Abstract
Introduction
Implantation of toric intraocular lenses (IOLs) in patients with Fuchs endothelial corneal dystrophy (FECD) is still considered relatively contraindicated, without sufficient clinical evidence. Therefore, this study was designed to evaluate the results of toric IOL implantation in patients with FECD.
Methods
A retrospective case–control study of 28 eyes of FECD patients and 84 eyes of healthy control patients who received toric IOLs during routine cataract surgery was performed. The outcome measures were uncorrected and corrected distance visual acuity, spherical equivalent, and refractive residual astigmatism.
Results
The mean postoperative uncorrected and corrected distance visual acuity in the FECD eyes compared to the control eyes were 0.15 ± 0.14 vs. 0.13 ± 0.17, respectively (P = 0.32), and 0.05 ± 0.08 vs. 0.06 ± 0.10, respectively (P = 0.95). The spherical equivalent in the FECD eyes compared to the control eyes was − 0.29 ± 0.43 vs. − 0.21 ± 0.50, respectively (P = 0.19). The preoperative corneal centroid astigmatism in the FECD eyes compared to the control eyes was 0.85 D@93° ± 2.42° vs. 0.23 D@68° ± 2.50°, respectively (P = 0.43), and the mean preoperative corneal astigmatism magnitude was 2.26 ± 1.1 D vs. 2.28 ± 1.03 D, respectively (P = 0.82). A trend toward higher postoperative refractive centroid astigmatism was found in the FECD eyes compared with the control eyes: 0.24 D@28° ± 0.57° vs. 0.03 D@127° ± 0.53°, respectively (P = 0.09). However, the mean refractive astigmatism magnitude was similar in FECD eyes and the healthy control eyes: 0.52 ± 0.31 D vs. 0.42 ± 0.31 D, respectively (P = 0.44) (D diopters).
Conclusion
The postoperative refractive astigmatism (both centroid astigmatism and mean magnitude astigmatism) was no higher than 0.52 D in both groups. Therefore, FECD patients without corneal edema can be considered for toric IOLs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Implantation of toric intraocular lenses (IOLs) in patients with Fuchs endothelial corneal dystrophy (FECD) is considered relatively contraindicated, without sufficient evidence. |
As a result, FECD patients with significant astigmatism cannot enjoy the benefits of toric lenses, which include spectacle independence and higher quality of vision. |
What was learned from the study? |
FECD and control patients had similar visual acuity and postoperative refraction results. |
FECD patients had a trend toward slightly higher postoperative refractive centroid astigmatism. This difference between the groups is probably not clinically significant. |
Therefore, FECD patients without corneal edema can be considered for toric IOL implantation, and can enjoy the previously mentioned benefits. |
Introduction
Up to 30% of patients have a significant corneal astigmatism before cataract surgery [1,2,3,4]. Corneal astigmatism can be treated during cataract surgery with different methods: relaxing limbal incisions (for 1–4 D astigmatism), opposite clear corneal incision, adjusting the main corneal incision to the steep meridian, femtosecond laser-assisted astigmatic keratotomy, and toric IOL implantation [1, 5, 6]. However, toric IOL implantation is more predictable and precise, can fix a higher corneal astigmatism, can achieve more spectacle independence, and can provide a higher quality of vision without image distortion compared to the other methods [1, 2, 5, 6]. Recently, the implantation of toric IOLs in eyes with comorbidities has burgeoned, and patients with age-related macular degeneration (AMD), as well as patients with mild to moderate corneal ectasias, are being offered toric IOLs and spectacle independence with satisfactory refraction results [6,7,8]. However, the implantation of toric IOLs in patients with corneal dystrophies such as FECD is still considered by some surgeons to be contraindicated, which lacks supporting clinical evidence [6]. In this study, we investigated the clinical outcomes of the implantation of toric IOLs in patients with mild to moderate FECD without corneal edema. Sex and/or gender differences were not expected.
