Abstract
Introduction
This study analysed the causative factors and clinical characteristics of acute and chronic ocular sequelae of Stevens–Johnson syndrome and toxic epidermal necrolysis (SJS/TEN) treated at a large third-referral centre in a developed country (Hungary) over a 15-year period.
Methods
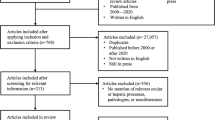
This was a retrospective review of patients with acute and/or chronic SJS/TEN who were managed between 2006 and 2020 at the Department of Ophthalmology of Semmelweis University in Budapest, Hungary. For each subject, clinical data, including patient demographics, clinical history, causative agents of SJS/TEN, and conservative and surgical treatment details, were reviewed.
Results
Ninety-six eyes of 48 patients were included (28 female; 58.3%); the age at disease onset was 32.1 ± 22.4 years. The most common causative factors were medicines (n = 36; 75.0%). Among these drugs, 29.2% were nonsteroidal anti-inflammatory drugs (NSAIDs) (n = 14), 20.8% were antibiotics (n = 10) and 14.6% were antiepileptic drugs (n = 7). In patients with chronic SJS/TEN, the most commonly found ocular sequelae were conjunctival hyperaemia in 45 (56.3%) eyes, symblepharon in 38 (47.5%) eyes, trichiasis/distichiasis in 37 (46.3%) eyes, corneal neovascularization in 31 (38.8%) eyes and corneal scarring in 29 (36.3%) eyes. In patients with chronic SJS/TEN, the most frequently used topical conservative treatment included antibiotics in 53 (66.3%) eyes, preservative-free artificial tears in 50 (62.5%) eyes and topical corticosteroids in 42 (52.5%) eyes of 40 patients. The most frequently performed ocular surgeries for managing chronic ocular sequelae in patients with SJS/TEN were epilation for trichiasis (n = 27; 33.8%), cataract surgery (n = 14; 17.5%), entropion surgery (n = 12; 15.0%), penetrating keratoplasty (PK) (n = 11; 13.8%) and amniotic membrane transplantation (n = 4; 5.0%).
Conclusion
Our results suggest that NSAIDs, antibiotics and antiepileptic drugs are the most common causative factors for SJS/TEN in Hungary. Like in other countries, in Hungary, the ocular management of patients with acute and chronic SJS/TEN is heterogeneous, and most cases do not follow modern therapeutic guidelines.
Similar content being viewed by others
Nonsteroidal anti-inflammatory drugs, antibiotics and antiepileptic drugs represent the most common causative factors of Stevens–Johnson syndrome and toxic epidermal necrolysis in Hungary. |
However, studies are needed to determine which SJS/TEN grading system is most suitable for estimating the prognosis and clinical course of these rare diseases. |
Penetrating keratoplasty alone is not a curative procedure for people with severe limbal stem cell deficiency in chronic SJS/TEN. |
Timely surgical interventions, such as removal of inflammatory debris and amniotic membrane transplantation as a patch, combined with the use of conformers, symblepharon rings or ProKera within the first 10 days in the acute stage, are essential to avoid chronic ocular sequelae of SJS/TEN. |
Introduction
Stevens–Johnson syndrome (SJS) and its severe form, toxic epidermal necrolysis (TEN), constitute a spectrum of diseases that are life-threatening immunologic dermatological disorders affecting the skin and mucous membranes [1]. The incidence of SJS/TEN is reported to be 0.93–12.35 per million people [2]. Although SJS and TEN are rare, they are associated with high morbidity and mortality rates. Ocular surface abnormalities are observed in more than 88% of patients during the acute phase [3]. SJS/TEN are characterized by epidermal necrolysis and sloughing, accompanied by active inflammation of the ocular surface, leading to excessive epidermal and keratinocyte necrosis [2].
Chronic ocular complications develop in approximately 30–90% of patients with acute SJS/TEN and include entropion/ectropion, trichiasis, lid margin keratinization, meibomian gland destruction, conjunctival scarring, symblepharon and severe dry eye. Microtrauma caused by eyelid anomalies leads to corneal neovascularization, limbal stem cell deficiency, persistent epithelial defects, conjunctivalization, keratinization, scarring, ulceration and sometimes corneal perforation [4].
