Abstract
Introduction
To report the incidence, demographics, and cost of eyelid lacerations (ELs) in the USA.
Methods
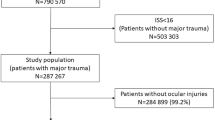
The Nationwide Emergency Department Sample is the largest publicly available emergency department database in the US. We conducted a retrospective longitudinal analysis to identify all emergency department (ED) visits in the sample from 2006 to 2014 with a primary or secondary diagnosis of EL. Descriptive statistics were calculated for hospital characteristics, patient demographics, and inflation-adjusted patient ED and in-patient (IP) charges.
Results
The incidence of primary and total ELs from 2006 to 2014 decreased by 50 per million and 7.1 per million, respectively. In the same period, the total ED and average ED charge, corrected for inflation, increased by almost $37 million and $1600 per person, respectively.
Motor vehicle accidents (MVAs) were the mechanism of injury (MOI) associated with the highest average ED and IP costs at $5391 and $42,677, respectively. However, object- (42.2%) and fall-related (28.8%) were the most reported MOI overall. Peak months of EL presentations were seen in May and July, and > 90% of primary ELs were classified as periocular. Most ELs occurred in men and children, representing 69% and 44% of all primary EL cases, respectively.
Conclusion
The incidence of ELs declined from 2006 to 2014. ELs occurred most frequently in children and young adults. The high proportion of object and fall-related injuries in this population highlights an area to develop strategies to reduce the frequency of preventable eye injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Over 2 million eye injuries are presented to emergency departments in the US every year |
Eyelid lacerations were amongst the top three oculoplastic-related eye injuries that presented to US emergency departments from 2006 to 2015 |
This study analyzed the incidence, characteristics, and costs associated with eyelid lacerations in the US from 2006 to 2014 |
What was learned from the study? |
The incidence of eyelid lacerations has decreased, but the inflation-adjusted costs associated with this injury have increased |
While the incidence of eyelid lacerations has declined, there is still a need for public health initiatives which can help mitigate the incidence of preventable ocular trauma |
Introduction
Eyelid lacerations (ELs) are a common form of ocular trauma that can result in complications of eyelid malposition and disruption to lacrimal outflow [1]. Over 2 million eye-related injuries are reported annually in the US, making trauma the most common reason for ophthalmology consultation in emergency department (EDs) [2,3,4,5]. ELs were among the top three urgent oculoplastics-related diagnoses presenting to US EDs from 2006 to 2015, accounting for almost 10% of such diagnoses [6]. Most ELs will be repaired surgically based on the anatomy involved in the laceration [2, 7,8,9]. Limiting the complications of ELs such as epiphora, ptosis, corneal injury, and infections is a primary concern for US ED physicians and ophthalmologists [9,10,11].Although EL injuries frequently present to EDs in the US, surgical repair can be delayed until ophthalmic care is available without increasing the risk of ocular complications [8, 10].
The current literature on ELs and ocular trauma focuses on cases of childhood trauma and the surgical management of specific trauma-related etiologies by institution [2, 12,13,14,15,16,17]. There is no analysis of national-level data focusing on EL incidence, demographics, mechanism of injury (MOI), and costs in the US population to our knowledge. We present data from the Nationwide Emergency Department Sample (NEDS) to determine the incidence, demographics, MOI, and associated healthcare costs of ELs that presented to US EDs from 2006 to 2014.
Methods
Data Set
NEDS is the largest publicly available ED database in the US, developed as part of the Healthcare Cost and Utilization Project (HCUP). NEDS contains data from billing records of 31 million annual ED visits from nearly 1000 hospital-owned EDs in the US, accounting for approximately 20% of all ED visits. The sample is stratified based on geographic region, trauma center designation, urban/rural location, and teaching status. Patient characteristics (such as age, sex, median income of household zip code, and primary payment method) and International Classification of Diseases 9 (ICD-9) diagnosis codes are included in the database [18]. From 2006 to 2014, NEDS contained up to 15 diagnosis codes per patient entry and 4 causes of injury (E-codes). The primary diagnosis for an encounter is the diagnosis primarily responsible for presentation to care, while secondary diagnoses are any other diagnoses accompanying the primary diagnosis for that encounter.
