Abstract
This phase II, open-label, single-treatment arm study evaluated the pharmacodynamics, efficacy, and safety of tafamidis in patients with non-Val30Met transthyretin (TTR) amyloidosis. Twenty-one patients with eight different non-Val30Met mutations received 20 mg QD of tafamidis meglumine for 12 months. The primary outcome, TTR stabilization at Week 6, was achieved in 18 (94.7 %) of 19 patients with evaluable data. TTR was stabilized in 100 % of patients with non-missing data at Months 6 (n = 18) and 12 (n = 17). Exploratory efficacy measures demonstrated some worsening of neurological function. However, health-related quality of life, cardiac biomarker N-terminal pro-hormone brain natriuretic peptide, echocardiographic parameters, and modified body mass index did not demonstrate clinically relevant worsening during the 12 months of treatment. Tafamidis was well tolerated. In conclusion, our findings suggest that tafamidis 20 mg QD effectively stabilized TTR associated with several non-Val30Met variants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transthyretin amyloidosis (ATTR) is both an inherited and an age-related amyloidosis. The most common phenotypic presentations of hereditary ATTR are sensorimotor and autonomic polyneuropathy (TTR familial amyloid polyneuropathy (TTR-FAP)) and cardiomyopathy [1]. The protein implicated in ATTR, TTR, is a tetrameric transport protein for thyroxine and the retinol-binding protein–retinol (vitamin A) complex [2, 3]. TTR is synthesized primarily in the liver [4]. Mutations in the gene that encodes for TTR cause dissociation of the TTR tetramer to monomers. This leads to the formation of insoluble fibrillar proteins (or amyloid) that accumulate and produce deleterious effects on tissues and organ function [5–8].
The age at onset of ATTR varies between the second and ninth decades of life, and there is great heterogeneity in genetic penetrance, depending on phenotype, genotype, and environmental factors [1, 9]. However, the outcome of ATTR is invariably progressive and fatal: After a mean interval of 10 years from initial presentation of symptoms, patients usually die from progressive and relentless worsening of the neuropathy, secondary infections, cachexia, or cardiac complications [1, 9, 10].
More than 100 amyloidogenic TTR point mutations have been identified in patients with familial ATTR [11, 12]. The most common genetic variant associated with polyneuropathy is Val30Met (valine replaced by methionine at position 30 of the amino acid chain), which accounts for ≈85 % of TTR-FAP cases worldwide [13, 14]. Generally, non-Val30Met mutations are associated with greater cardiac involvement than Val30Met mutations [12, 14], and patients with non-Val30Met mutations and a cardiac phenotype tend to be older men and have lower survival rates [15].
Liver transplantation, which removes the main site of mutant TTR production, has been the only disease-modifying treatment option for TTR-FAP. Following transplantation, mutant transthyretin protein becomes undetectable in serum [16, 17]; neurological symptoms frequently halt or improve [18]; and the reported 5-year survival rate is 77 % [18, 19]. However, cardiac disease tends to progress even after successful liver transplantation, especially in non-Val30Met patients, most likely due to the deposition of wild-type TTR on pre-existing amyloid deposits [1, 9]. Indeed, several non-Val30Met variants, including Glu42Gly, Ala36Pro [20], Ser52Pro, and Ile84Thr [21], have been linked to rapid postoperative progression of TTR cardiac amyloidosis. This partially explains why, according to recent data from the Familial Amyloid Polyneuropathy World Transplant Registry, the rate of survival at 5 years is significantly worse in patients with non-Val30Met mutations compared to patients with the Val30Met mutation (59 % versus 82 %; p < 0.0001) [14] and has led to the proposal to consider the extremely challenging procedure of combined heart and liver transplantation in certain ATTR patients with cardiac involvement [1, 22]. Taken together, this underlines the need for additional treatment options not only for patients with ATTR in general but also for patients with non-Val30Met mutants in particular.
Tafamidis meglumine (Pfizer Inc, New York, NY, USA) is an oral agent that occupies the two thyroxine binding sites on TTR. This is associated with inhibition of dissociation of TTR into monomers, the rate-limiting step in amyloid formation [11, 23]. In an 18-month, double-blind, placebo-controlled, randomized trial, tafamidis demonstrated TTR stabilization and slowed the progression of peripheral neurological impairment compared with placebo in patients who had TTR-FAP associated with Val30Met mutations [24]. Individuals with other TTR variants were excluded from that study. The primary objective of our open-label, single-arm study was to determine the pharmacodynamic stabilization effects of tafamidis on non-Val30Met TTR variants. The safety and exploratory efficacy of tafamidis were also evaluated.
Materials and Methods
Study Design
This 12-month study (ClinicalTrials.gov NCT00630864) enrolled men and women at four research centers in France, Germany, Italy, and the United States between June 2008 and January 2010. An open-label design was used, given the low prevalence of non-Val30Met mutations and the fact that TTR stabilization is a laboratory-determined measure that would not be influenced by knowledge of treatment assignment.
The study was conducted in two parts. In part 1, patients received tafamidis 20 mg QD for 6 weeks. At Week 6, blood samples were collected to determine TTR stabilization. Patients who did not demonstrate TTR stabilization at Week 6 were to be discontinued from the study. In part 2, all patients demonstrating stabilization at the Week 6 visit continued to receive tafamidis 20 mg QD for up to a total of 12 months. Additional laboratory evaluations for TTR stabilization were performed at Months 6 and 12. The study was approved by the local institutional review boards at each site and conducted in accordance with the Declaration of Helsinki. All patients gave written informed consent.
