Abstract
Introduction
We aim to introduce a method using confocal scanning laser ophthalmoscopy (cSLO) images for measuring retinal vascular geometry, including vessel branch angle (BA), vessel diameter, vessel tortuosity, and fractal dimension (Df), and to elucidate the relationship between hypertension and these metrics.
Methods
A total of 119 participants (119 eyes) were enrolled, among which 72 were normotensive and 47 were hypertensive. Infrared cSLO images were extracted from the circular scan around the optics disc using a commercial cSLO + optical coherence tomography instrument. Preprocessed cSLO images were further analyzed using the appropriate tool/macro/plugin of ImageJ.
Results
Intraclass correlation coefficients of selected methods used for conducting the cSLO-based geometric analyses were all higher than 0.80. Arterial/arteriolar BA, arteriolar vessel diameter, and total Df in normotensive subjects were 85.80 ± 7.79°, 116.80 ± 12.58 μm, and 1.430 ± 0.037, respectively, significantly higher than those of hypertensive subjects (82.13 ± 10.83°, 108.2 ± 11.12 μm, and 1.361 ± 0.044, all P < 0.05). The aforementioned metrics remained negatively correlated with hypertension even after adjusting for age alone or age and gender (P < 0.05). However, the difference between arteriolar tortuosity and all studied venous/venular geometric parameters in both subjects was insignificant (all P > 0.05).
Conclusion
Proposed cSLO-based methods for assessing various vascular geometric parameters were highly repeatable and reproducible. Arterial/arteriolar BA, arteriolar vessel diameter, and total Df were retinal vascular parameters significantly correlated with hypertension in a negative manner.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The imaging system combining optical coherence tomography with confocal laser ophthalmoscopy (cSLO) is commonly used for monitoring ocular and systemic diseases; however, its ability to observe retinal vasculatures is still poorly studied. |
The study aims to explore the feasibility of using cSLO to measure four of the most studied retinal vascular geometries: branch angle (BA), vessel diameter, tortuosity, and fractal dimension (Df), and further to ascertain the relationships between the four parameters with hypertension. |
What was learned from the study? |
The proposed cSLO-based methodology for measuring retinal vascular geometry exhibited high repeatability and reproducibility; furthermore, arterial/arteriolar BA, diameter, and total Df were negatively correlated with hypertension even after adjusting for other variables. |
The cSLO-based analyses for retinal vascular geometry could serve as an alternative to observe and investigate abnormalities in retinal vasculature. |
Introduction
Systemic hypertension exerts significant influence on the structures of the microcirculation system. Besides myographic and histological investigations, there are few clinical methods to measure the change of small vessels [1]. As a component of the human vascular system, retinal vasculature can be visualized noninvasively and provide a wealth of diagnostic and prognostic information for several systemic diseases, including hypertension, cardiac diseases, and diabetes, as well as vision-threatening ocular diseases, including age-related macular degeneration, diabetic retinopathy, and glaucoma [2,3,4,5,6,7].
The need for the quantitative measurements of retinal vasculature generated the concept of retinal vascular geometry, comprising retinal vessel branch angle (BA), retinal vessel diameter, vessel tortuosity, fractal dimension (Df), etc. [2, 3]. Presently, the most commonly used modality to analyze retinal vascular geometry is fundus photographs (FPs). Aided by semi-automated software, digital FPs can precisely measure the aforementioned vascular parameters and have been used to observe retinal vascular characteristics related to various diseases in numerous population-based studies [2, 8,9,10]. However, fundus camera has intrinsic disadvantages, including poor penetration, image quality greatly influenced by pupil diameter, and theoretical concerns about magnified vessels induced by a linear perspective [11].
The past two decades have seen rapid advances in ophthalmic imaging techniques, of which optical coherence tomography (OCT) has been widely applied to monitor various ocular diseases. Recently, some studies have used OCT images to measure retinal vessel diameters [12,13,14]. However, due to the inherent nature of cross-sectional images, OCT is unable to evaluate retinal vascular Df and BA. Currently, some multimodal imaging systems have integrated confocal scanning laser ophthalmoscopy (cSLO) and OCT, enabling the simultaneous attainment of cSLO and OCT images. The cSLO has the advantages of good penetration, high resolution, and lower demands of pupil diameter, which is also free from the vessel magnification effect as a planar imaging technique. Also, unlike tomography, a cSLO image, resembling a fundus photograph, is mainly used to evaluate retinal morphology. It might thus have the potential to be a feasible alternative for the comprehensive assessment of retinal vascular geometry.