Study Design
We conducted a retrospective longitudinal study using NEDS to identify ED visits from 2006 to 2014 with a primary or secondary diagnosis of EL (ICD-9 codes 870.0, 870.1, and 870.2) [18]. ELs were divided into three categories: full-thickness EL not involving lacrimal passages, full-thickness EL involving lacrimal passages, and EL involving periocular area. Institutional Review Board approval was obtained, and this study adheres to the tenets of the Declaration of Helsinki. Informed consent was not required because NEDS does not contain direct patient identifiers. To maintain adherence with the HCUP data user agreement and maintain patient confidentiality, estimates for any characteristics with ≤ 10 patients are not reported here.
Data Analysis
National estimates were calculated using NEDS-supplied sampling weights. Unless otherwise stated, cases with primary ELs were analyzed. US Census Bureau population and age data were used to calculate total and age-specific incidence of primary ELs. Age was grouped into the following categories: children (10 years and younger), adolescents (11–20 years), young adults (21–44 years), adults (45–64 years), and the elderly (≥ 65 years). Descriptive statistics were calculated for hospital characteristics (region, teaching status, and trauma designation), patient demographics (age, sex, primary payer, and median household income quartile of patient’s zip code), and patient ED and IP charges. ED and IP charges were inflation-adjusted based on the January 2021 US dollar, using the Consumer Price Index for Hospital Services from the US Bureau of Labor Statistics. ED cost was defined as the total charge to the patient for the ED visit, whereas IP cost was defined as the total of hospital charges for an inpatient stay. Linear regression was used to estimate trends in incidence, disposition, demographics, total and mean ED/IP costs, associated ocular diagnosis, and MOI. MOIs studied include objects, falls, assault, MVAs, and others. Associated ocular injuries include contusion, superficial injury, nasal fracture, open wound, maxillary fracture, low vision, open fracture of the orbital floor, optic neuropathy, diplopia, enophthalmos, orbital edema, orbital hemorrhage, orbital cellulitis, retinal tear, hyphema, vitreous hemorrhage, and burn. E-codes for external causes of injury and ICD-9 codes for associated ocular diagnoses are displayed in Supplementary Tables S1 and S2 [18]. Multivariate logistic regression was used to assess factors associated with IP admission. Sex, primary payer, median household income of patient zip code, hospital region, hospital teaching status, hospital trauma level designation, associated ocular injuries, and MOI were included as covariates. Stata version 15 (StataCorp LP) was used for all statistical analyses.
Results
Incidence
The incidence of total ELs decreased from 243.2 per million (95% CI 219.6–266.8) in 2006 to 185.9 per million (95% CI 167.3–204.5, p < 0.001) in 2014 (Fig. 1A). Primary EL incidence also decreased from 173.97 per million (95% CI 156.8–191.1) in 2006 to 123.71 per million (95% CI 111.2–136.3, p < 0.001) in 2014 (Fig. 1A). Children had the highest EL incidence in every year for the study period (Fig. 1B). The incidence of ELs in children decreased from 469.99 per million (95% CI 410.8–529.2) in 2006 to 356.48 per million (95% CI 304.5–408.4) in 2014 (Fig. 1B). Children represented 43.7% of primary ELs and adolescents represented 19.5% of primary ELs (Fig. 2).
The monthly variation of primary ELs for all calendar months over our study period is presented in Fig. 3. The incidence of primary EL presentations was highest in July and May representing 3.53 per 10,000 cases (95% CI 3.33–3.74) and 3.34 per 10,000 cases (95% CI 3.15–3.53), respectively (Fig. 3). Presentations to the ED were less frequent in February and December, 2.67 per 10,000 (95% CI 2.51–2.82) and 2.89 per 10,000 (95% CI 2.73–3.05), respectively (Fig. 3).
Types of EL
Periocular ELs represented > 91% of primary ELs reported from 2006 to 2014 (data not shown). Full thickness ELs and ELs involving lacrimal passages were less frequently reported in the US at 6.5% and 2.6%, respectively (data not shown). Periocular EL presentations showed a downward trend from 48,129 (95% CI 43,390–52,867) cases in 2006 to 35,722 (95% CI 32,143–39,301, p < 0.001) cases in 2014 (data not shown). Figure 4 illustrates the type of EL by age group. Periocular ELs represented over 90% of primary ELs for almost all age groups except for the young adult and adult populations. Full thickness and lacrimal passage ELs were most frequently seen in adults (Fig. 4).
