Abstract
Introduction
Optimizing treatment protocols for wet age-related macular degeneration (wAMD) is an ongoing challenge, as it involves a delicate balance between achieving therapeutic efficacy and minimizing invasive procedures' frequency. This study aimed to apply the Lean methodology and evaluate the effectiveness of this new setting on intravitreal therapy for wAMD, employing different anti-vascular endothelial growth factors (VEGF) drugs (bevacizumab, brolucizumab, aflibercept, ranibizumab), drawing data from the Bari Intravitreal Injections Registry (BIVIR).
Methods
This was a retrospective, monocentric, nonrandomized, comparative study. Lean methodology was employed to design the new setting and the BIVIR collected information from electronic medical records. Clinical data of four groups, stratified based on the first-line anti-VEGF agents used, were compared. Best-corrected visual acuity (BCVA) and central retinal thickness (CRT) changes were compared between the four groups at 3 and 12 months.
Results
Out of 4990 eyes and 41,323 intravitreal injections (IVs) recorded in BIVIR, 1421 eyes of 1182 patients were included. The mean number of IVs in first year was 6.1 ± 2.5, with no significant differences among the four subgroups. The mean change in BCVA was + 6.2 letters [95% confidence interval (CI) 5.6–6.8] after two IVs, and + 5.9 (95% CI 5.1–6.8) letters after three IVs; at three months, brolucizumab was associated with a greater mean increase in BCVA than bevacizumab (p = 0.050); aflibercept (p = 0.044) and ranibizumab p = 0.047). At the 1-year follow-up, the mean change was + 6.3 letters (95% CI 5.4–7.2), brolucizumab and ranibizumab were associated with a superior improvement in BCVA compared to aflibercept (p = 0.033). Regarding the CRT, a significant reduction was observed in the subgroup treated with brolucizumab at the 3-month follow-up, compared to bevacizumab (p = 0.003), aflibercept (p = 0.015), and ranibizumab (p < 0.001); Aflibercept exhibited a superior effect than ranibizumab (p = 0.001). At 1-year follow-up, aflibercept resulted in a more significant reduction of macular thickness compared to ranibizumab (p = 0.016) while no significant differences were observed among the other drugs.
Conclusions
Our practical experience showed the effectiveness of the new setting in the treatment of wAMD. This comparative study at 1 year suggested a predominant brolucizumab efficacy on functional outcomes. In addition, brolucizumab and aflibercept appeared to have similar efficacy in fluid control.
Similar content being viewed by others
Why carry out this study? |
Wet age-related macular degeneration (wAMD) leads to blindness, with anti-vascular endothelial growth factor (anti-VEGF) injections as the main treatment. Healthcare facilities struggle to provide effective care. |
This study presents data on the effectiveness of intravitreal anti-VEGF therapy in wAMD, employing an innovative Lean-designed setting. This approach minimizes time and travel for patients and hospital staff, enabling sterile, non-operating room injections. |
What was learned from the study? |
After 1 year, brolucizumab and ranibizumab treatments significantly improved best-corrected visual acuity (BCVA) compared to aflibercept, even for patients with a baseline BCVA of 35–70 letters. At 1 year, only aflibercept showed a substantial thickness improvement over ranibizumab, with no significant differences in other comparisons. |
Applying Lean methodology to organize an Intravitreal Injection Centre proved more effective for treating patients with wAMD than standard methods. Electronic data collection was essential for predicting anti-VEGF responses, particularly with emerging therapies. |
Introduction
Age-related macular degeneration (AMD) is an acquired degeneration of the macula and is the first cause of blindness in industrialized countries. The disease is more prevalent in the elderly population because age is the principal risk factor [1].
The prevalence of AMD in industrialized countries is 1.6%, with the exudative form associated with macular neovascularization (MNV) being present in one eye 1.2% of the time, and geographic atrophy in one eye 0.6% of the time. Two hundred million people worldwide are estimated to have AMD; by 2040, this number is projected to rise to nearly 300 million [2].
The intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) have revolutionized the treatment of wet AMD (wAMD). Currently, these are the drugs on the market:
-
Bevacizumab (Avastin, off-label), a monoclonal antibody;
-
Ranibizumab (Lucentis), a monoclonal antibody fragment
-
Aflibercept (Eylea), a receptor-antibody fusion protein;
-
Brolucizumab (Beovu), single chain antibody fragment;
-
Faricimab (Vabysmo), a bi-specific antibody directed against both VEGF and angiopoietin-2.
While best practices recommend an initial loading dose followed by ongoing treatment, there is no consensus on the ideal regimen for the subsequent phase of therapy. The frequency of injections varies significantly, as ophthalmologists can choose between fixed or customized regimens.
Historically, monthly injections of ranibizumab were used [3, 4], but this proved burdensome for both patients and healthcare systems. The VIEW study introduced aflibercept as a promising alternative, extending the time between injections [5].
