Abstract
Exercise training represents a health behavior for the treatment and management of the multi-faceted manifestations of multiple sclerosis (MS). This paper provides a comprehensive overview of evidence from randomized controlled trials (RCTs) regarding benefits, safety, participation, and guidelines for exercise training in MS, based on systematic reviews and meta-analyses. The paper then provides our opinions based on extensive experience regarding challenges for improving and expanding future RCTs that will advance our understanding of exercise training in MS. The comprehensive review of evidence from RCTs indicates that exercise training yields substantial improvements in aerobic and muscle fitness, mobility, fatigue and depression, quality of life, and participation outcomes. There is a non-significant increase in the risk of adverse events or serious adverse events with exercise training compared with control conditions or healthy populations. Rates of adherence and compliance with exercise training (i.e., participation) approximate 80% and 70%, respectively. The current prescriptive guidelines suggest 2–3 days per week of aerobic and resistance exercise training as the minimal dose for safely benefiting from exercise training in MS. We propose 10 important topics as avenues for expanding the body of research and improving its scope for evidence-based practice in MS. Overall, the research on exercise training in MS is strong, but it can get stronger. The expansion and advancement of evidence are critical for moving exercise training into the clinical armamentarium of MS disease treatment and management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Randomized controlled trials indicate that exercise training is safe and yields substantial benefits from improvements in fitness through quality of life for people with multiple sclerosis. |
The benefits of exercise can be achieved by meeting the prescriptive guidelines of 2–3 days per week of both aerobic and resistance modes of training. |
There are opportunities for expanding and improving the quality of evidence from randomized controlled trials of exercise training in multiple sclerosis. |
The provision of even higher-quality evidence will further support the inclusion of exercise training into clinical care of managing multiple sclerosis. |
Introduction
There are an estimated 1 million adults living with multiple sclerosis (MS) in the United States [1]. MS is an immune-mediated and neurodegenerative disease resulting in demyelination and transection of axons and loss of neurons in the central nervous system (CNS) [2]. The extent and location of CNS damage (e.g., lesions) manifests as cognitive and walking dysfunction, symptoms, and compromised participation and quality of life (QOL).
Disease-modifying therapies are the first-line approach for management of MS itself, and these medications are effective for reducing rates of relapses, lesions, and disability progression [3]. Nevertheless, people with MS still demonstrate cognitive and walking dysfunction and symptoms perhaps based on residual CNS damage and/or smoldering disease [4] or alterations in health behaviors resulting in comorbidity [5].
Exercise training is a health behavior and second-line approach for management of disease manifestations among people with MS. Exercise training is defined as planned, structured, and repetitive physical activity with the objective of improving or maintaining health-related physical fitness [6], and often includes aerobic (e.g., walking) and resistance (e.g., muscle strengthening) training modalities separately or together in MS. Of note, a search of PubMed on May 21, 2024, using the keywords “multiple sclerosis” and “exercise” with a focus on randomized controlled trials (RCTs) as article type identified 388 publications. This large body of research from RCTs serves as a foundation of evidence-based practice for the application of exercise training in people with MS.