Demographics
Most primary ELs occurred in males (69%) (Table 1). Private insurance was the primary payer for health services for all age groups except the elderly, where the primary payer was Medicare (Table 1). Almost 38% of children with primary EL were covered with Medicaid (Table 1). The young adult group had the highest percentage of self-pay patients at 29.3% (Table 1). Households in the southern region of the US had the highest incidence of primary EL for all age groups (Table 1). Almost 62% of patients with primary EL presented to a non-trauma metropolitan teaching hospital (Table 1). Primary EL incidence was highest for the fourth median household income for almost all age-specific groups (Table 1).
MOI
The MOI for primary ELs observed during the study period is presented in Fig. 5. Object-related injuries were the most common MOI overall as well as among all age groups, except for the elderly, accounting for 42.2% of primary ELs (Fig. 5). Fall-related injuries represented almost 30% of primary ELs and were significantly higher for elderly patients (74.2%) (Fig. 5). Falls were the second most common MOI for children (40.6%) and adults (29.6%) (Fig. 5). Assault was responsible for 9.2% of primary ELs and was the second-highest MOI for adolescents and young adults (Fig. 5).
Associated Ocular Injuries
Contusions were the most common associated ocular injury for all age groups. Associated contusions were highest in young adults (6.3%), adults (5.9%), and the elderly (5.8%) (Table 2). Superficial injuries were the second most common associated ocular injury for most age groups and were highest for adults (3.4%) and young adults (3.2%) (Table 2). Associated superficial injuries were reported in < 3% of primary ELs and associated wounds < 2% (Table 2). Nasal fractures, open globe injuries, and maxillary fractures associated with ELs represented less than 1% of primary ELs (Table 2).
Disposition and Factors Associated with Admissions
Almost 95% of all primary ELs that presented to EDs had routine disposition, with > 90% of patients in most age groups being discharged directly from the ED after routine care. Notably, only 1.7% of all EL presentations were admitted to the hospital to which they presented and 5.3% of elderly patients were transferred (data not shown). Elderly (2.9%) and young adults (2.4%) had the highest rate of being admitted for inpatient service (data not shown).
Most patients admitted were young adults (33.7%) followed by children at (23.9%) (Table 3). Patients admitted to the hospital were mostly male (68.6%), had private insurance (33.1%), were from the lowest income quartile (33.8%), lived in southern states (31.2%), and presented to metropolitan teaching hospitals (76.5%) (Table 3). Patients who presented to a Level I trauma center had an increased likelihood of admission (OR: 3.77, 95% CI 1.96–7.27, p < 0.001). A MVA was the only MOI associated with a higher risk of being admitted (OR: 7.80, 95% CI 2.41–25.26, p < 0.001). ELs associated with hyphema (OR: 66.25, 95% CI 8.98–488.91, p < 0.001), diplopia (OR: 11.77, 95% CI 1.00–139.04, p = 0.05), open globe (OR: 11.07, 95% CI 3.89–31.55, p < 0.001), and maxillary fractures (OR: 9.94, 95% CI 3.89–31.55, p < 0.001) were linked to a higher chance of being admitted (Table 3).
Emergency Department and In-Patient Costs
The total ED charges, corrected for inflation, for primary EL presentations increased from $66.9 million (95% CI 58.0–76.0) to $103.8 million (95% CI 89.2–118.4, p < 0.001) from 2006 to 2014 (Fig. 6A). The average ED charge per patient, corrected for inflation, also increased from $1629 (95% CI 1513–1745) in 2006 to $3195 (95% CI 2932–3458, p < 0.001) in 2014 (Fig. 6B). The total charges for IP ELs did not change significantly over the study period (Fig. 6C). The average IP per visit increased from $34,742 (95% CI 27,647–41,836) in 2006 to $49,346 (95% CI 28,339–70,353) in 2014 (Fig. 6D). From 2006 to 2014, the total US ED costs for children increased from $17.44 million (95% CI 14.33–20.55) to $21.10 million (95% CI 17.16–24.96, p = 0.011) (data not shown).
