Abstract
Introduction
Since hematopoietic stem cell transplant (HSCT) is an important therapy for malignant and non-malignant pediatric diseases, improving transplant-related mortality remains a challenge. Currently, rituximab, a monoclonal antibody of anti-CD20, is widely used for several post-HSCT complications. However, few studies have focused on the application of rituximab before HSCT.
Methods
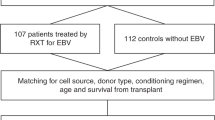
We conducted a retrospective case–control study from January 2019 to July 2021 to determine this effect in a single center. Forty-eight patients were included in the rituximab group, with a one-to-one ratio matched to the control group.
Results
Both the occurrence rate and cumulative incidence rate of Epstein–Barr virus (EBV) infection were significantly lower in the rituximab group than in the without-rituximab group (10.4% vs. 33.3%, p = 0.014 and 12.2% vs. 39.3% p = 0.0026, respectively). Furthermore, without the application of rituximab was identified as a risk factor for post-HSCT EBV infection via both univariate [hazard ratio (HR) = 4.17, 95%CI (1.52–11.43), p = 0.005] and multivariate analyses [HR = 4.65, 95%CI (1.66–13.0), p = 0.003]. Although the overall survival (OS) probability of the rituximab group was comparable to the without-rituximab group, a markedly improved OS of the rituximab group was found in the malignant disease subgroup (78.9% vs. 42.1%, p = 0.032). The outcomes of graft-versus-host disease, neutrophil and platelet engraftment, other viral infections, and the reconstitution of lymphocytes showed no significant differences between the two groups.
Conclusions
The administration of rituximab before HSCT may prevent EBV infection following HSCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Less Epstein–Barr virus infection occurred post-hematopoietic stem cell transplant in the setting of applying rituximab during the conditioning regimen. |
Among malignant disease patients, improved overall survival was indicated in the with-rituximab group. |
No difference in graft-versus-host disease and recovery of both neutrophil and platelet was found between the with- or without-rituximab groups. |
No delayed immune reconstitution was found in the applying rituximab group. |
Introduction
Hematopoietic stem cell transplant (HSCT) is a potent therapy for malignant and non-malignant hematologic diseases in children [1, 2]. Both T- and B-cell lymphocytes play a critical role in the different stages of HSCT, including the mechanism of graft-versus-host disease (GVHD), promotion of engraftment, response to infection, and eradication of minimal residual leukemia [3,4,5,6]. Here, we summarize the B-cell-relevant complications of HSCT. First, B-cell lymphocytes play a crucial role in the production of autoantibodies. Hence, B cells are commonly involved in the mechanisms of autoimmune hemolytic anemia (AIHA), immune thrombocytopenic purpura (ITP) in both pre- and post-HSCT periods [7,8,9], and donor-specific antibodies (DSAs), which may lead to graft failure following HSCT [10]. Second, B cells also mediate the activation of T cells and induce the release of cytokines via antigen presentation. This effect is one of the potential mechanisms of transplant-associated thrombotic microangiopathy (TA-TMA) [11]. Third, this effect might lead to the promotion of acute GVHD (aGVHD). For chronic GVHD (cGVHD), B-cell activating factor (BAFF) seems to be important in the reconstitution and survival of B cells following HSCT, promoting the production of autoreactive B cells and the inhibition of regulatory T cells [8]. And fourth, memory B cells are the main host of the Epstein–Barr virus (EBV) [12]. EBV infection mainly results in EBV viremia, EBV diseases, EBV-associated post-transplant lymphoproliferative disease (PTLD), and lymphoma after HSCT [13]. This information indicates the critical role of B cells in the entire procedure of HSCT; therefore, depleting B cells with rituximab, a monoclonal antibody of anti-CD20, may represent a potentially feasible strategy for minimizing post-HSCT complications. To date, the use of rituximab as part of a conditioning regimen has not yet been thoroughly investigated. Therefore, we conducted a retrospective nested case–control study to address the effect of the strategy.
Methods
Patients
All cases were enrolled from 232 children who underwent allogeneic HSCT in the Department of Pediatrics, Nanfang Hospital, Southern Medical University, China, from January 2019 to July 2021. Forty-eight cases who received rituximab as an agent in their conditioning regimen of HSCT were included in the with-rituximab group. For each with-rituximab case, one without-rituximab control case was randomly selected from the same cohort and was matched according to the following criteria: (1) age at the time of HSCT (± 5 years), (2) consistent diseases (± 1 case), (3) ratio of HLA-matched/mismatched types of HSCT (± 15%), (4) positive rate of direct antiglobulin test (Coomb’s test) (± 15%), and (5) positive rate of platelet antibody test (solid-phase assay) (± 15%). Patients who had severe organ disorders, severe anemia (< 40 g/L) and thrombocytopenia (< 5 × 109/L), or positive DSA prior to transplantation were excluded from this study. The median follow-up time was 3 years. All guardians of the subjects provided informed consent for their inclusion in the retrospective study. The study was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments, and the protocol was approved by the Ethics Committee of Nanfang Hospital, Southern Medical University (NFEC-2022–522).