This study had two aims: first, to ascertain the feasibility of using cSLO images for measuring the four most studied vascular parameters (BA, retinal vessel diameter, vessel tortuosity, and Df), and second, to elucidate the alternations of these vascular geometries in hypertensive subjects.
Methods
Study Population
This prospective observational study was carried out at the Department of Ophthalmology in Eye and ENT Hospital, Shanghai, between January 2022 and June 2022. All enrolled subjects were healthy volunteers with no acute or chronic systemic disease besides primary systemic hypertension. All subjects had no vascular-related disease or ocular diseases such as retinal vein occlusion, retinal artery occlusion, glaucoma, or uveitis, or previous history of ocular trauma or ocular surgery except for age-related cataract surgery. Hypertension was defined as blood pressure higher than 140/90 mmHg at a clinic encounter, or current antihypertensive medication use [8]. All participants underwent a comprehensive ocular examination, including best-corrected visual acuity (BCVA), slit-lamp bio-microscopy, intraocular pressure measurement using a noncontact tonometer, and ultra-widefield retinal imaging. Refractive error (measured by an autorefractometer) < −3 diopters and age ≥ 18 years were accepted. All procedures strictly conformed to the tenets of the Declaration of Helsinki, and the study was approved by the ethics committee. Written informed consent was obtained from all participants.
Image Acquisition
All subjects were measured with a circular scan using the Spectralis HRA + OCT (Heidelberg Engineering, Heidelberg, Germany). Eye tracking and automatic real-time (ART) averaging technique were used to improve image quality. Once the cross-sectional OCT of the circular scan around the optic disc was obtained, a cSLO 30° image was simultaneously acquired. A high-resolution mode with a mean ART ≥ 30 was used to ensure image quality for the cSLO scan, thereby providing a fine demonstration of the retinal vessel arcades. Only the right eyes were analyzed [15,16,17]. The infrared reflectance modality of cSLO was selected for further analysis.
Measurement Key Points
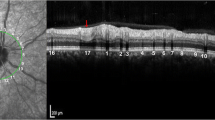
Careful identification of venous and arterial vessels was performed on cSLO images according to anatomical features before various measurements. On the images, compared with arteries, the veins have two wider dark layers (plasma layers) on both sides of a narrower visible light-reflex centerline (Fig. 1a).
cSLO image and measurement methods of various vascular geometric parameters. The cSLO image was acquired by the circular scan mode with four overlaid concentric circles. Compared with arteries (white asterisk), veins are thicker and darker and have a narrower light luminal reflex (blue asterisk). Zone A [0–0.5 disc diameter (DD) from the optic margin], zone B (0.5–1.0 DD from the optic margin), and zone C (0.5–2.0 DD from the optic margin) are labeled. b–d Magnified cSLO image (white box in a). The white arc represents the vessel branch angle. b Method 1 (vessel reflex to vessel reflex): all three measurement points (dots on the yellow line) are on the vessel reflex, two on the daughter’s vessels (blue arrow), and one on the parent vessel (green arrow). c Method 2 (plasma layers to plasma layers): all three points are on the plasma layers. d Method 3 (plasma layers to vessel reflex to plasma layers): two points are on the plasma layers, and one is on the luminal reflex. e–g Magnified cSLO image (blue box in a). The measurement of retinal vessel diameter and vessel tortuosity. e Positioning a through-line along the lumen. f The automatic generation of the cross-line perpendicular to the vessel with prespecified 10 μm space calculates vessel diameter on the basis of an intensity profile algorithm. g The blue line represents the actual length, and the white line the shortest length. h Fractal dimension within zone C after binarization and skeletonization
All measurements were performed using ImageJ software (version 1.8.0) by two ophthalmologists, who assessed all images independently. The characteristics of subjects were blinded to the two operators. All images were sharpened and magnified to 200–300% using ImageJ before measurement to improve the recognition of vascular details. For evaluating BA, vessel diameter, and vessel tortuosity, vessels in the superotemporal quadrant were analyzed first; if the vessels could not be measured due to brightness or artery–vein intertwining, then the corresponding vessels in the inferotemporal quadrant would be selected for measurement. The supero- or inferotemporal quadrant was selected because vessels within the quadrant could be more reliably identified [11]. Furthermore, vessel diameter and vessel tortuosity were measured in zone B [the region 0.5–1.0-disc diameter (DD) away from the disc margin] and Df was measured in zone C (the region 0.5–2.0 DD away from the disc margin). The parameters and corresponding measuring tool/macro/plugin are described in the following corresponding sections.
