Abstract
Introduction
Listeriosis is a severe food-borne disease caused by Listeria monocytogenes infection. The data of listeriosis in Xi’an population are limited. The aim of this study is to evaluate the clinical features and fatality risk factors for listeriosis in three tertiary-care hospitals in Xi’an, China
Methods
The characteristics of demographic data, underlying diseases, clinical manifestations, laboratory indicators, cranial imaging examination, antibiotics therapeutic schemes, and clinical outcomes were collected between 2011 and 2023. Logistic regression analysis was performed.
Results
Seventy-one etiologically confirmed listeriosis patients were enrolled, including 12 neonatal and 59 non-neonatal cases. The majority of neonatal listeriosis presented as preterm (50%) and fetal distress (75%). The main clinical manifestations of non-neonatal listeriosis included fever (88%), headache (32%), disorder of consciousness (25%), vomiting (17%), abdominal pain (12%), and convulsions (8%). The fatality rate in neonatal cases was higher than in non-neonatal listeriosis (42 vs. 17%). Although no deaths were reported in maternal listeriosis, only two of 23 patients had an uneventful obstetrical outcome. Five maternal listeriosis delivered culture-positive neonates, three of whom decreased within 1 week post-gestation due to severe complications. Twenty-eight cases were neurolisteriosis and 43 cases were bacteremia. Neurolisteriosis had a higher fatality rate compared with bacteremia listeriosis (36 vs. 12%). The main neuroradiological images were cerebral edema/hydrocephalus, intracranial infection, and cerebral hernia. Listeria monocytogenes showed extremely low resistance to ampicillin (two isolates) and penicillin (one isolate). The fatality risk factors were the involvement of the central nervous system, hyperbilirubinemia, and hyponatremia for all enrolled subjects. Hyperuricemia contributed to the elevation of fatality risk in non-neonatal listeriosis.
Conclusions
When the patients suffered with symptoms of fever and central nervous system infection, they should be alert to the possibility of listeriosis. Early administration of ampicillin- or penicillin-based therapy might be beneficial for recovery of listeriosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Listeriosis, which is caused by Listeria monocytogenes infection, presents a variety of syndromes, ranging from subclinical and uncomplicated febrile gastroenteritis to severe invasive infection. The data of listeriosis in Xi’an population are limited. |
We want to analyze the clinical characteristics, outcomes, and risk fatality factors of listeriosis from three tertiary-care hospitals in Xi’an between 2011 and 2023. |
What was learned from the study? |
The main presentations of neonatal listeriosis were preterm and fetal distress, with higher fatality rate. The main clinical manifestations of non-neonatal listeriosis were fever, headache, disorder of consciousness, vomiting, abdominal pain, and convulsions. Maternal listeriosis always led to eventful obstetrical outcomes. |
The fatality risk factors were the involvement of the central nervous system, hyperbilirubinemia, and hyponatremia for all enrolled subjects. Hyperuricemia contributed to the elevation of fatality risk in non-neonatal listeriosis. |
When patients suffer from symptoms of fever and central nervous system infection, they should be alert to the possibility of listeriosis. Early administration of ampicillin- or penicillin-based therapy might be beneficial for recovery of listeriosis. |
Introduction
Listeria monocytogenes (L. monocytogenes) is a Gram-positive intracellular pathogen that is widespread in the environment [1]. The main routes of L. monocytogenes transmission are believed to be contracted through consumption of contaminated food (especially processed meat, prepared vegetables and fruits, pre-packed sandwiches, soft cheeses, and unpasteurized milk) [2,3,4,5,6] and vertical transmission from mother to newborn [7,8,9]. L. monocytogenes infection in human, which is known as listeriosis, is mostly sporadic, but food-borne outbreaks are also observed [10,11,12]. Listeriosis presents a variety of syndromes in humans, ranging from subclinical and uncomplicated febrile gastroenteritis to severe invasive infection [1, 13]. Invasive listeriosis can be categorized into three main clinical forms, including non-maternal listeriosis, maternal listeriosis, and neonatal listeriosis. Non-maternal listeriosis also mainly manifests as bacteremia or septicemic listeriosis as well as central nervous system infection, such as meningitis or meningoencephalitis (generically referred as neurolisteriosis) [1, 13, 14]. Listeriosis manifestations also include peritoneal cavity infection, osteoarthritis, pneumonia, myocarditis, urinary tract infection, and endophthalmitis, accounting for approximate 1% of total L. monocytogenes infections [1].
