Abstract
Introduction
Concentrations of plasma biomarkers associated with Alzheimer’s disease have been reported to be as low as several tens of picograms/milliliter (pg/ml). However, in assays measuring these biomarkers, it is likely that repeated measurements are necessary to obtain reliable values.
Methods
We performed assays as a single test or as duplicate, quadruplicate, fivefold and tenfold repeated tests, on samples spiked with different concentrations of amyloid β 1–40 (Aβ1–40; 1–1000 pg/ml), Aβ1–42 (1–30,000 pg/ml) and total Tau protein (T-Tau; 0.1–1000 pg/ml), with the aim to to calculate the coefficients of variation (CVs).
Results
The results demonstrated common changes in the CVs with changes in the number of tests for a given sample: the CVs decreased with increases in the number of tests from one to ten. All CV values were distributed within the range of 0.35 to 15.5%; as such, the CV values were all lower than the acceptable value of 20%.
Conclusion
Based on this study, a single assay of Aβ1–40, Aβ1–42 and T-Tau, respectively, provides reliable results in terms of the measurement of that plasma biomarker.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Ultrasensitive systems are increasingly being used to detect dementia by detecting proteins at ultralow concentrations in blood samples. However, to date there are no scientific data to show how many analytical replicates are needed to ensure reliable plasma biomarker measurements. |
In this study, we applied the immunomagnetic reduction (IMR) platform to investigate how many measurements are necessary to obtain reliable values. |
What was learned from the study? |
The plasma total Tau protein (T-Tau) concentration determined in a single test was found to have the same clinical significance for left hippocampus atrophy as that obtained in duplicate tests. |
The measured plasma T-Tau concentrations determined in a single test showed equivalent significance for monitoring hippocampus atrophy to that obtained in duplicate tests. |
For clinical samples, the effectiveness of a single IMR test was as effective as the duplicate test for discriminating normal subjects and patients with Alzheimer's disease. |
Introduction
Plasma biomarkers related to pathology have become important parameters for the assessment of Alzheimer’s disease (AD) [1]. Although the concentrations of these biomarkers, such as amyloid β 1–40 (Aβ1–40), Aβ1–42 and total Tau protein (T-Tau), have been observed to be very low, assays of these plasma biomarkers are feasible due to the successful development of ultrasensitive assay technologies [2,3,4,5,6,7], such as immunomagnetic reduction (IMR) [7]. Many research groups have validated the clinical significance of discriminating AD or amnesic mild cognitive impairment (aMCI) from normal controls (NCs) [8,9,10]. In addition, correlations between plasma Aβ1–42/Aβ1–40 and Aβ plaques that were obtained using positron emission tomography (PET) have been demonstrated [11, 12]. The elevation of plasma T-Tau levels caused by atrophy of the brain (especially in the hippocampus) has also been observed [12, 13]. All of these previous results have demonstrated that assays of plasma Aβ1–40, Aβ1–42 and T-Tau using IMR are useful for the diagnosis of AD in clinical practice. Consequently, assays of plasma Aβ1–40, Aβ1–42 and T-Tau using IMR have been approved for clinical uses in Europe and Taiwan.
In previously published studies [7,8,9,10,11,12,13], biomarkers using IMR have been measured in duplicate. The original reason underlying the need for duplicate measurements using IMR was the ultralow concentrations of these plasma biomarkers, present approximately at concentrations of picograms per milliliter (pg/ml); to obtain reliable results, therefore, the measurement procedure was based on duplicate measurements. However, there are no scientific results to demonstrate that even duplicate measurements are needed for assaying such low biomarker concentrations; it may be that three or more measurements are necessary to obtain reliable results.
In the present study, we examined the coefficients of variation (CVs) of measured concentrations of Aβ1–40, Aβ1–42 and T-Tau in cases of a single test and tests carried out in duplicate, quadruplicate, fivefold and tenfold. The number of tests required to obtain reliable results was also determined. In addition, 242 subjects at four hospitals were enrolled in 2015 and 2016, including 134 cognitively normal controls and 108 patients with aMCI or AD [14]. The plasma Aβ1–42, Aβ1–40 and T-Tau concentrations of the duplicate tests have been previously reported. The correlations between hippocampal volume and measured plasma T-Tau concentrations, as well as the agreement between clinical diagnoses and plasma biomarker diagnoses, have also been investigated. In the present study, instead of using the results of duplicate measurements, we used the concentrations of a single test for Aβ1–42, Aβ1–40 and T-Tau to explore the correlations between hippocampal volume and measured plasma T-Tau concentrations, as well as the agreement between clinical diagnoses and plasma biomarker diagnoses.
