Abstract
Introduction
Dorsal root ganglion pulsed radiofrequency (DRG-PRF) is frequently used for the treatment of chronic lumbar radicular pain with good outcomes in terms of pain management. Transforaminal epidural steroid injection (TFESI) is often administered immediately after DRG-PRF to increase the anti-inflammatory effects, but support for the synergic mechanism is lacking in the literature. The aim of this study was to investigate the potential role of TFESI immediately after DRG-PRF and its possible role on pain intensity and patient disability.
Methods
A database of patients who underwent DRG-PRF with or without TFESI immediately after DRG-PRF was retrospectively analysed; propensity score matching was applied to the analysis to reduce possible bias. Pain intensity (numerical rating scale [NRS]) and Oswestry disability index (ODI) were recorded pre-operatively and at the 1- and 3-month follow-up in the two groups of patients.
Results
A total of 252 patients were included in this retrospective analysis, 126 patients in the DRG-PRF + TFESI group and 126 patients in the DRG-PRF group after propensity score matching. Both groups displayed a significant reduction in pain intensity (NRS score reduction; p < 0.0001) and improvement in the ODI (p < 0.0001) from baseline at the 3-month follow-up. Interestingly, the use of TFESI after DRG-PRF was not associated with any clinical benefit as no difference in NRS and ODI was found between the two groups at the 1- and 3-month follow-ups.
Conclusions
Our study revealed a significant pain reduction and disability improvement after DRG-PRF in patients with lumbar radicular pain. Interestingly, no positive role of TFESI immediately after DRG-PRF was observed. These findings suggest that DRG-PRF provides substantial pain relief, and no added benefit is obtained with subsequent steroid injection. Future prospective studies with expanded follow-up periods are needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Transforaminal epidural steroid injection (TFESI) is frequently administered immediately after dorsal root ganglion pulsed radiofrequency (DRG-PRF) to increase the anti-inflammatory effects of PRF |
However, this supposed synergic mechanism has not been confirmed and no definitive results have supported this strategy |
The aim of this study was to investigate the potential role of TFESI immediately after DRG-PRF and its possible effects on pain intensity and patient disability |
What was learned from the study? |
DRG-PRF effectively reduces pain and improves disability in patients with chronic lumbar radicular pain |
TFESI administered immediately after DRG-PRF does not demonstrate additional clinical benefits in terms of pain intensity or patient disability |
Propensity score matching ensures reduced bias in comparing the outcomes of DRG-PRF alone versus DRG-PRF with TFESI, enhancing the reliability of the study findings |
Prospective studies with longer follow-up periods are warranted to validate these findings and further explore the efficacy of DRG-PRF and TFESI in managing lumbar radicular pain |
Introduction
Chronic spinal pain is a leading cause of disability among adults worldwide with detrimental effects on quality of life and burdensome costs for healthcare systems [1]. Lumbar disc herniations and degenerative spine conditions (stenosis, osteoarthritis, listhesis, scoliosis and vertebral compression fractures) are common conditions involved in low back pain and lumbosacral radicular pain [2]. The main components of the pathophysiology of chronic radicular pain are nerve root compression, inflammation and glial activation [3, 4]. Transforaminal epidural steroid injection (TFESI) is a common interventional option for the treatment of these conditions [5], and although a significant pain reduction has been reported by many published studies with the use of TFESI [6, 7], the efficacy is generally time-dependent and effectiveness in reducing radicular pain is often transient [8, 9].
In the last 25 years, pulsed radiofrequency (PRF) has emerged as a percutaneous, minimally invasive technique that uses an electrical current to achieve medium to long-term pain reduction, especially for neuropathic pain [10]. The procedure was originally described in 1998 for radicular lumbar pain but its application has since been been expanded to include different pain conditions [11].
The dorsal root ganglion (DRG) is a common target of PRF when the aim is to effectively control lumbar radicular pain [12,13,14,15,16,17]. This technique relies on the intermittent administration of high-frequency, short-duration current at a temperature below 42 °C to induce an electrical neuromodulation without structural damage [18]. The PRF current comprises alternatively repeated electromagnetic waves with a frequency of 500 kHz and pulse width of 20 ms with 480 ms resting phase [19].
Recently, different therapeutic mechanisms have been reported to explain PRF-induced pain relief. The C-fiber long-term depression was the first described mechanism of pain signalling inhibition [20]. Many other mechanisms were subsequently reported, including microglia downregulation [21], increased levels of endogenous opioid messenger RNA [22], enhancement of noradrenergic and serotonergic descending pain inhibitory pathways [23] and microscopic damages of membranes, mitochondria, microfilaments and microtubules [24]. Recent studies have highlighted the anti-inflammatory effects of PRF as a result of a reduction of proinflammatory cytokines [25, 26], along with an increase of nestin and matrix metalloproteinase-2 expression at the level of the DRG [27].
TFESI is frequently used immediately after DRG-PRF to increase the anti-inflammatory effects of PRF [28]. However, the supposed synergic mechanism has not been confirmed, and no definitive results have supported this strategy. Notably, steroid injections can cause possible severe adverse effects, such as an increase in blood sugar levels, especially in patients with diabetes [29], epidural lipomatosis, spinal cord infarct, menstrual changes, adrenal suppression, Cushing’s syndrome, osteoporosis and steroid myopathy [30, 31].
The aim of this study was to investigate the potential role of TFESI immediately after DRG-PRF and its possible effects on pain intensity and patient disability.
Methods
Study Population
The data of consecutive patients with low back pain and radicular pain who underwent DRG-PRF at our Interventional and Surgical Pain Centre, Guglielmo da Saliceto Hospital, Piacenza, Italy, from January 2019 to December 2021 was entered into a retrospective database specifically created for this study. This study was approved by the local Ethics Committee (747/2023/DISP/AUSLPC) and performed in accordance with the principles of the Declaration of Helsinki.
The inclusion criteria consisted of patients with chronic low back pain, radicular pain, no response to medical and physical treatments and with transitory response to previous epidural or transforaminal steroid injections. Patients with incomplete clinical data and those who were pregnant were not entered into the database. Patients with localized infection, haemorrhagic diathesis, spinal pathologies (e.g. tumours), vertebral fractures, instability, central canal stenosis, clinical signs of motor palsy, uncontrolled diabetes, heart failure or comorbid psychiatric condition were not included.
