Abstract
Introduction
Myasthenia gravis (MG) has a negative impact on patients’ health-related quality of life; however, many clinicians do not fully understand their patients’ lived experience of the disease. To understand the actual conditions of patients with MG and clarify the problems they perceive, we conducted a survey to evaluate the effects of the disease on patients’ daily life and work.
Methods
A questionnaire-based, qualitative, cross-sectional, non-interventional survey was conducted in Japan between April and May 2022 in patients with MG who were receiving regular outpatient treatment. The questionnaire included items regarding the patients’ disease characteristics and experience, satisfaction with life, current treatment status, and treatment satisfaction.
Results
In total, 452 patients were included in the survey population (66.6% aged ≥ 60 years; 64.6% with MG disease duration ≥ 10 years; 76.6% acetylcholine receptor [AChR] autoantibody positive). The symptoms of MG had a significant impact on the patients’ daily lives, with the most common symptoms being fatigability (74.8%), ptosis (59.7%), diplopia (54.2%), and weakness in the arms and/or legs (50.9%). Patients commonly identified exercise (73.7%), work 68.0%), hobbies (60.4%), travel (60.0%), and socializing with friends (59.7%) as being difficult to perform, with approximately 50% of patients reporting that hospitalization sometimes interfered with their ability to work. In total, 27.2% of patients were dissatisfied with life, with the highest rates of dissatisfaction among patients who were either positive for muscle-specific kinase (MuSK) autoantibodies or seronegative for both AChR and MuSK autoantibodies.
Conclusion
In Japanese patients with MG, over 25% are dissatisfied with life, indicating several unmet needs in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Understanding the impact of myasthenia gravis (MG) on patients’ quality of life may help bridge the gap between healthcare professionals and their patients in perceptions of MG and improve overall patient care in Japan |
This survey evaluated the effects of MG on Japanese patients’ daily life and work to understand their actual conditions and clarify the perceived problems |
What was learned from this study? |
There were several unmet needs among Japanese patients with MG, with symptoms having a significant impact on patients’ daily lives, including their ability to exercise, work, and socialize with friends |
Many patients reported difficulties with making people around them understand their disease, indicating a need to raise awareness of the symptoms of MG and their impact on the daily lives of these patients |
In total, 27.2% of patients were dissatisfied with their life, with higher rates of dissatisfaction among patients who were positive for muscle-specific kinase (MuSK) autoantibodies or double seronegative for acetylcholine receptor and MuSK autoantibodies |
Introduction
Myasthenia gravis (MG) is a rare, chronic, autoimmune, neuromuscular disease that is characterized by fluctuating symptoms of fatigue and weakness in the ocular, bulbar, limb, and respiratory muscles [1, 2]. It was designated as an intractable disease by the Ministry of Health, Labour, and Welfare of Japan in 1972; therefore, MG requires continuous research and public support for patients’ welfare [3]. According to a nationwide epidemiological survey, the prevalence of MG was 23.1 cases per 100,000 in Japan in 2017, which was double that recorded in 2006 [3].
MG can develop at any age, but symptoms often emerge at a younger age in women (< 40 years) and at an older age in men (> 60 years) [4]. Approximately 15% of patients with MG have only ocular symptoms (e.g., ptosis [drooping eyelids] and/or diplopia [double vision]), whereas approximately 85% have more generalized MG symptoms, including weakness in the face, neck, hands, and/or limbs [4, 5]. Based on the clinical features and severity, the Myasthenia Gravis Foundation of America (MGFA) clinical classification has five classes (Class I–V), with two further subclassifications in Classes II, III, and IV [1]. According to the MGFA clinical classification, Class I is characterized by ocular symptoms, Classes II, III, and IV by mild, moderate, and severe weakness, respectively, mainly affecting limb and/or axial muscles (Classes IIa, IIIa, or IVa) or oropharyngeal and/or respiratory muscles (Classes IIb, IIIb, or IVb), and Class V is defined by the need for intubation (with or without mechanical ventilation) [1].
