Abstract
Several recent epidemiological studies attempted to identify risk factors for Alzheimer’s disease. Age, family history, genetic factors (APOE genotype, trisomy 21), physical activity, and a low level of schooling are significant risk factors. In this review, we summarize the known psychosocial risk factors for the development of Alzheimer’s disease in patients with Down syndrome and their association with neuroanatomical changes in the brains of people with Down syndrome. We completed a comprehensive review of the literature on PubMed, Google Scholar, and Web of Science about psychosocial risk factors for Alzheimer’s disease, for Alzheimer’s disease in Down syndrome, and Alzheimer’s disease in Down syndrome and their association with neuroanatomical changes in the brains of people with Down syndrome. Alzheimer’s disease causes early pathological changes in individuals with Down syndrome, especially in the hippocampus and corpus callosum. People with Down syndrome living with dementia showed reduced volumes of brain areas affected by Alzheimer’s disease as the hippocampus and corpus callosum in association with cognitive decline. These changes occur with increasing age, and the presence or absence of psychosocial risk factors impacts the degree of cognitive function. Correlating Alzheimer’s disease biomarkers in Down syndrome and cognitive function scores while considering the effect of psychosocial risk factors helps us identify the mechanisms leading to Alzheimer’s disease at an early age. Also, this approach enables us to create more sensitive and relevant clinical, memory, and reasoning assessments for people with Down syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
People with Alzheimer’s disease living with Down syndrome show (early) degenerative alterations in specific brain areas, so Down syndrome could contribute to our understanding of the early stage of Alzheimer’s disease. |
We searched in the literature the common psychosocial risk factors of Alzheimer’s disease in Down syndrome such as cognitive status, educational level, social standing, employment, physical activity, psychosocial activity, ethnic group, sleep, and smoking habits, and other risk factors as age, sex, and genetic factors (APOE) which have a synergistic effect for the development of dementia. |
Hippocampus and corpus callosum are the most affected brain regions in Alzheimer’s disease and people with Down syndrome living with dementia, so they are possible biomarkers for Alzheimer’s disease. |
The presence or absence of psychosocial risk factors can influence the cognitive function in individuals with Down syndrome living with dementia, which correlates with changes in brain regions impacted by Alzheimer’s disease, such as the hippocampus and corpus callosum. |
Identifying psychosocial risk factors will increase our understanding of the genetic and molecular elements that cause Alzheimer’s disease and how to avoid them with different interventions. |
Introduction
Down syndrome (DS) is a genetic condition caused by the presence of all or part of chromosome 21. People with DS usually have mild to severe intellectual disabilities, growth retardation, and distinctive facial traits [1]. Alzheimer’s disease (AD) is a neurodegenerative condition marked by neuronal loss, neuritic plaques, neurofibrillary tangles on neuropathology, and a gradual and irreversible decline in cognition and behavior on clinical examination [2, 3]. Around 40–80% of adults with DS acquire AD-like dementia by their fifth to sixth decade of life [4] at a considerably earlier age than sporadic AD [5,6,7]. In DS, the developing characteristic brain neuropathological lesions (i.e., amyloid plaques) identical to those in AD preceded the beginning of dementia symptoms [8]. Both conditions appear to have a genetic foundation, as demonstrated by the triplication of the gene encoding the amyloid beta (A4) precursor protein (APP) in persons with DS [9], while the existence of a duplicate of the APP gene in people without DS causes familial AD [10]. Despite their genetic similarities, people with DS and AD have different clinical presentations of dementia [8]. Behavioral issues and personality changes are early symptoms of dementia in persons with DS, unlike “forgetfulness,” a typical sign of early-stage dementia in the general population [7, 11].
There is evidence that amyloid load originates in the frontal cortex in people with DS having AD before spreading to other brain areas, which is not necessarily the case in sporadic AD [12], revealing pathophysiological distinctions between conditions [8]. Since people with DS having AD show (early) pathological changes in specific brain regions such as the amygdala, hippocampus, and corpus callosum [13,14,15], they offer a possibility to investigate the first changes in this disease and observe its progression stage along with the course of the disease. Both people with AD living with and without DS will benefit from the improved diagnosis and treatment of dementia syndrome [13]. The development of extracellular plaques of insoluble amyloid peptide (A) and neurofibrillary tangles (NFT) composed of phosphorylated tau protein (P-tau) in neuronal cytoplasm is a defining feature of AD [16, 17]. AD results from neuronal death with the accumulation of neurofibrillary tau tangles and beta-amyloid plaques, although the root cause of insoluble plaque formation and neurofibrillary tangle propagation is uncertain [16]. Considering that risk factors of AD are known [16], psychosocial risk factors are essential to understand because, unlike genetic risk factors, they are modifiable. People who were just moderately physically and cognitively engaged in the past and those who have marginally social involvement are more likely to acquire dementia [18, 19]. The current study focuses on the psychosocial risk factors for AD in children and adults with DS such as cognitive status, educational level, physical activity, employment, psychosocial stress, sleep, marital status, depression and smoking, and the neuroanatomical alterations observed in these individuals using high-resolution neuroimaging (MRI imaging).
We included factors such as age, sex, and some genetic factors, which are not identified as a psychosocial risk factor, such as apolipoprotein E (APOE). Our inclusion of such factors is justified since they have a synergistic effect with other psychosocial risk factors for the development of AD. The risk factors analyzed included age, sex, cognitive status, genetic factors (APOE), educational level, social status, employment, physical activity, psychosocial activity, ethnic group, sleep, and smoking habits (e.g., family members). The risk of dementia is much reduced in individuals with a high cognitive reserve and is much higher in people with low educational levels and intellectual problems. This finding results from more than 20 published studies with more than 29,000 participants and a median follow-up period of more than 7 years [20]. Mullins et al. [20] concluded that people with DS living with dementia and persons with AD in the general population have significantly reduced volumes of the same brain regions and the hippocampus and other temporal lobe structures. These volume reductions have an association with cognitive decline in both groups. Preliminary evidence indicates that DS individuals may be more sensitive to tissue loss than others and have less “cognitive reserve” [20]. Few studies used functional brain imaging to study DS [20, 21]. These are characterized by small samples and using many different methods and scanning tasks with low image resolution so that the results are not easily comparable.
Additionally, previous neuroimaging studies of child development have limitations due to their coarse resolution, small group size, and limited age range [22]. Previous research studies did not significantly analyze temporal lobe anomalies, parahippocampal gyrus volume, and corpus callosum changes. For instance, Rodrigues, Nunes et al. [23] conducted a survey to assess neuroimaging abnormalities of the corpus callosum linked to DS, but further studies are needed to confirm their findings. This review collects data from various resources in order to understand this gap. We intend to provide a preliminary assessment for future examinations attempting to produce new data sets for structural neuroimaging of DS (MRI studies) compared to patients with AD in the average population and cognitive-behavioral phenotypes. Thus, we focus on research data related to individuals with DS compared neuroanatomically with the psychosocial risk factors for AD occurrence.
According to the National Institute on Aging (NIH) recommendations regarding patients with AD in general populations, we can also suggest using these recommendations to develop diagnostic criteria for people with DS at risk of dementia. These recommendations represent the criteria for the clinical diagnosis of AD. The Alzheimer’s Association (AA) and the National Institute on Aging (NIA) sponsored a series of advisory round table meetings to produce a revision of diagnostic and research criteria for AD. On the basis of the current scientific data, the workgroups evaluated biomarker, epidemiological, and neuropsychological findings and developed conceptual frameworks and practical research requirements [24]. Asymptomatic amyloidosis, asymptomatic amyloidosis + neurodegeneration, and amyloidosis + neurodegeneration + slight cognitive loss are postulated as three preclinical phases of AD. The preclinical workgroup suggested identifying the characteristics that best predict the probability of progression from normal cognition to moderate cognitive impairment (MCI) and AD dementia. Longitudinal clinical research investigations are required to refine these models.