Data Collection
Electronic medical records were reviewed to collect demographic and clinical data. Pre- and intra-operative variables such as age, gender, body mass index (BMI), pain duration, level of DRG-PRF, single or dual level (L4L5 + L5S1) DRG-PRF, pain intensity (numerical rating scale [NRS]) and Oswestry disability index (ODI) were collected. The ODI score was calculated from a 10-item questionnaire to assess patients’ pain and its impact on daily life activities. This score ranges from minimal disability (0–20), moderate disability (21–40), severe disability (41–60), crippled (61–80) and bed-bound (81–100).
Due to the limited sample size, patients who underwent lumbar (L) spine DRG-PRF at L1, L2 and L3 were not included in the present study. NRS and ODI were collected at 1 and 3 months after DRG-PRF to evaluate the outcome of the procedure. All of the included patients underwent a previous transforaminal injection with lidocaine 1% to confirm radicular involvement. The last transforaminal injection was performed at least 1 month prior to DRG-PRF.
DRG-PRF Procedure
Patients were placed in the prone position with a pillow under the lower abdomen to reduce the physiological lordosis and to provide an easy approach to the intervertebral foramen. A conscious sedation with midazolam 0.05 mg/kg was induced and a 20G, 10-cm radiofrequency cannula with a 10-mm curved active tip was placed near the DRG under fluoroscopic guidance and strict aseptic conditions. Sedation was administered, if necessary, to certain patients to alleviate discomfort and anxiety associated with the procedure. We opted for a curved-tip needle to enhance needle mobility in cases of foraminal stenosis or bone hypertrophy, as its design allows it to be rotated for easier passage beneath the pedicle. However, these are merely personal impressions, and well-designed studies are necessary to confirm these considerations. The DRG is typically located in the dorsal-cranial quadrant of the intervertebral foramen on lateral fluoroscopic view and in the middle of the pedicle in the anteroposterior view [32]. The position of the cannula was confirmed by contrast injection to exclude a vascular placement and to evaluate the dye distribution along the medial and lateral border of the root and around the thecal sac [33]. The final location of the cannula was checked with sensory and motor stimulations. For the sensory stimulation at 50 Hz, a ≤ 0.4 V threshold was considered and confirmed by paraesthesia onset in the usual distribution of radicular pain. A motor stimulation (2 Hz) threshold greater than 1.5- to twofold the sensory threshold was considered appropriate to ensure the proper position of the cannula away from the ventral root and close to the DRG [34]. An impedance < 400 Ω was also required. The stylet of the cannula was consequently replaced by the radiofrequency probe and a PRF current was applied at 45 V with 20-ms pulse width and 2-Hz pulse rate for a duration of 360 s. The choice of a 360-s duration for PRF was based on prior studies demonstrating efficacy and safety within this timeframe [35,36,37]. Additionally, a recently published in vitro study suggests a potential effect of PRF on sensitized DRG neurons by reducing central sensitization biomarkers, such as phosphorylated extracellular signal-regulated kinase (pERK) and Ca2+ influx when PRF is performed at 2 Hz, 20 ms for 360 s [38]. Increasing the length of the PRF period ensures that each patient receives the precise amount of current necessary to achieve optimal therapeutic effects. However, it is important to note that no definitive protocol exists regarding the optimal PRF settings for clinical effectiveness. The maximum target temperature was 42 °C. However, as previously reported, it is possible for PRF to produce bursts of heat, causing the temperature to briefly exceed this limit around the radiofrequency electrodes by microseconds [39]. This brief increase in temperature is carefully controlled, and during these short periods, the machine will not deliver current to prevent any potential tissue damage while maintaining the therapeutic effects of the treatment.
Immediately after DRG-PRF, 1 ml of 1% lidocaine mixed with 40 mg triamcinolone was injected at the DRG level in the DRG-PRF + TFESI group. The decision to perform a TFESI immediately after DRG-PRF was based only on physicians’ choice and personal experience, and no randomization was done. This important issue was adequately addressed in the statistical analysis to avoid possible bias.
Statistical Analysis
Continuous variables are reported as the median and interquartile range (IQR) while categorical data are reported as the relative number and percentage. A propensity score was calculated using different statistical techniques with the use of frequentist and machine learning approaches. Logistic regression, random forest, generalized boosted model (GBM) and covariate balance propensity score (CBPS) were used to estimate propensity scores and for covariate weighting. The best overlap of the distribution of propensity scores (common support) was obtained with the logistic regression model, which was consequently used for the final analysis. Age, gender, BMI, pain duration, level of DRG-PRF, dual level DRG-PRF, basal NRS and basal ODI were considered as covariates. Different calipers (from 0.05 to 0.50) with 0.10 increase were tested for the matching. The standardized mean difference (SMD) was used as covariate balance measurement before and after propensity score matching. As previously recommended, a 0.10 SMD distance between covariates after the propensity score matching was the cut-off value [40]. The best propensity score matching was obtained with exact matching, caliper = 0.30, 1:1 ratio, with no replacement. Therefore, a database with matched patients was implemented, and the average treatment effect (ATE) related to NRS and ODI at 1 and 3 months after DRG-PRF was estimated with the Holm–Šídák correction for multiple comparisons. Statistical significance was set at a two-tailed p value < 0.05. R software v4.2.2 (R Foundation for Statistical Computing, Vienna, Austria; www.r-project.org) was used for the analyses.
Results
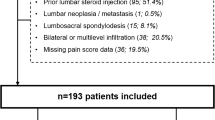
A total of 158 patients in the DRG-PRF + TFESI group and 150 patients in the DRG-PRF group were initially considered for the study; of these 61 patients were excluded due to incomplete or missing data. After the propensity score matching, 126 patients in the DRG-PRF + TFESI group and 126 patients in the DRG-PRF group were matched. Consequently, 32 patients in the DRG-PRF + TFESI group and 24 patients in the DRG-PRF group were discarded due to covariate imbalance. As previously reported, the best overlap between propensity score values (common support) was obtained after logistic regression estimation (Fig. 1).