The etiology of MG involves the binding of autoantibodies to post-synaptic membrane receptors (mainly acetylcholine receptors [AChR]) at neuromuscular junctions, which prevents the muscle fibers from contracting and causes muscle weakness [5]. Although these autoantibodies are most often against AChR (in ~ 80% of patients), autoantibodies against other proteins, including muscle-specific kinase (MuSK) or lipoprotein-related peptide (LRP4), also can impair synaptic transmission at neuromuscular junctions [5, 6]. Around 30–40% of AChR autoantibody-seronegative patients have MuSK autoantibodies, and 13–18% of patients who are seronegative for AChR and MuSK autoantibodies (i.e., double seronegative) have LRP4 autoantibodies [7]. Predisposing genetic factors, as well as some environmental factors, are known to play a role in triggering MG [5], and there is no known cure or prevention measure [5, 8].
The current medications for MG mostly focus on managing symptoms (e.g., acetylcholinesterase inhibitors) or providing non-specific chronic immunosuppression (e.g., corticosteroids and nonsteroidal immunosuppressants) [5, 8]. In the previous nationwide epidemiology study, Japanese patients with AChR antibody-positive MG were frequently prescribed acetylcholinesterase inhibitors, corticosteroids, and calcineurin inhibitors, while intravenous immunoglobulin (IVIg) and plasmapheresis were mainly used in those with MuSK antibody-positive disease [3]. Molecular-targeted treatments, including the neonatal Fc receptor inhibitors efgartigimod and rozanolixizumab [9, 10] and the complement C5 inhibitors eculizumab and ravulizumab [11, 12], are also available for treatment of patients with refractory symptoms.
MG has a negative impact on patients’ health-related quality of life (HRQoL), affecting physical and social functioning, as well as mental and emotional health [2, 8, 13, 14]. Furthermore, common comorbidities, such as dyslipidemia, diabetes, and hypertension, combined with the adverse effects of their associated treatments, may add to the disease burden [8]. The symptoms of MG are well known, and ongoing clinical studies are underway to better understand and address the physiological manifestations of the disease; however, there is a lack of understanding among clinicians about the patients’ lived experience of MG, which is not routinely discussed in clinical practice [4, 8]. This information may help clinicians to better understand which MG symptoms are most bothersome to patients, the impact of the disease on their daily activities, social relationships, and work, and their treatment goals [4]. This may also help bridge the gap in perceptions of MG between the healthcare providers (which are based on objective clinical data) and patients (which are based on their subjective everyday experiences), thereby helping to improve overall patient care [8].
Patients with MG often have difficulty obtaining long-term remission, and many experience difficulties with their social activities. In MG Awareness Month (June), argenx Japan K.K. organizes programs to create awareness about the disease and the challenges faced by those diagnosed with MG. As part of these programs, argenx Japan K.K. conducted a survey of Japanese patients with MG to evaluate the effects of the disease on patients’ daily life and work, with the aim of understanding the actual conditions of patients with MG and clarifying the problems they perceive. The current article reports the findings from this survey.
Methods
Survey Design and Population
This questionnaire-based, qualitative, cross-sectional, non-interventional survey of patients with MG was conducted in Japan between April 20 and May 8, 2022. Patients who were diagnosed with MG and undergoing regular outpatient treatment in Japan were eligible to participate. Participants were recruited through two MG patient advocacy organizations, Japan MG Association (JMGA) and MG Japan (a non-profit organization of individuals with MG). Data were collected online or via standard postal mail, keeping participants’ information/identity anonymous.
The survey was conducted in accordance with the 1964 Declaration of Helsinki. We did not obtain approval from an ethics committee/institutional review board, because this survey did not require ethics committee approval for the following reasons: (1) the survey did not involve an investigation of clinical outcomes with any intervention; (2) no identifying information was included in this manuscript; (3) participants were fully informed of the research purpose, provided consent to participate, and agreed for their data to be published; (4) this survey was approved by argenx.
Questionnaire and Outcomes
The questionnaire included items regarding the patients’ demographics and other disease characteristics; the impact of the disease on their daily activities, work, and social life/interactions; the ease of communication about the disease with others; their current satisfaction with life; treatment status and goals; and current satisfaction with MG treatment (Appendix 1). Each item in the questionnaire had a checkbox option, with the option to answer it as a single- or multiple-choice question.
