Abstract
Introduction
Chronic pain is a distressing condition that should be treated in specialized pain clinics. Pain clinics offer a holistic, evidence-based approach, including pharmacological, complementary, and invasive treatments. This study aimed to provide preliminary information regarding chronic pain treatments and identify reasons for accessing an important hub-spoke pain clinic network.
Methods
A retrospective multicenter cross-sectional study was carried out. A total of 1606 patients’ records were included. Patients were selected from the 26 pain clinics of a single region in Italy. Univariate and multivariate logistic regression models were used.
Results
Multivariate models showed that the use of opioids were considered effective for severe or moderate pain [odds ratio (OR) 0.41; 95% 0.33–0.51], while the use of invasive treatments (OR 2.45; 95% 1.95–3.06) and the use of complementary therapy (OR 1.87; 95% 1.38–2.51) were associated with severe or moderate pain. Overall, age, sex, nonsteroidal anti-inflammatory drugs (NSAID) use, a combination of NSAIDs, complementary therapies, and a combination of opioids and invasive treatments did not seem to be significantly associated with the nature of pain. Multivariate models confirmed that clinical parameters such as the nature of pain, multi-diagnosis, more than one site of pain, treatments, and general practitioner, but not the severity of pain and use of invasive treatments, had an impact on the choice of a pain clinic.
Conclusion
Opioids are useful in managing moderate or severe chronic pain. Multimodal approaches are used for the management of chronic pain. Moreover, it is not clear how patients are addressed to access different pain clinics (spoke versus hub) networks. More widespread adoption is needed for an interdisciplinary approach to managing chronic pain and adopting guideline recommendations, and rigorous research is required to provide more substantial evidence and support clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
To our knowledge, there is only one study that describes treatments in pain clinics in Italy. |
The use of the new pain therapy network has never been investigated. |
What was learned from this study? |
Chronic non-cancer pain is a public health problem that frequently requires specialist treatment in pain clinics. A network would be preferable if well coordinated. |
This study describes the prevalence of multimodal pain management approaches in a pain clinic network. |
Invasive treatments and complementary therapies are useful in managing severe or moderate chronic pain. |
The use of opioids and invasive treatments are an integral part of the multimodal approach for chronic non-cancer pain management and are considered useful in severe or moderate pain. |
The clinical complexity of patients with chronic pain often does not represent a requirement for choosing a hub versus a spoke pain center. |
Introduction
Chronic pain (CP) is one of the most common reasons for patients to seek medical care [1], and it is a personal, subjective, multidimensional, and intangible experience. CP is defined as “pain that persists past normal healing time, and/or recurs for more than three months” [2]. In Italy, CP affects about a quarter of the population [3, 4]. The new definition and classification of CP introduces chronic primary pain syndromes and chronic secondary pain syndromes [2]. Primary is defined as chronic pain in one or more anatomical regions. Secondary pain syndromes are linked to other diseases as the underlying cause. In all cases, CP syndromes are associated with significant emotional distress or functional disability, which negatively affect quality of life [5, 6] or the enjoyment of life [4], as well as with significant increases in morbidity and mortality [7]. Targeted and appropriate prevention and management strategies need to take into account the bio-psycho-socio-demographic and lifestyle determinants, and outcomes of pain [8]. However, it is estimated that about half of the patients with chronic pain receive inadequate pain management [9]. With regards to pain management interventions, it is recommended that the following results should be measured in each clinical trial evaluating the effectiveness of any pain treatment: pain, physical functioning, emotional functioning, participant ratings of improvement and satisfaction with treatment, symptoms and adverse events, and participant disposition [10]. Nevertheless, the situation is not as clear as it seems, since the characteristics of chronic pain and of pain suffered by patients are as heterogeneous as the diversity of therapy approaches to chronic pain syndromes [11]. Therefore, it is necessary to adopt a comprehensive and inter/trans-disciplinary approach to treating CP, considering both pharmacological and nonpharmacological treatments [8, 12]. The approach to CP management should reflect the biopsychosocial nature of chronic pain, typically requiring a multidimensional treatment strategy. A wide range of analgesics have been used in the treatment of chronic pain, but there is inconsistent evidence on the effectiveness of pain management programs [13]. Pharmacological interventions should include a multimodal analgesic approach and use principles that maximize efficacy and minimize the adverse effects of these treatments. A multimodal analgesic approach includes non-opioid analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, complementary therapies, and adjuvants [13,14,15,16,17]. There is a scientific basis for the use of polypharmacy owing to the complex nature of pain neurobiology [18]. According to the best available evidence, some treatments exist, even for painful neuropathic chronic pain. Spinal cord stimulation and other invasive techniques can effectively manage patients with refractory pain [14, 19, 20].