A Total inflation-adjusted emergency department (ED) costs for visits with primary eyelid lacerations diagnosis from 2006 to 2014 (with standard error). B Mean inflation-adjusted ED cost per visit for primary ELs from 2006 to 2014 (with standard error). C Total inflation-adjusted in-patient (IP) costs for visits with primary EL diagnosis from 2006 to 2014 (with standard error). D Mean inflation-adjusted IP cost per visit for primary EL diagnosis from 2006 to 2014 (with standard error)
The highest total costs were observed for young adults with $226.6 million (95% CI 208.2–244.9) for ED costs and $87.7 million (95% CI 67.6–107.7) for IP costs (Fig. 7A). Elderly patients faced the highest average ED cost per patient at $3703 (95% CI 3529–3877) (p < 0.0001) (Fig. 7B). Adults and young adults had the highest IP charge per visit (Fig. 7C). Total US ED costs for primary ELs were highest for fall-related injuries at $193.6 million (95% CI 179.6–207.7) and object-related injuries at $192.9 million (95% CI 179.8–207.1) (Fig. 8A). Total US IP costs of primary EL injuries were highest for MVAs at $84.4 million (95% CI 64.8–104.0) (Fig. 8B). MVA was the MOI associated with the highest average ED and IP costs at $5391 (95% CI 5040–5742) and $42,677 (95% CI 35,152–50,202), respectively (Fig. 8C, D).
A MOI specific breakdown of the mean emergency department (ED) charge per visit for primary eyelid lacerations in the US from 2006 to 2014. B Total ED charge per visit for primary EL between 2006 and 2014. C Mean inpatient charge per visit for primary EL between 2006 and 2014. D Total inpatient charge per visit for primary EL between 2006 and 2014
Discussion
ELs can lead to complications that decrease visual acuity and require long-term management. Our study analyzes data from NEDS to examine the incidence, demographics, and associated healthcare costs of ELs presenting to US EDs from 2006 to 2014. We note a decline in incidence in EL presentations alongside increasing total and average ED costs. Over 70% of ELs were due to object- and fall-related injuries, with children and elderly patients representing the most at-risk population for preventable eyelid injuries.
The incidence of total EL presentations decreased from 243.23 per million in 2006 to 185.91 per million in 2014, with the steepest decline noted from 2008 to 2009. A similar downward trend of ocular injuries was observed in US EDs from 1992 to 2001, where the incidence declined at a rate of 4.2% per year [19]. McGwin and colleagues referenced the Occupational Health and Safety Act (OHSA) of 1970 as a conceivable cause of the trend due to their endorsement of the American National Standards Institute's (ANSI) recommendation of using certified protective eyewear in workplace settings [19]. In addition to the policies and legislation put forth by the US government, there have been advances in the design and functionality of protective eyewear for athletes and Americans in the workplace [20]. Despite the benefits reported, compliance remains an issue often due to a perceivably weakened appearance and altered field of view [20, 21]. Our observation of a steep decline in ELs between 2008 and 2009 corresponds closely with the end of the Great Recession in the US, which began in 2007. This crisis devastated the US workforce and led to almost 2 million jobs being lost by the last third of 2008 [22]. The sharp drop in the number of ELs may be attributable to the recession as multiple studies have reported work-related injuries compromise up to 18–28% of total eye injuries that present to US EDs [5, 23]. We also observe the greatest number of ELs in July (3.53 per 10,000) and the lowest in February (2.67 per 10,000). These peak and nadir months are consistent with the seasonal distribution of traumatic and ocular injuries reported in the literature [24,25,26].
We observe a decline in the incidence of primary ELs, accompanied by an increase in total and average US ED charges after correcting for inflation. In 2021, Ahmad and colleagues reported similar findings for oculoplastic-related ED visits in the US between 2006 and 2015 [6]. While the incidence of oculoplastic-related diagnoses declined from 4.71 to 3.16 per 100,000 people, they report an almost twofold increase in median inflation-adjusted cost per visit from 2006 to 2015 [6]. Among children, we also report a decrease in incidence along with an increase in costs. The incidence of ELs for children declined from 469.99 per million in 2006 to 356.48 per million in 2014, while the total US ED charges for children increased from $17.44 million in 2006 to $21.06 million in 2014. However, Luo and colleagues observed a decline in incidence of eye injuries in children in the US along with a significant decrease in medical costs from 2002 to 2004 ($193 million) to 2012–2014 ($66 million) [27]. This suggests the cost of managing ELs in children has increased while the cost of caring for pediatric eye injuries overall has decreased [27].