Conditioning Regimens and the Administration of Rituximab
The conditioning regimens were depicted in previous studies [14,15,16,17]. Briefly, the myeloablative conditioning regimens consisted of busulfan/cyclophosphamide/fludarabine with or without thiotepa. Post-transplant cyclophosphamide (PTCY) was applied on day + 3 and day + 4 for haploidentical HSCT patients. Anti-thymocyte globulin (ATG) was administrated for HLA-matched HSCT and thalassemia major (TM) haploidentical HSCT patients. Non-relative CB was applied on day+6 as a complementary graft source in haploidentical HSCT patients. Rituximab was administrated at a dose of 375 mg/m2 per day on day–1 and day–8 within the conditioning regimen. The reduced-intensity conditioning (RIC) regimen comprised cyclophosphamide/fludarabine/thiotepa with PTCY.
Definitions
EBV infection included EBV DNAemia and end-organ disease. EBV DNAemia was measured in plasma using quantitative PCR (qPCR) (positive when > 100 IU/ml). EBV disease was defined as a positive EBV-encoded RNA (EBER) biopsy or positive EBV-DNA in bronchoalveolar lavage fluid or cerebral spinal fluid by qPCR with supporting clinical manifestation. Cytomegalovirus (CMV) infection was defined as the detection of > 500 IU/ml viral nucleic acid in plasma by qPCR [18]. PTLD and lymphoma were diagnosed using a biopsy in addition to positron emission tomography-computed tomography (PET-CT) [19]. Other viruses, including human herpesvirus 6, polyomaviruses, varicella-zoster virus, and herpes simplex virus 1 were detected via qPCR or metagenomic next-generation sequencing. Neutrophil recovery was defined as achieving an absolute neutrophil count of ≥ 0.5 × 109/L for 3 consecutive days; platelet recovery as platelets ≥ 20 × 109/L without transfusion for 7 days; and hemoglobin recovery as hemoglobin ≥ 70 g/L without transfusion for 7 days. Graft failure (GF) was indicated by an ANC of < 0.5 × 109/L by day+30 with associated pancytopenia [20]. Poor graft function (PGF) was defined as persistent neutropenia (ANC < 0.5 × 109/L), thrombocytopenia (platelets < 20 × 109/L), and/or hemoglobin < 70 g/L for at least 3 consecutive days by day+28 with transfusion requirement in the presence of complete donor chimerism without disease relapse [20, 21]. Secondary failure of platelet recovery (SFPR) was defined as a platelet level of < 20 × 109/L for 7 consecutive days or transfusion requirement after reaching a platelet level of ≥ 50 × 109/L without transfusion for 7 days post-HSCT [22]. Both acute and chronic GVHD were strictly diagnosed according to the published criteria [23, 24]. The diagnosis of TA-TMA referred to the criteria of Jodele et al. [25].
Statistic Analyses
Continuous variables were compared using t tests or the Kruskal–Wallis test. Categorical variables were compared via the χ2 or Fisher’s exact test. Hazard ratios (HR) for EBV infection post-HSCT were computed from univariate and multivariate Cox regression analyses. All the factors with p < 0.25 in the univariate analysis were included in the multivariate regression. Competing risk analysis was used to calculate the cumulative rates of GVHD and EBV infection. The probability of overall survival (OS) was determined using the Kaplan–Meier method, and the OS between the two groups was compared using the log-rank test. A p value of < 0.05 was considered statistically significant. All analyses were conducted in the R software (v.4.2.2, http://www.r-project.org).
Results
Characteristics and Overall Outcome of Patients
Forty-eight patients were enrolled in the rituximab group, and the same number of patients were placed in the without-rituximab group. The baseline statistical information for the groups is shown in Table 1. The mean age was 7 years old for the entire population. The most common disease was TM, accounting for 39.6%, followed by acute leukemia, including acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML), accounting for 22.9%. Other malignant diseases included juvenile myelomonocytic leukemia (JMML), chronic myeloid leukemia (CML), and hemophagocytic lymphohistiocytosis (HLH), while the non-malignant diseases comprised primary immunodeficiency disorders, such as Wiskott–Aldrich syndrome (WAS), chronic granulomatous disease (CGD), and severe combined immunodeficiency (SCID). Other malignancies accounted for 16.7%, while other non-malignancies accounted for 10.4%; severe aplastic anemia (SAA) accounted for 10.4%. More than half of the patients underwent HLA-mismatched HSCT. None of the major characteristics of HSCT were significantly different between the groups, apart from the pre-HSCT platelet antibodies (p = 0.047).
