Abstract
Introduction
Meropenem is a carbapenem antibiotic, which has demonstrated excellent antimicrobial activity against gram-negative clinical isolates. It is also commonly used in critically ill patients. This study aimed to determine the pharmacokinetics/pharmacodynamics of meropenem in critically ill patients and whether prolonged injection duration is really beneficial to meropenem therapy.
Methods
We included 209 samples in 64 patients in this prospective study. PPK analysis and Monte Carlo dosing simulations were developed using Phoenix.
Results
A two-compartment model described the data adequately. Clearance (CL), volume (V), clearance of peripheral compartment (CL2), and volume of peripheral compartment (V2) were 6.15 l/h, 2.83 l/h, 17.40 l, and 17.48 l, respectively. Creatinine clearance and uric acid were significant covariates. Patients with creatinine clearance ≤ 60 ml/min and uric acid > 400 μmol/l could achieve the target > 90% under the minimum inhibitory concentration (MIC) of 8 mg/l, even with the administration dose of 500 mg/8 h with a 2-h infusion. Prolonging the infusion time significantly improved the therapeutic effect when MIC < 4. However, for the pharmacodynamic (PD) effects of 100% fT > MIC and 100% fT > 4 MIC, no significant statistical difference was observed in critically ill patients.
Conclusions
Critically ill patients with lower creatinine clearance and higher uric acid levels tended to need a lower dosage of meropenem. Prolonged infusion time was not always beneficial for those who needed a higher therapeutic target (100% fT > MIC, 100% fT > 4 MIC) or with MIC > 4 mg/l. Increasing dose or alternative therapeutic strategies may be required for critically ill patients with drug-resistant or severe infections. The study is of great significance to guide the rational use of meropenem in critically ill patients.
Trial Registration
The trial was registered in the China Clinical Trial (ChiCTR1900020672). Registered on 12 January 2019.
Plain Language Summary
Meropenem is commonly used empirically or targeted in critically ill patients for bacterial infection. Many studies have reported that prolonged infusion time can improve the efficacy of meropenem therapy. However, we are skeptical about that. Meanwhile, prolonged injections can sometimes cause mobility problems for patients. A quantitative method is used to evaluate meropenem use. It is called the population pharmacokinetic model or pharmacodynamic study. Using this method, we found two significant influencing factors of meropenem metabolism: creatinine clearance and uric acid level. It is likely that patients with a lower level of creatinine clearance and a high uric acid level tend to require lower dosages of meropenem. As for the effect of infusion time, Monte Carlo simulation was used, which can do 3000 simulations on an individual. The result was complex. We found infusion time was beneficial only when bacteria were sensitive to meropenem. The evidence suggests that prolonged injection duration sometimes does not significantly improve the outcome of antimicrobial therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Meropenem is commonly used empirically or targeted in critically ill patients. However, pathophysiological factors of this cohort are different from those of healthy people. We are skeptical about the effect of prolonged injection duration on therapeutic efficacy of meropenem. |
The core problem was to establish a meropenem pharmacokinetic model in critically ill patients and analyze the effect of infusion time on the probability of target attainment (PTA) under different therapeutic effects and different minimum inhibitory concentration (MIC) values. |
What was learned from the study? |
Patients with a lower level of creatinine clearance and a high uric acid level tend to require lower dosages. |
Prolonged infusion time is beneficial only when MIC ≤ 4 mg/l, while for those patients with drug-resistant or severe infections (MIC > 4 mg/l) who need a higher therapeutic target, prolonged infusion time is not beneficial at all. |
Introduction
Severe pneumonia as well as the epidemiology of carbapenem-resistant Enterobacterales (CRE) is a risk factor for in-hospital patients, with high morbidity and mortality rates [1,2,3,4,5]. In recent years, carbapenems have been widely used in patients and are considered the last line of defense in treating gram-negative bacterial infections [6,7,8]. Meropenem is a second-generation carbapenem antibiotic. Unlike the first generation, the 1-β methyl modification of the chemical structure enhances the stability of the drug to renal dehydropeptidase I [9, 10]. It is also a broad-spectrum antimicrobial used empirically or as directed therapy in critically ill patients. Meropenem shows time-dependent antibacterial activity and is characterized by linear pharmacokinetics in vivo; higher doses correspond to higher peak and trough concentrations [11, 12]. In healthy volunteers, the elimination half-life of meropenem in plasma was about 1 h [13, 14]. Severe pathophysiological changes in critical illness can lead to dramatically altered antimicrobial pharmacokinetics (PK). In populations such as children, the elderly, obese patients, those with severe burns, those treated with continuous renal replacement therapy, and patients on extracorporeal membrane oxygenation, meropenem shows significant individual differences in plasma concentrations and pharmacokinetic parameters [15,16,17,18,19]. These effects are related to the time that the free concentration is maintained above the minimum inhibitory concentration (MIC) (fT > MIC), at least 40% [20]. Several clinical studies suggest that 100% fT > MIC in plasma is associated with better therapeutic effects [21,22,23,24,25]. Additionally, it has been widely reported that prolonged injection duration can improve the therapeutic effect of meropenem [26, 27]. Nevertheless, it remains unclear whether standard meropenem dosing regimens achieve this target in critically ill patients.
