Abstract
Introduction
Alzheimer’s disease (AD) is a chronic neurodegenerative disorder associated with a high burden of illness. New therapies under development include agents that target amyloid-beta (Aβ), a key component in AD pathogenesis. Understanding the decision-making process for new AD drugs would help determine if such therapies should be adopted by society. Multicriteria decision analysis (MCDA) was applied to three key stakeholder groups to assess treatment alternatives for AD based on a multitude of decision trade-offs covering main components of care.
Methods
AD caregivers (n = 117), neurologists (n = 90), and payors (n = 90) from the USA received an online survey. The decision problem was broken down into four decision criterion and 12 subcriteria for two treatment scenarios: an Aβ-targeted therapy vs. the standard of care (SOC). Respondents were asked to indicate how much they preferred one option over another on a scale from 1 (equal preference) to 9 (high preference) based on each criterion and subcriterion. The decision criteria and subcriteria were weighted and presented as partial utility scores (pUS), with higher scores suggesting an increased preference for that decision-making component.
Results
Caregivers and payors applied the highest value to need for intervention (mean pUS = 0.303 and 0.259) and clinical outcomes (mean pUS = 0.286 and 0.377). In contrast, neurologists placed the highest value on clinical outcomes and types of benefits (mean pUS = 0.436 and 0.248). When decision subcriteria were examined, efficacy (mean pUS = 0.115, 0.219, and 0.166) and the type of patient benefits (mean pUS = 0.135, 0.178, and 0.126) were among the most valued by caregivers, neurologists, and payors.
Conclusion
All groups placed the highest value on drug efficacy and types of benefit derived by patients. In contrast, cost implications were among the least important aspects in their decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Monoclonal antibody therapies targeting amyloid-beta to delay Alzheimer’s disease (AD) progression represent an active area of drug development, with several trials nearing readout in late 2022 and early 2023 |
Given the multiple product attributes that require consideration in health policy decision-making, there is merit in understanding the values and preferences for drug adoption by key stakeholders involved in the care of patients with AD |
Multicriteria decision analysis was used to determine the relative importance of key therapeutic attributes of Aβ therapies for early-stage AD |
Caregivers, neurologists, and payors placed the highest value on drug efficacy and the types of benefit derived by patients as being the most relevant product attributes. In contrast, all three groups considered cost implications to be among the least important factors in their decision. In addition, more caregivers than neurologists or payors preferred an amyloid-beta (Aβ)-targeted therapy over the standard of care, likely driven by their perceived need for a new intervention |
Health policy and drug formulary committees need to consider these outcomes and the relative weighting of the different components of new AD treatments in deciding which drugs to make available to patients |
Introduction
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder and the most common form of dementia, being responsible for approximately 80% of all diagnoses [1]. The onset of AD is characterized by memory loss, struggles with thinking, speech, and problem-solving skills [1, 2]. AD has a high prevalence, with approximately 45 million cases worldwide [3]. Given the aging global population and increases in life expectancy, the number of cases is expected to triple by 2050 [2, 3]. Therefore, AD is one of the most significant global health challenges faced by governments. Indeed, the socioeconomic impact associated with AD is staggering. In the USA alone, the total direct and indirect costs were estimated to be US $305 billion annually, with costs expected to more than double by 2050 [4, 5].
Patients with newly diagnosed AD typically progress through three stages: mild, moderate to severe disease. Each successive stage is characterized by worsening cognitive impairment, which presents as memory loss, speech difficulties, and disorientation in space and time [1, 6]. Furthermore, patients also display a decline in physical performance such as apraxia; impaired body coordination with frequent falls and uncontrolled sphincters [1, 7]. As patients transition through the different stages of the disease, there is also a steady decline in quality of life (QOL) and general well-being [7]. The impact is not only felt by patients. Family members and caregivers are also affected. It has been reported that caregiver’s supporting a patient with more memory and behavioral problems have greater stress, depression, and anxiety compared to those supporting patients with less advanced disease [8].