The primary outcomes of HSCT are summarized in Table 2. There was a statistically higher incidence of positive platelet antibodies following HSCT and a markedly lower incidence of EBV infection in the rituximab group than in the without-rituximab group (p = 0.021 and p = 0.014, respectively). The median times of neutrophil and platelet recovery were not statistically different between the rituximab group and the without-rituximab group (23 days and 30 days vs. 22 days and 17 days, p = 0.895 and p = 0.186, respectively). Furthermore, the incidences of GF, PGF, SFPR, and TA-TMA were quite similar between groups, showing no statistically significant differences.
The cumulative incidence rate (CIR) of grade III–IV aGVHD was 14.6% ± 5.1% in the rituximab group and 27.1% ± 6.4% in the without-rituximab group (p = 0.15) (Fig. S1A). Furthermore, according to Cox-model multivariate analysis (including all p < 0.05 factors from univariate analysis) of III–IV aGVHD, malignant disease (p = 0.001), mismatched donor (p = 0.022), PTCY + ATG prophylaxis (vs. PTCY alone, p = 0.002), TA-TMA (p < 0.001) were identified as risk factors (Supplementary Table S1). Regarding cGVHD, although the CIR of the rituximab group was lower than that of the without-rituximab group (38.6% ± 7.3% and 50.7% ± 7.9%, respectively), no statistically significant difference was found (p = 0.26) (Fig. S2A). In addition, no significant differences were found in aGVHD and cGVHD in the malignancy (Figs. S1B, S2B) and non-malignancy (Figs. S1C, S2C) subset analyses.
Overall Survival
The OS rate of the rituximab group was 83.3% ± 5.1% [95%CI (73.3%–94.6%)], while the OS rate was 68.7% ± 6.7% [95%CI (56.8–83.2%)] in the without-rituximab group (p = 0.1) (Fig. 1A). Furthermore, the OS of the rituximab group was significantly higher than in the without-rituximab group in the malignancy subset {78.9% ± 9.4% [95%CI (62.6–99.6%)] vs. 42.1% ± 1.1% [95%CI (24.9–71.3%)], respectively, p = 0.032} (Fig. 1B). However, the same OS was observed in both the with and without-rituximab groups in the non-malignancy subset {86.2% ± 6.4% [95%CI (74.5–99.7%)], p = 0.97} (Fig. 1C). In the univariate Cox regression analysis, non-malignancy was a protective factor (p = 0.006), while a higher number of MNC (p = 0.038), TA-TMA (p = 0.002), and grade III–IV aGVHD (p = 0.001) were risk factors. In the multivariate analysis, non-malignancy was still a protective factor (p = 0.023), and only TA-TMA was identified as an independent risk factor (p = 0.017) (Supplementary Table S2). Severe pneumonia, aGVHD, TA-TMA, and relapse were the main causes of death (Supplementary Table S3).
Overall survival probability with and without-rituximab for: A the whole population; B the malignant disease subset; and C the non-malignant disease subset. The red curve shows the without (w/o)-rituximab group accompanied by a red shadow indicating a 95%CI, while the blue curve and blue shadow show the with (w/)-rituximab group
EBV Infection
All donors and recipients tested negative for EBV DNA before HSCT. The CIR of EBV infection was dramatically lower in the rituximab group than in the without-rituximab group (12.2% ± 5.1% vs. 39.3% ± 8.1, p = 0.0026, respectively) (Fig. 2A). Similar results were found in the further subset analyses. In the context of the malignancy subset, the CIR of EBV infection was 13.1% ± 8.7% in the rituximab group and 53.7% ± 15.3% in the without-rituximab group, with a p value of 0.024 (Fig. 2B). Similarly, in the setting of non-malignant disease, the CIRs of EBV infection were 11.8% ± 6.4% and 32.7% ± 9.0% in the with and without-rituximab groups, respectively (p = 0.037) (Fig. 2C). There were no statistical differences in EBV infection between matched donors and mismatched/haploidentical donors (Fig. S3).