Methods
We conducted a retrospective case–control study of FECD patients implanted with three different optical types of toric IOLs (multifocal, extended depth of focus (EDOF) and monofocal IOLs) in a case–control ratio of 1:3. All the patients underwent cataract surgeries without surgical complications in the Ein-Tal Eye Center, Tel Aviv, Israel, between March 2013 and March 2020 by one of two surgeons (GK and EIA).
The control was matched by age and IOL type. Three different optical types of IOLs were used: the monofocal IOLs were Ankoris (PhysIOL SA, Liège, Belgium) or AcrySof IQ Toric (Alcon Laboratories, Inc., Fort Worth, Texas, United States), EDOF IOLs was Tecnis Symfony IOL (Johnson and Johnson, New Brunswick, NJ, USA), and multifocal IOLs consisted of either FineVision trifocal IOL (PhysIOL Inc., Liège, Belgium) or AcrySof ReSTOR IOL (Alcon Laboratories, Inc, Fort Worth, TX, USA).
The study adhered to the tenets of the Declaration of Helsinki, and was approved by the Meir Medical Center Institutional Ethics Committee.
FECD grading was based on Louttit et al.’s grading system [9] (Table 1). This grading system is based on a slit lamp examination that checks for the number, area and confluence of the guttae as well as corneal edema: grade 1—mild disease: up to 12 central or paracentral nonconfluent guttae; grades 2–5—moderate disease: more than 12 nonconfluent guttae or confluent guttae up to an area of 5 mm; grade 6—advanced disease: 5 mm or more of confluent guttae with corneal edema. The FECD grading was done preoperatively by one of the two surgeons, who are both experienced anterior segment specialists.
The inclusion criteria for the study group were: patients age 18 years old and above with FECD but without corneal edema (grade 2–5) who underwent implantation of toric IOLs during uneventful cataract surgery and were followed up for at least 4 weeks after the surgery. Only cooperative patients who were able to perform the full preoperative and postoperative evaluations, including biometry, specular microscopy and refraction examinations, were included.
The exclusion criteria were age below 18 years old, corneal edema (grade 6 FECD), other significant ocular morbidities that may affect the visual outcome, previous ocular surgeries, previous ocular trauma, patients who couldn’t complete the full eye evaluation, and patients who were lost to follow-up. Eyes with irregular astigmatism based on tomography were also excluded from the study and from the implantation of toric IOLs.
The inclusion and exclusion criteria for the control group were the same, except for the presence of FECD.
Preoperatively, we calculated the IOL power using biometric data (Lenstar LS900, Haag-Streit, Koeniz, Switzerland) and the Barrett online calculator for toric IOLs. To consider the posterior corneal astigmatism (PCA), we used the default Barrett toric calculator option that uses the prediction method of PCA based on anterior corneal measurements. A Scheimpflug camera (Pentacam Oculus, Optikgerate GmbH, Wetzlar, Germany) was used for corneal tomography. The target refraction was emmetropia or the nearest myopic alternative for both the FECD and the control patients. The corneal endothelial cell count was performed using an EM‐3000 specular microscope (Tomey Corporation, Nagoya, Japan). IOL selection was done after a thorough discussion between the surgeon and the patient, revealing all the advantages and disadvantages of each IOL model while considering the patient’s individual needs and desires.
The cataract surgeries were performed through a 2.2- to 2.4-mm superior clear corneal incision using phacoemulsification. The toric IOLs were implanted into the capsular bag and dialed to the preplanned axis. Toric IOLs were considered only for regular corneal astigmatism. We used similar methods and criteria to those in our previous study on FECD patients [10].
The primary outcome measures were uncorrected and corrected distance visual acuity, spherical equivalent and residual refractive astigmatism 4 weeks after the surgeries.
Statistical Analysis
The statistical analysis was done with SPSS software ((version 21.0; IBM Corp., Armonk, NY, USA). For categorical variables, we used Pearson’s χ2 or Fisher’s exact test. For continuous variables, we used the Mann–Whitney U test. We calculated the centroid astigmatism after the division of each centroid into its X and Y components and used the double-angle plot and the paired Hotelling’s T-square test for bivariate analysis [11, 12]. For multivariate correlation, we used the ANOVA test. A P value of less than 0.5 was considered as statistically significant.