In addition, the epidemiology of carbapenem-resistant Enterobacterales (CRE) is increasing worldwide [28]. The mechanisms of carbapenem resistance are heterogeneous, including carbapenemase production, efflux pump overexpression and specific porin blocking at the bacterial cell membrane to limit permeability of the antibiotics [5, 29, 30]. The most common is carbapenemase enzyme production, resulting in limited therapy options. Therefore, knowledge of an accurate minimum inhibitory concentration (MIC) value, coupled with therapeutic drug monitoring (TDM)-based PK/PD optimization of meropenm exposure, especially in critically ill patients, is necessary.
Methods
Study Design and Patients
This prospective study was conducted at the Department of Respiratory and Intensive Care Unit, the Second Xiang-ya Hospital of Central South University, between January and December 2019. Ethics approval was obtained from the local ethics committee (The Second Xiang-ya Hospital of Central South University; approval no. 2019-005). It was registered in China Clinical Trials (no. ChiCTR1900020672). Written informed consent was obtained from either the patient or their appointed legal guardian. The study was fully compliant with the Declaration of Helsinki.
Patients treated with meropenem and admitted to the Department of Respiratory and Critical Care Medicine were eligible. Written informed consent was obtained from all participants. Inclusion criteria were as follows: (1) patients admitted to the Department of Respiratory and Critical Care Medicine in our hospital with a diagnosis of pneumonia; (2) use of meropenem empirically or therapeutically; (3) time of continuous medication > 2 days; (4) at least one steady-state plasma concentration could be obtained; (5) age > 18 years, and (6) gram-negative bacteria were isolated from specimen culture if possible. Exclusion criteria were as follows: (1) pregnancy and lactation; (2) allergy to carbapenems; (3) concomitant uses of sodium valproate; (4) incomplete dosing information or clinical data. The data were prospectively collected.
Initial courses of meropenem commenced at a conventional intravenous infusion dose of 1 g every 8 h, while if the patients had poor renal function (the common criterion is creatinine clearance < 51 ml/min) the clinicians may give a lower dosage of 0.5 g every 8 h. After ≥ 48 h of therapy, the dose could be adjusted based on the concentration result. The patients could choose whether the duration of injection was 0.5 h, 1 h, or 2 h. All infusion durations were > 30 min. From the electronic medical record information system, we recorded demographic information, clinical data and laboratory test results using a standardized data collection form on the day of serum sampling. The endogenous creatinine clearance rate was calculated using the Cockcroft-Gault formula [31, 32].
According to the MICs of bacteria to meropenem in our hospital, various meropenem MICs (1, 2, 4, and 8 mg/l) were evaluated using the following PK/PD targets: 40% fT \(>\) MIC, 100% fT \(>\) MIC, and 100% fT \(>\) 4 MIC [24, 25]. The MICs were tested by automatic microbial identification and a drug sensitivity analysis system directed by the guideline of the Clinical and Laboratory Standards Institute.
Sampling and Assays
Blood samples (about 3 ml) were collected at the following times: pre-dose and 0.5 h, 1 h, 2 h, 4 h, 6 h, 8 h, and 12 h after infusion (ensuring that at least 2 samples could be collected from every patient). Meropenem serum concentrations were measured using automatic two-dimensional high-performance liquid chromatography (Demeter Instrument Co., Ltd., Hunan, China). The first-dimensional chromatographic column was an Aston SNCB (4.6 × 50 mm, 5 µm), and the second-dimensional chromatographic column was an Aston SBN (4.6 × 200 mm, 5 µm) [33, 34]. There was an excellent linear relationship between peak area and the concentration range of 0.78 to 58.52 μg/ml. The lower limits of detection and quantification were 0.04 μg/ml and 0.1 μg/ml, respectively. The intra-day precision, inter-day precision, and accuracy were 1.21–2.58%, 0.83–1.80%, and 100.51–101.69%, respectively. The extraction recoveries of the high, medium, and low concentrations were 99.47%, 97.77%, and 97.23%, respectively.