The features of EBV infection are depicted in Table 3. Only five patients suffered an EBV infection in the rituximab group, while 16 patients were infected in the without-rituximab group. Although the recurrence of EBV, organs involved by EBV, EBV-related PTLD, and EBV-related lymphoma were only found in the without-rituximab group, there were no statistically significant differences. In detail, among the six organ-involved patients, two were involved in the respiratory system, two in the gastrointestinal system, and two in the central nervous system. Of note, the median time of onset of EBV infection was later in the rituximab group than in the without-rituximab group, despite no statistically significant difference (430 days vs. 118 days, p = 0.057).
Univariate and multivariate analyses were then performed to determine the relevant factors (Table 4). The results showed that only the application of rituximab was identified as a significant protective factor in both univariate (p = 0.005) and multivariate analyses (p = 0.003).
Reconstitution of Lymphocytes
Although the reconstitution of B cells (CD3-CD19 +) was lower in the rituximab group, no statistically significant difference was found. The mean number of B cells (CD3-CD19 +) was 11.3/μl ± 25.1/μl in the rituximab group and 82.3/μl ± 155.2/μl in the without-rituximab group, with a p value of 0.101 at 3 months post-HSCT (Fig. 3A). In addition, 419.8/μl ± 404.6/μl B cells were found in the rituximab group at 12 months post-HSCT, while 395.7/μl ± 520.0/μl B cells were found in the without-rituximab group (p = 0.868) (Fig. 3B). There were no significant differences among the lymphocyte T cells (CD3 +), subtypes of T cells (CD3 + CD4 + CD8- and CD3 + CD4-CD8 +), and NK cells (CD3-CD16 + CD56 +), neither at 3 months nor 12 months post-HSCT (Fig. 3).
Discussion
The present nested case–control study compared the survival outcomes and major complications reported with or without rituximab in the conditioning regimen in a children’s cohort. To the best of our knowledge, our study is the first report of its kind in a pediatric cohort. Both multivariate analysis and the comparison of CIR showed that the occurrence of EBV infection was significantly lower in the rituximab group than in the without-rituximab group, despite having comparable OS probability. The subgroup of patients with malignant diseases had a higher OS probability in the rituximab group than in the without-rituximab group. Thus, our results indicate the possibility of exploring the administration of rituximab in patients with malignant diseases and a high risk of EBV infection.
Overall, the two groups were comparable according to their age, sex, diseases, direct antiglobulin test, platelet antibody test, HLA disparity and donor type, cord blood engraftment, prophylaxis of GVHD, conditioning regimen, and number of transfused stem cells (Table 1). Only the platelet antibody test was statistically different between the two groups, although all patients with platelet antibodies were enrolled in the without-rituximab group. The reason for this was that, originally, rituximab was designed for patients with autoantibodies, indicated by a positive direct antiglobulin test and platelet antibody test. As a result, there was no significant difference in the post-HSCT direct antiglobulin test between the groups, while a higher rate of positive platelet antibody tests post-HSCT was observed with rituximab (Table 2). According to our literature review, the incidence of post-HSCT AIHA is about 5%, whereas it can reach up to 20% in children with non-malignant diseases [7]. Moreover, the direct antiglobulin test may be positive in the absence of hemolysis resulting from other autoimmune conditions, intravenous immunoglobulin (IVIG), ATG, and daratumumab [26]. On the other hand, platelet antibodies were found to be one of the main causes of thrombocytopenia following HSCT [27]. Rituximab was recommended as an effective agent for the treatment of post-HSCT AIHA and ITP [28]. Both post-HSCT AIHA and ITP may result in poor survival outcomes [7, 27, 29]. The results of our study indicate that the application of rituximab in the conditioning regimen may not help with decreasing the occurrence of both hemoglobin and platelet antibodies. Furthermore, the engraftment of neutrophils and platelets and the occurrence of TA-TMA, PGF, and SFPR were quite comparable between the two groups in the present study (Table 2). These results are consistent with a recent study that also focused on the administration of rituximab before HSCT [30, 31]. Since rituximab has been a recommended treatment for DSA in several studies [32,33,34,35], the DSA-positive patients were excluded from the present study.
Several studies have demonstrated that B cells contribute to acute GVHD, which may be abrogated by rituximab as part of a myeloablative or nonmyeloablative conditioning regimen in malignant diseases [30]. Patel et al. [31] stated that rituximab-based conditioning regimens did not reduce the incidence of aGVHD. Additionally, according to an animal study, host B cells may confer a protective effect on the initiation of aGVHD via the secretion of IL-10 [39]. Importantly, rituximab administered before transplantation appears to be safe [30, 40]. In our study, regarding aGVHD and cGVHD, there were no marked differences with or without the administration of rituximab before HSCT (Figs. S1, S2). Apart from lymphoma patients, incorporating rituximab into the conditioning regimen in HSCT has not been well investigated with respect to survival outcomes. According to a recent retrospective study, no differences in prognosis were observed between rituximab and non-rituximab groups, including non-relapse mortality, leukemia-free survival, and OS in adult patients undergoing allo-HSCT [30]. These results were similar to our study except for the malignant disease subgroup (Fig. 1), although there were the same number of acute leukemia and other malignant diseases between groups. Nonetheless, it may not be appropriate to draw conclusions due to the relatively small sample size used in this study.