Measurement of Branch Angle
The BA of the first branch was analyzed using the Angle Tool of ImageJ. To the best of our knowledge, there was no reported protocol for BA measurements using cSLO images; hence we first tested the performance of three prespecified methods: method 1 (vessel reflex to vessel reflex), method 2 (plasma layers to plasma layers), and method 3 (plasma layers to vessel reflex to plasma layers) (Fig. 1b–d). Measurements from each method were performed three times to average the values to improve precision. After assessing the measurement performance (repeatability and reproducibility) among the three methods, the method with the highest performance was selected for the study.
Measurement of Vessel Diameter
The parent trunks of major vessels were evaluated, and vessel diameters were analyzed using VasoMetrics, a macro of ImageJ. The details of the measurement procedures have been reported elsewhere [18]. Briefly, we first drew a “through-line” (line along the central axis of the measured vessel) to create the trajectory along the vessel, then the macro would automatically generate a “cross-line” (line perpendicular to the “through-line,” thus perpendicular to the measured vessel). After determining the spacing between each “cross-line” (prespecified 10 μm across the study), the averaged vessel diameter could be automatically calculated (Fig. 1e, f).
Measurement of Vessel Tortuosity
Similar to measuring vessel diameters, only the parent trunks of major vessels were measured. Vessel tortuosity was assessed by simple tortuosity (ST), defined as the ratio between the actual length of the vessel and the Euclidean distance (the shortest linear length) of the initial and final point (Fig. 1g). Segmented line and straight line, the measuring tool of ImageJ, were used to measure actual distance and shortest distance, respectively.
Measurement of Fractal Dimension
cSLO images were processed by an in-house written program based on Python (version 3.9.8) and Open CV (version 4.5.5) to facilitate manual segmentation of retinal vessels. The segmented image was further binarized and skeletonized using ImageJ (Fig. 1h), and Df was derived with FracLac (ImageJ plugin), a box-counting method.
Assessment of Reproducibility and Repeatability
Images of 20 healthy participants without hypertension who had completed measurements by one operator were selected for inter-rater reproducibility and intra-rater repeatability assessment. Another operator independently performed the measurements of the corresponding parameters following the aforementioned instructions. During the measurement processes, the operator was masked to his measurement results and those of the other operator.
Statistical Analysis
Statistical analysis was conducted using Prism (version 8.0.1, GraphPad Software, San Diego, CA) and SPSS (version 23, SPSS Inc., Chicago, IL). A P value < 0.05 was considered statistically significant. The Kolmogorov–Smirnov test was used to check whether the data conformed to a normal distribution. Comparisons between subjects with and without hypertension were using an independent t-test, Mann–Whitney test, or chi-square test. Univariate (adjusted for age) and multivariate regression (adjusted for age plus gender) analyses were constructed to analyze the associations between various vascular parameters and hypertension. Inter-rater reproducibility and intra-rater repeatability were evaluated by intraclass correlation coefficient (ICCs), with ICCs of ≥ 0.8 as almost perfect reliability, ≥ 0.6, and < 0.8 as substantial reliability. Bland–Altman analyses were conducted to visualize repeatability and reproducibility and evaluate measurement errors.
Results
Participants
A total of 119 right eyes from 119 participants (63 males and 56 females) were enrolled in the study, with a mean age of 41.89 ± 5.16 years (range 18–83 years). The mean age of the normotensive subjects and hypertensive subjects was 28.22 ± 5.20 and 62.83 ± 7.97 years (P < 0.001), respectively. The BCVA of all eyes was ≥ 20/25, with refractive errors at −1.03 ± 0.91 (range 0.75–2.75) diopters (Table 1).