Research has explored different injection schedules for ranibizumab, bevacizumab, and aflibercept, including non-monthly options like fixed or customized regimens. In pro-re-nata (PRN), injections are given when disease activity is observed using optical coherence tomography (OCT) or clinical signs. In contrast, the treat-and-extend (T&E) regimen involves treatment upon recurrence, with intervals between injections gradually increasing unless recurrence is detected. Both regimens require injections to be scheduled on the same day as the examination [5,6,7,8,9,10,11,12,13,14,15].
The ideal treatment protocol aims to minimize injections to reduce potential adverse effects and optimize therapeutic outcomes. Monthly injections are slightly more effective than PRN regimens in the short term, but the difference is not clinically significant. The T&E regimen, despite requiring more injections, provides results similar to monthly protocol. In contrast, monthly regimens are associated with a higher risk of complications and greater costs, especially with specific drugs. Even after 2 years, the slight visual benefit difference between PRN and monthly regimens persists [16].
The challenge lies in translating these trial results into clinical practice, as PRN regimens may lead to undertreatment. Patients' compliance with treatment and regular follow-up appointments is crucial, but various factors, including affordability, accessibility, and lack of perceived improvement in vision, can hinder this.
Noncompliance often leads to reactivation of the disease, causing irreversible visual losses [17]. To address these issues effectively, it is essential to strike a balance between optimizing treatment outcomes and ensuring patients can access and afford the necessary care.
The Lean methodology [18, 19], originally developed by Toyota to improve productivity, has also been applied in the healthcare and ophthalmology fields [20, 21]. The Lean approach aims to create more value for customers with fewer resources and minimize waste by implementing Lean principles such as identifying value, mapping the value stream, creating flow, establishing a pull-based system, and striving for perfection. There are several tools that support Lean organization, such as identifying waste (the seven wastes of Ohno), mapping material and information flow (Value Stream Mapping), and analyzing the movement of people within a facility (Spaghetti Chart), among others.
This study aimed to apply the Lean methodology to the management of patients with wet age-related macular degeneration and to verify the effectiveness of this new setting on intravitreal therapy with different anti-VEGF, using the Bari Intravitreal Injections Registry (BIVIR).
Methods
At the Eye Clinic of the Policlinic in Bari, Italy, the Lean methodology was implemented using both its principles to identify and eliminate waste (transportation, inventory, motion, waiting, over-production, over-processing, defects, and skills) and some of its tools, such as Value Stream Mapping to define the process, measure it, and identify areas for improvement in the use of resources and the organization of patient and information flow, and Spaghetti Charts to map the physical movement of patients and materials within the Eye Clinic.
We have created a new Intravitreal Injection Center (IVIC) to provide a fast and streamlined route, minimize the waste of time and space, and enhance the center's capacity management.
The IVIC is a diagnostic-surgical office that exclusively serves patients who require intravitreal injections of any drug and the sterility of the operating field is guaranteed by a device called ArcSterile®, which generates laminar flows and meets the ISO5 class of sterility criteria. The route is on a single floor, within a single clinic, and follows a circular path. The patient travels a distance of 68 m and goes through the spaces in sequence. We had previously described this innovative setting [22]. Here, we summarized the clinical evaluation.
The new pre-visit process involves collecting informed consent and completing or updating a computerized form (Microsoft Excel® worksheet), including anamnestic and clinical data. The form records the best-corrected visual acuity (BCVA) as Early Treatment Diabetic Retinopathy Study (ETDRS) letters, central retinal thickness (CRT), tonometry, and injected drug for each visit. These sheets are kept in both paper and electronic form at the IVIC. All patients undergo an examination of visual acuity, OCT, and OCT-angiography; tonometry is reserved for all patients at first access; for those on anti-glaucoma therapy, or receiving a corticosteroid injection/implant; it is performed at each visit.
Based on the results of the pre-visit and the patient's ocular clinical history, the diagnosis, drug indication, and treatment schedule must be confirmed before the injection. If additional examinations or procedures (such as fluorescein angiography, bulbar ultrasound, laser capsulotomy, cataract surgery, vitreoretinal surgery, etc.) are required, the request and reservation will be made while the patient continues their journey in the surgical room.
The study adhered to the principles outlined in the Declaration of Helsinki. This study is retrospective in nature, and in accordance with Italian regulations, ethical approval is not necessary for such studies. Instead, only notification to the ethics committee is required. Therefore, the institutional review board was notified. Written consent was obtained from all participants included in the study, allowing for the retrospective use of their clinical data.
Medical Records
In the previous setting, paper medical records (PMR) were required for each patient, kept in a department archive and obtained the day before the patient's appointment. Every year, all PMR were moved to an external archive and a new PMR was created for each patient.