Pharmacokinetic Study
The PK model of meropenem in critically ill patients was developed using Phoenix NLME software (version 8.1, Pharsight, A Certara Company, USA). Serum meropenem concentrations were fit to a two-compartment model using the logarithmic additive residual. The first-order conditional estimation-extended least-squares method was used to estimate model parameters. The goodness of fit and visual predictive check (VPC) were used to evaluate the model. Objective function values (OFV) were used to compare the model fit. Covariates were retained in the model if the additional covariates were significant at a P value of 0.01 (△OFV > 6.635). VPC was used to evaluate the goodness of fit [13, 35,36,37,38].
Probability of Target Attainment
We used Monte Carlo simulations (n = 3000) to determine the probability of target attainment (PTA) with different significant covariates. Meropenem doses of 500 mg, 1000 mg, and 2000 mg given intravenously every 8 h (q8h) with durations of 0.5 h, 2 h, and 4 h were simulated at different levels of selected covariates. The PTA was calculated after 3 days of therapy. The MIC at which PTA was equal to 90% was derived to enable a numeric comparison among the regimens [17, 19, 39]. MIC values were selected for the most common value of pathogenic bacteria such as Enterobacter cloacae, Pseudomonas aeruginosa, Klebsiella pneumoniae, and Acinetobacter baumannii obtained from our hospital. PTA was calculated for single doses of 500 mg, 1000 mg, and 2000 mg. The therapeutic target adopted the effect of 40% fT > MIC, 100% fT > MIC, and 100% fT > 4 MIC [20, 24, 25].
Statistical Analysis
Continuous variables are expressed as means (standard deviations [SD]) or medians (interquartile ranges) depending on the normality of distribution. Enumeration data were expressed as absolute numbers and relative frequencies. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to test for normality. A two-sided P value of < 0.05 was considered statistically significant. One-way analysis of variance was used to test the differences in selected significant covariate groups. All analyses were performed using IBM SPSS Statistics version 25 (IBM, New York, NY). Figures were generated using Phoenix NLME and Graphpad Prism version 8 (San Diego, CA, USA).
Results
Demographic and Clinical Data of Study Patients
Sixty-four patients were enrolled in this prospective study. A total of 210 meropenem plasma samples were obtained; 73.43% of the patients were male. The average weight and age of the study cohort were 62.5 kg and 63.5 years, respectively. The mean Acute Physiology and Chronic Health Evaluation (APACHE) score was 17.2. More details about the demographic and clinical characteristics are shown in Table 1.
Meropenem sensitivity test was performed in 71.86% of the patients, most of whom had more than one kind of gram-negative bacterium. A total of 80 meropenem MIC values were collected, 53.75% of which were > 8 mg/l. The detection rate of A. baumannii was the highest (21 [26.3%]). Notably, the MIC values for this pathogen were > 8 mg/l, suggesting resistance to meropenem. Notably, 45 (56.3%) of the gram-negative bacteria were multi-drug resistant. Microbiological data and distributions of MICs are displayed in Table 2.
Pharmacokinetic Model
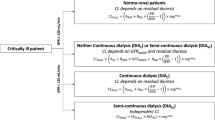
A total of 210 meropenem plasma concentrations were included in the population analysis. The meropenem PPK was best described by a two-compartment linear model with first-order elimination. A stepwise method was used to determine all the covariates that might affect the pharmacokinetic parameters. For covariates, we selected gender, age, body weight, APACHE score, Cockcroft-Gault CLCR (CG-CLCR), white blood cells, red blood cells, platelets, hemoglobin, alanine aminotransferase, aminotransferase, albumin, urea nitrogen, and uric acid. Inflammatory indicators were also included in the covariate selection. Despite various covariates having relationships with the estimated clearance, they were not included in the final model. To avoid the effects of collinearity and confounding factors between covariates, the correlation between covariates was considered. Uric acid was finally found to be closely connected to meropenem V2 and CL. CG-CLCR was closely connected to CL. These two factors for meropenem V2 and CL improved the model fit best. When they were added to the model, the log-likelihood value from the previous model was significantly improved (P < 0.01). The covariate model was as follows:
In these equations, CG-CLCR was calculated using the Cockcroft-Gault equation; tvCL is the typical value of meropenem clearance, CL is the population parameter of meropenem clearance, tvV is the typical value of volume in the central compartment, \(V_{2}\) is the population parameter estimate for the volume of the peripheral compartment, and \({\upeta }\) CL,\({\upeta }\) V, \({\upeta }CL_{2}\), and \({\upeta }V_{2}\) are the inter-individual random effects of the parameter.
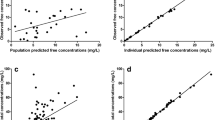
Individual and population predicted serum meropenem concentrations vs. observed concentrations are shown in Fig. 1. The population predicted concentrations strongly deviated from the observed meropenem concentrations in the base model but they fit well with the Y = X axis in the final model. The distribution of conditional weighted residuals is presented in Fig. 2. The values of conditional weighted residuals were between − 2 and 2. Both plots indicated the fitting advantages of the final model. The final covariate model was used for Monte Carlo dosing simulations.
