Abstract
Introduction
The effectiveness of tafamidis for the treatment of transthyretin familial amyloid polyneuropathy (TTR-FAP) was evaluated using data from the Transthyretin Amyloidosis Outcomes Survey (THAOS) registry.
Methods
Subjects receiving tafamidis (n = 252) were compared with untreated subjects in a non-randomized, matched cohort analysis. Subjects were matched with up to four untreated controls by genetic mutation, region of birth, and mean treatment propensity score.
Results
The matched, treated sample consisted predominantly of subjects with the Val30Met genotype (92.5%), from Portugal, and with a mean age of 40.4 years. Over the course of the 2-year follow-up period, subjects treated with tafamidis showed significantly less deterioration on the Neuropathy Impairment Score for Lower Limbs (p < 0.001) and its subscales (p < 0.023) compared with untreated subjects. There was significantly less deterioration among tafamidis-treated subjects compared with untreated subjects on the Norfolk Quality of Life scale (p < 0.001). There were no significant differences observed in functional (assessed by Karnofsky Performance Status Scale score) or nutritional (assessed by modified body mass index) status between the treated and untreated groups. The primary model which examined survival from baseline using the matched cohort was not able to yield estimates of the hazard ratio, as there were no deaths in the tafamidis-treated subjects.
Conclusion
These findings support the results from clinical trials and strengthen evidence of the effectiveness of tafamidis beyond conventional clinical trials.
Trial Registration
ClinicalTrials.gov: NCT00628745
Funding
Pfizer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transthyretin familial amyloid polyneuropathy (TTR-FAP) is a rare, life-threatening, autosomal-dominant illness caused by TTR gene mutations that result in the deposition of amyloid fibrils in peripheral nerves and organs [1,2,3]. The disease is predominantly characterized by debilitating sensorimotor and autonomic polyneuropathy, but complications due to organ involvement are common [4]. Of the more than 100 TTR genotypes identified, the most common is Val30Met [5,6,7,8].
Survival time from disease onset to death is approximately 10 years on average [2, 3, 9], but this may vary by genotype and phenotype. For example, in a study in France, Val30Met patients with a later onset of disease (median age 64 years), together with patients with the Ile107Val mutation, showed a more rapid and severe disease progression than did more slowly progressing Portuguese Val30Met patients with an earlier onset of disease (median age 32 years) and patients with the Ser77Tyr mutation [10]. Liver transplantation is a recognized treatment option for selected Val30Met patients in the early stages of TTR-FAP. However, transplantation is associated with the risk of mortality and the need for lifelong immunosuppressant therapy, and recent evidence suggests that survival rates are lower in patients with mutations other than Val30Met [11, 12].
Tafamidis, a highly specific TTR-stabilizer, is the only approved medicine to delay progression of TTR-FAP and has emerged as the new standard of care [13]. While the efficacy and safety of tafamidis in the treatment of TTR-FAP have been demonstrated in clinical trials, little is known about its real-world effectiveness [14,15,16,17,18]. In one recent observational study of approximately 3000 Val30Met patients from Portuguese referral centers, both liver transplantation and treatment with tafamidis were associated with a survival benefit when compared with untreated patients [19].
The Transthyretin Amyloidosis Outcomes Survey (THAOS) is the largest ongoing international disease registry collecting longitudinal data in patients with amyloid TTR (ATTR) amyloidosis [20]. Comprising data from symptomatic and asymptomatic patients who may be either treated or untreated, THAOS offers a valuable opportunity to study the real-world effectiveness of treatments. The objective of the current study was to examine the effectiveness of tafamidis among patients enrolled in THAOS using matching techniques to allow meaningful comparison with an untreated control group.
Materials and Methods
Study Design
The present analysis is a non-randomized, matched cohort analysis of longitudinal data, up to 2 years from baseline, among patients enrolled in THAOS. Details regarding the basic design and methodology of THAOS (ClinicalTrials.gov: NCT 00628745) are described elsewhere [20]. THAOS is an observational registry for which any individual with a confirmed TTR mutation or wild-type ATTR amyloidosis is eligible, and includes some patients participating in ongoing clinical trials [20]. All study sites received ethical or institutional review board approval prior to subject enrollment, and each subject provided written informed consent. The study followed the International Conference on Harmonisation Good Clinical Practice guidelines and the principles of the Declaration of Helsinki.