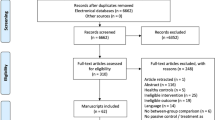
This paper provides a comprehensive overview of evidence from RCTs regarding benefits, safety, participation, and guidelines for exercise training in MS based on systematic reviews and meta-analyses. We focused on systematic reviews and meta-analyses as the 388 publications were too many for review in a single paper. The systematic reviews and meta-analyses included in the current paper were identified through a PubMed search and we selected those published within the last 3–5 years for inclusion, when possible. This paper then provides our opinions based on knowledge and experiences with exercise training in MS regarding challenges for improving and expanding future RCTs that will advance our understanding of the subject. Importantly, this article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Benefits of Exercise Training
We provide a summary of the benefits of exercise training in people with MS based on evidence from meta-analyses of RCTs. This summary was organized consistent with the ICF model for understanding the effects of exercise training on outcomes in MS [7], and Fig. 1 presents a graphical summary of the current evidence for the magnitude of exercise training effects on the outcomes. To our knowledge, there are no meta-analyses of RCTs examining exercise training effects on inflammatory markers in MS, yet two meta-analyses have examined changes in markers of neurodegeneration based on neurotrophic factors, and have reported a large, statistically significant effect of exercise training on BDNF (ES range = 0.78–2.40) [8, 9], but small non-significant effects on NGF (ES = 0.28) and CNTF (ES = 0.24) [8]. There are no meta-analysis of RCTs examining exercise training effects on MRI markers of axonal damage or neuronal loss in MS; however, there are abundant meta-analyses of exercise training effects on body functions in MS. Regarding mental functions, meta-analyses of exercise training have reported effects for fatigue (ES range = 1.15–0.09) [10,11,12,13,14,15] and depression (ES range = 0.36–0.45) [16,17,18], but not cognition (ES = 0.04) [19]. Regarding cardiovascular, neuromusculoskeletal, and sensory functions, meta-analyses of exercise training have reported effects for aerobic power (ES range = 0.32–0.88) [9, 20] and muscle strength (ES range = 0.34–0.93) [9, 11, 20], as well as balance (ES range = 0.54–4.22) [10, 11]. There are numerous examples of meta-analyses examining the effects of exercise training on activities in MS, and exercise training improves walking mobility including walking speed (ES range = 0.27–1.01) and endurance (ES = 0.25–0.37) in MS [9,10,11]. There are numerous examples of meta-analyses examining the effects of exercise training on participation in MS, and exercise training improves QOL and activities of daily living in MS (ES range = 0.41–0.64) [17, 21, 22].
Safety of Exercise Training
There has been a long-standing concern regarding the safety of exercise training in MS. We initially addressed this topic based on a systematic review of adverse events (AEs) reported in RCTs of exercise training in MS [23]. The review included 26 studies with 1,295 participants. The rate of AEs was 2.0% and 1.2% for exercise training and control conditions, respectively, and this yielded a relative risk (RR) of 1.67. Of note, the RR of AEs was not higher than reported in healthy populations [23]. The types of AEs with exercise training included stroke, illness, infection, trigeminal neuralgia, back and joint pain, fracture, hernia, and a traffic accident, and musculoskeletal injuries typically occurred with resistance exercise training.
We subsequently designed [24] and reported [25] on a more comprehensive and updated meta-analysis of AEs and serious adverse events (SAEs) in RCTs of exercise training in MS published after the initial systematic review. This meta-analysis included 40 studies with 1,780 participants. The rate of AEs was 38% and 22% for exercise and control conditions, respectively, and this yielded a non-statistically significant RR of 1.40; the higher rate of AEs likely reflects calls and standards for better documentation and reporting based on the initial systematic review and CONSORT reporting requirements, respectively. The rate of SAEs was 10% and 9% for exercise and control conditions, respectively, and this yielded a non-statistically significant RR of 1.05. There was no evidence for variability in AE and SAE risk for exercise training by exercise type, delivery style, or participant disability. Of note, people with MS included in exercise training RCTs are often screened and excluded for the presence of contraindications such as heart conditions, chest pain, and high blood pressure.
Adherence and Compliance with Exercise Training
The Moving Exercise Research in Multiple Sclerosis Forward (MoXFo) initiative provided a series of papers on moving the agenda on exercise training in MS forward, and one area of importance involved understanding participation based on rates of drop-out, adherence, and compliance with RCTs of exercise training in MS [26]. We recently documented the reporting and rates of drop-out, adherence, and compliance from 40 RCTs of exercise training in MS [27]. Drop-out was reported in 100% of the RCTs and rates were 11.2% and 8.9% for exercise training and control conditions, respectively. Adherence and compliance with exercise training were reported in 63% and 6.5% of the RCTs, respectively, and rates were 79.7% and 69.8%, respectively. Those rates are comparable with the general population, and there was limited evidence for variation in rates between modalities of exercise training.
Guidelines for Exercise Training
The initial prescriptive guidelines for exercise training in MS [28] were informed based on a systematic review of evidence from pre-post trials and RCTs [29]. The guidelines indicated that adults with MS, who have mild or moderate disability (EDSS 0–6.5) resulting from relapsing or progressive forms of the disease, need at least 30 min of moderate intensity aerobic activity 2 days per week and strength-training exercises for major muscle groups 2 days per week. These guidelines were later revised and updated based on a harmonizing review of published guidelines in MS [30]. The harmonizing review altered the number of days/weeks of aerobic and strength-training exercise in MS (now 2–3 days per week rather than 2 days per week), and further generated an advanced exercise prescription of 5 days/week of high-intensity aerobic exercise for those who exercise regularly or who seek greater benefits from exercise training [30].