Study Population
Men and nonpregnant women aged 18–75 years were eligible if they had symptomatic, biopsy-confirmed TTR amyloidosis with a Karnofsky Performance Status of ≥50 and a known pathogenic TTR-FAP mutation other than Val30Met or Val122Ile. Other exclusion criteria were primary or secondary amyloidosis, prior liver transplant (or expected liver transplant within 12 months of enrollment), hepatitis B or C or HIV infection, impaired renal or hepatic function, a New York Heart Association functional class of ≥3, other causes of sensorimotor neuropathy (e.g., vitamin B12 deficiency, diabetes mellitus), any prior non-amyloid cardiac disease or cardiomyopathy, or a life expectancy of <12 months due to any comorbidity. Two patients who were over 75 years of age but met all other inclusion criteria were granted waivers and enrolled in the study.
Outcome Measures
TTR stabilization was determined by a validated immunoturbidimetric method [23]. Briefly, the TTR tetramer concentration in each plasma sample was measured before and after 2 days of denaturation in 4.8 M urea. The ratio of the post-denaturation to the pre-denaturation values was recorded as the fraction of initial (FOI) tetramer concentration. Because the mechanism of action of tafamidis is to bind to TTR and inhibit dissociation, it should result in a higher FOI than pretreatment baseline values in patients. The FOI at each on-study timepoint was compared with the pretreatment FOI, yielding a percent stabilization using the following formula: [25]
A stabilization cut-off value was derived from data obtained from placebo-treated healthy volunteers in a phase I single and multiple ascending-dose study. Values above the 95 % confidence interval (CI) of placebo-treated healthy volunteers (32 %) were classified as “stabilized” [25].
Neurological impairment was assessed using the Neuropathy Impairment Score (NIS), which captures clinically meaningful changes in neurological function (i.e., sensation, muscle weakness, reflexes) over time [26, 27]. The NIS has been validated in patients with diabetic neuropathy [28, 29]. Measures included both of the lower limbs (NIS-LL; 0–88 points) and upper limbs (NIS–UL; 0–156 points) NIS subscales, as well as the composite NIS score (0–244 points). In addition, large nerve fiber function was assessed using the summated five nerve conduction study normal deviate (Σ5 NCS nds) composite score, which combines results from five nerve conduction studies (sural nerve sensory nerve action potential, peroneal nerve compound muscle action potential, peroneal nerve motor conduction velocity, peroneal nerve distal motor latency, and tibial nerve distal motor latency) [30]. Scores range from −15 to 15, with higher scores indicating poorer large-fiber neurological function.
Quality of life (QOL) was evaluated using the Norfolk Quality of Life–Diabetic Neuropathy (Norfolk QOL-DN) questionnaire [31]. The 35-item version of this patient-completed questionnaire was used, which yielded a total QOL (TQOL) score ranging from −2 to 138, with higher scores indicating worse QOL.
The modified body mass index (mBMI) was calculated by multiplying the BMI (kilograms per square meter) by the serum albumin concentration (grams per liter) to correct for weight gains due to swelling and edema, common features of TTR amyloidosis [32]. The mBMI provides a more accurate indicator of malnutrition and gastrointestinal dysfunction than the BMI and is an important measure of wasting in patients with TTR-FAP [32].
Troponin I and N-terminal pro-hormone brain natriuretic peptide (NT-pro-BNP) are cardiac biomarkers; the latter may have prognostic value for patients with ATTR [33]. Measurements of both biomarkers were made from patient plasma samples, and changes from baseline were calculated at each follow-up visit. Given the likelihood of cardiac involvement in patients with ATTR, echocardiography was performed at baseline and at Months 6 and 12 according to the American Society of Echocardiography and the European Association of Echocardiography guidelines [34] and was centrally over-read by a core laboratory to ensure consistent interpretation. Measurements included left ventricular (LV) wall thickness (LVW); interventricular septal thickness (IVS); left atrial diameter; LV Mass; left ventricular ejection fraction; and ratio of mitral peak velocity of early filling to early diastolic mitral annular velocity (E/E’ ratio). Likewise, conventional 12-lead electrocardiograms were recorded at baseline and throughout the study.
Adverse events (AEs) were monitored from the start of the study through 30 days after administration of the last tafamidis dose. Serious AEs (SAEs) were those that resulted in death, were considered life-threatening, required hospitalization, resulted in significant disability/incapacity, or were otherwise considered important medical events by the principal investigator.
Statistical Analysis
The primary endpoint was TTR stabilization (percent stabilization response defined as >32 %) at Week 6 compared with baseline; secondary endpoints were TTR stabilization at Months 6 and 12. The number and proportion of patients who achieved stabilization were calculated at each point, and the 95 % CI of the proportion of patients stabilized was calculated. Exploratory efficacy endpoints included change from baseline at Months 6 and 12 in the NIS, NIS-LL, NIS-UL, TQOL score, Σ5 NCS nds composite score, mBMI, and cardiac biomarkers. For these, change from baseline over time was summarized at each follow-up visit by descriptive statistics, with the 95 % CI calculated for mean changes. Analyses were performed based on observed data from the intent-to-treat population, defined as all patients who received at least one dose of study medication.
We undertook a post hoc analysis to assess changes in NT-pro-BNP levels in patients whose concentrations of this biomarker suggested an increased risk for heart failure (NT-pro-BNP >1,000 pg/mL) or a lower risk for heart failure (NT-pro-BNP <300 pg/mL). These NT-pro-BNP cut-off points were based on studies of patients presenting to the emergency department with dyspnea: Higher NT-pro-BNP concentrations have been demonstrated to be a strong predictor of heart failure mortality at 1 year [35], while the lower concentration has been used as a cut-off to rule out heart failure [36, 37]. The mean and median changes in NT-pro-BNP levels from pretreatment (the average of the screening and baseline levels) were examined at Months 6 and 12.