The estimated incidence of listeriosis ranges between 0.1 and 11.3 cases per 100,000 persons, depending on geographical location and surveillance [5]. Most listeriosis cases have been reported from industrialized Western countries. In the United States, the Foodborne Disease Active Surveillance Network has been implementing laboratory-based surveillance in listeriosis epidemiology since 1996 [1], revealing a stable incidence rate estimated to be 0.3 per million population in United States over the period from 2006 to 2022 [15,16,17], leading L. monocytogenes as the fourth causative pathogen in bacterial meningitis [18]. Since 2000, China has made strong effects and improved surveillance systems for monitoring and controlling listeriosis [14, 19]. Feng et al. reviewed the listeriosis patients reported in China from 1964 to 2010 and found 147 sporadic listeriosis cases reported, with the only outbreak recorded among students in an elementary school in Zhejiang Province in October of 2003 [20]. Chen et al. also investigated listeriosis in China from 2008 to 2017 and showed that 759 cases were reported from 22 provinces, with an overall fatality rate of 18% [19]. All listeriosis cases were recorded as being sporadic, and no outbreaks were reported during this period [19, 21]. However, the data is still limited regarding the clinical features and prognostic factors of L. monocytogenes infection in China due to the relatively late start of the monitoring system [14, 19]. In particular, there were limited investigations describing L. monocytogenes infection in Xi’an, China. Thus, we retrospectively reviewed all identified listeriosis cases in three tertiary-care hospitals in Xi’an, Shaanxi Province, from 2011 to 2023, and described the clinical characteristics, outcomes, and risk factors of death of L. monocytogenes-infected patients.
Methods
Ethics
The study protocol was approved by the Institutional Review Board of Tangdu Hospital (No. K202309-10), Shaanxi Provincial People’s Hospital (No. 2023-0135), and The Second Affiliated Hospital of Xi’an Medical University (No. 23EC027). This study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. We used an anonymized database for all analyses, and all potentially identifying variables were removed.
Definition and Data Collection
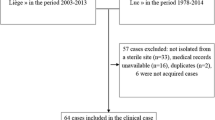
This was a hospital-based retrospective study on patients infected with L. monocytogenes from May 2011 to July 2023 in the above three tertiary care hospitals in Xi’an. The diagnosis of listeriosis was based on one of the following factors: isolation of L. monocytogenes from blood, cerebrospinal fluid (CSF), or placenta; detection of L. monocytogenes species-specific reads in body fluid using metagenomic next-generation sequencing (mNGS). The cases were categorized as maternal, neonatal, and non-maternal infections [22]. Maternal infection was defined based on the isolation of L. monocytogenes from pregnant women [13, 14, 22]. Neonatal infection was defined based on the isolation of L. monocytogenes from 1-month-old or younger neonates [14, 22]. Bacteremia was defined as isolation or detection of L. monocytogenes from blood without neurolisteriosis [13, 14]. Neurolisteriosis was defined as isolation or detection of L. monocytogenes from CSF or isolation of L. monocytogenes from blood while accompanied by symptoms of central nervous system infection [13, 14].
Clinical data from identified cases were abstracted from the medical records, including demographic information, underlying diseases, sites from which the organism was isolated or detected, clinical manifestations, laboratory indicators when identified as listeriosis, cranial imaging examinations, anti-microbial therapeutic schemes, and clinical outcomes.
Statistical Analyses
Statistical analyses were performed using SAS Version 9.4 (SAS Institute Inc, Cary, NC, USA) and SPSS Version 25.0 (IBM SPSS Software, Chicago, IL, USA). For categorical variables, data were presented as n (%). Fisher’s exact test was used for comparison. Continuous variables following normal distribution were presented as mean ± standard deviation. Student’s t test was used for comparison between two groups. One-way analysis of variance was used for comparison among groups, and Student–Newman–Keuls-q test was further used for comparison between the two groups. Continuous variables following skewed distribution were presented as median (interquartile range) [M (Q1, Q3)]. Mann–Whitney U test was used for comparison between two groups. Kruskal–Wallis H test was used for comparison among groups, and Dunn’s multiple comparison test was further used for comparison between the two groups. The influencing factors of death were examined using univariate and multivariate stepwise logistic regression models, with results expressed as odds ratios (OR) with 95% confidence intervals (CI). A P value less than 0.05 was considered statistically significant.
Results
Characteristics of Neonatal and Non-neonatal Listeriosis
A total of 71 patients with listeriosis, including 12 neonatal and 59 non-neonatal cases, diagnosed between 2011 and 2023 in three tertiary hospitals in Xi’an, Shaanxi Province, China. The clinical characteristics of neonatal and non-neonatal listeriosis are shown in Table 1. All neonatal listeriosis were diagnosed less than 6 days of life (age range, 20 min ~ 4 days) and were identified as early onset infection. The majority of neonatal cases presented as preterm (50%) and fetal distress (75%). The fatality rate in the neonatal group was slightly higher than in the non-neonatal group (Table 1; 42 vs. 17%). The main clinical manifestations in non-neonatal group included fever (88%), headache (32%), disorder of consciousness (25%), vomiting (17%), abdominal pain (12%), and convulsions (8%). Twenty-three non-neonatal listeriosis patients had underlying diseases (Table 1). Among them, seven cases were receiving steroid administration and nine cases were receiving chemotherapy. Both groups had elevated median white blood cell (WBC) count (> 10 × 109/l). The mean percentage of neutrophils was elevated in the non-neonatal group but was in the normal range in the neonatal group (Table 1). The median aspartate aminotransferase (AST) and total bilirubin (T-BIL) levels were elevated, while the median albumin and globulin levels were reduced in the neonatal group (Table 1). The median procalcitonin level was also strongly increased in the neonatal group (Table 1).
