Abstract
Introduction
To evaluate the corneal epithelial thickness (CET) profiles and their correlations with axial length (AL) and anterior corneal radius of curvature (Rm F) across different refractive error groups.
Methods
A total of 1225 eyes of 616 normal patients were included. CET mapping, AL, and Rm F were obtained using spectral-domain optical coherence tomography, optical biometry, and Scheimpflug corneal tomography, respectively. In the CET map, one central (2 mm), eight paracentral (2–5 mm), and eight peripheral (5–6 mm) quadrants were evaluated separately. The subjects were divided into four groups based on their refractive status: hyperopia (spherical equivalent [SE] ≥ +0.50 D), emmetropia (SE > −0.50 D and < +0.50 D), low myopia (SE ≤ −0.50 D and > −3.0 D), and moderate–high myopia (SE ≤ −3.0 D) groups. Linear mixed model analysis with Bonferroni correction was used to compare CET according to refractive error groups. The correlations between the CET profile and the AL and Rm F were analyzed.
Results
The central CET was 53.7 ± 3.3 μm in hyperopia (n = 34), 53.2 ± 2.9 μm in emmetropia (n = 353), 52.8 ± 2.9 μm in low myopia (n = 677), and 52.0 ± 3.1 μm in moderate–high myopia (n = 161). Although thinning was observed in CET in all quadrants from hyperopia to moderate–high myopia, it was only significant in the superior and superonasal quadrants at the 2–5 mm and 5–6 mm-diameter rings. While AL and CET were significantly positively correlated (r range 0.17–0.28) in the moderate–high myopia group, Rm F and CET were significantly positively correlated (r range 0.08–0.10) in the low and moderate–high myopia groups.
Conclusion
CET varied according to different refractive error groups and was positively correlated with AL and Rm F, particularly in the moderate–high myopia group.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Why carry out this study? |
Measurement profiles of corneal epithelial thickness (CET) in refractive error groups provide important information for refractive surgery planning and follow-up. |
This study was designed to investigate epithelial thickness profiles across different refractive error groups and correlate the CET of various quadrants with biometry. |
What was learned from the study? |
The corneal epithelium becomes progressively thinner from hyperopia to myopia, with the superior quadrants showing a more pronounced change. |
The corneal epithelium thickened in most quadrants as the axial length and anterior corneal radius of curvature (Rm F) increased in the moderate–high myopia group, while the corneal epithelium thickened in most quadrants only as Rm F increased in the low myopia group. |
Introduction
The corneal epithelium is the outer layer of the cornea that provides protection against external factors and increases optical quality by ensuring a smooth front surface [1]. The corneal epithelium contributes to 1.03 diopters (D) and 0.85 D to refractive power in the central 2 mm and 3.6 mm-diameter zones, respectively [2]. Its thickness shows a nonuniform distribution across the corneal surface ranging from 48 to 60 μm [2, 3]. Techniques available to measure the corneal epithelium include in vivo confocal microscopy, very-high-frequency ultrasound, optical coherence tomography (OCT), and Scheimpflug imaging [1]. Optical coherence tomography, a noncontact method, accurately shows the corneal epithelial thickness (CET) pattern thanks to its high axial resolution [4]. Previous studies have reported good repeatability of corneal and epithelial thickness measurements using OCT imaging systems [5, 6]. Clinically, measurement of CET and its distribution across the corneal surface aids in the early diagnosis of ectatic disorders, in screening before refractive surgery, and in evaluating the remodeling processes after refractive surgery [7]. In early ectasia, epithelial thinning on the cone apex may mask the topographical changes in the anterior corneal surface [8]. Also, CET imaging performed before refractive surgery may be useful in the planning of refractive surgery and may contribute positively to the outcome of the surgery [9]. Accurate knowledge of CET provides the opportunity to accurately treat underlying stromal irregularities in phototherapeutic keratectomy (PTK) [1]. CET mapping can also convey information on whether myopic regression after excimer laser treatment is due to epithelial hyperplasia or corneal biomechanical changes and can improve the safety and predictability of retreatment [1, 10, 11]. There are some concerns regarding the correction of refractive errors with refractive surgery due to interindividual CET profile variability and the associated potential refractive effect [12, 13]. Hence, precisely identifying refractive errors and examining the epithelial thickness maps before refractive surgery are essential to avoid under- or overcorrection and provide helpful information to measure remodeling post-corneal refractive surgery [14].
