Abstract
Introduction
This study aimed to assess the efficacy and safety of adalimumab in pediatric patients with chronic non-infectious posterior uveitis and panuveitis (not associated with juvenile idiopathic arthritis).
Methods
The medical records of children (< 18 years old) with chronic non-infectious posterior uveitis and panuveitis were collected and analyzed in this retrospective cohort study. Children were allocated to a conventional adalimumab-free treatment (CT) or adalimumab (ADA) group based on whether they additionally received adalimumab.
Results
In total, 69 children (138 eyes) were included, with 21 (42 eyes) and 48 (96 eyes) in the CT and ADA groups, respectively. During the average follow-up period of 24 months, the improvement in all ocular parameters (best-corrected visual acuity, intraocular inflammation, fluorescein angiography score) was better in the ADA group than in the CT group, except for changes in central macular thickness, which did not significantly differ between the groups. The mean time of first alleviation, which was after 1.03 ± 0.12 months of therapy, was earlier in the ADA group than in the CT group (2.30 ± 0.46 months). In the ADA group, 90.6% of children had remission within 3 months, and 47.9% had no relapse during follow-up. Cough and cold were the most common adverse events in the ADA group; however, the number of adverse events was similar between both the groups.
Conclusions
Adalimumab was effective in the treatment of chronic noninfectious posterior uveitis and panuveitis in pediatric patients, and disease inactivity was accomplished in the majority of the patients, thereby improving visual outcomes and maintaining disease stability. Adverse events were limited and tolerable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
To further strengthen and enlarge evidence on the effectiveness of adalimumab in pediatric patients with chronic non-infectious posterior uveitis and panuveitis. |
What was learned from the study? |
Adalimumab was efficacious and tolerated in reducing ocular inflammation, especially in the retina, and significantly improved long-term visual acuity in pediatric patients with chronic non-infectious posterior uveitis and panuveitis. |
Adalimumab demonstrated limited superiority over conventional adalimumab-free treatment in terms of reducing macular edema in pediatric patients with non-infectious posterior uveitis and panuveitis. |
Although it took a few weeks to regulate inflammation, adalimumab assured a high response rate of remission and long-term remission stability in pediatric patients with non-infectious posterior uveitis and panuveitis. |
Introduction
Pediatric uveitis is a severe inflammatory eye disease that results in vision loss in one-third of patients, eventually leading to permanent blindness [1]. More severe complications in idiopathic pediatric uveitis require special considerations [2]. The most commonly identified cause of pediatric uveitis is juvenile idiopathic arthritis (JIA), presenting mostly as anterior uveitis. However, few studies have focused on non-JIA uveitis [3, 4]; moreover, research on improving treatment options for pediatric posterior uveitis or panuveitis is lacking, which is often chronic, persistent, and threatens vision.
The goal of pediatric uveitis treatment is controlling inflammation and achieving stable remission [5]. Topical, peribulbar, or systemic corticosteroids are used as a first-line treatment, usually combined with immunomodulatory agents (IMTs), such as methotrexate, azathioprine, cyclosporine, and mycophenolate mofetil [6]. However, this can result in severe adverse effects not only concerning ocular conditions, such as cataracts and glaucoma, but also physical and mental health in children [5]. Randomized controlled trials (RCTs) have demonstrated the success of biological therapy for JIA-associated uveitis mostly in pediatric patients [7,8,9], and meta-analyses have investigated administering anti-tumor necrosis factor (TNF)-α drugs for childhood chronic uveitis [10, 11]. Therefore, switching to biotherapy in the early stages of uveitis has recently been considered.
Anti-TNF-α agents are the most widely used biotherapies for noninfectious uveitis (NIU). Among these, adalimumab (ADA) is the most effective [12] and has the advantage of less autoreactive antibodies and higher drug responses because its human monoclonal antibody acts against TNF-α [13, 14]. Since ADA was approved by the Food and Drug Administration (FDA) in 2018 as a second-line therapy for uveitis in children (> 2 years old), the evidence of its efficacy in pediatric uveitis has accumulated. ADA may represent a valid alternative in children with anterior refractory uveitis, with similar efficacy for JIA, idiopathic uveitis, and systemic disorders such as Behçet’s disease (BD) [15]. However, there is a paucity of research on the efficacy of ADA in pediatric uveitis involving posterior inflammation, characterized by few case studies and limited assessment methodologies. Therefore, we conducted this retrospective cohort study to assess the efficacy and safety of ADA in the treatment of chronic pediatric posterior uveitis and panuveitis compared to conventional ADA-free treatment (CT).