The main causative agents of SJS/TEN are systemic medications, infections and vaccines, with patterns that vary worldwide [1, 5]. As a result of the rarity of SJS/TEN, only a few studies are available on the causes and ocular complications of SJS/TEN [6,7,8,9,10,11,12,13,14,15,16].
The aim of this study was to provide a comprehensive review of the causative factors and clinical characteristics of patients with acute and chronic ophthalmic sequelae of SJS/TEN at a tertiary eyecare centre in a developed country (Hungary).
Methods
The present study was approved by the Regional and Institutional Committee of Science and Research Ethics of Semmelweis University, Hungary (number 242/2020) and was performed in accordance with the Declaration of Helsinki Guidelines for Human Research and its later amendments.
This retrospective study was undertaken to analyse the demographic and clinical characteristics of patients with acute and/or chronic ocular sequelae of SJS/TEN between January 2006 and December 2020 at a tertiary eyecare centre in the Department of Ophthalmology of Semmelweis University in Budapest, Hungary.
The diagnosis of SJS/TEN was based on dermatological examination. SJS/TEN was defined on the basis of the affected total body surface area (BSA): SJS with less than 20% BSA and TEN with greater than 20% BSA involvement [2]. During the 15-year study period, 96 eyes of 48 patients were examined at our clinic with a diagnosis of acute or chronic SJS/TEN; 20 (41.7%) were male, and 28 (58.3%) were female, with a mean age of 43.7 ± 21.3 years (range 2–81 years) at first attendance at the tertiary eyecare centre. There were 27 patients (54 eyes) with SJS (56.2%) and 21 patients (42 eyes) with TEN (43.8%).
For each subject, clinical data, including patient demographics, causative agents, age of onset, time between onset of SJS/TEN and first visit at our clinic, clinical history, ocular involvement, administered topical therapies, operative details, length of follow-up, age and best corrected visual acuity (BCVA; Snellen chart values were converted to logMAR format) at the first visit and at last follow-up at the Department of Ophthalmology of Semmelweis University, were reviewed. The classification of visual impairment was performed in accordance with the International Classification of Diseases (ICD-10) and the revision proposed by the World Health Organization: blindness referred to a BCVA worse than 1.3 log MAR.
Statistical analysis was performed using Statistica 11.0 (StatSoft, Inc., Tulsa, OK, USA). The data are expressed herein as the mean ± standard deviation (SD). The chi-square test was used to compare proportions of categorical variables. For numeric variables, the Mann–Whitney U test was used to compare the SJS and TEN groups. To compare the BCVA values between the first visit and the last examination at the clinic, the nonparametric Wilcoxon test was used. A p value lower than 0.05 was considered to indicate statistical significance.
Results
The descriptive characteristics of the included subjects are shown in Table 1. None of the summarized descriptive parameters differed significantly between patients with SJS and TEN (p ≥ 0.30). In 10 (20.8%) patients, both eyes had logMAR BCVA values worse than 1.3, indicating blindness at the first visit at our clinic. The BCVA values at the first visit and at the last examination were 0.73 ± 0.89 (range 3.00–0.00) and 0.89 ± 1.03 (range 3.00–0.00) logMAR in the complete study population (SJS/TEN) (p = 0.11); 0.77 ± 0.92 (range 3.00–0.00) vs. 0.99 ± 1.09 (range 3.00–0.00) logMAR in SJS (p = 0.92); and 0.67 ± 0.85 (range 2.30–0.00) vs. 0.75 ± 0.93 (3.00–0.00) logMAR in TEN (p = 0.012).
The causative agents were described in a total of 36 (75.0%) cases (Table 2). The most common causative drugs were nonsteroidal anti-inflammatory drugs (NSAIDs) (29.2%; n = 14), antibiotics (20.8%; n = 10) and antiepileptic drugs (14.6%; n = 7). Allopurinol was a causative agent of TEN in 4 (19.0%) subjects; nevertheless, the use of allopurinol did not trigger SJS in any of the analysed subjects.
A total of 12 people (25.0%) were examined in the acute stage of SJS/TEN. Eight eyes of 4 patients (8.3%) treated in both the acute and chronic stages of SJS/TEN at our clinic. Sixteen eyes of 8 patients (16.6%) were examined only at the acute stage and were lost to follow-up for the chronic stage; thus, 80 eyes of 40 patients were examined in the chronic stage of SJS/TEN at Semmelweis University.