Best overlap of propensity score values (common support) across the two treatment groups (DRG-PRF and DRG-PRF + TFESI) after propensity score estimation with logistic regression. In addition to overlapping, the propensity score values have a similar balanced distribution. DRG dorsal root ganglion, PRF pulsed radiofrequency, TFESI transforaminal epidural steroid injection
All of the covariates were also adequately balanced after propensity score matching (Fig. 2). Ppatients’ covariates before and after propensity score weighting are summarized in Table 1. The median age of the included patients was 61 (IQR 52–69) years in the DRG-PRF + TFESI group and 62 (IQR 52–69) years in the DRG-PRF group (SMD - 0.0506). The majority of patients in each treatment group were female (59% and 61% in the DRG-PRF + TFESI and DRG-PRF group, respectively). The median BMI was 26.2 (IQR 23–28.4) kg/m2 in the DRG-PRF + TFESI group and 25 (IQR 23–28) kg/m2 in the DRG-PRF group (SMD 0.0147). Pain duration at the time of the intervention was 3.1 (IQR 1.5–4.7) years and 3.4 years (1.8–4.6 IQR) (SMD 0.0887), baseline NRS was 7.9 (IQR 7.6–8.4) and 8 (IQR 7.4–8.4 IQR) (SMD -0.0201) and ODI was 53 (IQR 49–57) and 53 (IQR 49–58) (SMD - 0.0542), in the DRG-PRF + TFESI and DRG-PRF groups, respectively. DRG-PRF was mainly performed at the L4-L5 level (57.3% of patients in the DRG-PRF + TFESI group, 58.2% in DRG-PRF group).
No difference was found between baseline NRS (p = 0.87) and ODI values (p = 0.95) in the DRG-PRF and DRG-PRF + TFESI groups (p = 0.87). The ATE of the TFESI in the matched dataset revealed no difference between the DRG-PRF + TFESI and DRG-PRF groups in terms of NRS (NRS DRG-PRF + TFESI group: 4.3 ± 2.3; NRS DRG-PRF group: 4.4 ± 2.2; p = 0.88) and ODI (ODI DRG-PRF + TFESI group: 20 ± 7.9; ODI DRG-PRF group: 22 ± 7.8; p = 0.95) at the 1-month follow-up after DRG-PRF. The same results were obtained at the 3-month follow-up for NRS (NRS DRG-PRF + TFESI groups 4.8 ± 2.6; NRS DRG-PRF group: 4.2 ± 1.6; p = 0.80) and ODI improvement (ODI DRG-PRF + TFESI group: 27 ± 11; ODI DRG-PRF group: 27.6 ± 10; p = 0.96). Compared to baseline, the NRS was significantly reduced in both groups at the 1-month (p < 0.0001) and 3-month follow-ups (p < 0.0001), while the ODI score was similarly improved at the 1-month (p < 0.0001) and 3-month follow-ups (p < 0.0001) (Fig. 3).
Changes in pain scores (NRS) and disability index (ODI) during the follow-up, after DRG-PRF in the two groups (DRG-PRF and DRG-PRF + TFESI). DRG Dorsal root ganglion, NRS numerical rating scale, PRF pulsed radiofrequency, ODI Oswestry disability index, TFESI transforaminal epidural steroid injection
Discussion
In this study the use of TFESI (DRG-PRF + TFESI group) immediately after DRG-PRF was not associated with any clinically significant benefit. In fact, no difference in pain intensity (NRS scale) and disability index (ODI scale) was found at the 1- and 3-month follow-ups after DRG-PRF regardless of whether TFESI was administered or not. Significant pain relief and ODI improvement were maintained for up to 3 months in both groups.
DRG-PRF is frequently used with good results for the treatment of refractory radicular pain in patients with disc herniations, lumbar stenosis or persistent spinal pain syndrome (PSPS) [41]. The neuromodulatory and anti-inflammatory effects are the key elements of DRG-PRF but, as previously cited, other therapeutic mechanisms have been reported. Unfortunately, a complete description and a full understanding of all these complex mechanisms are still unavailable [42]. Various DRG-PRF protocols have been published, and analytical problems arise when attempting to compare different studies in a meta-analysis [43, 44]. In addition, DRG-PRF can be applied whether transforaminal or epidural, and the selection of the appropriate technique has not been adequately addressed. The same problems can be found in preclinical animal studies where the ideal voltage, number of cycles, pulse duration and optimal electrode distance are still far from being clarified [45]. All of these issues should be addressed in future studies for a better indication of the application of PRF for pain management. Indeed, the authors of a previously published review concluded that while there may be a convincing role of DRG-PRF for the treatment of cervical radicular pain, the evidence for PRF efficacy in treating lumbar radicular pain has yet to be confirmed by further studies, largely due to the absence of standardization of PRF parameters and enrolment criteria [46]. Moreover, as reported by Van Zundert et al., in the setting of a randomized controlled trial PRF treatment of the cervical DRG showed promising pain relief outcomes, indicating potential efficacy in patients with chronic cervical radicular pain [47].
In the present study, DRG-PRF was performed at 45 V with 20-ms pulse width and 2-Hz pulse rate, for a duration of 360 s, as previously suggested by many authors for the treatment of lumbar radicular pain [48,49,50]. High-voltage PRF has recently been proposed as a new method to increase the efficacy of the procedure and has been extensively studied for the treatment of herpes zoster-related pain [51,52,53]. However, the first encouraging results of high-voltage PRF [54, 55] were not confirmed in a recently published double-blind randomized control trial [56]. Taking all of these elements into account, high-voltage PRF cannot currently replace PRF performed at 45 V, and new evidence is needed to support the use of high-voltage PRF. Hopefully, the results of this ongoing trial will provide more information on this topic [57]. We believe that unresolved questions about the optimal “PRF dose”, including the voltage and duration of energy delivery, may significantly contribute to conflicting results in some studies and should be thoroughly addressed in future research. Finally, it is important to note that our results should be interpreted as strictly linked to the DRG-PRF protocol used and cannot be generalized.