Reproducibility and Repeatability Assessment
Intra-rater reliability of arterial/arteriolar and venous/venular BA was excellent, achieving ICCs greater than 0.80 for all methods tested on cSLO images (Table 2). However, the inter-rater reliability varied between the three different methods. Using method 1, ICCs for both venous/venular and arterial/arteriolar BA measurements were higher than 0.80. However, the ICCs for arterial/arteriolar BA measurements using method 2 and method 3 were below 0.80, suggesting that method 1 was more reliable than method 2 and method 3 for arterial/arteriolar BA measurements; hence, method 1 was selected across the study. The inter-rater and intra-rater ICCs for vessel diameter, Df, and ST were all greater than 0.80, indicating high reliability (Table 2). Table 2 showcases the values of biases and the range of limits of agreement in measuring all parameters.
Figures 2–4 are Bland–Altman plots for Table 2. The three BA methods have a similar range of limits of agreement (LoA) of intra-rater repeatability (Fig. 2). Method 1 has better inter-rater reproducibility compared to the other two methods (Fig. 3), consistent with the results of ICCs. Finally, both intra- and inter-rater reliability was high for assessing vessel diameter, tortuosity, and total Df (Fig. 4).
Intra-rater repeatability of vessel branch angle (BA) measurement using Bland–Altman analyses. The Bland–Altman plot shows 95% limits of agreement (LoA) in arterial/arteriolar BA using methods 1 (a), 2 (b), and 3 (c) and venous/venular BA using methods 1 (d), 2 (e), and 3 (f) performed by the same operator
Inter-rater reproducibility of vessel branch angle (BA) measurement using Bland–Altman analyses. The Bland–Altman plot shows 95% limits of agreement (LoA) in arterial/arteriolar BA using methods 1 (a), 2 (b), and 3 (c) and venous/venular BA using methods 1 (d), 2 (e), and 3 (f) performed by two operators
Intra-rater repeatability and inter-rater reproducibility of vessel diameter, tortuosity, and total fractal dimension (Df) measurement using Bland–Altman analyses. The Bland–Altman plot shows 95% limits of agreement (LoA) of intra-rater repeatability in arteriolar diameter (a), venular diameter (b), arteriolar tortuosity (c), venular tortuosity (d), and total Df (e), and LoA of inter-rater in arteriolar diameter (f), venular diameter (g), arteriolar tortuosity (h), venular tortuosity (i), and total Df (j)
Vascular Parameters between Subjects with and without Hypertension
Table 1 shows that arterial/arteriolar BA and arteriolar vessel diameter in healthy subjects were 85.80 ± 7.79° and 116.80 ± 12.58 μm, respectively, significantly larger than those of hypertensive subjects (82.13 ± 10.83°, 108.2 ± 11.12 μm, both P < 0.05). Also, total Df in normotensive subjects was statistically larger than that of hypertensive subjects (normotensive 1.430 ± 0.037 versus hypertensive 1.361 ± 0.044, P < 0.001). However, arteriolar ST and all studied venous/venular geometric parameters in both kinds of subjects were of insignificant difference (all P > 0.05).
Table 3 shows that hypertension was statistically associated with smaller arterial/arteriolar BA, arteriolar vessel diameter, and total Df (all P < 0.05). After adjusting for age alone or age and gender, the aforementioned two arterial/arteriolar parameters and Df were still significantly correlated with hypertension negatively (all P < 0.05). Regardless of the regression analysis, arteriolar ST and all venous/venular geometric parameters had no association with hypertension (all P > 0.05).
Discussion
Numerous studies have used FP to investigate the relationship between retinal vascular geometry and ocular or systemic diseases [8,9,10, 19,20,21]. FP can be easily combined with computer-aided software, which has been adopted by many epidemiological studies [8,9,10, 19, 20]. However, pupil diameter and media opacity can significantly influence FP quality and geometric measurements. Since cSLO has the advantages of greater penetration and lower demands of a dilated pupil, a cSLO-based method might be a noninvasive alternative to measure retinal vascular geometry. Importantly, as cSLO images are obtained simultaneously with the OCT images, there is no additional time and effort required from the subjects; therefore, retrospective studies can also use cSLO images extracted from routine OCT measurement for assessing vascular geometry, maximizing the use of clinical data, and enhancing the efficiency of data collection.