In the new setting, the author (M.O.G.) projected the electronic medical record (EMR) and the Bari Intravitreal Injections Registry (BIVIR) for the IVIC, using Microsoft Excel software. Each patient was assigned a single file with two spreadsheets. The first spreadsheet includes the demographic information and baseline systemic and local characteristics, as well as bilateral data from each visit (date, best-corrected visual acuity, central retinal thickness, intraocular pressure, and any drugs injected or adverse events during treatment in the IVIC); the BCVA and CRT of both eyes were automatically plotted in a graph to illustrate the functional and anatomical improvement or deterioration over time. The second spreadsheet was used to record the diagnostic and treatment schedule from the patient's first visit to the IVIC, and it was updated, printed, and given to the patient at each visit.
All files were collected in an electronic folder. Every January, we reviewed the death date of patients whose last visit was over 6 months ago (this screening was based on the last modified date of the patient's file). If a patient passed away, their file was moved to a designated folder.
All data were incorporated into the BIVIR. This Excel spreadsheet automatically calculated other parameters, such as the age of the patient at their first intravitreal injection, the number of injections given in the first year and over the total duration of follow-up, the interval between intravitreal injections, and the distribution of sex, age, residence, disease, and the first visit by percentage. Currently, the dataset includes information from 4990 eyes of 4058 patients.
Study Sample
This was a retrospective and comparative study. Inclusion criteria included a diagnosis of wet AMD and the first anti-VEGF injection administered between November 2017 and January 2023. Exclusion criteria comprised only prior intravitreal injections performed elsewhere or before the initiation of the IVIC. At initial access, the participants consented to the anonymous use of their data, and the BIVIR provided aggregate information. Additionally, the institutional review board was notified. This study adhered to the tenets of the Declaration of Helsinki. All continuous patients who met the inclusion criteria were enrolled. Data on BCVA, CRT, and type of injected drug were collected for each patient visit. BCVA was measured in ETDRS letter score; CRT was automatically estimated using the RTVue XR Avanti OCT software (Optovue Inc., Fremont, CA, USA).
Statistical Analysis
The data were analyzed using Microsoft Excel 2013. Count and percentage presented the discrete data, and normally distributed continuous data were reported as mean and standard deviation. For evaluating the correlation between unilateral and bilateral treatments, we utilized the standard regression method using STATA 14.0 software. The pair Student's t test was employed to compare the means of functional and anatomical data between the baseline and the various timepoints. To compare baseline values between four treatment groups, a one-way analysis of variance (ANOVA) test was used. To assess the varying efficacy of the molecules, we employed the Student’s t test to compare the different treatment groups pairwise and a p value of less than 0.05 was considered statistically significant. To assess the comparability of data with randomized clinical trials, a subgroup was formed, comprising eyes with a baseline BCVA ranging from 35 to 70 letters, and was analyzed as for the entire sample.
Results
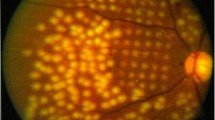
Overall, 1421 eyes of 1182 patients affected by treatment-naïve wet AMD were enrolled at IVIC of the University of Bari (Italy) from November 2017 to January 2023. The distribution of enrolled eyes over time is shown in Fig. 1.
The overall distribution of eye conditions during the observation period. In April 2020, no treatment-naive patients were observed due to the SARS-CoV-2 pandemic lockdown. During that period, only patients with scheduled intravitreal injections were treated because medical retina offices (both public and private) were closed in accordance with Italian regulations, and emergency rooms were overcrowded with patients suffering from respiratory disease
The mean age at diagnosis was 77 ± 8 years (range, 50–98). 52.4% of patients were female, 13.3% of cases had diabetes, and 7.0% had died during the follow-up; 1.5% of eyes were vitrectomized, and 48.8% were pseudophakic; 13.9% underwent cataract surgery during the anti-VEGF treatment and 6.2% used anti-glaucoma drugs.
First-line treatment was bevacizumab (6.5%), brolucizumab (5.6%), aflibercept (30.9%), ranibizumab (56.9%), and pegaptanib (0.1%); 13.0% of eyes were switched to another anti-VEGF after their initial option. For patients receiving anti-VEGF IV in both eyes, the median treatment interval between the first injection in two eyes was 6.1 weeks (range, 1–214).
A total of 1133 eyes had a follow-up longer than 48 weeks: in this subgroup, 24% completed the loading dose in 56 days, 54% in between 57 and 70 days, and 9% in 71–84 days.
During the loading phase, mean BCVA significantly improved after the first and the second IV: 50.2 ± 23.7 letters at baseline, 55.8 ± 23.1 letters after IV n.1 (p < 0.001), 57.0 ± 22.9 letters after IV n.2 (p < 0.001), and 57.7 ± 22.5 letters after IV n.3 (p = 0.18) (p value referred to paired Student's t test for BCVA when compared to the previous measurement). The average BCVA change was + 6.2 (95% confidence interval: 5.6–6.8) letters after two IVs, and + 5.9 (95% CI 5.1–6.8) letters after three IVs, with no significant difference observed between the gains at these two time points. For this reason, we considered the visual outcome following two IVs to the baseline: a higher proportion of patients (19.2%) showed a gain of ≥ 15 letters in BCVA, compared to those who experienced a loss of ≥ 15 letters (2.6%).