Methods
Patient Selection
This retrospective cohort study was conducted in pediatric patients with non-infectious uveitis treated at the Zhongshan Ophthalmic Center between March 2019 and September 2022 (Fig. 1). This study was performed according to the principles of the Declaration of Helsinki and was approved by the ethics committee of the Zhongshan Ophthalmic Center (No. 2019058). Written informed consent was obtained from each patient and/or their caregivers. Before treatment, patients were screened for tuberculosis, syphilis, and hepatitis.
The inclusion criteria were: (1) an onset of non-infectious uveitis before 18 years of age; (2) diagnosis by uveitis-trained ophthalmologists according to the Standardization of Uveitis Nomenclature working group guidelines for posterior uveitis or panuveitis [16]: inflammation observed in the retina combined with or without inflammation in the anterior chamber, vitreous, or choroid, including retinitis, retinal vasculitis, or papillitis; (3) no previous use of biological agents, especially anti-TNF-α drugs; and (4) regular follow-ups for at least 12 months after treatment. Patients with associated systemic disease, diabetes, ocular infection, trauma, or retinitis pigmentosa were excluded.
Drug Use and Follow-up
The patients were assigned to two groups (ADA and CT) according to whether they additionally received adalimumab. Apart from the conventional treatment, the ADA group received a double dose of ADA (HUMIRA; AbbVie Inc., North Chicago, IL, USA) for the first time at the initial treatment. One week after the first injection, 40-mg doses were administered by subcutaneous injection every other week, and the dose was halved in children weighing ≤ 30 kg. The interval could be prolonged in patients who remained stable for 1 year with no active inflammation confirmed upon slit-lamp examination. Relapse was suppressed by repeated injections of a double dose of ADA.
In the CT group, as in the basic treatment in the ADA group, patients were administered oral glucocorticoids (GC) at baseline (1–2 mg/kg/day) and all patients underwent a mandatory GC taper upon decreased intraocular inflammation starting in week 2. Repeated high doses of systemic oral GC followed by slow tapering suppressed rebound inflammation in relapsed patients. Supplemental periocular steroid injections could be administered to treat critical anterior and posterior segment inflammation.
Clinical visits were scheduled at screening, baseline (biological therapy initiation), at weeks 1, 2, and 4, and approximately every 4 weeks thereafter; visits were conducted every 2 weeks for patients in an active phase or relapse. ADA was discontinued in the ADA group or biological therapy was initiated in the CT group in the case of frequent recurrence of anterior chamber inflammation or massive retinal leakage (fluorescein angiography [FA]) or the appearance of systemic adverse events.
Data Collection
The standard tests included best-corrected visual acuity (BCVA), intraocular inflammation, specialty ocular examination for central macular thickness (CMT), and posterior inflammation scores, as assessed with FA at the beginning of ADA as the baseline and subsequently monthly standard tests, such as 3-months ocular coherence tomography (OCT) and 6-months FA after starting ADA. Moreover, information on the number of relapses, IMT reduction, GC-sparing effects, and systemic disorders were retrospectively collected and analyzed. The details are as follows:
-
Visual acuity: The logarithm of the minimum angle of resolution (logMAR) was used to assess BCVA. The “counting finger/hand motion/light perception” was converted to a quantified visual acuity value [17].
-
Intraocular inflammation: The Nussenblatt scale and Standardization of Uveitis Nomenclature Working Group schema were used to assess the degree of vitritis and anterior chamber inflammation, respectively [16]. The definition of alleviation of inflammation included patients who achieved either complete absence of inflammation or ≥ 2-step decrease in inflammation (anterior chamber score and vitreous haze score) or slight remnants (0.5 + anterior chamber cells). Relapse of uveitis was defined as a new flare or aggravation of uveitis, including a two-step increase in the inflammation level of anterior chamber cells and/or vitreous haze or an increase from grade 3 + to 4 + , retinal vasculitis, optic disc, or macular edema.
-
CMT: CMT was defined as the average retinal thickness within a 1-mm-diameter region in the macular fovea measured using Cirrus High-Definition-OCT (Carl Zeiss AG, Jena, Germany).