An additional post hoc analysis was performed to examine changes from baseline in echocardiographic parameters at Month 12 in patients meeting the primary echocardiographic criterion for amyloid heart involvement defined as thickness of the interventricular septum >12 mm [1, 38].
Safety analyses, including assessment of AEs, treatment-related AEs, and SAEs, were performed on the safety population, which included all enrolled patients who received at least one dose of study medication.
A sample size of up to 24 patients was chosen for the study based on the underlying size of the TTR-FAP population and as sufficient to adequately characterize the 95 % CI for the point estimate for TTR stabilization at Week 6. With a sample size ranging from 18 to 24 patients, assuming ≤2 patients did not achieve TTR stabilization at Week 6, the TTR stabilization rate would be ≥88 % and the lower bound of the two-sided 95 % CI would be ≥65 %.
Results
Patients
Of the 21 patients enrolled, 18 (85.7 %) completed the trial. One patient discontinued in part 1 due to an SAE (transient ischemic attack), and two patients discontinued in part 2 due to organ transplants. The baseline demographics for the intent-to-treat population are presented in Table 1. The mean (± standard deviation (SD)) duration of ATTR-related symptoms at baseline was 64.7 ± 60.8 months (median, 45.5 months), with a mean age at onset of 59.3 ± 9.2 years (median, 61.0). Table 2 displays the results of the patients’ baseline assessments. The patients demonstrated significant impairment in neurological function (NIS: mean ± SD, 48.7 ± 44.3 and median, 45.0; Σ5 NCS: mean ± SD, 6.1 ± 5.9 and median, 6.7) and disease-specific QOL (mean ± SD Norfolk TQOL score, 47.8 ± 35.1; median, 38.0). Of note, the mean mBMI at the baseline visit was 1,052.5 ± 206.7 kg/m2 × g/L (median, 1,047.8), which meaningfully exceeds the screening threshold associated with improved survival following liver transplantation of 600 kg/m2 × g/L [39].
The enrolled patients had eight different non-Val30Met TTR mutations (Table 1). All patients except one reported symptoms of peripheral neuropathy, 13 of 21 (62 %) reported symptoms of cardiac involvement, and 5 of 21 (23.8 %) had peripheral and autonomic neuropathy plus cardiomyopathy. All patients demonstrated at least one echocardiographic abnormality, the most common being left ventricular posterior wall thickness and left ventricular septal thickness of >12 mm, which were each observed in 17 of 19 (89.5 %) patients. Abnormalities on electrocardiography were also common at baseline, occurring in 16 of 21 (76.2 %) of patients. Of these, conduction abnormalities were the most common, in 13 of 21 (61.9 %) patients, and left anterior hemiblock and first-degree atrioventricular block were the most frequent conduction abnormalities.
TTR Stabilization
TTR stabilization at Week 6 was achieved in 18 (94.7 %) of the 19 intent-to-treat patients for whom both baseline and Week 6 data were available (Table 3). Two intent-to-treat patients were not included in the analysis at Week 6: One discontinued prior to Week 6 due to a SAE, and one had a missing baseline assay value (thus, postbaseline TTR stabilization could not be determined for this patient at any timepoint). Only one patient (TTR mutation Gly47Ala) did not demonstrate TTR stabilization at Week 6. In the absence of apparent issues with compliance or AEs, this patient was reassessed at Month 3 and allowed to continue in the study because he did achieve stabilization at Months 3 and 6 but discontinued before Month 12 to undergo an organ transplant. At Months 6 and 12 (the secondary endpoints), 100 % of the patients available for assessment achieved TTR stabilization (Table 3).
Changes in Neurological Function
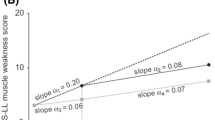
At Month 12, the mean increases from baseline in NIS, NIS-LL, and NIS-UL were 5.3 (95 % CI, –1.0, 11.5; median change, 1.6), 2.7 (95 % CI, –0.4, 5.8; median change, 1.0), and 2.5 (95 % CI, –1.2, 6.2; median change, 0.5), respectively (Fig. 1). Patients with a higher baseline NIS (>70) experienced a greater increase in NIS (i.e., a worsening of impairment) after 12 months compared with patients whose baseline scores were lower. Twelve of the 18 patients with data at Month 12 experienced a change in NIS of ≤4 points at 12 months. These 12 patients represented all enrolled mutations, suggesting a similar treatment effect across mutations.
Change from baseline in NIS, NIS-LL, and NIS-UL scores in the intent-to-treat population. While the baseline scores in the NIS (mean ± SEM, 48.7 ± 9.7; median, 45.0), NIS-LL (mean ± SEM, 27.6 ± 5.4; median, 18.0), and NIS-UL (mean ± SEM, 21.1 ± 4.7; median, 13.0) indicated the presence of significant neurological impairment affecting both lower and upper limbs, mean and median changes from baseline to Months 6 and 12 in NIS, NIS-LL, and NIS-UL presented in this figure increased marginally, with the maximal mean change from baseline being an increase of 5.3 (SEM = 3.0) in the NIS total score at Month 12. This suggests that neuropathy progressed minimally during tafamidis treatment. This is an observed cases analysis including the values of those patients for whom both baseline and Month 6 or baseline and Month 12 data were available. Bars indicate the range of scores; boxes span from the 25th to the 75th percentiles; the horizontal line within the box indicates the median change; plus sign indicates the mean change. SEM standard error of the mean, NIS Neuropathy Impairment Score, NIS-LL NIS of the lower limbs, NIS-UL NIS of the upper limbs
There was a small mean increase of 0.2 (95 % CI −1.5, 1.8) in Σ5 NCS nds score from baseline to Month 12, with a median change of −0.1. When the analysis was performed excluding patients with maximal abnormality in large nerve-fiber function at baseline (and, thus, no possibility of further worsening), the results at Month 12 were similar, with a mean change of 0.3 (95 % CI −2.1, 2.6).