Age-group demographics of ELs from our analysis were consistent with the literature. In our findings, the highest incidence of ELs was noted in children and adolescents. This is consistent with studies reporting a decline in incidence of ocular injuries among children and studies that still classify children and adolescents as high-risk populations [4, 28,29,30,31]. Children represent almost 47% of the primary ELs in our analysis. In an 11-year retrospective study of 222 patients of all age groups who underwent surgical repair of canalicular lacerations at Wills Eye Hospital, the majority of lacerations occurred in children and young adults, with a median age of 20 years [16]. The most common MOI overall was assault (23.4%), and the most frequent MOI among children was dog bites and scratches [16]. In our analysis of all ELs, object-related injuries represented the most common MOI overall, and the most common MOI for children. Similarly, in a review of 258 pediatric eye injuries leading to hospital admission in Newark, NJ, object-related injuries were the most common MOI among pediatric patients, and sports-related injuries were most common in children > 10 years of age [17]. Other studies have reported a high incidence of object and/or sport-related eye injuries in children and adolescents [4, 12, 14, 17, 30,31,32,33]. Children, adolescents, and young adults have remained a high-risk population for over a decade [28, 29]. In 2004, the American Academy of Pediatrics and the American Academy of Ophthalmology published a policy statement recommending the use of protective eyewear in sports where the risk of eye injury is present; most sport-related eye injuries have been documented in basketball and baseball players for pediatrics and young adults [26, 28]. ELs and abrasions made up 50.9% of eye injuries over a 1-year period among basketball players in the National Basketball Association, most caused by fingers or elbows [34]. The active lifestyles of children and adolescents increase their risk for serious, and potentially avoidable, eye-related injuries [35].
We observe falls to be the most common MOI for elderly patients, accounting for 74% of primary ELs in this age population. Among the age groups studied, elderly patients were more likely to be admitted as IP (2.9%) or transferred to a short-term hospital (2.1%). These findings are consistent with other analyses of eye trauma hospitalizations, which report an increasing number of eye trauma cases in patients ≥ 65 years due to falls [29, 36] and an increased likelihood for elderly patients to be admitted for eye-related trauma [37]. Interestingly, in 2021 Usmani et al. reported that the overall incidence of elderly ED fall-related eye trauma increased between 2006 to 2014, with a decline seen in 2015 [37]. Of all the eye trauma reported in this study, ELs were the second leading type of eye trauma [37]. Another analysis of eye-related ED visits in the US from 2006 to 2011 reported ocular trauma in patients ≥ 70 years had a 5.15 times higher odds of being admitted for in-patient care compared to younger patients in the study [3]. Increases in fall-related hospitalizations in the US have been observed as early as 2001, with a study reporting a > 50% increase in fall-related hospitalizations in patients ≥ 65 years from 2001 to 2008 [38]. These alarming rates highlight the need for focused interventions and policies to reduce preventable falls in the elderly as the US population continues to age.
In conclusion, we present the epidemiology and cost of ELs in the US between 2006 and 2014. Strengths of our analysis include the focus on primary ELs using a representative sample of the US. Limitations of our study include the use of a national database, which may contain errors in data entry and diagnosis of primary and/or secondary ELs and does not allow for long-term outcome analysis. Additionally, with use of the NEDS database, we were not able to capture the ELs that present to private practice or other settings outside of the ED. Our study period from 2006 to 2014 was selected to allow the ability to sub-categorize eyelid lacerations. With the ICD-10 revision, it is no longer possible to obtain specificity of coding for eyelid lacerations from a national database such as NEDS. However, detailed information of eyelid lacerations can still be obtained, on a smaller scale, from institutional chart reviews. Our observation of a decreased incidence of ELs is reflective of the successful US government policies put in place to reduce the incidence of preventable traumatic eye injuries.
Looking forward, a continued decline in EL incidence, beyond our study period, may have an impact on the management of such injuries. This stresses the importance of maintaining funding and the education and training of ED staff on the management of ELs. We observe an increase in the inflation-adjusted ED and IP costs for the ELs that were reported in NEDS over our study period. Reporting cost-related data from NEDS leaves out the costs associated with the out-patient management of ELs. Referrals to outpatient clinics for the management of less severe ELs, upon arrival to the ED, can be a potential way to decrease the total US ED costs.