Among the 12 patients examined in the acute phase, 24 eyes (100%) had ocular complications due to acute SJS/TEN: 24 eyes (100%) had conjunctival hyperaemia, 8 (33.3%) had pseudomembrane development, 4 (16.7%) had corneal erosion and 4 (16.7%) had eyelid margin necrosis.
Patients in the acute stage of SJS/TEN received topical lubricating eye drops in 22 eyes (91.7%), tobramycin 3 mg/ml in 18 eyes (75.0%), dexamethasone 1 mg/ml in 10 eyes (41.7%), levofloxacin 5 mg/ml in 6 eyes (25.0%), fluorometholone 1 mg/ml in 4 eyes (16.7%) and rifampicin 5 mg/ml in 2 eyes (8.3%) of 12 patients. Regarding surgical procedures, 8 eyes (33.3%) of 4 patients underwent pseudomembrane removal.
Eighty eyes of 40 patients were examined in the chronic stage of SJS/TEN at our clinic; among them, 72 eyes (90.0%) of 35 patients had ocular involvement. The most common chronic ocular manifestations or sequelae were conjunctival hyperaemia in 45 (56.3%) eyes, symblepharon in 38 (47.5%) eyes, trichiasis/distichiasis in 37 (46.3%) eyes, corneal neovascularization in 31 (38.8%) eyes, corneal scars in 29 (36.3%) eyes, dry eye disease in 27 (33.8%) eyes, meibomian gland dysfunction in 26 (32.5%) eyes, entropion in 13 (16.3%) eyes, lid margin or ocular surface keratinization in 12 (15.0%) eyes and superficial punctate keratopathy in 11 (13.8%) eyes of the included 80 eyes (Table 3). Conjunctival hyperaemia was documented more often in patients with SJS than in patients with TEN (p = 0.01).
In patients with chronic SJS/TEN, the most frequently used topical conservative treatment included antibiotics in 53 eyes (66.3%), preservative-free artificial tears in 50 (62.5%) eyes and topical corticosteroids in 42 (52.5%) eyes of 40 patients. Moreover, the most often administered topical antibiotics and corticosteroids were tobramycin (3 mg/ml) (n = 37; 46.3%) and dexamethasone (1 mg/ml) (n = 35; 43.8%) (Table 4). Artificial tears were applied more often in individuals with TEN than in individuals with SJS (p = 0.03). In cases of chronic SJS/TEN, 8 (20.0%) patients received systemic treatment in the form of systemic corticosteroids (n = 6; 15.0%), doxycycline (n = 4; 10.0%), azathioprine (n = 2; 5.0%) or mycophenolate mofetil (n = 1; 2.5%). Five patients (12.5%) did not receive any conservative topical or systemic treatment for chronic SJS/TEN.
In addition, 29 eyes (36.3%) of 18 patients (45.0%) with chronic SJS/TEN were treated with soft bandage contact lenses, 2 eyes (2.5%) of 1 patient (2.5%) were treated with a scleral contact lens and 1 eye (1.3%) of 1 patient (2.5%) was treated with moisture goggles.
The most frequently performed ocular surgeries for managing chronic ocular sequelae in patients with SJS/TEN were mechanical epilation/electrolysis for trichiasis in 27 eyes (33.8%), cataract surgery in 14 (17.5%) eyes, entropion surgery in 12 (15.0%) eyes, penetrating keratoplasty (PK) in 11 (13.8%) eyes, punctal plug insertion in 6 (7.5%) eyes, amniotic membrane transplantation in 4 (5.0%) eyes and keratoprosthesis implantation (KPro) in 4 (5.0%) eyes among 40 patients (Table 5). The frequency of different ophthalmic surgeries did not significantly differ between people with SJS and those with TEN (p ≥ 0.06).
Among the 8 patients (20.0%) who underwent corneal transplantation, 1 eye (1.3%) had 5, 1 (1.3%) eye had 4, 1 (1.3%) eye had 3, 2 (2.5%) eyes had 2 and 6 (7.5%) eyes had 1 PK procedure. Three people (7.5%) had PK performed on both eyes. In total, 33 (41.3%) eyes of 21 (52.5%) patients underwent no ocular surgery for chronic SJS/TEN.