Methods
Preparation of Biomarker-Phosphate-Buffered Saline (PBS) Samples
Amyloid β 1–40 (A1075; Sigma-Aldrich, St. Louis, MO, USA), Aβ1–42 (A9810; Sigma-Aldrich) and T-Tau (T7951; Sigma-Aldrich) were separately spiked into PBS solution (pH 7.4) to obtain the Aβ1–40, Aβ1–42 and T-Tau samples. The spiked concentrations of the Aβ1–40 samples ranged from 1 to 1000 pg/ml; those of the Aβ1–42 samples ranged from 1 to 30,000 pg/ml; and the spiked concentrations of T-Tau samples ranged from 0.1 to 1000 pg/ml.
Analysis of CVs of Multiple Tests for Biomarker–Phosphate-Buffered Saline Samples
Immunomagnetic reduction reagents for assaying Aβ1–40, Aβ1–42 and T-Tau in the biomarker–phosphate buffered saline (PBS) samples were used (MF-AB0-0060, MF-AB2-0060, MF-TAU-0060; MagQu Co. Ltd., New Taipei City, Taiwan). For each measurement, 80, 60 and 80 μl of reagents were mixed with 40, 60 and 40 μl, respectively, of biomarker–PBS samples. The concentrations of Aβ1–40, Aβ1–42 and T-Tau in a biomarker–PBS sample were detected using an IMR analyzer (XacPro-S; MagQu Co. Ltd.). For a given concentration of a biomarker, 20 measurements were performed (Table 1). With these two sets of data, which were denoted as sn with n = 1–20, the CVs for a single test and for duplicate, quadruplicate, fivefold repeated and tenfold repeated tests were calculated as follows:
-
In the case of a single test, the CV (%) was expressed as:
$$ {\text{CV}}\;(\% ) = \frac{{{\text{SD}}\;{\text{of}}\;\left\{ {s_{n} } \right\}}}{{{\text{Mean}}\;{\text{value}}\;{\text{of}}\;\left\{ {s_{n} } \right\}}} \times 100\% , $$(1)where SD denotes the standard deviation (n = 1–20).
-
In the case of duplicate tests, the CV (%) was expressed as:
$$ {\text{CV}}\;(\% ) = \frac{{{\text{SD}}\;{\text{of}}\;\left\{ {d_{n} } \right\}}}{{{\text{Mean}}\;{\text{value}}\,{\text{of}}\; \left\{ {d_{n} } \right\}}} \times 100\% , $$(2)where dn = (s2n + s2n−1)/2 and n = 1–10.
-
In the case of quadruplicate tests, the CV (%) was expressed as:
$$ {\text{CV}}\;(\% ) = \frac{{{\text{SD}}\,{\text{of}}\, \left\{ {q_{n} } \right\}}}{{{\text{Mean}}\;{\text{value}}\;{\text{of}} \left\{ {q_{n} } \right\}}} \times 100\% , $$(3)where qn = (d2n + dsn−1)/2 and n = 1–5.
-
In the case of fivefold repeated tests, the CV (%) was expressed as:
$$ {\text{CV}}\,(\% ) = \frac{{{\text{SD}}\,{\text{of}}\;\left\{ {f_{n} } \right\}}}{{{\text{Mean}}\;{\text{value}}\;{\text{of}} \left\{ {f_{n} } \right\}}} \times 100\% , $$(4)wherein fn = (\((\sum\nolimits_{5n - 4}^{5n} {s_{n} } )/5\), and n = 1–4.
-
In the case of tenfold repeated tests, the CV (%) was expressed as:
$$ {\text{CV}}\,(\% ) = \frac{{{\text{SD}}\;{\text{of}}\;\left\{ {t_{n} } \right\}}}{{{\text{Mean}}\;{\text{value}}\;{\text{of}} \left\{ {t_{n} } \right\}}} \times 100\% , $$(5)wherein tn = (f2n + fsn−1)/2 and n = 1, 2.