Characteristics of Maternal Listeriosis and the Connection with Neonatal L. monocytogenes Infection
There were 23 maternal cases of listeriosis identified. Thirteen patients were confirmed by isolation of L. monocytogenes from blood, while ten patients were diagnosed by isolation of L. monocytogenes from placenta. The mean gestation was 26.61 ± 6.79 weeks (range, 14 ~ 38 weeks). Twelve maternal infections (52%) occurred in the second trimester of pregnancy (14 ~ 28 weeks), and 11 patients (48%) were recognized in the third trimester of pregnancy (> 28 weeks). The median WBC count [16.76 (14.13, 21.08) × 109/l] and CRP level [88.00 (52.84, 116.2) mg/l] was strongly elevated. None of the maternal infections had central nervous system involvement and all cases fully recovered after delivery. Two cases had normal pregnancy outcome, and one case had paraplegia in a newborn (hedratresia). There were 15 abortions as a result of L. monocytogenes infections (11 cases in the second trimester and four cases in the third trimester of pregnancy). Importantly, obstetrical outcomes included five cases of listeriosis in the infants postpartum, which were the results of L. monocytogenes infections in the third trimester of pregnancy. The characteristics of maternal-neonatal listeriosis are shown in Table 2. These five neonatal listeriosis cases suffered with fetal distress and sepsis. Three neonatal cases with severe complications, such as respiratory failure and septic shock, decreased in less than 1 week (Table 2).
Characteristics of Bacteremia and Neurolisteriosis
There were 43 cases of bacteremia and 28 cases of neurolisteriosis identified. Sixteen cases of neurolisteriosis were isolated or detected L. monocytogenes from blood. Bacteremia listeriosis had a higher survival rate (88%) compared with neurolisteriosis (64%) (Table 3). There were no statistically significant differences in the levels of indicators for blood routine test, CRP, or procalcitonin between bacteremia and neurolisteriosis (P > 0.05, Table 3). Bacteremia listeriosis had lower levels of total protein, albumin, and urea nitrogen but higher levels of uric acid and chloride compared with neurolisteriosis (P < 0.05, Table 3). Neurolisteriosis revealed elevated blood glucose levels, which were higher than the upper limit of normal and significantly higher than in bacteremia (P < 0.001, Table 3).
Twenty-six neurolisteriosis received lumbar puncture. Twenty-five cases had abnormal appearance (turbid) and/or color (yellow) of CSF. Sixteen patients (62%) had elevated CSF pressure with median level of 240 (135, 300) mmH2O. However, the CSF pressure in the death cases was lower than in survival case of neurolisteriosis [128 (103, 247) mmH2O vs. 270 (185, 335) mmH2O, P = 0.022]. Pyocytes were detected in CFS in two neurolisteriosis. The total cell count in CSF was 522 (360, 746) × 106/l, while the WBC count in CSF was 429 (288, 674) × 106/l, which were significantly elevated than upper limits of normal. The median percentage of polymorphonuclear cells in CSF was 62.50 (28.75, 70.00)%, while the median percentage of mononuclear cells in CSF was 37.50 (30.00, 71.25)%. All 26 neurolisteriosis cases had robustly elevated protein level in CSF [2046 (809.1, 5630) mg/l]. The median CSF glucose [3.09 (1.39, 5.88) mmol/l] and chloride (112.0 ± 8.99 mmol/l) level was remarkably down-regulated. There were no significant differences in laboratory indicators of CSF between survival and death cases of neurolisteriosis (P > 0.05). Twenty-five neurolisteriosis patients received cranial imaging examinations (computed tomography and/or magnetic resonance imaging). Fifteen patients had abnormal cranial imaging. Eleven cases presented as cerebral edema/hydrocephalus (two patients underwent lateral ventricular drainage), five cases revealed intracranial infection, and three patients showed cerebral hernia. All neurolisteriosis death cases had cerebral edema/hydrocephalus or hernia.
Antibiotic Susceptibility and Therapeutic Strategy
Fifty-nine cases were positive for L. monocytogenes of blood culture, and 18 cases were positive for L. monocytogenes of CSF culture. Antibiotic susceptibility test for 59 of L. monocytogenes isolates from blood showed that one isolate was resistant to ampicillin, one resistant to penicillin, two resistant and two non-sensitive to meropenem, two resistant and one non-sensitive to trimethoprim-sulfonamide (SMZ), one resistant and five non-resistant to erythromycin. Antibiotic susceptibility test for 18 of L. monocytogenes isolates from CSF revealed that no isolates were resistant to ampicillin, one intermediate to penicillin, one non-sensitive to meropenem, one resistant to SMZ, one intermediate and seven non-resistant to erythromycin. Thirty-nine patients were administrated ampicillin or penicillin-based therapy. Fifteen patients received meropenem-based therapy. Fifteen patients received piperacillin/tazobactam treatment. Two cases, who received empirical ceftriaxone therapy, unfortunately died before obtaining antibiotic susceptibility test results.