Furthermore, the four groups stratified by anti-VEGF IV had no significant difference in the baseline BCVA (p = 0.273). The mean increase in BCVA in eyes treated with brolucizumab was significantly higher than in eyes treated with all other drugs (vs. bevacizumab p = 0.050; vs aflibercept p = 0.044; vs. ranibizumab p = 0.047). In the subgroup with limited baseline BCVA, the results of the head-to-head study revealed no significant variations among the four anti-VEGF agents.
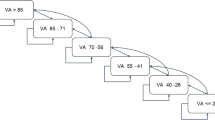
For the purpose of evaluating the anatomical response, compared to other drugs, a significant reduction in CRT was observed in the subgroup treated with brolucizumab at a 3-month follow-up (vs. bevacizumab p = 0.003; vs. aflibercept p = 0.015; vs. ranibizumab p < 0.001). Aflibercept demonstrated a superior effect only compared to ranibizumab (p = 0.001). The same statistical significance was also confirmed by the t-test performed on the percentage values of CRT reduction or increase. When eyes with a baseline BCVA between 35 and 70 letters were selected, only aflibercept significantly reduced CRT compared to ranibizumab (p = 0.014) (Fig. 2).
Comparison of best-corrected visual acuity (BCVA) and central retinal thickness (CRT) changes to baseline measurements at 3-month follow-up for the whole sample and a subgroup categorized by their baseline BCVA (35 to 70 ETDRS letters), stratified by the drug used. ETDRS Early Treatment Diabetic Retinopathy Study, IV intravitreal injection
At the 1-year follow-up, the mean IV number was 6.1 ± 2.5, and there were no significant differences observed between the four subgroups that were treated with different anti-VEGF drugs. The mean BCVA was 58 ± 23 letters, and the mean change was + 6.3 ± 14.8 letters (95% CI 5.4–7.2). 23.8% of eyes showed a gain of 15 letters or more in BCVA, while 5.4% had a loss of 15 letters or more.
CRT also significantly decreased from the baseline to the 1-year follow-up, 350 ± 121 μm and 259 ± 80 μm, respectively (p < 0.001).
Based on the type of first-line anti-VEGF, eyes were divided into four groups. The visual and anatomic outcomes at the 1-year follow-up are presented in Table 1. The statistical analysis only included patients with data available at baseline and 1-year follow-up.
The results indicated that brolucizumab was associated with a superior improvement in BCVA compared to aflibercept (p = 0.033), and that ranibizumab was superior to aflibercept (p = 0.033). These significant differences were maintained even after analysis of the subgroup with a baseline BCVA ranging from 35 to 70 letters (p = 0.027 and p = 0.036, respectively).
With regard to CRT, aflibercept resulted in a more significant reduction of macular thickness compared to ranibizumab (p = 0.016) in both the whole sample and subgroup; there were no notable differences among the other drugs (Fig. 3). The statistical analysis conducted on the percentage change values from the baseline yielded results that were comparable to those obtained using absolute data. Figure 4 and Tables 1–2 summarize the visual and anatomical outcomes at three time points (baseline, 3 months, and 1 year), stratified by the drug administered. The results of the regression analysis presented significant findings. Patients receiving treatment in both eyes did not show a significant difference in BCVA change, but they demonstrated a notable reduction in CRT (− 9.0 μm) compared to those undergoing treatment in only one eye. Additionally, the number of injections administrated in the first year was also statistically significant, positively impacting functional outcomes while not affecting CRT.
Comparison of best-corrected visual acuity (BCVA) and central retinal thickness (CRT) changes to baseline measurements at 1-year follow-up for the whole sample and a subgroup categorized by their baseline BCVA (35 to 70 ETDRS letters), stratified by the drug used. ETDRS Early Treatment Diabetic Retinopathy Study
In the observational period, adverse events reported were: sub-macular hemorrhage (0.44%), iatrogenic cataracts (0.22%), and endophthalmitis (0.07%). During the anti-VEGF treatment, other surgical procedures were performed: phacoemulsification for cataracts (4.7%), vitrectomy (0.3%), laser capsulotomy (0.6%), and keratoplasty (0.15%). Three patients (0.3%) after enrollment in the IVIC received IVs elsewhere but later returned to IVIC.
Discussion
The health system's implementation in managing patients affected by wet AMD is crucial for two reasons. The first reason is that anti-VEGF intravitreal injections (the approved therapy for this disease) are effective and safe. Still, better outcomes are achieved with timely treatment, a proper initial dosage, and a tailored maintenance plan.
