Abstract
Introduction
Perioperative opioid use has been associated with adverse clinical outcomes. Additionally, opioid disposal carries significant costs, due to the waste of pharmaceutical products and the time needed by skilled labor to report the waste. In this study, we aimed to estimate costs and predict factors of opioid-associated intraoperative product waste, as well as to evaluate whether higher intraoperative opioid doses are associated with increased risk of adverse postoperative outcomes.
Methods
We included 170,607 patients undergoing general anesthesia and receiving intraoperative fentanyl, hydromorphone, or morphine at Beth Israel Deaconess Medical Center, Boston, MA, USA, between January 2010 and June 2020. We estimated product waste-associated costs based on various opioid syringe sizes and determined predictors of opioid waste. Further, we evaluated whether higher opioid doses were associated with postoperative adverse events according to the severity-indexed, incident report-based medication error-reporting program classification. The primary outcome included post-extubation desaturation, postoperative nausea or vomiting, or postoperative somnolence or sedation.
Results
The use of the smallest syringe sizes (50 mcg for fentanyl, 0.2 mg for hydromorphone, and 2 mg for morphine) resulted in the lowest product waste-associated costs. The main predictor of opioid waste was the administration of more than one intraoperative opioid (adjusted odds ratio [aOR] = 7.64, 95% CI 7.40–7.89, P < 0.001). Intraoperative doses of fentanyl > 50–100 mcg (aOR = 1.17 [1.10–1.25], P < 0.001, adjusted risk difference [ARD] 2%) and > 100 mcg (aOR = 1.24 [1.16–1.33], P < 0.001, ARD 3%), hydromorphone > 1 mg (aOR = 1.13 [1.06–1.20], P < 0.001, ARD 2%), and morphine > 2–4 mg (aOR = 1.26 [1.02–1.56], P = 0.04, ARD 3%) and > 4 mg (aOR = 1.45 [1.18–1.77], P < 0.001, ARD 5%) were associated with higher risk of the primary outcome.
Conclusion
Smaller syringe sizes of intraoperative opioids may help to reduce product waste and associated costs, as well postoperative adverse events through utilization of lower intraoperative opioid doses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Perioperative opioid use has been associated with adverse clinical outcomes. |
Opioid disposal, as a result of intraoperative opioid use, is associated with significant costs (waste costs and skilled labor needed to report the waste). |
We estimated the cost of waste based on different syringe sizes and factors that could predict it. Further, we investigated whether higher intraoperative opioid doses are associated with greater risk of adverse postoperative outcomes in surgical patients. |
What was learned from the study? |
Smaller syringe sizes are associated with lower waste costs, and administration of more than one opioid is the strongest predictor of intraoperative opioid waste. |
Smaller syringe sizes of intraoperative opioids may help to reduce product waste, associated costs, and postoperative adverse events. |
Introduction
Preventable adverse drug events and harmful errors when administering inpatient injectable medications result in more than one million hospitalizations per year, with an annual medical cost increase to the United States (US) healthcare system between (US)$2.7 billion and $5.1 billion [1]. Perioperative opioid use has been associated with adverse clinical outcomes, including postoperative respiratory complications [2] and increased risk of readmission in surgical patients [3], thereby further burdening the healthcare system. Moreover, disposal of opioids has been associated with significant healthcare costs, related to both the waste of pharmaceutical products and the time of skilled labor needed to report the waste of the controlled substances [4]. Therefore, strategies to reduce opioid use and associated waste might facilitate avoidance of serious complications, as well as reducing costs.
However, opioid dosing in the operating room is complex [5]. Indeed, some providers may choose the dose of an opioid based on literature or manufacturer suggestions, while others may choose the dose to avoid waste, also defined as unit dosing. With the latter approach, larger product sizes can potentially result in larger unit dosing and may be associated with increased risk of adverse outcomes. This suggests that systematic adoption of smaller product size (lower unit dose) may have significant value for organizations through reduced waste, improved perioperative outcomes, and eventually decreased total costs.