Scatter plots of conditional weighted residuals in the basic model and final model. The distribution of conditional weighted residuals for the basic model (a and c) and final model (b and d). The conditional weighted residuals versus population predicted concentrations (a and b) and time (c and d). Both the blue and orange lines are conditional weighted residual trend lines reflecting the trend of the residual distribution, where the blue line is obtained by locally weighted regression (LOESS), and the orange line is obtained by taking the absolute value and its mirror image
Simulations
Monte Carlo simulations and meropenem probabilities of target attainment for various CG-CLCR values, uric acid values, dosage regimens, and MICs with a duration of 0.5 h, 2 h, and 4 h are presented in additional files. Details are shown in Additional file 1–3. MIC values listed in the tables were chosen according to the sensitivity of pathogenic bacteria to meropenem at our hospital. We found that at the lowest dosage (500 mg/q8h), patients with uric acid levels of > 400 mol\(\mu\)/l can achieve an optimal PTA (\(\ge 90\% )\) of 40% fT > MIC for isolates with MICs of 8 mg/l with a duration of 4 h. However, those with uric acid levels > 40 mol\(\mu\)/l and CG-CLCR of 120 ml/min could not achieve optimal PTA (\(\ge 90\% )\) of 40% fT > MIC for isolates with MICs of 1 mg/l, even with the highest dosage of 2000 mg/8 h with a duration of 0.5 h. Moreover, the numbers of targeted PTA \((\ge 90\%)\) for the three infusion time groups were 55.56%, 62.96%, and 77.78%, respectively. These findings suggest that to achieve an optimal PTA, a prolonged infusion time, higher dose, or alternative administration protocol is needed for this cohort. Notably, patients with uric acid levels of 800 μmol/l and CG-CLCR of 30 ml/min can achieve optimal PTA (\(\ge 90\%)\) for all targeted therapeutic effects, including 100% fT > 4 MIC for isolates with MICs of 8 mg/l using a dosage of 2000 mg/8 h with infusion durations of 2 h and 4 h. The low uric acid group of 40 mol\(\mu\)/l failed to achieve the PK/PD target of 100% fT > MIC and 100% fT > 4 MIC for all the simulated dosing regimens. In general, high levels of CG-CLCR and low levels of uric acid were associated with lower PTA. Detailed influences of creatinine and uric acid on PTA are shown in Fig. 3. Patients with high creatinine clearance rates were likely to have lower PTA (P = 0.003), while those with high levels of uric acid were likely to have higher PTA (P < \(0.001)\) (Fig. 3).
We analyzed the PTA obtained from the simulation result and found that infusion times of 2 h and 4 h appeared to have a PTA value > 0.5 h on average (P = 0.047, Fig. 4). However, the number of targeted PTAs (\(\ge 90\%\)) showed no significant difference among the three groups (P = 0.6847). Given this surprising result, various MICs and therapeutic targets were analyzed. The results are presented in Fig. 5. We found that the duration of infusion affected the improvement of PTA (Fig. 5). For the target of 40% fT \(>\) MIC, PTA was significantly different among the three groups of simulated data when MIC < \(4\) mg/l (P < 0.05). Under these circumstances, PTA could be improved by prolonged infusion time. The difference in PTA was close to significant when MIC was 4 mg/l (P = 0.0568). Notably, the P value of the three groups was 0.234 for the target of 40% fT \(>\) MIC when MIC was 8 mg/l\(.\) This finding suggests that, for drug-resistant bacteria with high MICs, prolonged infusion time does not improve PTA level. There was no significant difference in PTA among the three groups for the targets 100% fT \(>\) MIC and 100% fT \(>\) 4 MIC, even though MIC was 1 mg/l.