Regarding the disease characteristics, patients were asked about their current symptoms as well as the three most bothersome symptoms, duration of the disease, MGFA clinical classification, autoantibody status (i.e., autoantibodies against AChR or MuSK, or double seronegative [defined as seronegative for both AChR and MuSK autoantibodies]), and comorbidities.
Regarding the treatment status, patients were asked about the frequency, duration, and burden of hospital visits and their current treatments for MG.
Statistical Analysis
The questionnaires were processed and analyzed using SAS software, version 9.4 (SAS Institute, Cary, NC, USA). Descriptive statistics (i.e., number and proportion of patients) were used to present the data, all of which were categorical values.
Results
Target Population
Questionnaire responses were collected from 464 patients with MG (390 from JMGA and 74 from MG Japan), of whom 452 patients met the inclusion criteria (Fig. 1). Twelve patients from JMGA who did not receive outpatient treatment were excluded from the survey.
The survey population included many older patients with long-term disease (Table 1). Approximately two-thirds of patients (n = 301; 66.6%) were aged ≥ 60 years, with 142 patients (31.4%) aged 60–69 years and 159 (35.2%) aged ≥ 70 years. Most patients (n = 366) were receiving treatment for concurrent conditions, most commonly hypertension (n = 169; 37.4%) and osteoporosis (n = 128; 28.3%). In total, 64.6% of the population (n = 292) had a MG disease duration of ≥ 10 years. Regarding the MGFA classification (which was known for 202 patients), 31 patients (15.3%) reported having Class I disease, 105 (52.0%) had Class II, 60 (29.7%) had Class III, five (2.5%) had Class IV, and one (0.5%) had Class V. MG autoantibody status (which was known in 368 patients) was AChR autoantibody-positive in 282 patients (76.6%), MuSK autoantibody-positive in 14 patients (3.8%), and double seronegative in 72 patients (19.6%).
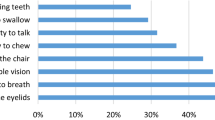
Patient Experience
The most common symptoms (reported by ≥ 50% of patients) were fatigability (74.8%), ptosis (59.7%), diplopia (54.2%), and weakness in the arms and/or legs (50.9%; Fig. 2). When patients were asked to identify their three most bothersome symptoms, the most commonly reported bothersome symptoms were fatigability (51.5%), diplopia (32.1%), ptosis (29.2%), and weakness in the arms and/or legs (26.3%; Fig. 2).
The most commonly identified activities that were difficult to perform (i.e., “unable to do” or “sometimes unable to do”) after developing MG were exercise (by 73.7% of patients) followed by work (68.0% when “not applicable” and “no response” were excluded), hobbies (60.4%), travel (60.0%), and going out with friends (59.7%; Fig. S1A).
Among the patients who were or had been employed or enrolled in school (n = 327), 50.4% reported being unable to work properly sometimes because of hospitalizations, and MG caused an increase in work/school absences in 46.7% of patients, reduction in working hours in 44.2%, moving to a different company/job in 36.1%, and quitting work/school in 39.6% (Fig. S1B). Almost one-quarter of patients (23.0%) reported that their colleagues or superiors did not understand the symptoms of their disease and thought they were “lazy.” Among all patients (n = 452), 41.6% reported that their friends and acquaintances thought they were “lazy,” and 32.1% stated that their family did not understand their disease and thought they were “lazy” (Fig. S1B).
When asked why patients found it difficult to talk about their disease with the general population, work supervisor(s), work colleagues, or friends, the most common reason was that patients felt that these people did not understand the seriousness of MG and its symptoms (50.3%, 51.0%, 49.0%, and 52.1%, respectively; Fig. S2). In contrast, when talking to a child or parent, the most common reason why patients found it difficult to talk about their disease was that the patient did not want to cause them to worry (67.9% and 60.4%, respectively). When talking to a spouse or partner, patients mainly felt that they did not understand the seriousness of the disease or symptoms (38.2%) or did not think they were interested or wanted to understand the disease (38.2%).
Satisfaction with Life
In total, 50.9% of the patients responded that they were satisfied with life overall, while 27.2% were dissatisfied (Fig. 3a). The proportion of patients who were satisfied with life was highest among patients with AChR autoantibody-positive disease (54.6%) and lowest among those who were positive for MuSK autoantibodies (28.6%); 34.7% of double seronegative patients reported being satisfied with life.