Given the severe consequences of AD for both patients and caregivers, research evaluating primary prevention has identified several modifiable risk factors. These include diabetes, smoking, depression, intellectual inactivity, a sedentary lifestyle, and a poor diet [2]. In cases where early AD is diagnosed, one focus of drug development is monoclonal antibody (mAb) therapies targeting amyloid-beta (Aβ) to delay disease progression. Unfortunately, trials with the first-generation agents yielded disappointing results, indicating that most patients upon diagnosis may have exceeded the therapeutic window to delay disease progression [9]. Notwithstanding, the knowledge gained from these early clinical trials has informed the development of the next-generation mAbs.
In 2021, the US Food and Drug Administration (FDA) approved aducanumab, the first mAb targeting Aβ and the first drug to be approved for AD in nearly 20 years [10]. However conflicting clinical trial results, safety concerns in terms of vasogenic edema and cortical microhemorrhages as well as the high drug cost dampened the initial enthusiasm [11, 12]. There are at least three other agents targeting Aβ in clinical development (i.e., donanemab, gantenerumab, and lecanemab) [13]. Therefore, it is possible that several new targeted agents will be available for patients with AD to intervene in the disease in its early stages. To learn from the controversy following the authorization of aducanumab and apply the information towards future drug approvals, there is merit in understanding the values and viewpoints of the various stakeholders involved in the care of patients with AD. Such insights will help inform health policy decision-making in the provision of optimal pharmacotherapy for AD. Stated differently, important insights can be gained if we can identify and quantify the key factors in the selection of new treatment for AD used by individuals involved in the care of patients.
Given the difficulties in weighting the different attributes of a new treatment, challenges in clinical and reimbursement decision-making arise. Fortunately, there are a broad range of techniques under the umbrella of multicriteria decision analysis (MCDA) that can be used to inform and make the decision-making process more transparent. Initially used in the operations research, MCDA is a methodology that facilitates the complex appraisal of treatment alternatives based on a multitude of decision trade-offs and has now been applied to health care to assist in regulatory and reimbursement decisions [14,15,16]. To our knowledge, MCDA has not been applied to therapeutic decision-making for early AD. In this study, the MCDA process was used to assess how three key stakeholder groups consisting of patient caregivers, neurologists, and payors determine the relative importance of therapeutic attributes of Aβ therapies for early-stage AD using a broad set of decision criteria that include clinical, health economic, and societal values.
Methods
Designing a Multicriteria Decision Analysis
MCDA is a quantitative method used to evaluate the various criteria in decision-making that may be in conflict [14, 17, 18]. The MCDA process requires the decision problem to be broken down into more comprehensible parts [15]. Each part is presented to the key stakeholders and their preferences are analyzed, a weighing for each part is estimated, and the final outcomes are integrated to generate a final meaningful solution. As an illustration, if a person is considering selecting an automobile between several choices, the relevant attributes may include safety, comfort, affordability, color, and fuel efficiency. The steps in applying MCDA to a decision situation consist of problem identification, measuring the opinions or preferences of the individual or group, presenting the decision alternatives, evaluating the decision criteria, and then presenting the outcomes associated with each alternative. When used at the group level, MCDA can facilitate discussion within a group about the decision to be made in a way that allows them to consider the values that each member deems to be important. The methodology also provides an opportunity for group members to discuss complex trade-offs that are often made between alternative courses of action [14, 15]. To collect information required to conduct an MCDA at the group level, survey methodology is typically used on a sample of respondents faced with the decision problem [14].
Target Population
The primary data for the MCDA were obtained via an online survey. The survey population consisted of three samples from the USA: caregivers who care for family members or friends with AD, neurologists who actively treat patients with AD, and payors who have worked at a health insurance plan within the past 2 years. Sampling of these individuals was achieved from a database of neurologists, AD caregivers, and payers managed by a third-party vender. Invitations were sent out to group members to participate in the survey. Respondents were given background information on the intent of the study, and all provided written informed consent to participate. Respondents were also informed that complete confidentiality would be maintained, and their personal information would not appear in any study report or publication. The study protocol received ethical approval by Pearl IRB (Indianapolis, IN; IRB protocol # 22-BCGR-101). The study was completed in accordance with the declaration of Helsinki. Respondents were provided background information on the intent of the study, and all provided written informed consent to participate.