Effect of infusion time on PTA under different MICs and therapeutic effect. Distinctions of injection time (0.5 h, 2 h, and 4 h) on simulated PTA values of different MICs: 1 mg/l (a,b,c,d), 2 mg/l (a1,b1,c1,d1), 4 mg/l (a2,b2,c2,d2), and 8 mg/l (a3,b3,c3,d3) and PK/PD targets: 40% fT > MIC (a,a1,a2,a3), 100% fT > MIC (b,b1,b2,b3), and 100% fT > 4 MIC (c,c1,c2,c3). Red circles, injection time of 0.5 h; blue triangles, injection time of 2 h; yellow squares, injection time of 4 h
Discussion
We developed a PPK model of meropenem in patients with severe pulmonary infection. In the previous literature, correlations of antibiotic CL with creatinine clearance were often reported. To the best of our knowledge, our study is the first to determine that uric acid is a significant covariate describing the pharmacokinetic parameters of meropenem. See Table S1–S3 in the electronic supplementary material for details. These tables display the PTAs for all simulated dosage regimens using 40% fT > MIC, 100% fT > MIC, and 100% fT > 4 MIC pharmacodynamic (PD) thresholds, respectively. According to further PTA analysis, we observed that higher levels of CG-CLCR and lower levels of uric acid were associated with the lower achievement of PK/PD targets for critically ill patients. Many studies found that the characteristics of meropenem pharmacokinetics could be described in different populations using a two-compartment model, which is consistent with the results of our study [17, 18, 40,41,42]. Adela et al. found that the administration of 2000 mg/8 h of meropenem as a continuous infusion allowed higher serum meropenem concentrations [41]. Similar results were found in other studies of meropenem [15, 17, 40, 41, 43]. Ivan Chytra et al. reported that continuous infusion of meropenem generated superior bacteriological efficacy and offered the encouraging alternative of antimicrobial therapy in critically ill patients [44]. Zhenhong Wang et al. compared 3-h extended infusion of meropenem with a conventional regime of 30-min infusion in ICU patients and found that the clinical outcome can be improved [45]. However, these studies mainly focused on the clinical outcomes, while our study mainly focused on the pharmacodynamic antibacterial effect of meropenem.
In the following analysis, we found that the duration of infusion had a complex effect on the improvement of PTA. It was significant only when using the traditional target of 40% fT > MIC with MIC < 4 (Fig. 4). For the PD effects of 100% fT > MIC and 100% fT > 4 MIC, no significant statistical differences were discovered. This finding suggests that, for patients with sensitivity to meropenem and mild infection, prolonging the infusion time can improve the therapeutic effect (MIC < 4). By contrast, those with meropenem resistance or severe infections (who require a higher therapeutic target) had no significant clinical benefit from prolonged infusion time. A. baumannii and K. pneumoniae generally have high MICs. Therefore, higher dosages are needed to achieve the targeted therapeutic effect. However, Mohd et al. conducted an observational study of 211 patients receiving piperacillin/tazobactam and meropenem and found that administration of meropenem by prolonged infusion in critically ill patients was beneficial. Several studies showed similar results and encouraged extended infusions because this maximizes the likelihood of achieving target blood concentrations [41, 43, 46,47,48].
The reason for this distinction is probably that few studies have compared the differences in therapeutic responses of 100% fT > MIC, 100% fT > 4 MIC, and 40% fT > MIC caused by infusion time; we did so and identified the distinction. It is worth noting that De Waele et al. mentioned that, in a significant subpopulation of critically ill patients with normal renal function, a 100% fT > MIC target is not reached, even with 3-h extended infusions. This finding agrees with our results.
We also assessed the achievement of different PK/PD targets (40% fT > MIC, 100% fT > MIC and 100% fT > 4 MIC) under MIC values ranging from 1 to 8 mg/l. The effect of meropenem dosage and infusion duration was also assessed. In particular, patients with creatinine clearance ≤ 60 ml/min and uric acid > 400 μmol/l can achieve the target of PTA \(>\) 90% under the MIC of 8 mg/l, even with the administration dose of 500 mg/8 h with a 2-h infusion (Additional file 2). This finding suggests that 500 mg/8 h is sufficient for critically ill renal failure patients with high uric acid levels.
Although the correlation of antibiotic CL with creatinine clearance has been widely reported [12, 13, 17], to our knowledge this study represents the first finding of uric acid having a significant impact on meropenem use. We also found that patients with lower creatinine clearance and high uric acid levels tend to require lower dosages. Our findings suggest that dose adjustment based on these two factors appears to be reasonable.
However, our study also has some limitations. First, it is a relatively small single-center study, and the sample size is small. The relatively limited sample size made it difficult to correlate the PK/PD target with clinical and microbiological outcomes. Second, some patients think the MIC test is worthless and refuse to do it. Ethically, we have to follow the patient's will, which resulted in a small fraction of isolates without meropenem susceptibility. Third, the influence of plasma concentration on adverse effects and clinical outcome was not assessed. Further study is needed to associate meropenem trough concentration with its adverse and therapeutic effects. Moreover, the factor of drug combination is not recorded in the study, and the simulation results of this study could be a little different from actual drug use. Further actual tissue concentrations can also be studied [27, 49] to assess the concentrations in the epithelial lining fluid of the lung [41, 50]. In addition, most of the samples were collected at the trough concentration time; these sparsely sampled data may affect the fitting of the model and intraindividual variability during the treatment period that could not be measured [27, 51].Nevertheless, our study still provides essential information about the optimized dosage regimen of meropenem in critically ill patients. During empirical therapy of severe pneumonia caused by gram-negative bacteria, clinicians should consider both the achievement of clinical cure and the prevention of drug resistance. Therapeutic drug monitoring is one of the best means to achieve precision therapy.