Moreover, some pain management methods use non-pharmacological approaches, such as psychological interventions, physical therapies, and complementary therapies [13, 21]. Primary care and pain clinics are healthcare services that use a basic and advanced interdisciplinary approach to help people to manage their pain and regain control of their life in many countries, including Italy [1, 7, 22]. In Italy and all regions, the organizational model of the pain management network provides a concentration of the most complex cases in a small number of centers of excellence (hubs), responsible for providing highly complex diagnostic and therapeutic interventions, supported by a network of local services (spokes) operating on an outpatient basis [23]. Pain clinics use holistic, evidence-based models with an interdisciplinary team approach, where the health practitioners share the same goal and treatment plan, thus representing the gold standard of multimodal approaches [24]. Moreover, education programs and interprofessional education delivered by advanced health practitioners can improve the assessment of chronic pain and the understanding and accepting of pain control, quality of life, or psychological distress [16, 25]. Although there are studies that describe treatments used in pain clinics around the world [26, 27], to our knowledge, only one study describes treatments in pain clinics in Italy [22]. The use of the new pain therapy network has never been investigated. This study aims to provide preliminary information regarding the treatments of chronic pain in pain management clinics (PMCs) in one region of Italy, and to identify the reasons for choosing a hub over a spoke pain clinic network.
Methods
Design
This was an observational, multicenter, cross-sectional study retrospectively reviewing clinical records. The target population were patients who attended a PMC clinic in central Italy (Latium region) at least once in 2011 (either as a first visit or successive visits). Data were collected between January 2012 and February 2014. This study represents the third step of an epidemiological research project. We adhered to the recommendations issued by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Initiative.
Sampling
A random sample of 1606 patients (considering a 5% significance level and a power of 80%) was calculated to identify a quantitative effect size equal to about 0.15 (Student’s t-test) and an odds ratio (OR) of about 1.35 using the chi-square test for the analyses of qualitative data. In the study, the sample was stratified by PMC, and thus the power was probably increased. Patients were selected from the 26 PMCs active in 2011 in the Latium region [23, 28], of which 4 were hubs and 22 were spoke PMCs. The hub–spoke model involves a network of health care institutions, with one centralized hub offering specialized services complemented by secondary pain clinics, the spokes, which provide more limited care. Information was extracted from the clinical records of the PMCs, using a structured template because of the different assessment tools used by each PMC.
Data Collection
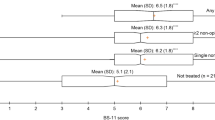
Sociodemographic variables (age and sex) were extracted from the records. The following variables were considered: severity of pain, number of sites, and duration (< 24 months or ≥ 24 months). Pain intensity was classified according to the Numeric Rating Scale (NRS) (scores ranging from 0 to 10) and categorized into four distinct classes: absent (0), mild (1–3), moderate (4–6), and severe (7–10). Pain intensity was included in the first follow-up. We used the following classification of CP: chronic primary and secondary musculoskeletal pain, chronic neuropathic pain, and chronic visceral pain. When CP had more than one component, it was classified as mixed [2]. In addition, pharmacological treatments, such as NSAIDs, weak opioids (tramadol, tapentadol, codeine, acetaminophen-codeine, tramadol-acetaminophen), strong opioids (morphine, oxycodone, fentanyl, methadone, hydromorphone, oxycodone-acetaminophen, oxycodone-naloxone, buprenorphine, others), adjuvants (antidepressants, anticonvulsants, benzodiazepines, corticosteroids, others), and non-pharmacological treatments (psychological-based interventions, physical therapies, acupuncture, others) used to treat the chronic pain were described.