Recruitment of Subjects
A total of 242 subjects were enrolled from the memory clinics of the Taipei Medical University Shuang-Ho Hospital, the Renai Branch of Taipei City Hospital, the En Chu Kong Hospital and the National Taiwan University Hospital (master), from 2015 to 2016 [14]. Exclusion criteria were neurologic diseases that affect brain structure, such as epilepsy head injury or stroke; medical diseases involving cardiopulmonary failure; hepatic or renal failure; and poor control of diabetes (HbA1c > 8.5). A neuropsychological test (NPT) battery was performed by a Board-certified clinical neuropsychologist to help demarcate mild changes in the cognition and normal daily function of those subjects with MCI. Those subjects who had a Geriatric Depression Scale (GDS) score ≥ 8 were excluded from the study. In addition, the subjects were required to have had at least 6 years of formal education or to be capable of reading and writing in Chinese to complete the comprehensive NPT battery. The diagnostic criteria for MCI due to AD, as well as the criteria for dementia due to AD, followed the National Institute on Aging/Alzheimer's Association Diagnostic Guidelines [15,16,17]. All of the subjects and/or their primary caregivers provided written informed consent prior to their participation in this investigation. This study was approved by the ethics committees and institute review boards of the involved hospitals (National Taiwan University Hospital: 201406125DS; En Chu Kong Hospital: 1040102; Renai Branch of Taipei City Hospital: 1031203; Taipei Medical University Shuang-Ho Hospital: 201408011) and was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments.
Preparation of Human Plasma
Blood samples were collected in a 6-ml EDTA blood collection tube. The collected blood was centrifuged at 1500–2500 g for 15 min at room temperature with a swing-bucket rotor, followed by transfers of each 1 ml of plasma to a 0.5-ml microcentrifuge tube and storage at − 80 °C until biomarker assays were performed. All of the plasma samples were packaged in dry ice and shipped to the National Taiwan University Hospital in Taipei City, Taiwan, for blind testing of plasma biomarkers.
Assays of Plasma Biomarkers
Plasma biomarkers were assayed using IMR, with IMR kits MF-AB0-0060, MF-AB2-0060 and MF-TAU-0060 (MagQu Co. Ltd.) for assaying Aβ1–40, Aβ1–42 and T-Tau, respectively, and IMR analyzer model XacPro-S (MagQu Co. Ltd.). For assaying Aβ1–40, Aβ1–42 and T-Tau, 80, 60 and 80 μl of reagents were mixed with 40, 60 and 40 μl of plasma, respectively, for a single measurement. Duplicate measurements were conducted for each biomarker per sample and are denoted as the first measurement and second measurement hereafter.
Magnetic Resonance Imaging Scans
High-resolution structural brain magnetic resonance imaging (MRI) scans were acquired by using a 1.5 T MRI scanner (EXCITE; General Electric Co., Boston, MA, USA), as described in [13]. The MRI images were corrected for intensity inhomogeneities and reoriented, after which they were registered against the MNI 152 space by using FSL (FMRIB Software Library; Analysis Group, FMRIB, Oxford) tools [18]. The FIRST and SIENAX FSL tools were used to extract the relevant regions of interest and to calculate the volumes of the right and left hippocampus [19].
Statistical Methods
The continuous variables for each measurement are presented as the mean ± standard deviation (SD). The continuous variables were compared by using Spearman correlation, t tests and p values.
Results
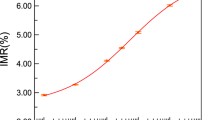
Using Eqs. (1)–(5), the CVs (%), as functions of the number of tests for Aβ1–40, Aβ1–42 and T-Tau at various concentrations, were calculated; these are shown in Fig. 1a–c, respectively. The number of tests ranged from a single test (n = 1) to the test repeated tenfold (n = 10). The curves in Fig. 1a–c can be seen to have common trends. First, all of the CVs (%) are < 20%. Second, CVs (%) obtained from a single test have the highest values; for example, the CV (%) for the single test of 1 pg/ml Aβ1–40 was 12.2%, that for 1 pg/ml Aβ1–42 was 15.0% and that for 0.1 pg/ml T-Tau was 15.5%. Third, the CV (%) decreased with increasing number of tests from one to five and remained almost unchanged as the number of tests increased to > 5; this indicated that the CV (%) was significantly suppressed by multiple measurements (for example, at the fivefold repeated test).