The second reason is that the number of patients with wet AMD is on the rise due to both an aging global population and improved diagnostic techniques. Due to a shortage of personnel, funding, and accessible facilities, the global healthcare system is struggling to keep up with the need for anti-VEGF IV treatment and follow-up visits for patients with wet AMD. This chronic condition necessitates ongoing management, including regular administration of anti-VEGF IV and OCT exams. This results in a strain on the healthcare system, leading to delays in exams and treatment and on the patient and their support network, causing low compliance and an increase in missed appointments.
Ultimately, improper treatment leads to visual impairment and blindness, resulting in increased disability pensions for the blind.
The IVIC was designed to fight wet AMD-induced blindness by providing a patient-friendly environment where patients can be seen and treated in a timely manner with minimal wait time, enabling the center to see more patients per day. The center also offers specialized staff and dedicated spaces to ensure the best possible care for patients. Furthermore, the transition to electronic medical records and data storage ensures the accumulation of large amounts of data, resulting in a higher statistical significance.
Previous research has already established the safety of the ArcSterile® laminar flow system [23]. This solution makes it possible to perform IV procedures outside of the operating room, even in areas where IV is considered a high-risk procedure for infection and an ISO5 cleanroom is required.
Additionally, our group was the first to demonstrate how the implementation of Lean methodology had improved the process of IV administration [22]. We measured the efficiency of the IVIC by tracking the time patients spent waiting in the waiting room, which decreased by an average of − 2 ± 28 min and the mean time to complete the entire pathway was 32 ± 16 min. We studied patient compliance by tracking down patients who had been lost to follow-up for over 6 months and found that none of them had chosen to stop monitoring or treatment on their own. Additionally, this research provided our first insights into the distribution of diseases among our patients, with 40.5% of patients in our hospital diagnosed with wAMD.
To the best of our knowledge, this study is the first to evaluate the effectiveness of the new Lean methodology-based approach in patients with wAMD. Our analysis of data from the IVIC, compared with real-world data, revealed that patients with wAMD experienced better visual outcomes after anti-VEGF therapy as demonstrated in a 1-year follow-up; this was measured by the mean number of IV (6.1 ± 2.5), the mean BCVA change (+ 6.5 ± 14.8 letters) and the percentage of patients with ≥ 15 letters gain (23.8%). The AURA study, a retrospective multicenter study, enrolled patients that started ranibizumab therapy for wAMD between January 2009 and August 2009 from eight countries. The study found that patients experienced an average gain of 2.4 letters on a vision test and received a mean of 5.0 injections during the first year of treatment. In the analysis by country, Italian patients showed a change in VA score to year 1 of 0.0 letters with a mean number of IVs to year 2 of 5.2 [24]. Moreover, a successive analysis of the AURA data revealed that ≥ 5.1 ranibizumab injections were necessary to maintain baseline VA to year 1 [25]. After this dramatic scenario, much effort was spent on improving anti-VEGF therapy.
Better visual outcomes were seen in aflibercept in a clinical setting. The RAINBOW study across France showed a BCVA improvement over 1 year and a 6.0 ± 2.1 mean number of IVs of + 5.5 ± 15.0 letters. In patients who received a loading dose, the mean change in VA was + 6.8 ± 14.5 letters and 6.6 ± 1.8 IVs [26].
For brolucizumab, observational studies on treatment-naive patients with almost 1-year follow-up still presented a small sample and were dedicated to a specific sub-type MNV. The recent one enrolled 45 eyes with type 1 MNV and estimated 6.4 ± 0.6 as the average number of IVs over the 1 year using a treat-and-extend regimen. This study reported VA improvement as the mean LogMAR score at baseline and 1 year (exactly between 44 and 52 weeks), 0.25 ± 0.30 and 0.10 ± 0.26, respectively [27].
Clinical trials usually presented better visual outcomes due to the strict inclusion criteria and fixed monitoring visits. For example, in the CATT study, the mean change in BCVA during the first-year follow-up was + 8.5 ± 0.8, + 8.0 ± 1.0, + 6.8 ± 0.8, and 5.9 ± 1.0 in the four groups (ranibizumab-monthly, bevacizumab-monthly, ranibizumab-as-needed, bevacizumab-as-needed, respectively). Moreover, the proportion of patients who lost ≥ 15 letters was 5.6, 6.0, 4.6, and 8.2% in the four previously described groups to year 1 [28]. Comparable results were seen in trials involving aflibercept, in which mean change in BCVA was + 9.0 and + 8.4 in two groups with 2- or 4-week adjustments, respectively, in the T&E regimen, after a mean number of IVs of 7.2 ± 0.9 and 6.9 ± 1.0, respectively [29]. Brolucizumab demonstrated non-inferiority to aflibercept in two randomized clinical trials, with a BCVA change from baseline at 48 weeks of + 6.6 letters, and the probability for maintaining on q12w dosing throughout year 1 was estimated to > 50% [30].