-
FA scores of posterior inflammation: oral or intravenous FA examination was performed at baseline and every half year following ADA administration. Angiography Scoring for Uveitis Working Group scoring was used to assess posterior inflammation in FA images [18]. To minimize errors, FA scores were evaluated by two specialists (TTY and YSZ). In the case of a dispute, the final decision was made by the senior specialist SWR.
-
IMT reduction and GC-sparing effects: A corticosteroid-sparing effect was defined as complete withdrawal from systemic corticosteroid therapy while maintaining clinical stability.
-
Systemic disorder: Routine blood examinations and liver and renal function tests were performed every 2 months.
Statistical Analysis
Mean ± standard deviation and median (interquartile range) were used for continuous parameters and numbers (%) were used for categorical parameters. The Shapiro–Wilk test and histograms were used to assess the normality of continuous data. Normally distributed variables are reported as mean (standard deviation) and were compared using the Student’s t test, while non-normally distributed variables are summarized as median (interquartile range) and were compared using the Mann–Whitney U test. For categorical parameters, groups were compared using the chi-squared test or Fisher’s exact test. Survival curves were constructed using the Kaplan–Meier method. SPSS software 16.0 (NCSS, LLC, USA) was used for analysis. P values < 0.05 were considered statistically significant. All significance values were two-tailed.
Results
Patient Characteristics Before Treatment Initiation
In total, 69 patients (138 eyes) with chronic non-infectious posterior uveitis and panuveitis were included, with 21 (42 eyes) and 48 (96 eyes) patients in the CT and ADA groups, respectively. The baseline profiles were compared between the groups (Table 1). The mean age at initial treatment (CT 13.00 ± 3.69 years; ADA 12.23 ± 3.37 years; p = 0.398), and the mean age at diagnosis of uveitis (CT 12.76 ± 3.73 years; ADA 11.08 ± 3.32 years; p = 0.085) did not differ between groups. The sex ratio was similar (girls: boys; CT 16:5; ADA 29:19; p = 0.206). The refractive power in both the groups did not differ significantly (CT − 0.80 ± 3.58 D; ADA − 0.45 ± 1.20 D; p = 0.545). The time from disease onset to presentation differed between groups (CT 5.55 ± 8.07 months; ADA 12.57 ± 16.46 months; p = 0.074). The follow-up period did not differ between groups (CT 24.56 ± 12.48 months; ADA 25.64 ± 8.57 months; p = 0.677). The number of anatomic-type uveitis cases was similar in both groups (CT four posterior uveitis, 17 panuveitis; ADA eight posterior uveitis, 40 panuveitis; p = 1.000). The diagnoses included 14 cases of BD (66.7%), six NIU (28.6%), and one Vogt–Koyanagi–Harada disease (VKH) (4.8%) in the CT group, and 24 cases of BD (50.0%), 20 NIU (41.7%), and four VKH (8.3%) in the ADA group (p = 0.503).
Inflammation in the anterior chamber and vitreous humor at baseline were slightly more severe in the ADA group (Table 2). Fifteen affected eyes (35.7%) showed no active inflammation in the CT group, which was higher than in the ADA group (18 eyes [18.8%]; p = 0.032). Six affected eyes (15.8%) had no active inflammation in the CT group, which was higher than in the ADA group (three eyes [3.2%] p = 0.027). Other parameters (BCVA, CMT, FA scores) were similar at baseline in both groups.
Secondary ocular complications of uveitis before treatment included central band keratopathy (CT three eyes; ADA six eyes; p = 1.000), synechia (CT four eyes; ADA 22 eyes; p = 0.064), cataract (CT nine eyes; ADA 27 eyes; p = 0.410), and macular edema (CT 13 eyes; ADA 19 eyes; p = 0.255).
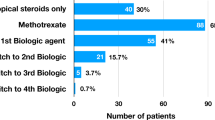
Table 3 shows the regimens and changes in IMTs in both groups. No significant difference was observed between the groups in the prescription of immunosuppressive agents, especially dosage of systemic GCs (CT 40 [21, 60] mg; ADA 55 [21.3, 60] mg; p = 0.935).