Satisfaction with life a in the total population and by autoantibody status, b by sex and age group (< 60 and ≥ 60 years), and c by Myasthenia Gravis Foundation of America classification. aNegative for both AChR and MuSK AAbs. AAb autoantibody, AChR acetylcholine receptor, MGFA Myasthenia Gravis Foundation of America, MuSK muscle-specific tyrosine kinase
When assessed by sex and age group, higher proportions of patients reported satisfaction with life among male versus female patients (58.2% vs 47.6%) and in those aged ≥ 60 versus < 60 years (54.2% vs 44.4%; Fig. 3b). When assessed by MGFA classification, the proportion who were satisfied with life decreased as disease severity increased, being highest (71.0%) in patients with Class I disease (Fig. 3c).
Treatment
Treatment Status and Goals
Current treatments included oral corticosteroids (in 71.7% of patients), immunosuppressants (60.2%), and acetylcholinesterase inhibitors (53.5%; Fig. S3).
When asked about their treatment status, 42.7% of patients reported that their current treatment controlled their symptoms so that their disease had no impact on their daily activities; 8.2% of patients had no MG symptoms at all and 34.5% had some remaining symptoms (Fig. S4). Among patients who reported an impact of disease on their daily activities despite treatment, 25.9% did not require any support, 16.6% required occasional support, 4.4% required some support at all times, 4.6% felt that there was a heavy burden of disease, and 5.3% reported adverse effects or burdens depending on treatment. In most patients (85.0%), the treatment goal was to be able to perform daily activities with no interference from symptoms (73.3%) or without any support (11.7%; Fig. S4).
When the patients were asked about the top three activities they wanted their treatment to allow them to perform without difficulty, the most common first responses were daily living activities (23.2%), exercise (12.4%), and work (11.5%; Fig. S5). However, after the second and third responses for each activity were included, the top priority became exercise (35.4%) followed by daily living activities (32.2%) and work (28.7%).
Burden of Hospital Visits
The frequency of hospital visits was once every 2 months in 38.9% of patients, once a month in 28.1%, and once every 3 months in 25.4% (Supplementary Table S1). The duration of hospital commute was most commonly ≥ 15 to < 30 min (in 24.1% of patients) followed by ≥ 1 to < 1.5 h (19.9%) and ≥ 30 to < 45 min (19.7%).
Regarding the burden of hospital visit (round trip to and from the hospital), 48.5% of patients responded that going to the hospital was either “somewhat burdensome” (29.4%), “burdensome” (13.3%), or “very burdensome” (5.8%), while 34.7% responded that it was not burdensome (Supplementary Table S2). Among patients who reported that the hospital visit was burdensome (n = 219), the most common duration of hospital commute (one way) was ≥ 1 to < 1.5 h (30.1%) followed by ≥ 30 to < 45 min (20.1%). In contrast, among those who reported that their hospital visit was not burdensome (n = 157), the most common hospital commute duration was ≥ 15 to < 30 min (37.6%) followed by < 15 min (27.4%).
Satisfaction with Treatment
When the patients were asked about their satisfaction with current treatment, 70.4% of the total population reported being satisfied with their current treatment (Fig. 4a). The proportion of patients who were satisfied with treatment was highest among patients who were positive for AChR autoantibodies (73.4%) and lowest in those with MuSK autoantibody-positive disease (42.8%). When assessed across age groups that included > 20 patients, the proportion of patients with treatment satisfaction was highest in those aged 60–69 years (77.5%) and lowest in those aged 30–39 years (51.9%; Fig. 4b). Of note, all patients aged 15–29 years (n = 7) reported being satisfied with treatment.
a Treatment satisfaction in the total population and by autoantibody status, b treatment satisfaction by age group (15–29, 30–39, 40–49, 50–59, 60–69, and ≥ 70 years), c quality of communication with attending physician in the total population and in patients with treatment dissatisfaction, and d patients’ evaluation of attending physician in the total population and in patients with treatment dissatisfaction. aNegative for both AChR and MuSK AAbs. AAb autoantibody, AChR acetylcholine receptor, MG myasthenia gravis, MuSK muscle-specific tyrosine kinase
Among patients with treatment dissatisfaction (n = 49), the proportion who were dissatisfied with the communication with their attending physician was 38.8% (vs 12.2% among all patients), while approximately one-quarter (26.5%) responded that their treatment had not been chosen in consultation with their physician or felt that they did not have a trusting relationship with their physician (Fig. 4c).