Our analysis of specific drug efficacy suggests that when a baseline BCVA more similar to that used in randomized clinical trials is considered, the visual outcome at month 3 after two IVs was non-inferior among the four molecules. However, when considering an actual population, brolucizumab significantly improved BCVA from the baseline. At year 1, eyes treated with brolucizumab and ranibizumab showed a significantly greater improvement in visual acuity compared to aflibercept. This difference was maintained even in the subgroup with a baseline BCVA between 35 and 70 letters.
Concerning the CRT, at the 3-month follow-up, brolucizumab demonstrated a greater ability to reduce fluid exudation than all drugs, and aflibercept was superior to ranibizumab; in the subgroup with limited baseline BCVA, only aflibercept showed a significant difference versus ranibizumab. At 1-year follow-up, only eyes treated with aflibercept presented a significant improvement in thickness compared to ranibizumab, both in the entire sample and in the subgroup; no significant differences were observed in the other head-to-head comparisons.
These results were different from those found in clinical trials or observational data. The HAWK and HARRIER studies compared brolucizumab and aflibercept and enrolled patients with a baseline BCVA between 23 and 78 letters. Data from the 1-year follow-up did not reveal a significant difference between the two anti-VEGFs; this outcome was not affected by the baseline BCVA. In addition, concerning the IRF and SRF reabsorption, these brolucizumab phase III trials demonstrated its statistical superiority compared to aflibercept in fluid control. This result contrasted with our experience, but some clarifications were needed. Our two groups had quite different sample sizes, with the mean baseline CRT being significantly higher in the brolucizumab and aflibercept group than in the ranibizumab group. A randomized comparative study between ranibizumab and aflibercept in T&E regimen, the RIVAL study, showed no difference regarding the average VA gain and number of IV during 1 year; our study confirmed these results [31].
The comprehensive electronic register dedicated to patients with retinal diseases has become essential in managing this population. Big data has attracted much attention from both clinicians and the drug industry because it helps gather new information and make appropriate decisions.
The first big register was the Fight Retinal Blindness! Project [32], a web-based system developed to track the effectiveness and safety of new treatments for macular disease. The first countries that used this software were Australia and Switzerland, but now it is widespread. In this registry, data were input since 2006.
In the US, patients’ data were collected in a multicenter registry, the American Academy of Ophthalmology (AAO) Intelligent Research in Sight (IRIS) Registry since January 2013 [33].
Successively, other European countries introduced a national registry, particularly dedicated to patients with AMD, such as the Swedish Macula Register (SMR),72 Polish National AMD Treatment Program since 2015 [34].
However, the first monocentric database was the UK Moorfields AMD database, which collected the EMR from October 2008. It was implemented in September 2012, and then the data were merged into a centralized repository, the data warehouse [35]. Recently, the Berlin Macula Registry was used to present the outcomes of switching to bevacizumab in patients with wAMD [36, 37].
In Italy, to the best of our knowledge, our Bari Intravitreal Injections Registry (BIVIR) was the first to progressively enroll every patient who receives an intravitreal injection of any drug, enabling us to gather a larger number of patients compared to multicenter clinical trials. This improved the strength of our results and provided greater awareness of our patients' demographic and clinical characteristics.
The Lean Six Sigma methodology has been frequently applied in the healthcare system in recent years. In the ophthalmology clinic, it was used to improve efficiency in vitreoretinal practice [21] or cataract surgery unit [38].
Our group, for the first time, applied Lean principles in the design of a new Intravitreal Injection Center [22]. Our experience inspired other groups, especially during the COVID-19 pandemic when long waiting times and crowded places increased the risk of infection [39]. In fact, the IVIC organization was not changed during the pandemic because it already guaranteed safety during the patient journey and compliance with anti-COVID regulations; the decrease in IVIC accesses was due only to patients' systemic illness or fear. In the present study, we showed the outcomes of anti-VEGF treatment in patients with wAMD in this new setting. We observed that the visual improvement was comparable to clinical trials or worldwide general experience, but better than Italian results as presented by the AURA study.
The study has several limitations. Firstly, the EMR were stored in an Excel spreadsheet within the hospital network, which was not accessible online. The retrospective design introduced biases like selection bias, variations in treatment, and the absence of strict retreatment criteria.
Another important limitation is that we did not consider inter-eye correlations in our analysis, as we included both eyes in a number of cases. However, our analysis did not show significant differences in BCVA modifications between patients treated in one eye vs. those treated in either eye. More importantly, it must be considered that this study represents a crude assessment of a real-world experience in which several factors including neovascularization type, development of macular complications, and drug choice were not considered.
In the study, data collected before the last intravitreal injection served as the final visit for the 1-year follow-up. The preferred maintenance approach was the T&E method, which minimizes follow-up gaps. Yet, in cases of visual deterioration, patients received prompt treatment after referral to their ophthalmologist or the emergency room. Consequently, it was assumed that the last available data represented 1 year of visual and anatomical outcomes.