Among people with acute and chronic SJS/TEN, the most commonly coexisting systemic diseases included hypertension (n = 8; 16.7%), cardiac disease (n = 5; 10.4%) and diabetes mellitus (n = 3; 6.3%) (see Table S1 in the electronic Supplementary Materials for more details). Additionally, 3 patients (6.3%) had an autoimmune disease. The percentage of patients with different systemic diseases did not significantly differ between those with SJS and those with TEN (p ≥ 0.25).
Discussion
SJS/TEN are rare diseases; nevertheless, there are no accurate population-based data on their prevalence. End-stage SJS/TEN often results in corneal blindness, which seriously impairs quality of life. Therefore, it is important to obtain a better understanding of its pathogenesis and treatment options to avoid potential ocular complications as much as possible [2].
We analysed the demographic, aetiological and clinical details of people with ocular complications of SJS/TEN over a 15-year period at a tertiary eyecare centre in Hungary. To the best of our knowledge, this is the first study to report on the causative agents and clinical characteristics of patients with acute and chronic ophthalmic sequelae of SJS/TEN in detail in Hungary. Although there is a single study from the UK [11] reporting on ophthalmic signs in patients with SJS/TEN, it does not include detailed information regarding the causative factors or clinical characteristics of patients with SJS/TEN.
In our sample, the mean age of SJS/TEN onset was 32.1 years, which was lower than that reported in China (45.8 years) [9] but higher than that reported in Japan (21.5 years) [10], the UK (24.9 years) [11] and India (28.2 years) [8].
Like China (54.5%) [9], India (55.0%) [8, 12], Japan (63.6%) [10], Thailand (61.8%) [7] and the UK (61.9%) [15], our sample (58.3%) showed a female predominance in people with SJS/TEN. This may be explained by the fact that autoimmune diseases appear with a higher incidence among women than among men, and SJS/TEN is thought to be associated with changes in the innate immune system. The X chromosome contains 15 times more genes than the Y chromosome and possesses more immunoregulatory genes [17]. Therefore, the greater number of immune-related genes on the X chromosome increases the risk of mutations. Moreover, the presence of two X chromosomes further enhances the risk of autoimmune diseases among women [18]. Nevertheless, the most important genetic risk factors for the most common systemic autoimmune diseases (rheumatoid arthritis and systemic lupus erythematosus) are attributed to human leukocyte antigen (HLA) alleles [19, 20]. Moreover, the risk of SJS/TEN is greater in people with autoimmune diseases and diabetes mellitus [21]. In our sample, 6.3% of the patients had an autoimmune disease, and 6.3% has been diagnosed with diabetes mellitus.
The mean time between first symptoms and presentation at the tertiary eye care centre at Semmelweis University (11.9 years) was longer than that in the UK (3 years) [13] and shorter than that in Japan (15 years) [10]. Nevertheless, the time range between first symptoms and presentation at a tertiary eye care centre in Budapest (0–56 years) was similar to that in Japan (1–59 years) [10] but broader than that in India (0–18 years) [12].
Similar to the findings of our survey, all available previous reports revealed that medicines are the most common causative factors for SJS/TEN [5, 14, 22,23,24]. In the present study, the most common causative drugs were NSAIDS (29.2%), antibiotics (20.8%) and antiepileptic drugs (14.6%). Interestingly, in our study, NSAIDS were the most common causative factor for SJS/TEN. Previous studies have reported antibiotics as the primary causative factors, followed by NSAIDS and antiepileptic drugs. Jabbour et al. in the UK (48.0%) [11], Patel et al. in India (37.2%) [5], Jongkhajornpong et al. in Thailand (28.1%) [7] and Gueudry et al. in France (26%) [14] reported that antibiotics were the drugs that most commonly caused SJS/TEN. In contrast, Ganekal and Nagarajappa reported in India [8] that antiepileptic drugs were the most common cause of SJS/TEN. NSAIDS may be the leading aetiological factor for SJS/TEN in Hungary, as the NSAID use rate is significantly greater in developed countries than in developing countries [25]. Carbamazepine was reported to be the most common causative antiepileptic drug, and sulfonamides were the most common causative antibiotics in India (18.2% and 6.1%) [8] and Thailand (6.7% and 8.9%) [7]. Similar results were observed in our series, with 6.3% for carbamazepine, 6.3% for lamotrigine and 10.5% for sulfonamides. Carbamazepine is commonly prescribed for both psychiatric and neurological diseases [26]. Moreover, carbamazepine-induced SJS/TEN is strongly associated with the HLA-B*1508, HLA-B*1511, HLA-B*1518, HLA-B*3101 and HLA-B*12 genotypes, which play important roles in sulfonamide-induced SJS/TEN [2]. Lamotrigine-induced SJS/TEN is reported to cause severe ocular complications and visual impairment [16]. Nevertheless, regional differences in causative factors may also be attributed to varying patterns of medication use.