Questionnaire Development and Administration of the MCDA
The first part of questionnaire captured respondent demographic data. Information on caregivers consisted of sex, age group, race, ethnicity, education, annual household income, and caregiving experience (e.g., AD stage of patients under care, type of care provided, duration and frequency of caregiving, cohabitation with patients). Demographic data on the neurologists’ sample consisted of practice setting, years of practice, volumes of patients with AD managed, and prior use of aducanumab. For the payer sample, demographic data collection included type of insurance plan, whether it was regional or national, plan size, number of patients with AD in health plan, and current coverage of aducanumab.
The second part of the questionnaire collected data reflecting individual preferences for key therapeutic attributes in the care of patients with AD. The MCDA process requires the selection of decision criteria, the application of preference scores to the alternatives, weighting the criteria, and calculating aggregate scores [19]. There are several methods for scoring and weighting such as conjoint analysis, best–worst scaling, point allocation, and analytic hierarchy process (AHP). While no one method is clearly superior, AHP was selected because it allows the use of an explicit hierarchy to organize decision criteria, uses pairwise comparisons to assess decision criteria against one another, and employs a uniform 1–9 scale for both the scoring and weighting tasks [20, 21].
The AHP contained within the questionnaire had one decision objective, four decision criteria, and 12 decision subcriteria for two alternative scenarios: an Aβ-targeted therapy and the standard of care (SOC) (Fig. 1). The objective was to explore whether society should offer an Aβ-targeted therapy to treat early AD (i.e., patients with mild cognitive impairment or mild AD dementia). Respondents were asked to answer the survey questions from a societal perspective and not necessarily from their existing organizational view or practice. The decision (sub)criteria were selected and defined (see Supplemental Material S1) on the basis of the EVIDEM framework because it encapsulates a wide range of considerations in healthcare decision-making, structures them into largely independent clusters, and has been empirically tested and broadly applied in real-world decision-making [18, 22].
At the beginning of the survey, introductory content that briefly described the disease process, the Aβ-targeted therapies under development, and the MCDA structure were presented to each respondent. Preference scores using pairwise comparisons were then obtained between the alternative scenarios on each criterion (12 pairwise comparisons), followed by subcriteria within each criterion (13 pairwise comparisons), and lastly between criteria (six pairwise comparisons). Respondents were presented with brief evidence summaries for each comparison between the alternatives and were asked to indicate how much they prefer one alternative over another on a scale 1 (equal preference) to 9 (extremely high preference). Participants were then asked to assess the alternatives before comparing decision (sub)criteria because knowledge of the alternatives may help contextualize the (sub)criteria defined in the survey. Finally, because the need-for-intervention criterion and its subcriteria apply equally to both alternatives, their importance set to be equal a priori.
A utility is a preference-based score between 0 and 1, with higher scores indicating greater preferences for that decision criterion. Each criterion and subcriterion evaluated by the MCDA was presented as a partial utility, where a larger value indicated a greater mean preference by the sample of respondents being evaluated [14, 18]. The overall utility score consisted of the sum of all the criteria and subcritera and it totaled one.
Statistical Analysis
Respondent characteristics were summarized descriptively as means, medians, or proportions, with appropriate levels of variance (i.e., standard error (SE), standard deviation (SD) and 95% CI). The respondent data were analyzed to quantify preferences across decision subcriteria, decision criterion and subcriterion weights, and overall preference scores for each alternative. At the respondent level, alternative preference and decision weights were calculated as the principal right eigenvectors of corresponding comparison matrices, where the overall preference score was calculated as the weighted sum of alternative preference by decision weights [23]. At the group level, aggregated preference for each respondent group was derived from similar matrix calculations but based on the geometric means of all individual pairwise comparisons. Geometric means were chosen for data aggregation because they are recommended when reflecting preferences of the group as a whole and are less vulnerable to outliers than arithmetic means in cases of non-perfectly consistent judgments [24]. Group-level preference and the interquartile range of respondent-level preferences were reported, as well as the consistency index and consistency ratio (CR) for group-level decision (sub)criterion weights [23].