The MCI and AD dementia workgroups wanted to make sure that the revised criteria were flexible enough to be used by both general healthcare providers who did not have access to neuropsychological testing, advanced imaging, or cerebrospinal fluid measurements and specialist experts working on research or clinical trials who would have access to these tools. MCI owing to AD refers to the symptomatic predementia phase of AD. The final set of criteria for MCI related to AD contains four levels of confidence based on the existence and kind of biomarker results. There was a discussion about the requirements for all-cause dementia and AD dementia. For study purposes, dementia caused by AD is divided into three categories: probable AD dementia, possible AD dementia, and probable or possible AD dementia with evidence of the AD pathophysiological process. In clinical practice, the fundamental clinical criteria for AD dementia will remain the cornerstone of the diagnosis, although biomarker evidence is likely to improve the pathophysiology specificity of the diagnosis [24]. So, people with DS could have evaluation tests and measurements developed according to these recommendations by considering the early diagnosis with cognitive and imaging assessments, as discussed later in this review.
This review study will help us better understand the pathological and neuroanatomical linkages between AD and DS and the role of psychosocial risk factors in establishing remedies to prevent or hinder AD development at an early stage.
Methods
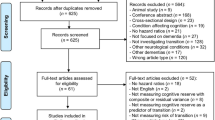
We performed a comprehensive literature search on PubMed, Google Scholar, and Web of Science. PubMed provides a thorough overview of current literature on a given topic and is more extensive than any other database regarding biomedical and health science issues. Furthermore, the use of MeSH (Medical Subject Headings) indexing enables more precise and comprehensive searching than other databases, and in our search, we used some MeSH terms. Google Scholar explores the full text for keywords and a broader range of sources, such as conference proceedings and books, which are not included in regular databases, making it a practical resource for gray literature searches. These characteristics are beneficial for our investigation and ensure effective search results. Google Scholar can show you articles and books with links to them. Web of Science provides access to scientific material in abstracts and full text. Through Web of Science, you can search across several databases, including the Web of Science Core Collection and databases included with NEOMED subscriptions such as MEDLINE. This tool allowed us to review many studies related to our topic.
First, we reviewed articles using the search terms “Psychosocial risk factors for Alzheimer’s disease” with “Risk factors, Psychosocial risk factors, Alzheimer’s disease”. We also used the search term “Risk factors, Psychosocial risk factors for Alzheimer’s Disease in Down syndrome” with the keywords “Risk factors, Psychosocial risk factors, Alzheimer’s disease, dementia, Down syndrome” for further detailed research. We found related terms such as dementia and dementia of Alzheimer’s type as they are used interchangeably within the literature. We selected structural neuroimaging studies (MRI studies) focusing on the neuroanatomical changes in DS involved in memory functions, specifically changes in regions of the hippocampus, corpus callosum, and temporal lobe in association with psychosocial risk factors related to the occurrence of AD. To avoid heterogeneous results, we focused on MRI studies, which use safe and attractive alternative non-invasive imaging techniques compared to other imaging modalities such as positron emission tomography (PET). An increasing number of PET studies using tracers, e.g., amyloid, are being published but we consider PET studies irrelevant to our search area and we focus only on structural imaging for the aforementioned reasons. MRI techniques can provide a detailed assessment of brain regions throughout childhood and adulthood without ionizing radiation. Besides PET studies, our search area did not include neuropathological evidence, which is limited for practical reasons to small brain sampling, leading to biased conclusions. We searched using the keywords “Risk factors, Psychosocial risk factors, Alzheimer’s disease, Dementia, Down Syndrome, Neuroimaging, Neuroanatomical changes”.
We did not use statistical methods but summarized related data published between 1978 and 2021 to review the recently published studies. This study does not represent a systematic review of the literature as little literature is available regarding our search topic. We did not use the PRISMA guidelines as our review is not systematic. To ensure that we did not miss essential papers during our search, we developed a strategy by identifying sources to be searched and keywords and search terms used in the literature and rerunning the search many times. We selected publications and research articles for inclusion if they presented relevant outcomes related to AD and people with DS groups. Those reporting on the psychosocial risk factors of AD in DS have priority.
In contrast, articles reporting on other AD risk factors in DS have no priority unless they include specific information on individuals with DS related to our search topic. When there were several articles on a given topic, those that contained unique information have priority for inclusion. We added more recently published publications and studies of more significant patient populations, and studies with more extended follow-up periods to the list of priorities. We found 26 articles that fulfilled our inclusion criteria (Table 1). The authors of reviewed literature used clinical records to collect information about the individuals’ cognitive functioning levels based on the evaluated papers. They examined case files and gathered information on cognitive performance from previous psychological or psychiatric tests. Because not all participant files provided numerical IQ values, the authors used an ordinal scale to guarantee consistency of the level of the functioning variable. According to the DSM-IV (APA 1994), the categories are mild, moderate, and severe intellectual impairment classifications, with intermediate levels, added to designate participants on each level’s boundary. This article is based on previously conducted studies, and does not contain any new studies with human participants or animals performed by any of the authors.
Results
We present our results in three sections, as shown in Table 1.
Psychosocial Risk Factors for Alzheimer’s Disease
Although research data identified various neurophysiological risk factors for AD and dementia, little knowledge is available regarding psychosocial determinants [25]. Previous studies identified many psychosocial risk factors for AD (Table 2). Still, we will present a few of these studies discussing psychosocial risk factors for AD as an introductory background as our focus is mainly on psychosocial risk factors for AD in DS. Also, our review of psychosocial risk factors for AD in the general population can help determine common and distinct pathways and mechanisms underlying the increased risk of dementia compared to people with DS. Zhang et al. [26] performed a 5- and 10-year follow-up study in Shanghai, China. The essential psychosocial risk factors for AD onset and development suggested by this study were not working (jobless or retired), no participation in community activities, analphabetism, and blue-collar status. Burke et al. [27] established a connection between depression, sleep disturbance, and anxiety (as individual factors and comorbid conditions) and the risk of AD development. This study, however, did not use neuroimaging to confirm the diagnosis of AD pathology [27]. A survey by Burnes and Burnette [25] indicated that previous life trauma and posttraumatic stress disorder (PTSD) are good candidates as psychosocial risk factors for AD, according to the evidence presented in this research, by creating a conceptual model relating these factors to AD. Kropiunigg et al. [28] discussed psychosocial stress resulting from adapting to an active but ineffective work style and living with a domineering spouse as a link to an increased risk of AD. Persson and Skoog [29] studied different psychosocial risk factors before the age of 70 in various age groups, such as the death of a parent, divorce of parents, growing up with one parent, different guardians, extreme poverty, death of a spouse, death of a child, serious illness in a child, shift or piece work, arduous manual labor, physical disease in a spouse, mental illness in a spouse, death of siblings or friends, change of residence, and financial status deterioration. Their findings suggest that psychosocial risk factors early in life contribute to the development of dementia later in life [29].
Marital status, stress, depression, inadequate sleep, smoking, cognitive reserve, and physical activity are among the psychosocial risk factors discussed by Silva et al. [16] as risk and protective factors for AD development. The aforementioned studies did not perform any tests to distinguish between familial/early-onset AD and sporadic/late-onset AD in the studied populations. Silva et al. [16] discussed the genetic risk factors associated with the occurrence of both AD types in their review. According to that study and other related studies, familial/early-onset AD compared to sporadic/late-onset AD has significant genetic risk factors influencing AD development, like DS [16, 30].
Wang et al. [31] investigated the association between psychosocial stress at work and an increased risk of dementia at a late age and found that stress conditions associated with the job contributed to a high risk of dementia and AD at a late age. Additionally, a similar study by Seidler et al. [32] explored the role of psychosocial work factors in the onset of dementia. He et al. [33] found that low educational level, low cognitive function, low occupational status, lack of social interaction and leisure activities, and poor well-being affect the onset and development of AD. Bernhardt et al. [34] provided a thorough systemic review of all reported psychosocial risk factor outcomes from controlled trials between 1994 and 2001. That review concluded that factors studied in the articles, such as living alone, having no intimate social links, not participating in social and recreational activities, and never having married, are all linked to dementia. That also review suggests that AD is adversely associated with intellectual diversity and intensity and favorably associated with psychosocial inactivity, unproductive working style, living with a domineering spouse, and physical inactivity in recent studies [34].