Of note, we consistently found that rituximab administrated in the conditioning regimen prevented the incidence of EBV infection (Fig. 2). Although the serostatus of EBV was not available in our center, the seroprevalence of EBV stabilizes at over 90% after age 8 years in China [41]. Therefore, most EBV infections in the study were considered as reactivation rather than de novo infections. Similarly, two recent studies demonstrated that rituximab applied before HSCT in adult patients led to the elimination of EBV reactivation and EBV-related PTLD [30, 31]. The underlying mechanisms remain largely unclear. Typically, EBV can directly drive the proliferation of B cells, which are the primary targets and hosts of EBV [42]. Progressive EBV-associated PTLD or lymphoma are dismal outcomes of EBV infection [43, 44]. Adequate evidence has been found to support rituximab as a potent agent for the treatment of post-HSCT EBV infection in both children and adults [45,46,47]. Critically, it was a worthwhile strategy that closely monitored EBV reactivation and preemptive therapy using rituximab, especially for the patients at high risk of EBV-lymphoproliferative disease [48, 49]. Furthermore, serial studies have found that the main risk factors for EBV infection include high cumulative levels of immunosuppression, older age at transplantation, profound T-cell depletion, and the administration of ATG or alemtuzumab [13, 43, 44, 50]. Interestingly, PTCY, a strategy for T-cell depletion, was not used in the treatment of EBV infection, especially PTLD [51, 52]. In another recent study, no EBV reactivation was found in PTCY-based haploidentical HSCT in children with TM [53]. The potential reasons for this include the destruction of EBV-infected B cells, the allowance of a considerable dose of stem cells accompanying memory T cells, and rapid T-cell immune reconstitution [54, 55]. Regarding GVHD prophylaxis, about 25% of patients underwent ATG alone while about 40% of patients experienced ATG plus PTCY, and therefore the hazardous effect of ATG may be compensated by the protective effect of PTCY in the setting of combination in the current study (Tables 1, 4). Moreover, a reduction in immunosuppression, rituximab, or cellular immunotherapy are well-established methods in the management of EBV infection [13]. All patients who underwent EBV infection in the current study were treated as above. Although the post-HSCT administration of rituximab has been reported to be relatively safe, Launspach et al. demonstrated that the post-HSCT administration of rituximab caused prolonged B-cell impairment and increased the risk of infections in a children’s cohort [56]. Unlike applying rituximab in the post-HSCT period [6, 56], we found that using rituximab prior to HSCT had little effect on delayed B cell immune reconstitution (Fig. 3). This still requires further prospective studies for verification.
This study has certain limitations, including the general weaknesses of retrospective studies, the relatively small scale of the population, and the various conditioning regimens. Further prospective large cohort studies are required to confirm the results presented here.
Conclusions
We have evaluated the clinical outcomes in the setting of applying rituximab in the conditioning regimen. Crucially, the incidence of EBV reactivation was effectively decreased in the with-rituximab group. Moreover, the with-rituximab regimen may improve OS in malignant diseases. However, there was no significant effect on the prophylaxis of GVHD and the inhibition of the production of autoimmune antibodies, along with no delayed immune reconstitution.
References
Algeri M, Merli P, Locatelli F, Pagliara D. The role of allogeneic hematopoietic stem cell transplantation in pediatric leukemia. J Clin Med. 2021;10(17):3790.
Passweg JR, Baldomero H, Bader P, et al. Use of haploidentical stem cell transplantation continues to increase: the 2015 European Society for Blood and Marrow Transplant activity survey report. Bone Marrow Transplant. 2017;52(6):811–7.
Divito SJ, Aasebø AT, Matos TR, et al. Peripheral host T cells survive hematopoietic stem cell transplantation and promote graft-versus-host disease. J Clin Investig. 2020;130(9):4624–36.
Ye W, Kong X, Zhang W, Weng Z, Wu X. The roles of γδ T cells in hematopoietic stem cell transplantation. Cell Transplant. 2020;29:963689720966980.