In the primary analysis, all respondents were included except the top decile whose time taken to complete the survey was less than 5 min, suggesting inadequate attention. In the AHP, the judgment CR is an index of the consistency of judgements across all pairwise comparisons [25]. A sensitivity analysis was conducted where only respondents whose overall judgment CR was less than 0.2 or those who self-reported the survey as “very easy” were included. These sensitivity analyses assessed the robustness of decision (sub)criterion weights in the main analyses with respect to individual judgment consistency and comprehension of MCDA. Of note, CR < 0.2 is used to indicate acceptable judgment consistency in the context of moderated group decision-making [24], but the optimal threshold of CR is unclear in the setting of a self-administered online survey designed to elicit diverse preferences. Since there was large variation in the decision weights observed in both the main and sensitivity analysis, and AHP group consensus indicator “S”, was calculated on the basis on Shannon entropy [26, 27], where S ≤ 50% indicates very low consensus and S ≥ 85% indicates very high consensus. Given the low group consensus, we additionally reported respondent-level rank distributions of decision criteria based on ordinal levels of decision weights in each comparison matrix and contributions of individual decision subcriteria to overall treatment preference in subgroups that favored SOC over Aβ-targeted therapy overall. All the statistical analyses were performed using Stata, release 16.0 (Stata Corp., College Station, Texas, USA).
Results
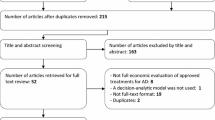
A sample of 188 caregivers, 140 neurologists, and 186 caregivers were approached and 130, 100, and 100 provided consent to participate in the study. Of the caregivers, neurologists, and payers who completed the online survey, 43, 10, and 10 were excluded, respectively, from the analyses because of inadequate attention characterized by completing the survey in less than 5 min. No difference in respondent characteristics was observed between the initial sample and the retained sample (p > 0.05 for all chi-square tests by respondent characteristics, data not shown).
Demographic characteristics within the three respondent groups are presented in Table 1. In the caregiver sample, approximately 53.0% of the sample was female, 48.8% was older than 45 years of age, and there was comparable regional distribution across the country (Table 1). The majority of the caregiver sample was white (77.8%), 53.9% were married, and 28.8% had an annual household income of $100,000 or more. Furthermore, 59% of caregiver respondents had at least a bachelor’s degree and 58 of 117 (49.6%) had experience as a healthcare professional. The majority of the caregiver cohort (95.7%) were a family member to the patient(s) with AD and 84 of 117 respondents (71.8%) indicated that at least one of the patients in their care had moderate or severe disease (Table 1). The type of care provided was broad, from self-care activities to management of behavioral symptoms. Overall, 44.4% of caregivers provided support for a patient with AD six or more times per week and 64.9% of the sample had been doing this for at least 3 years (Table 1). Among neurologist respondents, 41.1% practiced in an academic center, 20.0% in a rural setting, 44.4% had over 20 years of practice experience, 44.4% had treated over 100 patients with AD within the last 12 months, and 21.1% had experience using aducanumab (Table 1). Finally in the payor sample, 82.2% were involved in a Medicare medical plan, 51.1% worked in plans that provided national insurance coverage, and 36.7% in plans that covered over 500,000 people. In addition, 46.7% of respondents also indicated their plans cover aducanumab as of April 2022 (Table 1).