Inclusion and Exclusion Criteria
Male and female adults aged between 18 and 70 years who attended a PMC in the Latium region between 1 January 2011 and 31 December 2011, and whose medical records reported a CP diagnosis were included. Patients with migraine or headaches, and those affected by chronic cancer pain were excluded. Patients with incomplete or unclear medical records were also excluded.
Ethical Consideration
An independent ethics committee approved the study protocol of the Policlinic of Tor Vergata University of Rome (master), Italy, and for each independent ethics committee of the participating investigational pain centres: (1) Policliclinic Gemelli of Rome, (2) ASL Latina of Latina, (3) AO San Camillo-Forlanini Hospital of Rome, (4) AO San Giovanni-Addolorata Hospital of Rome, (5) Policlinic Umberto I, Sapienza University of Rome, and (6) Policlinic Campus Bio-Medico, Rome, Italy. This study was conducted in compliance with the Declaration of Helsinki's ethical principles and Good Clinical Practice Guidelines.
Statistical Analysis
We synthesized quantitative variables according to mean values and their relative standard deviations (SD), whereas for qualitative variables, absolute and percentage frequencies were used. When appropriate, comparisons between groups were evaluated by Pearson’s chi-square test and Student’s t-test. Univariate and multivariate logistic regression models were used to estimate the risk of having musculoskeletal pain versus other types, moderate or severe pain intensity versus mild or absent pain, and being directed to spoke versus hub clinics. We built the multivariate models by choosing as explanatory variables those found to be statistically significant in the univariate models. The forward selection method was chosen with a probability of entry and exit from the model equal to 0.05 and 0.10, respectively. A p-value < 0.05 was considered statistically significant. All analyses were conducted using SPSS statistical software v.21.0.
Results
The pharmacological, non-pharmacological, and interventional treatments documented in the 1606 outpatient records of the pain clinics were described. Pharmacological treatments were used in 68.7% (1103), invasive treatments in 48.1% (772), and complementary treatments in 15.4% (248). The type of pharmacological (chi-square = 4.337, df = 11, p = 0.959) and invasive (chi-square = 0.967, df = 1, p = 0.325) treatments showed no statistically significant differences between the two sexes. Females tended to a greater use of complementary therapies (chi-square = 3.723, df = 1, p = 0.054).
Types of Treatment and Pain Severity
Table 1 summarizes the therapeutic approaches relative to the intensity of pain. While opioids, adjuvants, and complementary and pharmacological treatments increase significantly with pain severity, NSAIDs and paracetamol do not.
Types of Treatment and Nature of Pain
Table 2 describes the relationship between the type of treatment and the nature of chronic non-cancer pain. Each treatment resulted in statistically significance, except for paracetamol and NSAIDs. Chronic pain was primarily musculoskeletal (44%) in nature, followed by mixed (29.9%), neuropathic (21%), and visceral (1%). CP was caused by musculoskeletal conditions such as lumbago (16.1%), lumbosciatica (11.5%), and arthritis (11.3%). Neuropathic chronic pain was mainly reported in the case of lumbosacral root lesions (13.4%), trigeminal neuralgia (10.1%), and fibromyalgia (3%). Visceral pain was very seldom reported (< 1%). More information on diagnoses, classified according to the International Classification of Diseases, Ninth Revision (ICD-9), can be found in Latina et al. (2019) [28].