Conclusions
Lower CG-CLCR and higher uric acid levels were likely to achieve higher exposure in serum and were associated with lower PTA. A dose of 500 mg/8 h may be necessary to achieve optimal coverage in critically ill patients for all susceptible isolates (MIC ≤ 8 mg/l) in patients with high uric acid levels associated with severe renal injury. Moreover, for those with drug-resistant or severe infections (MIC > 4 mg/l\()\) and critically ill patients who need a higher therapeutic target (100% fT > MIC, 100% fT > 4 MIC), prolonged infusion time does not appear to be beneficial. Increasing dose or alternative therapeutic strategies may be required for critically ill patients with drug-resistant or severe infections who need a higher therapeutic target.
References
Wongsurakiat P, Chitwarakorn N. Severe community-acquired pneumonia in general medical wards: outcomes and impact of initial antibiotic selection. BMC Pulm Med. 2019;19:179.
Lanks CW, Musani AI, Hsia DW. Community-acquired pneumonia and hospital-acquired pneumonia. Med Clin N Am. 2019;103:487–501.
Chahin A, Opal SM. Severe pneumonia caused by legionella pneumophila: differential diagnosis and therapeutic considerations. Infect Dis Clin N Am. 2017;31:111–21.
Marti C, Garin N, Grosgurin O, et al. Prediction of severe community-acquired pneumonia: a systematic review and meta-analysis. Crit Care (Lond, Engl). 2012;16:R141.
Smith HZ, Kendall B. Carbapenem resistant enterobacteriaceae. StatPearls. Treasure Island (FL): StatPearls Publishing. Copyright © 2021, StatPearls Publishing LLC., 2021.
Hraiech S, Alingrin J, Dizier S, et al. Time to intubation is associated with outcome in patients with community-acquired pneumonia. PLoS ONE. 2013;8:e74937.
Restrepo MI, Mortensen EM, Rello J, et al. Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest. 2010;137:552–7.
Restrepo MI, Mortensen EM, Velez JA, et al. A comparative study of community-acquired pneumonia patients admitted to the ward and the ICU. Chest. 2008;133:610–7.
Wiseman LR, Wagstaff AJ, Brogden RN, et al. Meropenem. A review of its antibacterial activity, pharmacokinetic properties and clinical efficacy. Drugs. 1995;50:73–101.
Dhillon S. Meropenem/vaborbactam: a review in complicated urinary tract infections. Drugs. 2018;78:1259–70.
Jaruratanasirikul S, Thengyai S, Wongpoowarak W, et al. Population pharmacokinetics and Monte Carlo dosing simulations of meropenem during the early phase of severe sepsis and septic shock in critically ill patients in intensive care units. Antimicrob Agents Chemother. 2015;59:2995–3001.
Ramon-Lopez A, Allen JM, Thomson AH, et al. Dosing regimen of meropenem for adults with severe burns: a population pharmacokinetic study with Monte Carlo simulations. J Antimicrob Chemother. 2015;70:882–90.
Zhou QT, He B, Shen N, et al. Meropenem dosing based on a population pharmacokinetic-pharmacodynamic model in elderly patients with infection of the lower respiratory tract. Drugs Aging. 2017;34:115–21.
Conte JE Jr, Golden JA, Kelley MG, et al. Intrapulmonary pharmacokinetics and pharmacodynamics of meropenem. Int J Antimicrob Agents. 2005;26:449–56.
Cies JJ, Moore WS 2nd, Enache A, et al. Population pharmacokinetics and pharmacodynamic target attainment of meropenem in critically ill young children. J Pediatr Pharmacol Ther. 2017;22:276–85.
Usman M, Frey OR, Hempel G. Population pharmacokinetics of meropenem in elderly patients: dosing simulations based on renal function. Eur J Clin Pharmacol. 2017;73:333–42.
Alobaid AS, Wallis SC, Jarrett P, et al. Effect of obesity on the population pharmacokinetics of meropenem in critically ill patients. Antimicrob Agents Chemother. 2016;60:4577–84.
Doh K, Woo H, Hur J, et al. Population pharmacokinetics of meropenem in burn patients. J Antimicrob Chemother. 2010;65:2428–35.
Hanberg P, Öbrink-Hansen K, Thorsted A, et al. Population pharmacokinetics of meropenem in plasma and subcutis from patients on extracorporeal membrane oxygenation treatment. Antimicrob Agents Chemother. 2018;62:e02390.