According to previously reported studies on bioanalytical method validation [20,21,22], the acceptable CV (%) for clinical use should be < 20–30%. As shown in Fig. 1a–c, the highest value of CV (%) for individual biomarkers occurred in the case of a single test, i.e. number of tests = 1. These highest values of CV (%) for these three biomarkers were < 20%, indicating that the measured results of a single test for Aβ1–40, Aβ1–42 and T-Tau were reliable, even at ultralow concentrations in the pg/ml range.
A single test for assaying Aβ1–40 in human plasma was performed. Two rounds of single-test measurements were performed (i.e. first and second measurement, respectively). The correlation of the measured Aβ1–40 concentrations between the first measurement and second measurement is shown in Fig. 2a. The slope of the linearity in Fig. 2a was 0.99, and the coefficient of determination (R2) was 0.987; these values demonstrated the high consistency between the two rounds of a single test for Aβ1–40 in human plasma by using IMR.
The consistency in the measured plasma Aβ1–42 and T-Tau concentrations between the first measurement and second measurement was also investigated. The results are shown in Fig. 2b, c. For plasma Aβ1–42 (Fig. 2b), the slope of the linearity was 0.99 and the R2 was 0.995; for plasma T-Tau (Fig. 2c), the slope of the linearity was 0.96 and the R2 was 0.950. These results demonstrate the high consistency between the two rounds of a single test for Aβ1–42 and T-Tau in human plasma using IMR. In a next step, we investigated whether the difference/performance is affected when the CV varies to the extremes of the concentration range. Analysis of the CVs of the lowest and highest three concentrations of biomarkers in the clinical samples demonstrated that: (1) for Aβ1–40 measurements, the CV values of the lowest and highest three concentrations were 4.37–8.62% and 6.90–12.58%, respectively, which are lower than the standard CV value of 20%; (2) for Aβ1–42 measurements, the CV values of the lowest and highest three concentrations were 1.32–1.68% and 1.50–14.51%, respectively, which are lower than the standard CV value of 20%; (3) for Tau measurements, the CV values of the lowest and highest three concentrations were 7.27–12.73% and 1.50–14.51%, respectively, which are lower than the standard CV value of 20%. These results show that for clinical samples with extreme values, the CV value can still be within 20% and, consequently, that the measured concentrations of Aβ1–40, Aβ1–42 and T-Tau in a single test using IMR are reliable.
Discussion
In studies utilizing IMR published so far [7,8,9,10,11,12,13,14], the concentration of plasma samples of Aβ1–40, Aβ1–42 or T-Tau represented the averaged value of duplicate measurements. It has also been observed that plasma T-Tau is negatively correlated with hippocampal volume [12, 13]. Aβ1–42 × T-Tau or Aβ1–42/Aβ1–40 in plasma has been shown to discriminate NCs from subjects with aMCI and AD [8,9,10]. These results reveal the impacts of plasma biomarkers on clinical applications, such as in assisting in the diagnosis of AD, the prediction of cognitive decline in aMCI [23, 24], assessment of results from neurological imaging studies [11, 25] and the monitoring of interventions, among other impacts. The authors of an earlier study reported that there was a negative correlation between plasma and cerebral spinal fluid Aβ1–42 levels in patients with AD (r = − 0.352) [26], suggesting that IMR is no less useful than single molecule array (SIMOA; r = 0.288) testing in clinical applications [27]. According to the results shown in Figs. 1 and 2, reliable measurements of plasma Aβ1–40, Aβ1–42 or T-Tau concentrations were achieved in a single test by using IMR. This result was the underlying motivation to investigate the associations of plasma biomarkers that were obtained in a single test with the use of MRI and clinical diagnoses.
Two subjects withdrew their consent after blood sampling and diagnosis based on the MRI scan. A total of 240 enrolled subjects underwent MRI scans to analyze the right hippocampal volume and left hippocampal volume (Table 2). Two rounds of single-test T-Tau plasma concentrations with the use of IMR (referred to as the first and second measurement , respectively) were performed. The relationships between the left hippocampal volume and the first measurement of T-Tau concentration are plotted in Fig. 3a. The measured plasma T-Tau concentration was found to increase with decreasing hippocampal volume. Additionally, we observed a negative correlation between hippocampal volume and plasma T-Tau levels. This result is consistent with that reported in a previous study [13] and indicates that atrophy of the hippocampus results in an elevation of plasma T-Tau. The Spearman correlation coefficient in Fig. 3a was found to be − 0.4723 (p < 0.0001). Figure 3b shows the relationship between the left hippocampal volume and the second measurement of T-Tau concentration. The Spearman correlation coefficient was found to be − 0.4446 (p < 0.0001). The measured T-Tau concentrations of the first and second measurements for a subject were averaged and referred to as duplicate measurements. The averaged T-Tau concentrations versus the left hippocampal volume are plotted in Fig. 3c. The Spearman correlation coefficient was found to be − 0.4767 (p < 0.0001). The values of the Spearman correlation coefficient of the first measurement, second measurement and duplicate measurements were similar to each other (approximate range − 0.4446, − 0.4767), which indicates that the plasma T-Tau concentration obtained in a single test has the same clinical significance for left hippocampal atrophy as that obtained in duplicate tests.