Based on different aliquots of opioids, we aimed to estimate the costs of opioid-associated, intraoperative product waste, as well as predictors of intraoperative opioid waste and postoperative adverse drug events, defined according to the National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) categories, based on the severity-indexed, incident report-based medication error-reporting program classification [6].
Methods
Study Design
In this hospital registry study, we analyzed surgical cases performed between January 2010 and June 2020 at Beth Israel Deaconess Medical Center (BIDMC) in Boston, MA, USA. Data were obtained from several hospital databases, and were subsequently de-identified and merged into a data repository. The local institutional review board reviewed the study and determined that the study met the criteria for exempt status, and the requirement for informed consent was waived (protocol numbers: #2022P000709 and #2022P001059). This study was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments. This manuscript adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [7].
Study Population
Adult patients who underwent surgery or interventional procedures under general anesthesia and received fentanyl, morphine, or hydromorphone intraoperatively were considered for inclusion. We excluded patients with American Society of Anesthesiologists (ASA) physical status classification > IV, those undergoing cardiac surgeries, and those kept intubated after the procedure. For each of the opioids, a single cohort was created. Cases with missing data for confounding variables were excluded, adopting a complete-case method approach.
Product Waste Description
Data on opioids administered intraoperatively to patients undergoing general anesthesia were retrospectively collected from January 2010 to June 2020. In addition, data on actual intraoperative opioid product waste were available from the hospital controlled substance dispensing system records (Omnicell, Mountain View, CA, USA) between June 5, 2020, and June 15, 2022. Hypothetical estimates of intraoperative opioid product waste were calculated based on available ready-to-administer (RTA) syringe sizes as the difference between the syringe size (or multiples of the syringe size) and the actual dose of opioid administered. Specifically, RTA syringe sizes of 50 mcg and 100 mcg were used for fentanyl; 0.2 mg, 0.5 mg, 1 mg, and 2 mg for hydromorphone; and 2 mg and 4 mg for morphine. Hypothetical estimates of product waste were also predicted for the following vial sizes: fentanyl 50 mcg and 100 mcg; hydromorphone 1 mg and 2 mg; morphine 2 mg and 4 mg. We calculated costs associated with product waste, defined as the sum of the cost of the wasted syringe or vial and the cost of skilled labor needed to discard the product. A loss of provider time of 76.2 s to report the waste for syringes was assumed [4]. An additional time of 60 s was assumed to report the waste for vials and to account for the time for vial drawing up. The cost of provider time was calculated on a median hourly wage for nurse anesthetists of $94.04, as estimated by the US Bureau of Labor Statistics [8]. The cost of medications is the average wholesale price (AWP) in the USA and is expressed as US dollars ($) [9].
Identification of Independent Predictors of Opioid Waste
Confounder Model and Outcome Measure
Based on literature review and clinical plausibility, the following variables were evaluated as predictors of intraoperative opioid waste: age, sex, ethnicity and race, ideal body weight, ASA physical status, Charlson Comorbidity Index (CCI) [10], score for prediction of postoperative respiratory complications (SPORC) [11], admission type, source of admission, outpatient use of opioids within 90 days before surgery, year of surgery, duration of anesthesia, emergency surgery, anesthesia technique, and age-adjusted minimum alveolar concentration; use of succinylcholine, non-depolarizing neuromuscular blocking agents, neostigmine, or sugammadex; total volume of intravenous fluids, red blood cell transfusions, vasopressor requirements, and duration of intraoperative hypotension (minutes of mean arterial pressure below 55 mmHg). Further, number of opioids used, individual opioids administered, and use of remifentanil were included, as well as the use of non-opioid adjuvants, such as premedication with oral acetaminophen and/or gabapentinoids, and intraoperative use of ketamine, lidocaine, non-steroidal anti-inflammatory drugs (NSAIDs), magnesium, esmolol, or dexmedetomidine. Lastly, the provider type (i.e., nurse anesthetist, resident, or attending anesthesiologist) was included.
