induced cancers.
Brenner DJ, Georgsson MA. Mass screening with CT colonography: should radiation exposure be of concern? Gastroenterology. 2005;129:328–37.
Bauhs JA, Vrieze TJ, Primak AN, Bruesewitz MR, McCollough CH. CT dosimetry: comparison of measurement techniques and devices. Radiographics. 2008;28:245–53.
Thakur Y, McLaughlin PD, Mayo JR. Strategies for radiation dose optimization. Curr Radiol Rep. 2013;1:1–10.
American Association of Physicists in Medicine Report #96. Diagnostic Imaging Council CT Committee Task Group #23. The measurement, reporting and management of radiation dose in CT. www.aapm.org/pubs/reports/RPT_96.pdf. Accessed 20 June 2013.
Habibzadeh MA, Ay MR, Asl AR, Ghadiri H, Zaidi H. Impact of miscentering on patient dose and image noise in X-ray CT imaging: phantom and clinical studies. Phys Med. 2012;28:191–9.
Li J, Udayasanker UK, Toth TL, et al. Automatic patient centering for MDCT: effect on radiation dose. Am J Roentgenol. 2007;188(2):547–52.
Burling D, Taylor SA, Halligan S, et al. Automated insufflation of carbon dioxide for MDCT colonography: distention and patient experience compared with manual insufflation. Am J Roentgenol. 2006;186(1):96–103.
Christner JA, Zavaletta VA, Eusemann DC, et al. Dose reduction in helical CT: dynamically adjustable z-axis X-ray beam collimation. Am J Roentgenol. 2010;94(1):W49–55.
McCollough CH, Primak AN, Bruan N, et al. Strategies for reducing radiation dose in CT. Radiol Clin N Am. 2009;47(1):27–40.
van Gelder RE, Venema HW, Serlie IW, et al. CT Colonography at different radiation dose levels: feasibility of dose reduction. Radiology. 2002;224(1):25–33.
Ginsburg M, Obara P, Wise L, et al. BMI-based radiation dose reduction in CT colonography. Acad Radiol. 2013;20(4):486–92.
Haaga JR, Miraldi F, MacIntyre W, LiPuma JP, Bryan PJ, Wiesen E. The effect of mAs variation upon computed tomography image quality as evaluated by in vivo and in vitro studies. Radiology. 1981;138(2):449–54.
Kalender WA, Wolf H, Suess C. Dose reduction in CT by anatomically adapted tube current modulation. II. Phantom measurements. Med Phys. 1999;26(11):2248–53.
Lim HK, Lee KH, Kim SY, Kim KJ, Kim B, Lee H, et al. Does the amount of tagged stool and fluid significantly affect the radiation exposure in low-dose CT colonography performed with an automatic exposure control? Eur Radiol. 2011;21(2):345–52.
Schindera ST, Nelson RC, Toth TL, Nguyen GT, Toncheva GI, DeLong DM, et al. Effect of patient size on radiation dose for abdominal MDCT with automatic tube current modulation: phantom study. Am J Roentgenol. 2008;190(2):W100–5.
Duan X, Wang J, Christner JA, Leng S, Grant KL, McCollough CH. Dose reduction to anterior surfaces with organ-based tube-current modulation: evaluation of performance in a phantom study. Am J Roentgenol. 2011;197(3):689–95.
Hopper KD, King SH, Lobell ME, TenHave TR, Weaver JS. The breast: in-plane X-ray protection during diagnostic thoracic CT—shielding with bismuth radioprotective garments. Radiology. 1997;205(3):853–8.
Hohl C, Wildberger JE, Suss C, Thomas C, Muhlenbruch G, Schmidt T, et al. Radiation dose reduction to breast and thyroid during MDCT: effectiveness of an in-plane bismuth shield. Acta Radiol. 2006;47(6):562–7.
Elojeimy S, Tipnis S, Huda W. Relationship between radiographic techniques (kilovolt and milliampere-second) and CTDI(VOL). Radiat Prot Dosim. 2010;141(1):43–9.
Brooks RA. A quantitative theory of the Hounsfield Unit and its application to dual energy scanning. J Comput Assist Tomogr. 1977;1(4):487–93.
Guimaraes LS, Fletcher JG, Harmsen WS, Yu L, Siddiki H, Melton Z, et al. Appropriate patient selection at abdominal dual-energy CT using 80 kV: relationship between patient size, image noise, and image quality. Radiology. 2010;257(3):732–42.
Schabel C, Fenchel M, Schmidt B, et al. Clinical evaluation and potential radiation dose reduction of the novel Sinogram-Affirmed Iterative Reconstruction Technique (SAFIRE) in abdominal computed tomography angiography. Acad Radiol. 2013;20:165–72.
Compliance with Ethics Guidelines
Conflict of Interest
Judy Yee, Kevin J. Chang, and Stefanie Weinstein declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yee, J., Chang, K.J. & Weinstein, S. Applying Dose Reduction to CT Colonography. Curr Radiol Rep 1, 286–293 (2013). https://doi.org/10.1007/s40134-013-0025-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40134-013-0025-9