Univariate and Multivariate Analysis: Severity and Nature of Pain Influenced by Treatments
Table 3A presents the results of univariate and multivariate logistic regressions. Univariate analysis suggests that opioids, invasive treatments, and complementary therapies were the only parameters associated with the severity of pain, but on the multivariate model, we found that severe/moderate pain was significantly associated only with the use of invasive treatments (OR 3.35; 95% 2.01–5.59). In Table 3B, we evaluated the variables associated with the nature of pain (musculoskeletal pain versus mixed/neuropathic pain). Univariate analysis suggests that opioids, invasive treatments, and complementary therapies were the only parameters associated with musculoskeletal pain, and these results are maintained in a multivariate model: the use of opioids protects from musculoskeletal pain rather than mixed/neuropathic pain (OR 0.41; 95% 0.33–0.51), while patients who use invasive treatments (OR 2.45; 95% 1.95–3.06) and complementary therapy (OR 1.87; 95% 1.38–2.51) are more likely to suffer from musculoskeletal pain. Overall, age, sex, NSAID use, a combination of NSAIDs and complementary therapies, and a combination of opioids and invasive treatments did not seem to be significantly associated with the nature of pain.
Univariate and Multivariate Analysis: Choice of Spoke Versus Hub Pain Clinics
We describe the last sets of models in Table 4. In these logistic regression models, we evaluated the choice of therapy pain clinic (spoke versus hub) associated with clinical characteristics and complexity of chronic pain.
Univariate models showed that the choice of spokes was associated with intermittent pain, other-than-bodily pain, mild/no pain, a multi-diagnosis, more than one site of pain, the use of noninvasive treatments, pharmacological treatments, complementary treatment therapies, and GP referral. Multivariate models confirmed that all these parameters, but not the severity of pain and use of invasive therapies, impacted the choice of pain clinic.
Discussion
This study aimed to provide preliminary information regarding the treatments of CP in PMCs in Italy, and to identify the reasons for accessing the Italian network (hub versus spoke pain clinics) to manage CP. This study sheds light on CP management after the Italian Law 38/2010 was enacted and the Regional Network for the management of CP was established. Pain management aims to improve the psycho–physical, emotional, and social dimensions of health and functioning in CP patients using a holistic approach by an interdisciplinary team [29, 30]. We found that integrated treatment approaches were used in pain clinics, mainly pharmacological and invasive therapies, since pain clinics can offer advanced treatments, which primary care cannot fully provide for very complex patients owing to the complex nature of pain [18] or for patients with refractory pain. A multimodal analgesic approach includes NSAIDs, opioids, and adjuvants [14, 15]. Over half of the studied patients use opioid therapy, and their choice shows a statistically significant association with the intensity and nature of the CP. Although National Institute for Health and Care Excellence (NICE) guidelines recommend not starting with opioids to manage primary chronic pain in people aged 16 years and over [16], in our case, the results of multivariate logistic regressions suggest that the nature seems to influence the use of opioids and the use of complementary treatments, as well as invasive treatments for pain management. The results of multivariate logistic regressions suggest that severe/moderate pain was significantly associated with the benefit of invasive therapies. Given the high use of these treatments, it is plausible that many of these patients have been suffering from pain for a long time (more than 24 months) [28].
Moreover, opioid use has benefits as well as potentially serious risks. However, many Americans have been impacted by the severe harm associated with their use [31], but this is not the case in Italy or Europe as a whole, where the prevalence of opioid dependence among adults is low and varies considerably between countries [32]. In Italy, the use of pain medication has progressively increased over the years, with an average annual variation of 1.7%, rising from 6.9 defined daily dose (DDD)/1000 inhabitants. In particular, the use of effective opioids for pain therapy has progressively increased over time (from 2014 to 2020), with an annual average variation of 5.5% [33].