To compare data and outcomes between the new and previous settings, the assumption was made that patient management in the previous setting was similar to what the AURA study found in Italian ophthalmological clinics. The changes in patient management primarily centered around streamlining the patient journey and digitalizing data, with limited impact from the introduction of the new anti-VEGF. These changes are believed to be the main drivers of the center's enhanced patient management.
Conclusions
In conclusion, this study showed that the application of Lean methodology to the organization of an Intravitreal Injection Center was more effective in treating patients affected by wet age-related macular degeneration than in standard organization. The electronic transition was crucial to obtain big data and, therefore, predictive information on the anti-VEGF response, especially when several drugs and new therapeutic options become available shortly. In the future perspective, the registry should be implemented with MNV-type classification and fluid subtype monitoring.
Data Availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Vyawahare H, Shinde P. Age-related macular degeneration: epidemiology, pathophysiology, diagnosis, and treatment. Cureus. 2022;14(9)
Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2)
Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–31.
Brown DM, Michels M, Kaiser PK, et al. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology. 2009;116(1):57–65.
Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration [published correction appears in Ophthalmology. 2013 Jan;120(1):209–10]. Ophthalmology. 2012;119(12):2537–2548.
Abedi F, Wickremasinghe S, Islam AF, Inglis KM, Guymer RH. Anti-VEGF treatment in neovascular age-related macular degeneration: a treat-and-extend protocol over 2 years. Retina. 2014;34(8):1531–8.
Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group, Martin DF, Maguire MG, et al. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology. 2012;119(7):1388–1398.
Heier JS, Boyer D, Nguyen QD, et al. The 1-year results of CLEAR-IT 2, a phase 2 study of vascular endothelial growth factor trap-eye dosed as-needed after 12-week fixed dosing [published correction appears in Ophthalmology. 2011 Sep;118(9):1700]. Ophthalmology. 2011;118(6):1098–1106.
Ho AC, Busbee BG, Regillo CD, et al. Twenty-four-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology. 2014;121(11):2181–2192.
IVAN Study Investigators, Chakravarthy U, Harding SP, et al. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial [published correction appears in Ophthalmology. 2012 Aug;119(8):1508] [published correction appears in Ophthalmology. 2013 Sep;120(9):1719]. Ophthalmology. 2012;119(7):1399–1411.
Abraham P, Yue H, Wilson L. Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular age-related macular degeneration: PIER study year 2. Am J Ophthalmol. 2010;150(3):315–24.
Lalwani GA, Rosenfeld PJ, Fung AE, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. Am J Ophthalmol. 2009;148(1):43–58.
Schmidt-Erfurth U, Eldem B, Guymer R, et al. Efficacy and safety of monthly versus quarterly ranibizumab treatment in neovascular age-related macular degeneration: the EXCITE study. Ophthalmology. 2011;118(5):831–9.
Silva R, Axer-Siegel R, Eldem B, et al. The SECURE study: long-term safety of ranibizumab 0.5 mg in neovascular age-related macular degeneration. Ophthalmology. 2013;120(1):130–139.
Holz FG, Amoaku W, Donate J, et al. Safety and efficacy of a flexible dosing regimen of ranibizumab in neovascular age-related macular degeneration: the SUSTAIN study. Ophthalmology. 2011;118(4):663–71.
Li E, Donati S, Lindsley KB, Krzystolik MG, Virgili G. Treatment regimens for administration of anti-vascular endothelial growth factor agents for neovascular age-related macular degeneration. Cochrane Database Syst Rev. 2020;5(5):CD012208. Published 2020 May 5.
Kelkar A, Webers C, Shetty R, et al. Factors affecting compliance to intravitreal anti-vascular endothelial growth factor therapy in Indian patients with retinal vein occlusion, age-related macular degeneration, and diabetic macular edema. Indian J Ophthalmol. 2020;68(10):2143–7.
Ohno T. Toyota production system: beyond large-scale production. Portland: Productivity Press; 1988.
Womack JP, Jones DT, Roos D. The machine that changed the world: the story of lean production-Toyota’s secret weapon in the global car wars that is now revolutionizing world industry. New York: Harper Perennial; 2007.
Fillingham D. Lean healthcare: improving the patient’s experience, vol. 26. Chichester: Kingsham Press; 2008.
Ciulla TA, Tatikonda MV, ElMaraghi YA, et al. Lean six sigma techniques to improve ophthalmology clinic efficiency. Retina. 2018;38(9):1688–98.
Grassi MO, Furino C, Recchimurzo N, et al. Implementation of Lean healthcare methodology in designing an Intravitreal Injection Center: first Italian experience. Int Ophthalmol. 2020;40(10):2607–15.
Furino C, Grassi MO, Bini V, et al. Intravitreal injections in Arc sterile setting: safety profile after more than 10,000 treatments. J Ophthalmol. 2020;2020:3680406.
Holz FG, Tadayoni R, Beatty S, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99(2):220–6.