Results
Twenty-eight eyes of 18 FECD patients and 84 eyes of healthy control patients who had cataract surgery with the implantation of similar toric IOLs were included in the study (a case:control ratio of 1:3).
The demographic and ocular characteristics were similar between the FECD patients and the healthy control before the surgeries (Table 2).
Preoperatively, the mean endothelial cell count was 1701 ± 573.24 cells/mm2 (range 664–2737 cells/mm2) and the mean central corneal thickness (CCT) was 557.12 ± 32.82 microns (range 481–618 microns) in the FECD patients. No correlation was found using a multivariate correlation analysis between endothelial cell count and CCT, postoperative uncorrected distance visual acuity, residual refractive astigmatism and spherical equivalent (R2 = 0.37, P = 0.20).
Mean postoperative follow-up time for the FECD patients was 8.45 ± 13.59 months (range 1 month to 5.8 years). No patients required corneal transplantation during the follow-up period.
Visual Acuity Results
The mean postoperative uncorrected distance visual acuity (UDVA, LogMAR) of the FECD patients was 0.15 ± 0.14 compared to 0.13 ± 0.17 in the control group (P = 0.32). The mean postoperative corrected distance visual acuity (CDVA, LogMAR) of the FECD patients was 0.05 ± 0.08 compared to 0.06 ± 0.10 in the control group (P = 0.95).
The spherical equivalent of FECD patients was − 0.29 ± 0.43, compared to − 0.21 ± 0.50 in the control group (P = 0.19).
The mean postoperative uncorrected near visual acuity (UNVA, LogMAR) among the FECD patients implanted with multifocal IOLs was 0.07 ± 0.13 vs. 0.03 ± 0.06 among the control patients implanted with multifocal IOLs (P = 0.58).
Astigmatism
Preoperative Astigmatism
The FECD patients had a preoperative corneal centroid astigmatism of 0.85 D@93° ± 2.42°, compared to 0.23 D@68° ± 2.50° in the control group (P = 0.43), and a mean corneal astigmatism magnitude of 2.26 ± 1.1 D, compared to 2.28 ± 1.03 D in the control group (P = 0.82).
Postoperative Astigmatism
The FECD patients had a postoperative refractive centroid astigmatism of 0.24 D@28° ± 0.57°, compared to 0.03 D@127° ± 0.53° in the control group (P = 0.09), and a mean refractive astigmatism magnitude of 0.52 ± 0.31 D, compared to 0.42 ± 0.31 D in the control group (P = 0.44) (D diopters).
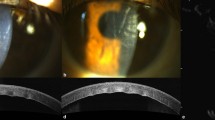
Eighty-four percent of FECD patients had postoperative refractive astigmatism of 0.75 D or less and 92% had postoperative refractive astigmatism of 1 D or less, compared with 90% and 94% in the control group (P = 0.36, P = 0.71, respectively; Fig. 1).
Discussion
The global prevalence of FECD was found to be 7.33% in a recent meta-analysis, with 300 million people with FECD in 2020 and an expected increased number of 415 million by 2050 [13]. The late-onset form of FECD, which is the most common one, is prevalent in the fifth or sixth decade of life and coincides with the time that people develop cataracts [13, 14]. Cataract surgery among FECD patients requires a meticulous preoperative evaluation, including an assessment grading FECD severity, corneal thickness measurements, a corneal endothelial cell count, anterior chamber depth measurements and cataract density assessment [15].
In this study, we found similar results for toric IOLs implanted in FECD eyes compared with healthy eyes. The expanding indications for the implantation of toric IOLs in eyes with comorbidities such as AMD and even corneal ectasias such as keratoconus enables more patients to be spectacle independent and enjoy a higher quality of vision [6,7,8].
In a meta-analysis by Kessel et al. that included 13 randomized controlled trials with 707 eyes implanted with toric IOLs versus 706 eyes implanted with nontoric IOLs, the UDVA, residual refractive astigmatism and spectacle independence were better in the toric IOLs group, even when relaxing incision was used in the nontoric IOLs group [4].