Decision Criterion and Subcriterion Weighting
An index in considered to be consistent in aggregation when the outcome of interest has the same value, whether it is calculated directly in a single operation or is calculated in two or more steps by first calculating separate components. The aggregate consistency indices and ratios were 0.19 and 0.14 for caregivers, 0.01 and 0.01 for neurologists, and 0.14 and 0.10 for payors respectively. The decision criterion and subcriterion weights for caregivers, neurologists, and payors are presented in Table 2. The total of all decision criterion or subcriterion weighted scores was an overall utility score of 1.0. A higher partial utility for a decision criterion or subcriterion indicates a greater preference for that component of the decision-making process. Overall, caregivers and payors applied the highest value to need for intervention and intervention outcomes. In contrast, neurologists placed the highest value on intervention outcomes and types of benefits. Notwithstanding, need for intervention, intervention outcomes, and type of benefit accounted for over 80% of total decision weights in each respondent group (Table 2).
When the decision subcriteria were examined, efficacy and the type of patient benefits were among the most valued, while subcriteria for economic impact had the lowest weighting for all the respondent groups. Neurologists also applied the highest partial utility weighting to drug efficacy compared to caregivers and payors (mean = 0.219 vs. 0.115 vs. 0.166) indicating this was a major driver in their decision-making. Other decision subcriteria with weights greater than 0.10 at the group level included disease severity and the type of public health benefits as reported by caregivers (Table 2). Surprisingly, caregivers gave a value rating of less than 0.10 for safety, in contrast to a higher score provided by neurologists and payers. These findings were largely consistent as indicated by the results of the sensitivity analyses (data not shown).
A breakdown of the respondent-level rank distributions of decision criteria and subcriteria is presented in Fig. 2. With respect to decision criteria, 64% and 54% of neurologists considered efficacy and intervention outcomes to be the most important. In contrast, 64% of neurologists considered economic impact the least important (Fig. 2). In the other groups, 52% of caregivers and 41% of payors considered need for intervention to be the most important, while 32% and 33% considered economic impact the least important. With respect to decision subcriteria, approximately 1 in 3 caregivers (33%) considered patient/caregiver reported outcomes the most important within intervention outcomes, while more than 50% of the neurologists and payors considered it the least important. In addition, 72% of neurologists valued patient benefits over public health benefits, while 50% of caregivers shared this preference. Within comparisons of four economic subcriteria, approximately 50% of caregivers, neurologists, and payors considered direct medical costs the most important and indirect costs the least important of all decision subcriteria within economic impact (Fig. 2).
The final parameter evaluated how much each of the decision subcriteria contributed to the overall preference in each respondent subgroup that preferred either Aβ-targeted therapy or SOC. In the evaluation of overall treatment preference, 77 (65.8%) of caregivers favored Aβ-targeted therapy over SOC. In contrast, only 40 (44.4%) neurologists and 40 (44.4%) payors favored targeted therapy over SOC. The contribution of each decision subcriterion to the overall preference is the difference between the preference score for amyloid-targeting drugs and the preference score for the SOC with respect to that decision subcriterion. The contributions of decision subcriteria to overall treatment preference in the subgroups who favored Aβ-targeted therapy over SOC are presented in Fig. 3. Among caregivers who preferred Aβ-targeted therapy, patient benefits and public health benefits were key drivers in their decision-making process. Among neurologists who preferred amyloid-targeting drugs over SOC (N = 40), efficacy and the type of benefits to patients were the most important factors, while uncertainty in efficacy, safety and direct medical costs were drivers against the selection of amyloid-targeting drugs (Fig. 3). In the payer subgroup who preferred Aβ-targeted therapy (n = 40), efficacy and patient benefits were the most relevant factors. Surprisingly, direct medical and nonmedical costs as well as indirect costs were not deemed to be important factors by payors in their selection of Aβ-targeted therapy (Fig. 3).
Discussion
Decision-making for pharmacotherapy in AD in complicated, as there are multiple factors that need to be considered and weighted simultaneously. Furthermore, these factors and their relative importance are not consistent between key stakeholders involved is patient care. MCDA is an effective method to identify and assess the relative importance of each component used in decision-making [14, 18]. The current investigation applied the MCDA framework to four decision criteria and 12 subcriteria that contribute to the selection of pharmacotherapy for early-stage AD, which was applied to the three stakeholder groups. Among the three groups, the decision criteria selected as being the most important by respondents consisted of need for an intervention and the outcomes associated with a new treatment (e.g., efficacy, safety patient/caregiver outcomes).