Relationships between left hippocampal volume and measured plasma Tau concentrations in two rounds of a single test, referred to as the 1st measurement (a), 2nd measurement (b) and duplicate measurements (c). d–f Relationships between right hippocampal volume and measured plasma Tau concentrations in two rounds of single tests and duplicate measurements
Figure 3d–f plot the relationships between the right hippocampal volume and plasma T-Tau in the first measurement, second measurement and duplicate measurements. Negative correlations were found in Fig. 3d–f, with Spearman correlation coefficients of − 0.4267, − 0.4081 and − 0.4306 (p < 0.0001), respectively. Thus, the measured plasma T-Tau concentrations obtained in a single test showed equivalent significance in monitoring hippocampal atrophy to that obtained in duplicate tests.
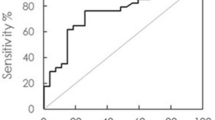
Among the enrolled subjects, 132 were NCs (mean age 67.6 ± 7.7 years), 34 were patients with MCI due to AD (aMCI; mean age 71.5 ± 8.9 years) and 74 were patients with AD dementia (mean age: 77.2 ± 8.9 years). For the purposes of this study, we combined the aMCI and AD patients to represent the patient group (Table 3). According to a previously published study [8], the cutoff value of plasma Aβ1–42 × T-Tau using IMR that discriminates patients from NCs is 455.49 pg/ml2. Using the single-test concentrations of Aβ1–42 and T-Tau in the plasma, the subjects showing Aβ1–42 × T-Tau values that are not lower than 455.49 pg/ml2 were regarded as being positive, whereas subjects showing Aβ1–42 × T-Tau values that are lower than 455.49 pg/ml2 were regarded as being negative. The agreement between the clinical diagnosis and the plasma biomarker diagnosis using single-test Aβ1–42 × T-Tau was analyzed, as shown in Table 3. Two rounds of single tests were performed (1st and 2nd measurements, respectively). Both the agreements of these two rounds of a single test and the duplicate tests are listed in Table 3. The Aβ1–42 and T-Tau concentrations in the duplicate measurements are presented as the averaged values of those concentrations in the 1st measurement and 2nd measurement. Although the duplicate tests showed slightly higher agreements than those of the first measurement and second measurement, the agreements in all of the cases were > 0.85 (or 85%). Thus, the single-test plasma Aβ1–42 × T-Tau assay using IMR is a promising parameter to discriminate NCs from patients with MCI due to AD and AD.
In addition to discriminating between patients and NCs, plasma Aβ1–42 × T-Tau showed promise to differentiate AD from aMCI, with a cutoff value of 642.58 pg/ml2, as has been previously reported [8]. The data used in Table 3 were further analyzed to investigate the agreement between the clinical diagnosis and the plasma biomarker diagnosis using Aβ1–42 × T-Tau for discriminating AD from aMCI. In Table 4, the overall percentage agreement in the duplicate measurements was 82.4%, which was higher than those in the first measurement and second measurement by 5.5%. In fact, the overall percentage agreement in a single test was 76.9%, which is sufficient for the clinical purpose of discriminating AD from aMCI.
Another plasma biomarker index to differentiate NCs from patients with AD and aMCI is Aβ1–42/Aβ1–40. According to a previously published study, the cutoff value to discriminate NCs from patients was 0.325 [8]. Hence, subjects showing Aβ1–42/Aβ1–40 values that were not < 0.325 were regarded as being positive, and subjects with Aβ1–42/Aβ1–40 values that were < 0.325 were regarded as being negative. The agreements between the clinical diagnosis and the plasma biomarker diagnosis using single-test Aβ1–42/Aβ1–40 were also analyzed, as shown in Table 5. Notably, two rounds of single tests were performed in this study ( 1st measurement and 2nd measurement). The averaged values of those tests in the first measurement and second measurement were reported as Aβ1–42 and T-Tau concentrations in the duplicate tests. In Table 5, the agreement between the two rounds of single tests (1st measurement and 2nd measurement), duplicate tests and clinical diagnosis are shown. Regardless of whether a single test or duplicate tests were performed, the agreements were > 0.85 (or 85%). Similar to the case of plasma Aβ1–42 × T-Tau, single-test plasma Aβ1–42/Aβ1–40 using IMR represents a promising parameter for differentiating NCs from patients with MCI due to AD and AD.