When patients were asked to evaluate their attending physician, 47.3–71.0% of the total population agreed with the statements regarding the abilities of their attending physicians to be knowledgeable and fully inform them of MG treatment options (including new treatments), provide sufficient information about MG, provide sufficient consultation time, clearly explain the adverse effects and goals of treatment, and be fully responsive to concerns and questions and make it easy to ask questions (Fig. 4d). In patients with treatment dissatisfaction, the proportion who disagreed with these statements (34.7–59.2%) was generally higher than in the total population (11.5–23.0%).
Discussion
This questionnaire-based survey of Japanese patients with MG found that 27.2% of the population was dissatisfied with life and 10.8% was dissatisfied with treatment. Compared with AChR autoantibody-positive patients, patients who were positive for MuSK autoantibodies and double seronegative patients had higher rates of life dissatisfaction and MuSK autoantibody-positive patients had higher rates of treatment dissatisfaction, which suggests that there is an unmet need for new treatments.
In this survey, patients reported that the symptoms of MG had a significant impact on their daily lives, with exercise, work, hobbies, travel, and going out with friends being commonly identified as activities that were difficult to perform. Consistent with previous studies [2, 4, 8, 14], the current survey found that the most common symptoms were fatigability, ptosis, diplopia, and weakness in the arms and legs; interestingly, these were also the most bothersome symptoms. Previous studies of patient-reported and registry data have shown that patients often experience impaired daily functions, even with only mild-to-moderate muscle weakness [15,16,17]. This may be because fatigability (i.e., including lack of energy, tiredness, and exhaustion), rather than muscle weakness, is one of the main drivers of overall impairment regarding the activities of daily living [18].
In the current survey, MG had a large impact on work or school, with 50.4% of the population reporting that hospitalization sometimes interfered with their ability to work effectively, 46.7% reporting an increased absence from work/school, and 44.2% reporting the need to work shorter hours. In addition, over one-third of the population had to change their company or switch career paths, or quit work or school because of MG. These observations are consistent with a previous report from Japan about the negative impact of MG on patients’ ability to work [19] as well as from studies conducted in Europe [20, 21], the USA [4, 22], and Australia [23]. These previous studies reported that MG has an adverse impact on employment, including reduced labor market participation, increased absenteeism and sick leave, unwilling job transfers, decrease in income, and limitations in work-related capabilities [4, 19,20,21,22,23]. A qualitative study from the US reported that, among working people with MG, treatments and hospitalizations led to them missing work [4], consistent with our findings that hospitalization sometimes negatively impacted the working lives of MG patients. These data suggest that there is a need for more treatments that can be administered in the outpatient setting, thereby reducing the need for hospital visits.
People with MG often have concerns that the emotional stress of their condition will affect their work or that the stress of their work will exacerbate their condition [8]. Therefore, it is important that employers and work colleagues are well informed about MG to create a work environment that fully accommodates the symptoms and needs of patients with MG [19]. In the current survey, the most common reason why patients expressed hesitation when talking about their disease at their workplace, with the general population, or their friends was because they felt that the other person would not understand the seriousness of the disease and symptoms. By comparison, when talking to a child or parent, patients felt uncomfortable talking about their disease because they did not want to worry their child or parent. Interestingly, a previous Taiwanese study has indicated that dedicated support from the spouse or family is important for patients with MG, allowing them to cope better with their symptoms [17].
In the current survey, 59.8% of patients reported that going out with friends was difficult, in line with previous studies that reported a substantial disease impact on patients’ social wellbeing [4, 19]. A previous US study found that some patients feel anxious at social gatherings because they are worried about being judged or pitied for their condition or because they fear that family and friends will not understand how debilitating MG can be [4]. In a Japanese study, patients often reported feeling depressed because long-term treatment with high doses of oral corticosteroids had a negative effect on their mood and behavior as well as on their appearance [19].