When assessing the most relevant subcriteria, caregivers and payors valued disease severity, treatment efficacy, and patient benefits as being highly relevant. However, neurologists placed less importance on disease severity and more on treatment efficacy and patient benefits. Surprisingly, all three groups place the lowest impact on all aspects of the economic impact of a new Aβ-targeted therapy. This finding was unexpected, given the clinical uncertainty and high acquisition cost of aducanumab [11, 12]. The insight gained is the notable consensus among the key AD stakeholder groups that cost should not be a driver or a key factor in offering a new Aβ-targeted therapy to society. One caveat to this finding is that cost data were not presented as out-of-pocket patient expenses for treatment but as societal costs for a new intervention. Hence, how caregivers value costs in this study may differ from how they would in the real world where out-of-pocket costs are a reality. Heterogeneity of responses was also identified among the three groups of respondents. As an illustration, two distinct subgroups were identified where one favored an AD-targeted therapy over the SOC because of efficacy considerations. In contrast, the other subgroup favored SOC over an AD-targeted therapy, primarily because of efficacy considerations. Both subgroups were presented with the same efficacy and safety data. This contrasting pattern suggests that stakeholders may interpret the clinical evidence differently and draw different conclusions from the same information.
A review of the AD literature was unable to identify any studies that applied the MCDA methodology to quantify the various parts of AD treatment decision-making. There are several Aβ-targeting agents in AD that are in clinical development [13, 28]. When the results of these trials are reported, there will be a need for information on stakeholder preferences to support public health policy and drug reimbursement decision-making. Therefore, this study provides insights from three relevant stakeholder groups that can be used to inform health policy and drug reimbursement. The study confirmed and measured the relative importance of disease severity and humanistic burden, incremental patient benefit as well as the need for improved efficacy over the SOC as being important components in new treatments for AD. Direct medical cost was a modestly important subcriterion, but other economic components such as direct nonmedical and indirect costs were of lesser importance. Therefore, drug formulary committees at the regional or national level should place a preferential weighting on burden of illness, patient-reported outcomes, and improved efficacy over cost considerations.
The strengths of this investigation are the selection of three important groups involved in the care of patients with AD. However, there are limitations that need to be acknowledged. The sample size in all three respondent groups was small and limited to the USA. This may compromise the generalizability of the findings to other countries, particularly those with socialized healthcare systems and a formal health technology assessment process for new drug reimbursement submissions. Heterogeneity was found with respect to overall treatment preferences. This finding was expected, as the directionally opposite interpretations of the same evidence observed across respondents suggest that both discussion and education are necessary in public and scientific domains before a meaningful consensus may be reached for group decisions. All stated preference techniques such as MCDA measure intent, as opposed to revealed preference in a real-world situation. The survey was administered using an online format, so there may have been a selection bias towards younger respondents or those with easier access or a greater affinity to the internet. The sample size of caregivers was 117 compared to 90 for neurologists and payers respectively. We have to acknowledge that the slight imbalance may affect the precision of the final estimates within the neurologists and payers groups. Lastly, patients with early-stage AD who would be potential candidates for these new therapies were not included in the study.
Conclusions
The MCDA technique was used to measure caregiver, neurologist, and caregiver preferences for the various components in decision-making for new AD drugs from a societal perspective. Caregivers, neurologists, and payors placed the highest value on drug efficacy and the types of benefits derived by patients. In contrast, all three groups considered cost implications to be among the least important factors in their decision. Furthermore, more caregivers than neurologists or payors preferred Aβ-targeted therapy over SOC, likely driven by their perceived need for a new intervention. There was also considerable heterogeneity regarding the relative importance of the various decision criteria and treatment preferences amongst the three stakeholder groups. Therefore, health policy and drug formulary committees need to consider these differences and the relative weighting of the different components of new treatments in deciding on which drugs to make available to patients.