QOL and mBMI
The mean changes from baseline in the TQOL were −4.3 (95 % CI, –10.7, 2.1; median change, 0.0) at Month 6 and 0.1 (95 % CI, –8.9, 9.0; median change, 1.0) at Month 12 (Fig. 2). The mean mBMI (kilograms per square meter × grams per liter) decreased by −22.4 (95 % CI, –62.0, 17.2; median change, –26.7) at Month 6 and increased by 16.6 (95 % CI, –31.0, 64.2; median change, 8.3) at Month 12 (Fig. 3).
Change from baseline in Norfolk QOL-DN (TQOL) scores in the intent-to-treat population. While the baseline TQOL score (mean ± SEM, 47.8 ± 7.7; median, 38.0) indicated impaired quality of life, this figure shows that mean and median changes from baseline in TQOL at Months 6 and 12 were negligible, indicating that overall quality of life was maintained during 12 months of tafamidis treatment. This is an observed cases analysis. Bars indicate the range of scores; boxes span from the 25th to the 75th percentiles; the horizontal line within the box indicates the median change; plus sign indicates the mean change. SEM standard error of the mean, QOL-DN quality of life–diabetic neuropathy, TQOL total quality of life, CI confidence interval
Change from baseline in mBMI scores (expressed as kilograms per square meter × grams per liter) in the intent-to-treat population. Starting with a relatively normal mBMI at baseline (mean ± SEM, 1,052.5 ± 46.2; median, 1,047.8), the mBMI decreased slightly from baseline to Month 6 (mean change ± SEM, –22.4 ± 18.7; median change, –26.7) and subsequently increased, producing a small positive overall change from baseline to Month 12 (mean change ± SEM, 16.6 ± 22.3; median change, 8.3), indicating that the overall nutritional status was maintained after 12 months of tafamidis treatment. The mBMI has been adapted as a measure of nutritional status in TTR amyloidosis patients, as multiplying the BMI (kilograms per square meter) by serum albumin level (grams per liter) corrects for weight gains due to swelling and edema formation frequently associated with TTR amyloidosis. Bars indicate the range of scores; boxes span from the 25th to the 75th percentiles; the horizontal line within the box indicates the median change; plus sign indicates the mean change. SEM standard error of the mean, mBMI modified body mass index
Cardiac Function and Progression of Amyloid Heart Disease
Table 4 summarizes echocardiographic parameters in the study group at baseline and 12-month follow-up (pre-specified analysis). Values remained relatively stable from baseline to Month 12, with no clinically relevant changes.
Results of the post hoc analysis in patients with amyloid heart involvement at baseline (based on the standard diagnostic criterion IVS >12 mm [1, 38]) and a valid assessment at Month 12 (n = 12) were consistent with the findings for the entire group; no clinically meaningful changes in morphological or functional parameters were observed over the 12-month treatment period. Four of the 12 patients did demonstrate disease progression as indexed by International Society of Amyloidosis criteria (increase in IVS thickness ≥2 mm [38]).
Mean baseline troponin I concentrations were normal compared with established laboratory test ranges and remained stable throughout the study. Baseline mean and median NT-pro-BNP levels were elevated in all patients, with no clinically relevant changes over time. Mean increases in NT-pro-BNP concentrations were 228.4 (95 % CI −186.8, 643.6) pg/mL at Month 6 and 306.6 (95 % CI −464.8, 1078.0) pg/mL at Month 12. Median values for change from baseline in NT-pro-BNP were 66.5 pg/mL at Month 6 and 75.5 pg/mL at Month 12.
Figure 4 indicates the median baseline values and median changes from baseline in NT-pro-BNP levels in: (a) the ten patients classified as having a high likelihood of heart failure (based on NT-pro-BNP levels >1,000 pg/mL at the Screening or baseline visit); and (b) in the nine patients with a low likelihood of heart failure (based on NT-pro-BNP levels <300 pg/mL at the Screening or Baseline visit). Patients with a high likelihood of heart failure had a median increase in NT-pro-BNP levels of 521 pg/mL at Month 12, compared with a median increase of 47 pg/mL in patients with a low likelihood of heart failure. Nine of the ten patients with a high likelihood of heart failure had a pretreatment history of cardiac events, including heart failure/dyspnea (three patients) and arrhythmias (three patients). While on treatment, six of these ten patients experienced events that were suggestive of heart failure (four occurrences of peripheral edema and two of dyspnea were reported). One of the cases of moderate peripheral edema occurred in a high likelihood heart failure patient with no reported cardiac history at baseline. In addition, one of these patients was recognized to have moderate coronary artery stenosis during treatment and one required the insertion of a pacemaker. In the patients considered to be at low likelihood of heart failure, one experienced arrhythmia while on treatment with no identified prior history of arrhythmia.