Study Population
This analysis included subjects with confirmed TTR mutations (subjects with wild-type ATTR were excluded) who were symptomatic at enrollment or became symptomatic post enrollment, and who had baseline data with at least one follow-up visit. Data were extracted from the THAOS database on January 6, 2015. Subjects with TTR mutations known to have a predominantly cardiac phenotype (i.e., Val122Ile, Ile68Leu, Leu111Met, and Thr60Ala) or who received any treatment (other than tafamidis) intended to target the course of the disease (i.e., liver transplant or diflunisal) pre-enrollment were excluded. The analysis was limited to subjects in Coutinho stage 1 (as defined by the modified Polyneuropathy Disability [mPND]) score, with subjects either having sensory disturbances in their feet but able to walk without difficulty [mPND score I], or having some difficulties walking but able to walk without aid [mPND score II] [21].
For patients receiving tafamidis, dosage recommendations (including dosage strength and timing of the dosing) were based on the prescribing physician’s clinical judgment and the local approved product label, or the open-label study protocol for those patients receiving tafamidis as part of their participation in a clinical study (the indicated dose of tafamidis is 20 mg once daily) [22].
Disease duration was calculated from the earliest onset date of any symptoms commonly associated with TTR-FAP that the treating physician had flagged as definitively or possibly attributable to the disease. An examination of disease duration at enrollment in all THAOS subjects identified a subgroup with unusually long disease duration, raising the possibility that these unusually long disease duration values could distort the multiple imputation and treatment propensity score models. Because disease duration was an important factor in the matching process, subjects in the highest quartile (≥ 8.6 years) were excluded from the analysis due to these concerns and concerns that there would be an insufficient number of appropriate matches for subjects who had been symptomatic for many years prior to enrollment in THAOS.
Outcome Measures
Subject data from the participating THAOS registry sites included medical, laboratory, neurologic, and quality-of-life assessments collected as part of the local standard of care [20]. The focus of the present analysis was disease progression, based on neurologic and quality-of-life assessments, and mortality. Outcome assessments performed at regular clinic visits were examined based on approximately 6-month intervals (± 3 months). Using data from the clinical neurologic examination, the Neurologic Composite Score (NCS; range 0–294, with higher scores reflecting worsening neurologic functioning) and subscale scores (NCS-Reflex [range 0–10, with items rated as present or absent], NCS-Motor [range 0–160, with items rated from 0 = no contractions to 5 = full range of motion and maximum resistance], NCS-Sensory [range 0–124, with items rated as normal, decreased, or absent]) were calculated as the sum of quantitative ratings for subjects’ neurologic assessments of both upper and lower limbs. The mapped Neuropathy Impairment Score-Lower Limbs (NIS-LL, range 0 [normal] to 88 [total impairment]) was calculated from a subset of neurologic assessment items for lower limbs and assesses function of the extremities most affected early in disease progression [23]. Coutinho stage was derived using the mPND (mPND score I or II equating to Coutinho stage 1; mPND score IIIa or IIIb equating to Coutinho stage 2), and time to progression from Coutinho stage 1 to stage 2 (or higher) was determined [21]. Total Quality of Life (TQoL) score (range − 4 to 136) was derived from the patient-reported Norfolk Quality of Life-Diabetic Neuropathy questionnaire, with higher scores reflecting poorer quality of life [23, 24]. The Karnofsky Performance Status Scale score was used to quantify the subjects’ ability to perform normal daily life activities and their need for assistance (ranging from 0 [dead] to 100 [normal; no complaints]).
Statistics
Matching Methodology
The matching methodology was designed to ensure that the heterogeneity among TTR-FAP cases worldwide, including variability in mutation, age of onset, phenotype, and course of disease, was well balanced between the treated and untreated analysis populations. Matching was accomplished in a three-step process by matching on mutation group, country of origin, and by mean treatment propensity score to account for clinical status.
Subjects were matched within mutation groups, defined as Val30Met and non-Val30Met. Thus, treated Val30Met subjects were matched with untreated Val30Met subjects. Within the group of subjects with non-Val30Met mutations, it was not possible to match on the exact mutation owing to low numbers; therefore, treated subjects were matched to untreated subjects within the non-Val30Met mutation group. Although country of ancestry may be the closest approximation of genetic background, this information was not captured consistently; thus, data on country of birth, which were available for > 99% of subjects, were used as the indicator of genetic background.