In the acute stage, patients with SJS/TEN often do not receive appropriate eye care. In this stage, there is more focus on intensive systemic patient care and on saving the patients’ lives [27]. This is also well supported by the fact that the grading of ocular sequelae of acute SJS/TEN could not be performed in our retrospective study because of the lack of documentation. In addition, people in the acute phase in our sample underwent solely bedside examinations at the department of dermatology of our university using a direct ophthalmoscope. However, careful examination and adequate aggressive ophthalmic management in the acute stage are essential to prevent chronic SJS/TEN complications [28]. Remarkably, in our sample, no patient underwent amniotic membrane transplantation or received a conformer, symblepharon ring or ProKera in the acute stage of the disease. Nevertheless, 33.3% of the eyes underwent bedside pseudomembrane removal. The topical therapeutic regimen in the acute phase typically includes lubricants, antibiotics and corticosteroids [2].
There are no exact European data on ocular manifestations of chronic SJS/TEN. In 2021, a British study by Jabbour et al. [11] reported only the raw data of chronic SJS/TEN ocular complications as supplementary material for their publication. In addition, as a result of differences in methodologies, comparisons between the results of different surveys are not easy. Chow et al. (China) [9], Rashad et al. (USA) [16] and Yoshikawa et al. (Japan) [10] used solely Sotozono’s grading system [29], and Ganekal and Nagarajappa (India) [8] used a modified Sotozono’s classification system. In contrast, Basu et al. (India) [30], Iyer et al. (India) [31], Jabbour et al. (UK) [11] and Jongkhajornpong et al. (Thailand) [7] processed their data in four different grading systems.
Chronic ocular complications in patients with SJS/TEN are unpredictable and are poorly correlated with acute SJS/TEN [32]; however, the severity of acute SJS/TEN is the best predictor of chronic eye complications [2]. Similar to Jongkhajornpong et al. from Thailand (56.8%) [7] and Iyer et al. from India (26.5%) [31], we found corneal neovascularization (38.8%) and lid margin keratinization (15.0%) to be among the most common chronic ocular complications.
Gueudry et al. observed ocular surface dryness, superficial punctate keratopathy, trichiasis/distichiasis and symblepharon among the most frequent chronic sequelae of SJS/TEN in France [14]. Nevertheless, other chronic ocular complications in our study population were not comparable with those described in previous studies. Timely performed surgical interventions, such as removal of inflammatory debris and amniotic membrane transplantation as a patch combined with conformer, symblepharon ring or ProKera use within the first 10 days in the acute stage, are essential for avoiding chronic ocular sequelae, such as symblepharon, trichiasis/distichiasis, corneal neovascularization, lid margin keratinization, corneal scarring, persistent/recurrent corneal epithelial defects, corneal ulcers and perforation, which were the most frequent in our sample [28].