Refractive surgery is becoming widely available globally and is performed within specific limits for refractive errors such as myopia, hyperopia, and astigmatism. However, there is limited research on the correlation of CET with refractive errors, axial length (AL), and corneal curvature [15,16,17,18,19]. Therefore, this study aimed to investigate the epithelial thickness profiles across different refractive error groups and correlate the CET of various quadrants with biometry.
Methods
This study was approved by the Ethical Board of Non-interventional Clinical Research of the Eskişehir Osmangazi University and was conducted in adherence to the tenets of the Declaration of Helsinki. Acquisition of informed consent was waived.
Subjects
Subjects were recruited from an extended sample of a population-based keratoconus prevalence study conducted across different faculties of Eskişehir Osmangazi University. The subjects who did not meet the criteria for keratoconus and ectasia susceptibility based on our previously published keratoconus prevalence study [20] were considered topographically normal. Hence, only these subjects were included in the study. Eyes with steepening on the tangential map, thinning on the relative pachymetry map, and an elevation of more than 10 µm on the posterior elevation map on the Holladay 6 map display, as well as those with a Topographical Keratoconus Classification (TKC) value of 1 and above in Scheimpflug corneal tomography (Pentacam) were classified as keratoconus [21]. Eyes that did not fulfill the Holladay map or TKC criteria but had a posterior elevation difference of more than 12 μm and a Belin/Ambrosio Expanded Ectasia D value above 1.6 standard deviation (SD) were considered as ectasia susceptibility. The other eyes were classified as topographically normal. The presence of keratoconus or ectasia susceptibility according to corneal topography, any corneal disease, and history of refractive surgery were exclusion criteria.
All subjects underwent a standardized examination protocol in the following order: autorefractokeratometry (Tonoref II tonometer–refractometer; Nidek Co, Ltd, Gamagori, Japan), uncorrected and best spectacle-corrected visual acuity assessment with logMAR chart, slit-lamp examination, optical biometry (Lenstar LS 900, Haag-Streit AG, Switzerland), Scheimpflug corneal tomography (Pentacam HR, Oculus, Wetzlar, Germany), and anterior segment optical coherence tomography (AS-OCT, Optovue Inc., Fremont, CA) imaging. Pentacam imaging was repeated twice for each eye, whereas optical biometry and anterior segment optical coherence tomography imaging were repeated three times. Spherical equivalent (SE) refraction was calculated in diopters by adding half of the cylindrical value to the spherical value. The subjects were divided into four groups based on their refractive status: SE ≥ +0.50 D was defined as hyperopia, SE > −0.50 D and < +0.50 D as emmetropia, SE ≤ −0.50 D and > −3.0 D as low myopia, and SE ≤ −3.0 D as moderate–high myopia. Myopia was divided into axial, refractive, and mixed according to ocular biometry. Myopia was classified as axial myopia in the presence of maximum keratometry (Kmax) < 46 D and AL ≥ 24 mm, and refractive myopia as Kmax ≥ 46 D and AL < 24 mm. The remaining cases were considered mixed myopia.