Finally, propensity score estimation was used to balance the treated and untreated groups on disease characteristics (e.g., severity and duration). Propensity scores are frequently employed to reduce indication bias associated with treatment status in observational studies, thus facilitating causal inference [25]. Propensity score matching is widely used in observational studies and, when appropriately applied, has been shown to be an effective method [26, 27]. Indication bias occurs in real-world (i.e., non-randomized) scenarios, in which treatment decisions are made by clinicians based on disease severity and any number of other important demographic and clinical factors. The estimated treatment propensity scores reflect the probability of receiving treatment based on observed baseline covariates and allow imbalances observed in the study population to be addressed in the analysis [28].
Baseline for treated subjects was defined as the enrollment date (if tafamidis treatment started before enrollment) or the treatment start date (if tafamidis treatment started on or after enrollment). Baseline for untreated subjects was defined as any visit occurring after symptom onset and not more than 3 months prior to enrollment (the THAOS registry permits collection of retrospective data). Owing to the observational nature of the THAOS registry, clinical data are collected and reported as part of routine care. Given variability in practice patterns and the influence of disease status on care decisions, data are assumed not to be missing at random, that is, the probability of a data point being missing is related to other factors of interest at both the site and patient levels. Missing baseline data were imputed for the purpose of propensity score modeling to avoid possible selection bias associated with excluding subjects with incomplete data. Missing data were imputed via multiple imputation using a Markov chain approach. The propensity score models included eight selected baseline clinical variables: TQoL; disease duration; Karnofsky score; the three NCS sub-scores (Reflex, Sensory, and Motor); blood urea nitrogen (BUN); and modified body mass index (mBMI). Up to 101 imputations were performed, separately for Val30Met and non-Val30Met populations, resulting in a corresponding number of fully imputed datasets. Each imputed dataset was entered into a logistic regression model of treatment probability, as predicted by the same set of eight baseline clinical variables.
The mean propensity score for each subject at baseline was used for matching in a nearest-neighbor approach [29]. To enhance the quality of matched sets of patients, propensity scores for the treated and untreated subjects were required to be within 0.25 standard deviations (SD) on the logit scale (i.e., logit of the propensity score) [29]. Furthermore, multiple baseline dates were considered for the untreated population (i.e., any THAOS visit occurring after disease onset and otherwise meeting eligibility criteria). This allowed for the matching of treated and untreated at a point in time where clinical status was most similar rather than at an arbitrary point in time, such as enrollment. Finally, the quality of the matches was maintained through the use of matching “with replacement” of untreated subjects. Untreated subjects were allowed to be used in more than one matched set, but not more than once with a given treated subject.
Analyses
Descriptive statistics were calculated for demographic and baseline clinical characteristics. Treated subjects are presented at a given time point only if one or more of their matched controls also had data available. Untreated subjects are presented at a given time point only if their matched treated subject also had data available. Values for matched controls within each matched set are weighted. Treatment effects were evaluated by repeated measures analyses with appropriate covariates (age at baseline, gender, duration of symptoms, treatment propensity score, time and treatment-by-time interaction, and baseline values). Survival and time to progression from Coutinho stage 1 were analyzed using Cox proportional hazards regression models. Subjects who received alternative disease-modifying treatment (i.e., liver transplant or diflunisal) were censored at the earlier of liver transplant date or the start of diflunisal treatment. For time-to-event analyses, age at baseline and gender were used as covariates for the primary analysis.
Secondary and tertiary models were used to more fully characterize the survival and time-to-progression results. The secondary analysis included all subjects (unmatched) who were ever at Coutinho stage 1 during the THAOS registry. As the start time was unrelated to the treatment start date, the treatment effect was estimated through use of a time-varying covariate for tafamidis treatment. The tertiary analysis included the matched cohorts but was limited to subjects with mPND score I (having sensory disturbances in their feet but able to walk without difficulty) at baseline (i.e., excluding subjects with mPND score II; some difficulties walking but could walk without aid) to account for the truncated time to progression in subjects with a higher mPND score. Covariates for the secondary analysis also included age at baseline, genetic mutation, and birth region, while covariates for the tertiary analysis included age at the start of Coutinho stage 1 and gender.
Sensitivity Analysis
Assessment data for the period from the start of treatment to enrollment in the registry generally were not available for subjects treated with tafamidis prior to enrolling in THAOS. Furthermore, these subjects typically had a longer overall duration of treatment than those who began receiving treatment at or after enrollment. To evaluate the robustness of the model, given the uncertainty of the effect of these two factors, a sensitivity analysis was performed, analyzing matched cohorts that excluded subjects who received tafamidis treatment prior to THAOS enrollment.