In our results, the multivariate analysis describes how the use of invasive treatments relates to the nature and intensity of the pain. A recent review shows that invasive treatments as adjuvants to conventional medical treatment can be effectively used for managing patients with refractory pain [20]. Despite the publications on these therapies, considerable controversy surrounds the efficacy of most invasive treatments. The primary purpose of most invasive treatments continues to be pain severity or the reduction of opioid use. For example, most experts would not consider a two-point decrease in pain score a successful outcome if the study participant doubled their opioid dosage and stopped working due to increasing functional impairment [34].
Moreover, the quality of the outcomes depends on research. In scenarios where blinding of the participant is not possible or feasible, blinding of the outcome assessor can still function to reduce bias. Surprisingly, most invasive pain therapy trials have not been double-blinded [35].
Our results showed that the use of complementary therapies is minimal. This is in contrast with many other studies [17]. Among complementary treatments, acupuncture is the most prevalent. Its use is related to increased pain intensity; it is used in therapy with intensive pharmacological treatments in cases of severe pain. Studies also focus on the treatment of musculoskeletal and mixed chronic pain. Acupuncture reduced pain and improved quality of life in the short term (up to 3 months) compared with sham acupuncture or usual care [16]. There was not enough evidence to determine longer-term benefits [16]. A previous survey shows a partial use of complementary therapies to treat chronic pain and reduced use caused by economic and cultural barriers [34]. However, there is a lack of good-quality studies focusing on non-pharmacological approaches to treating CP [20].
Finally, the authors want to point out that this research did not demonstrate the effectiveness of the treatment strategies but only described treatment prescribed in outpatient records. First, every pain therapy center uses approaches that do not always clearly consider the guidelines (GL) available. This could reflect the heterogeneity of the treatments provided by the individual pain center in the same network. Although there are guidelines in some countries [14,15,16, 21], in Italy, no guidelines have been published on chronic non-cancer pain management. The Italian National Institute of Health is working hard to adapt international guidelines, using the International Guideline Evaluation Screening Tool (IGEST) [36] and the GRADE-ADOLOPMENT approach [37, 38]. This last approach combines the advantages of adolopment/adoption and the development of the new guidelines, which guarantees a high methodological rigor so that the recommendations are applicable in a health system context different from the ones produced.
The results of our univariate and multivariate logistic regression (Table 4) regarding the choice of type of pain clinic (spoke versus hub) demonstrate that some clinical characteristics (nature/quality of pain, multi-diagnosis in chronic pain, and > 1 sites of pain), pharmacological and complementary therapies, and free choice of pain clinic, were significantly associated with the intention of spoke pain clinics for pain management. Based on the advice of specialists, patients with severe/moderate pain and those needing invasive treatments were directed to the hub clinic for pain management. The complexity of their case did not appear to affect whether patients were referred to the spoke or the hub. They are characterized by different levels of care intensity and are distributed throughout the region and the country, according to a structured network. The pain therapy hub hospital centers represent regional reference structures with high care complexity and guarantee pain management through an interdisciplinary approach for complex pathologies, using dedicated multidisciplinary teams. Spokes, on the other hand, are outpatient pain therapy centers, which aim to carry out various integrated diagnostic, pharmacological, instrumental and/or surgical treatments aimed at reducing pain and disabilities associated with people assisted on an outpatient basis, independent of the etiology/pathogenesis of the painful condition. A recent study in the same network showed a lack of a multi-professional or interdisciplinary approaches to chronic pain management [23]. The main problem is that many patients wait a long time before consulting with a specialist in pain clinics. The activation of the treatment path starts from an initial evaluation of the patient by the GP, who can request specialist consultations to manage the patient’s chronic pain. At least in Italy, pain therapy consultations do not have clear priority criteria for rapid access to tertiary pain clinics. A proposed model uses priority criteria for admission to consultation with a pain specialist [39]. The tool allows a fast and straightforward numerical validated instrument, to correctly manage the priority assignation of patients affected by chronic pain. This model avoids either improper admission to the emergency room if not indicated, or consulting a specialist too early for patients who could still be managed appropriately by their GP.