Psychosocial Risk Factors for Alzheimer’s Disease in Down Syndrome
Determining the risk factors is essential to assessing the risk of AD in individuals with DS. While identifying risk factors helps evaluate individual and community risk for developing AD, they do not guarantee that all persons with known risk factors will get the disease, nor that individuals without such risk factors would not contract the disease [35]. Neuropathological changes related to triplication of amyloid precursor protein (APP) contribute mainly to the first clinical signs of AD in DS [36]. In autopsy, Alzheimer-type neuritic plaques and neurofibrillary tangles have been found and reported in the brains of 7.5% of people with DS in the early second decade of life, reaching 80% by the fourth decade and 100% in people over 60 years old [37]. Other risk factors that can add more explanations and understanding of the mechanism of the occurrence of the predementia stage in people with DS should be studied and identified [38]. The study of risk factors for dementia in people with DS faces challenges due to the lack of specific and compelling cognitive and neuropsychological status measurements in this population [38]. The most available assessment methods and instruments to assess dementia in persons with intellectual disabilities, including DS, are informants-based tests and do not directly assess cognitive function in those groups [39]. We focused on psychosocial risk factors such as cognitive status, education, years of living in a care institution, physical activity, smoking, sleep, and other risk factors such as age, sex, and some genetic factors (APOE) which contribute additively to the development of dementia (Table 3). Age is considered a strong common risk factor for dementia in DS, and the association between increasing age and the increased risk for dementia in DS is widely indicated [35, 38, 40]. Few studies have assessed sex as a risk factor, with controversial results [38]. Some evidence reports that women are at greater risk due to the low level of postmenopausal estrogen and that women have a higher life expectancy than men [35]. A recent study by Lai, Mhatre et al. [41] evaluated sex differences in AD risk in adults with DS. It showed no significant sex difference in the risk for AD development in adults with DS. However, they found that women with DS had a nearly 2-year duration of dementia more than male individuals with DS from AD onset until death, although having equal mean ages at the beginning of AD. These findings [41] contrast with earlier DS research conducted on a smaller scale [42, 43]. In men with DS, Schupf, Kapell et al. [42] found a greater risk of AD, but Lai, Kammann et al. [43] found the opposite.
In the general population, there is an evidence-based suggestion that a higher level of cognitive functioning, which is linked to a higher level of education, a higher IQ, years of living in a care institution, and employment, is associated with a low incidence of dementia [44]. This study investigated the correlation between education and other environmental factors, such as years of living in a care institution and occupation, and the occurrence of dementia in people with DS. It resulted in the theory that environmental changes can improve cognitive function, leading to the delay of the onset of dementia [44]. These data led to the cognitive reserve hypothesis, suggesting that patients compensate for neuronal loss when the brain works actively to deal with neuronal damage [45]. People with better baseline cognitive abilities can tolerate more AD pathology and neuronal loss than patients with worse baseline cognitive skills [46]. Also, Zigman and Lott [35] assumed that IQ level and cognitive reserve could be possible risk factors for dementia in DS. They suggested that people with DS who function at higher levels (e.g., more excellent premorbid IQ, education, occupation, and language ability) have a reduced risk of AD dementia than their counterparts who perform at lower levels. Another decisive risk factor is a family history caused by genetic or environmental factors. The apolipoprotein E gene (APOE), encoded by three alleles, ε2, ε3, and ε4, is associated with a risk for AD in DS [47]. The apolipoprotein ε4 allele is the most well-known genetic risk factor for sporadic AD, and it is linked to early symptoms and pathology in the general population [48]. The APOE ε4 allele is also a significant risk factor for AD in DS compared to the APOE ε2 allele, which is associated with low risk and a protective role [35, 38, 47]. Although an early meta-analysis of association studies revealed that dementia was higher in individuals with DS carrying APOE ε4 [49], one case–control study in a Dutch community found no effect of APOE genotype on the incidence or onset of dementia in DS [50]. The minimal number of patients studied was a critical limitation of these investigations [47].
In contrast to noncarriers, APOE ε4 carriers are at increased risk for dementia in DS, with an earlier start and rapid progression, according to a recent longitudinal, large cohort study of people with DS [51]. According to the available data, the evidence for a link between APOE ε4 and dementia in DS is very suggestive [48]. Few studies reported the effect of physical activity on cognitive function and dementia risk in DS [52]. Some of these studies used the mouse model of DS (Ts65Dn mice) and found essential evidence that physical activity may help with cognition. Voluntary wheel running in mice, for example, was linked to improved performance in cognitive tasks when compared to sedentary controls, especially when considering hippocampal-mediated processes, which are essential during AD [53,54,55]. Previous mouse model reports found that physical activity impacts gene and protein expression, neurogenesis, and brain morphology [53, 54, 56]. The Ts65Dn mouse is the most well-studied and extensively utilized DS animal model. It has a freely segregating additional chromosome with the triplication of mouse chromosome 16’s distal region, which is syntenic to a portion of human chromosome 21’s long arm [57]. The Ts65Dn mice mimicked many characteristics of DS, including cognitive impairment and hippocampus-dependent memory function [57,58,59]. Despite some genetic limitations caused by partial triplication of human chromosome 21 (HSA21) orthologous genes and concurrent triplication of some non-HSA21 genes [60], the Ts65Dn model reproduces many of the phenotypic aspects of the human disease, including brain changes and impaired learning and memory and is presently the sole mouse model utilized for preclinical discovery of pharmaceutical treatments targeting cognitive deficits in DS [61]. A 12-week exercise program improved episodic memory in human studies, including people with DS [62]. These studies documented improvements in executive function assessments such as inhibition [63, 64], attention shifting [65], response time [66, 67], and semantic fluency [68, 69]. However, there are differences in effect sizes and findings between these studies [52]. A recent survey by Pape et al. [52] examined the association between physical activity, regular exercise, and cognitive function in DS. The findings of their investigation indicated that frequent moderate and high-intensity exercise might reduce the possibility of clinically detectable mental deterioration in the DS group, with possible long-term benefits [52]. In 61 adults without dementia living with DS, Fleming et al. [70] investigated the relationship between everyday physical activity measured with an actigraph accelerometer and cognitive functioning and early AD pathology measured with PET amyloid-β and tau and diffusion tension imaging measures of white matter integrity. The amount of time spent on sedentary and moderate-to-vigorous activity was related to cognitive performance (negatively and positively, respectively; correlation coefficient (r) = − 0.472–0.572, significance (p) < 0.05). Both sedentary behavior and moderate-to-vigorous exercise are linked to white matter integrity in the superior and inferior longitudinal fasciculi (fractional anisotropy: r = − 0.397 to − 0.419, p < 0.05; mean diffusivity: r = 0.400, p = 0.05) [70].
No specific study from our reviewed literature correlated ethnicity as a risk factor for AD in DS, so future studies should consider this data. Also, no published research directly discussed the role of sleep as a risk factor for AD in DS. Chen et al. [71] examined the impact of sleep disturbance on executive function in individuals with DS. The results indicated an association between obstructive sleep apnea, common in people with DS with high body mass index, and more significant impairments in executive functions, including verbal fluency and inhibitory control. According to these findings, understanding the relationships between poor sleep, cognitive impairment, and deterioration in individuals with DS requires further research. These findings reveal a link between poor sleep and cognition in young individuals with DS and how their sleep issues affect AD development [71].
Considering smoking as a risk factor for dementia in the general population is unclear [72]. Research supported by the tobacco industry (conflict of interest) indicated a low risk of dementia associated with smoking [73]. Nonetheless, research data with no tobacco industry affiliation (e.g., tobacco companies providing study funding, study author(s) currently or previously employed by a tobacco company) reported a significantly increased risk of AD [73]. We did not find a study investigating the relationship between smoking in DS directly or passively (e.g., family members) and the risk of AD development. Many researchers who looked at potential psychosocial risk factors struggled with assessment and diagnostic challenges, making it difficult to compare results from different studies [38]. Future researchers looking into the prevalence rates and psychosocial risk factors for AD in people with DS should consider these observations.
Psychosocial Risk Factors for Alzheimer’s Disease in Down Syndrome and Their Association with Neuroanatomical Changes in the Brains of People with Down Syndrome
No specific study investigated DS brain areas changes related to AD, specifically the hippocampus or corpus callosum, and correlated such changes with psychosocial risk factors. Here, we correlate the results of previously published studies regarding the neuroanatomical changes related to dementia in DS with the results discussing the effect of psychosocial factors on cognitive function. All people with DS develop neuropathological features of AD by 40 years of age [13, 37, 74, 75]. The aging processes in DS are associated with the deposition of senile plaques and neurofibrillary bundles [76]. The buildup of these deposits, their distribution pattern in the brain, and the involvement of specific neurons are remarkably similar to the pathological changes that characterize AD [37]. A better understanding of how the DS brain develops with the help of a development-oriented approach will shed light on critical neurological principles of DS in children and illuminate the basics of the phenotype in adults, particularly the increased risk of early AD [35]. Therefore, DS provides a framework for studying the morphological brain changes in the early stages of AD [77].