Compared with FP, the cSLO-based approach has several advantages. First, retinal vascular geometry is subject to pulse or cardiac cycle [22,23,24]. The images in FP are obtained only at the moment of capture (diastole or systole). In contrast, vessels in the acquired cSLO images are dynamically superimposed (both diastolic and systolic images of vessels are superimposed to produce a cSLO image by the aid of real-time overlay technology of the Heidelberg), which might theoretically produce a more consistent result. Second, some diseases, such as retinal vein occlusion, have a distinct superotemporal quadrant predisposition, for which conventional summarized values from a certain region (usually zone B or zone C) in FP-based semi-automated software might weaken the geometric characteristics of individual vessels. In this way, using cSLO for retinal vessel measurements might facilitate the future study of individual vessels. Third, to monitor retinal or systemic diseases, the cSLO-based method can obtain the follow-up scan in the same location as the baseline scan to make the results more comparable (AutoRescan of the Heidelberg). Besides FP, other imaging techniques have been used to assess retinal vascular parameters, including adaptive optics scanning laser ophthalmoscopy (AOSLO), scanning laser Doppler flowmetry, and Doppler Fourier-domain optical coherence tomography. However, these imaging systems are not widely applied in clinical practices [25,26,27].
The main purpose of the present study is to verify the feasibility of using cSLO for measuring various geometric parameters. To the best of our knowledge, this is the first research applying cSLO to comprehensively measure the four most studied vascular geometric parameters. For image acquisition, a built-in scanning module, namely the circular scan, for the routine measurement of peri-optic nerve thickness was used. As one of the most clinically applied modules, the circular scan is high-speed and can acquire high-quality images within seconds. The acquired cSLO images were preprocessed in advance before various assessments (the images were enlarged to 200–300% times and sharpened using ImageJ) to show the boundaries and details of vessels more clearly. As the preprocessed images were more helpful for identifying vessel boundaries and luminal centerline, this setup is recommended for future studies manually analyzing vascular geometry using cSLO images.
For measuring vessel BA, we evaluated three methods. The FP-based BA measurement approach, tracing the vascular lumen before calculating BA, is similar to our method 1 [16], and the BA measurement approach using AOSLO is similar to our method 2 [25]. Finally, method 3 was an original method we envisioned for measuring BA. All three methods had a similar intra-rater repeatability. As for the reproducibility of BA measurements, the values of ICCs for all three measurement methods were greater than 0.80 for assessing venous/venular BA. However, only method 1 had ICC > 0.80 for inter-rater reproducibility for measuring the arterial/arteriolar BA. Therefore, we recommend method 1 for future BA evaluations using cSLO.
Interestingly, the values of ICCs for venous/venular BA were all greater than those of arterial/arteriolar one. The arterial/arteriolar own factors were assumed responsible for the performance of reproducibility and reproducibility. Angle evaluation using ImageJ requires placing two straight lines through three points. However, blood vessels are not always straight, especially arterial/arteriolar vessels, which often have a certain bend at the bifurcation. Thus, it might lead to disagreement in the identification of vessel boundaries, affecting the placement of measured lines and the consistency of the measurement, which could decrease the ICCs for arterial/arteriolar BA. Intriguingly, in a study published in 1979 exploring bifurcations in retinal arteries, researchers also suggested that most retinal arteries were not straight [28]. In light of this, for each method, we performed three measurements of vessel BA to obtain an average value to improve precision.
Although BA is not mandatory to be measured within zone B or zone C, only a small percentage of BAs were from zone A (0–0.5 DD away from the disc margin). Therefore, the reported BA was inclined to reflect arteriolar or venular characteristics. For healthy subjects, venous/venular BA values using method 1 were 77.12 ± 11.48°, similar to studies using FP and AOSLO [25, 29]. Also, arterial/arteriolar BA of normotensive subjects in our research (85.80 ± 7.79°) was in agreement with Stanton’s work (84°) [30]. Furthermore, previous fluorescein angiography and FP studies reported a blood-pressure-dependent reduction in arterial/arteriolar BA, consistent with our study [30, 31].
Retinal vessel diameter was also analyzed in the study. The arteriolar and venular diameters of the healthy subjects in our study (arteriolar, 116.8 ± 12.58 μm; venular, 145.1 ± 16.32 μm) were slightly larger than vascular outer diameters measured by a built-in caliper tool of the OCT software (arterial, 109–115 μm; venous, 136–139 μm) [14, 32]; however, another study using full width at half maximum (FWHM) analysis to measure retinal arteriolar diameter on the OCT cross-section images revealed the outer and luminal diameters of arterioles were 136 μm and 106 μm, respectively [33], highlighting the need to report the measurement tool and its principle. The VasoMetrics used in our study calculates vascular diameters based on the FWHM principle. We found that arteriolar diameters were negatively correlated with hypertension even after adjusting for age alone or age and gender, consistent with population-based studies [3, 8]. Muraoka and associates investigated the effect of hypertension on vessel diameters in zone A using OCT; they observed that vascular luminal and outer diameters were similar between subjects with and without hypertension [14]. The analyzed zone might contribute to the discrepancy [32]. Furthermore, vessel diameter in our study was measured along its course instead of a cross-section based on the OCT method. Of note, the course-based approach might be more reliable because vascular profile changes along the vessel.