In our study, the postoperative spherical equivalent as well as the uncorrected and corrected distance visual acuity were similar between the FECD patients and the control patients (P = 0.19, P = 0.32, P = 0.95, respectively). The preoperative corneal centroid astigmatism and the mean preoperative corneal astigmatism magnitude as well as the mean postoperative refractive astigmatism magnitude were similar between the groups (P = 0.43, P = 0.82, P = 0.44; respectively). There was a trend toward higher postoperative refractive centroid astigmatism in the FECD group (P = 0.09). However, the postoperative centroid astigmatism of 0.24 D in the FECD group is probably not clinically significant, as supported by the similar UDVA and mean refractive astigmatism magnitude (P = 0.32, P = 0.44, respectively). Hasegawa et al. collected data from 1535 pseudophakic eyes after cataract surgeries with monofocal IOL implantation and showed a significant correlation between the residual astigmatism and the UDVA (r2 = 0.795) [16].
Furthermore, the residual postoperative refractive astigmatism was 0.75 D or less in 84% of FECD patients and 1 D or less in 92% of FECD patients (Fig. 1). These results are comparable to healthy eyes in the literature and in the current study.
In a recent Indian study, Patil et al. reported that 90% of the patients had less than 1 D and 62.5% of the patients had less than 0.5 D of residual refractive astigmatism 1 month after cataract surgeries when implanting monofocal toric IOLs in healthy patients [2]. Another study by Abulafia et al. compared different toric IOL calculators. They found that the Barrett toric calculator was the most accurate, with a residual astigmatism of less than 0.5 D in 75.8% of the cases and less than 0.75 D in 92.9% of the cases in healthy eyes [17]. However, Savini et al. reported that only 57.81% of the 64 eyes included in the study obtained an absolute error in astigmatism magnitude of less than 0.5 D, even when using optimized astigmatism values, the Barrett toric IOL calculator and the Abulafia–Koch calculator [18].
Hayashi et al. studied the long-term centroid astigmatism at least 5 years postoperatively in 120 healthy eyes. The baseline refractive centroid astigmatism after the surgeries was 0.36 D@177° in eyes with against-the-rule (ATR) preoperative corneal astigmatism, and after 5–10 years follow-up it had risen to 0.58 D@178°. In eyes with with-the-rule (WTR) preoperative corneal astigmatism, the baseline postoperative refractive astigmatism was 0.1 D@46°, and it was stable at 0.084 D@63° 5–10 years postoperatively [19].
Another concern may arise regarding the need for future corneal transplantation in pseudophakic FECD patients that received toric IOLs. Viberg et al. collected data on 276,362 cataract patients and 2,091 patients who underwent corneal transplantation from the Swedish National Cataract Registry [20]. Corneal guttae were observed in 3338 patients [20]. Although the relative risk for corneal transplantation among FECD patients was significantly higher (relative risk 68.2 (95% CI 54.0–86.2)), only 152 patients (4.6%) from the 3,338 patients with corneal guttae needed a corneal transplantation [20]. Another recent study investigated 719,066 FECD patients 65 years of age or older from the Medicare database [21]. Among them, 31,372 (4.4%) needed endothelial keratoplasty and 2426 (0.3%) needed penetrating keratoplasty. The risk for endothelial keratoplasty after cataract surgery in this study was 1.3% after 1 year and 2.3% after 8 years [21].
Furthermore, with advanced lamellar keratoplasty methods, the refractive error and induced surgical astigmatism are minimal. In a report by the American Academy of Ophthalmology, the results of a meta-analysis of 47 articles demonstrated an overall spherical equivalent change of 0.43 D and a minimal surgically induced astigmatism of 0.03 D after Descemet membrane endothelial keratoplasty (DMEK) [22]. In our study, none of the participants required corneal transplantation during the study follow-up time. However, this risk of further surgical intervention and the refraction shift that may occur afterward should be discussed in detail with the patients before choosing the IOL model.