Hippocampal and temporal lobe volume reductions are typical of AD and people with DS living with dementia [15, 78, 79]. These volume reductions are associated with cognitive decline in both AD and people with DS living with dementia groups in a study by Mullins et al. [20]. Th results of that study showed a positive correlation in patients with AD between the Mini-Mental State Examination (MMSE) score and the corrected hippocampus and temporal lobe volumes. Previous research reported a similar finding and revealed that performance on the MMSE correlates directly with hippocampal volume [80]. The decline in the hippocampus and temporal lobe volumes affects their functions, which is observable by the correlation between MMSE scores and the reduced volume in these regions [20]. The hippocampal structures involved in explicit memory deficits, the dentate gyrus, the essential core areas of hippocampal efferences and afferences, and the corpus callosum are crucial areas for studying structural changes related to AD. Memory impairment was one of the first clinical signs identified when evaluating the existing evidence of structural changes in the hippocampus in patients with AD [77]. This symptom worsened slowly over time and manifested as personality changes, loss of language skills, and affection of the extrapyramidal motor system. Histopathological examinations show the hippocampus structure as one of the first and most severely affected areas by AD [77]. A longitudinal assessment study of brain anatomy changes preceding dementia in DS by Pujol et al. [81] found that the brain volume changes and their links to cognitive impairment progression are generally consistent with well-known anatomical abnormalities that signify dementia development in AD. Thus, even though it occurs in a complicated scenario with extensive baseline pathology and a high potential for interactions between developmental and age-related alterations, brain involution in older people with DS appears to reflect the degenerative process of AD. The basal forebrain, hippocampus, and prefrontal lobe, which are impacted early in AD, were specifically impaired in DS before dementia in this study. Neurofibrillary damage and the loss of projection neurons responsible for the afferent and efferent connections of the hippocampal formation result in both disconnections of the intra-hippocampal relationships and the isolation of the hippocampus from other parts of the brain responsible for memory loss in AD [82,83,84]. By the age of 40, the proportion of individuals with DS who undergo a process of cognitive impairment, such as that in AD, is observably high [14]. The chronological hierarchy of symptoms begins with slowly progressing memory loss and leads to a general decline in cognitive skills accompanying dementia and emotional changes [85,86,87,88]. Research based on MRI scans indicated that hippocampal atrophy, which is significant in sporadic and DS-associated AD, can serve as a measure of allocortical neuronal degeneration [14, 77, 83, 84, 89].
Previous MRI studies proposed atrophy of the corpus callosum as a possible marker for the loss of intracortical-projecting neocortical association neurons in AD [90,91,92,93,94]. The projecting neurons from the corpus callosum are a subgroup of the large pyramidal neurons in the association cortex’s lamina III and V [95,96,97], which are particularly vulnerable to AD [98,99,100]. Therefore, several studies reported atrophy of the corpus callosum in Alzheimer-type dementia [14, 101,102,103,104,105,106]. Clinical symptoms of dementia in DS are memory loss, behavioral changes, language difficulties, neurological alterations, and decreased cognitive skills [107, 108].
Teipel et al. [14] investigated the effect of age on volume changes in the hippocampus and corpus callosum and found a correlation between neuropsychological scores and regional volumes in people with DS without dementia. This study demonstrated a decreased volume of hippocampus and corpus callosum regions with increased age and also showed a correlation between the size of corpus callosum areas and the global cognitive score, orientation, language, and visuospatial test scores in people with DS [14]. Kesslak et al. [109] and Raz et al. [110] found that the parahippocampal gyrus (PHG) is significantly larger in people with DS compared with normal aging and AD. Pathological and neuroimaging studies revealed that AD significantly impacts this structure, particularly its anterior portions [111, 112]. Raz et al. [110] indicated a correlation between the enlargement of the PHG and decreased total cognitive function. Mullins et al. [20] investigated the medial temporal lobe and found a reduced volume of this region associated with cognitive decline. A study by Krasuski et al. [113] found that the right and left amygdala, hippocampus, and posterior parahippocampal gyrus in the DS group have a smaller volume than in the control group. These regional brain volumes were significantly associated with greater age; this association was not observable in the anterior part of the parahippocampal gyrus. The hippocampus and amygdala volumes were positively correlated with memory assessment results [113] (Table 4). However, AD has the character of a gradual beginning and inevitable atrophy development in the medial temporal lobe [114]. The entorhinal cortex is usually the first part of the brain to deteriorate, followed by the hippocampus, amygdala, and parahippocampus [115,116,117,118]. The posterior cingulate and other limbic lobe components, including the amygdala, are also affected early. The temporal neocortex is ultimately affected, followed by all neocortical association regions, generally in a balanced way. The loss pattern differs between disorders, indicating preferential neuronal vulnerability and disease manifestation at the regional level [119].
Discussion
In this review, we discussed psychosocial risk factors for the occurrence of dementia in people with DS. An association between the DS phenotype and an increased risk of developing Alzheimer’s dementia is now powerfully demonstrated [38]. Previous studies indicate no significant difference between psychosocial risk factors for AD in the general population and psychosocial risk factors for AD in individuals with DS. This indication shows that studying DS provides a pattern for studying and understanding the clinical and pathological changes associated with the early stage of AD [13, 37, 120, 121]. As a result of the congenital neurological anomalies in DS, it is critical to distinguish between changes associated with AD and behavioral characteristics (e.g., depression, aggression, sleep disturbances, and social problems) that are frequent in the DS community independent of AD as reported by Dekker et al. [122]. So, it is essential to carefully assess any behavioral or emotional changes in older people with DS that can be psychiatric symptoms or associated with dementia and consider caregivers’ information as reliable [123]. There are few studies on dementia in people with severe/profound intellectual disabilities, including DS, as evidenced by the limited number of studies focusing on this complex combination [124]. Wissing et al. [124] reviewed available literature on observable dementia symptoms in DS and other intellectual disabilities. This study identified a range of dementia symptoms subdivided into cognitive decline (e.g., memory loss, forgetfulness, speech deterioration, loss of social skills), the reduction in activities of daily living (e.g., self-care skills, everyday functioning/skills), behavioral and psychological symptoms of dementia (BPSD) (e.g., apathy, aggression, altered eating/drinking behavior), and neurologic and other physical symptoms. Changes in general function, personality, and behavior may be more typical early AD indicators in persons with DS than memory loss and forgetfulness. Reduced interest in being sociable, conversing, or expressing thoughts, decreased enthusiasm for usual activities, a decline in the ability to pay attention, sadness, fearfulness, or anxiety, irritability, uncooperativeness, or aggression, restlessness or sleep disturbances, adult-onset seizures, changes in coordination and walking, increased noisiness or excitability are some of the early symptoms (National Institute on Aging, https://www.nia.nih.gov/health/topics/down-syndrome).
A rising amount of information suggests that increasing age is not the sole risk factor to consider when determining AD development in people with DS [38]. We evaluated previous reports and concluded that the APOE ε4 allele is a substantial risk factor for AD in individuals with DS, but the APOE ε2 allele is a protective factor [35, 38]. The exact role of APOE alleles in pathogenesis is unknown, despite considerable research aiming to clarify the underlying mechanism for this elevated risk. Current research, however, reveals that changes in APOE isoform effects on Aβ aggregation and clearance play an essential role in AD pathogenesis. Other putative pathways, such as various APOE isoforms influencing neuronal toxicity and tau phosphorylation and its function in synaptic plasticity and neuronal inflammation, are not ruled out. Inconsistent findings across studies made it difficult to determine whether the APOE ε4 allele signals increased harmful activity, decreased neuroprotective effect, or both. APOE-based therapeutic approaches suggest lowering the adverse effects of APOE ε4 or restoring APOE’s physiological and protective functions [125]. In DS there is a correlation between the effect of decreased clearance resulting from APOE ε4 with the increased production of APP due to trisomy of chromosome 21. Thus, the combination of trisomy 21 (perhaps resulting in increased Aβ deposition) and APOE ε4 (possibly resulting in impaired Aβ clearance or Aβ aggregates) results in considerably enhanced Aβ deposition [13, 126].