In the current survey, female patients had higher rates of dissatisfaction with life compared with male patients (28.9% vs 23.4%). This is probably because female patients generally have more symptoms, more work limitations, and a poorer disease-specific HRQoL than males [14, 16, 20]. Female patients are also more likely than males to lose their job or not find a new one and to be absent from work for extended periods of time [20]. The proportion of patients who reported dissatisfaction with life was also higher in younger (aged < 60 years) versus older (aged ≥ 60 years) patients (35.8% vs 22.9%). This is in line with the findings of a patient-led analysis, in which people with MG (particularly younger patients) reported often feeling a sense of loss due to restrictions in activity and limited life choices [8]. The current study also found that levels of dissatisfaction with life tended to increase as MGFA Class increased. Consistent with this, previous studies have indicated that life dissatisfaction may be caused by increased disease severity and duration, the adverse effects of treatment, depression, fatigue, or reduced HRQoL [24, 25].
Regarding hospital visits, patients usually went to the hospital once every 2 months, and the duration of their hospital commute was usually ≥ 15 to < 30 min. Almost half of the population (48.5%) reported that the round trip to the hospital was burdensome. This burden appeared to be related to their distance from the hospital, with 50.2% of these patients having a one-way hospital commute duration of ≥ 30 to < 45 min or ≥ 1 to < 1.5 h, whereas 65.0% of patients who stated that their hospital visit was not burdensome had a one-way commute of < 15 min or ≥ 15 to < 30 min. These findings highlight the need for improved home self-care and long treatment intervals to decrease the need for hospital visits and to promote improved social life.
In the current survey, 70.4% of the total population reported being satisfied with their current treatment, with the lowest treatment satisfaction rates observed in patients with MuSK autoantibody-positive disease. This high rate of treatment satisfaction in the overall population may have been influenced by the fact that all patients were enrolled in MG patient advocacy organizations, had a long disease duration, and were familiar with existing treatments. Of note, patients aged 30–39, 40–49, and 50–59 years (i.e., the working population) had higher rates of dissatisfaction with treatment than older or younger patients, which suggests that a reduced ability to work may influence treatment dissatisfaction. Not surprisingly, the most common treatment goals of these patients were symptomatic relief and the ability to perform daily activities without any interference or the need for support. This is consistent with a previous US study, which found that symptom management (e.g., reduction in fatigue or weakness, achieving consistent control of disease manifestation, and remission/cure) and minimizing the impact of symptoms (e.g., reduction of emotional impact and return to normal life/activities) were the two main categories of treatment goals [4].
Among patients who were dissatisfied with treatment, the proportion who were dissatisfied with communication with their attending physician was higher than that reported in the total population. Furthermore, higher proportions of patients with treatment dissatisfaction felt that their physician did not fully inform them of new treatments, provide sufficient information about MG, or clearly explain the adverse effects of treatment. Indeed, treatment adverse effects are known to impose a considerable burden on daily lives of patients [8, 24]. In addition, some patients with MG have reported a sense of disconnect with their healthcare providers regarding their treatment goals and the treatment burden (including treatment of comorbidities) in terms of side effects and monitoring [8].
The main strength of this survey is the large number of participants. The limitations of this survey also need to be considered. All patients were from Japan, and this may affect the generalizability of the results to populations/ethnicities from other countries. In addition, all patients were members of patient advocacy organizations and were asked to participate, which might have introduced selection bias towards patients motivated to actively manage their MG and to participate in survey research. The survey population included a higher proportion of female than male respondents as well as a high proportion of older patients and individuals with concurrent chronic diseases, which may also have affected their HRQoL. We did not collect information about depression, which may also have affected some of the parameters evaluated in our survey. This was a close-ended survey, where patients had to choose from the options provided to them, and was not a validated questionnaire. Diagnoses and treatment types were patient reported and not confirmed by a clinician. However, in Japan, MG is diagnosed by confirming positive autoantibodies in addition to clinical symptoms and by confirming neuromuscular junction disorders by electrophysiology or edrophonium testing, even if negative. We therefore consider it unlikely that the cohort included patients who did not have a confirmed diagnosis of MG since we included only patients who answered, ‘yes’ to the question "Do you regularly visit a hospital or clinic for the treatment of myasthenia gravis now?". However, it is possible that recall bias may have affected the data relating to symptoms and treatment.