In the future, preoperative risk assessment of the need for endothelial keratoplasty after cataract surgery can be added to the preoperative evaluation. Arnalich-Montiel et al. described a model to assess the risk of endothelial keratoplasty after uneventful cataract surgery based on Scheimpflug tomography features such as a loss of parallel isopachs, displacement of the thinnest point and depression of the posterior surface combined with pachymetry measures [23].
The limitations of our study are its retrospective nature and the relatively small sample size. Furthermore, IOLs with different optical modalities were incorporated into the study (monofocal, EDOF and multifocal IOLs). Additionally, all patients had clear corneas after the surgeries, and therefore we didn’t repeat the endothelial cell count. A repeat endothelial cell count could have added an objective assessment of the endothelial cell loss after the surgeries. The mean follow-up time was 8.45 ± 13.59 months (range 1 month to 5.80 years), and no patient required corneal transplantation in this period. However, there was a variability in the follow-up times between the patients, and some patients were followed for only 1 month.
Conclusions
FECD patients without corneal edema who were implanted with toric IOLs had a trend toward slightly higher postoperative refractive centroid astigmatism compared to healthy patients (P = 0.09). However, a postoperative refractive centroid astigmatism of 0.24 D in the FECD group and a mean postoperative astigmatism magnitude difference of 0.1 D between the groups are probably not clinically significant, as reflected by the similar UDVA, CDVA and spherical equivalent values. FECD patients without corneal edema can be considered for toric IOL implantation, which has the advantages of a higher quality of vision and spectacle independence, with the above-mentioned reservations. However, a larger randomized controlled trial is warranted to validate our results.
References
Lake JC, Victor G, Clare G, Porfírio GJM, Kernohan A, Evans JR. Toric intraocular lens versus limbal relaxing incisions for corneal astigmatism after phacoemulsification. Cochrane Database Syst Rev. 2019;2019(12):CD012801.
Patil MS, Nikose AS, Bharti S. Visual outcome and refractive status with monofocal toric intraocular lens implantation to correct astigmatism during cataract surgery. Indian J Ophthalmol. 2020;68(12):3016–9.
Vedana G. Fuchs endothelial corneal dystrophy: current perspectives. Clin Ophthalmol. 2016;321–30.
Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123(2):275–86.
Zvorni J, Zvorni E. ScienceDirect premium intraocular lenses: the past, present and future. J Curr Ophthalmol. 2018;30:287–96.
Singh VM, Ramappa M, Murthy SI, Rostov AT. Toric intraocular lenses: Expanding indications and preoperative and surgical considerations to improve outcomes. Indian J Ophthalmol. 2022;70(1):10.
Mehta H. Management of cataract in patients with age-related macular degeneration. J Clin Med. 2021;10(12):2538.
Yahalomi T, Achiron A, Hecht I, Arnon R, Levinger E, Pikkel J, et al. Refractive outcomes of non-toric and toric intraocular lenses in mild, moderate and advanced keratoconus: a systematic review and meta-analysis. J Clin Med. 2022;11:2456.
Louttit MD, Kopplin LJ, Igo RPJ, Fondran JR, Tagliaferri A, Bardenstein D, et al. A multicenter study to map genes for Fuchs endothelial corneal dystrophy: baseline characteristics and heritability. Cornea. 2012;31(1):26–35.
Blau-Most M, Reitblat O, Levy A, Assia EI, Kleinmann G. Clinical outcomes of presbyopia-correcting intraocular lenses in patients with Fuchs endothelial corneal dystrophy. Sci Rep. 2023;13(1):1–9.
Næser K. Assessment and statistics of surgically induced astigmatism. Acta Ophthalmol. 2008;86:349.
Abulafia A, Koch DD, Holladay JT, Wang L, Hill W. Pursuing perfection in intraocular lens calculations: IV. Rethinking astigmatism analysis for intraocular lens-based surgery: suggested terminology, analysis, and standards for outcome reports. J Cataract Refract Surg. 2018;44(10):1169–74.