Results
Population
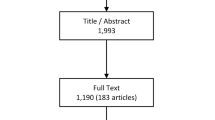
As of January 6, 2015 (data extraction date), 2535 subjects were enrolled in the THAOS registry; of these, 274 tafamidis-treated subjects and 255 untreated controls met the inclusion criteria for the current analysis (Fig. 1). A total of 22 treated and 88 untreated subjects were unable to be matched, per the pre-specified matching criteria. Prior to the matching, treated subjects had higher disease burden at baseline than untreated subjects, as evidenced by higher NIS-LL and TQoL scores. Box plots of treated and untreated treatment propensity scores on a logit scale before matching indicated overlap between the groups, and thus there were potential matches for all treated subjects (Fig. 2a).
Each of the 252 treated subjects was matched with up to four untreated subjects, with a total of 167 unique untreated subjects. In total, 208 (82.5%) treated subjects were each matched to four untreated subjects, 13 (5.2%) to three untreated subjects, eight (3.2%) to two untreated subjects, and 23 (9.1%) to one untreated subject. This resulted in 910 unique matched treated–untreated pairs. The majority of pairs had an exact match on country of birth (n = 762; 83.7%). Approximately half the pairs matched exactly on gender (n = 451; 49.6%).
Box plots of treated and untreated treatment propensity scores on a logit scale after matching are shown in Fig. 2b. The mean (SD) difference between propensity scores for the 910 matched pairs was 0.012 (0.013) logits.
Demographic and Baseline Characteristics
Baseline demographic characteristics were broadly similar between tafamidis-treated subjects and matched controls, with a mean (SD) duration since disease onset of 3.18 (1.9) and 3.27 (1.3) years, respectively (Table 1). The median post-baseline follow-up time was 23.6 months for treated subjects and 21.4 months for untreated subjects. In the treated cohort, Val30Met (n = 233; 92.5%) was the predominant TTR-FAP genotype, the gender ratio was approximately equal (n = 131 male; 52.0%), and the majority of subjects (n = 202; 80.2%) were born in Portugal. Other reported countries of birth were Angola, Argentina, Austria, Brazil, France, Germany, Italy, Japan, Sweden, Turkey, United States, and Venezuela.
At baseline, treated subjects had higher scores across all neurologic endpoints, indicating greater impairment (Table 1). However, a comparison of baseline values in the matched sample analysis, which adjusted for baseline treatment propensity score, gender, age at baseline, and duration of TTR-FAP–related symptoms at baseline, found no statistically significant differences for the mapped NIS-LL, NCS-Motor and NCS-Sensory scores, TQoL, mBMI, and BUN. There were statistically significant differences between the treated and untreated groups for NCS-Reflex (p = 0.018) and the Karnofsky score (p = 0.040), with scores indicating that treated subjects had diminished reflexes, but better daily functioning, compared with untreated subjects at baseline.
Change in Neurologic, Quality of Life, Functional, and Nutritional Status
Over the course of 2 years, tafamidis-treated subjects had a significantly lower rate of disease progression than untreated subjects, as demonstrated by measures of neurologic function and quality of life (Table 2 and Fig. 3). Lower rates of progression in tafamidis-treated subjects compared with untreated subjects were statistically significant for the NIS-LL, NCS, and each of the NCS subscale scores (p ≤ 0.023 for each; Table 2).There was also a significantly lower rate of worsening in quality of life, as assessed by TQoL (p < 0.001).
The trends in the estimated rate of change between tafamidis-treated and untreated subjects for daily functioning (Karnofsky score) and nutritional status (assessed using mBMI) were not significant (Table 2). The estimated rate of change per year in BUN demonstrated a statistically significant lower rate of worsening in tafamidis-treated subjects (p = 0.004). While BUN is not considered a direct measure of ATTR amyloidosis disease, it was included in this analysis, as it correlated with disease severity at baseline.
Sensitivity Analyses
The sensitivity analyses excluded subjects who initiated tafamidis treatment prior to enrollment in THAOS (n = 53). Of the remaining 199 subjects, matches were found for 196 subjects. Demographics and clinical characteristics at baseline were similar to those of the overall population, with the exception that the mean total time (SD) on tafamidis (n = 196) was 19.01 (7.05) months, compared with 29.11 (22.97) for the overall population. The results of the sensitivity analyses were generally similar to those for the full population (Table 3). There were statistically significant differences between the treated and untreated groups for NIS-LL, NCS, NCS-Motor subscale, NCS-Sensory subscale, TQoL, and BUN (p ≤ 0.029 for each), but there was no significant difference in the Karnofsky score or mBMI. In contrast to the full cohort, there was no significant difference in the NCS-Reflex subscale in the sensitivity analysis. A total of 44 subjects in the full population had also participated in a tafamidis clinical trial and were among those excluded in the sensitivity analysis.