Fatality Risk Factors for Listeriosis Patients
A total of 56 listeriosis patients survived in response to therapy, but 15 patients died due to L. monocytogenes infection. The death group had a higher ratio of male patients (73 vs. 30%, P = 0.002, Table 4), and elevated T-BIL level compared with survival group (P = 0.017, Table 4). Although the death group had increased levels of eosinophils percentage, hemoglobin, AST, urea nitrogen, Ca2+, procalcitonin, but decreased Cl− level, these differences just missed statistical significance (Table 4).
We firstly included all enrolled subjects (both non-neonatal and neonatal listeriosis) to analyze the fatality risk factors. The results showed that male gender (OR 4.83; 95% CI 1.08–21.56; P = 0.039), neurolisteriosis (OR 6.03; 95% CI 1.33–27.22; P = 0.020), T-BIL (OR 6.03; 95% CI 1.33–27.22; P = 0.020), and uric acid (OR 5.14; 95% CI 1.17–22.61; P = 0.030) presented an increased fatality risk in the univariate model (Table 5). After adjusting for age, gender, neurolisteriosis, blood routine, liver and kidney function indicators, electrolytes, blood glucose, CRP, and procalcitonin, we found that neurolisteriosis (OR 10.88; 95% CI 1.61–73.53; P = 0.014) and T-BIL (OR 13.74; 95% CI 1.85–101.94; P = 0.010) increased the fatality risk (Table 4). However, Na+ showed a reduced fatality risk in the multivariate-adjusted regression analysis (OR 0.10; 95% CI 0.01–0.82; P = 0.032) (Table 5). We then separately analyzed the fatality risk factors for non-neonatal and neonatal listeriosis. Age (OR 1.07; 95% CI 1.01–1.14; P = 0.030), male gender (OR 10.38; 95% CI 1.10–98.20; P = 0.041), neurolisteriosis (OR 11.67; 95% CI 1.23–110.80; P = 0.032), immunosuppression (OR 8.00; 95% CI 1.24–51.68; P = 0.029) and uric acid (OR 11.33; 95% CI 1.68–76.26; P = 0.013) revealed an increased fatality risk of non-neonatal listeriosis in the univariate model (Table 6). After adjusting for age, gender, neurolisteriosis, blood routine, liver and kidney function indicators, electrolytes, blood glucose, CRP, and procalcitonin, uric acid (OR 11.33; 95% CI 1.68–76.26; P = 0.013) elevated the fatality risk in non-neonatal listeriosis (Table 6). However, no correlates of the risk of neonatal listeriosis fatality were observed (Table 7).
Discussion
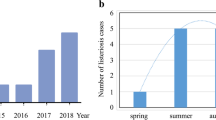
In this retrospective study, we found that listeriosis was sporadic in Xi’an from 2011 to 2023, without the evidence of an outbreak. Similar to the previous reports [19,20,21], L. monocytogenes infection predominantly manifested as bacteremia (61%), while others presented as central nervous system infection (39%). The current study involved 23 maternal L. monocytogenes infections, leading to the predominance of female cases (61%), which was different to the large-scale analyses in China [19,20,21]. The total fatality rate was 21% (15/71), which was similar to the published retrospective reviews in China by Chen et al. in total infected population (18%) [19] and by Fan et al. in non-perinatal listeriosis (24%) [21]. The overall case fatality rate was notably lower than the international average rate of 30% [23]. It was shown that the evolution rate of L. monocytogenes was lower, leading to a specific geographical distribution of L. monocytogenes [24]. Although we did not perform the molecular characterization analysis of L. monocytogenes isolates, the lower fatality rate in Xi’an and other cities in China might be associated with the differences in predominance of serogroup, sequence types, and clone complexes between L. monocytogenes strains in China and other countries/regions [25,26,27]. L. monocytogenes infections analyzed in this study revealed that human listeriosis in Xi’an was mainly concentrated in spring and summer, which was related to the transmission feature of food-borne disease by contaminated food. The similar seasonal variation has been observed in other Chinese studies [19, 21], which might be the seasonal pattern of listeriosis in China. The prevalence of L. monocytogenes in food products in Shaanxi province was 11%, which was the highest value and significantly higher than the average prevalence of 4.42% in Chinese food products from 28 provinces [28]. However, only one non-neonatal case in this analysis confirmed the history of contaminated food ingestion. This might be due to the fact that listeriosis was characterized by a wide spectrum of infections and L. monocytogenes infection has a long incubation period, resulting in the difficulty in tracking an accurate food eating history [5]. Thus, listeriosis can be easily misdiagnosed in clinical practice. It is also important to understand the clinical features of L. monocytogenes infection for a timely diagnosis of listeriosis.