References
Soria Lopez JA, González HM, Léger GC. Alzheimer’s disease. Handb Clin Neurol. 2019;167:231–325.
Crous-Bou M, Minguillón C, Gramunt N, Molinuevo JL. Alzheimer’s disease prevention: from risk factors to early intervention. Alzheimers Res Ther. 2017;12:71. https://doi.org/10.1186/s13195-017-0297-z.
Alzheimer’s Disease International. The global impact of dementia: an analysis of pervalence, incidence, cost and trends. World Alzheimer Report 2015. London: Alzheimer’s Disease International; 2015.
Takizawa C, Thompson PL, van Walsem A, et al. Epidemiological and economic burden of Alzheimer’s disease: a systematic literature review of data across Europe and the United States of America. J Alzheimers Dis. 2015;43:1271–84.
Deb A, Thornton JD, Sambamoorthi U, Innes K. Direct and indirect cost of managing Alzheimer’s disease and related dementias in the United States. Expert Rev Pharmacoecon Outcomes Res. 2017;17:189–202.
Weller J, Budson A. Current understanding of Alzheimer's disease diagnosis and treatment. F1000Res 2018;31:F1000 Faculty Rev-1161.
Koca E, Taşkapilioğlu Ö, Bakar M. Caregiver burden in different stages of Alzheimer’s disease. Noro Psikiyatr Ars. 2017;54:82–6.
Pereira MG, Abreu AR, Rego D, Ferreira G, Lima S. Contributors and moderators of quality of life in caregivers of Alzheimer’s disease patient. Exp Aging Res. 2021;47:357–72.
Schneider LS, Mangialasche F, Andreasen N, et al. Clinical trials and late-stage drug development for Alzheimer’s disease: an appraisal from 1984 to 2014. J Intern Med. 2014;275:251–83.
Yang P, Sun F. Aducanumab: the first targeted Alzheimer’s therapy. Drug Discov Ther. 2021;15:166–8.
Rabinovici GD. Controversy and progress in Alzheimer’s Disease—FDA approval of aducanumab. N Engl J Med. 2021;385:771–4.
Mullard A. Landmark Alzheimer’s drug approval confounds research community. Nature. 2021;594:309–10.
Decourt B, Boumelhem F, Pope ED 3rd, et al. Critical appraisal of amyloid lowering agents in AD. Curr Neurol Neurosci Rep. 2021;21. https://doi.org/10.1007/s11910-021-01125-y.
Chisholm O, Sharry P, Phillips L. Multi-criteria decision analysis for benefit-risk analysis by national regulatory authorities. Front Med. 2022;8: 820335. https://doi.org/10.3389/fmed.2021.820335.
Adunlin G, Diaby V, Montero AJ, Xiao H. Multicriteria decision analysis in oncology. Health Expect. 2015;18:1812–26.
Vermersch P, Martinelli V, Pfleger C, et al. Benefit-risk assessment of cladribine using multi-criteria decision analysis for patients with relapsing-remitting multiple sclerosis. Clin Ther. 2019;41:249–60.
Pohekar S, Ramachandran M. Application of multi-criteria decision making to sustainable energy planning-a review. Renew Sustain Energy Rev. 2004;8:2004.
Goetghebeur MM, Wagner M, Khoury H, et al. Bridging health technology assessment (HTA) and efficient health care decision making with multicriteria decision analysis: applying the EVIDEM framework to medicines appraisal. Med Decis Mak. 2012;32:376–88.