Median and median change from baseline/screening in NT-pro-BNP levels in patients with a high likelihood of heart failure (baseline NT-pro-BNP >1,000 pg/mL) and b low likelihood of heart failure (baseline NT-pro-BNP <300 pg/mL). Based on their highest NT-pro-BNP level at baseline/screening, ten patients with values >1,000 pg/mL were categorized as having a high likelihood, and nine patients with levels <300 pg/mL were classified as having a low likelihood of congestive heart failure, where the normal range is <160 pg/mL. The median NT-pro-BNP level in patients with high likelihood of heart failure increased by 521 pg/mL at Month 12. In contrast, the median NT-pro-BNP level in patients with low likelihood of heart failure increased only marginally by 47 pg/mL at Month 12. NT-pro-BNP N-terminal pro-hormone brain natriuretic peptide
Safety Results
Seventeen patients (81 %) experienced at least one AE, the most common of which (reported in ≥10 % of patients) were falls (five patients, 24 %), diarrhea (five patients, 24 %), extremity pain (four patients, 19 %), and dizziness, dyspnea, vomiting, and constipation (three patients each, 14 %). Four SAEs occurred that were considered possibly related to treatment (ankle fracture, malaise, urinary retention, and transient ischemic attack). The transient ischemic attack was considered mild, and the patient had a history of hypertension and ATTR-related congestive heart failure. This patient discontinued but was treated and recovered. No patient died during the study.
Abnormalities observed on echocardiography and electrocardiography after the beginning of treatment did not indicate adverse treatment effects of tafamidis and were consistent with underlying cardiac morbidity. The most frequently reported treatment-emergent electrocardiograph abnormality was arrhythmia, which occurred in 3 of 21 (14.3 %) patients at baseline and 8 of 18 (44.4 %) patients on treatment. The most common arrhythmia was represented by premature atrial contractions. Analysis of heart rate and electrocardiography interval measurements showed no effect of tafamidis on cardiac conduction or repolarization. Similarly, most echocardiographic parameters remained stable throughout the 12-month study period, and reported changes were not considered clinically meaningful (Table 4).
Discussion
In this phase II, open-label study, we demonstrated the efficacy of tafamidis in stabilizing TTR in a series of patients with TTR-FAP associated with eight different non-Val30Met TTR mutations. Stabilization of TTR was seen in all but one patient at the 6-week primary endpoint and in all patients remaining at the 6- and 12-month secondary endpoints. This finding was accompanied by some worsening of neurological function at Month 12 (NIS-LL score) but also with maintenance of QOL (Norfolk QOL-DN total score) and mBMI.
A relationship between TTR tetramer stabilization and clinical outcomes has been established in carriers of the Val30Met mutation that simultaneously carry an Arg104His or Thr119Met trans-suppressor mutation on their second TTR allele [40–42]. Such compound heterozygotes develop mild pathology or no disease because the trans-suppressor mutation increases the kinetic barrier for tetrameric dissociation, thereby blocking the rate-limiting step of amyloid formation [40–42]. Given that tafamidis also increases the threshold for tetramer dissociation, it appears reasonable to assume a similar causal relationship between TTR stabilization and the positive clinical outcomes seen in this trial.
The finding of TTR stabilization in this study is consistent with the 18-month, double-blind, placebo-controlled trial of tafamidis in patients with Val30Met TTR-FAP, in which 98 % of patients treated with tafamidis achieved TTR stabilization at 18 months [24]. Overall, tafamidis has been shown to stabilize TTR in 36 of 37 studied genotypes. In addition to the nine variants in these two studies, these genotypes include Val122Ile and wild-type TTR (from an open-label study in TTR amyloid cardiomyopathy) [43], as well as an additional 25 of 26 mutations tested in an ex vivo study, with one TTR mutation (Pro24Ser) demonstrating equivocal results potentially related to the long storage time of the plasma sample [23, 25]. This consistent response across variants is notable, given the large number of point mutations that are associated with ATTR [12].
One unexpected finding is that the one patient who did not achieve TTR stabilization at Week 6 (but was allowed to continue tafamidis treatment as a protocol deviation) did actually achieve stabilization at later time points. This interesting result shows that a decision to exclude this patient based on the Week 6 assessment would have been premature and will be reflected in our future study designs.
In the double-blind, placebo-controlled, randomized trial of tafamidis, patients on active treatment had 52 % less neurological deterioration on the NIS-LL after 18 months compared with placebo (a secondary endpoint), with a change from baseline of 2.81 versus 5.83 points, respectively; p = 0.027 [24]. In the present study, a similar change from baseline (2.7 points) was observed on the NIS-LL after 12 months of treatment. It is possible that our trial duration was not long enough to detect a significant change in neurological course of the disease. The patients in our study were also older than those in the double-blind trial, with more severe cardiac involvement and more advanced neuropathy [24].
It should be noted that efforts to address the need for data on long-term outcomes of treatment are in progress. Longer-term data are expected from an open-label extension study that includes the patients who completed the current trial as well as those from the 18-month trial (NCT00925002). All patients will be followed in the open-label study until tafamidis is commercially available in their respective countries. Of note, since European Medicines Agency approval in 2011, tafamidis is now available in most European countries for the treatment of TTR amyloidosis in adult patients with Stage 1 symptomatic polyneuropathy. In addition, long-term data on TTR-FAP patients enrolled in the Transthyretin Amyloidosis Outcomes Survey (THAOS) registry, including data from tafamidis-treated patients, will become available. These efforts are also expected to provide data on survival and functional outcomes such as ambulation.