We defined occurrence of product waste as the discrepancy between the actual dose administered and an aliquot (or the combination of multiple available aliquots) of 50 mcg for fentanyl, 1 mg for hydromorphone, and 4 mg for morphine, which represents the current syringe sizes at BIDMC.
Statistical Analyses
A multivariable logistic regression model was built to assess independent predictors of intraoperative opioid waste. Stepwise elimination was performed for variables with a P value > 0.01, and bootstrapping with 1000 replications was used to confirm the appropriate identification of predictors. The relative importance of each predictor was assessed through dominance analysis [12].
Intraoperative Opioid Dose and Clinical Adverse Outcomes
Exposure and Outcome Measures
The primary exposure was the intraoperative opioid dose, categorized as follows: fentanyl > 0–50 mcg, > 50–100 mcg, and > 100 mcg; hydromorphone > 0–0.5 mg, > 0.5–1 mg, and > 1 mg; and morphine > 0–2 mg, > 2–4 mg, and > 4 mg. Opioid categories were chosen according to available RTA syringes or their clinically reasonable combinations. In patients receiving more than one opioid, the total doses of the additional opioids were considered as confounders.
Outcomes were defined in accordance with NCC MERP categories [6]. The primary outcome was the occurrence of any safety events that resulted in temporary harm to the patient and required intervention, including post-extubation desaturation, postoperative nausea or vomiting needing rescue treatment in the post-anesthesia care unit (PACU), and postoperative somnolence or sedation needing nursing observation or administration of naloxone (Category E). The secondary outcomes were defined as (a) harm to the patient that required hospitalization, investigated only in outpatients, represented by delayed discharge from post-anesthesia care unit (length of stay ≥ 120 min), unplanned admission (booked outpatients who required unplanned admission), or delayed discharge from hospital (length of stay > 75th percentile), and readmission within 30 days after hospital discharge (Category F); (b) permanent patient harm, including cardiac arrest and stroke within 7 days postoperatively (Category G); and (c) need for interventions necessary to sustain life: unplanned intubation or intensive care unit admission (all-cause) within 7 days postoperatively (Category H).
Confounder Model
All analyses were adjusted for a priori-defined confounding variables based on literature review and clinical plausibility. These variables included patient demographics such as age, sex, body mass index, and ASA physical status, as well as comorbidities, including chronic heart failure, preoperative drug abuse, obstructive and restrictive lung disease, obstructive sleep apnea, and smoking status. Further, the CCI [10] and SPORC [11] were considered as confounding variables. Case-specific confounders, such as surgical specialty, emergency status, duration of surgery, work relative value units, and year of surgery, were included. Analyses were further adjusted for intraoperative and anesthesia-related factors, including the use of adjunct analgesic or sedative medications (ketamine, dexmedetomidine, regional anesthesia), age-adjusted mean alveolar concentration of inhalational anesthetics, use of neuromuscular blocking agents (non-depolarizing agents and succinylcholine), reversal agents (neostigmine and sugammadex), total volume of intravenous fluids administered, red blood cell transfusions, vasopressor requirements, duration of intraoperative hypotension (minutes of mean arterial pressure < 55 mmHg), ventilation parameters (fraction of inspired oxygen, positive end-expiratory pressure, peak inspiratory pressure, tidal volume), number of anti-emetic medications, and Apfel score [13].
Exploratory Analysis
In an exploratory intent, we investigated the association between the amount of opioids wasted and the primary outcome (Category E).
Statistical Analyses
In the primary analysis, we assessed the association between the categorized dose of each opioid agent and the primary outcome. A multivariable logistic regression model adjusted for the previously mentioned confounders was used. Statistical models, study endpoints, and confounding variables were defined a priori. Potential multicollinearity between confounding variables and the primary exposure was assessed using the variable inflation factor and coefficients of correlation matrix. Continuous confounding variables were categorized into quintiles or clinically relevant categories. All the analyses were performed using Stata software (version 16.0, StataCorp LLC, College Station, TX, USA).