Holz FG, Tadayoni R, Beatty S, et al. Determinants of visual acuity outcomes in eyes with neovascular AMD treated with anti-VEGF agents: an instrumental variable analysis of the AURA study [published correction appears in Eye (Lond). 2017 Jan;31(1):166]. Eye (Lond). 2016;30(8):1063–1071.
Weber M, Velasque L, Coscas F, Faure C, Aubry I, Cohen SY. Effectiveness and safety of intravitreal aflibercept in patients with wet age-related macular degeneration treated in routine clinical practices across France: 12-month outcomes of the RAINBOW study. BMJ Open Ophthalmol. 2019;4(1)
Matsumoto H, Hoshino J, Mukai R, Nakamura K, Akiyama H. One-year results of treat-and-extend regimen with intravitreal brolucizumab for treatment-naïve neovascular age-related macular degeneration with type 1 macular neovascularization. Sci Rep. 2022;12(1):8195.
CATT Research Group, Martin DF, Maguire MG, et al. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364(20):1897–1908.
Ohji M, Takahashi K, Okada AA, et al. Efficacy and safety of intravitreal aflibercept treat-and-extend regimens in exudative age-related macular degeneration: 52- and 96-week findings from ALTAIR: a randomized controlled trial. Adv Ther. 2020;37(3):1173–87.
Dugel PU, Koh A, Ogura Y, et al. HAWK and HARRIER: phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2020;127(1):72–84.
Gillies MC, Hunyor AP, Arnold JJ, et al. Effect of ranibizumab and aflibercept on best-corrected visual acuity in treat-and-extend for neovascular age-related macular degeneration: a randomized clinical trial. JAMA Ophthalmol. 2019;137(4):372–9.
Gillies MC, Walton R, Liong J, et al. Efficient capture of high-quality data on outcomes of treatment for macular diseases: the fight retinal blindness! Project Retina. 2014;34(1):188–95.
Rao P, Lum F, Wood K, et al. Real-world vision in age-related macular degeneration patients treated with single anti-VEGF drug type for 1 year in the IRIS registry. Ophthalmology. 2018;125(4):522–8.
Granstam E, Westborg I, Barkander A, et al. Reduced occurrence of severe visual impairment after introduction of anti-Vascular Endothelial Growth Factor in wet age-related macular degeneration—a population- and register-based study from northern Sweden. Acta Ophthalmol. 2016;94(7):646–51.
Teper SJ, Nowińska A, Figurska M, Rękas M, Wylęgała E. The need for treatment of neovascular age-related macular degeneration: a study based on the polish national registry. Ophthalmol Ther. 2022;11(5):1805–16.
Fasler K, Moraes G, Wagner S, et al. One- and two-year visual outcomes from the Moorfields age-related macular degeneration database: a retrospective cohort study and an open science resource. BMJ Open. 2019;9(6)
Riemer T, Berndt D, Böker A, et al. Treatment of neovascular age-related macular degeneration: insights into drug-switch real-world from the Berlin Macular Registry [published online ahead of print, 2023 Jan 12] [published correction appears in Graefes Arch Clin Exp Ophthalmol. 2023 Feb 16;:]. Graefes Arch Clin Exp Ophthalmol. 2023
Taner MT. Application of Six Sigma methodology to a cataract surgery unit. Int J Health Care Qual Assur. 2013;26(8):768–85.
Verolino M, Grassi P, Sosto G, D'Onofrio G, De Simone S, Costagliola C. Lean approach to the management of patients undergoing intravitreal injections during COVID-19 pandemic. Ther Adv Ophthalmol. 2021;13.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Maria Oliva Grassi. Teresa Molfetta, Maria Giovanna Malerba and Maria D’Addario contributed in data collection. The first draft of the manuscript was written by Maria Oliva Grassi, Pasquale Viggiano and Francesco Boscia. Pasquale Viggiano, Enrico Borrelli, Giacomo Boscia, Ermete Giancipoli and Giovanni Alessio commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Maria Oliva Grassi, Pasquale Viggiano, Enrico Borrelli, Giacomo Boscia, Teresa Molfetta, Maria Giovanna Malerba, Maria D’Addario, Ermete Giancipoli, Giovanni Alessio, and Francesco Boscia have nothing to disclose.
Ethical Approval
The study adhered to the principles outlined in the Declaration of Helsinki. This study is retrospective in nature, and in accordance with Italian regulations, ethical approval is not necessary for such studies. Instead, only notification to the ethics committee is required. Therefore, the institutional review board was notified. Written consent was obtained from all participants included in the study, allowing for the retrospective use of their clinical data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Grassi, M.O., Viggiano, P., Borrelli, E. et al. Comparative Study on Anti-VEGF in Wet Age-Related Macular Degeneration in the Setting Based on Lean Methodology from the Bari Intravitreal Injection Registry (BIVIR). Ophthalmol Ther (2024). https://doi.org/10.1007/s40123-024-00927-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40123-024-00927-w