Surgical procedures for patients with chronic SJS/TEN are performed only if inevitably necessary. Eyelid surgery, autologous cultivated oral mucosal epithelial transplantation, amniotic membrane transplantation and limbo-keratoplasty are general surgical interventions for people with severe chronic ocular sequelae of SJS/TEN [2]. Eye care in patients in the chronic stage of SJS/TEN also differs from the established guidelines [1]. In this study, no patient (0%) bore a PROSE (prosthetic replacement of the ocular surface ecosystem) lens, only 1 (2.5%) subject received a scleral contact lens and no patient (0%) underwent limbal stem cell transplantation or autologous cultivated oral mucosal epithelial transplantation in the long term. Nevertheless, 3.8% of the eyes underwent oral mucosal transplantation, and 45.0% of the patients with chronic SJS/TEN bore soft bandage contact lenses. Soft contact lenses do not assure enough fluid fills the space between the corneal surface and the contact lens in SJS/TEN [33]. Nevertheless, PROSE and scleral contact lenses are hardly available in Hungary. As a result of their high costs and difficulties in organizing financial support for their purchases, these options were barely used in our sample. Nevertheless, as lid margin keratinization is the most important causative risk factor for ocular surface damage and limbal stem cell deficiency in chronic SJS/TEN [34], scleral contact lenses or PROSE lenses are the most appropriate therapeutic solutions for patients with SJS/TEN [31].
In the UK, 49.5% of patients with chronic ocular sequelae of SJS/TEN had bare rigid gas-permeable or scleral contact lenses [11]. Moreover, Basu et al. reported that the use of a PROSE lens combined with oral mucosal transplantation has an even more beneficial effect and favourable synergistic effect on chronic SJS/TEN, as these conditions arrest corneal damage and improve vision [30].
In the entire sample, 13.8% of the patients underwent PK (1 eye had 5, 1 had 4, 1 had 3, and 2 had 2 PKs). PK may help in urgent situations such as corneal perforation or ulceration [33] but is not suitable for SJS/TEN treatment alone, as PK alone does not facilitate regeneration of corneal epithelial stem cells. Appropriate surgical management also includes limbal stem cell transplantation [1, 2]. In the UK, 80.2% of the patients with chronic SJS/TEN underwent lid surgery, 18.7% underwent amniotic membrane transplantation and 13.2% underwent PK/KPro surgery. These procedures were performed at lower rates in our sample (51.3%, 5.0% and 13.8%) [11].
Limitations of our study include the following: Only a small proportion of patients were examined in the acute stage, and acute ocular complications were not adequately classified using the Gregory [35] grading system. As many patients were referred to the Department of Ophthalmology of Semmelweis University only in the chronic phase, as a result of incomplete documentation, the complete course of all the cases, for example, the development of ocular surface scarring, could not be analysed. Therefore, and as a result of the retrospective nature of the study, grading of chronic ocular sequelae of SJS/TEN could also not be performed using either the Sotozono [29] or Sharma [36] classifications for the analysed subjects.
Conclusion
Our results suggest that NSAIDs, antibiotics and antiepileptic drugs are the most common causative agents of SJS/TEN in Hungary. In most cases, the ocular management of patients with acute and chronic SJS/TEN did not follow the actual suggested treatment modalities during the analysed time period. Prospective studies with larger sample sizes and the use of proper classification systems in daily clinical practice are necessary to facilitate comparisons between countries and eyecare centres and to enable better treatment of the involved subjects.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Jain R, Sharma N, Basu S, et al. Stevens-Johnson syndrome: the role of an ophthalmologist. Surv Ophthalmol. 2016;61:369–99.
Tóth G, Lukács A, Schirra F, et al. Ophthalmic aspects of Stevens-Johnson ayndrome and toxic epidermal necrolysis: a narrative review. Ophthalmol Ther. 2023;12:1795–811.
Panpruk R, Puangsricharern V, Klaewsongkram J, et al. Clinical parameters and biological markers associated with acute severe ocular complications in Stevens-Johnson syndrome and toxic epidermal necrolysis. Sci Rep. 2021;11:20275.
Chronopoulos A, Mockenhaupt M, Pleyer U. Ocular involvement in Stevens-Johnson syndrome and toxic epidermal necrolysis. Ophthalmologe. 2021;118:519–32.
Patel TK, Barvaliya MJ, Sharma D, Tripathi C. A systematic review of the drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in Indian population. Indian J Dermatol Venereol Leprol. 2013;79:389–98.
Chow LLW, Shih KC, Chan JCY, Lai JSM, Ng ALK. Comparison of the acute ocular manifestations of Stevens-Johnson syndrome and toxic epidermal necrolysis in Chinese eyes: a 15-year retrospective study. BMC Ophthalmol. 2017;17:65.