Improvement of Primary Outcomes
Inflammation, either in the anterior chamber or the vitreous humor, was present in every patient at the initiation of therapy. The primary and secondary outcomes of ocular inflammation during follow-up are shown in Table 4. BCVA improved by 0.0097 ± 0.47 (LogMAR) at the final visit compared with the baseline in the CT group, which was less than that in the ADA group (0.30 ± 0.47 LogMAR; p = 0.001). BCVA was better and more stable during follow-up in the ADA group (Fig. 2A). Alleviation of anterior chamber cellular flare was observed in 12 eyes in the CT group (44.4%) and in < 69 eyes in the ADA group (88.5%) (p < 0.001). Alleviation of vitreous humor cellular flares was observed in 14 eyes in the CT group (43.8%) and in < 85 eyes in the ADA group (92.4%) (p < 0.001). FA in the ADA group improved significantly more than in the CT group (mean reduction of FA: CT 7.09 ± 8.21; ADA 12.23 + 5.88; p = 0.002). The reduction in CMT and prevalence of macular edema improved in both groups, with no significant difference between groups (p = 0.291 and p = 0.058, respectively). Changes in OCT and FA values of a child with panuveitis are shown in Fig. 3.
Continuous changes in visual acuity and daily oral corticosteroid use during follow-up; A BCVA variations in children in both therapeutic groups; B daily GC dosage variations in children in both therapeutic groups. CT conventional treatment, ADA adalimumab, BCVA best-corrected visual acuity, GCs glucocorticoids
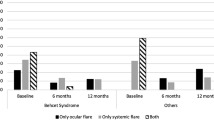
Alleviation, Relapse, and Systemic IMTs During Follow-up
Evident and typical responses to ocular inflammation occurred after 2.30 ± 0.46 months of therapy in the CT group and after 1.03 ± 0.12 months in the ADA group (p = 0.002). The rate of remission at 3 months was 90.6% (ADA) and 61.9% (CT) (p < 0.001; Table 4). The first alleviation was earlier in the ADA group after 3 weeks of initial treatment than in the CT group (log-rank = 0.002; Fig. 4A). The earliest time to response was 4 days in the CT group and 1 week in the ADA group. The time of first relapse after alleviation differed significantly between the groups. The median time to maintain alleviation was shorter in the CT group (3.20 [1.43, 7.08] months; ADA 9.70 [4.30, 14.50] months; p = 0.001; Fig. 4B). The number of relapses ranged from 0 to 9 in the CT group and from 0 to 4 in the ADA group (p < 0.001). The rate of patients without relapse was higher in the ADA group (46 eyes [47.9% of alleviated eyes]; CT four eyes [10.5% of alleviated eyes]; p < 0.001). All patients could progressively taper at least one of the other medications (Table 3). The median decreased dosage of GCs was similar in both groups (CT 30.0 mg [range, 13.5–57.5 mg]; ADA 50.0 mg [range, 20.0–60.0 mg]; p = 0.397), and the rate of GCs-free was slightly higher in the ADA group than in the CT group at the final visit; however, no significant difference was observed (25 patients [55.6%]; ADA six patients [30.0%]; p = 0.102). The changes in the systemic GCs are shown in Fig. 2B. During follow-up, all other treatments are not different, such as peribulbar injection (CT four eyes [19.0%]; ADA eight eyes [16.7%]; p = 1.000), intraocular injection (CT 0 eyes [0.0%]; ADA three eyes [6.3%]; p = 0.548), laser peripheral iridotomy (CT one eye [4.8%]; ADA one eye [2.1%]; p = 0.519).
First alleviation after initial treatment and first relapse after alleviation over time in both groups; A hazard ratio for first alleviation with adalimumab versus placebo was 1.79 (95% CI 1.21–2.64; p = 0.003); a crossover can be seen at about 3 weeks; B hazard ratio for first relapse after alleviation with adalimumab versus placebo was 0.46 (95% CI 0.29–0.71; p = 0.001). Dots indicate censored data. CT conventional treatment, ADA adalimumab, CI confidence interval, SD standard deviation
Adverse Events and Treatment Discontinuation
Thirty-three percent of patients in the CT group (n = 7) and 31.3% of patients in the ADA group (n = 15) had transient abnormal blood test results, including elevated liver function enzymes, leukopenia, and elevated white blood cells or platelets (p = 0.864). A total of 24 children experienced adverse events (CT seven patients; ADA 16 patients; p = 1.000). Of the adverse events in the ADA group, common cold (12.5%), nausea/vomiting (8.3%), rash/eczema (6.3%), fatigue (6.3%), growth retardation (4.2%), and weight fluctuation (2.1%) were reported in 6, 4, 3, 3, 2, and 1 case(s), respectively. No deaths, malignancies, demyelinating diseases, serious infections, or lupus-like reactions were observed during ADA treatment (Table 3).