TFESIs are frequently used with good short-term results for the management of radicular pain [58]. Steroids can reduce the inflammatory cascade by inhibiting the synthesis and the release of pro-inflammatory cytokines [59, 60]. When injected trasforaminally, they can potentially act at the anterior epidural space, where higher concentrations of substance P and glutamate are present [61, 62]. Adding steroids to PRF treatment has the potential to enhance the efficacy of this treatment by reducing inflammation. Steroids are known for their anti-inflammatory properties, which may complement PRF’s mechanism of action. However, as we previously noted, there are potential local (epidural lipomatosis and spinal cord infarct) and systemic (increase in blood sugar levels, menstrual changes, adrenal suppression, Cushing’s syndrome, osteoporosis and steroid myopathy) negative effects to consider. Moreover, steroids could attenuate some of the intended effects of PRF by altering the physiological response at the DRG level or potentially affecting the healing process.
A direct correlation with clinical improvement was found when an anterior epidural spread of the medication was obtained [63]. Although PRF was superior to TFESI and associated with positive results in previous studies for the treatment of radicular pain [64, 65], some authors have reported no difference in patients who received PRF or sham treatment [14, 66]. A recent retrospective study by Yang et al. [67] showed a 60% median pain reduction at the 1-month follow-up in patients with disk herniation, spinal stenosis or PSPS after DRG-PRF combined with TFESI, while no control group without steroids was considered. Our findings are in line with this publication. Indeed, our DRG-PRF + TFESI group showed a 46% NRS reduction at the 1-month follow-up. Unfortunately, it is not possible to fully compare the two studies since Yang et al. analysed only pain intensity and no ODI data were reported. Moreover, it is possible to argue that some patients in the Yang et al. study [67] underwent more than one DRG-PRF before the 1-month follow-up, since the number of DRG-PRF procedures performed is higher than the number of enrolled patients and DRG-PRF application at multiple spinal levels was not allowed by the protocol.
The same findings were reported in a subsequent study on the use of DRG-PRF with TFESI in 42 patients with different spine-related, pain-associated diagnoses [28]. If we consider only the lumbar spine group, DRG-PRF was able to reduce the NRS by 53% and 52% at the 1- and 3-month follow-ups, respectively. Notably, the authors were also able to show a 64% reduction in the NRS at 1 week after DRG-PRF, and a general decrease in the use of analgesics at 3 months after the procedure. Although this study highlights a number of important elements, such as the earlier follow-up and the decrease in analgesic use after DRG-PRF, the limited sample size and a possible covariate imbalance among the included patients prevents a possible comparison with our data and data from other studies.
To the contrary, in another published study PRF was considered to be an adjuvant treatment in conjunction with TFESI to increase the efficacy and the response rate of the injected steroid [14]. In this randomized controlled study, the authors reported a better pain relief at 2 and 3 months after DRG-PRF + TFESI when compared to TFESI alone while no difference was found at the 1-month follow-up, thus demonstrating a possible short-term role of TFESI. However, it is important to note that the results of this study should be interpreted cautiously since the primary outcome (pain reduction) was underpowered due to loss to follow-up and possible change of concomitant analgesic medication use, as allowed by the protocol. Consequently, is not possible to rule out that TFESI, PRF and analgesic medications can interact over the observed outcome.
In a retrospective study, 135 patients with lumbar radicular pain were treated with TFESI alone, DRG-PRF alone or TFESI combined with DRG-PRF [68]. All of the patients experienced an early analgesic effect, but only the second and third group obtained a more prolonged period of pain relief up to 3 months, as compared to patients treated with TFESI alone. Interestingly, at the 1-month follow-up, the lowest pain intensity and ODI improvements were obtained by patients in the TFESI + DRG-PRF group. In contrast, our data did not show any difference at the 1-month follow-up between the DRG-PRF + TFESI and DRG-PRF groups. This apparent difference could be related to the enrolled patients: in their retrospective study Ding et al. [68] enrolled a more heterogeneous group of patients with axial (non-radicular) or radicular chronic low back pain without a subgroup analysis, while we considered only selected patients with only radicular pain. Moreover, Ding et al. [68] also used 1 mg of vitamin B12 as an adjuvant in TFESI. Another study compared the use of TFESI in combination with DRG-PRF to TFESI alone in patients with lumbar or cervical radicular pain due to disc herniation [69]. Although pain intensity was significantly reduced in both groups after the treatment and the NRS score was lower in the DRG-PRF group, no statistically significant difference was found during the 12-week follow-up period.
To the best of our knowledge, no previously published studies comparing DRG-PRF + TFESI and DRG-PRF exist. The results of our study confirm that DRG-PRF does not require the injection of steroids to increase its efficacy for the treatment of radicular pain. DRG represents a key aspect due to its unique neuroanatomical structure and function on pain transmission [70, 71], along with a possible role as rescue therapy in patients with spinal cord stimulation failure [72]. All of these elements underline the crucial importance of DRG in radicular pain. This is the first study that directly compares pain reduction and ODI improvements in patients with radicular pain treated with DRG-PRF with and without TFESI immediately after PRF.
Although our study showed no clear advantages for the use of steroids after DRG-PRF in patients with radicular pain, additional prospective studies are needed to confirm these results and to expand on the clinical role of DRG-PRF in radicular pain. Moreover, it is important to consider our results as being strictly linked to the DRG-PRF protocol that was used. Another future area of research includes the development of well-constructed DRG-PRF outcome prediction models with a validation process. Indeed, as was recently outlined, different results can be obtained when a validation analysis is carried out to evaluate the strengths and weaknesses of the models [73, 74].
This study has several limitations. First, it is a single-centre, retrospective study. However, this potential weakness is counterbalanced by a significant sample size and the use of a propensity score-based analysis. In retrospective studies a wide distribution of observed covariates can be observed, and this can lead to biased estimates of the treatment’s effect. The propensity score has been used to reduce this bias. Indeed, as previously suggested, it could be considered comparable to a randomized trial [75, 76]. No data were collected regarding previous spine surgery; recently published data suggest that PRF is more effective in patients with disc herniation and spinal stenosis compared to patients with PSPS [12, 77]. However, these findings were not confirmed by Yang et al. [67]. We are not able to confirm these findings since data on the occurrence of previous lumbar surgery were collected in only a small number of patients and the required minimum sample size to be analysed and matched was not reached. Moreover, it was not possible to systematically collect the concomitant analgesic medications used by our enrolled patients. This is related to inaccuracies and failures in reporting these data during follow-up visits.