Marsh K, IJzerman M, Thokala P, et al. ISPOR Task Force. Multiple criteria decision analysis for health care decision making-emerging good practices: report 2 of the ISPOR MCDA emerging good practices task force. Value Health. 2016;19:125–37.
van Til J, Groothuis-Oudshoorn C, Lieferink M, et al. Does technique matter; a pilot study exploring weighting techniques for a multi-criteria decision support framework. Cost Eff Resour Alloc. 2014. https://doi.org/10.1186/1478-7547-12-22.
van Til JA, Dolan JG, Stiggelbout AM, et al. The use of multi-criteria decision analysis weight elicitation techniques in patients with mild cognitive impairment: a pilot study. Patient. 2008;1:127–35.
Garau M, Hampson G, Devlin N, Mazzanti NA, Profico A. Applying a multicriteria decision analysis approach to elicit stakeholders’ preferences in Italy: the case of obinutuzumab for rituximab-refractory indolent non-Hodgkin lymphoma. Pharmacoecon Open. 2018;2:153–216.
Saaty TL. Highlights and critical points in the theory and application of the analytic hierarchy process. Eur J Oper Res. 1984;74:426–47.
Pauer F, Schmidt K, Babac A, et al. Comparison of different approaches applied in analytic hierarchy process—an example of information needs of patients with rare disease. BMC Med Inform Decis Mak. 2016;16:117. https://doi.org/10.1186/s12911-016-0346-8.
Schmidt K, Babac A, Pauer F, et al. Measuring patients’ priorities using the analytic hierarchy process in comparison with best-worst-scaling and rating cards: methodological aspects and ranking tasks. Health Econ Rev. 2016;6:50. https://doi.org/10.1186/s13561-016-0130-6.
Goepel KD. Implementation of an online software tool for the analytic hierarchy process (AHP-OS). IJAHP, 10 2018. https://ijahp.org/index.php/IJAHP/article/view/590. Accessed June 15, 2022.
Jost L. Partitioning diversity into independent alpha and beta components. Ecology. 2007;88:2427–39.
Se Thoe E, Fauzi A, Tang YQ, Chamyuang S, Chia AYY. A review on advances of treatment modalities for Alzheimer’s disease. Life Sci. 2021;276:119–29.
Acknowledgements
The authors would like to express their gratitude to Dr. Kathryn Phillips, Professor of Health Economics, University of California, San Francisco and Dr. Omolola Adepoju, Clinical Associate Professor, University of Houston for reviewing and providing feedback on the design of this study. The authors would also like to express their gratitude to the participants who responded to the MCDA questionnaire.
Funding
The study and the rapid service fee were funded by Eisai, Inc., Nutley, NJ.
Authors’ Contributions
Amir Abbas Tahami Monfared and Quanwu Zhang conceived of the study and managed the overall direction, planning and provided critical feedback to the co-authors. Erik Dysdale, George Dranitsaris, Alex Quill, Lin Mu, Christopher Weyrer, and Peter Neumann provided support to the design and implementation of the search strategy. Amir Abbas Tahami Monfared, Erik Dysdale, Quanwu Zhang, and Christopher Weyrer were responsible for administrative, technical, or material support. Alex Quill, Lin Mu, and George Dranitsaris prepared the tables and figures. George Dranitsaris wrote the initial manuscript, and all authors were involved in interpreting the results, editing and critically reviewing the manuscript.
Disclosures
George Dranitsaris has received consulting fees from Eisai Inc. Amir Tahami and Quanwu Zhang are employees of Eisai Inc. Alex Quill, Lin Mu, Erik Dysdale and Christopher Weyrer are employees of the Boston Consulting Group. Peter Neumann has nothing to disclose.
Compliance with Ethics Guidelines
The study protocol received ethical approval by Pearl IRB (Indianapolis, IN; IRB protocol # 22-BCGR-101). The study was completed in accordance with the declaration of Helsinki. Respondents were provided background information on the intent of the study, and all provided written informed consent to participate.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Dranitsaris, G., Zhang, Q., Quill, A. et al. Treatment Preference for Alzheimer’s Disease: A Multicriteria Decision Analysis with Caregivers, Neurologists, and Payors. Neurol Ther 12, 211–227 (2023). https://doi.org/10.1007/s40120-022-00423-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-022-00423-y