Crooks GM, Weinberg K, Mackall C. Immune reconstitution: from stem cells to lymphocytes. Biol Blood Marrow Transplant. 2006;12(1 Suppl 1):42–6.
van der Maas NG, Berghuis D, van der Burg M, Lankester AC. B cell reconstitution and influencing factors after hematopoietic stem cell transplantation in children. Front Immunol. 2019;10:782.
Gabelli M, Ademokun C, Cooper N, Amrolia PI. Pathogenesis, risk factors and therapeutic options for autoimmune haemolytic anaemia in the post-transplant setting. Br J Haematol. 2022;196(1):45–62.
Ratanatharathorn V, Pavletic S, Uberti JP. Clinical applications of rituximab in allogeneic stem cell transplantation: anti-tumor and immunomodulatory effects. Cancer Treat Rev. 2009;35(8):653–61.
Cooper N, Ghanima W. Immune thrombocytopenia. N Engl J Med. 2019;381(10):945–55.
Chang Y-J, Zhao X-Y, Xu L-P, et al. Donor-specific anti-human leukocyte antigen antibodies were associated with primary graft failure after unmanipulated haploidentical blood and marrow transplantation: a prospective study with randomly assigned training and validation sets. J Hematol Oncol. 2015;8:84.
Kim SS, Patel M, Yum K, Keyzner A. Hematopoietic stem cell transplant-associated thrombotic microangiopathy: review of pharmacologic treatment options. Transfusion. 2015;55(2):452–8.
Hatton OL, Harris-Arnold A, Schaffert S, Krams SM, Martinez OM. The interplay between Epstein-Barr virus and B lymphocytes: implications for infection, immunity, and disease. Immunol Res. 2014;58(2–3):268–76.
Al Hamed R, Bazarbachi AH, Mohty M. Epstein-Barr virus-related post-transplant lymphoproliferative disease (EBV-PTLD) in the setting of allogeneic stem cell transplantation: a comprehensive review from pathogenesis to forthcoming treatment modalities. Bone Marrow Transplant. 2020;55(1):25–39.
Li C, Wu X, Feng X, et al. A novel conditioning regimen improves outcomes in beta-thalassemia major patients using unrelated donor peripheral blood stem cell transplantation. Blood. 2012;120(19):3875–81.
Xiao Y, Liu S, Li C, et al. Post Transplantation fludarabine and cyclophosphamide selected and promoted low dose of unrelated UCB implanation in combined transplantation of haploid and UCB stem cells in childhood leukemia: 40 cases report in double center. Blood. 2021;138(Supplement 1):2875–2875.
Ruan Y, Kim HN, Ogana HA, et al. In vitro and in vivo effects of AVA4746, a novel competitive antagonist of the ligand binding of VLA-4, in B-cell acute lymphoblastic leukemia. Exp Ther Med. 2022;23(1):47.
Li C, Liu S, He Y, et al. Complementary transplantation improved results of both peripheral blood stem cells and unrelated cord blood transplants in thalassemia: a multi-center study from China. Blood. 2019;134(Supplement_1):4617–4617.
Ruan Y, Luo T, Liu Q, et al. Features of cytomegalovirus infection and evaluation of cytomegalovirus-specific T cells therapy in children’s patients following allogeneic hematopoietic stem cell transplantation: a retrospective single-center study. Front Cell Infect Microbiol. 2022;12:1027341.
Green M, Michaels MG. Epstein-Barr virus infection and posttransplant lymphoproliferative disorder. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2013;13(Suppl):3.
Kharfan-Dabaja MA, Kumar A, Ayala E, et al. Standardizing definitions of hematopoietic recovery, graft rejection, graft failure, poor graft function, and donor chimerism in allogeneic hematopoietic cell transplantation: a report on behalf of the american society for transplantation and cellular therapy. Transplant Cell Ther. 2021;27(8):642–9.
Kong Y. Poor graft function after allogeneic hematopoietic stem cell transplantation-an old complication with new insights(). Semin Hematol. 2019;56(3):215–20.
Bruno B, Gooley T, Sullivan KM, et al. Secondary failure of platelet recovery after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2001;7(3):154–62.
Dignan FL, Clark A, Amrolia P, et al. Diagnosis and management of acute graft-versus-host disease. Br J Haematol. 2012;158(1):30–45.
Filipovich AH, Weisdorf D, Pavletic S, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11(12):945–56.
Jodele S, Davies SM, Lane A, et al. Diagnostic and risk criteria for HSCT-associated thrombotic microangiopathy: a study in children and young adults. Blood. 2014;124(4):645–53.
Jäger U, Barcellini W, Broome CM, et al. Diagnosis and treatment of autoimmune hemolytic anemia in adults: Recommendations from the First International Consensus Meeting. Blood Rev. 2020;41: 100648.