Time to Progression and Survival
None of the primary, secondary, or tertiary statistical models examining time to disease progression from Coutinho stage 1 to 2 over the course of 2 years demonstrated a statistically significant difference between tafamidis-treated and untreated subjects. However, it should be noted that only a small number of subjects progressed from Coutinho stage 1 (sensory disturbances in feet but able to walk without difficulty, or having difficulties walking but able to walk without aid) to stage 2 (able to walk with cane[s] or crutch[es]) during the observation period. All subjects were at stage 1 at baseline, and 98.6% of the treated and 97.3% of the untreated subjects remained in stage 1 through the 24 months.
Seven deaths were observed; all were in the untreated group. The primary causes of death were as follows: sudden death due to cardiac arrhythmia (two subjects), cardiac arrest (one subject), pneumonia (one subject), unknown cause (one subject), and post-organ transplant complications (two subjects; these subjects were censored from the analysis at the date they received their liver transplantation). As there were no deaths reported for the tafamidis-treated subjects, the primary model that examined survival from baseline using the matched cohort was unable to yield estimates of the hazard ratio. A secondary analysis of all subjects (unmatched) examining survival from symptom onset, using a time-varying treatment covariate and a delayed entry model without regard to matching, yielded a statistically significant hazard ratio of 3.95 (95% confidence interval: 1.54 to 10.14) for untreated versus treated subjects (p = 0.0042). Results of the sensitivity analyses for survival, excluding subjects treated with tafamidis prior to baseline, showed a similar trend to that seen for the full cohort.
Discussion
In this non-randomized, matched cohort analysis of data from THAOS, the largest observational disease registry of TTR-FAP patients, tafamidis treatment resulted in significantly less neurologic disease progression (based on NCS and NIS-LL) and less deterioration in quality of life (TQoL) compared with untreated matched controls. No effect on nutritional status or functional impairment was observed. The results from this large international study of predominantly Val30Met subjects, but including non-Val30Met subjects, extend the efficacy of tafamidis observed in clinical trials [14,15,16,17,18] to real-world clinical settings.
No difference was observed between treated and untreated subjects in the time to disease progression (beyond Coutinho stage 1–2 or higher) in the present study. This is most likely due to the low number of subjects who progressed beyond Coutinho stage 1 during the course of available follow-up. The median follow-up time was 23.6 months for treated subjects and 21.4 months for untreated subjects; stage 1 is estimated to last 5.6 (± 2.8) years [21]. The primary survival analysis did not yield hazard ratios due to a lack of deaths among treated subjects, but a secondary analysis that included all subjects without regard to matching found that untreated subjects had a greater risk of death than did tafamidis-treated subjects.
The results of the analysis in this study population showing that tafamidis delayed disease progression in real-world clinical settings are consistent with data from tafamidis clinical trials [14,15,16, 18, 30]. Together, these data provide further support for early intervention with tafamidis when treating patients with TTR-FAP. These results are also consistent with a phase 2 open-label trial in 21 patients with non-Val30Met mutations that showed stabilization of TTR after 12 months of treatment with tafamidis [18], and with a real-world study using registry data from Portuguese TTR-FAP referral centers that demonstrated the effectiveness of tafamidis for long-term survival in 373 Val30Met patients [19]. In the real-world study, estimated median survival time from disease onset was about 12 years for the untreated group and about 25 years in the liver transplantation group, while median survival time was not reached in the tafamidis group [19]. The tafamidis-treated patients had 5- and 10-year survival rates of 99.7 and 94.6%, respectively [19].