Other possible covariates, such as lifestyle habits (e.g. smoking, physical activity) or psychological factors (depression, anxiety and pain catastrophizing), were not studied, although all of these elements can certainly affect the observed results. Even if radicular pain was the leading symptom in these patients, it was not possible to rule out the presence of other minor contributing factors (e.g. facet or sacroiliac joints pain, muscular pain, postural imbalance) that could have influenced the DRG-PRF outcome.
In our study, only 1- and 3-month follow-up data were collected, and no data on early follow-up (e.g. 1 and 2 weeks) were available. This is related to our internal organization since patients are normally reassessed 1 month after an interventional procedure. Due to the retrospective nature of this study, these data cannot be documented. Consequently, a possible short-term benefit after steroid injection cannot be ruled out. Future studies with early follow-up, ranging from a few days post DRG-PRF to the first 2 weeks after treatment, are needed to clarify the potential role of steroid injection during the early period following DRG-PRF.
Conclusions
Our propensity scores matching analysis revealed a significant pain reduction and disability improvement after DRG-PRF in patients with lumbar radicular pain. Interestingly, no positive role of steroid injection immediately after DRG-PRF was observed. These findings would suggest that DRG-PRF does not require the injection of steroids to increase its efficacy. Future prospective studies with earlier and longer follow-up are needed to confirm our findings.
Data Availability
The dataset used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Breivik H, Eisenberg E, O’Brien T, OPENMinds. The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013;13:1229. https://doi.org/10.1186/1471-2458-13-1229.
Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, Cohen SP. Low back pain. Lancet. 2021;398(10294):78–92. https://doi.org/10.1016/S0140-6736(21)00733-9.
Wuertz K, Haglund L. Inflammatory mediators in intervertebral disk degeneration and discogenic pain. Glob Spine J. 2013;3(3):175–84. https://doi.org/10.1055/s-0033-1347299.
Albrecht DS, Ahmed SU, Kettner NW, et al. Neuroinflammation of the spinal cord and nerve roots in chronic radicular pain patients. Pain. 2018;159(5):968–77. https://doi.org/10.1097/j.pain.0000000000001171.
Manchikanti L, Knezevic NN, Boswell MV, Kaye AD, Hirsch JA. Epidural injections for lumbar radiculopathy and spinal stenosis: a comparative systematic review and meta-analysis. Pain Physician. 2016;19(3):E365-410.
Manchikanti L, Benyamin RM, Falco FJE, Kaye AD, Hirsch JA. Do epidural injections provide short- and long-term relief for lumbar disc herniation? A systematic review. Clin Orthop. 2015;473(6):1940–56. https://doi.org/10.1007/s11999-014-3490-4.
Helm Ii S, Harmon PC, Noe C, et al. Transforaminal epidural steroid injections: a systematic review and meta-analysis of efficacy and safety. Pain Physician. 2021;24(S1):S209–32.
Olguner SK, Celiktas M, Oktay K, et al. Comparison of 1-year results of single transforaminal epidural steroid injection among patients with different spinal pathologies-related radicular pain. Niger J Clin Pract. 2020;23(6):835–41. https://doi.org/10.4103/njcp.njcp_24_19.
Oliveira CB, Maher CG, Ferreira ML, et al. Epidural corticosteroid injections for lumbosacral radicular pain. Cochrane Database Syst Rev. 2020;4(4):CD013577. https://doi.org/10.1002/14651858.CD013577.
Napoli A, Alfieri G, Scipione R, Andrani F, Leonardi A, Catalano C. Pulsed radiofrequency for low-back pain and sciatica. Expert Rev Med Devices. 2020;17(2):83–6. https://doi.org/10.1080/17434440.2020.1719828.
Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008;12(1):37–41. https://doi.org/10.1007/s11916-008-0008-3.
Abejón D, Garcia-del-Valle S, Fuentes ML, Gómez-Arnau JI, Reig E, van Zundert J. Pulsed radiofrequency in lumbar radicular pain: clinical effects in various etiological groups. Pain Pract. 2007;7(1):21–6. https://doi.org/10.1111/j.1533-2500.2007.00105.x.
Chao SC, Lee HT, Kao TH, et al. Percutaneous pulsed radiofrequency in the treatment of cervical and lumbar radicular pain. Surg Neurol. 2008;70(1):59–65. https://doi.org/10.1016/j.surneu.2007.05.046. (Discussion: 65).
Koh W, Choi SS, Karm MH, et al. Treatment of chronic lumbosacral radicular pain using adjuvant pulsed radiofrequency: a randomized controlled study. Pain Med. 2015;16(3):432–41. https://doi.org/10.1111/pme.12624.
Nagda JV, Davis CW, Bajwa ZH, Simopoulos TT. Retrospective review of the efficacy and safety of repeated pulsed and continuous radiofrequency lesioning of the dorsal root ganglion/segmental nerve for lumbar radicular pain. Pain Physician. 2011;14(4):371–6.
Shanthanna H, Chan P, McChesney J, Paul J, Thabane L. Pulsed radiofrequency treatment of the lumbar dorsal root ganglion in patients with chronic lumbar radicular pain: a randomized, placebo-controlled pilot study. J Pain Res. 2014. https://doi.org/10.2147/JPR.S55749.
Van Boxem K, de Meij N, Kessels A, Van Kleef M, Van Zundert J. Pulsed radiofrequency for chronic intractable lumbosacral radicular pain: a six-month cohort study. Pain Med. 2015;16(6):1155–62. https://doi.org/10.1111/pme.12670.
Chua NHL, Vissers KC, Sluijter ME. Pulsed radiofrequency treatment in interventional pain management: mechanisms and potential indications—a review. Acta Neurochir (Wien). 2011;153(4):763–71. https://doi.org/10.1007/s00701-010-0881-5.