Bento L, Canaro M, Bastida JM, Sampol A. Thrombocytopenia and therapeutic strategies after allogeneic hematopoietic stem cell transplantation. J Clin Med. 2022;11(5):1364.
Bhatt V, Shune L, Lauer E, et al. Autoimmune hemolysis and immune thrombocytopenic purpura after cord blood transplantation may be life-threatening and warrants early therapy with rituximab. Bone Marrow Transplant. 2016;51(12):1579–83.
Kuzmina Z, Eder S, Böhm A, et al. Significantly worse survival of patients with NIH-defined chronic graft-versus-host disease and thrombocytopenia or progressive onset type: results of a prospective study. Leukemia. 2012;26(4):746–56.
Wei X, Xie Y, Jiang R, et al. The impact of Rituximab administered before transplantation in patients undergoing allogeneic hematopoietic stem cell transplantation: a real-world study. Front Immunol. 2022;13: 967026.
Patel C, Pasciolla M, Abramova R, et al. Pre-Hematopoietic stem cell transplantation rituximab for epstein-barr virus and post-lymphoproliferative disorder prophylaxis in alemtuzumab recipients. Transplant Cell Therapy. 2022.
Krummey SM, Gareau AJ. Donor specific HLA antibody in hematopoietic stem cell transplantation: Implications for donor selection. Front Immunol. 2022;13: 916200.
Ciurea SO, Al Malki MM, Kongtim P, et al. Treatment of allosensitized patients receiving allogeneic transplantation. Blood Adv. 2021;5(20):4031–43.
Bailén R, Vicario JL, Solán L, et al. Management of donor-specific antibodies in haploidentical transplant: multicenter experience from the madrid group of hematopoietic transplant. Front Immunol. 2021;12: 674658.
Anurathapan U, Hongeng S, Pakakasama S, et al. Hematopoietic stem cell transplantation for severe thalassemia patients from haploidentical donors using a novel conditioning regimen. Biol Blood Marrow Transplant. 2020;26(6):1106–12.
Christopeit M, Schütte V, Theurich S, Weber T, Grothe W, Behre G. Rituximab reduces the incidence of acute graft-versus-host disease. Blood. 2009;113(13):3130–1.
Kebriaei P, Saliba RM, Ma C, et al. Allogeneic hematopoietic stem cell transplantation after rituximab-containing myeloablative preparative regimen for acute lymphoblastic leukemia. Bone Marrow Transplant. 2006;38(3):203–9.
Marini BL, Markstrom D, Frame D. Risk of graft-versus-host disease with rituximab-containing conditioning regimens in allogeneic hematopoietic stem cell transplant. J Oncol Pharm Pract. 2017;23(4):255–63.
Rowe V, Banovic T, MacDonald KP, et al. Host B cells produce IL-10 following TBI and attenuate acute GVHD after allogeneic bone marrow transplantation. Blood. 2006;108(7):2485–92.
Kharfan-Dabaja MA, Tate C, Perkins J, et al. Administration of rituximab is feasible and does not affect engraftment of allograft recipients with advanced CD20+ malignancies. Blood. 2007;110(11):3016–3016.
Xiong G, Zhang B, Huang M-y, et al. Epstein-Barr virus (EBV) infection in Chinese children: a retrospective study of age-specific prevalence. PLoS ONE. 2014;9(6):e99857.
Dolcetti R. B lymphocytes and Epstein-Barr virus: the lesson of post-transplant lymphoproliferative disorders. Autoimmunity Rev. 2007;7(2):96–101.
Lindsay J, Yong MK, Greenwood M, et al. Epstein-Barr virus related post-transplant lymphoproliferative disorder prevention strategies in allogeneic hematopoietic stem cell transplantation. Rev Med Virol. 2020;30(4): e2108.
Styczynski J, Gil L, Tridello G, et al. Response to rituximab-based therapy and risk factor analysis in Epstein Barr Virus-related lymphoproliferative disorder after hematopoietic stem cell transplant in children and adults: a study from the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Clin Infect Dis. 2013;57(6):794–802.
Liu L, Liu Q, Feng S. Management of Epstein-Barr virus-related post-transplant lymphoproliferative disorder after allogeneic hematopoietic stem cell transplantation. Therap Adv Hematol. 2020;11:2040620720910964.
Chiereghin A, Prete A, Belotti T, et al. Prospective Epstein-Barr virus-related post-transplant lymphoproliferative disorder prevention program in pediatric allogeneic hematopoietic stem cell transplant: virological monitoring and first-line treatment. Transplant Infect Dis. 2016;18(1):44–54.