Future Research Directions for Exercise Training
There are many important avenues for expanding the body of research and improving its scope for evidence-based practice in MS. These avenues provide the scope of the content for the remainder of the paper. The avenues were selected based on the expert opinions of the two authors, who have 30+ years of experience with exercise training and MS. We recognize that this list is neither exhaustive nor without possible controversy, but we believe that these areas are central for expanding the quality of evidence necessary for the inclusion of exercise training in MS clinical care.
Importance of Feasibility Trials
Science is in the midst of a crisis regarding the reproducibility of research results [31], and this has its roots in the design of RCTs [32], including RCTs of exercise training [33]. The application of RCTs of exercise training in MS may be improved through the adoption of the NIH stage model of clinical trials (https://www.nia.nih.gov/research/dbsr/nih-stage-model-behavioral-intervention-development). This model articulates the sequential progression of research from Stage 1 through Stage 5 for establishing the basis of an intervention for management of an outcome in real-world settings. Stage 1 (e.g., creation and preliminary testing of a new intervention) can include the generation of new exercise training interventions as well as the modification, adaptation, or refinement of existing interventions (Stage 1A), and culminates in feasibility and pilot testing (Stage 1B). Stage 5 research examines strategies of implementation and adoption of empirically supported exercise training interventions in community settings. One critical, yet seldom undertaken, research design as a basis for future RCTs of exercise training involves feasibility trials (Stage 1B). The idea of feasibility trials involves examining and understanding the “processes” involved in conducting a clinical trial of exercise training, and involves four main areas of inquiry, namely (1) process (e.g., recruitment/retention), (2) resource (e.g., monetary costs), (3) management (e.g., personnel time), and (4) scientific (e.g., safety/PROMs) metrics [34]. Such feasibility trials are the bedrock for subsequent efficacy and effectiveness RCTs, as if the approach is not feasible, then there are likely major issues requiring resolution before moving forward with testing efficacy and effectiveness of an exercise training intervention.
Discovery Model for Selection of Exercise Training Interventions
One important approach for decisions regarding selection of exercise training interventions for RCTs involves the implementation of a discovery model [35]. This approach starts with examining acute or short-term responses with a single exposure of an intervention stimulus (e.g., change in mood pre/post one bout of cycling for 30 min at 60% of heart rate reserve), and transitions into chronic, repeated exposure of the same stimulus over a long-term period (e.g., change in mood pre/post 12 weeks of cycling for 30 min at 60% of heart rate reserve 3 days/week). The notion is that, if a single stimulus exposure exerts a short-term or temporary effect on an outcome of interest, repeated exposure of the same stimulus over longer periods of time will result in adaptations within a human system. If an acute stimulus does not perturb the system (i.e., temporary effect), then it may be unlikely that repeated exposure over time as a chronic stimulus would yield adaptations within a system (i.e., long-term effect). We do recognize, importantly, that there are some outcomes wherein the discovery model might not be ideal (e.g., muscle changes might not be obvious with a single session, but adaptations can still occur with chronic exercise training).
Primary End-Points in Samples Screened for Presence of Symptoms/Dysfunction
RCTs of exercise training in MS often include a multitude of outcomes and samples that are not pre-screened for a focal, primary problem. For example, RCTs of exercise training for depression in MS often include depression symptom scales as secondary or tertiary/exploratory outcomes, and seldom recruit focal samples with elevated depressive symptom status as part of inclusion criteria [36]. This is an issue because we do not know (1) if depressed persons with MS can actually adhere with an exercise training program or (2) if an exercise training program actually improves or worsens depression as a primary outcome in depressed persons with MS. The principle of screening for persons with depression and identifying depression as a primary end-point is further important for inferences regarding an intervention as a “treatment” modality for outcomes (i.e., restoring normal levels of depression in depressed people with MS).