Anterior segment OCT imaging was employed for epithelial thickness data, while Pentacam Scheimpflug imaging was used for anterior radius of curvature and keratometric data. Pachymetric measurements with AS-OCT covered an area of 6 mm divided into a total of 17 sectors: one central 2 mm-diameter zone, eight paracentral zones within an annulus between the 2–5 mm-diameter rings, and eight peripheral zones within an annulus between the 5–6 mm-diameter rings. Only scans with examination quality specifications of “OK” were chosen for analysis in Pentacam Scheimpflug imaging. For biometry and OCT measurements, the absence of blinking and fixation loss were considered as quality measures. The results for data analysis were obtained by averaging three repeated measurements in which intra-session differences were no greater than 0.02 mm for biometry and 3 μm for OCT [22, 23].
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics Version 26.0 (IBM Corp., Armonk, NY, USA). Continuous data were expressed as mean ± SD, and categorical data were expressed as proportions. The normal distribution of the variables was tested using Shapiro–Wilk tests. The relationship between CET and the anterior radius of curvature (Rm F) and AL parameters was assessed using Pearson’s or Spearman’s correlation analysis based on the normality of the data. The false discovery rate method was used to eliminate the effect of multiple comparisons. This method has been shown to provide a better balance between type I or type II error handling if the number of tests, and therefore the denominator required for Bonferroni correction, is substantial [24, 25]. Linear mixed model analysis with Bonferroni correction was used to compare CET measurements according to refractive error groups. The covariance type was selected considering the smallest values of the Akaike information criterion (AIC) and Schwarz Bayesian information criterion (BIC). Statistical significance was assumed at a level of p < 0.05.
Results
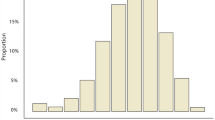
A total of 1225 eyes of 616 patients fulfilled the inclusion and exclusion criteria and were included in the analyses. The mean age of subjects was 21.5 ± 2.1 years (range 18–30 years) and 69% were female. The mean Rm F, Kmax, SE, AL, central corneal thickness (CCT), central stromal thickness, (CST) and central CET among all subjects were 7.8 ± 0.3 mm (range 7.2 to 8.7 mm), 44.2 ± 1.6 D (range 39.6 to 51.1 D), −1.3 ± 1.7 D (range −11.9 to 7.1 D), 23.9 ± 0.9 mm (range 21.0 to 27.6 mm), 527.0 ± 33.4 μm (range 428.8 to 637.9 μm), 474.2 ± 32.7 μm (range 377.5 to 585.1 μm), and 52.8 ± 3.0 μm (range 43.2 to 63.8 μm), respectively. Thirty-four of 1225 eyes were evaluated as hyperopia, 353 as emmetropia, 677 as low myopia, and 161 as moderate–high myopia. The mean age and corneal biometric parameters according to refractive errors are given in Table 1. The gender distribution and mean age of the subjects according to the refractive error groups were 53% female and 21.1 ± 2.3 years in hyperopia, 60% female and 21.4 ± 2.3 years in emmetropia, 73% female and 21.5 ± 1.9 years in low myopia, and 75% female and 21.5 ± 2.5 years in moderate–high myopia, respectively.
There was a thinning trend in all quadrants from hyperopia to moderate–high myopia. However statistical significance was only noted in the superior and superonasal quadrants of both the 2–5 mm and 5–6 mm-diameter rings (Table 2). The 2–5 mm and 5–6 mm superior quadrants did not differ significantly between the individual refractive error groups. The 2–5 mm superonasal quadrant showed a statistically significant difference only between hyperopia and moderate–high myopia groups (p = 0.02). On the other hand, the 5–6 mm superonasal quadrant showed a statistically significant difference between moderate–high myopia and the other three groups (hyperopia [p = 0.01], emmetropia [p = 0.02] and low myopia [p = 0.02]). For all refractive error groups, CET was the thinnest in the 5–6 mm superior quadrant, and the thickest in the 5–6 mm inferior quadrant. In addition, the nasal epithelium was thicker than the temporal epithelium for both 2–5 mm and 5–6 mm-diameter rings in all refractive errors.