Results
Product Waste Description and Related Costs
A total of 182,109 patients underwent general anesthesia and received intraoperative fentanyl, morphine, or hydromorphone between January 2010 and June 2020. After exclusion criteria, 170,607 patients were included, of which, 148,806 (87.2%) received at least one dose of intraoperative fentanyl, 81,786 (47.9%) at least one dose of hydromorphone, and 10,693 (6.3%) at least one dose of morphine. Patient characteristics according to the intraoperative opioid administered are presented in Table 1. Comparisons among different opioid cohorts are provided in Table S1. Minimal hypothetical product waste and lowest costs associated with product waste were observed for the smallest RTA syringe sizes (Table 2) and for the smallest vials (Table S2). Total product costs were higher for smaller syringes (Table 2). Estimated product waste-associated cost per year, based on a median of 17,076 annual cases, ranged between $513 (morphine RTA 2 mg) and $52,997 (hydromorphone RTA 2 mg). Similarly, for vials, product waste-associated costs varied from a minimum of $661 (morphine 2 mg) to a maximum of $59,895 (hydromorphone 2 mg) (Table S2). Product waste-associated costs, relative to the smallest available RTA syringe, are shown in Fig. 1. Data regarding actual product waste are presented in Supplemental Document, Section S1.
Relative change in product waste-associated cost (cases with waste and without waste) compared to the reference RTA syringes. Reference RTA syringes: fentanyl 50 mcg, hydromorphone 0.2 mg, morphine 2 mg. Costs include the cost of the syringe or vial wasted and the cost of the skilled workforce. RTA ready-to-administer
Independent Predictors of Product Waste
After exclusion criteria and removal of cases with missing data for the selected potential independent predictors of opioid waste, the study cohort for this analysis comprised 139,374 patients (Table S3). Intraoperative opioid waste occurred in 90,155 (64.7%) cases.
Age, clinical referral, intraoperative administration of esmolol, remifentanil, or vasopressors, use of analgesic adjuvants such as ketamine, lidocaine, or dexmedetomidine, total fluids administered, and use of more than one opioid during anesthesia were identified as predictors for waste (Figure S1). Dominance analysis of the individual independent predictors showed that the administration of more than one opioid intraoperatively had the strongest dominance, as determined by its contribution to waste prediction (ranking 1, pseudo-R2 = 0.0654; Figure S1).
Intraoperative Opioid Dose and Adverse Postoperative Outcomes
Study Population
The final study cohorts for this analysis comprised 119,113 patients for fentanyl, 71,483 for hydromorphone, and 8906 for morphine (Fig. 2). The median (IQR) dose of opioids administered was 100 mcg (100–200), 1 mg (0.6–1.2), and 5 mg (4–8) for fentanyl, hydromorphone, and morphine, respectively (Table S4).
Study flow diagram for the analysis of intraoperative opioid use and adverse postoperative outcomes, indicating numbers of patients excluded due to exclusion criteria and missing data. ASA American Society of Anesthesiology, Pts patients, BMI body mass index, SPORC score for the prediction of postoperative respiratory complications, RVU relative value units, NMBA neuromuscular blocking agent, FiO2 fraction of inspired oxygen, PEEP positive end-expiratory pressure, PIP peak inspiratory pressure
Primary Analysis
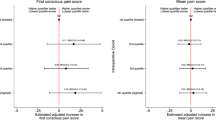
The primary outcome, Category E, including post-extubation desaturation, postoperative nausea and vomiting needing rescue treatment in the PACU, or postoperative somnolence or sedation needing nursing observation or administration of naloxone, was observed in 19,916 (16.7%), 14,332 (20.1%), and 1500 (16.8%) patients of the fentanyl, hydromorphone, and morphine cohorts, respectively. In adjusted analysis, compared to doses of > 0–50 mcg, fentanyl was associated with higher risk of Category E, at doses of > 50–100 mcg (adjusted odds ratio [aOR] = 1.17 [1.10–1.25], P < 0.001, adjusted risk difference [ARD] 2%) and > 100 mcg (aOR = 1.24 [1.16–1.33], P < 0.001, ARD 3%). Compared with > 0–0.5 mg, hydromorphone was not associated with the outcome at doses of > 0.5–1 mg, while it was at doses > 1 mg (aOR = 1.13 [1.06–1.20], P < 0.001, ARD 2%). Compared with doses > 0–2 mg, morphine was associated with an increased risk of Category E, at doses of both 2–4 mg (aOR = 1.26 [1.02–1.56], P = 0.04, ARD 3%) and > 4 mg (aOR = 1.45 [1.18–1.77], P < 0.001, ARD 5%). Results with opioid doses expressed in oral morphine equivalents (OMEs) [14] are reported in Tables S5 and S6. Dose dependency of postoperative Category E per dose of opioids in oral morphine equivalents (mg) is presented in Fig. 3.