A total of 35 cases of L. monocytogenes infections (23 maternal and 12 neonatal listeriosis) during perinatal period were reported in this study, accounting for 49% cases in overall studied patients. All maternal patients presented as bacteremia without the involvement of central nervous system infection. The main symptom was fever, and no cases of death were reported. This was consistent with the previous findings that listeriosis in pregnancy usually revealed non-specific, influenza-like clinical presentation with a low fatality rate [7, 8, 29,30,31]. Although most maternal listeriosis showed mild febrile illness, the laboratory testing results revealed remarkably higher WBC counts and CRP levels in this study, indicating the strong inflammatory response in L. monocytogenes-infected pregnant women. This might be the reason that maternal listeriosis always leads to adverse pregnancy outcomes. Although all maternal listeriosis cases accepted proposals for sensitive antibiotics therapy, 65% (15/23) had abortions due to listeriosis because these patients revealed the histopathological and/or micrological-proven L. monocytogenes infection in the placenta. Eight cases had singleton live births, but five of them delivered culture-positive neonates. Three maternal listeriosis patients who delivered uninfected neonates received penicillin therapy, which might prevent direct transmission of infection to the fetus or neonate. Taken together with other published literature [7, 8, 13, 29,30,31], maternal listeriosis could induce devastating consequences for the fetus and newborns. All 12 enrolled neonatal listeriosis cases were identified as early onset infection, and the most common symptom was fetal distress with the fatality rate of 42% (5/12). The WBC count was slightly increased, but the procalcitonin level was robustly elevated. This was in line with the findings in clinical features of neonatal L. monocytogenes infection reported in China [30, 31]. However, the fatality rate was still higher than the L. monocytogenes-infected newborns in France [9] and other early onset bacterial infection in term infants [32], owing to the intrapartum antibiotic prophylaxis only in high-risk pregnant women.
A total of 36 cases of non-maternal adult listeriosis were reported in this study, accounting for 51% of cases in the overall enrolled patients. Two-thirds of non-maternal listeriosis patients were neurolisteriosis. Invasive L. monocytogenes infection mainly affected non-maternal individuals with immunocompromised conditions [33]. The MONALISA perspective study in France showed that 97% of bacteremia listeriosis cases had underlying diseases, including neoplasm, diabetes, or were receiving immunosuppressive therapy [13]. Neurolisteriosis also mainly occurred in the elderly and immunocompromised patients [1, 34, 35]. A retrospective study in the Netherlands revealed that L. monocytogenes infection accounted for approximately 16% of community-acquired bacterial meningitis in patients 80 years or older [36]. The symptoms of non-maternal listeriosis included fever (85–90%) patients and disorder of consciousness (20%) [13, 37]. In this study, the average age of non-maternal listeriosis was > 50 years, and > 60% patients (22 cases) had underlying diseases. Among them, 17 cases underwent immunocompromised conditions, including steroid administration (seven cases), chemotherapy (nine cases), and AIDS (one case). Only one patient met the criteria of “healthcare-associated case”, which was defined as an onset of listeriosis symptoms more than 48 h post admission for medical conditions other than listeriosis [22]. This bacteremia listeriosis case was diagnosed as multiple myeloma, and received stem cells transplantation. This patient suffered from a sudden onset of high fever 4 days post transplantation, with WBC count only 0.03 × 109/l. Previous findings show that only 40% neurolisteriosis patients had the classical triad of bacterial meningitis as fever, neck stiffness, and a change in mental status [1, 37,38,39]. Neurolisteriosis patients also typically present with a slow onset of symptoms, with a lesser extent elevation of CSF leukocyte counts, high CSF level, and low CSF to blood glucose ratio [13, 37]. The main neuroradiological images are meningeal enhancement, abscess, hemorrhages, contrast-enhancing ventricles, or hydrocephalus [40, 41]. The clinical characteristics of neurolisteriosis cases enrolled in this study matched all the above features. Thus, when the patients with underlying diseases or in the immunocompromised conditions suffered from clinical symptoms of fever or central nervous system infection, they should be alert to the possibility of listeriosis. Early administration of ampicillin- or penicillin-based therapeutic strategy might be beneficial in clinical recovery of listeriosis.