There was a significant positive linear correlation between CCT and central CET for all refractive error groups. Among other biometric parameters, AL had a positive correlation with CET only in the moderate–high myopia group, whereas Rm F was positively associated with CET in hyperopia and moderate–high myopia groups. (Fig. 1). Figure 2 shows the correlations of AL and Rm F with CET for each quadrant in all refractive error groups. While biometric parameters (AL and Rm F) and most corneal epithelial quadrants were positively correlated in the moderate–high myopia group, most corneal epithelial quadrants were positively correlated with Rm F and not with AL in the low myopia group. In a sub-analysis performed in the moderate–high myopia group, a significant positive correlation was detected between AL and Rm F (Supplementary Material). Although AL and Rm F were more positively correlated with CET in the upper quadrants compared to the lower quadrants in the emmetropia and hyperopia groups, there was no statistical significance in any quadrant. In the axial, refractive, and mixed myopia groups, there was a positive correlation between Rm F and central CET separately for all groups. Nevertheless, it was statistically significant only in the axial and mixed myopia groups (Fig. 3).
Correlation scheme illustrating the linear relationship between the corneal epithelial thickness map and ocular biometric determinants (axial length and anterior corneal radius of curvature). Warmer colors indicate an increasing positive (uphill) linear relationship, while cooler colors indicate an increasing negative (downhill) linear relationship
Discussion
The present study demonstrated that the corneal epithelium becomes progressively thinner from hyperopia to myopia, with the superior quadrants showing a more pronounced change. There was a significant positive correlation between central CET and AL in the moderate–high myopia group only, whereas Rm F was shown to correlate with CET in the hyperopia and moderate–high myopia groups. It was observed that the corneal epithelium thickened in most quadrants as the AL and Rm F increased in the moderate–high myopia group, while the corneal epithelium thickened in most quadrants as only Rm F increased in the low myopia group.
There is a correlation between CET and total thickness, and a relationship between CET and other ocular parameters has been frequently investigated in the literature [3, 16, 17]. A study of Korean children aged 6–17 years found that CET is not associated with ocular factors such as AL, mean keratometry, and refractive error [19]. These results could be related to the pediatric cohort studied in whom refractive errors can often progress [19]. On the other hand, a randomized study evaluating children aged 7–15 years showed that AL and CET were not correlated in any quadrant, while the corneal curvature radius was positively correlated with CET in the paracentral and peripheral corneal quadrants [26]. In our study, AL and Rm F were positively correlated with CET, particularly in the moderate–high myopia group. The increases in AL does not directly increase CET; it causes flattening of the cornea and indirectly increases the CET due to increasing Rm F. In our sub-analysis that supports this relationship, a positive correlation was observed between AL and Rm F in all refractive error groups.
To date, there is very limited information on the relationship between refractive errors and CET [17,18,19]. Wang et al. reported no statistical difference was found between the CET of highly myopic patients and normal subjects, but a correlation between AL and CET was not investigated [17]. Gowrisankaran et al. found that refractive error was associated with blink rate [27]. Furthermore, Wu et al. concluded that thin CET in the high myopia group compared to low and moderate myopia groups was due to frequent blinking [16]. Although it was found in the same study that anterior corneal curvature was not associated with CET, no evaluation was performed according to myopia subgroups [16]. Similarly, in another study, no correlation was found with the degree of myopia, whereas CET was significantly thinner in some paracentral and mid-peripheral quadrants in high myopia compared to other myopic groups [18]. In the present study, the CET was thinnest in the moderate–high myopia group with high AL compared to the other groups. Wu et al. [16], suggested that a longer AL may increase eyelid friction and cause thinning of the epithelium which corresponded with this study findings. Hence, it is tempting to speculate that a longer AL in myopic eyes may bring the cornea closer approximation to the eyelids, enhancing the effect of the lid wiper phenomenon in shaping the corneal epithelium.