This survey has some limitations. Firstly, the research was restricted to only one Italian region (Latium), and it is a retrospective study, despite collecting a numerically and statistically significant sample. Secondly, this study is not able to evaluate the efficacy and the appropriateness of the application of therapeutic regimes. Lastly, we have not been able to assess the effectiveness and efficiency of the pain therapy network because, to date, a series of indicators capable of measuring the pain therapy network has not been determined, as already in use in the palliative care setting [40].
A strength of this study is that this is one of the very few studies on tertiary pain clinics in Italy, and all clinical information was provided by the medical records filled in by the medical and nursing staff working in the tertiary pain clinics, thus limiting or avoiding errors and recall bias.
Conclusions
Pain clinic networks offer multimodal treatments to patients suffering from chronic pain of different clinical complexity. It is unclear how patients access other pain clinics (spoke versus hub) and which approach is used for pain management. The method mainly observed appears more oriented toward medical science, given the lack of a holistic, interdisciplinary approach. Opioids were considered useful in the management of moderate/severe chronic pain. There is promising evidence of a positive impact of advanced clinical and nursing practice in the interdisciplinary management of pain on health and economic outcomes. More widespread adoption of a multidisciplinary approach to managing chronic pain is needed, especially in pain clinics. Recommendations for guidelines and further rigorous research are required to provide more substantial evidence in the field, to support the clinical practice of the practitioners. Furthermore, the complexity of chronic pain patients should represent a requirement for choosing a hub versus a spoke pain center.
Change history
04 April 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40122-023-00503-3
References
Camilloni A, et al. Chronic non-cancer pain in primary care: an Italian cross-sectional study. Signa Vitae. 2021;17(2):54–62.
Treede RD, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19–27.
Del Giorno R, et al. Assessment of chronic pain and access to pain therapy: a cross-sectional population-based study. J Pain Res. 2017;10:2577–84.
Notaro P, et al. Chronic, acute and acute-on-chronic pain prevalence in a tertiary care hospital setting. Eur Rev Med Pharmacol Sci. 2021;25(10):3848–58.
Girach A, et al. Quality of life in painful peripheral neuropathies: a systematic review. Pain Res Manag. 2019;23:2091960.
Paterniani A, et al. Quality of life and disability of chronic non-cancer pain in adults patients attending pain clinics: a prospective, multicenter, observational study. Appl Nurs Res. 2021;14: 151332.
Mills S, Torrance N, Smith BH. Identification and management of chronic pain in primary care: a review. Curr Psychiatry Rep. 2016;18(2):22.
Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019;123(2):e273–83.
Breivik H. A major challenge for a generous welfare system: a heavy socio-economic burden of chronic pain conditions in Sweden and how to meet this challenge. Eur J Pain (Lond Engl). 2012;16(2):167.
Dworkin RH, et al. Research design considerations for confirmatory chronic pain clinical trials: IMMPACT recommendations. Pain. 2010;149(2):177–93.
Deckert S, et al. A systematic review of the outcomes reported in multimodal pain therapy for chronic pain. Eur J Pain. 2016;20(1):51–63.
Holliday S, et al. Prescribing wellness: comprehensive pain management outside specialist services. Aust Prescr. 2018;41(3):86–91.
National Institute for Health and Care Excellence (NICE). Chronic pain in over 16s: assessment and Management. Draft for consultation, August 2020. https://ww.nice.org.uk/guidance/gid-ng10069/documents/draft-guideline. Accessed 5 July 2022.
Scottish Intercollegiate Guidelines Network (SIGN). Management of chronic pain. Edinburgh: SIGN. (SIGN publication no. 136). [First published December 2013 Revised edition published August 2019]. https://www.sign.ac.uk/media/1108/sign136_2019.pdf. Accessed 25 Aug 2022.
Registered Nurses’ Association of Ontario (RNAO). Assessment and Management of Pain. 3rd ed. Toronto: Registered Nurses’ Association of Ontario; 2013.