Sex as a possible risk factor has inconclusive data [38]. Previous reports in humans with DS and mouse models found an association between physical activity in different forms and improvement in memory and cognition [52]. We did not find studies that consider ethnicity and smoking as risk factors for AD in DS, although their role in the general population is reported [72, 127]. No published studies directly discussed the effect of psychosocial risk factors on the occurrence of AD in DS or related them to neuroanatomical changes depending on neuroimaging. Therefore, we assume a correlation between some of these risk factors for dementia in DS and neuroanatomical changes in brain areas related to memory and cognitive function. Aging is considered a significant risk factor for dementia in people with DS [38], in addition to genetic factors (e.g., APOE genotype) and cognitive reserve [35]. At the same time, no study controlled for age as a risk factor while studying the potential causality of psychosocial risk factors in disease progression, which future research efforts should consider. Understanding the risk factors for AD in DS will help us diagnose the disease and prevent other pathological conditions [35]. The difficulty in diagnosing dementia in individuals with DS faces complications by baseline intellectual disability (ID) [128]. Within the DSM-IV or ICD-10 classifications, no guidelines are available for diagnosing dementia associated with DS or any other learning disability. The Working Group for the Establishment of Criteria for the Diagnosis of Dementia in Individuals with Intellectual Disability, as reported by Aylward et al. [129], recommends using ICD-10 criteria as the worldwide diagnostic yardstick rather than DSM-IV criteria. The benefits observed include a stronger focus on “noncognitive” components of dementia (emotional instability, impatience, and apathy), which are frequently the earliest indicators of dementia in persons with Down syndrome.
Furthermore, ICD-10 uses a two-step diagnostic approach, in which a dementia diagnosis got established, and then dementia in DS is distinguished from other types of dementia [38]. The significant intra-individual variability in cognitive functioning, numerous diagnostic and methodological approaches employed in the field, and difficulty in collecting baseline levels of cognitive functioning in this group to measure behavioral changes are all factors to consider when diagnosing dementia in people with DS [130]. Most adults with DS will not admit to having memory problems. Because detecting thinking-skill impairments in people with intellectual disabilities can be challenging, diagnosing dementia in someone with DS can be difficult. Adult cognitive changes should have recognition to provide appropriate assistance and support to people with DS and their caregivers. The following concepts, according to a model proposed by Burt and Aylward [128], are essential for a person-centered diagnosis in people with DS: by the age of 35 years, there should be a documentation of a baseline of adult function; persons with DS should have their intellectual, behavioral, and social functions evaluated regularly, and each person’s medical record should ideally include thorough information about their adult abilities by the age of 35. This information is accessible from the person with DS, family members, and other trustworthy persons. Most individuals with intellectual impairments can benefit from this paradigm. A battery like this would increase diagnostic consistency and allow for cross-study comparisons. A skilled examiner should deliver the battery over a period.
This review is the first study comparing the effects of psychosocial risk factors for AD in DS and their association with neuroanatomical changes in hippocampus and corpus callosum regions. This study’s strengths include covering the most common psychosocial risk factors for dementia in DS that exist in the literature and presenting them in a summarized review considering the recently published information. Our review study also compared the relationship of these risk factors with neuroimaging biomarkers of AD, providing a clue for further research using imaging techniques to realize these results. However, the literature on neuroimaging in AD and DS spans multiple modalities, including diffusion tensor imaging and PET imaging of beta-amyloid, neurofibrillary tangles, glucose metabolism, and synaptic density. The findings on these imaging modalities are observable before anatomical changes occur in MRI, which may show earlier effects associated with psychosocial risk factors. There is a lack of other neuroimaging studies outside of anatomical MRI, which is considered a limitation in this study. These modalities may show differential presentation between DS and AD in the general population, elucidating underlying biochemical mechanisms that are yet to be proven. This study’s limitations include the lack of patients required to confirm our hypothesis to compare cognitive decline with neuroanatomy. Moreover, neuropsychological measures are becoming more sensitive for diagnosing AD dementia, and it can be difficult to correctly diagnose dementia in individuals with very low baseline cognitive performance. Individuals with DS have high variability in cognition, just like the general population, which AD studies consider.
Conclusions
The study of risk factors will improve our knowledge of genetic and biological factors causing AD and how to avoid them with various measures. There are no standard measurements for early diagnosis of dementia in people with DS, so consistent diagnostic criteria for dementia in people with DS and appropriate psychometric tests to identify cognitive changes are needed. In summary, we conclude that volume reductions in regions such as the hippocampus, other medial temporal lobe structures, and corpus callosum are considered the first Alzheimer’s-affected regions and are associated with age and other lifestyle factors in people with DS. This finding supports the theory that DS gives an approach to studying early-stage AD.
References
Akhtar F, Bokhari SRA. Down syndrome. Treasure Island: StatPearls; 2021.
Tiwari S, Atluri V, Kaushik A, Yndart A, Nair M. Alzheimer’s disease: pathogenesis, diagnostics, and therapeutics. Int J Nanomedicine. 2019;14:5541–54.
McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–9.
Holland A, Reinmuth O, editors. Aphasia or dementia: the cautionary tale of Dr. JJ. Seminars in speech and language. 1998. https://doi.org/10.1055/s-2008-1064034.
Zigman WB, Schupf N, Devenny DA, et al. Incidence and prevalence of dementia in elderly adults with mental retardation without Down syndrome. Am J Ment Retard. 2004;109(2):126–41.
Oliver C, Holland A. Down’s syndrome and Alzheimer’s disease: a review. Psychol Med. 1986;16(2):307–22.
Holland AJ, Hon J, Huppert FA, Stevens F, Watson P. Population-based study of the prevalence and presentation of dementia in adults with Down’s syndrome. Br J Psychiatry. 1998;172(6):493–8.
Salehi A, Wesson Ashford J, J Mufson E. Editorial (Thematic Issue: The Link between Alzheimer’s Disease and Down Syndrome. A Historical Perspective). Curr Alzheimer Res. 2016;13(1):2–6.
Korbel JO, Tirosh-Wagner T, Urban AE, et al. The genetic architecture of Down syndrome phenotypes revealed by high-resolution analysis of human segmental trisomies. Proc Natl Acad Sci. 2009;106(29):12031–6.
Rovelet-Lecrux A, Hannequin D, Raux G, et al. APP locus duplication causes autosomal dominant early-onset Alzheimer disease with cerebral amyloid angiopathy. Nat Genet. 2006;38(1):24–6.
Selkoe DJ. Cell biology of the beta-amyloid precursor protein and the genetics of Alzheimer’s disease. Cold Spring Harb Symp Quant Biol. 1996;61:587–96.
Handen BL, Cohen AD, Channamalappa U, et al. Imaging brain amyloid in nondemented young adults with Down syndrome using Pittsburgh compound B. Alzheimers Dement. 2012;8(6):496–501.
Lott IT, Head E. Dementia in Down syndrome: unique insights for Alzheimer disease research. Nat Rev Neurol. 2019;15(3):135–47.
Teipel SJ, Schapiro MB, Alexander GE, et al. Relation of corpus callosum and hippocampal size to age in nondemented adults with Down’s syndrome. Am J Psychiatry. 2003;160(10):1870–8.
Aylward EH, Li Q, Honeycutt NA, et al. MRI volumes of the hippocampus and amygdala in adults with Down’s syndrome with and without dementia. Am J Psychiatry. 1999;156(4):564-8
Silva MVF, Loures CdMG, Alves LCV, de Souza LC, Borges KBG, Carvalho MdG. Alzheimer's disease: risk factors and potentially protective measures. J Biomed Sci. 2019;26(1):33.
Kang S, Lee Y-h, Lee JE. Metabolism-centric overview of the pathogenesis of Alzheimer's disease. Yonsei Med J. 2017;58(3):479–88.
Ruthirakuhan M, Luedke AC, Tam A, Goel A, Kurji A, Garcia A. Use of physical and intellectual activities and socialization in the management of cognitive decline of aging and in dementia: a review. J Aging Res. 2012;2012:384875.
Qiu C, Kivipelto M, von Strauss E. Epidemiology of Alzheimer’s disease: occurrence, determinants, and strategies toward intervention. Dialogues Clin Neurosci. 2009;11(2):111–28.