Because of the reported high prevalence of cardiac manifestations in non-Val30Met ATTR, we assessed cardiac involvement by multiple modalities, including cardiac biomarkers, electrocardiography, and echocardiography. Only one patient had elevated concentrations of troponin I at baseline which remained elevated at all post-baseline timepoints. Patients with NT-pro-BNP levels >1,000 pg/mL (high risk for heart failure) experienced cardiac events consistent with the presence of heart failure while receiving treatment, including peripheral edema and dyspnea. This group demonstrated a median increase in NT-pro-BNP of 520.5 pg/mL over time. Patients with baseline NT-pro-BNP concentrations of <300 pg/mL (low risk for heart failure) demonstrated a median increase in NT-pro-BNP concentrations of 47 pg/mL during treatment.
Despite a large proportion of patients with electrocardiographic and echocardiographic abnormalities at baseline, some of which were of several years duration, there was very little apparent change in cardiac morbidity during the year of treatment. Only four patients demonstrated an increase in IVS thickness of ≥2 mm.
Tafamidis appeared to be well tolerated over 12 months. The AEs reported were not unexpected for the age, neurological status, and cardiac conditions of patients in the study.
In addition to its relatively short duration, this study has several other limitations, most notably the single-arm, open-label design that makes it impossible to determine the efficacy of tafamidis to slow or halt disease progression. While a double-blind, placebo-controlled trial is ideal, the exceedingly low prevalence of TTR-FAP associated with mutations other than Val30Met made such a design impractical. An inherent limitation of the primary endpoint measure is that the immunoturbidimetric assay performed under non-physiological conditions has been developed as a qualitative measure of TTR stabilization and thus cannot quantitate the degree of stabilization in vivo. The cardiac biomarkers (troponin I and NT-proBNP) may be influenced by other factors, such as sodium and fluid ingestion, blood pressure, and paroxysmal supraventricular arrhythmia.
Overall, in patients with TTR-FAP due to the eight mutations evaluated, tafamidis at a dose of 20 mg QD was well tolerated and effectively stabilized TTR in all but one patient by Week 6 and in all patients by Month 6. Although some worsening of neurological function was observed, mBMI and QOL were maintained, and there did not appear to be clinically relevant worsening in cardiac status. Longer-term follow-up is needed to delineate the potential longer-term effects of TTR stabilization on these outcomes, as well as controlled trials specifically evaluating the effects of tafamidis on cardiac function and outcomes.
References
Rapezzi, C., Quarta, C. C., Riva, L., Longhi, S., Gallelli, I., Lorenzini, M., et al. (2010). Transthyretin-related amyloidoses and the heart: a clinical overview. Nature Reviews Cardiology, 7, 398–408.
Blake, C. C., Geisow, M. J., Swan, I. D., Rerat, C., & Rerat, B. (1974). Structure of human plasma prealbumin at 2–5 A resolution. A preliminary report on the polypeptide chain conformation, quaternary structure and thyroxine binding. Journal of Molecular Biology, 88, 1–12.
Monaco, H. L., Rizzi, M., & Coda, A. (1995). Structure of a complex of two plasma proteins: Transthyretin and retinol-binding protein. Science, 268, 1039–1041.
Mita, S., Maeda, S., Shimada, K., & Araki, S. (1986). Analyses of prealbumin mRNAs in individuals with familial amyloidotic polyneuropathy. Journal of Biochemistry, 100, 1215–1222.
Saraiva, M. J. (2001). Transthyretin amyloidosis: a tale of weak interactions. FEBS Letters, 498, 201–203.
Hammarström, P., Jiang, X., Hurshman, A. R., Powers, E. T., & Kelly, J. W. (2002). Sequence-dependent denaturation energetics: a major determinant in amyloid disease diversity. Proceedings of the National Academy of Sciences of the United States of America, 99(Suppl 4), 16427–16432.
Hammarström, P., Wiseman, R. L., Powers, E. T., & Kelly, J. W. (2003). Prevention of transthyretin amyloid disease by changing protein misfolding energetics. Science, 299, 713–716.
Hou, X., Aguilar, M. I., & Small, D. H. (2007). Transthyretin and familial amyloidotic polyneuropathy. Recent progress in understanding the molecular mechanism of neurodegeneration. FEBS Journal, 274, 1637–1650.
Ando, Y., Coelho, T., Berk, J. L., Cruz, M. W., Ericzon, B. G., Ikeda, S., et al. (2013). Guideline of transthyretin-related hereditary amyloidosis for clinicians. Orphanet Journal of Rare Diseases, 8, 31.
Coutinho, P., Martins da Silva, A., Lopes Lima, J., & Resende Barbosa, A. (1980). Forty years of experience with type I amyloid neuropathy. Review of 483 cases. In G. G. Glenner, P. Pinho e Costa, & A. Falcao de Freitas (Eds.), Amyloid and amyloidosis (pp. 88–98). Amsterdam: Excerpta Medica.
Planté-Bordeneuve, V., & Said, G. (2011). Familial amyloid polyneuropathy. Lancet Neurology, 10, 1086–1097.
Connors, L. H., Lim, A., Prokaeva, T., Roskens, V. A., & Costello, C. E. (2003). Tabulation of human transthyretin (TTR) variants, 2003. Amyloid, 10, 160–184.
Saraiva, M. J. (2001). Transthyretin mutations in hyperthyroxinemia and amyloid diseases. Human Mutation, 17, 493–503.
Wilczek, H. E., Larsson, M., & Ericzon, B. G. (2011). Long-term data from the Familial Amyloidotic Polyneuropathy World Transplant Registry (FAPWTR). Amyloid, 18(Suppl 1), 193–195.