National Institute for Heath and Care Excellence (NICE) and Royal College of Physicians. Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and Management of chronic primary pain (NG193–2021). Available from: nice.org.uk. Accessed 6 Sep 2022.
Almutairi NM, et al. Efficacy of acupuncture, intravenous lidocaine, and diet in the management of patients with fibromyalgia: a systematic review and network meta-analysis. Healthcare. 2022;10(7):1176.
Dworkin RH, et al. Considerations for extrapolating evidence of acute and chronic pain analgesic efficacy. Pain. 2011;152(8):1705–8.
Hylands-White N, Duarte RV, Raphael JH. An overview of treatment approaches for chronic pain management. Rheumatol Int. 2018;37(1):29–42.
Liampas A, et al. Non-pharmacological management of painful peripheral neuropathies: a systematic review. AdvTher. 2020;37(10):4096–106.
Smith BH, Hardman JD, Stein A, Colvin L, SIGN Chronic Pain Guideline Development Group, et al. Managing chronic pain in the non-specialist setting: a new SIGN guideline. Br J Gen Pract. 2014;64(624):e462–4.
Leuter C, et al. Care strategies and therapeutic pathways for chronic pain patients in Abruzzo Region. Italy Ann Ig. 2017;29(1):63–72.
Latina R, et al. Features and organization of Pain Centers in the Lazio Region, Italy, in 2011. Ann Ig. 2014;26(4):367–79.
Gordon RM, et al. A transdisciplinary team approach to pain management in inpatient health care settings. Pain ManagNurs. 2014;15(1):426–35.
Courtenay M, Carey N. The impact and effectiveness of nurse-led care in the Management of acute and chronic pain: a review of the literature. J Clin Nurs. 2008;17(15):2001–13.
Wan T, Gurupur V, Patel A. A Longitudinal analysis of total pain scores for a panel of patients treated by pain clinics. Health Serv Res Manag Epidemiol. 2019;6:2333392818788420.
Gouvinhas C, et al. Interventional pain management in multidisciplinary chronic pain clinics: a prospective multicenter cohort study with one-year follow-up. Pain Res Treat. 2017;2017:8402413.
Latina R, et al. Epidemiology of chronic pain in the Latium region, Italy: A cross-sectional study on the clinical characteristics of patients attending pain clinics. Pain Manag Nurs. 2019;20(4):373–81.
British Pain Society.Guidelines for Pain Management Programmes for adults An evidence-based review prepared on behalf of the British Pain Society. Published by: The British Pain Society, 3rd floor Churchill House, 35 Red Lion Square, London WC1R 4SG, 2013. https://www.britishpainsociety.org/static/uploads/resources/files/pmp2013_main_FINAL_v6.pdf. Accessed 11 July 2022.
Andraka-Christou B, et al. Pain clinic definitions in the medical literature and U.S. state laws: an integrative systematic review and comparison. Subst Abuse Treat Prev Policy. 2018;13(1):17.
US Food and Drug Administration (FDA). Opioid Medications. www.fda.gov/drugs/information-drug-class/opioid-medications. 2021. Accessed 30 June 2022.
European Monitoring Centre for Drug and Drug Addiction. Opioids: Health and Social Responses 2021. https://www.emcdda.europa.eu/best-practice/briefings/tackling-opioid-dependence_en. Accessed 30 Aug 2021.
Italian Medicines Agency (AIFA). The Medicines Utilisation Monitoring Centre. National Report on Medicines use in Italy. Year 2020. Rome: AIFA. First Edition 2021. https://www.aifa.gov.it/documents/20142/1542390/Rapporto-OsMed-2020.pdf. Accessed 5 July 2022.
Cohen SP, et al. Unique aspects of clinical trials of invasive therapies for chronic pain. Pain Rep. 2018;4(3):e687.
Latina R, et al. The use of complementary therapies for chronic pain in Italian hospices. Prof Inferm. 2012;65(4):244–50.