Mullins D, Daly E, Simmons A, et al. Dementia in Down’s syndrome: an MRI comparison with Alzheimer’s disease in the general population. J Neurodev Disord. 2013;5(1):19.
Head E, Powell DK, Schmitt FA. Metabolic and vascular imaging biomarkers in Down syndrome provide unique insights into brain aging and Alzheimer disease pathogenesis. Front Aging Neurosci. 2018;10:191.
Pinter JD, Eliez S, Schmitt JE, Capone GT, Reiss AL. Neuroanatomy of Down’s syndrome: a high-resolution MRI study. Am J Psychiatry. 2001;158(10):1659–65.
Rodrigues M, et al. Neuroimaging assessment in Down syndrome: a pictorial review. Insights Imaging. 2019;10(1):52. https://doi.org/10.1186/s13244-019-0729-3. https://www.ncbi.nlm.nih.gov/pubmed/31111268.
Croisile B, Auriacombe S, Etcharry-Bouyx F, Vercelletto M. The new 2011 recommendations of the National Institute on Aging and the Alzheimer’s Association on diagnostic guidelines for Alzheimer’s disease: preclinal stages, mild cognitive impairment, and dementia. Rev Neurol (Paris). 2012;168(6–7):471–82.
Burnes DPR, Burnette D. Broadening the etiological discourse on Alzheimer’s disease to include trauma and posttraumatic stress disorder as psychosocial risk factors. J Aging Stud. 2013;27(3):218–24.
Zhang X, Li C, Zhang M. Psychosocial risk factors of Alzheimer’s disease. Zhonghua Yi Xue Za Zhi. 1999;79(5):335–8.
Burke SL, Cadet T, Alcide A, O’Driscoll J, Maramaldi P. Psychosocial risk factors and Alzheimer’s disease: the associative effect of depression, sleep disturbance, and anxiety. Aging Ment Health. 2018;22(12):1577–84.
Kropiunigg U, Sebek K, Leonhardsberger A, Schemper M, Dal-Bianco P. Psychosocial risk factors for Alzheimer’s disease. Psychother Psychosom Med Psychol. 1999;49(5):153–9.
Persson G, Skoog I. A prospective population study of psychosocial risk factors for late onset Dementia. Int J Geriatr Psychiatry. 1996;11(1):15–22.
Mendez MF. Early-onset Alzheimer disease. Neurol Clin. 2017;35(2):263–81.
Wang H-X, Wahlberg M, Karp A, Winblad B, Fratiglioni L. Psychosocial stress at work is associated with increased dementia risk in late life. Alzheimers Dement. 2012;8(2):114–20.
Seidler A, Nienhaus A, Bernhardt T, Kauppinen T, Elo AL, Frölich L. Psychosocial work factors and dementia. Occup Environ Med. 2004;61(12):962.
He YL, Zhang XK, Zhang MY. Psychosocial risk factors for Alzheimer's disease. Hong Kong J Psychiatry. 2000;10:2–7.
Bernhardt T, Seidler A, Frölich L. The effect of psychosocial factors on risk of dementia. Fortschr Neurol Psychiatr. 2002;70(6):283–8.
Zigman WB, Lott IT. Alzheimer’s disease in Down syndrome: neurobiology and risk. Ment Retard Dev Disabil Res Rev. 2007;13(3):237–46.
Schupf N, Sergievsky GH. Genetic and host factors for dementia in Down’s syndrome. Br J Psychiatry. 2002;180:405–10.
Mann DM. Alzheimer’s disease and Down’s syndrome. Histopathology. 1988;13(2):125–37.
Bush A, Beail N. Risk factors for dementia in people with Down syndrome: issues in assessment and diagnosis. Am J Ment Retard. 2004;109(2):83–97.
Zeilinger EL, Komenda S, Zrnic I, Franken F, Woditschka K. Informant-based assessment instruments for dementia and their measurement properties in persons with intellectual disability: systematic review protocol. BMJ Open. 2020;10(12): e040920.
Zis P, Strydom A. Clinical aspects and biomarkers of Alzheimer’s disease in Down syndrome. Free Radical Biol Med. 2018;114:3–9.
Lai F, Mhatre PG, Yang Y, Wang MC, Schupf N, Rosas HD. Sex differences in risk of Alzheimer’s disease in adults with Down syndrome. Alzheimers Dement (Amst). 2020;12(1): e12084.
Schupf N, Kapell D, Nightingale B, Rodríguez Á, Tycko B, Mayeux RP. Earlier onset of Alzheimer’s disease in men with Down syndrome. Neurology. 1998;50:991–5.
Lai F, Kammann E, Rebeck GW, Anderson A, Chen YF, Nixon R. APOE genotype and gender effects on Alzheimer disease in 100 adults with Down syndrome. Neurology. 1999;53:331–6.
Temple V, Jozsvai E, Konstantareas MM, Hewitt TA. Alzheimer dementia in Down’s syndrome: the relevance of cognitive ability. J Intellect Disabil Res. 2008;45(1):47–55.
Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8(3):448–60.
Stern Y. Cognitive reserve and Alzheimer disease. Alzheimer Dis Assoc Disord. 2006;20(3 Suppl 2):S69-74.
Verghese PB, Castellano JM, Holtzman DM. Apolipoprotein E in Alzheimer’s disease and other neurological disorders. Lancet Neurol. 2011;10(3):241–52.
Bejanin A, Iulita MF, Vilaplana E, et al. Association of apolipoprotein E ɛ4 Allele with clinical and multimodal biomarker changes of Alzheimer disease in adults with Down syndrome. JAMA Neurol. 2021;78(8):937–47.
Coppus AMW, Evenhuis HM, Verberne GJ, et al. The impact of apolipoprotein E on dementia in persons with Down’s syndrome. Neurobiol Aging. 2008;29(6):828–35.
van Gool WA, Evenhuis HM, van Duijn CM. A case-control study of apolipoprotein E genotypes in Alzheimer's disease associated with Down's syndrome. Dutch Study Group on Down's Syndrome and Ageing. Ann Neurol. 1995;38(2):225–30.
Prasher VP, Sajith SG, Rees SD, et al. Significant effect of APOE epsilon 4 genotype on the risk of dementia in Alzheimer’s disease and mortality in persons with Down syndrome. Int J Geriatr Psychiatry. 2008;23(11):1134–40.
Pape SE, Baksh RA, Startin C, Hamburg S, Hithersay R, Strydom A. The association between physical activity and CAMDEX-DS changes prior to the onset of Alzheimer’s disease in Down syndrome. J Clin Med. 2021;10(9):1882.
Parrini M, Ghezzi D, Deidda G, et al. Aerobic exercise and a BDNF-mimetic therapy rescue learning and memory in a mouse model of Down syndrome. Sci Rep. 2017;7(1):16825.
Kida E, Rabe A, Walus M, Albertini G, Golabek AA. Long-term running alleviates some behavioral and molecular abnormalities in Down syndrome mouse model Ts65Dn. Exp Neurol. 2013;240:178–89.
Llorens-Martín MV, Rueda N, Tejeda GS, Flórez J, Trejo JL, Martínez-Cué C. Effects of voluntary physical exercise on adult hippocampal neurogenesis and behavior of Ts65Dn mice, a model of Down syndrome. Neuroscience. 2010;171(4):1228–40.
Walus M, Kida E, Rabe A, Albertini G, Golabek AA. Widespread cerebellar transcriptome changes in Ts65Dn Down syndrome mouse model after lifelong running. Behav Brain Res. 2016;296:35–46.
Reeves RH, Irving NG, Moran TH, et al. A mouse model for Down syndrome exhibits learning and behaviour deficits. Nat Genet. 1995;11(2):177–84.
Contestabile A, Greco B, Ghezzi D, Tucci V, Benfenati F, Gasparini L. Lithium rescues synaptic plasticity and memory in Down syndrome mice. J Clin Invest. 2012;123(1):348–61.
Costa A, Scott-McKean JJ, Stasko MR. Acute injections of the NMDA receptor antagonist memantine rescue performance deficits of the Ts65Dn mouse model of Down syndrome on a fear conditioning test. Neuropsychopharmacology. 2008;33(7):1624–32.