Heterogeneity for Informing Precision Medicine
RCTs of exercise training interventions in MS document overall or group-level changes in outcomes, but often overlook the substantial variability of change within groups (i.e., individual-level changes) that has implications for broad, prescriptive application and precision medicine. For example, there is evidence of within-study heterogeneity of changes in outcomes (e.g., aerobic fitness, walking performance) with exercise training in people with MS [37]. This indicates that, with a standardized aerobic exercise training stimulus, some participants demonstrate improvements, others no change, and some a worsening on the study outcome, and this does not solely represent measurement error [38]. The heterogeneity of changes with exercise training may be explainable by other factors (e.g., baseline fitness, disability, MS type, etc.), and this informs the application of precision medicine in MS. The premise of precision medicine focuses on identifying factors that explain heterogeneity of change in an outcome for an exercise training intervention, and then using that information for delivery of an individually-centered treatment stimulus that optimizes outcomes of exercise training interventions [39].
Comorbidity
Comorbidity, particularly vascular comorbidity, is prevalent in MS, and further influences the progression and severity of the disease [5]. There have been surprisingly few examinations of exercise training and vascular comorbid conditions in MS, particularly examining effects on markers of vascular dysfunction (e.g., arterial stiffness or endothelial function) [40]. This is noteworthy, as exercise training is recognized as a powerful health behavior for preventing and managing vascular conditions and dysfunction in the general population [41], and one would imagine similar benefits in MS, yet this proposition should be directly examined in RCTs. If exercise training is effective for preventing and managing vascular conditions and dysfunction in MS, this might translate into secondary effects on the disease and its progression over time [42].
Adherence and Compliance for Guiding Future Prescriptions/Applications
The quantification and reporting of dropout within RCTs of exercise training has improved profoundly based on it representing a component with the CONSORT reporting criteria. The same is not true for adherence and compliance [27] as these are reported in only 63% and 6.5% of RCTs, respectively. To that end, the adherence expert panel of the MoXFo initiative provided definitions and metrics for documenting adherence and compliance as important participation variables possibly influencing the benefits of exercise training in MS [26]. If researchers adopt the standardized definitions and metrics for documenting and reporting adherence and compliance in future RCTs of exercise training, we can make informed decisions about dose of exposure for accruing outcomes in MS.
Neural Mechanisms Through Experimental Medicine
There has been an expanding interest in the neural mechanisms of action for outcomes of exercise training interventions in MS. We recently proposed an experimental medicine model for understanding neural mechanisms of action (e.g., changes in brain structure, function, and connectivity based on magnetic resonance imaging) for neuroperformance outcomes of exercise training in MS [43]. This model moves beyond standard efficacy RCTs, and involves a systematic, sequential approach of identifying three pre-conditions (Paths A–C) before applying a fourth condition (Path D) for fully testing a mechanistic neural pathway for improvements in outcomes of exercise training in MS. Path A involves identifying putative neural mechanisms based on conceptual frameworks or models. Path B involves validating the putative neural mechanisms based on correlations with neuroperformance outcomes. Path C involves examining exercise training effects on the putative neural mechanisms using an RCT. And Path D involves a full test of putative neural mechanisms by simultaneously examining exercise training effects on neuroperformance outcomes and putative neural mechanisms as mediators in a RCT. This model, if applied broadly, can identify neural, and perhaps other, mechanisms of action for exercise training effects on a variety of outcomes in people with MS.
Under-Researched Populations
The demography of MS has changed profoundly over the past decade or longer, and we now know much more about the prevalence and consequences of MS by race, ethnicity, and chronological age [1, 44]. Nevertheless, researchers have lagged considerably in conducting RCTs of exercise training with broad inclusion in this changing demography. For example, there is limited inclusion of people who identify as Black/African-American or Hispanic/Laxinx in RCTs of exercise training in MS [45]. Furthermore, there has been scant research involving RCTs of exercise training in older adults with MS [46]. The extension of RCTs of exercise training into these under-researched populations is necessary to meet the unique needs that map with the evolving demography of MS, as we cannot simply assume that what works in some populations universally works in others—this is not consistent with evidence-based practice. There are likely unique features of conducting and designing exercise training interventions that differ by race, ethnicity, and chronological age, and the results of RCTs might depend heavily on understanding these features and tailoring the design and administration of interventions for yielding positive outcomes.