Many studies have reported that the corneal epithelium is thinner in the superior and temporal quadrants than when compared to their counterparts [5, 23, 26, 28,29,30]. There are several theories regarding the thinness of the superior quadrant compared to the inferior quadrant. One reason for this could be that the stronger superior eyelid causes more friction in the superior corneal quadrants, leading to an increased lid wiper effect [10]. Secondly, the upper eyelid covers a larger portion of the eye than the lower eyelid, and due to gravity, the eyelid exerts greater force on the upper cornea [31]. Lastly, the fact that the contact time of the tear film is shorter in the upper quadrant than in the lower quadrant causes less lubricating and nourishing effects in the upper quadrant, resulting in faster desquamation of the epithelium [30]. Cui et al. also found that CET was significantly thinner in the upper corneal quadrants in patients with dry eye compared to normal patients, which also shows the relationship between tear film and CET and supports the third theory [32]. In this study, similar to previous reports, the superior and inferior quadrants had the thinnest and thickest thicknesses, respectively. Additionally, the nasal quadrant was thicker than the temporal quadrant in all refractive groups. Theoretically, the nasal cornea is thicker because it is more protected than the temporal cornea [29].
Assessment of the CET profile before refractive surgery and knowing how it changes after surgery may contribute positively to the refractive outcome and may be helpful in the planning of surgery [1, 9, 10]. The Arba Mosquera and Awwad study reported that the theoretical calculation of induced refractive errors varied between −1.32 and +1.27 D according to different epithelial profiles [13]. Khamar et al. noted that if refractive surgery is performed with standard flap thickness in an eye with thick CET, it will lead to under-correction due to less stromal ablation [14]. A study by Guglielmetti et al. also showed improvement in postoperative vision by planning the depth of epithelial ablation to treat irregular astigmatism with transepithelial PTK [33]. In our study, it was observed that there was a difference in CET according to the refractive error groups, although it was not clinically significant. Therefore, the importance of personalized surgical planning in refractive surgery is shown.
The strength of this study is that the study cohort is population-based and was randomly recruited, and represents the largest number of subjects in the current literature comparing CET and evaluating biometric determinants of CET profiles according to different refractive error groups. The most important limitation of this study was that the distribution of refractive error groups was not homogeneous. Since our study included population-based randomized participants, large differences between the sample numbers across different refractive error groups could not be avoided. Nonetheless, the proportional distribution of refractive errors found in our sample is representative of the overall population studied because the subjects were randomly selected. Likewise, a similar hyperopia prevalence was found among university students in Israel and Iran, reflecting the possible prevalence of hyperopia within the Middle East region [34, 35]. Although the number of subjects in the low myopia group was high, the moderate and high myopia groups were evaluated together, due to the low number of patients in both groups. Another limitation of the study was that dry eye evaluation was not performed in subjects, and the possible effect of tear film on CET was ignored. Although SD-OCT used in our study has been shown to provide good CET mapping repeatability and reproducibility in normal eyes and eyes with corneal disease in all map regions, the axial resolution of 5 μm may create a disadvantage compared to other OCT devices [36, 37].
Conclusions
In conclusion, the findings of this study showed an increasing corneal epithelial thinning from hyperopia to high myopia. Regardless of the refractive group, the thinnest quadrant of the corneal epithelium was the 5–6 mm superior quadrant, and the thickest quadrant was the 5–6 mm inferior quadrant. Axial length and CET were positively correlated in the moderate–high myopia group. In comparison, Rm F and CET were significantly positively correlated in the low and moderate–high myopia groups.
References
Hwang ES, Schallhorn JM, Randleman JB. Utility of regional epithelial thickness measurements in corneal evaluations. Surv Ophthalmol. 2020;65(2):187–204.
Simon G, Ren Q, Kervick GN, Parel JM. Optics of the corneal epithelium. Refract Corneal Surg. 1993;9(1):42–50.