Rapezzi, C., Quarta, C. C., Obici, L., et al. (2013). Disease profile and differential diagnosis of hereditary transthyretin-related amyloidosis with exclusively cardiac phenotype: An Italian perspective. European Heart Journal, 34, 520–528.
Holmgren, G., Steen, L., Ekstedt, J., Groth, C. G., Ericzon, B. G., Eriksson, S., et al. (1991). Biochemical effect of liver transplantation in two Swedish patients with familial amyloidotic polyneuropathy (FAP-met30). Clinical Genetics, 40, 242–246.
Skinner, M., Lewis, W. D., Jones, L. A., Kasirsky, J., Kane, K., Ju, S. T., et al. (1994). Liver transplantation as a treatment for familial amyloidotic polyneuropathy. Annals of Internal Medicine, 120, 133–134.
Herlenius, G., Wilczek, H. E., Larsson, M., & Ericzon, B. G. (2004). Ten years of international experience with liver transplantation for familial amyloidotic polyneuropathy: Results from the Familial Amyloidotic Polyneuropathy World Transplant Registry. Transplantation, 77, 64–71.
Takei, Y., Ikeda, S., Ikegami, T., Hashikura, Y., Miyagawa, S., & Ando, Y. (2005). Ten years of experience with liver transplantation for familial amyloid polyneuropathy in Japan: Outcomes of living donor liver transplantations. Internal Medicine, 44, 1151–1156.
Dubrey, S. W., Davidoff, R., Skinner, M., Bergethon, P., Lewis, D., & Falk, R. H. (1997). Progression of ventricular wall thickening after liver transplantation for familial amyloidosis. Transplantation, 64, 74–80.
Stangou, A. J., Hawkins, P. N., Heaton, N. D., Rela, M., Monaghan, M., Nihoyannopoulos, P., et al. (1998). Progressive cardiac amyloidosis following liver transplantation for familial amyloid polyneuropathy: Implications for amyloid fibrillogenesis. Transplantation, 66, 229–233.
Arpesella, G., Chiappini, B., Marinelli, G., Mikus, P. M., Dozza, F., Pierangeli, A., et al. (2003). Combined heart and liver transplantation for familial amyloidotic polyneuropathy. Journal of Thoracic and Cardiovascular Surgery, 125, 1165–1166.
Bulawa, C. E., Connelly, S., Devit, M., Wang, L., Weigel, C., Fleming, J. A., et al. (2012). Tafamidis, a potent and selective transthyretin kinetic stabilizer that inhibits the amyloid cascade. Proceedings of the National Academy of Sciences of the United States of America, 109, 9629–9634.
Coelho, T., Maia, L., Martins da Silva, A., et al. (2012). Tafamidis for transthyretin familial amyloid polyneuropathy: A randomized, controlled trial. Neurology, 79, 785–792.
Packman, J., Fleming, J. N., Souther, E., Grogan, D. R. (2010). Stabilization of transthyretin by tafamidis in transthyretin amyloidosis across different amyloidogenic variants. Paper presented at the The Annual Meeting of the American Society of Human Genetics; November 2–6, 2010, Washington, DC, USA.
Dyck, P. J., Litchy, W. J., Lehman, K. A., Hokanson, J. L., Low, P. A., & O’Brien, P. C. (1995). Variables influencing neuropathic endpoints: The Rochester Diabetic Neuropathy Study of Healthy Subjects. Neurology, 45, 1115–1121.
Casellini, C. M., Barlow, P. M., Rice, A. L., Casey, M., Simmons, K., Pittenger, G., et al. (2007). A 6-month, randomized, double-masked, placebo-controlled study evaluating the effects of the protein kinase C-beta inhibitor ruboxistaurin on skin microvascular blood flow and other measures of diabetic peripheral neuropathy. Diabetes Care, 30, 896–902.
Dyck, P. J., Karnes, J. L., O’Brien, P. C., Litchy, W. J., Low, P. A., & Melton, L. J., 3rd. (1992). The Rochester Diabetic Neuropathy Study: Reassessment of tests and criteria for diagnosis and staged severity. Neurology, 42, 1164–1170.
Dyck, P. J., Davies, J. L., Litchy, W. J., & O’Brien, P. C. (1997). Longitudinal assessment of diabetic polyneuropathy using a composite score in the Rochester Diabetic Neuropathy Study cohort. Neurology, 49, 229–239.
Dyck, P. J., O’Brien, P. C., Litchy, W. J., Harper, C. M., & Klein, C. J. (2005). Monotonicity of nerve tests in diabetes: Subclinical nerve dysfunction precedes diagnosis of polyneuropathy. Diabetes Care, 28, 2192–2200.
Vinik, E. J., Hayes, R. P., Oglesby, A., Bastyr, E., Barlow, P., Ford-Molvik, S. L., et al. (2005). The development and validation of the Norfolk QOL-DN, a new measure of patients’ perception of the effects of diabetes and diabetic neuropathy. Diabetes Technology & Therapeutics, 7, 497–508.
Suhr, O., Danielsson, A., Holmgren, G., & Steen, L. (1994). Malnutrition and gastrointestinal dysfunction as prognostic factors for survival in familial amyloidotic polyneuropathy. Journal of Internal Medicine, 235, 479–485.
Lehrke, S., Steen, H., Kristen, A. V., Merten, C., Lossnitzer, D., Dengler, T. J., et al. (2009). Serum levels of NT-proBNP as surrogate for cardiac amyloid burden: New evidence from gadolinium-enhanced cardiac magnetic resonance imaging in patients with amyloidosis. Amyloid, 16, 187–195.