Other recent uncontrolled studies in different patient groups have demonstrated mixed results. In one study in 61 Italian patients with a notably late age at disease onset (59 years) and the majority with a non-Val30Met mutation, only one-third of tafamidis-treated patients did not show significant disease progression (defined as an increase in NIS-LL of < 2 points from baseline), although this appeared to be independent of mutation type and disease stage [31]. The authors also noted that disease progression was observed primarily in the first 6 months of treatment [31]. Another study in 46 French patients, also with a late age at disease onset (59 years) and majority non-Val30Met, suggested that tafamidis slowed disease progression in only some patients (approximately one-third) after 3 years of follow-up [32]. The change in NIS-LL in both the tafamidis and matched control groups in this analysis was less pronounced than in these past studies in which the change in NIS-LL with tafamidis at 1 year was 4 [32] and 5.9 [31]. This difference may be related to the differences in patient populations, especially disease severity at baseline and the response to tafamidis, with higher neurological severity at baseline having been shown to be predictive of greater neurological progression over time regardless of treatment [33]. The difference may also be related to differences in disease course with some genotypes and phenotypes [10]. Past clinical trials have demonstrated significant improvements in BMI with tafamidis [15, 16]. This improvement was not seen at most time points in these recent uncontrolled studies, although a higher BMI or mBMI at baseline was associated with less disease progression with treatment [31, 32]. There was no significant improvement in mBMI in this analysis, which may have been related to the large amount of missing mBMI data at later time points (see Table 2).
Rare disease registries offer an important opportunity to study the effectiveness of treatments in real-world clinical settings and provide a practical approach for ensuring adequate statistical power and long-term follow-up [34]. Careful matching between treated and untreated cohorts is essential to facilitate causal inference. The propensity scoring technique used in the present analysis to address variability in clinical status has been successfully implemented to evaluate the effectiveness of treatments in a variety of disease states [35,36,37,38,39,40], including rare diseases [41]. In the current study, there was substantial overlap between the two cohorts on treatment propensity scores, indicating comparability between the treated and untreated groups. Additionally, all resulting pairs matched exactly on genotype group (Val30Met or non-Val30Met), and the majority were matched exactly on region of birth. This close matching is fundamentally important in analyses using data from observational studies and strengthens the interpretation of the delayed disease progression observed in the tafamidis group compared with untreated controls.
As with any observational study, there are potential sources of bias associated with subject selection; in this study, efforts were taken to minimize this bias by employing established, robust, multi-step matching techniques. Specific limitations associated with THAOS as a disease registry are described elsewhere [20]. The majority of treated subjects in this analysis were from Portugal (80.2%), were relatively young (with a mean age of 40.4 years), and had the Val30Met mutation (92.5%). This broadly reflects the population enrolled in THAOS who have been treated with tafamidis. The matching analysis used in this study requires a sufficiently large number of subjects for assessment, so it was not possible to perform comparisons between different subject sub-groups to determine whether there were any differences in their response to treatment. Therefore, these findings may not be able to be extrapolated to subjects with non-Val30Met mutations or late-onset Val30Met. This may be particularly relevant, as some past studies have suggested that tafamidis may be less effective in older patients with more advanced disease [32, 42].
Conclusion
This is the largest international study to comprehensively assess the effectiveness of tafamidis, using multiple clinical outcome measures, under real-world conditions in a predominantly Val30Met population which also included non-Val30Met subjects. These findings demonstrate that tafamidis both delayed neurologic disease progression and maintained quality of life compared with untreated matched controls. These findings confirm previous results and provide evidence for the effectiveness of tafamidis outside conventional clinical trials.
References
Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med. 1997;337:898–909.
Plante-Bordeneuve V, Said G. Familial amyloid polyneuropathy. Lancet Neurol. 2011;10:1086–97.
Ando Y, Coelho T, Berk JL, et al. Guideline of transthyretin-related hereditary amyloidosis for clinicians. Orphanet J Rare Dis. 2013;8:31.
Plante-Bordeneuve V. Update in the diagnosis and management of transthyretin familial amyloid polyneuropathy. J Neurol. 2014;261:1227–33.
Benson MD, Kincaid JC. The molecular biology and clinical features of amyloid neuropathy. Muscle Nerve. 2007;36:411–23.
Rowczenio DM, Noor I, Gillmore JD, et al. Online registry for mutations in hereditary amyloidosis including nomenclature recommendations. Hum Mutat. 2014;35:E2403–12.
Coelho T, Maurer MS, Suhr OB. THAOS—The transthyretin amyloidosis outcomes survey: initial report on clinical manifestations in patients with hereditary and wild-type transthyretin amyloidosis. Curr Med Res Opin. 2013;29:63–76.
Connors LH, Lim A, Prokaeva T, Roskens VA, Costello CE. Tabulation of human transthyretin (TTR) variants, 2003. Amyloid. 2003;10:160–84.
Plante-Bordeneuve V, Lalu T, Misrahi M, et al. Genotypic-phenotypic variations in a series of 65 patients with familial amyloid polyneuropathy. Neurology. 1998;51:708–14.