Podhajsky RJ, Sekiguchi Y, Kikuchi S, Myers RR. The histologic effects of pulsed and continuous radiofrequency lesions at 42 °C to rat dorsal root ganglion and sciatic nerve. Spine. 2005;30(9):1008–13. https://doi.org/10.1097/01.brs.0000161005.31398.58.
Park D, Chang MC. The mechanism of action of pulsed radiofrequency in reducing pain: a narrative review. J Yeungnam Med Sci. 2022;39(3):200–5. https://doi.org/10.12701/jyms.2022.00101.
Cho HK, Kang JH, Kim SY, et al. Changes in neuroglial activity in multiple spinal segments after caudal epidural pulsed radiofrequency in a rat model of lumbar disc herniation. Pain Physician. 2016;19(8):E1197–209.
Moffett J, Fray LM, Kubat NJ. Activation of endogenous opioid gene expression in human keratinocytes and fibroblasts by pulsed radiofrequency energy fields. J Pain Res. 2012;5:347–57. https://doi.org/10.2147/JPR.S35076.
Hagiwara S, Iwasaka H, Takeshima N, Noguchi T. Mechanisms of analgesic action of pulsed radiofrequency on adjuvant-induced pain in the rat: roles of descending adrenergic and serotonergic systems. Eur J Pain. 2009;13(3):249–52. https://doi.org/10.1016/j.ejpain.2008.04.013.
Erdine S, Bilir A, Cosman ER, Cosman ER. Ultrastructural changes in axons following exposure to pulsed radiofrequency fields. Pain Pract. 2009;9(6):407–17. https://doi.org/10.1111/j.1533-2500.2009.00317.x.
Vallejo R, Tilley DM, Williams J, Labak S, Aliaga L, Benyamin RM. Pulsed radiofrequency modulates pain regulatory gene expression along the nociceptive pathway. Pain Physician. 2013;16(5):E601-613.
Jiang R, Li P, Yao YX, et al. Pulsed radiofrequency to the dorsal root ganglion or the sciatic nerve reduces neuropathic pain behavior, decreases peripheral pro-inflammatory cytokines and spinal β-catenin in chronic constriction injury rats. Reg Anesth Pain Med. 2019. https://doi.org/10.1136/rapm-2018-100032.
Arons M, Pilmane M, Bhaskar A, Kopsky DJ, Romanenko V, Rohof O. Pulsed radiofrequency increases nestin and matrix metalloproteinase-2 expression in porcine lumbar dorsal root ganglion. Anesthesiol Pain Med. 2022;12(1): e110531. https://doi.org/10.5812/aapm.110531.
Hong LW, Chen KT. A real-world evidence of a consecutive treatment of 42 spine-related pain using dorsal root ganglion-pulsed radiofrequency (DRG-PRF). Clin Neurol Neurosurg. 2020;197:106186. https://doi.org/10.1016/j.clineuro.2020.106186.
Kim WH, Sim WS, Shin BS, et al. Effects of two different doses of epidural steroid on blood glucose levels and pain control in patients with diabetes mellitus. Pain Physician. 2013;16(6):557–68.
Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000;81(8):1045–50. https://doi.org/10.1053/apmr.2000.7166.
Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003;103(1–2):211–5. https://doi.org/10.1016/s0304-3959(02)00343-3.
Moon HS, Kim YD, Song BH, Cha YD, Song JH, Lee MH. Position of dorsal root ganglia in the lumbosacral region in patients with radiculopathy. Korean J Anesthesiol. 2010;59(6):398–402. https://doi.org/10.4097/kjae.2010.59.6.398.
Viswanathan VK, Kanna RM, Farhadi HF. Role of transforaminal epidural injections or selective nerve root blocks in the management of lumbar radicular syndrome—a narrative, evidence-based review. J Clin Orthop Trauma. 2020;11(5):802–9. https://doi.org/10.1016/j.jcot.2020.06.004.
Malik K, Benzon HT. Radiofrequency applications to dorsal root ganglia: a literature review. Anesthesiology. 2008;109(3):527–42. https://doi.org/10.1097/ALN.0b013e318182c86e.
Cahana A, Van Zundert J, Macrea L, van Kleef M, Sluijter M. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006;7(5):411–23. https://doi.org/10.1111/j.1526-4637.2006.00148.x.
Vuka I, Došenović S, Marciuš T, et al. Efficacy and safety of pulsed radiofrequency as a method of dorsal root ganglia stimulation for treatment of non-neuropathic pain: a systematic review. BMC Anesthesiol. 2020;20(1):105. https://doi.org/10.1186/s12871-020-01023-9.
Fei Y, Deng J, Lv H, Yao M, Wang T, Huang B. Pulsed radiofrequency of dorsal root ganglion of upper thoracic segment for herpes zoster neuralgia: case report. Medicine (Baltimore). 2020;99(25):e20807. https://doi.org/10.1097/MD.0000000000020807.
Laksono RM, Kalim H, Rohman MS, Widodo N, Ahmad MR, Halim W. Pulsed radiofrequency decreases pERK and affects intracellular Ca2+ influx, cytosolic ATP level, and mitochondrial membrane potential in the sensitized dorsal root ganglion neuron induced by N-methyl D-aspartate. J Pain Res. 2023;16:1697–711. https://doi.org/10.2147/JPR.S409658.
Cosman ER, Cosman ER. Electric and thermal field effects in tissue around radiofrequency electrodes. Pain Med. 2005;6(6):405–24. https://doi.org/10.1111/j.1526-4637.2005.00076.x.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107. https://doi.org/10.1002/sim.3697.
Kim SJ, Park SJ, Yoon DM, Yoon KB, Kim SH. Predictors of the analgesic efficacy of pulsed radiofrequency treatment in patients with chronic lumbosacral radicular pain: a retrospective observational study. J Pain Res. 2018;11:1223–30. https://doi.org/10.2147/JPR.S164414.
De la Cruz J, Benzecry Almeida D, Silva Marques M, Ramina R, Fortes Kubiak RJ. Elucidating the mechanisms of pulsed radiofrequency for pain treatment. Cureus. 2023;15(9):e44922. https://doi.org/10.7759/cureus.44922.