Lang, R. M., Bierig, M., Devereux, R. B., Flachskampf, F. A., Foster, E., Pellikka, P. A., et al. (2005). Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. Journal of the American Society of Echocardiography, 18, 1440–1463.
Januzzi, J. L., Jr., Sakhuja, R., O’Donoghue, M., Baggish, A. L., Anwaruddin, S., Chae, C. U., et al. (2006). Utility of amino-terminal pro-brain natriuretic peptide testing for prediction of 1-year mortality in patients with dyspnea treated in the emergency department. Archives of Internal Medicine, 166, 315–320.
Januzzi, J. L., Jr., Camargo, C. A., Anwaruddin, S., et al. (2005). The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. American Journal of Cardiology, 95, 948–954.
Behnes, M., Brueckmann, M., Ahmad-Nejad, P., Lang, S., Wolpert, C., Elmas, E., et al. (2009). Diagnostic performance and cost effectiveness of measurements of plasma N-terminal pro brain natriuretic peptide in patients presenting with acute dyspnea or peripheral edema. International Journal of Cardiology, 135, 165–174.
Gertz, M. A., Comenzo, R., Falk, R. H., Fermand, J. P., Hazenberg, B. P., Hawkins, P. N., et al. (2005). Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): A consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18–22 April 2004. American Journal of Hematology, 79, 319–328.
Suhr, O. B., Ericzon, B. G., & Friman, S. (2002). Long-term follow-up of survival of liver transplant recipients with familial amyloid polyneuropathy (Portuguese type). Liver Transplantation, 8, 787–794.
Coelho, T., Chorao, R., Sousa, A., Alves, I., Torres, M., & Saraiva, M. (1996). Compound heterozygotes of transthyretin Met 30 and transthyretin Met 119 are protected from the devastating effects of familial amyloid polyneuropathy. Neuromuscular Disorders, 6(Suppl 1), S20.
Terazaki, H., Ando, Y., Misumi, S., Nakamura, M., Ando, E., Matsunaga, N., et al. (1999). A novel compound heterozygote (FAP ATTR Arg104His/ATTR Val30Met) with high serum transthyretin (TTR) and retinol binding protein (RBP) levels. Biochemical and Biophysical Research Communications, 264, 365–370.
Hammarström, P., Schneider, F., & Kelly, J. W. (2001). Trans-suppression of misfolding in an amyloid disease. Science, 293, 2459–2462.
Falk, R. H., Maurer, M. S., Fedson, S. E., Judge, D., Zeldenrust, S., Quyymi, A., Pano, A., Packman, J., Grogan, D. R. (2011). Tafamidis in transthyretin amyloid cardiomyopathy: Effects on transthyretin stabilization and clinical outcomes. Paper presented at the Heart Failure Society of America—15th Annual Scientific Meeting, September 18–21, 2011, Boston, MA, USA.
Acknowledgments
This study was sponsored by FoldRx, which was acquired by Pfizer Inc in October 2010. The authors wish to thank Peter J. Dyck, P. James B. Dyck, Wolfgang Singer, and Michelle L. Mauermann, from the Mayo Clinic in Rochester, Minnesota, for their assistance with the evaluation and interpretation of key secondary endpoints. The authors also wish to acknowledge Aaron I. Vinik and Etta J. Vinik from the Eastern Virginia Medical School in Norfolk, Virginia, for their development of the Norfolk Quality of Life–Diabetic Neuropathy Questionnaire. Editorial support was provided by Harold P. Schombert and Johanna Nordlie of Scientific Strategy Partners and by Susanne Vidot of Engage Scientific Solutions and was funded by Pfizer Inc.
Conflict of interest statement
Dr. Planté-Bordeneuve received support from FoldRx Pharmaceuticals, which was acquired by Pfizer Inc in October 2010, as a clinical investigator, and serves on the THAOS (natural history disease registry) scientific advisory board but did not receive compensation for this involvement. Dr. Judge received support from FoldRx Pharmaceuticals, which was acquired by Pfizer Inc in October 2010, as a site principal investigator, and has also served as an advisory board member to Pfizer Inc at a meeting in London, UK, in October 2012. Dr. Schmidt received support from FoldRx Pharmaceuticals, which was acquired by Pfizer Inc in October 2010, as a clinical investigator, and has also received payment from Pfizer Inc for serving as an advisor at an advisory board held in Germany. Dr. Merlini has received speaker honoraria payment from Pfizer Inc and is partly supported by a grant from “Associazione Italiana per la Ricerca sul Cancro” Special Program Molecular Clinical Oncology 5 per mille n. 9965; Dr. Obici has received consulting fees from Pfizer Inc; Mr. Packman was an employee of FoldRx Pharmaceuticals during the conduct of this trial and preparation of the manuscript. Ms. Tripp’s employer, DM-STAT, Inc., has received funding for clinical data management and biostatistics of this study from FoldRx Pharmaceuticals. Dr. Perlini received no compensation for his contributions to this manuscript. At the time of manuscript development, Dr. Grogan was an employee of FoldRx Pharmaceuticals, which was acquired by Pfizer Inc in October 2010.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Jozef Bartunek oversaw the review of this article.
Merlini and Planté-Bordeneuve contributed equally as lead authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Merlini, G., Planté-Bordeneuve, V., Judge, D.P. et al. Effects of Tafamidis on Transthyretin Stabilization and Clinical Outcomes in Patients with Non-Val30Met Transthyretin Amyloidosis. J. of Cardiovasc. Trans. Res. 6, 1011–1020 (2013). https://doi.org/10.1007/s12265-013-9512-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-013-9512-x