ADA treatment was discontinued in 19 children in the ADA group, and 16 children switched to biologics in the CT group (39.6% vs. 76.2%, p = 0.005). Adverse events were cited as the reason for discontinuation in a significantly higher number of children treated with CT than in those treated with ADA (six [28.6%] vs. one [2.1%]; p < 0.001). No significant differences were observed between the groups in the number of patients who discontinued the main regimen for other reasons (CT vs. ADA: seven [33.3%] vs. nine [18.8%] due to recurrent inflammation, two [9.5%] vs. eight [16.7%] due to remission, one [4.8%] vs. one [2.1%] due to patient requests; Table 3).
Discussion
This retrospective cohort study investigated the efficacy of ADA in 48 children with chronic posterior uveitis and panuveitis, not associated with JIA, and compared it with 21 children treated with CT. To the best of our knowledge, this study has the highest number of cases dedicated exclusively to non-infectious pediatric posterior uveitis and panuveitis. It offers the distinct advantage of encompassing a well-defined control group, thereby enhancing the robustness of the study. In this study, during an average follow-up period of 24 months, improvement in all ocular parameters (BCVA, intraocular inflammation, FA score) was better in the ADA group than in the CT group, except for improvements in CMT, which did not differ between the groups. The mean time of first alleviation often occurred earlier in the ADA group than in the CT group. There were significantly fewer relapses and more GC-free patients in the ADA group at the final follow-up visit. Moreover, the number of adverse events was similar between the groups. Cough and cold were the most common adverse events observed in the ADA group.
Systemic JIA was one of the most common causes of pediatric uveitis and the only FDA-approved disease for which ADA could be administered in children before 2018, studies on the effectiveness of ADA have focused on pediatric anterior uveitis associated with JIA, such as the SYCAMORE and ADJUVITE RCTs [19, 20]. After ADA was approved for patients aged > 2 years with uveitis, a small number of studies further supported the use of ADA in children [3, 4, 21]. Deitch et al. [4] first studied the effects of anti-TNF-α agents on outcomes of pediatric uveitis of diverse types, including 20 (46.5%) cases of panuveitis. The rates of achievement of the inactive state and success were 23.3% and 46.5%, respectively, during 1 year of treatment with ADA or infliximab. Kouwenberg et al. [3] demonstrated that treatment with ADA led to prompt inactivity of non-JIA uveitis in the majority of children (90.6%), whereas this study included 15 (35%) and eight (18.6%) patients with anterior and intermediate uveitis, respectively. Another study that included the largest number of panuveitis cases (28 patients, 90%) demonstrated that anterior and posterior inflammation reached inactivity after 4 weeks in all cases [21]. Although these studies included children with varying anatomies and etiologies of uveitis, the results were consistent with our findings.
Our study demonstrated that ADA was effective in children with chronic posterior uveitis and panuveitis, with 90.6% attaining remission after 3 months, which was consistent with previous studies [3, 21] including anterior uveitis cases. In our study, 46 eyes achieved symptom alleviation without relapse during follow-up. This suggested that, within 9–43 months of follow-up, 52.9% of the patients achieving an early response maintained a persistent state of inactivity. This proportion was much higher than that reported in studies of chronic pediatric uveitis mostly with JIA, which reported a pooled response rate of 56.3–84.5% [9, 20, 22]. This could be attributed to the adequate use of concomitant immunosuppressants in our study, which may have reduced the production of anti-ADA antibodies and maintained the response to ADA [23]. Further, a higher probability of uveitis remission was observed in pediatric patients with chronic uveitis who used ADA as the first biologic compared to other anti-TNF-α therapies [8]. The patients in our study were all undergoing their first biologic treatment, and 16.7% were treatment-naive. Notably, this variance in treatment response may stem from the potential differences between NIU and JIA, which could be considered distinct entities in terms of their responses to ADA in children.