Due to the limited enrolled subjects of the current study, we divided all patients into bacteremia and neurolisteriosis. Although neurolisteriosis seemed to have a higher fatality rate than bacteremia, only urea nitrogen and blood glucose revealed statistically significant differences between the two groups. Thus, we attempted to seek the risk factors associated with death in all cases with invasive L. monocytogenes infection. Niu et al. showed that consumption of Chinese cold dishes increased the risk of L. monocytogenes infection by 3.43-fold in Beijing, China [42]. The MONALISA perspective study indicated that the strongest fatality predictors for bacteremia and neurolisteriosis were ongoing cancer, multi-organ failure, aggravation of pre-existing organ dysfunction, and monocytopenia [13]. A Spanish retrospective study also showed that the main factors associated with early fatality (less than 5 years) after recovery were age and with the comorbidities of diabetes, chronic kidney disease, liver disease, and cancer [43]. Herein, our present data showed that neurolisteriosis and elevated T-BIL increased the fatality risk, but serum sodium level showed a reduced fatality risk in all enrolled subjects. This indicated that the risk factors of fatality for listeriosis were the involvement of central nervous system, hyperbilirubinemia, and hyponatremia in all enrolled subjects. It was also well accepted that craniocerebral injury caused by trauma or meningitis always resulted in hyperkalemia, which contributed to the elevation of fatality rate [44]. Although we did not find statistically significant differences of serum potassium levels between the survival and death cases, the serum potassium level should be monitored, especially in neurolisteriosis. Hyperbilirubinemia increased the risk of infection in the surgical intensive care unit even though the sepsis-related jaundiced patients were excluded [45]. Hyponatremia also reflected the severity of the underlying process, although it did not induce specific symptoms and might be overlooked by clinicians [46]. Of note, Shuaib et al. revealed that hyperbilirubinemia and hyponatremia yielded a discriminatory value for the diagnosis of complicated appendicitis [47]. Thus, T-BIL and serum sodium levels can be considered as adjuvant predictors of poor clinical outcomes in neurolisteriosis in all enrolled subjects. We further separately analyzed the fatality risk factors for neonatal and non-neonatal listeriosis because the neonates had different backgrounds in anatomy, physiology, and biochemistry with adults. We found that no correlates of the risk of neonatal listeriosis fatality were observed. In our point of view, the limited enrolled number (n = 12) probably contributed to this negative result. Interestingly, hyperuricemia contributed to the elevation of fatality risk in non-neonatal listeriosis. Previous reports revealed that hyperuricemia was associated with increased risk of 90-day all-cause mortality and the incidence of acute kidney injury in patients with sepsis [48]. High uric acid levels were also associated with adverse outcomes in patients hospitalized for coronavirus disease 2019 [49]. Thus, we suggested that evaluating hyperuricemia as a potential marker might reflect poor prognostic baseline characteristics in non-neonatal listeriosis.
There were several limitations in this study. On the one hand, due to the limited sample size, the interpretation of the current findings still needs further elucidation in a larger-scale cohort. On the other hand, L. monocytogenes infection is strongly associated with host immune status. We only described the immunocompromised conditions of the listeriosis patients, and objective clinical index reflecting immune conditions, such as CD4+/CD8+ T cell count and cytokine levels, should be investigated in these patients.
Conclusions
When patients suffer from symptoms of fever or central nervous system infection, they should be alert to the possibility of listeriosis. The main risk factors for death due to listeriosis are the involvement of the central nervous system, hyperbilirubinemia, and hyponatremia. Early administration of ampicillin- or penicillin-based therapy might be beneficial for recovery of listeriosis.
Data Availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Koopmans MM, Brouwer MC, Vazquez-Boland JA, et al. Human listeriosis. Clin Microbiol Rev. 2023;36(1): e0006019.
Schlech WF 3rd, Lavigne PM, Bortolussi RA, et al. Epidemic listeriosis–evidence for transmission by food. N Engl J Med. 1983;308(4):203–6.
Farber JM, Peterkin PI. Listeria monocytogenes, a food-borne pathogen. Microbiol Rev. 1991;55(3):476–511.
Barza M. Listeriosis and milk. N Engl J Med. 1985;312(7):438–40.
Swaminathan B, Gerner-Smidt P. The epidemiology of human listeriosis. Microbes Infect. 2007;9(10):1236–43.
Ravindhiran R, Sivarajan K, Sekar JN, et al. Listeria monocytogenes an emerging pathogen: a comprehensive overview on listeriosis, virulence determinants, detection, and anti-listerial interventions. Microb Ecol. 2023;86(4):2231–51.
Wang Z, Tao X, Liu S, et al. An update review on Listeria infection in pregnancy. Infect Drug Resist. 2021;14:1967–78.
Khsim IEF, Mohanaraj-Anton A, Horte IB, et al. Listeriosis in pregnancy: an umbrella review of maternal exposure, treatment and neonatal complications. BJOG. 2022;129(9):1427–33.
Charlier C, Kermorvant-Duchemin E, Perrodeau E, et al. Neonatal listeriosis presentation and outcome: a prospective study of 189 cases. Clin Infect Dis. 2022;74(1):8–16.
Popovic I, Heron B, Covacin C. Listeria: an Australian perspective (2001–2010). Foodborne Pathog Dis. 2014;11(6):425–32.