Styczynski J, van der Velden W, Fox CP, et al. Management of Epstein-Barr Virus infections and post-transplant lymphoproliferative disorders in patients after allogeneic hematopoietic stem cell transplantation: Sixth European Conference on Infections in Leukemia (ECIL-6) guidelines. Haematologica. 2016;101(7):803–11.
van Esser JWJ, Niesters HGM, van der Holt B, et al. Prevention of Epstein-Barr virus-lymphoproliferative disease by molecular monitoring and preemptive rituximab in high-risk patients after allogeneic stem cell transplantation. Blood. 2002;99(12):4364–9.
Stocker N, Labopin M, Boussen I, et al. Pre-emptive rituximab treatment for Epstein-Barr virus reactivation after allogeneic hematopoietic stem cell transplantation is a worthwhile strategy in high-risk recipients: a comparative study for immune recovery and clinical outcomes. Bone Marrow Transplant. 2020;55(3):586–94.
Kharfan-Dabaja MA, Bazarbachi A. Emerging role of CD20 blockade in allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;16(10):1347–54.
Kanakry JA, Kasamon YL, Bolaños-Meade J, et al. Absence of post-transplantation lymphoproliferative disorder after allogeneic blood or marrow transplantation using post-transplantation cyclophosphamide as graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant. 2013;19(10):1514–7.
Mohyuddin GR, Roller J, Shune L, et al. Epstein-Barr viremia and post-transplant lymphoproliferative disorders in patients undergoing haploidentical stem cell transplantation with post-transplant cyclophosphamide. Hematol Oncol Stem Cell Ther. 2019;12(3):171–3.
Vellaichamy Swaminathan V, Ravichandran N, Ramanan KM, et al. Augmented immunosuppression and PTCY-based haploidentical hematopoietic stem cell transplantation for thalassemia major. Pediatr Transplant. 2021;25(2): e13893.
Retière C, Willem C, Guillaume T, et al. Impact on early outcomes and immune reconstitution of high-dose post-transplant cyclophosphamide vs anti-thymocyte globulin after reduced intensity conditioning peripheral blood stem cell allogeneic transplantation. Oncotarget. 2018;9(14):11451–64.
Fujimoto A, Suzuki R. Epstein-Barr virus-associated post-transplant lymphoproliferative disorders after hematopoietic stem cell transplantation: pathogenesis, risk factors and clinical outcomes. Cancers. 2020;12(2):328.
Launspach M, Temel D, Ohlendorf E, et al. Rituximab therapy after pediatric hematopoietic stem cell transplantation can cause prolonged B cell impairment and increases the risk for infections—a retrospective matched cohort study. Haematologica. 2022;108:267–72.
Acknowledgements
Funding
This research was funded by the Guangdong Basic and Applied Basic Research Foundation, Grant number 2022A1515010012 (Yongsheng Ruan), Grant number 2022A1515220153 (Xuedong Wu), and the Clinical Research Program of Nanfang Hospital, Southern Medical University, grant number 2021CR005 (Xiaoqin Feng). Xuedong Wu and Xiaoqin Feng are funding the journal’s Rapid Service fee.
Author Contributions
Yongsheng Ruan, Xuedong Wu, and Xiaoqin Feng contributed to the conception and design; Yongsheng Ruan, Xuedong Wu, and Xiaoqin Feng contributed to administrative support; Yongsheng Ruan wrote the manuscript; Yongsheng Ruan, Libai Chen, Tingting Luo, Danfeng Xie, Wei Cao, Xuan Liu, Qiujun Liu, Yuhua Xiao, Cuiling Wu, Jianyun Wen, Juan Li, and Jiangnan Meng contributed to the provision of study materials or patients; Yongsheng Ruan, Libai Chen, and Tingting Luo collected and assembled data; Yongsheng Ruan, Libai Chen, and Tingting Luo interpreted and analyzed data; and all authors contributed to manuscript writing, confirmed the final version of the manuscript, approved it for publication, and completed the STROBE statement checklist.
Disclosures
All named authors confirm that they have no conflicts of interest to declare.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments, and the protocol was approved by the Ethics Committee of Nanfang Hospital, Southern Medical University (NFEC-2022–522).
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ruan, Y., Chen, L., Luo, T. et al. Applying Rituximab During the Conditioning Regimen Prevents Epstein–Barr Virus Infection Following Allogeneic Hematopoietic Stem Cell Transplant in a Children’s Cohort: A Retrospective Case–Control Study. Infect Dis Ther 12, 2071–2086 (2023). https://doi.org/10.1007/s40121-023-00841-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00841-x