Jongkhajornpong P, Lekhanont K, Siriyotha S, Kanokrungsee S, Chuckpaiwong V. Factors contributing to long-term severe visual impairment in Stevens-Johnson syndrome and toxic epidermal necrolysis. J Ophthalmol. 2017;2017:2087578.
Ganekal S, Nagarajappa A. Acute and chronic ophthalmic involvement, severity, and sequelae in Stevens-Johnson syndrome and toxic epidermal necrolysis. Korean J Ophthalmol. 2021;35:179–87.
Chow LLW, Ng ALK, Chow SSW, et al. A cross-sectional comparative study on chronic ocular manifestations of Stevens-Johnson syndrome and toxic epidermal necrolysis in Chinese eyes: a 15-year case series. Int Ophthalmol. 2018;38:1155–60.
Yoshikawa Y, Ueta M, Fukuoka H, et al. Long-term progression of ocular surface disease in Stevens-Johnson syndrome and toxic epidermal necrolysis. Cornea. 2020;39:745–53.
Jabbour S, Din N, Logeswaran A, Sanchez ST, Ahmad S. Clinical characteristics of patients with chronic Stevens-Johnson syndrome treated at a major tertiary eye hospital within the United Kingdom. Front Med. 2021;8: 644795.
Kompella VB, Sangwan VS, Bansal AK, Garg P, Aasuri MK, Rao GN. Ophthalmic complications and management of Stevens-Johnson syndrome at a tertiary eye care centre in South India. Indian J Ophthalmol. 2002;50:283–6.
De Rojas MV, Dart JKG, Saw VPJ. The natural history of Stevens Johnson syndrome: patterns of chronic ocular disease and the role of systemic immunosuppressive therapy. Br J Ophthalmol. 2007;c91:1048–53.
Gueudry J, Roujeau J-C, Binaghi M, Soubrane G, Muraine M. Risk factors for the development of ocular complications of Stevens-Johnson syndrome and toxic epidermal necrolysis. Arch Dermatol. 2009;145:157–62.
Rajaratnam R, Mann C, Balasubramaniam P, et al. Toxic epidermal necrolysis: retrospective analysis of 21 consecutive cases managed at a tertiary centre. Clin Expert Dermatol. 2010;35:853–62.
Rashad R, Shanbhag SS, Kwan J, Chodosh J, Saeed S, Saeed HN. Chronic ocular complications in lamotrigine vs. trimethoprim-sulfamethoxazole induced Stevens-Johnson syndrome/toxic epidermal necrolysis. Ocul Surf. 2021;21:16–8.
Schurz H, Salie M, Tromp G, Hoal E, Kinnear CJ, Möller M. The X chromosome and sex- specific effects in infectious disease susceptibility. Hum Genomics. 2019;13:2.
Angum F, Khan T, Kaler J, Siddiqui L, Hussain A. The prevalence of autoimmune disorders in women: a narrative review. Cureus. 2020;12:e8094.
Kurko J, Besenyei T, Laki J, Glant TT, Mikecz K, Szekanecz Z. Genetics of rheumatoid arthritis—a comprehensive review. Clin Rew Allergy Immunol. 2013;45:170–9.
Cui Y, Sheng Y, Zhang X. Genetic susceptibility to SLE: recent progress from GWAS. J Autoimmun. 2013;41:25–33.
Ubukata N, Nakatani E, Hashizume H, Sasaki H, Miyachi Y. Risk factors and drugs that trigger the onset of Stevens–Johnson syndrome and toxic epidermal necrolysis: a population-based cohort study using the Shizuoka Kokuho database. JAAD Int. 2022;11:24–32.
Frantz R, Huang S, Are A, Motaparthi K. Stevens-Johnson syndrome and toxic epidermal necrolysis: a review of diagnosis and management. Medicina. 2021;57:895.
Shanbhag SS, Sangwan VS, Singh A, et al. Clinical aspects of Stevens-Johnson syndrome/toxic epidermal necrolysis with severe ocular complications in India. Front Med (Lausanne). 2021;8:643955.
Imatoh T, Saito Y. Associations between Stevens-Johnson syndrome and infection: overview of pharmacoepidemiological studies. Front Med (Lausanne). 2021;8:644871.