Mariani LL, Lozeron P, Theaudin M, et al. Genotype-phenotype correlation and course of transthyretin familial amyloid polyneuropathies in France. Ann Neurol. 2015;78:901–16.
Ericzon BG, Wilczek HE, Larsson M, et al. Liver transplantation for hereditary transthyretin amyloidosis: after 20 years still the best therapeutic alternative? Transplantation. 2015;99:1847–54.
Suhr OB, Larsson M, Ericzon BG, Wilczek HE. Survival after transplantation in patients with mutations other than Val30Met: extracts from the FAP world transplant registry. Transplantation. 2016;100:373–81.
Adams D, Suhr OB, Hund E, et al. First European consensus for diagnosis, management, and treatment of transthyretin familial amyloid polyneuropathy. Curr Opin Neurol. 2016;29(Suppl 1):S14–26.
Ando Y, Yoshiki S, Konen O, et al. Effects of tafamidis treatment on transthyretin (TTR) stabilization, efficacy, and safety in Japanese patients with familial amyloid polyneuropathy (TTR-FAP) with Val30Met and non-Val30Met: a phase III, open-label study. J Neurol Sci. 2016;362:266–71.
Coelho T, Maia LF, da Silva AM, et al. Long-term effects of tafamidis for the treatment of transthyretin familial amyloid polyneuropathy. J Neurol. 2013;260:2802–14.
Coelho T, Maia LF, Martins da Silva A, et al. Tafamidis for transthyretin familial amyloid polyneuropathy: a randomized, controlled trial. Neurology. 2012;79:785–92.
Coelho T, Merlini G, Bulawa CE, et al. Mechanism of action and clinical application of tafamidis in hereditary transthyretin amyloidosis. Neurol Ther. 2016;5:1–25.
Merlini G, Plante-Bordeneuve V, Judge DP, et al. Effects of tafamidis on transthyretin stabilization and clinical outcomes in patients with non-Val30Met transthyretin amyloidosis. J Cardiovasc Transl Res. 2013;6:1011–20.
Coelho T, Inês M, Conceição I, Saramago P, de Carvalho M, Costa J. Long-term survival of 3000 transthyretin familial amyloid polyneuropathy patients over a century. Int J Clin Neurosci Mental Health. 2016;3(Suppl. 1):P126.
Plante-Bordeneuve V, Suhr OB, Maurer MS, White B, Grogan DR, Coelho T. The transthyretin amyloidosis outcomes survey (THAOS) registry: design and methodology. Curr Med Res Opin. 2013;29:77–84.
Coutinho P, de Martins SA, Lopes LJ, Resende BA. Forty years of experience with type I amyloid neuropathy. Review of 483 cases. In: Glenner G, Costa P, de Freitas A, editors. Amyloid and Amyloidosis. Amsterdam: Execerpta Medica; 1980. p. 88–98.
Pfizer Ltd. Vyndaqel® Summary of Product Characteristics. Sandwich, UK. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002294/WC500117862.pdf. Accessed: March 10, 2017.
Coelho T, Vinik A, Vinik EJ, Tripp T, Packman J, Grogan DR. Clinical measures in transthyretin familial amyloid polyneuropathy. Muscle Nerve. 2017;55:323–32.
Vinik EJ, Vinik AI, Paulson JF, et al. Norfolk QOL-DN: validation of a patient reported outcome measure in transthyretin familial amyloid polyneuropathy. J Peripher Nerv Syst. 2014;19:104–14.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Martens EP, Pestman WR, de Boer A, Belitser SV, Klungel OH. Systematic differences in treatment effect estimates between propensity score methods and logistic regression. Int J Epidemiol. 2008;37:1142–7.
Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med. 2008;27:2037–49.
Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the Propensity Score. Am Stat. 1985;39:33–8.
Dehejia RH, Wahba S. Propensity Score-Matching Methods for Nonexperimental Causal Studies. Rev Econ Stat. 2002;84:151–61.
Waddington Cruz M, Amass L, Keohane D, Schwartz J, Li H, Gundapaneni B. Early intervention with tafamidis provides long-term (5.5-year) delay of neurologic progression in transthyretin hereditary amyloid polyneuropathy. Amyloid. 2016;23:178–83.
Cortese A, Vita G, Luigetti M, et al. Monitoring effectiveness and safety of Tafamidis in transthyretin amyloidosis in Italy: a longitudinal multicenter study in a non-endemic area. J Neurol. 2016;263:916–24.