The effect of hypertension on retinal vessel tortuosity remains disputable. Cheung et al. described a negative relationship between hypertension and retinal arteriolar tortuosity [3, 9]. However, a recent population-based study of 54,714 participants showed that increased arteriolar and venular tortuosity were associated with higher blood pressure [8]. In the current study, no correlation was detected, although this can be attributed to the small sample size and the dichotomous variable (hypertension recorded as present or absent). Also, the aforementioned studies used curvature tortuosity to reflect vessel tortuosity; since we could not find an available plugin, ST was applied in our study. Reportedly, both methods differed in distinguishing between increased length from bowing and that from multiple inflection points [34].
Df is a geometric index that can quantify retinal vascular branching patterns, with a higher value indicating a more complex and denser retinal vascular network [10]. Findings to date have confirmed that decreases in total Df are correlated with several systemic diseases, including hypertension [2, 5, 10]. This association is also observed in our measurements of cSLO images. Besides total Df, FP-based semi-automated retinal vascular analysis software can also assess Df of the venule, arterioles, and main vessels separately [5]. A recent study found that the Df of main venular vessels might be more sensitive than other Df metrics in patients with macrovascular cardiac disease [5]. We only investigated total Df, similar to previously established studies [2, 10]. Future studies could explore retinal microvascular change in hypertension through subclassifying Df metrics.
In our study, Df was measured within a predetermined area (zone C), as in previous studies using FP; however, the angle of a default cSLO image is 30°, significantly smaller than the 45° image using a conventional fundus camera. For the acquired cSLO image aided by the internal fixation target, the optic disc is not perfectly centered in the image but slightly towards the nasal quadrant (Fig. 1a). Therefore, analysis of vascular geometry within zone C using cSLO images would encounter nasal quadrant missing data. However, the impact of missing data could be contained because of a constant scanning configuration. Future studies could acquire cSLO images with the optic disc well centered by adjusting the external fixation target; however, the internal fixation target is built into the OCT machine, and thus more consistent and applicable to a clinical context. Therefore, narrowing the analyzed region (such as performing Df measurements at the region 0.5–1.5 DD from the optic margin or zone B instead of zone C) might be another option.
There are limitations to our study. First, this study is a cross-sectional study with inherent drawbacks. Second, some metrics were measured only in the superotemporal or inferotemporal quadrant, unable to comprehensively clarify the vascular geometry characteristics in all quadrants of the retina. Third, the small sample size would attenuate the statistical power. Fourth, the results were not adjusted for other systemic factors, including fasting glucose, cholesterol, smoking, and body mass index. Moreover, the treatment status (naïve or treated) of hypertension was not collected. Therefore, the study could not reveal how these factors influenced retinal vascular geometry. Additionally, automated software is required to standardize the measurement steps further.
Conclusions
We evaluated a cSLO-based method for retinal vascular geometry and tested this in hypertensive and nonhypertensive participants. We demonstrated that hypertension is negatively correlated with arterial/arteriolar BA, arteriolar diameter, and total Df. Future longitudinal studies are required to validate this new methodology in monitoring ocular and systemic diseases.
References
Koch E, Rosenbaum D, Brolly A, Sahel JA, Chaumet-Riffaud P, Girerd X, et al. Morphometric analysis of small arteries in the human retina using adaptive optics imaging: relationship with blood pressure and focal vascular changes. J Hypertens. 2014;32:890–8.
Forster RB, Garcia ES, Sluiman AJ, Grecian SM, McLachlan S, MacGillivray TJ, et al. Retinal venular tortuosity and fractal dimension predict incident retinopathy in adults with type 2 diabetes: the Edinburgh type 2 diabetes study. Diabetologia. 2021;64:1103–12.