Maltsev DS, Kudryashova EV, Kulikov AN, Mareichev AY. Relationship between central epithelial thickness and central corneal thickness in healthy eyes and eyes after laser in situ keratomileusis. Cornea. 2018;37(8):1053–7.
Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254(5035):1178–81.
Kanellopoulos AJ, Asimellis G. In vivo three-dimensional corneal epithelium imaging in normal eyes by anterior-segment optical coherence tomography: a clinical reference study. Cornea. 2013;32(11):1493–8.
Ma XJ, Wang L, Koch DD. Repeatability of corneal epithelial thickness measurements using Fourier-domain optical coherence tomography in normal and post-LASIK eyes. Cornea. 2013;32(12):1544–8.
Salomao MQ, Hofling-Lima AL, Lopes BT, et al. Role of the corneal epithelium measurements in keratorefractive surgery. Curr Opin Ophthalmol. 2017;28(4):326–36.
Matalia H, Swarup R. Imaging modalities in keratoconus. Indian J Ophthalmol. 2013;61(8):394–400.
Reinstein DZ, Archer TJ, Dickeson ZI, Gobbe M. Transepithelial phototherapeutic keratectomy protocol for treating irregular astigmatism based on population epithelial thickness measurements by artemis very high-frequency digital ultrasound. J Refract Surg. 2014;30(6):380–7.
Reinstein DZ, Archer TJ, Gobbe M, Silverman RH, Coleman DJ. Epithelial thickness in the normal cornea: three-dimensional display with Artemis very high-frequency digital ultrasound. J Refract Surg. 2008;24(6):571–81.
Reinstein DZ, Srivannaboon S, Gobbe M, et al. Epithelial thickness profile changes induced by myopic LASIK as measured by Artemis very high-frequency digital ultrasound. J Refract Surg. 2009;25(5):444–50.
Salah-Mabed I, Saad A, Gatinel D. Topography of the corneal epithelium and Bowman layer in low to moderately myopic eyes. J Cataract Refract Surg. 2016;42(8):1190–7.
Arba Mosquera S, Awwad ST. Theoretical analyses of the refractive implications of transepithelial PRK ablations. Br J Ophthalmol. 2013;97(7):905–11.
Khamar P, Rao K, Wadia K, et al. Advanced epithelial mapping for refractive surgery. Indian J Ophthalmol. 2020;68(12):2819–30.
Reinstein DZ, Archer T. Combined Artemis very high-frequency digital ultrasound-assisted transepithelial phototherapeutic keratectomy and wavefront-guided treatment following multiple corneal refractive procedures. J Cataract Refract Surg. 2006;32(11):1870–6.
Wu Y, Wang Y. Detailed distribution of corneal epithelial thickness and correlated characteristics measured with SD-OCT in myopic eyes. J Ophthalmol. 2017;2017:1018321.
Wang X, Dong J, Wu Q. Corneal thickness, epithelial thickness and axial length differences in normal and high myopia. BMC Ophthalmol. 2015;15:49.
Kim BJ, Ryu IH, Lee JH, Kim SW. Correlation of sex and myopia with corneal epithelial and stromal thicknesses. Cornea. 2016;35(8):1078–83.
Kim WK, Ryu IH, Yoo J, Kim SW. Effect of gender, age, and ocular and growth-related factors on corneal epithelial and stromal thickness in children. J Clin Med. 2020;9(12):3849.
Ozalp O, Atalay E, Yildirim N. Prevalence and risk factors for keratoconus in a university-based population in Turkey. J Cataract Refract Surg. 2021;47(12):1524–9.
Mas Tur V, MacGregor C, Jayaswal R, O’Brart D, Maycock N. A review of keratoconus: diagnosis, pathophysiology, and genetics. Surv Ophthalmol. 2017;62(6):770–83.
Liu G, Rong H, Zhang P, et al. The effect of axial length elongation on corneal biomechanical property. Front Bioeng Biotechnol. 2021;9:777239.