Dose dependency of postoperative Category E in patients who received fentanyl (in green), hydromorphone (in red), and morphine (in blue), stratified by oral morphine equivalent dose. The adjusted risk estimates with corresponding 95% confidence intervals (CI) for Category E are presented. The figure shows a direct increase in the risk of Category E at the increased dose of opioid administered. Conversion of oral morphine equivalents to common aliquots for each opioid is shown at the bottom left. Category E is defined as post-extubation desaturation, postoperative nausea and vomiting needing rescue treatment in the post-anesthesia care unit, and postoperative somnolence or sedation needing nursing observation or administration of naloxone
Secondary Analyses
Category F was observed in 44,809 (37.6%), 23,130 (32.4%), and 2835 (31.8%) cases in the fentanyl, hydromorphone, and morphine cohorts, respectively. The risk of Category F was increased for all fentanyl and hydromorphone doses, while only high morphine doses (> 4 mg) were associated with higher risk of this outcome. Category G occurred in 31 (0.03%) and 19 (0.03%) patients in the fentanyl and hydromorphone cohorts, respectively, while only one event was observed in the reference exposure category of the morphine cohort, and therefore the regression model was not applicable. No association was observed between any of the opioid doses and Category G. Category H was observed in 5480 (4.6%), 3760 (5.3%), and 325 (3.6%) cases in the fentanyl, hydromorphone, and morphine cohorts, respectively. The risk of Category H was increased in high (> 100 mcg) fentanyl doses. No association with Category H was observed for morphine. Detailed results of adjusted analyses for secondary outcomes are summarized in Table S6.
Exploratory Analysis
We did not find any association between the dose of opioid wasted and the primary outcome (Category E). Results are detailed in Table S7.
Discussion
In this study, we estimated the product waste for different aliquots of injectable opioids. For all the different opioids, product waste was minimized by reducing RTA syringe or vial size, and was therefore lowest for 50-mcg aliquots of fentanyl, 0.2-mg aliquots of hydromorphone, and 2-mg aliquots of morphine. In addition, we observed that the main predictor of intraoperative opioid waste was the administration of more than one opioid during general anesthesia, which was associated with a sixfold increase in the occurrence of opioid waste. Further, higher doses of intraoperative opioids were associated with a higher risk of adverse events causing temporary harm to the patient and requiring intervention (Category E), specifically post-extubation desaturation, postoperative nausea and vomiting requiring antiemetic administration, and postoperative somnolence and sedation needing observation or naloxone treatment. Higher opioid doses were also associated with increased risk of adverse events resulting in hospitalization or readmission of outpatients (Category F), but were not associated with permanent harm to the patient (Category G) or the need for life-saving treatments (Category H).
Smaller sizes of RTA syringes and vials presented the lowest product waste-associated costs. For example, a 100-mcg fentanyl RTA syringe produced a product waste-associated cost of $2.72, 5.3 times that of a 50-mcg fentanyl RTA syringe, which produced a waste-associated cost of $0.43 per case. This finding is explained by the lower number of vials and RTA syringes wasted with the smallest aliquots. Indeed, this leads to lower cost related to the product discarded and to decreased cost related to waste reports that are required for controlled substances. Considering the high volume of these medications, especially for fentanyl—the most commonly administered intraoperative opioid in our study population—the financial costs may pose a substantial burden to the healthcare system. Compared with the smallest morphine RTA syringes, morphine vials presented lower product waste-associated costs. However, the additional time considered for vial drawing up, assumed to be 60 s, may vary, and no study measured this time directly. In addition, the costs of other disposable items including syringes and needles were not considered for this estimate.