Conclusions
This questionnaire-based survey provided valuable insight into the experiences of Japanese patients with MG. In total, 27.2% of patients reported being dissatisfied with life, implying that there are several unmet needs in Japanese patients with MG. More effective treatments are needed that target broad MG serotypes, including patients who are positive for MuSK autoantibodies or seronegative for both AChR and MuSK autoantibodies. There is also a need for improved communication between physicians and patients to optimize treatment selection, including shared decision-making. These findings may increase our understanding of how patients perceive their burden of MG and their treatment goals, which will be essential for guiding patient-clinician interactions and improving patients’ HRQoL.
Data Availability
The datasets used and/or analyzed during the current survey are available from the corresponding author on reasonable request.
Change history
27 June 2024
The original online version of this article was revised to include the open access license statement.
25 June 2024
A Correction to this paper has been published: https://doi.org/10.1007/s40120-024-00639-0
References
Gwathmey KG, Burns TM. Myasthenia gravis. Semin Neurol. 2015;35:327–39.
Dewilde S, Philips G, Paci S, et al. Patient-reported burden of myasthenia gravis: baseline results of the international prospective, observational, longitudinal real-world digital study MyRealWorld-MG. BMJ Open. 2023;13: e066445.
Yoshikawa H, Adachi Y, Nakamura Y, et al. Two-step nationwide epidemiological survey of myasthenia gravis in Japan 2018. PLoS ONE. 2022;17: e0274161.
Jackson K, Parthan A, Lauher-Charest M, Broderick L, Law N, Barnett C. Understanding the symptom burden and impact of myasthenia gravis from the patient’s perspective: a qualitative study. Neurol Ther. 2023;12:107–28.
Gilhus NE, Tzartos S, Evoli A, Palace J, Burns TM, Verschuuren J. Myasthenia gravis. Nat Rev Dis Primers. 2019;5:30.
Gilhus NE, Verschuuren J, Hovland SIB, Simmonds H, Groot F, Palace J. Myasthenia gravis: do not forget the patient perspective. Neuromuscul Disord. 2021;31:1287–95.
Rivner MH, Pasnoor M, Dimachkie MM, Barohn RJ, Mei L. Muscle-specific tyrosine kinase and myasthenia gravis owing to other antibodies. Neurol Clin. 2018;36:293–310.
Law N, Davio K, Blunck M, Lobban D, Seddik K. The lived experience of myasthenia gravis: a patient-led analysis. Neurol Ther. 2021;10:1103–25.
Bril V, Druzdz A, Grosskreutz J, et al. Safety and efficacy of rozanolixizumab in patients with generalised myasthenia gravis (MycarinG): a randomised, double-blind, placebo-controlled, adaptive phase 3 study. Lancet Neurol. 2023;22:383–94.
Heo YA. Efgartigimod: first approval. Drugs. 2022;82:341–8.
Meisel A, Annane D, Vu T, et al. Long-term efficacy and safety of ravulizumab in adults with anti-acetylcholine receptor antibody-positive generalized myasthenia gravis: results from the phase 3 CHAMPION MG open-label extension. J Neurol. 2023;270:3862–75.
Murai H, Suzuki S, Hasebe M, Fukamizu Y, Rodrigues E, Utsugisawa K. Safety and effectiveness of eculizumab in Japanese patients with generalized myasthenia gravis: interim analysis of post-marketing surveillance. Ther Adv Neurol Disord. 2021;14:17562864211001996.
Szczudlik P, Sobieszczuk E, Szyluk B, Lipowska M, Kubiszewska J, Kostera-Pruszczyk A. Determinants of quality of life in myasthenia gravis patients. Front Neurol. 2020;11: 553626.
Lehnerer S, Jacobi J, Schilling R, et al. Burden of disease in myasthenia gravis: taking the patient’s perspective. J Neurol. 2022;269:3050–63.
Cutter G, Xin H, Aban I, et al. Cross-sectional analysis of the Myasthenia Gravis Patient Registry: disability and treatment. Muscle Nerve. 2019;60:707–15.
Dong D, Chong MKC, Wu Y, et al. Gender differences in quality of life among patients with myasthenia gravis in China. Health Qual Life Outcomes. 2020;18:296.