Aiello F, Gallo Afflitto G, Ceccarelli F, Cesareo M, Nucci C. Global prevalence of Fuchs endothelial corneal dystrophy (FECD) in adult population: a systematic review and meta-analysis. J Ophthalmol. 2022;3091695.
Ong Tone S, Kocaba V, Böhm M, Wylegala A, White TL, Jurkunas UV. Fuchs endothelial corneal dystrophy: the vicious cycle of Fuchs pathogenesis. Prog Retin Eye Res. 2021;80: 100863.
Moshirfar M, Huynh R, Ellis JH. Cataract surgery and intraocular lens placement in patients with Fuchs corneal dystrophy: a review of the current literature. Curr Opin Ophthalmol. 2022;33(1):21–7.
Hasegawa Y, Honbo M, Miyata K, Oshika T. Type of residual astigmatism and uncorrected visual acuity in pseudophakic eyes. Sci Rep. 2022;12(1):1225.
Adi A, Hill WE, Maria F, Barrett GD. Comparison of methods to predict residual astigmatism after intraocular lens implantation. J Refract Surg. 2015;31(10):699–707.
Savini G, Næser K, Schiano-Lomoriello D, Ducoli P. Optimized keratometry and total corneal astigmatism for toric intraocular lens calculation. J Cataract Refract Surg. 2017;43(9):1140–8.
Hayashi K, Yoshida M, Hayashi S, Hirata A. Long-term changes in the refractive effect of a toric intraocular lens on astigmatism correction. Graefe’s Arch Clin Exp Ophthalmol. 2022;260(2):509–19.
Viberg A, Samolov B, Claesson Armitage M, Behndig A, Byström B. Incidence of corneal transplantation after phacoemulsification in patients with corneal guttata: a registry-based cohort study. J Cataract Refract Surg. 2020;46(7):961–6.
Heckenlaible NJ, Dun C, Prescott C, Eghrari AO, Woreta F, Makary MA, et al. Predictors of receiving keratoplasty for Fuchs’ endothelial corneal dystrophy among Medicare beneficiaries. Ophthalmology. 2023;130(1):28–38.
Deng SX, Lee WB, Hammersmith KM, Kuo AN, Li JY, Shen JF, et al. Descemet membrane endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmology. 2018;125(2):295–310.
Arnalich-Montiel F, de-Arriba-Palomero P, Muriel A, Mingo-Botín D. A risk prediction model for endothelial keratoplasty after uncomplicated cataract surgery in Fuchs endothelial corneal dystrophy. Am J Ophthalmol. 2021;231:70–8.
Acknowledgements
Funding
No funding or sponsorship was received for this study or the publication of this article. The journal’s Rapid Service Fee was funded by the authors.
Author Contributions
Ehud Assia and Guy Kleinmann developed the project’s concept. Michal Blau-Most and Adi Levy were responsible for data collection and analysis. Michal Blau-Most drafted the paper, which was reviewed and revised by all authors. Michal Blau-Most and Guy Kleinmann are accountable for the data integrity. All authors approved the final paper.
Prior Presentation
Presented at the International Annual Conference on Ocular Microsurgery, January 2023, Eilat, Israel.
Disclosures
Prof. Assia is a consultant for Hanita Lenses, Vision Care Technologies; is founder and CMO of APX Ophthalmology and VisiDome; and is a shareholder in IOPtima and CorNeat. Prof. Kleinmann is a consultant for Hanita Lenses, Johnson and Johnson Vision and CorNeat. Michal Blau-Most and Adi Levy have nothing to disclose.
Compliance with Ethics Guidelines
The study adhered to the tenets of the Declaration of Helsinki, and was approved by the Meir Medical Center Institutional Ethics Committee.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Blau-Most, M., Levy, A., Assia, E.I. et al. Clinical Outcomes of Toric Intraocular Lenses in Patients with Fuchs Endothelial Corneal Dystrophy. Ophthalmol Ther 12, 1747–1755 (2023). https://doi.org/10.1007/s40123-023-00700-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00700-5