There is little evidence regarding when to withdraw biologic treatments for pediatric uveitis. Guidelines recommend at least 2 years of well-controlled immunomodulatory therapy before tapering in children with JIA uveitis [24]. However, the duration of suppression maintained for over 1.5 years with ADA did not significantly affect the likelihood of reactivation [25]. Likewise, the 5-year outcomes of the SYCAMORE trial revealed that drug-induced remission of JIA uveitis did not persist when ADA was withdrawn after 1–2 years of treatment [19]. Retrospective studies have documented that frequent uveitis recurrence was corelated with prolonged drug withdrawal, older age at uveitis onset, and shorter time to achieve persistent inactivity following treatment [19, 26, 27]. Interestingly, idiopathic uveitis may have a better prognosis than JIA uveitis due to the higher probability of maintaining remission following ADA discontinuation [27]. This suggested that JIA and idiopathic uveitis may be different and should be discussed separately. However, the exact duration of ADA treatment has not been defined for these two uveitides. Therefore, in our study, a treatment period of 2 years was maintained for patients who did not develop complications. The first phase-4 RCT (NCT03816397) is currently recruiting, assessing the feasibility of discontinuing ADA in adults and children with quiescent uveitis [28].
Although ADA alleviates pediatric uveitis activity (even up to the level of complete quiescence), it does not exclude the possibility of relapse. In our study, the ADA group could maintain alleviation for approximately 9.7 months longer than the CT group. A total of 52.1% of patients treated with ADA experienced at least one relapse during follow-up, although this was fewer than the number of relapses in patients treated with CT (90.5%). Uveitis relapse occurred in five (26%) patients without an identifiable cause and in 14 (33%) with an identifiable cause in a similar retrospective study of patients with non-JIA chronic uveitis [3]. However, the reason for flare-ups following ADA therapy remains unclear. Although ADA has a relatively lower uveitis recurrence rate than other anti-TNF biologics [10, 29], regular ophthalmic monitoring of children with uveitis is recommended, even in cases of stable posterior inactivity and panuveitis.
Adverse events requiring discontinuation of therapy were more common in children treated with CT than in those treated with ADA. However, 16 children in the ADA group (33.3%) experienced adverse events, including common cold (12.5%), nausea/vomiting (8.3%), rash/eczema (6.3%), fatigue (6.3%), growth retardation (4.2%), and weight fluctuation (2.1%). No deaths, malignancies, demyelinating diseases, serious infections, or lupus-like reactions were observed during ADA exposure. Only one child discontinued ADA owing to serious eczema. Our results coupled with the reports previously published in the literature suggest the safety of the use of ADA in children with uveitis [3, 30]. Moreover, the blood test results in the children treated with ADA were similar to those in the children in the CT group, which mostly showed elevated liver function enzymes. In all the cases, adjustment of conventional IMTs and administration of liver-protecting Chinese herbs resulted in transient abnormal blood test results. Therefore, ADA may be well tolerated in children with uveitis, with an acceptable side-effect profile.
Another important finding in our study was the prompt response time, which was 4 days in the CT group and 1 week in the ADA group. Notably, until 3 weeks after the initial treatment, the remission rate in the ADA group exceeded that in the CT group. Sonmez et al. demonstrated that intraocular inflammation significantly improved within 4 weeks, and vitreous haze decreased in the fourth week and stabilized in the 12th week [21]. ADA has a delayed onset of action and can require up to a few weeks to regulate inflammation. Little is known about the timing of effects of ADA in uveitis; however, lag has been seen in the onset of biologics in other rheumatic diseases [31]. Therefore, periocular and pulse steroid therapy is indispensable, especially in children with uveitis who require regulation of ocular inflammation to prevent vision-threatening complications. Therefore, more rigorous early follow-up studies are warranted.
To date, several before–after cohort studies have attempted to identify the efficacy of ADA in chronic non-infectious or non-anterior uveitis in children [3, 4, 21, 30]; but the data have lacked control groups for the maintenance of other IMTs and FA assessment, which are used as the gold standard for the diagnosis of posterior uveitis. Although the samples and focuses have been slightly different, these studies showed CMT thinning and reduction of systemic IMTs in children receiving ADA. However, ADA demonstrated no significant advantage over CT in reducing macular edema and increasing GC-sparing effects; even the rate of disappearances of macular edema were 77.8% (14/18) to 86.7% (13/15) in a similar study, lower than that seen herein [3, 30]. We also highlighted that ADA should be administered for a certain amount of time to ensure effects in children with NIU. Consequently, our study provided comprehensive and compelling evidence concerning the effects and characteristics of ADA in children with chronic non-infectious posterior uveitis and panuveitis.