There are several limitations in this study. First, the clinical samples were re-analyzed using the original duplicate data. More subjects with single measurements should be enrolled to further validate the discrimination in patients with AD and NCs. Second, this is a cross-sectional study. Therefore, a longitudinal study is needed to confirm whether the feasibility is as good as suggested by the results of this cross-sectional study.
Conclusion
Both the analytical performance and the clinical results demonstrated the reliability of the single-test assay of Aβ1–40, Aβ1–42 and T-Tau using IMR. The clinical equivalence between a single test and duplicate tests was also demonstrated. The measured plasma Aβ1–42 × T-Tau and Aβ1–42/Aβ1–40 in a single test showed > 85% agreement with the clinical diagnosis for assessing aMCI and AD.
References
O’Bryant SE, Mielke MM, Rissman RA, et al. Blood-based biomarkers in Alzheimer disease: current state of the science and a novel collaborative paradigm for advancing from discovery to clinic. Alzheimers Dement. 2017;13:45–58.
Xia W, Yang T, Shankar G, et al. A specific enzyme-linked immunosorbent assay for measuring beta-amyloid protein oligomers in human plasma and brain tissue of patients with Alzheimer disease. Arch Neurol. 2009;66:190–9.
Oh ES, Mielke MM, Rosenberg PB, et al. Comparison of conventional ELISA with electrochemiluminescence technology for detection of amyloid-β in plasma. J Alzheimers Dis. 2010;21:769–73.
Birkmann E, Henke F, Weinmann N, et al. Counting of single prion particles bound to a capture-antibody surface (surface-FIDA). Vet Microbiol. 2007;123:294–304.
Kim JS, Ahn HS, Cho SM, Lee JE, Kim YS, Lee C. Detection and quantification of plasma amyloid-β by selected reaction monitoring mass spectrometry. Anal Chim Acta. 2014;840:1–9.
Mondello S, Buki A, Barzo P, et al. CSF and plasma amyloid-β temporal profiles and relationships with neurological status and mortality after severe traumatic brain injury. Sci Rep. 2014;4:6446–511.
Chiu MJ, Horng HE, Chieh JJ, et al. Multi-channel SQUID-based ultrahigh-sensitivity in-vitro detections for bio-markers of Alzheimer’s disease via immunomagnetic reduction. IEEE Trans Appl Supercond. 2011;21:477–80.
Chiu MJ, Yang SY, Horng HE, et al. Combined plasma biomarkers for diagnosing mild cognition impairment and Alzheimer’s disease. ACS Chem Neurosci. 2013;4:1530–6.
Lue LF, Sabbagh MN, Chiu MJ, et al. Plasma levels of Aβ42 and Tau identified probable Alzheimer’s dementia: findings in two cohorts. Front Aging Neurosci. 2017;9:226.
Jiao F, Yi F, Wang Y,et al. The validation of multifactor model of plasma Aβ42 and total-Tau in combination with MoCA for diagnosing probable Alzheimer disease. Front Aging Neurosci. 2020;12:212.
Tzen KY, Yang SY, Chen TF, et al. Plasma Aβ but not Tau is related to brain PiB retention in early Alzheimer’s disease. ACS Chem Neurosci. 2014;5:830–6.
Fan LY, Tzen KY, Chen YF, et al. The relation between brain amyloid deposition, cortical atrophy, and plasma biomarkers in amnesic mild cognitive impairment and Alzheimer’s disease. Front Aging Neurosci. 2018;10:175.
Chiu MJ, Chen YF, Chen TF, et al. Plasma Tau as a window to the brain-negative associations with brain volume and memory function in mild cognitive impairment and early Alzheimer’s disease. Hum Brain Mapp. 2014;35:3132–42.