Xie X, Ren K, Zhou Z, Dang C, Zhang H. The global, regional and national burden of peptic ulcer disease from 1990 to 2019: a population-based study. BMC Gastroenterol. 2022;22:58.
James J, Sushma M, Guido S, Elizabeth J. Cutaneous adverse drug reactions in a South Indian tertiary care center. Indian J Dermatol. 2005;50:17–21.
Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011;7:803–15.
Shanbhag SS, Hall L, Chodosh J, Saeed HN. Long-term outcomes of amniotic membrane treatment in acute Stevens-Johnson syndrome/toxic epidermal necrolysis. Ocul Surf. 2020;18:517–22.
Sotozono C, Ang LPK, Koizumi N, et al. New grading system for the evaluation of chronic ocular manifestations in patients with Stevens-Johnson syndrome. Ophthalmology. 2007;114:1294–302.
Basu S, Shanbhag SS, Gokani A, Kedar R, Bahuguna C, Sangwan VS. Chronic ocular sequelae of Stevens-Johnson syndrome in children: long-term impact of appropriate therapy on natural history of disease. Am J Ophthalmol. 2018;189:17–28.
Iyer G, Srinivasan B, Agrawal S, Pillai VS, Ahuja A. Treatment modalities and clinical outcomes in ocular sequelae of Stevens-Johnson syndrome over 25 years—a paradigm shift. Cornea. 2016;35:46–50.
Chang VS, Chodosh J, Papaliodis GN. Chronic ocular complications of Stevens-Johnson syndrome and toxic epidermal necrolysis: the role of systemic immunomodulatory therapy. Semin Ophthalmol. 2016;31:178–87.
Saeed HN, Chodosh J. Ocular manifestations of Stevens-Johnson syndrome and their management. Curr Opin Ophthalmol. 2016;27:522–9.
Sing S, Jakati S, Shanbhag SS, Elhusseiny AM, Djalilian AR, Basu S. Lid margin keratinization in Stevens-Johnson syndrome: review of pathophysiology and histopathology. Ocul Surf. 2021;21:299–305.
Gregory DG. New grading system and treatment guidelines for the acute ocular manifestations of Stevens-Johnson syndrome. Ophthalmology. 2016;123:1653–8.
Sharma N, Venugopal R, Maharana PK, et al. Multistep grading system for evaluation of chronic ocular sequelae in patients with Stevens-Johnson syndrome. Am J Ophthalmol. 2019;203:69–77.
Medical Writing/Editorial Assistance.
Springer Nature English Language Editing Service provided professional language editing.
Funding
The work of Dr. Tóth at the Dr. Rolf M. Schwiete Center has been supported by the Eötvös Scholarship. The funding organization had no role in the conduct of this article. No funding or sponsorship was received for the publication of this article.
Author information
Authors and Affiliations
Contributions
Gábor Tóth designed and wrote the manuscript. Andrea Lukács, Tanja Stachon, Frank Schirra, Gábor László Sándor and Zoltán Zsolt Nagy collected the data and edited the manuscript. Nóra Szentmáry planned, designed and reviewed the manuscript. All authors agree with the final version of the manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The work of Gábor Tóth at the Dr. Rolf M. Schwiete Center has been supported by the Eötvös Scholarship and the work of Nóra Szentmáry and Tanja Stachon at the Dr. Rolf M. Schwiete Center has been supported by the Dr. Rolf M. Schwiete Foundation. Nóra Szentmáry is an Editorial Board member of Ophthalmology and Therapy and was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions. Gábor Tóth, Andrea Lukács, Tanja Stachon, Frank Schirra, Gábor László Sándor, Zoltán Zsolt Nagy and Nóra Szentmáry have no competing interests.
Ethical Approval
The study was approved by the Regional and Institutional Committee of Science and Research Ethics of Semmelweis University, Hungary (Number 242/2020). The study was performed in accordance with the Declaration of Helsinki Guidelines for Human Research and its later amendments.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tóth, G., Lukács, A., Stachon, T. et al. Clinical Characteristics and Treatment of Ophthalmic Sequelae of Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis at a Tertiary Eyecare Centre in Hungary. Ophthalmol Ther 13, 1343–1356 (2024). https://doi.org/10.1007/s40123-024-00924-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00924-z