Our study had certain limitations, such as its single-center design, lack of objective and quantified inflammation indicators, and lack of a prospective, randomized, masked, and controlled clinical trial design. However, certain observations herein can be useful owing to the paucity of reports on ADA for noninfectious childhood posterior uveitis and panuveitis. A larger, placebo-controlled trial is warranted to conclusively demonstrate the efficacy of ADA therapy in childhood uveitis, and not only in JIA-associated anterior uveitis.
Conclusions
This study demonstrated that ADA was effective and tolerated in pediatric patients with non-infectious posterior uveitis and panuveitis. Although ADA showed no superior advantage over CT in reducing macular edema, GC-sparing, and the speed of remission at early onset, it could significantly improve long-term visual acuity, stabilize ocular inflammation, and ensure a high remission rate in children with non-infectious posterior uveitis and panuveitis.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Chan NS, Choi J, Cheung CMG. Pediatric uveitis. Asia Pac J Ophthalmol (Phila). 2018;7(3):192–9.
Chang MH, et al. Uveitis in children and adolescents. Rheum Dis Clin North Am. 2021;47(4):619–41.
Kouwenberg CV, Koopman-KalininaAyuso V, de Boer JH. Clinical benefits and potential risks of adalimumab in non-JIA chronic paediatric uveitis. Acta Ophthalmol. 2022;100(4):e994–1001.
Deitch I, et al. The effect of anti-tumor necrosis factor alpha agents on the outcome in pediatric uveitis of diverse etiologies. Graefes Arch Clin Exp Ophthalmol. 2018;256(4):801–8.
Sood AB, Angeles-Han ST. An update on treatment of pediatric chronic non-infectious uveitis. Curr Treatm Opt Rheumatol. 2017;3(1):1–16.
Stolowy N, et al. Immunosuppressive therapy in severe or chronic pediatric uveitis: review of the literature. J Fr Ophtalmol. 2021;44(2):252–8.
Song H, et al. The efficacy and safety of adalimumab in treating pediatric noninfectious chronic anterior uveitis with peripheral retinal vascular leakage: a pilot study. Front Med (Lausanne). 2022;9: 813696.
Simonini G, et al. Superior efficacy of Adalimumab in treating childhood refractory chronic uveitis when used as first biologic modifier drug: adalimumab as starting anti-TNF-α therapy in childhood chronic uveitis. Pediatr Rheumatol Online J. 2013;11:16.
Ramanan AV, et al. Adalimumab plus methotrexate for uveitis in juvenile idiopathic arthritis. N Engl J Med. 2017;376(17):1637–46.
Maccora I, et al. Changing evidence over time: updated meta-analysis regarding anti-TNF efficacy in childhood chronic uveitis. Rheumatology (Oxford). 2021;60(2):568–87.
Simonini G, et al. Does switching anti-TNFα biologic agents represent an effective option in childhood chronic uveitis: the evidence from a systematic review and meta-analysis approach. Semin Arthritis Rheum. 2014;44(1):39–46.
LaMattina KC, Goldstein DA. Adalimumab for the treatment of uveitis. Expert Rev Clin Immunol. 2017;13(3):181–8.
Neri P, et al. Adalimumab (HUMIRA™): a promising monoclonal anti-tumor necrosis factor alpha in ophthalmology. Int Ophthalmol. 2011;31(2):165–73.
Neri P, et al. Adalimumab (HUMIRA™) in ophthalmology: a review of the literature. Middle East Afr J Ophthalmol. 2010;17(4):290–6.
Silvestri E, et al. Adalimumab effectively controls both anterior and posterior noninfectious uveitis associated with systemic inflammatory diseases: focus on Behçet’s syndrome. Inflammopharmacology. 2020;28(3):711–8.
Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol. 2005;140(3):509–16.
Schulze-Bonsel K, et al. Visual acuities “hand motion” and “counting fingers” can be quantified with the Freiburg Visual Acuity test. Invest Ophthalmol Vis Sci. 2006;47(3):1236–40.
Tugal-Tutkun I, Herbort CP, Khairallah M. Scoring of dual fluorescein and ICG inflammatory angiographic signs for the grading of posterior segment inflammation (dual fluorescein and ICG angiographic scoring system for uveitis). Int Ophthalmol. 2010;30(5):539–52.