Duchon A, Raveau M, Chevalier C, Nalesso V, Sharp AJ, Herault Y. Identification of the translocation breakpoints in the Ts65Dn and Ts1Cje mouse lines: relevance for modeling Down syndrome. Mamm Genome. 2011;22(11):674–84.
Gardiner KJ. Pharmacological approaches to improving cognitive function in Down syndrome: current status and considerations. Drug Des Dev Ther. 2015;9:103.
Ptomey LT, Szabo AN, Willis EA, et al. Changes in cognitive function after a 12-week exercise intervention in adults with Down syndrome. Disabil Health J. 2018;11(3):486–90.
Chen CC, Ringenbach S, Crews D, Kulinna P, Amazeen EL. The association between a single bout of moderate physical activity and executive function in young adults with Down syndrome: a preliminary study. J Intellect Disabil Res. 2015;59(7):589–98.
Ringenbach SD, Albert AR, Chen CC, Alberts JL. Acute bouts of assisted cycling improves cognitive and upper extremity movement functions in adolescents with Down syndrome. Intellect Dev Disabil. 2014;52(2):124–35.
Holzapfel SD, Ringenbach SDR, Mulvey GM, et al. Improvements in manual dexterity relate to improvements in cognitive planning after assisted cycling therapy (ACT) in adolescents with Down syndrome. Res Dev Disabil. 2015;45–46:261–70.
Chen CC, Ringenbach S. Dose–response relationship between intensity of exercise and cognitive performance in individuals with Down syndrome: a preliminary study. J Intellect Disabil Res. 2016;60(6):606–14.
Ringenbach SD, Holzapfel SD, Mulvey GM, Jimenez A, Benson A, Richter M. The effects of assisted cycling therapy (ACT) and voluntary cycling on reaction time and measures of executive function in adolescents with Down syndrome. J Intellect Disabil Res. 2016;60(11):1073–85.
Chen C-C, Ringenbach SDR. The effect of acute exercise on the performance of verbal fluency in adolescents and young adults with Down syndrome: a pilot study. J Intellect Disabil Res. 2019;63(6):614–23.
Holzapfel SD, Ringenbach SDR, Mulvey GM, Sandoval-Menendez AM, Birchfield N, Tahiliani SR. Differential effects of assisted cycling therapy on short-term and working memory of adolescents with Down syndrome. J Cogn Psychol. 2016;28(8):990–1003.
Fleming V, Piro-Gambetti B, Patrick A, et al. Physical activity and cognitive and imaging biomarkers of Alzheimer’s disease in Down syndrome. Neurobiol Aging. 2021;107:118–27.
Chen CC, Spanò G, Edgin JO. The impact of sleep disruption on executive function in Down syndrome. Res Dev Disabil. 2013;34(6):2033–9.
Anstey KJ, von Sanden C, Salim A, O’Kearney R. Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. Am J Epidemiol. 2007;166(4):367–78.
Durazzo TC, Mattsson N, Weiner MW, Alzheimer's Disease Neuroimaging Initiative. Smoking and increased Alzheimer's disease risk: a review of potential mechanisms. Alzheimers Dement. 2014;10(3 Suppl):S122–45.
Wisniewski K, Howe J, Williams DG, Wisniewski HM. Precocious aging and dementia in patients with Down’s syndrome. Biol Psychiatry. 1978;13(5):619–27.
Wisniewski KE, Wisniewski HM, Wen GY. Occurrence of neuropathological changes and dementia of Alzheimer’s disease in Down’s syndrome. Ann Neurol. 1985;17(3):278–82.
Head E, Silverman W, Patterson D, Lott I. Aging and Down syndrome. Curr Gerontol Geriatrics Res. 2012;2012: 412536.
Höhne C, Messungen der regionalen Corpus-callosum-und Hippocampus-Atrophie bei nicht dementen Erwachsenen mit Down-Syndrom C. Hoehne lmu. 2007. https://doi.org/10.5282/edoc.7687.
Pearlson GD, Breiter SN, Aylward EH, et al. MRI brain changes in subjects with Down syndrome with and without dementia. Dev Med Child Neurol .1998;40(5):326–34.
Prasher VP, Cumella S, Natarajan K, Rolfe EB, Shah S, Haque MS. Magnetic resonance imaging, Down’s syndrome and Alzheimer’s disease: research and clinical implications. J Intellectual Disability Res. 2003;47(Pt 2):90–100.
Ball M, Schapiro M, Rapoport SI. Neuropathological relationships between Down syndrome and senile dementia Alzheimer type. In: Epstein CJ, editor. The neurobiology of Down syndrome. New York: Raven; 1986. p. 45–58.
Pujol J, Fenoll R, Ribas-Vidal N, et al. A longitudinal study of brain anatomy changes preceding dementia in Down syndrome. Neuroimage Clin. 2018;18:160–6.
Hyman BT, Van Hoesen GW, Damasio AR, Barnes CL. Alzheimer’s disease: cell-specific pathology isolates the hippocampal formation. Science. 1984;225(4667):1168–70.
Bobinski M, Wegiel J, Wisniewski HM, et al. Neurofibrillary pathology—correlation with hippocampal formation atrophy in Alzheimer disease. Neurobiol Aging. 1996;17(6):909–19.
Nagy Z, Jobst KA, Esiri MM, et al. Hippocampal pathology reflects memory deficit and brain imaging measurements in Alzheimer’s disease: clinicopathologic correlations using three sets of pathologic diagnostic criteria. Dementia. 1996;7(2):76–81.
Lai F, Williams RS. A prospective study of Alzheimer disease in Down syndrome. Arch Neurol. 1989;46(8):849–53.
Schapiro MB, Haxby JV, Grady CL. Nature of mental retardation and dementia in Down syndrome: Study with PET, CT, and neuropsychology. Neurobiol Aging. 1992;13(6):723–34.
Alexander GE, Saunders AM, Szczepanik J, et al. Relation of age and apolipoprotein E to cognitive function in Down syndrome adults. NeuroReport. 1997;8(8):1835–40.
Nelson LD, Orme D, Osann K, Lott IT. Neurological changes and emotional functioning in adults with Down syndrome. J Intellect Disabil Res. 2001;45(Pt 5):450–6.
Bobinski M, Leon MJd, Wegiel J, et al. The histological validation of post mortem magnetic resonance imaging-determined hippocampal volume in Alzheimer's disease. Neuroscience. 1999;95:721–5.
Yamauchi H, Fukuyama H, Harada K, et al. Callosal atrophy parallels decreased cortical oxygen metabolism and neuropsychological impairment in Alzheimer’s disease. Arch Neurol. 1993;50(10):1070–4.
Teipel SJ, Hampel H, Pietrini P, et al. Region-specific corpus callosum atrophy correlates with the regional pattern of cortical glucose metabolism in Alzheimer disease. Arch Neurol. 1999;56(4):467–73.
Teipel SJ, Hampel H, Alexander GE, et al. Dissociation between corpus callosum atrophy and white matter pathology in Alzheimer’s disease. Neurology. 1998;51(5):1381–5.
Teipel SJ, Bayer W, Alexander GE, et al. Progression of corpus callosum atrophy in Alzheimer disease. Arch Neurol. 2002;59(2):243–8.
Hampel H, Teipel SJ, Alexander GE, Pogarell O, Rapoport SI, Möller HJ. In vivo imaging of region and cell type specific neocortical neurodegeneration in Alzheimer's disease. Perspectives of MRI derived corpus callosum measurement for mapping disease progression and effects of therapy. Evidence from studies with MRI, EEG and PET. J Neural Transm (Vienna). 2002;109(5–6):837–55.
Aboitiz F, Scheibel AB, Fisher RS, Zaidel E. Fiber composition of the human corpus callosum. Brain Res. 1992;598(1–2):143–53.
Innocenti GM. General organization of callosal connections in the cerebral cortex. Sensory-motor areas and aspects of cortical connectivity: Springer; 1986. p. 291–353.
Jones EG, Peters A. Cellular components of the cerebral cortex. In: Cerebral Cortex, Vol 1. US: Springer; 1984. https://books.google.de/books?id=SxwrjwEACAAJ.
Hof PR, Morrison JH, Cox K. Quantitative analysis of a vulnerable subset of pyramidal neurons in Alzheimer's disease: I. Superior frontal and inferior temporal cortex. J Comp Neurol. 1990;301(1):44–54.