Clinical Characteristics of MS
The majority of RCTs on exercise training in MS have included samples with mild or moderate disability, relapsing–remitting disease courses, and low risk for undertaking exercise training [47]. There is a clear need for research enrolling people with severe disability, including wheelchair users, and progressive clinical courses, as this will broaden our understanding of exercise training effects across the spectrum of MS. We further believe that researchers should enroll samples with a greater risk profile for adverse events with exercise training, as the majority of people with MS have vascular conditions, yet we do not know if exercise is safe, tolerated, and/or beneficial outside of those pre-screened for low-risk status. This obviously requires greater oversight with exercise screening, testing and training, but represents a major step forward with creating a more generalizable knowledge base on the safety, tolerability, and benefits of exercise training in MS.
Combined Interventions
The notion that one health behavior, rehabilitation, or educational/behavioral intervention alone is sufficient for managing or treating outcomes in MS is likely naïve, yet researchers often study the effects of exercise training in isolation from other approaches such as diet, cognitive behavioral therapy, cognitive rehabilitation, or falls prevention. There have been recent noteworthy exceptions such as CogEx [48] that examined exercise training and cognitive rehabilitation alone and combined for improving slowed processing speed in progressive MS, but that study is largely a unicorn in the field. We particularly note that, with the expanding body of research supporting the benefits of diet in MS [49], an obvious next step involves combined dietary and exercise intervention for combinatory or additive effects, as these are complimentary health behaviors likely working on different underlying pathways. We further envision research examining the inclusion of exercise training along with educational/behavioral interventions for fall prevention.
Summary
The research on exercise training in MS is strong, but it can get stronger. We have outlined 10 areas based on our collective experience for expanding the body of research on exercise training in MS. We recognize this list of areas is neither exhaustive nor based on a consensus process, but we believe that our perspective regarding challenges and opportunities for improving and expanding future RCTs will advance the understanding of exercise training in MS. Such expansion and advancement are critical for moving exercise training into the clinical armamentarium of MS disease management [50].
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92:1029–40.
Trapp BD, Nave K. Multiple sclerosis: an immune or neurodegenerative disorder? Ann Rev Neurosci. 2008;31:247–69.
Rae-Grant A, Day GS, Marrie RA, et al. Comprehensive systematic review summary: disease-modifying therapies for adults with multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Acedmy of Neuology. Neurology. 2018;90:789–800.
Giovannoni G, Popescu V, Wuerfel J, et al. Smouldering multiple sclerosis: the ‘real MS.’ Ther Adv Neurol Disord. 2022;15:17562864211066752.
Marrie RA. Comorbidity in multiple sclerosis: implcations for patient care. Nat Rev Neurol. 2017;13:375–82.
Bouchard C, Shephard RJ. Physical activity, fitness, and health: the model and key concepts. In: Bouchard C, Shephard RJ, Stephens T, editors. Physical activity, fitness, and health: international proceedings and consensus statement. Champaign: Human Kinetics Publishers; 1994. p. 77–88.
Motl RW, Pilutti LA. The benefits of exercise training in multiple sclerosis. Nat Rev Neurol. 2012;8:487–97.
Diechmann MD, Campbell E, Coulter E, Paul L, Dalgas U, Hvid LG. Effects of exercise training on neurotrophic factors and subsequent neuroprotection in persons with multiple sclerosis—a systematic review and meta-analysis. Brain Sci. 2021;11:1499.
Ruiz-González D, Hernández-Martínez A, Valenzuela PL, Morales JS, Soriano-Maldonado A. Effects of physical exercise on plasma brain-derived neurotrophic factor in neurodegenerative disorders: a systematic review and meta-analysis of randomized controlled trials. Neurosci Biobehav Rev. 2021;128:394–405.
Taul-Madsen L, Connolly L, Dennett R, Freeman J, Dalgas U, Hvid LG. Is Aerobic or resistance training the most effective exercise modality for improving lower extremity physical function and perceived fatigue in people with multiple sclerosis? A systematic review and meta-analysis. Arch Phys Med Rehabil. 2021;102:2032–48.
Andreu-Caravaca L, Ramos-Campo DJ, Chung LH, Rubio-Arias JÁ. Dosage and effectiveness of aerobic training on cardiorespiratory fitness, functional capacity, balance, and fatigue in people with multiple sclerosis: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2021;102:1826–39.
Andreu-Caravaca L, Ramos-Campo DJ, Chung LH, Martínez-Rodríguez A, Rubio-Arias JÁ. Effects and optimal dosage of resistance training on strength, functional capacity, balance, general health perception, and fatigue in people with multiple sclerosis: a systematic review and meta-analysis. Disabil Rehabil. 2023;45:1595–607.