Horton S, et al. Adalimumab in juvenile idiopathic arthritis-associated uveitis: 5-year follow-up of the Bristol Participants of the SYCAMORE trial. Am J Ophthalmol. 2019;207:170–4.
Quartier P, et al. ADJUVITE: a double-blind, randomised, placebo-controlled trial of adalimumab in early onset, chronic, juvenile idiopathic arthritis-associated anterior uveitis. Ann Rheum Dis. 2018;77(7):1003–11.
Sonmez HK, Evereklioglu C, GulmezSevim D. Prompt and sustained suppression of intraocular inflammation with adalimumab in pediatric patients with non-infectious uveitis resistant to traditional managements: a 6-month follow-up research. Ocul Immunol Inflamm. 2022. https://doi.org/10.1080/09273948.2022.2139274.
Simonini G, et al. Prevention of flare recurrences in childhood-refractory chronic uveitis: an open-label comparative study of adalimumab versus infliximab. Arthritis Care Res (Hoboken). 2011;63(4):612–8.
Skrabl-Baumgartner A, et al. Drug monitoring in long-term treatment with adalimumab for juvenile idiopathic arthritis-associated uveitis. Arch Dis Child. 2019;104(3):246–50.
Angeles-Han ST, et al. 2019 American College of Rheumatology/Arthritis foundation guideline for the screening, monitoring, and treatment of juvenile idiopathic arthritis-associated uveitis. Arthritis Rheumatol. 2019;71(6):864–77.
Lerman MA, et al. Uveitis reactivation in children treated with tumor necrosis factor alpha inhibitors. Am J Ophthalmol. 2015;160(1):193-200.e1.
Castiblanco C, Meese H, Foster CS. Treatment of pediatric uveitis with adalimumab: the MERSI experience. J aapos. 2016;20(2):145–7.
Simonini G, et al. Predictors of relapse after discontinuing systemic treatment in childhood autoimmune chronic uveitis. J Rheumatol. 2017;44(6):822–6.
Acharya NR, et al. Discontinuing adalimumab in patients with controlled juvenile idiopathic arthritis-associated uveitis (ADJUST-Adalimumab in Juvenile Idiopathic Arthritis-associated Uveitis Stopping Trial): study protocol for a randomised controlled trial. Trials. 2020;21(1):887.
Wendling D, et al. New onset of uveitis during anti-tumor necrosis factor treatment for rheumatic diseases. Semin Arthritis Rheum. 2011;41(3):503–10.
Vitale A, et al. Efficacy and safety of adalimumab in pediatric non-infectious non-anterior uveitis: real-life experience from the international AIDA network uveitis registry. Ophthalmol Ther. 2023;12(4):1957–71.
Nast A, et al. Which antipsoriatic drug has the fastest onset of action? Systematic review on the rapidity of the onset of action. J Invest Dermatol. 2013;133(8):1963–70.
Acknowledgements
We extend our heartfelt gratitude to all the participants and their parents who generously dedicated their time and effort to contribute to this research.
Medical Writing/Editorial Assistance.
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This work was supported by the National Outstanding Youth Science Fund Project of China (No. 82122016) and the National Key Research and Development Program of China (2017YFA0105804). The journal's Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Study design: Wenru Su. Clinical information: Shizhao Yang and Daquan He. Intellectual input: Tianyu Tao, Xuening Peng and Qi Jiang. Formal analyses: Tianyu Tao and Zhenyu Wang. Writing–original draft preparation: Tianyu Tao. Writing–review, editing, and supervision: Wenru Su, Tianyu Tao and Tianfu Wang. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Tianyu Tao, Shizhao Yang, Daquan He, Xuening Peng, Zhenyu Wang, Qi Jiang, Tianfu Wang, and Wenru Su have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
Ethical Approval
The studies involving human participants were reviewed and approved by Zhongshan Ophthalmic Center Ethics Committee (No. 2019058). The patients and their legal guardian provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tao, T., Yang, S., He, D. et al. The Efficacy of Adalimumab in Children with Chronic Non-infectious Posterior Uveitis and Panuveitis: A Retrospective Cohort Study. Ophthalmol Ther 13, 1239–1253 (2024). https://doi.org/10.1007/s40123-024-00884-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00884-4