Conclusion
The incidence of ELs in the US declined from 2006 to 2014, while the inflation-adjusted costs associated with this injury have increased. Object- and fall-related injuries represent the top MOI for ELs, notably in the children and elderly populations. US policies focusing on safety, in these two specific age groups, can reduce the incidence of preventable eye injuries.
References
Rishor-Olney CR, Hinson JW. Canalicular laceration. In: StatPearls. StatPearls Publishing; 2021.
Beadles KA, Lessner AM. Management of traumatic eyelid lacerations. Semin Ophthalmol. 1994;9(3):145–51.
Haring RS, Canner JK, Haider AH, Schneider EB. Ocular injury in the United States: emergency department visits from 2006–2011. Injury. 2016;47(1):104–8.
Brophy M, Sinclair SA, Hostetler SG, Xiang H. Pediatric eye injury-related hospitalizations in the United States. Pediatrics. 2006;117(6):e1263–71.
Nash EA, Margo CE. Patterns of emergency department visits for disorders of the eye and ocular adnexa. Arch Ophthalmol. 1998;116(9):1222–6.
Ahmad M, Zhao J, Iftikhar M, et al. Epidemiologic trends in oculoplastics-related emergency department visits in the United States, 2006–2015. Ophthal Plast Reconstr Surg. 2021. https://doi.org/10.1097/IOP.0000000000002047.
Cochran ML, Czyz CN. Eyelid laceration. In: StatPearls. StatPearls Publishing; 2021.
Chang EL, Rubin PAD. Management of complex eyelid lacerations. Int Ophthalmol Clin. 2002;42(3):187–201.
Nelson CC. Management of eyelid trauma. Aust NZ J Ophthalmol. 1991;19(4):357–63.
Chiang E, Bee C, Harris GJ, Wells TS. Does delayed repair of eyelid lacerations compromise outcome? Am J Emerg Med. 2017;35(11):1766–7.
Qin YY, Li ZH, Lin FB, et al. Risk factors for persistent epiphora following successful canalicular laceration repair. Int J Ophthalmol. 2021;14(1):106–11.
Sadiq MAA, Corkin F, Mantagos IS. Eyelid lacerations due to dog bite in children. J Pediatr Ophthalmol Strabismus. 2015;52(6):360–3.
Savar A, Kirszrot J, Rubin PAD. Canalicular involvement in dog bite related eyelid lacerations. Ophthal Plast Reconstr Surg. 2008;24(4):296–8.
Ramsay C, Murchison AP, Bilyk JR. Pediatric eye emergency department visits: retrospective review and evaluation. J Pediatr Ophthalmol Strabismus. 2021;58(2):84–92.
Yuan H, Zhang YZ, Jie H, Li SL. The application of tissue glue in eyelid laceration repair in children during the Coronavirus disease 2019 pandemic lockdown in Wuhan. Clin Cosmet Investig Dermatol. 2021;14:541–6.
Kennedy RH, May J, Dailey J, Flanagan JC. Canalicular laceration. An 11-year epidemiologic and clinical study. Ophthal Plast Reconstr Surg. 1990;6(1):46–53.
DeRespinis PA, Caputo AR, Fiore PM, Wagner RS. A survey of severe eye injuries in children. Am J Dis Child. 1989;143(6):711–6.
Medicode (Firm). ICD-9-CM: international classification of diseases, 9th revision, clinical modification. Medicode; 1996.
McGwin G, Hall TA, Xie A, Owsley C. Trends in eye injury in the United States, 1992–2001. Invest Ophthalmol Vis Sci. 2006;47(2):521–7.
Hoskin AK, Mackey DA, Keay L, Agrawal R, Watson S. Eye injuries across history and the evolution of eye protection. Acta Ophthalmol. 2019;97(6):637–43.
Woods SE, Diehl J, Zabat E, Daggy M, Engel A, Okragly R. Is it cost-effective to require recreational ice hockey players to wear face protection? South Med J. 2008;101(10):991–5.
Mandal B, Ayyagari P, Gallo WT. Job loss and depression: the role of subjective expectations. Soc Sci Med. 2011;72(4):576–83.
White MF Jr, Morris R, Feist RM, Witherspoon CD, Helms HA Jr, John GR. Eye injury: prevalence and prognosis by setting. South Med J. 1989;82(2):151–8.
Ramirez DA, Porco TC, Lietman TM, Keenan JD. Ocular injury in United States Emergency Departments: seasonality and annual trends estimated from a nationally representative dataset. Am J Ophthalmol. 2018;191:149–55.