Harrison AM, Safari R, Mercer T, Picariello F, van der Linden ML, White C, et al. Which exercise and behavioural interventions show most promise for treating fatigue in multiple sclerosis? A network meta-analysis. Mult Scler. 2021;27:1657–78.
Moss-Morris R, Harrison AM, Safari R, Norton S, van der Linden ML, Picariello F, et al. Which behavioural and exercise interventions targeting fatigue show the most promise in multiple sclerosis? A systematic review with narrative synthesis and meta-analysis. Behav Res Ther. 2021;137: 103464.
Torres-Costoso A, Martínez-Vizcaíno V, Reina-Gutiérrez S, Álvarez-Bueno C, Guzmán-Pavón MJ, Pozuelo-Carrascosa DP, et al. Effect of exercise on fatigue in multiple sclerosis: a network meta-analysis comparing different types of exercise. Arch Phys Med Rehabil. 2022;103:970–87.
Ensari I, Motl RW, Pilutti LA. Exercise training improves depressive symptoms in people with multiple sclerosis: results of a meta-analysis. J Psychosom Res. 2014;76:465–71.
Dalgas U, Stenager E, Sloth M, Stenager E. The effect of exercise on depressive symptoms in multiple sclerosis based on a meta-analysis and critical review of the literature. Eur J Neurol. 2015;22:443-e34.
Dauwan M, Begemann MJH, Slot MIE, Lee EHM, Scheltens P, Sommer IEC. Physical exercise improves quality of life, depressive symptoms, and cognition across chronic brain disorders: a transdiagnostic systematic review and meta-analysis of randomized controlled trials. J Neurol. 2021;268:1222–46.
Gharakhanlou R, Wesselmann L, Rademacher A, Lampit A, Negaresh R, Kaviani M, et al. Exercise training and cognitive performance in persons with multiple sclerosis: a systematic review and multilevel meta-analysis of clinical trials. Mult Scler. 2021;27:1977–93.
Reina-Gutiérrez S, Meseguer-Henarejos AB, Torres-Costoso A, Álvarez-Bueno C, Cavero-Redondo I, Núñez de Arenas-Arroyo S, et al. Effect of different types of exercise on fitness in people with multiple sclerosis: a network meta-analysis. Scand J Med Sci Sports. 2023;33:1916–28.
Flores VA, Šilić P, DuBose NG, Zheng P, Jeng B, Motl RW. Effects of aerobic, resistance, and combined exercise training on health-related quality of life in multiple sclerosis: systematic review and meta-analysis. Mult Scler Relat Disord. 2023;75: 104746.
Edwards T, Michelsen AS, Fakolade AO, Dalgas U, Pilutti LA. Exercise training improves participation in persons with multiple sclerosis: a systematic review and meta-analysis. J Sport Health Sci. 2022;11:393–402.
Pilutti LA, Platta ME, Motl RW, et al. The safety of exercise training in multiple sclerosis: a systematic review. J Neurol Sci. 2014;343:3–7.
Learmonth YC, Pilutti LA, Herring MP, Motl RW, Chan B, et al. Safety of exercise training in multiple sclerosis: a protocol for an updated systematic review and meta-analysis. Syst Rev. 2021;10:208.
Learmonth YC, Herring MP, Russel DI, Pilutti LA, Day S, Marck CH, et al. Safety of exercise training in multiple sclerosis: an updated systematic review and meta-analysis. Mult Scler (in press).
Motl RW, Casey B, Learmonth YC, et al. The MoXFo initiative—adherence: exercise adherence, compliance, and sustainability among people with multiple sclerosis: an overview and roadmap for research. Mult Scler. 2023;29:1595–603.
Motl RW, Russel DI, Pilutti LA, et al. Drop-out, adherence, and compliance in randomized controlled trials of exercise training in multiple sclerosis: short report. Mult Scler. 2024;30:605–11.
Latimer-Cheung AE, Pilutti LA, Hicks AL, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94:1800–28.
Latimer-Cheung AE, Martin Ginis KA, Hicks AL, et al. Development of evidence-informed physical activity guidelines for adults with multiple sclerosis. Arch Phys Med Rehabil. 2013;94:1829–36.