Chen YT, Shih FJ, Hayter M, Hou CC, Yeh JH. Experiences of living with myasthenia gravis: a qualitative study with Taiwanese people. J Neurosci Nurs. 2013;45:E3-10.
Barnett C, Bril V, Kapral M, Kulkarni A, Davis AM. A conceptual framework for evaluating impairments in myasthenia gravis. PLoS ONE. 2014;9: e98089.
Nagane Y, Murai H, Imai T, et al. Social disadvantages associated with myasthenia gravis and its treatment: a multicentre cross-sectional study. BMJ Open. 2017;7: e013278.
Frost A, Svendsen ML, Rahbek J, Stapelfeldt CM, Nielsen CV, Lund T. Labour market participation and sick leave among patients diagnosed with myasthenia gravis in Denmark 1997–2011: a Danish nationwide cohort study. BMC Neurol. 2016;16:224.
Twork S, Wiesmeth S, Klewer J, Pöhlau D, Kugler J. Quality of life and life circumstances in German myasthenia gravis patients. Health Qual Life Outcomes. 2010;8:129.
Harris L, Aban IB, Xin H, Cutter G. Employment in refractory myasthenia gravis: a Myasthenia Gravis Foundation of America Registry analysis. Muscle Nerve. 2019;60:700–6.
Blum S, Lee D, Gillis D, McEniery DF, Reddel S, McCombe P. Clinical features and impact of myasthenia gravis disease in Australian patients. J Clin Neurosci. 2015;22:1164–9.
Bacci ED, Coyne KS, Poon JL, Harris L, Boscoe AN. Understanding side effects of therapy for myasthenia gravis and their impact on daily life. BMC Neurol. 2019;19:335.
Andersen LK, Jakobsson AS, Revsbech KL, Vissing J. Causes of symptom dissatisfaction in patients with generalized myasthenia gravis. J Neurol. 2022;269:3086–93.
Acknowledgements
The authors thank JMGA and MG Japan and the patients who participated in this survey.
Medical Writing and Editorial Assistance
The authors thank Sarah Greig, PhD, CMPP, of inScience Communications, Springer Healthcare, who wrote the outline and subsequent drafts of this manuscript, and Catherine Rees, who provided editorial assistance with post-submission revisions on behalf of Springer Healthcare. This medical writing assistance was funded by argenx Japan K.K.
Funding
This survey and development of the manuscript was supported by argenx Japan K.K, who also paid the journal’s Rapid Service Fee. The funder was involved in the design, interpretation of aggregate results, manuscript reviews, and the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
Conception or design of the survey: Naoki Kawaguchi, Koichi Tsuda, Nozomu Tanaka, Daisuke Harada; Data acquisition: Daisuke Harada; Data analysis: Koichi Tsuda, Rene Kerstens; Data interpretation: Naoki Kawaguchi, Koichi Tsuda, Nozomu Tanaka, Daisuke Harada, Rene Kerstens; Writing (drafting/revising): Naoki Kawaguchi, Koichi Tsuda, Nozomu Tanaka, Daisuke Harada, Rene Kerstens. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
Naoki Kawaguchi has no conflicts of interest to disclose. Rene Kerstens is an employee of argenx. Koichi Tsuda, Nozomu Tanaka, and Daisuke Harada are employees of argenx Japan K.K.
Ethical Approval
We did not obtain approval from an ethics committee/institutional review board, because this survey did not require ethics committee approval for the following reasons: (1) the survey did not involve an investigation of clinical outcomes with any intervention; (2) no identifying information was included in this manuscript; (3) participants were fully informed of the research purpose, provided consent to participate, and agreed for their data to be published; and (4) this survey was approved by argenx.
Additional information
The original online version of this article was revised to replace Figure 4b.
Prior Presentation: The data in this article have previously been presented at the 64th Annual Meeting of the Japanese Society of Neurology, held on 31 May to 3 June 2023, in Chiba, Japan.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kawaguchi, N., Tsuda, K., Tanaka, N. et al. Myasthenia Gravis Disease Burden and Its Impact on Satisfaction with Life: A Qualitative Survey of Patients’ Perspectives in Japan. Neurol Ther 13, 1099–1113 (2024). https://doi.org/10.1007/s40120-024-00617-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-024-00617-6