Marliana A, Setyopranoto I, Setyaningsih I, Rhatomy S. The effect of pulsed radiofrequency on radicular pain in lumbal herniated nucleus pulposus: a systematic review and meta-analysis. Anesthesiol Pain Med. 2021;11(2): e111420. https://doi.org/10.5812/aapm.111420.
Park S, Park JH, Jang JN, et al. Pulsed radiofrequency of lumbar dorsal root ganglion for lumbar radicular pain: a systematic review and meta-analysis. Pain Pract. 2024;24(5):772–85. https://doi.org/10.1111/papr.13351.
Vuka I, Vučić K, Repić T, Ferhatović Hamzić L, Sapunar D, Puljak L. Electrical stimulation of dorsal root ganglion in the context of pain: a systematic review of in vitro and in vivo animal model studies. Neuromodulation. 2018;21(3):213–24. https://doi.org/10.1111/ner.12722.
Facchini G, Spinnato P, Guglielmi G, Albisinni U, Bazzocchi A. A comprehensive review of pulsed radiofrequency in the treatment of pain associated with different spinal conditions. Br J Radiol. 2017;90(1073):20150406. https://doi.org/10.1259/bjr.20150406.
Van Zundert J, Patijn J, Kessels A, Lamé I, van Suijlekom H, van Kleef M. Pulsed radiofrequency adjacent to the cervical dorsal root ganglion in chronic cervical radicular pain: a double blind sham controlled randomized clinical trial. Pain. 2007;127(1–2):173–82. https://doi.org/10.1016/j.pain.2006.09.002.
Chang MC, Cho YW, Ahn SH. Comparison between bipolar pulsed radiofrequency and monopolar pulsed radiofrequency in chronic lumbosacral radicular pain: a randomized controlled trial. Medicine (Baltimore). 2017;96(9): e6236. https://doi.org/10.1097/MD.0000000000006236.
Lee DG, Cho YW, Ahn SH, Chang MC. The effect of bipolar pulsed radiofrequency treatment on chronic lumbosacral radicular pain refractory to monopolar pulsed radiofrequency treatment. Pain Physician. 2018;21(2):E97–103.
Kim K, Jo D, Kim E. Pulsed Radiofrequency to the dorsal root ganglion in acute herpes zoster and postherpetic neuralgia. Pain Physician. 2017;20(3):E411–8.
Song Y, Yu Z, Guan J, et al. Efficacy of high-voltage pulsed radiofrequency in zoster-associated pain: a meta-analysis and systematic review. Anesthesiol Res Pract. 2023;2023:8479293. https://doi.org/10.1155/2023/8479293.
Sun CL, Li XL, Li CW, He N, Zhang J, Xue FS. High-voltage, long-duration pulsed radiofrequency to the dorsal root ganglion provides improved pain relief for herpes zoster neuralgia in the subacute stage. Pain Physician. 2023;26(3):E155–62.
Wang B, Du Z, Xia J, Zhang H. Efficacy of high-voltage pulsed radiofrequency for the treatment of elderly patients with acute herpes zoster neuralgia. Rev Assoc Med Bras (1992). 2021;67(4):585–9. https://doi.org/10.1590/1806-9282.20201124.
Erken B, Edipoglu IS. Efficacy of high-voltage pulsed radiofrequency of the dorsal root ganglion for treatment of chronic lumbosacral radicular pain: a randomized clinical trial. Neuromodulation. 2024;27(1):135–40. https://doi.org/10.1016/j.neurom.2022.10.056.
Vigneri S, Sindaco G, La Grua M, et al. Electrocatheter-mediated high-voltage pulsed radiofrequency of the dorsal root ganglion in the treatment of chronic lumbosacral neuropathic pain: a randomized controlled study. Clin J Pain. 2020;36(1):25–33. https://doi.org/10.1097/AJP.0000000000000766.
Jang JN, Park S, Park JH, et al. Output current and efficacy of pulsed radiofrequency of the lumbar dorsal root ganglion in patients with lumbar radiculopathy: a prospective, double-blind, randomized pilot study. Pain Physician. 2023;26(7):E797–804.
Jang JN, Park S, Park JH, et al. Comparison of efficacy according to voltage of pulsed radiofrequency treatment to lumbar dorsal root ganglion in patient with lumbar radiculopathy: pilot study. Medicine (Baltimore). 2023;102(17): e33617. https://doi.org/10.1097/MD.0000000000033617.
Smith CC, McCormick ZL, Mattie R, MacVicar J, Duszynski B, Stojanovic MP. The effectiveness of lumbar transforaminal injection of steroid for the treatment of radicular pain: a comprehensive review of the published data. Pain Med. 2020;21(3):472–87. https://doi.org/10.1093/pm/pnz160.
Manchikanti L, Singh V, Pampati V, Falco FJ, Hirsch JA. Comparison of the efficacy of caudal, interlaminar, and transforaminal epidural injections in managing lumbar disc herniation: is one method superior to the other? Korean J Pain. 2015;28(1):11–21. https://doi.org/10.3344/kjp.2015.28.1.11.
Manchikanti L, Cash KA, Pampati V, Falco FJE. Transforaminal epidural injections in chronic lumbar disc herniation: a randomized, double-blind, active-control trial. Pain Physician. 2014;17(4):E489-501.
Kraiwattanapong C, Wechmongkolgorn S, Chatriyanuyok B, et al. Outcomes of fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar spondylolisthesis patients. Asian Spine J. 2014;8(2):119–28. https://doi.org/10.4184/asj.2014.8.2.119.
Gharibo CG, Varlotta GP, Rhame EE, Liu ECJ, Bendo JA, Perloff MD. Interlaminar versus transforaminal epidural steroids for the treatment of subacute lumbar radicular pain: a randomized, blinded, prospective outcome study. Pain Physician. 2011;14(6):499–511.
Gupta R, Singh S, Kaur S, Singh K, Aujla K. Correlation between epidurographic contrast flow patterns and clinical effectiveness in chronic lumbar discogenic radicular pain treated with epidural steroid injections via different approaches. Korean J Pain. 2014;27(4):353–9. https://doi.org/10.3344/kjp.2014.27.4.353.