Cheung CY, Tay WT, Mitchell P, Wang JJ, Hsu W, Lee ML, et al. Quantitative and qualitative retinal microvascular characteristics and blood pressure. J Hypertens. 2011;29:1380–91.
Cheung CY, Xu D, Cheng CY, Sabanayagam C, Tham YC, Yu M, et al. A deep-learning system for the assessment of cardiovascular disease risk via the measurement of retinal-vessel calibre. Nat Biomed Eng. 2021;5:498–508.
Dinesen S, Jensen PS, Bloksgaard M, Blindbæk SL, De Mey J, Rasmussen LM, et al. Retinal vascular fractal dimensions and their association with macrovascular cardiac disease. Ophthalmic Res. 2021;64:561–6.
Lee SC, Tran S, Amin A, Morse LS, Moshiri A, Park SS, et al. Retinal vessel density in exudative and nonexudative age-related macular degeneration on optical coherence tomography angiography. Am J Ophthalmol. 2020;212:7–16.
Yoo E, Yoo C, Lee BR, Lee TE, Kim YY. Diagnostic ability of retinal vessel diameter measurements in open-angle glaucoma. Invest Ophthalmol Vis Sci. 2015;56:7915–22.
Tapp RJ, Owen CG, Barman SA, Welikala RA, Foster PJ, Whincup PH, et al. Associations of retinal microvascular diameters and tortuosity with blood pressure and arterial Stiffness: United Kingdom Biobank. Hypertension (Dallas, Tex: 1979). 2019;74:1383–90.
Cheung CY, Zheng Y, Hsu W, Lee ML, Lau QP, Mitchell P, et al. Retinal vascular tortuosity, blood pressure, and cardiovascular risk factors. Ophthalmology. 2011;118:812–8.
Cheung CY, Thomas GN, Tay W, Ikram MK, Hsu W, Lee ML, et al. Retinal vascular fractal dimension and its relationship with cardiovascular and ocular risk factors. Am J Ophthalmol. 2012;154:663-674.e661.
Moss HE, Treadwell G, Wanek J, DeLeon S, Shahidi M. Retinal vessel diameter assessment in papilledema by semi-automated analysis of SLO images: feasibility and reliability. Investig Ophthalmol Vis Sci. 2014;55:2049–54.
Goldenberg D, Shahar J, Loewenstein A, Goldstein M. Diameters of retinal blood vessels in a healthy cohort as measured by spectral domain optical coherence tomography. Retina (Philadelphia, Pa). 2013;33:1888–94.
Oruc Y, Kirgiz A. Alteration of retinal vessel diameter of the patients with pseudoexfoliation and optical coherence tomography images. Curr Eye Res. 2019;44:1253–7.
Muraoka Y, Tsujikawa A, Kumagai K, Akiba M, Ogino K, Murakami T, et al. Age- and hypertension-dependent changes in retinal vessel diameter and wall thickness: an optical coherence tomography study. Am J Ophthalmol. 2013;156:706–14.
Raff U, Harazny JM, Titze SI, Schmidt BM, Michelson G, Schmieder RE. Salt intake determines retinal arteriolar structure in treatment resistant hypertension independent of blood pressure. Atherosclerosis. 2012;222:235–40.
Sasongko MB, Wang JJ, Donaghue KC, Cheung N, Benitez-Aguirre P, Jenkins A, et al. Alterations in retinal microvascular geometry in young type 1 diabetes. Diabetes Care. 2010;33:1331–6.
Wu R, Cheung CY, Saw SM, Mitchell P, Aung T, Wong TY. Retinal vascular geometry and glaucoma: the Singapore Malay Eye Study. Ophthalmology. 2013;120:77–83.
McDowell KP, Berthiaume AA, Tieu T, Hartmann DA, Shih AY. VasoMetrics: unbiased spatiotemporal analysis of microvascular diameter in multi-photon imaging applications. Quant Imaging Med Surg. 2021;11:969–82.
Cheung CY, Sabanayagam C, Law AK, Kumari N, Ting DS, Tan G, et al. Retinal vascular geometry and 6 year incidence and progression of diabetic retinopathy. Diabetologia. 2017;60:1770–81.
Benitez-Aguirre PZ, Wong TY, Craig ME, Davis EA, Cotterill A, Couper JJ, et al. The Adolescent Cardio-Renal Intervention Trial (AdDIT): retinal vascular geometry and renal function in adolescents with type 1 diabetes. Diabetologia. 2018;61:968–76.