Kim Y, Lai B, Mehta T, et al. Exercise training guidelines for multiple sclerosis, stroke, and Parkinson disease: rapid review and synthesis. Am J Phys Med Rehabil. 2019;98:613–21.
Baker M. 1,500 scientists lift the lid on reproducibility. Nature. 2016;533:452–4.
Ioannidis JPA. Why most published research findings are false. PLoS Med. 2005;2: e124.
Bamman MM, Cutter GR, Brienza DM, et al. Medical rehabilitation: guidelines to advance the field with high-impact clinical trials. Arch Phys Med Rehabil. 2018;99:2637–48.
Learmonth YC, Motl RW. Important considerations for feasibility studies in physical activity research involving persons with multiple sclerosis: a scoping systematic review and case study. Pilot Feasibilty Stud. 2017;4:1.
Bamman MM, Cooper DM, Booth FW, et al. Exercise biology and medicine: innovative research to improve global health. Mayo Clin Proc. 2014;89:148–53.
Herring MP, Fleming KM, Hayes SP, et al. Moderators of exercise effects on depressive symptoms in multiple sclerosis: a meta-regression. Am J Prev Med. 2017;53:508–18.
Baird JF, Motl RW. Response heterogeneity with exercise training and physical activity interventions among persons with multiple sclerosis. Neurorehabil Neural Repair. 2019;33:3–14.
Erickson ML, Allen JM, Beavers DP, et al. Understanding heterogeneity of responses to, and optimizing clinical efficacy of, exercise training in older adults: NIH NIA Workshop summary. GeroScience. 2023;45:569–89.
Konig IR, Fuchs O, Hansen G, et al. What is precision medicine? Eur Respir J. 2017;50:1700391.
DuBose NG, DeJonge SR, Jeng B, et al. Vascular dysfunction in multiple sclerosis: scoping review of current evidence for informing future research directions. Mult Scler Relat Disord. 2023;78: 104936.
Fletcher GF, Balady G, Blair SN, et al. Statement on exercise: benefits and recommendations for physical activity programs for all Americans. Circulation. 1996;94:857–62.
Motl RW, Sandroff BM. Physical exercise in multiple sclerosis in not just a symptomatic therapy: it has a disease-modifying effect—yes. Mult Scler. 2022;28:859–61.
Sandroff BM, Motl RW, Salter A. Focusing on neural mechanisms of exercise training benefits in multiple sclerosis. Mult Scler Relat Disord. 2024;86: 105633.
Hittle M, Culpepper WJ, Langer-Gould A, et al. Population-based estimates for the prevalence of multiple sclerosis in the United States by race, ethnicity, age, sex, and geographic region. JAMA Neurol. 2023;80:693–701.
Lai B, Cederberg K, Vanderbom KA, et al. Characteristics of adults with neurologic disability recruited for exercise trials: a secondary analysis. Adapt Phys Activ Q. 2018;35:476–97.
Motl RW, Cutter G, Bamman MM, et al. The importance and opportunity for healthy aging through lifestyle, behavioral medicine among older adults with multiple sclerosis: the case based on physical activity. Curr Treat Options Neurol. 2021;23:23.
Motl RW, Sandroff BM, Kwakkel G, et al. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017;16:848–56.
Feinstein A, Amato MP, Brichetto G, et al. Cognitive rehabilitation and aerobic exercise for cognitive impairment in people with progressive multiple sclerosis (CogEx): a randomized, blinded, sham-controlled trial. Lancet Neurol. 2023;22:912–24.
Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of diet on fatigue and quality of life in multiple sclerosis: a systematic review and network meta-analysis of randomized trials. Neurology. 2023;100:e357–66.
Benito-Leon J. Physical activity in multiple sclerosis: the missing prescription. Neuroepidemiology. 2011;36:192–3.
Acknowledgements
We thank the participants who volunteered for the studies reviewed in this paper.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
Robert W. Motl was the main author responsible for the concept and design of the paper and drafting the manuscript. Lara A. Pilutti refined the concept and design of the paper, and critical reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Robert W. Motl and Lara A. Pilutti have nothing to disclose.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Motl, R.W., Pilutti, L.A. Advancements and Challenges in Exercise Training for Multiple Sclerosis: Comprehensive Review and Future Directions for Randomized Controlled Trials. Neurol Ther (2024). https://doi.org/10.1007/s40120-024-00656-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40120-024-00656-z