Chiu MJ, Chen TF, Hu CJ, et al. Nanoparticle-based immunomagnetic assay of plasma biomarkers for differentiating dementia and prodromal states of Alzheimer’s disease—a cross-validation study. Nanomed Nanotechnol Biol Med. 2020;26:10218.
Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:280–92.
McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9.
Jack CR Jr, Albert MS, Knopman DS, et al. Introduction to the recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:257–62.
Smith SM, Jenkinson M, Woolrich MW, et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23:S208–19.
Patenaude B, Smith SM, Kennedy D, Jenkinson M. A Bayesian model of shape and appearance for subcortical brain. Neuroimage. 2011;6:907–22.
DeSilva B, Smith W, Weiner R, et al. Recommendations for the bioanalytical method validation of ligand-binding assays to support pharmacokinetic assessments of macromolecules. Pharm Res. 2003;20:1885–900.
Smolec JM, DeSilva B, Smith W, et al. Bioanalytical method validation for macromolecules in support of pharmacokinetic studies. Pharm Res. 2005;22:1425–31.
Viswanathan CT, Bansal S, Booth B, et al. Quantitative bioanalytical methods validation and implementation: best practices for chromatographic and ligand binding assays. Pharm Res. 2007;24:1962–73.
Chen TB, Lee YJ, Lin SY, et al. Plasma Aβ42 and total Tau predict cognitive decline in amnestic mild cognitive impairment. Sci Rep. 2019;9:13984.
Tsai CL, Liang CS, Yang CP, et al. Indicators of rapid cognitive decline in amnestic mild cognitive impairment: the role of plasma biomarkers using magnetically labeled immunoassays. J Psychiatr Res. 2020;129:66–72.
Wang PN, Lin KJ, Liu HC, et al. Plasma pyroglutamate-modified amyloid beta differentiates amyloid pathology. Alzheimers Dement. 2020;12:e12029.
Teunissen CE, Chiu MJ, Yang CC, et al. Plasma amyloid-β (Aβ42) correlates with cerebrospinal fluid Aβ42 in Alzheimer’s disease. J Alzheimers Dis. 2018;62(4):1857–63.
Janelidze S, Stomrud E, Palmqvist S, et al. Plasma β-amyloid in Alzheimer’s disease and vascular disease. Sci Rep. 2016;31(6):26801.
Acknowledgements
The authors thank MagQu Co., Ltd., for providing the IMR reagents for this study.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the MagQu Co., Ltd.
Statistical Analysis and Other Assistance
Prism version 6 software (Graphpad Software Inc., San Diego, CA, USA) was used to calculate the mean, SD, Spearman correlation coefficent and t tests of the continuous variables.
Authorship
All of the named authors take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Authors’ Contributions
Huei-Chun Liu, Chia-Chun Lin and Shieh-Yueh Yang designed the study. Huei-Chun Liu and Shieh-Yueh Yang performed the statistical analysis. Shieh-Yueh Yang prepared the manuscript. Hsin-Hsien Chen and Ming-Jang Chiu performed the IMR measurements. Ming-Jang Chiu analyzed the MRI data. Chia-Shin Ho and Jui-Feng Chang prepared the IMR reagents. Ming-Jang Chiu, Ta-Fu Chen, Chaur-Jong Hu, Sui-Hing Yan and Yu Sun enrolled the subjects and performed the neurological tests for the participants.
Disclosures
Huei-Chun Liu, Hsin-Hsien Chen, Chia-Shin Ho, Jui-Feng Chang, Chia-Chun Lin and Shieh-Yueh Yang are employees of MagQu Co., Ltd. Ming-Jang Chiu, Ta-Fu Chen, Chaur-Jong Hu, Sui-Hing Yan and Yu Sun have nothing to disclose.
Compliance with Ethics Guidelines
All of the subjects and/or their primary caregivers provided written informed consent prior to their participation in this investigation. This study was approved by the ethics committees and institute review boards of the involved hospitals (National Taiwan University Hospital: 201406125DS; En Chu Kong Hospital: 1040102; Renai Branch of Taipei City Hospital: 1031203; Taipei Medical University Shuang-Ho Hospital: 201408011) and was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
All of the data generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Liu, HC., Chen, HH., Ho, CS. et al. Investigation of the Number of Tests Required for Assaying Plasma Biomarkers Associated with Alzheimer’s Disease Using Immunomagnetic Reduction. Neurol Ther 10, 1015–1028 (2021). https://doi.org/10.1007/s40120-021-00280-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-021-00280-1