D’angelo D, et al. The International Guideline Evaluation Screening Tool (IGEST): development and validation. BMC Med Res Methodol. 2022;22(1):134.
Schünemann HJ, et al. GRADE Evidence to Decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. J Clin Epidemiol. 2017;81:101–10.
Fauci AJ, et al. Clinical practice guideline for the integrated Management of major trauma by the Italian National Institute of Health: process and methods. Ann Ist Super Sanita. 2021;57(4):343–51.
Miceli L, et al. Management of chronic pain in Italy: proposal for specific priority criteria. Ig Sanita Pubbl. 2018;74:407–18.
D’Angelo D, et al. Palliative care quality indicators in Italy. What do we evaluate? Support Care Cancer. 2012;20(9):1983–9.
Acknowledgements
We thank all nurses and physicians who shared this publicly available data and PAIN CLINICS GROUP (PCG): Enrica Adducci, Roberto Arcioni, Laura Bertini, Concetta Bisbiglia, Mario Bosco, Massimiliano Carassiti, Maurizio Capogrossi, Gianni Colini Baldeschi, Maria Antonietta De Meo, Giorgio D’Este, Paolo Diamanti, Luigi D’Orazio, Stefano Fabroni, Amedeo Gagliardi, Santo Laganà, Emanuele La Placa, Ivano Mattozzi, Giuseppe Montone, Linda Natalini, Giuseppe Rabuffi, Carlo Reale, Riccardo Rinaldi, Giovanni Siena, Maurizio Stefani, Luca Quadrino.
Funding
This research received no specific grant from public, commercial, or not-for-profit funding agencies. No funding or sponsorship was received for this study or publication of this article.
Author Contributions
Roberto Latina, Gianfranco Tarsitani, Maria Grazia De Marinis, Paolo Notaro, Ettore Di Biagio and Giustino Varrassi contributed to the conception and study design. Diana Giannarelli, Irene Terrenato, Roberto Latina, Antonella Paladini, Rosaria Alvaro, Laura Iacorossi, Daniela D’Angelo, Dhurata Ivziku, Francesco Gravante, Nicola Veronese, Mario Barbagallo, Anna Marchetti, and PCG contributed to acquisition of data, analysis and interpretation of data. Giustino Varrassi, Cristina Martella, Rosaria Alvaro, Latina Roberto, Ettore Di Biagio and Francesco Gravante revised the article critically for important intellectual content and interpreted the results. All authors read and approved the final manuscript.
Disclosures
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. Roberto Latina, Giustino Varrassi, Ettore Di Biagio, Maria Grazia De Marinis, Gianfranco Tarsitani, Paolo Notaro, Diana Giannarelli, Irene Terrenato, Cristina Martella, Rosaria Alvaro, Antonella Paladini, Laura Iacorossi, Daniela D’Angelo, Dhurata Ivziku, Francesco Gravante, Anna Marchetti, and PCG have nothing to disclose.
Compliance with Ethics Guidelines
An independent ethics committee approved the study protocol of the Policlinic of Tor Vergata University of Rome (master), Italy, and for each independent ethics committee of the participating investigational pain centres (Policliclinic Gemelli of Rome, ASL Latina of Latina, AO San Camillo-Forlanini Hospital of Rome, AO San Giovanni-Addolorata Hospital of Rome, Policlinic Umberto I, Sapienza University of Rome, Policlinic Campus Bio-Medico, Rome, Italy,). This study was conducted in compliance with the Declaration of Helsinki's ethical principles and Good Clinical Practice Guidelines.
Data Availability
There are no shared data in the present study. Data is available on reasonable request to the Corresponding Author.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised to correct the affiliations of authors Laura Iacorossi and Irene Terrenato.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Latina, R., Varrassi, G., Di Biagio, E. et al. Chronic Non-cancer Pain Management in a Tertiary Pain Clinic Network: a Retrospective Study. Pain Ther 12, 151–164 (2023). https://doi.org/10.1007/s40122-022-00446-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00446-1