McCollum JT, Cronquist AB, Silk BJ, et al. Multistate outbreak of listeriosis associated with cantaloupe. N Engl J Med. 2013;369(10):944–53.
Gaul LK, Farag NH, Shim T, et al. Hospital-acquired listeriosis outbreak caused by contaminated diced celery–Texas, 2010. Clin Infect Dis. 2013;56(1):20–6.
Charlier C, Perrodeau E, Leclercq A, et al. Clinical features and prognostic factors of listeriosis: the MONALISA national prospective cohort study. Lancet Infect Dis. 2017;17(5):510–9.
Shi C, Lv D, Zhou K, et al. Clinical and laboratory characteristics of patients infected by Listeria monocytogenes at a Tertiary Hospital in Hefei City. China Infect Drug Resist. 2021;14:4409–19.
Marder Mph EP, Griffin PM, Cieslak PR, et al. Preliminary incidence and trends of infections with pathogens transmitted commonly through food - foodborne diseases active surveillance network, 10 US sites, 2006–2017. MMWR Morb Mortal Wkly Rep. 2018;67(11):324–8.
Collins JP, Shah HJ, Weller DL, et al. Preliminary incidence and trends of infections caused by pathogens transmitted commonly through food - foodborne diseases active surveillance network, 10 US sites, 2016–2021. MMWR Morb Mortal Wkly Rep. 2022;71(40):1260–4.
Delahoy MJ, Shah HJ, Weller DL, et al. Preliminary incidence and trends of infections caused by pathogens transmitted commonly through food - foodborne diseases active surveillance network, 10 US sites, 2022. MMWR Morb Mortal Wkly Rep. 2023;72(26):701–6.
Thigpen MC, Whitney CG, Messonnier NE, et al. Bacterial meningitis in the United States, 1998–2007. N Engl J Med. 2011;364(21):2016–25.
Chen S, Meng F, Sun X, et al. Epidemiology of human listeriosis in China during 2008–2017. Foodborne Pathog Dis. 2020;17(2):119–25.
Feng Y, Wu S, Varma JK, et al. Systematic review of human listeriosis in China, 1964–2010. Trop Med Int Health. 2013;18(10):1248–56.
Fan Z, Xie J, Li Y, et al. Listeriosis in mainland China: a systematic review. Int J Infect Dis. 2019;81:17–24.
Wang HL, Ghanem KG, Wang P, et al. Listeriosis at a tertiary care hospital in Beijing, China: high prevalence of nonclustered healthcare-associated cases among adult patients. Clin Infect Dis. 2013;56(5):666–76.
Lomonaco S, Nucera D, Filipello V. The evolution and epidemiology of Listeria monocytogenes in Europe and the United States. Infect Genet Evol. 2015;35:35172–83.
Moura A, Criscuolo A, Pouseele H, et al. Whole genome-based population biology and epidemiological surveillance of Listeria monocytogenes. Nat Microbiol. 2016;2:16185.
Ji S, Song Z, Luo L, et al. Whole-genome sequencing reveals genomic characterization of Listeria monocytogenes from food in China. Front Microbiol. 2022;13:1049843.
Li W, Guo Y, Cui Q, et al. Whole-genome sequencing-based characterization of Clinical Listeria monocytogenes isolates in China, 2013–2019. Foodborne Pathog Dis. 2023;20(4):158–68.
Zhu L, Ji X, Wu Y, et al. Molecular characterization of Listeria monocytogenes strains isolated from imported food in China from 14 countries/regions, 2003–2018. Front Cell Infect Microbiol. 2023;13:1287564.
Li W, Bai L, Fu P, et al. The epidemiology of Listeria monocytogenes in China. Foodborne Pathog Dis. 2018;15(8):459–66.
Madjunkov M, Chaudhry S, Ito S. Listeriosis during pregnancy. Arch Gynecol Obstet. 2017;296(2):143–52.
Zhan Y, Xu T, Liu H, et al. Perinatal infection with Listeria monocytogenes: a 10-year hospital-based study in Western China. J Inflamm Res. 2023;16:1243–54.
Qu L, Meng GL, Wang Q, et al. A comprehensive analysis of listeriosis in 13 pregnant women and 27 newborns in Xi’an from 2011 to 2020. Transl Pediatr. 2022;11(9):1482–90.
Polcwiartek LB, Smith PB, Benjamin DK, et al. Early-onset sepsis in term infants admitted to neonatal intensive care units (2011–2016). J Perinatol. 2021;41(1):157–63.
Munoz-Gallego I, Candela Ganoza G, Chaves F, et al. Listeria monocytogenes bacteraemia over an 11-year period: clinical and epidemiologic characteristics in the south area of Madrid. J Infect. 2017;75(3):276–8.
Lu X, Yang H, Wang Y, et al. Analysis of clinical and microbiological features of Listeria monocytogenes infection. Infect Drug Resist. 2023;16:2793–803.