Altunel O, Arifoglu HB. Evaluation of retinal vessel diameters in eyes with active central serous chorioretinopathy. Retina (Philadelphia, Pa). 2021;41:861–6.
Frame MD, Sarelius IH. Arteriolar bifurcation angles vary with position and when flow is changed. Microvasc Res. 1993;46:190–205.
Knudtson MD, Klein BE, Klein R, Wong TY, Hubbard LD, Lee KE, et al. Variation associated with measurement of retinal vessel diameters at different points in the pulse cycle. Br J Ophthalmol. 2004;88:57–61.
Hao H, Sasongko MB, Wong TY, Che Azemin MZ, Aliahmad B, Hodgson L, et al. Does retinal vascular geometry vary with cardiac cycle? Investig Ophthalmol Vis Sci. 2012;53:5799–805.
Luo T, Gast TJ, Vermeer TJ, Burns SA. Retinal vascular branching in healthy and diabetic subjects. Investig Ophthalmol Vis Sci. 2017;58:2685–94.
Rizzoni D, Mengozzi A, Masi S, AgabitiRosei C, De Ciuceis C, Virdis A. New noninvasive methods to evaluate microvascular structure and function. Hypertension (Dallas, Tex: 1979). 2022;79:874–86.
Wang Y, Lu A, Gil-Flamer J, Tan O, Izatt JA, Huang D. Measurement of total blood flow in the normal human retina using Doppler Fourier-domain optical coherence tomography. Br J Ophthalmol. 2009;93:634–7.
Zamir M, Medeiros JA, Cunningham TK. Arterial bifurcations in the human retina. J Gen Physiol. 1979;74:537–48.
Li X, Wong WL, Cheung CY, Cheng CY, Ikram MK, Li J, et al. Racial differences in retinal vessel geometric characteristics: a multiethnic study in healthy Asians. Investig Ophthalmol Vis Sci. 2013;54:3650–6.
Stanton AV, Wasan B, Cerutti A, Ford S, Marsh R, Sever PP, et al. Vascular network changes in the retina with age and hypertension. J Hypertens. 1995;13:1724–8.
Hughes AD, Stanton AV, Jabbar AS, Chapman N, Martinez-Perez ME, Mc GTSA. Effect of antihypertensive treatment on retinal microvascular changes in hypertension. J Hypertens. 2008;26:1703–7.
Zhu TP, Tong YH, Zhan HJ, Ma J. Update on retinal vessel structure measurement with spectral-domain optical coherence tomography. Microvasc Res. 2014;95:7–14.
Tong YH, Zhu TP, Zhao ZL, Zhan HJ, Jiang FZ, Lian HL. Retinal arteriolar morphometry based on full width at half maximum analysis of spectral-domain optical coherence tomography images. PLoS ONE. 2015;10: e0144437.
Witt N, Wong TY, Hughes AD, Chaturvedi N, Klein BE, Evans R, et al. Abnormalities of retinal microvascular structure and risk of mortality from ischemic heart disease and stroke. Hypertension (Dallas, Tex: 1979). 2006;47:975–81.
Acknowledgements
Funding
This work was supported by National Natural Science Foundation of China (82020108006, 81730025 to C.Z). No funding or sponsorship was received for the publication of this article. The Rapid Service Fee was funded by the authors.
Author Contributions
Hongyu Kong, Wei Lou, Jiaojie Li, Xueyan Zhang, Haiying Jin and Chen Zhao all made substantial contributions to the study conception and design. All authors read and approved the submission of this manuscript.
Disclosures
Hongyu Kong, Wei Lou, Jiaojie Li, Xueyan Zhang, Haiying Jin and Chen Zhao all confirm that they have nothing to disclosure.
Compliance with Ethics Guidelines
The study was approved by the Ethics Committee of Eye and ENT Hospital, Fudan University, Shanghai, China, and was conducted in accordance with the Helsinki Declaration. All patients provided written informed consent prior to enrollment.
Data Availability
All data generated or analyzed during this study are included in this published article.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kong, H., Lou, W., Li, J. et al. Retinal Vascular Geometry in Hypertension: cSLO-Based Method. Ophthalmol Ther 12, 939–952 (2023). https://doi.org/10.1007/s40123-022-00642-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00642-4