Kristoffersson AN, David-Pierson P, Parrott NJ, et al. Simulation-based evaluation of PK/PD indices for meropenem across patient groups and experimental designs. Pharm Res. 2016;33:1115–25.
Roberts JA, Abdul-Aziz MH, Lipman J, et al. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014;14:498–509.
Mendez A, Chagastelles P, Palma E, et al. Thermal and alkaline stability of meropenem: degradation products and cytotoxicity. Int J Pharm. 2008;350:95–102.
Jaruratanasirikul S, Sriwiriyajan S. Comparison of the pharmacodynamics of meropenem in healthy volunteers following administration by intermittent infusion or bolus injection. J Antimicrob Chemother. 2003;52:518–21.
McKinnon PS, Paladino JA, Schentag JJ. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T>MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents. 2008;31:345–51.
Tam VH, McKinnon PS, Akins RL, et al. Pharmacodynamics of cefepime in patients with gram-negative infections. J Antimicrob Chemother. 2002;50:425–8.
Abdul-Aziz MH, Lipman J, Akova M, et al. Is prolonged infusion of piperacillin/tazobactam and meropenem in critically ill patients associated with improved pharmacokinetic/pharmacodynamic and patient outcomes? An observation from the Defining Antibiotic Levels in Intensive care unit patients (DALI) cohort. J Antimicrob Chemother. 2016;71:196–207.
Veiga RP, Paiva JA. Pharmacokinetics-pharmacodynamics issues relevant for the clinical use of beta-lactam antibiotics in critically ill patients. Crit Care (Lond, Engl). 2018;22:233.
Kazmierczak KM, Karlowsky JA, de Jonge BLM, et al. Epidemiology of carbapenem resistance determinants identified in meropenem-nonsusceptible enterobacterales collected as part of a global surveillance program, 2012 to 2017. Antimicrob Agents Chemother. 2021;65:e0200020.
Hassuna NA, Darwish MK, Sayed M, et al. Molecular epidemiology and mechanisms of high-level resistance to meropenem and imipenem in Pseudomonas aeruginosa. Infect Drug Resist. 2020;13:285–93.
Sharma M, Singhal L, Gautam V, et al. Distribution of carbapenemase genes in clinical isolates of Acinetobacter baumannii & a comparison of MALDI-TOF mass spectrometry-based detection of carbapenemase production with other phenotypic methods. Indian J Med Res. 2020;151:585–91.
Shahbaz H, Gupta M. Creatinine clearance. StatPearls. Treasure Island (FL): StatPearls Publishing. Copyright © 2021, StatPearls Publishing LLC., 2021.
Nunes MBG, Filho AC, Alvares VRC, et al. CKD-EPI versus Cockcroft-Gault formula for predicting contrast-induced nephropathy following percutaneous coronary intervention in patients without significant renal impairment. Rev Port Cardiol. 2018;37:25–33.
Casals G, Hernández C, Hidalgo S, et al. Development and validation of a UHPLC diode array detector method for meropenem quantification in human plasma. Clin Biochem. 2014;47:223–7.
Zou L, Meng F, Hu L, et al. A novel reversed-phase high-performance liquid chromatographic assay for the simultaneous determination of imipenem and meropenem in human plasma and its application in TDM. J Pharm Biomed Anal. 2019;169:142–50.
Wong G, Farkas A, Sussman R, et al. Comparison of the accuracy and precision of pharmacokinetic equations to predict free meropenem concentrations in critically ill patients. Antimicrob Agents Chemother. 2015;59:1411–7.
Zhao W, Kaguelidou F, Biran V, et al. External evaluation of population pharmacokinetic models of vancomycin in neonates: the transferability of published models to different clinical settings. Br J Clin Pharmacol. 2013;75:1068–80.
Glen JB, Servin F. Evaluation of the predictive performance of four pharmacokinetic models for propofol. Br J Anaesth. 2009;102:626–32.
Egi A, Fukuda H, Kawamoto M, et al. Preoperative prediction of creatinine clearance by using serum creatinine. Masui Jpn J Anesthesiol. 2004;53:1306–10.
Chung EK, Cheatham SC, Fleming MR, et al. Population pharmacokinetics and pharmacodynamics of meropenem in nonobese, obese, and morbidly obese patients. J Clin Pharmacol. 2017;57:356–68.
Sjövall F, Alobaid AS, Wallis SC, et al. Maximally effective dosing regimens of meropenem in patients with septic shock. J Antimicrob Chemother. 2018;73:191–8.
Benítez-Cano A, Luque S, Sorlí L, et al. Intrapulmonary concentrations of meropenem administered by continuous infusion in critically ill patients with nosocomial pneumonia: a randomized pharmacokinetic trial. Crit Care (Lond, Engl). 2020;24:55.