Pagliano P, Ascione T, Boccia G, et al. Listeria monocytogenes meningitis in the elderly: epidemiological, clinical and therapeutic findings. Infez Med. 2016;24(2):105–11.
van Soest TM, Chekrouni N, van Sorge NM, et al. Community-acquired bacterial meningitis in patients of 80 years and older. J Am Geriatr Soc. 2022;70(7):2060–9.
Koopmans MM, Brouwer MC, Bijlsma MW, et al. Listeria monocytogenes sequence type 6 and increased rate of unfavorable outcome in meningitis: epidemiologic cohort study. Clin Infect Dis. 2013;57(2):247–53.
Dzupova O, Rozsypal H, Smiskova D, et al. Listeria monocytogenes meningitis in adults: the Czech Republic experience. Biomed Res Int. 2013;2013: 846186.
Amaya-Villar R, Garcia-Cabrera E, Sulleiro-Igual E, et al. Three-year multicenter surveillance of community-acquired Listeria monocytogenes meningitis in adults. BMC Infect Dis. 2010;10:324.
Charlier C, Poiree S, Delavaud C, et al. Imaging of human neurolisteriosis: a prospective study of 71 cases. Clin Infect Dis. 2018;67(9):1419–26.
Lainez-Ramos Bossini AJ, Redruello-Guerrero P, Martinez-Barbero JP, et al. Epidemiology, clinical and imaging features of rhombencephalitis caused by L. monocytogenes. A retrospective observational study. Rev Neurol. 2023;76(12):385–90.
Niu YL, Wang TY, Zhang XA, et al. Risk factors for sporadic listeriosis in Beijing, China: a matched case-control study. Epidemiol Infect. 2022;150:1–21.
Rivera-Izquierdo M, Galicia-Garcia MD, Lainez-Ramos-Bossini AJ, et al. Risk factors associated with early mortality after recovery from severe listeriosis: a multicentre 17-year longitudinal study. Infection. 2023;51(1):181–91.
Dao AQ, Mohapatra S, Kuza C, et al. Traumatic brain injury and RSI is rocuronium or succinylcholine preferred? Curr Opin Anaesthesiol. 2023;36(2):163–7.
Field E, Horst HM, Rubinfeld IS, et al. Hyperbilirubinemia: a risk factor for infection in the surgical intensive care unit. Am J Surg. 2008;195(3):304–6.
Liamis G, Milionis HJ, Elisaf M. Hyponatremia in patients with infectious diseases. J Infect. 2011;63(5):327–35.
Shuaib A, Alhamdan N, Arian H, et al. Hyperbilirubinemia and hyponatremia as predictors of complicated appendicitis. Med Sci (Basel). 2022;10(3):36.
Liu S, Zhong Z, Liu F. Prognostic value of hyperuricemia for patients with sepsis in the intensive care unit. Sci Rep. 2022;12(1):1070.
Feldman I, Natsheh A, Breuer GS. Hyperuricemia and adverse outcomes in patients hospitalized for COVID-19 disease. Clin Med Res. 2023;21(2):87–94.
Acknowledgements
We thank the participants of the study.
Funding
The study was supported by a grant from Clinical Research Center for Infectious Diseases of Shaanxi Province (2021LCZX-09). The journal’s Rapid Service fee was also funded by this grant.
Author information
Authors and Affiliations
Contributions
Study conception and design were performed by Ye Zhang, Wei-Lu Zhang, Yang Sun, Yu Li, and Jian-Qi Lian. Material preparation, data collection and analysis were performed by Wen Xu, Mei-Juan Peng, Lin-Shan Lu, Zhen-Jun Guo, A-Min Li, Jing Li, Yan Cheng, Jia-Yu Li, Yi-Jun Li, Jian-Qi Lian, Yu Li, Yang Sun, Wei-Lu Zhang, Ye Zhang. The first draft of the manuscript was written by Ye Zhang, Wei-Lu Zhang, Yang Sun, and Yu Li. All authors commented on previous versions of the manuscript, and read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
Wen Xu, Mei-Juan Peng, Lin-Shan Lu, Zhen-Jun Guo, A-Min Li, Jing Li, Yan Cheng, Jia-Yu Li, Yi-Jun Li, Jian-Qi Lian, Yu Li, Yang Sun, Wei-Lu Zhang, and Ye Zhang declare that they have no competing interests.
Ethical Approval
The study protocol was approved by the Institutional Review Board of Tangdu Hospital (No. K202309-10), Shaanxi Provincial People’s Hospital (No. 2023-0135), and The Second Affiliated Hospital of Xi’an Medical University (No. 23EC027). This study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. We used an anonymized database for all analyses, and all potentially identifying variables were removed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xu, W., Peng, MJ., Lu, LS. et al. Clinical Characteristics and Fatality Risk Factors for Patients with Listeria monocytogenes Infection: A 12-Year Hospital-Based Study in Xi’an, China. Infect Dis Ther (2024). https://doi.org/10.1007/s40121-024-00986-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40121-024-00986-3