While waste-associated cost was lower with smaller syringe sizes, the total product cost (cost per syringe multiplied by number of syringes needed to achieve the same dose) was higher due to the higher number of syringes needed. However, the cost–value relationship with the use of 50-mcg versus 100-mcg fentanyl RTA syringes (additional $189,761) and 0.5 mg versus 1.0 mg (additional $378,485) of hydromorphone as the default size has to be considered in light of important related factors. First, we predict that more users will switch to using lower unit doses, and therefore we expect a net reduction in total opioid utilization, favoring cost containment. Second, users who expect usage of 1 mg hydromorphone may need to have access to this RTA size, even if barriers are instituted to accessing the larger size such as storage in core dispensing stations rather than located inside the operating rooms, which may impact overall choice. Third, quality improvement strategies to limit the use of more than one opioid per case may also result in a large reduction in total RTA syringes consumed and a significant reduction in costs. In summary, the cost data are important balancing measures for the study and reflect an opportunity for process improvement.
Targeting a reduction in intraoperative opioid waste is important because it may lead to lower costs for the healthcare system, as we showed in our hypothetical estimates of product waste. Our analysis of the predictors of intraoperative product waste informs healthcare personnel on how to prevent opioid waste. When considering the occurrence of product waste, we found that the use of more than one intraoperative opioid was associated with a more than sevenfold increase in the occurrence of waste. Of note, among other predictors, we found that the use of analgesic adjuvants, including ketamine, dexmedetomidine, and lidocaine, was associated with increased opioid waste. This might reflect the provider's choice to adopt opioid-sparing analgesia, administering only a fraction of available vials and RTA syringes [15]. Although analgesic adjuvants were associated with increased opioid waste in our model, their relative contribution compared to the strongest predictor, use of multiple opioids, was negligible (e.g., adjusted absolute risk difference for dexmedetomidine 3.8% vs. 37.3% for using multiple opioids). In addition, given the increasing body of literature supporting multimodal analgesia during surgery to decrease the side effects of opioids, a slight increase in the risk of opioid waste might be tolerable in favor of safer anesthesia and a decrease in opioid adverse events [16].
To the best of our knowledge, our study is the first to use NCC MERP categories to analyze the association between the dose of opioids and their adverse effects. This classification is particularly important, as it associates the adverse effect of a medication with the severity of the outcome and was proposed in 1996 as a standardized categorization of medication errors and safety events [6]. We observed that higher doses of fentanyl, hydromorphone, and morphine were associated with an increased risk of Category E outcomes (adverse events that cause temporary harm to the patient). These findings are in line with a previously published study reporting that lower doses of fentanyl (60–120 mcg for a patient weighing 70 kg) were associated with lower risk of postoperative respiratory complications [2]. Of note, the increased risk per unit of oral morphine equivalents was not similar among the opioids. Indeed, morphine presented a consistently steeper increase in the estimated risk of Category E, when compared with hydromorphone and fentanyl (Fig. 3). This finding may be interpreted as an effect of the different pharmacokinetics and pharmacodynamics of morphine relative to fentanyl and hydromorphone, including a less favorable context-sensitive half time [17] and a longer equilibration half-life between plasma and effect-site (i.e., 2–3 h vs. 6 min for fentanyl) [18].
Regarding the secondary outcomes, higher doses of opioids were associated with an increased risk of delayed discharge from the PACU, unplanned admission, delayed discharge from hospital, and readmission within 30 days (Category F). Thirty-day readmission risk was investigated by Long et al., who showed that doses of intraoperative opioids of nearly 30 mg oral morphine equivalents (e.g., 10 mg intravenous [IV] morphine, 100 mcg of IV fentanyl, and 1.5 mg of IV hydromorphone) were associated with a 15% increase in 30-day readmission [3].