Bhattacharyya T, Millham FH. Relationship between weather and seasonal factors and trauma admission volume at a Level I trauma center. J Trauma. 2001;51(1):118–22.
Patel V, Pakravan P, Mehra D, Watane A, Yannuzzi NA, Sridhar J. Trends in Sports-Related Ocular Trauma in United States Emergency Departments from 2010 to 2019: Multi-Center Cross-Sectional Study. Semin Ophthalmol. 2022. https://doi.org/10.1080/08820538.2022.2107400
Luo H, Shrestha S, Zhang X, Saaddine J, Zeng X, Reeder T. Trends in eye injuries and associated medical costs among children in the United States, 2002–2014. Ophthalmic Epidemiol. 2018;25(4):280–7.
American Academy of Pediatrics Committee on Sports Medicine and Fitness. Protective eyewear for young athletes. Pediatrics. 2004;113(3):619–22.
Iftikhar M, Latif A, Farid UZ, Usmani B, Canner JK, Shah SMA. Changes in the incidence of eye trauma hospitalizations in the United States from 2001 through 2014. JAMA Ophthalmol. 2019;137(1):48–56.
Pollard KA, Xiang H, Smith GA. Pediatric eye injuries treated in US emergency departments, 1990–2009. Clin Pediatr. 2012;51(4):374–81.
Armstrong GW, Kim JG, Linakis JG, Mello MJ, Greenberg PB. Pediatric eye injuries presenting to United States emergency departments: 2001–2007. Graefes Arch Clin Exp Ophthalmol. 2013;251(3):629–36.
Murchison AP, Bilyk JR. Pediatric canalicular lacerations: epidemiology and variables affecting repair success. J Pediatr Ophthalmol Strabismus. 2014;51(4):242–8.
Tu AH, Girotta JA, Singh N. Facial fractures from dog bite injuries. Ann Emerg Med. 2003;41(5):764–5. https://doi.org/10.1016/s0196-0644(03)90201-9.
Zagelbaum BM, Starkey C, Hersh PS, Donnenfeld ED, Perry HD, Jeffers JB. The National Basketball Association eye injury study. Arch Ophthalmol. 1995;113(6):749–52.
Ashaye AO. Eye injuries in children and adolescents: a report of 205 cases. J Natl Med Assoc. 2009;101(1):51–6.
Chocron IM, Goduni L, Poulsen DM, MbekeanI JN. Patterns of ocular trauma in elderly patients in an urban population-the Bronx experience. Arq Bras Oftalmol. 2020;83(2):113–9.
Usmani B, Latif A, Iftikhar M, et al. Eye trauma in falls presenting to the emergency department from 2006 through 2015. Br J Ophthalmol. 2021;105(2):198–204.
Hartholt KA, Stevens JA, Polinder S, van der Cammen TJM, Patka P. Increase in fall-related hospitalizations in the United States, 2001–2008. J Trauma. 2011;71(1):255–8.
Acknowledgements
We thank Joseph Canner, BS, MHS, for assistance in study inception and IRB procurement.
Funding
No funding or sponsorship was received for this study or publication of this article. The journal’s Rapid Service Fee was funded by the authors.
Author Contributions
Keale Cade: Analyzed data and drafted the manuscript; Kamil Taneja: Obtained and analyzed the data from the NEDS database, and drafter the manuscript; Adrianna Jensen: Created figures and tables; Fatemeh Rajaii: Principal investigator, conceived of and designed the analysis, and edited the manuscript.
Prior Presentation
Howard University Research Symposium 2022, Washington, DC April 2022.
Disclosures
Keale Cade, Kamil Taneja, Adrianna Jensen, and Fatemeh Rajaii have nothing relevant to disclose.
Compliance with Ethics Guidelines
Institutional Review Board approval was obtained from The Johns Hopkins School of Medicine IRB (IRB00221778), and the study adhered to the tenets of the Declaration of Helsinki. Informed consent was not required because NEDS does not contain direct patient identifiers.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cade, K.L., Taneja, K., Jensen, A. et al. Incidence, Characteristics, and Cost of Eyelid Lacerations in the United States from 2006 to 2014. Ophthalmol Ther 12, 263–279 (2023). https://doi.org/10.1007/s40123-022-00605-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00605-9