Hof PR, Morrison JH. Quantitative analysis of a vulnerable subset of pyramidal neurons in Alzheimer's disease: II. Primary and secondary visual cortex. J Comparative Neurol. 1990;301(1):55–64.
Hof PR, Morrison JH. Neocortical neuronal subpopulations labeled by a monoclonal antibody to calbindin exhibit differential vulnerability in Alzheimer’s disease. Exp Neurol. 1991;111(3):293–301.
Weis S, Jellinger K, Wenger E. Morphometry of the corpus callosum in normal aging and Alzheimer’s disease. J Neural Transm Suppl. 1991;33:35–8.
Biegon A, Eberling JL, Richardson BC, et al. Human corpus callosum in aging and Alzheimer’s disease: a magnetic resonance imaging study. Neurobiol Aging. 1994;15(4):393–7.
Vermersch P, Roche J, Hamon M, et al. White matter magnetic resonance imaging hyperintensity in Alzheimer’s disease: correlations with corpus callosum atrophy. J Neurol. 1996;243(3):231–4.
Lyoo IK, Satlin A, Lee CK, Renshaw PF. Regional atrophy of the corpus callosum in subjects with Alzheimer’s disease and multi-infarct dementia. Psychiatry Res. 1997;74(2):63–72.
Pantel J, Schroder J, Essig M, et al. Corpus callosum in Alzheimer’s disease and vascular dementia–a quantitative magnetic resonance study. J Neural Transm Suppl. 1998;54:129–36.
Yamauchi H, Fukuyama H, Nagahama Y, et al. Comparison of the pattern of atrophy of the corpus callosum in frontotemporal dementia, progressive supranuclear palsy, and Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2000;69(5):623–9.
Visser FE, Aldenkamp AP, van Huffelen AC, Kuilman M, Overweg J, van Wijk J. Prospective study of the prevalence of Alzheimer-type dementia in institutionalized individuals with Down syndrome. Am J Mental Retardation. 1997;101(4):400–12.
Holland AJ, Hon J, Huppert FA, Stevens F, Watson P. Population-based study of the prevalence and presentation of dementia in adults with Down’s syndrome. Br J Psychiatry. 1998;172:493–8.
Kesslak JP, Nagata SF, Lott I, Nalcioglu O. Magnetic resonance imaging analysis of age-related changes in the brains of individuals with Down’s syndrome. Neurology. 1994;44(6):1039–45.
Raz N, Torres IJ, Briggs SD, et al. Selective neuroanatornic abnormalities in Down's syndrome and their cognitive correlates: evidence from MRI morphometry. Neurology. 1995;45(2):356–66.
Pearson RC, Powell TP. The neuroanatomy of Alzheimer’s disease. Rev Neurosci. 1989;2(2):101–22.
Kesslak JP, Nalcioglu O, Cotman CW. Quantification of magnetic resonance scans for hippocampal and parahippocampal atrophy in Alzheimer’s disease. Neurology. 1991;41(1):51–4.
Krasuski JS, Alexander GE, Horwitz B, Rapoport SI, Schapiro MB. Relation of medial temporal lobe volumes to age and memory function in nondemented adults with Down’s syndrome: implications for the prodromal phase of Alzheimer’s disease. Am J Psychiatry. 2002;159(1):74–81.
Scahill RI, Schott JM, Stevens J, Rossor MN, Fox NC. Mapping the evolution of regional atrophy in Alzheimer’s disease: unbiased analysis of fluid-registered serial MRI. Proc Natl Acad Sci USA. 2002;99:4703–7.
Lehericy S, Baulac M, Chiras J, et al. Amygdalohippocampal MR volume measurements in the early stages of Alzheimer disease. Am J Neuroradiol. 1994;15(5):929–37.
Chan D, Fox NC, Scahill RI, et al. Patterns of temporal lobe atrophy in semantic dementia and Alzheimer’s disease. Ann Neurol. 2001;49(4):433–42.
Dickerson BC, Goncharova I, Sullivan M, et al. MRI-derived entorhinal and hippocampal atrophy in incipient and very mild Alzheimer’s disease. Neurobiol Aging. 2001;22(5):747–54.
Killiany R, Hyman B, Gomez-Isla T, et al. MRI measures of entorhinal cortex vs hippocampus in preclinical AD. Neurology. 2002;58(8):1188–96.
Johnson KA, Fox NC, Sperling RA, Klunk WE. Brain imaging in Alzheimer disease. Cold Spring Harb Perspect Med. 2012;2(4):a006213-a.
Delabar J, Blouin J, Rahmani Z, et al. Down syndrome: a model for the study of Alzheimer’s disease and aging. Early markers in Parkinson’s and Alzheimer’s Diseases. Vienna: Springer; 1990. p. 165–79.
Hartley D, Blumenthal T, Carrillo M, et al. Down syndrome and Alzheimer’s disease: common pathways, common goals. Alzheimers Dementia. 2015;11(6):700–9.
Dekker AD, Sacco S, Carfi A, et al. The behavioral and psychological symptoms of dementia in Down syndrome (BPSD-DS) scale: comprehensive assessment of psychopathology in Down syndrome. J Alzheimers Dis. 2018;63(2):797–819.
Dekker AD, Strydom A, Coppus AMW, et al. Behavioural and psychological symptoms of dementia in Down syndrome: early indicators of clinical Alzheimer’s disease? Cortex. 2015;73:36–61.
Wissing MBG, Ulgiati AM, Hobbelen JSM, De Deyn PP, Waninge A, Dekker AD. The neglected puzzle of dementia in people with severe/profound intellectual disabilities: a systematic literature review of observable symptoms. J Appl Res Intellect Disabil. 2022;35(1):24–45.
Kim J, Basak JM, Holtzman DM. The role of apolipoprotein E in Alzheimer’s disease. Neuron. 2009;63(3):287–303.
Hyman BT, West HL, Rebeck GW, et al. Quantitative analysis of senile plaques in Alzheimer disease: observation of log-normal size distribution and molecular epidemiology of differences associated with apolipoprotein E genotype and trisomy 21 (Down syndrome). Proc Natl Acad Sci. 1995;92(8):3586–90.
Shiekh SI, Cadogan SL, Lin L-Y, Mathur R, Smeeth L, Warren-Gash C. Ethnic differences in dementia risk: a systematic review and meta-analysis. J Alzheimers Dis. 2021;80(1):337–55.
Burt DB, Aylward EH, Working Group for the Establishment of Criteria for the Diagnosis of Dementia in Individuals with Intellectual Disability. Test battery for the diagnosis of demntia in individuals with intellectual disability. J Intellect Disabil Res. 2000;44(2):175–80.
Aylward EH, Burt DB, Thorpe LU, Lai F, Dalton A. Diagnosis of dementia in individuals with intellectual disability. J Intellect Disabil Res. 1997;41(2):152–64.
Nieuwenhuis-Mark RE. Diagnosing Alzheimer’s dementia in Down syndrome: problems and possible solutions. Res Dev Disabil. 2009;30(5):827–38.
Acknowledgements
We want to thank Dr. Gonzalo Alvarez-Bolado (Department of Neuroanatomy, Institute of Anatomy and Cell Biology, University of Heidelberg) for his contributions by comments and corrections during the preparation of this manuscript.
Funding
This work is part of a doctoral research project funded by the Friedrich-Naumann Foundation for Freedom (Scholar Number 8683/P611, 2021). The funder had no role in the design and conduct of the study, collection, analysis, and interpretation of data, preparation of the manuscript, or the review or approval of the manuscript. The authors funded the journal’s Rapid Service Fee.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study’s conception and design. Osama Hamadelseed, Ibrahim H. Elkhidir, and Thomas Skutella performed material preparation, data collection, and analysis. Osama Hamadelseed wrote the first draft of the manuscript, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Osama Hamadelseed, Ibrahim H. Elkhidir, and Thomas Skutella declare that they have no conflict of interest.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
This paper does not qualify for data sharing since we created no datasets or evaluated them during the research, but we reviewed data from the literature.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hamadelseed, O., Elkhidir, I.H. & Skutella, T. Psychosocial Risk Factors for Alzheimer’s Disease in Patients with Down Syndrome and Their Association with Brain Changes: A Narrative Review. Neurol Ther 11, 931–953 (2022). https://doi.org/10.1007/s40120-022-00361-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-022-00361-9