Our findings suggest reduced dosing of opioids to minimize the risk of postoperative adverse events. However, providers may choose the dose of opioid based on the patient’s weight or may prefer to avoid waste reports and use so-called unit dosing. Previous studies have shown that providers usually administer different dosages of opioids based on the syringe/vial size available [19], and this was confirmed in our cohort, where we observed that the median dose for fentanyl and hydromorphone was equivalent to the aliquots or their multiples available at our institution. If this is the case, the availability of RTA syringes that were associated with lower risk of adverse outcome might be preferable. Based on our findings, fentanyl RTA syringes of 50 mcg and morphine of 2 mg may represent the best choices for institutions to decrease adverse events while minimizing costs. For hydromorphone, our analysis points to the 0.5-mg RTA syringe size as the optimal size, since it was not associated with the primary outcome, and it has the potential to further reduce intraoperative opioid exposure relating to unit dosing. While hydromorphone 0.2 mg was associated with the lowest waste and costs, it would be associated with a disproportionate use of disposable syringes with current dosing patterns.
These findings suggest that a quality improvement initiative that implements syringe size reduction may lead to decreased costs and complications. A similar strategy has already been implemented locally by decreasing the aliquot size of neostigmine [20]. This strategy was associated with a decreased incidence of postoperative respiratory complications when combined with a cognitive aid, an educational component, and a financial incentive to decrease postoperative complications in patients receiving neuromuscular blockade intraoperatively and reversal with neostigmine before end of anesthesia [20].
Our findings must be interpreted in the context of the study limitations that arise from its retrospective design. Variable definitions were further limited by the availability of electronically stored data. In addition, we performed a single-center study that limits the generalizability of the results. However, the large cohort size allowed for a wide range of adjustments for covariates derived from highly granular perioperative data. For the estimations of product waste-associated costs, we considered the time spent in preparing the waste report as an average time derived from a previous observational study [4]. This might not reflect the current practice of waste reporting at every institution.
Conclusion
The results of this study show that intraoperative opioid waste-associated costs may be reduced through utilization of smaller aliquots of RTA syringes. Lower doses of intraoperative opioids were further associated with a lower risk of post-procedural Category E and F events. The implementation of low-dose opioid RTA syringes might therefore help in reducing costs, while at the same time reducing postoperative complications by motivating physicians to choose smaller doses. These findings will further guide prospective studies to determine whether a decrease in opioid syringe sizes improves the quality of patient care, as well as alleviating the financial burden of waste and postoperative complications related to opioids.
Data Availability
Requests of qualified researchers trained in human subject research and confidentiality to access additional documents and the dataset may be sent to the corresponding author.
References
Lahue BJ, Pyenson B, Iwasaki K, Blumen HE, Forray S, Rothschild JM. National burden of preventable adverse drug events associated with inpatient injectable medications: healthcare and medical professional liability costs. Am Health Drug Benefits. 2012;5(7):1–10.
Friedrich S, Raub D, Teja BJ, Neves SE, Thevathasan T, Houle TT, et al. Effects of low-dose intraoperative fentanyl on postoperative respiratory complication rate: a pre-specified, retrospective analysis. Br J Anaesth. 2019;122(6):e180–8.
Long DR, Lihn AL, Friedrich S, Scheffenbichler FT, Safavi KC, Burns SM, et al. Association between intraoperative opioid administration and 30-day readmission: a pre-specified analysis of registry data from a healthcare network in New England. Br J Anaesth. 2018;120(5):1090–102.
Hertig J, Jarrell K, Arora P, Nwabueze J, Moureaud C, Degnan DD, et al. A continuous observation workflow time study to assess intravenous push waste. Hosp Pharm. 2021;56(5):584–91.
Wahr JA, Abernathy JH, Lazarra EH, Keebler JR, Wall MH, Lynch I, et al. Medication safety in the operating room: literature and expert-based recommendations. Br J Anaesth. 2017;118(1):32–43.