Plante-Bordeneuve V, Gorram F, Salhi H, et al. Long-term treatment of transthyretin familial amyloid polyneuropathy with tafamidis: a clinical and neurophysiological study. J Neurol. 2017;264:268–76.
Gundapaneni BK, Sultan MB, Keohane DJ, Schwartz JH. Tafamidis delays neurological progression comparably across Val30Met and non-Val30Met genotypes in transthyretin familial amyloid polyneuropathy. Eur J Neurol. 2018;25:464–8.
Gagne JJ, Thompson L, O’Keefe K, Kesselheim AS. Innovative research methods for studying treatments for rare diseases: methodological review. BMJ. 2014;349:g6802.
Lee J, Ko Y, Ahn S, et al. Comparison of US and CT on the effect on negative appendectomy and appendiceal perforation in adolescents and adults: a post hoc analysis using propensity-score methods. J Clin Ultrasound. 2016;44:401–10.
Lim C, Doussot A, Osseis M, et al. Primary tumor versus liver-first strategy in patients with stage IVA colorectal cancer: a propensity score analysis of long-term outcomes and recurrence pattern. Ann Surg Oncol. 2016;23:3024–32.
Lip GY, Keshishian A, Kamble S, et al. Real-world comparison of major bleeding risk among non-valvular atrial fibrillation patients initiated on apixaban, dabigatran, rivaroxaban, or warfarin. A propensity score matched analysis. Thromb Haemost. 2016;116:975–86.
Nduka CU, Stranges S, Bloomfield GS, et al. A plausible causal link between antiretroviral therapy and increased blood pressure in a sub-Saharan African setting: a propensity score-matched analysis. Int J Cardiol. 2016;220:400–7.
Tian F, Hong XF, Wu WM, et al. Propensity score-matched analysis of robotic versus open surgical enucleation for small pancreatic neuroendocrine tumours. Br J Surg. 2016;103:1358–64.
Wada T, Yasunaga H, Horiguchi H, et al. Ozagrel for patients with noncardioembolic ischemic stroke: a Propensity Score-matched analysis. J Stroke Cerebrovasc Dis. 2016;25:2828–37.
Grabowski GA, Kacena K, Cole JA, et al. Dose-response relationships for enzyme replacement therapy with imiglucerase/alglucerase in patients with Gaucher disease type 1. Genet Med. 2009;11:92–100.
Lozeron P, Theaudin M, Mincheva Z, Ducot B, Lacroix C, Adams D. Effect on disability and safety of Tafamidis in late onset of Met30 transthyretin familial amyloid polyneuropathy. Eur J Neurol. 2013;20:1539–45.
Acknowledgements
We thank all THAOS patients and investigators for their important contributions to this study. We thank the THAOS Scientific Board (thaos.net/THAOS/ScientificBoard.cfm), including Dr. Claudio Rapezzi and Dr. Márcia Waddington-Cruz as Scientific Board Chairs, for their partnership and guidance on this study.
Funding
The Transthyretin Amyloidosis Outcomes Survey (THAOS) and the analyses and the Article Processing Charges were sponsored by Pfizer. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Medical Writing, Editorial, and Other Assistance
Medical writing support was provided by Mary Kunjappu, PhD, and Joshua Fink, PhD, of Engage Scientific Solutions and was funded by Pfizer.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Rajiv Mundayat is an employee of Pfizer and hold stock and/or stock options. Michelle Stewart is an employee of Pfizer and hold stock and/or stock options. Jose Alvir is an employee of Pfizer and hold stock and/or stock options. Moh-Lim Ong is an employee of Pfizer and hold stock and/or stock options. Denis Keohane is an employee of Pfizer and hold stock and/or stock options. Denise Rill is an employee of Pfizer and hold stock and/or stock options. Marla B. Sultan is an employee of Pfizer and hold stock and/or stock options. Sarah Short is an employee of ICON plc, who were paid consultants to Pfizer in connection with the development of this work. Denis Keohane is a THAOS Scientific Board member.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for inclusion in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to https://doi.org/10.6084/m9.figshare.6015644.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mundayat, R., Stewart, M., Alvir, J. et al. Positive Effectiveness of Tafamidis in Delaying Disease Progression in Transthyretin Familial Amyloid Polyneuropathy up to 2 Years: An Analysis from the Transthyretin Amyloidosis Outcomes Survey (THAOS). Neurol Ther 7, 87–101 (2018). https://doi.org/10.1007/s40120-018-0097-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-018-0097-9