Burger R, Guidi M, Calpini V, et al. Effect of renal clearance and continuous renal replacement therapy on appropriateness of recommended meropenem dosing regimens in critically ill patients with susceptible life-threatening infections. J Antimicrob Chemother. 2018;73:3413–22.
Corcione S, D’Avolio A, Loia RC, et al. Pharmacokinetics of meropenem in burn patients with infections caused by Gram-negative bacteria: are we getting close to the right treatment? J Glob Antimicrob Resist. 2020;20:22–7.
Chytra I, Stepan M, Benes J, et al. Clinical and microbiological efficacy of continuous versus intermittent application of meropenem in critically ill patients: a randomized open-label controlled trial. Crit Care (Lond, Engl). 2012;16:R113.
Wang Z, Shan T, Liu Y, et al. Comparison of 3-hour and 30-minute infusion regimens for meropenem in patients with hospital acquired pneumonia in intensive care unit: a randomized controlled clinical trial. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2014;26:644–9.
Wunderink RG, Matsunaga Y, Ariyasu M, et al. Cefiderocol versus high-dose, extended-infusion meropenem for the treatment of Gram-negative nosocomial pneumonia (APEKS-NP): a randomised, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2021;21:213–25.
Nguyen CP, Dan-Do TN, Bruggemann R, et al. Clinical cure rate and cost-effectiveness of carbapenem-sparing beta-lactams vs meropenem for Gram-negative infections: a systematic review, meta-analysis, and cost-effectiveness analysis. Int J Antimicrob Agents. 2019;54:790–7.
Ehmann L, Zoller M, Minichmayr IK, et al. Development of a dosing algorithm for meropenem in critically ill patients based on a population pharmacokinetic/pharmacodynamic analysis. Int J Antimicrob Agents. 2019;54:309–17.
Roberts JA, Udy AA, Jarrett P, et al. Plasma and target-site subcutaneous tissue population pharmacokinetics and dosing simulations of cefazolin in post-trauma critically ill patients. J Antimicrob Chemother. 2015;70:1495–502.
Motos A, Kuti JL, Li Bassi G, et al. Is one sample enough? β-lactam target attainment and penetration into epithelial lining fluid based on multiple bronchoalveolar lavage sampling time points in a swine pneumonia model. Antimicrob Agents Chemother. 2019;63:e01922.
Neely MN, van Guilder MG, Yamada WM, et al. Accurate detection of outliers and subpopulations with Pmetrics, a nonparametric and parametric pharmacometric modeling and simulation package for R. Ther Drug Monit. 2012;34:467–76.
Acknowledgements
Funding
This study was funded by Hunan Pharmaceutical Association of China with fund number of (HMA202001002). The journals’ Rapid Service Fee was funded by Hunan Pharmaceutical Association of China.
Medical Writing, Editorial, and Other Assistance
The authors sincerely acknowledge Jing-jing Hou, Dan-Tang, and Jia-Min Wu for assistance in medical writing, manuscript editing, and data collecting. We also thank Doctor Mou-Ze Liu for helping with the concentration analysis. We also thank for the study participant(s) for their involvement.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization: Yi-Chang Zhao, Yang Zou, Yi-Wen Xiao, Feng Yu; Methodology: Yi-Chang Zhao, Yi-Wen Xiao, Feng Wang, Bi-Kui Zhang, Da-Xiong Xiang, Hong Luo; Formal analysis and investigation: Yi-Chang Zhao, Yang Zou; Writing-original draft preparation: Yi-Chang Zhao; Writing-review and editing: Indy Sandaradura; Funding acquisition: Miao Yan; Resources: Bi-Kui Zhang, Da-Xiong Xiang, Hong Luo, Miao Yan; Supervision: Miao Yan.
Disclosures
Yi-Chang Zhao, Yang Zou, Yi-Wen Xiao, Feng Wang, Bi-Kui Zhang, Da-Xiong Xiang, Feng Yu, Hong Luo, Indy Sandaradura, and Miao Yan have nothing to disclose.
Compliance with Ethics Guidelines
Ethics approval was obtained from the local ethics committee (The Second Xiang-ya Hospital of Central South University; approval no. 2019-005). It was also registered in China Clinical Trials (no. ChiCTR1900020672). Written informed consent was obtained from either the patient or their appointed legal guardian. The study was in full compliance with the Declaration of Helsinki.
Data Availability
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhao, YC., Zou, Y., Xiao, YW. et al. Does Prolonged Infusion Time Really Improve the Efficacy of Meropenem Therapy? A Prospective Study in Critically Ill Patients. Infect Dis Ther 11, 201–216 (2022). https://doi.org/10.1007/s40121-021-00551-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-021-00551-2