Hartwig SC, Denger SD, Schneider PJ. Severity-indexed, incident report-based medication error-reporting program. Am J Hosp Pharm. 1991;48(12):2611–6.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10): e296.
Occupational Employment and Wage Statistics. https://www.bls.gov/oes/current/oes_nat.htm. Accessed Dec 7, 2022.
Lexicomp Online. Lexi-Drugs Online UpToDate Inc. Accessed Dec 7, 2022.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Brueckmann B, Villa-Uribe JL, Bateman BT, Grosse-Sundrup M, Hess DR, Schlett CL, et al. Development and validation of a score for prediction of postoperative respiratory complications. Anesthesiology. 2013;118(6):1276–85.
Luchman JN. Determining relative importance in Stata using dominance analysis: domin and domme. Stand Genomic Sci. 2021;21(2):510–38.
Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91(3):693.
Arnold R, Weissman DE. Calculating opioid dose conversions. J Palliat Med. 2003;6:619–20.
Mariano ER, Dickerson DM, Szokol JW, Harned M, Mueller JT, Philip BK, et al. A multisociety organizational consensus process to define guiding principles for acute perioperative pain management. Reg Anesth Pain Med. 2022;47(2):118–27.
Kumar K, Kirksey MA, Duong S, Wu CL. A review of opioid-sparing modalities in perioperative pain management: methods to decrease opioid use postoperatively. Anesth Analg. 2017;125(5):1749–60.
Hughes MA, Glass PS, Jacobs JR. Context-sensitive half-time in multicompartment pharmacokinetic models for intravenous anesthetic drugs. Anesthesiology. 1992;76(3):334–41.
Lötsch J. Pharmacokinetic-pharmacodynamic modeling of opioids. J Pain Symptom Manag. 2005;29(5):90–103.
Stone A, Fields K, Rathmell J, Weiner S, Cotugno M, Pimentel M. Association between fentanyl vial size and dose given: an interrupted time series analysis of intraoperative opioid administration. Br J Anaesth. 2020;124(6):e219–21.
Rudolph MI, Chitilian HV, Ng PY, Timm FP, Agarwala AV, Doney AB, et al. Implementation of a new strategy to improve the peri-operative management of neuromuscular blockade and its effects on postoperative pulmonary complications. Anaesthesia. 2018;73(9):1067–78.
Funding
This study was funded by Fresenius Kabi, USA. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The funder is funding the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
Study concept and design: MSS, SKR. Acquisition, analysis, or interpretation of data: SR, AS, DW, SA, RM-A, NR, SN. Drafting of the manuscript: SR, AS, MSS, SKR. Critical revision of the manuscript for important intellectual content: all authors (SR, AS, DW, SA, RM-A, GC, MK, CS, NR, JH, SN, MSS, SKR). Statistical analysis: SR, AS, DW, SA, GC. Study supervision: JH, MSS, SKR.
Corresponding author
Ethics declarations
Conflict of Interest
Satya K. Ramachandran received honoraria from Fresenius Kabi, USA, and research funding from Fresenius Kabi, USA, and CRICO. The other authors (Simone Redaelli, Aiman Suleiman, Dario von Wedel, Sarah Ashrafian, Ricardo Munoz-Acuna, Guanqing Chen, Mitra Khany, Catriona Stewart, Nikolai Ratajczak, John Hertig, Sarah Nabel, Maximilian S. Schaefer) declare no conflict of interest.
Ethical Approval
The local institutional review board reviewed the study and determined that the study met the criteria for exempt status, and the requirement for informed consent was waived (protocol numbers: #2022P000709 and #2022P001059). This study was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments.
Additional information
Prior Presentation: Part of this work was presented in the form of abstract and poster at the IARS/AUA 2023 Conference in Denver, CO, USA.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Redaelli, S., Suleiman, A., von Wedel, D. et al. Intraoperative Opioid Waste and Association of Intraoperative Opioid Dose with Postoperative Adverse Outcomes: A Hospital Registry Study. Pain Ther 13, 211–225 (2024). https://doi.org/10.1007/s40122-023-00574-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00574-2