Park Y, Lee WY, Ahn JK, Nam HS, Lee KH. Percutaneous adhesiolysis versus transforaminal epidural steroid injection for the treatment of chronic radicular pain caused by lumbar foraminal spinal stenosis: a retrospective comparative study. Ann Rehabil Med. 2015;39(6):941–9. https://doi.org/10.5535/arm.2015.39.6.941.
Fathy W, Hussein M, Magdy R, et al. Effect of radiofrequency on dorsal root ganglion versus transforaminal steroids injection on tumor necrosis factor-alpha level in lumbar radicular pain. Pain Physician. 2023;26(6):E671–7.
Shanthanna H, Chan P, McChesney J, Thabane L, Paul J. Pulsed radiofrequency treatment of the lumbar dorsal root ganglion in patients with chronic lumbar radicular pain: a randomized, placebo-controlled pilot study. J Pain Res. 2014;7:47–55. https://doi.org/10.2147/JPR.S55749.
Yang L, Huang Y, Ma J, et al. Clinical outcome of pulsed-radiofrequency combined with transforaminal epidural steroid injection for lumbosacral radicular pain caused by distinct etiology. Front Neurosci. 2021;15:683298. https://doi.org/10.3389/fnins.2021.683298.
Ding Y, Li H, Zhu Y, Yao P, Zhao G. Transforaminal epidural steroid injection combined with pulsed radio frequency on spinal nerve root for the treatment of lumbar disc herniation. J Pain Res. 2018;11:1531–9. https://doi.org/10.2147/JPR.S174318.
Lee DG, Ahn SH, Lee J. Comparative effectivenesses of pulsed radiofrequency and transforaminal steroid injection for radicular pain due to disc herniation: a prospective randomized trial. J Korean Med Sci. 2016;31(8):1324–30. https://doi.org/10.3346/jkms.2016.31.8.1324.
Kent AR, Min X, Hogan QH, Kramer JM. Mechanisms of dorsal root ganglion stimulation in pain suppression: a computational modeling analysis. Neuromodulation. 2018;21(3):234–46. https://doi.org/10.1111/ner.12754.
D’Souza RS, Kubrova E, Her YF, et al. Dorsal root ganglion stimulation for lower extremity neuropathic pain syndromes: an evidence-based literature review. Adv Ther. 2022;39(10):4440–73. https://doi.org/10.1007/s12325-022-02244-9.
Chapman KB, Spiegel MA, van Helmond N, et al. Dorsal root ganglion stimulation as a salvage therapy following failed spinal cord stimulation. Neuromodulation. 2022;25(7):1024–32. https://doi.org/10.1016/j.neurom.2022.04.050.
Leoni MLG, Moschini E, Beretta M, Zanello M, Nolli M. The modified NUTRIC score (mNUTRIC) is associated with increased 28-day mortality in critically ill COVID-19 patients: Internal validation of a prediction model. Clin Nutr ESPEN. 2022;48:202–9. https://doi.org/10.1016/j.clnesp.2022.02.014.
Leoni MLG, Lombardelli L, Colombi D, et al. Prediction of 28-day mortality in critically ill patients with COVID-19: Development and internal validation of a clinical prediction model. PLoS ONE. 2021;16(7):e0254550. https://doi.org/10.1371/journal.pone.0254550.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424. https://doi.org/10.1080/00273171.2011.568786.
Leoni MLG, Schatman ME, Demartini L, Lo Bianco G, Terranova G. Genicular nerve pulsed dose radiofrequency (PDRF) compared to intra-articular and genicular nerve PDRF in knee osteoarthritis pain: a propensity score-matched analysis. J Pain Res. 2020;13:1315–21. https://doi.org/10.2147/JPR.S240138.
Jandura J, Vajda M, Kostysyn R, et al. Previous lumbar spine surgery decreases the therapeutic efficacy of dorsal root ganglion pulsed radiofrequency in patients with chronic lumbosacral radicular pain. J Pers Med. 2023;13(7):1054. https://doi.org/10.3390/jpm13071054.
Acknowledgements
The authors thank all the residents, nurses and radiologic technologists involved in the management of these patients.
Medical Writing/Editorial Assistance
The authors thank John Shaw, supervised by David Michael Abbot, for English revision and editorial assistance.
Funding
No funding was provided for this study from any source and no financial benefits were provided to the authors. No previous presentation of the research, manuscript, or abstract in any form has occurred.
Author information
Authors and Affiliations
Contributions
Matteo Luigi Giuseppe Leoni, Fabrizio Micheli collected the data. Matteo Luigi Giuseppe Leoni performed the statistical analysis. Matteo Luigi Giuseppe Leoni, David Michael Abbott and Marco Mercieri drafted the manuscript. David Michael Abbott, Marco Cascella, Giustino Varrassi, Pasquale Sansone, Roberto Gazzeri, Monica Rocco revised the final manuscript and contributed substantially to the study design.
Corresponding author
Ethics declarations
Conflict of Interest
All the authors (Matteo Luigi Giuseppe Leoni, Fabrizio Micheli, David Michael Abbott, Marco Cascella, Giustino Varrassi, Pasquale Sansone, Roberto Gazzeri, Monica Rocco and Marco Mercieri) have nothing to disclose regarding the topic of this article. They have no affiliation with, or involvement in any organization or entity with any financial or non-financial interest in the subject matter discussed in this manuscript. Giustino Varrassi is an Editor-in-Chief of Pain and Therapy. Giustino Varrassi was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions.
Ethical Approval
This study was approved by the Local Ethics Committee (747/2023/DISP/AUSLPC) and performed in line with the principles of the Declaration of Helsinki.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Leoni, M.L.G., Micheli, F., Abbott, D.M. et al. Transforaminal Steroid Injection After Dorsal Root Ganglion Pulsed Radiofrequency (DRG-PRF): Impact on Pain Intensity and Disability. Pain Ther (2024). https://doi.org/10.1007/s40122-024-00639-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40122-024-00639-w