Rocha KM, Perez-Straziota CE, Stulting RD, Randleman JB. SD-OCT analysis of regional epithelial thickness profiles in keratoconus, postoperative corneal ectasia, and normal eyes. J Refract Surg. 2013;29(3):173–9.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B (Methodol). 1995;57(1):289–300.
Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Stat. 2001;2:1165–88.
Ma Y, He X, Zhu X, Lu L, Zhu J, Zou H. Corneal epithelium thickness profile in 614 normal Chinese children aged 7–15 years old. Sci Rep. 2016;6:23482.
Gowrisankaran S, Sheedy JE, Hayes JR. Eyelid squint response to asthenopia-inducing conditions. Optom Vis Sci. 2007;84(7):611–9.
Kim BJ, Ryu IH, Kim SW. Age-related differences in corneal epithelial thickness measurements with anterior segment optical coherence tomography. Jpn J Ophthalmol. 2016;60(5):357–64.
Samy MM, Shaaban YM, Badran TAF. Age- and sex-related differences in corneal epithelial thickness measured with spectral domain anterior segment optical coherence tomography among Egyptians. Medicine (Baltimore). 2017;96(42):e8314.
Hashmani N, Hashmani S, Saad CM. Wide corneal epithelial mapping using an optical coherence tomography. Invest Ophthalmol Vis Sci. 2018;59(3):1652–8.
Du C, Wang J, Cui L, Shen M, Yuan Y. Vertical and horizontal corneal epithelial thickness profiles determined by ultrahigh resolution optical coherence tomography. Cornea. 2012;31(9):1036–43.
Cui X, Hong J, Wang F, et al. Assessment of corneal epithelial thickness in dry eye patients. Optom Vis Sci. 2014;91(12):1446–54.
Guglielmetti S, Kirton A, Reinstein DZ, Carp GI, Archer TJ. Repair of irregularly irregular astigmatism by transepithelial phototherapeutic keratectomy. J Refract Surg. 2017;33(10):714–9.
Hashemi H, Pakzad R, Ali B, et al. Prevalence of refractive errors in iranian university students in Kazerun. J Curr Ophthalmol. 2020;32(1):75–81.
Shneor E, Doron R, Ostrin LA, Gordon-Shaag A. The prevalence of refractive errors in college students in Israel. [published online ahead of print, 2021 Dec 27]. J Optom. 2021;S1888–4296(21)00052–2..
Sella R, Zangwill LM, Weinreb RN, Afshari NA. Repeatability and reproducibility of corneal epithelial thickness mapping with spectral-domain optical coherence tomography in normal and diseased cornea eyes. Am J Ophthalmol. 2019;197:88–97.
Ge L, Yuan Y, Shen M, Tao A, Wang J, Lu F. The role of axial resolution of optical coherence tomography on the measurement of corneal and epithelial thicknesses. Invest Ophthalmol Vis Sci. 2013;54(1):746–55.
Acknowledgements
We thank the participants of the study.
Funding
This study was supported by the Scientific Research Projects Fund of Eskişehir Osmangazi University by the Project number 2019–2492.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Onur Özalp and Eray Atalay. The first draft of the manuscript was written by Onur Özalp and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Onur Özalp and Eray Atalay declare that they have no conflict of interest. Onur Özalp was affiliated with Eskişehir Osmangazi University Hospital at the time of the study but his current affiliation is Devrek State Hospital, Zonguldak.
Compliance with ethics guidelines
All procedures performed were in accordance with the ethical standards of the Ethics Committee of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Prior Presentation
The material (in whole or part) is not under consideration by another journal, is not in press in any other format, and has not been previously published.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ozalp, O., Atalay, E. Biometric Determinants of Epithelial Thickness Profile Across a Wide Range of Refractive Errors. Ophthalmol Ther 11, 1089–1100 (2022). https://doi.org/10.1007/s40123-022-00489-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00489-9