Abstract
Introduction
The COVID-19 pandemic has underscored the importance of its potential long-term health effects, including its link to new-onset asthma in children. Asthma significantly impacts children’s health, causing adverse outcomes and increased absenteeism. Emerging evidence suggests a potential association between COVID-19 infection and higher rates of new-onset asthma in adults, raising concerns about its impact on children’s respiratory health.
Methods
A retrospective cohort study design was employed, using electronic medical records from the TriNetX database, covering January 1, 2021, to December 31, 2022. Two cohorts of children aged 5 to 18 who underwent SARS-CoV-2 RT-PCR testing were analyzed: unvaccinated children with and without COVID-19 infection, and vaccinated children with and without infection. Propensity score matching was used to mitigate selection bias, and hazard ratio (HR) and 95% CI were calculated to assess the risk of new-onset asthma.
Results
Our study found a significantly higher incidence of new-onset asthma in COVID-19 infected children compared to uninfected children, regardless of vaccination status. In Cohort 1, 4.7% of COVID-19 infected children without vaccination developed new-onset asthma, versus 2.0% in their non-COVID-19 counterparts within a year (HR = 2.26; 95% CI = 2.158–2.367). For Cohort 2, COVID-19 infected children with vaccination showed an 8.3% incidence of new-onset asthma, higher than the 3.1% in those not infected (HR = 2.745; 95% CI = 2.521–2.99). Subgroup analyses further identified higher risks in males, children aged 5–12 years, and Black or African American children. Sensitivity analyses confirmed the reliability of these findings.
Conclusion
The study highlights a strong link between COVID-19 infection and an increased risk of new-onset asthma in children, which is even more marked in those vaccinated. This emphasizes the critical need for ongoing monitoring and customized healthcare strategies to mitigate the long-term respiratory impacts of COVID-19 in children, advocating for thorough strategies to manage and prevent asthma amidst the pandemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic continues to pose significant challenges to global health. SARS-CoV-2, primarily recognized as a respiratory pathogen, is also associated with a spectrum of cardiovascular, pulmonary, neurologic, and metabolic complications [1].
Asthma, marked by airway inflammation and hyperreactivity, profoundly affects children’s health across the globe. Childhood asthma significantly impacts long-term health, leading to deteriorations in health status, increased obesity rates, and a 40–50% rise in absenteeism in early adulthood [2]. These outcomes highlight the profound influence of early health conditions on future health and societal outcomes. Historical data indicate a link between respiratory viruses, including rhinovirus and respiratory syncytial virus, and the exacerbation of asthma symptoms as well as the onset of asthma [3, 4]. Mechanisms involved may include epithelial inflammatory responses, leukocyte activation leading to cytokine and inflammatory factor production, and proliferation of fibroblasts and smooth muscle cells contributing to airway tissue remodeling [3].
Although the processes underlying the increase in asthma incidence from COVID-19 infection remain unclear and underexplored, they could be similar to those observed with other viral infections. Emerging evidences indicate a potential link between COVID-19 infection and an elevated rate of new-onset asthma in adults, possibly resulting from the virus’s inflammatory response, which may induce permanent alterations in airway functionality and sensitivity [5,6,7]. To date, there is limited and inconclusive literature on the risk of asthma following COVID-19 infection in children. A retrospective cohort study found that SARS-CoV-2 PCR positivity was not associated with a new asthma diagnosis in children aged 1-16 [8]. But another study indicated that an asthma diagnosis was negatively associated with COVID-19-related hospitalization in children [9].
COVID-19 vaccines are widely administered and have significantly reduced the risk of severe illness, hospitalization, and mortality [10], literature indicates that a minority of individuals may develop adverse effects after vaccination, such as myocarditis [11], and symptoms related to the menstrual cycle (irregular bleeding, dysmenorrhea, mood changes) [12]. However, the long-term effects of the COVID-19 vaccine remain to be further observed. A meta-analysis found that vaccination against COVID-19 consistently reduced the risk of long COVID symptoms in adult [13]. Despite promising results, further research is needed to fully understand the vaccine’s effectiveness in preventing long COVID across different populations and to identify any potential long-term side effects, especially in children.
We hypothesized that the risk of new-onset asthma in children increases following COVID-19 infection due to virus-induced inflammatory responses. Therefore, we performed a large, retrospective cohort study to assess the relationship between COVID-19 infection and the incidence of new-onset asthma in children. Additionally, we examined whether COVID-19 vaccination could mitigate this risk, aiming to provide a comprehensive understanding of the potential protective effects of vaccination against respiratory complications in this population.
Methods
Data source
This study utilized data from the TriNetX databasehttps://trinetx.com/?mc_cid=7e2ecd5bc5&mc_eid=%5BUNIQID%5D, a global health research network providing access to de-identified electronic medical records. This extensive database covers approximately 250 million individuals across 120 healthcare organizations worldwide, making it the largest COVID-19 dataset available. The available data include demographics, diagnoses (utilizing ICD-10-CM codes), procedures (using ICD-10-PCS or CPT codes), medications (coded in the Veterans Affairs National Formulary), laboratory measurements (LOINC-coded), and healthcare utilization details. The children in the study were recruited from the TriNetX US Collaborative Network, a real-time, multicenter national health network encompassing data from 64 healthcare organizations across all 50 states of the United States.
Data analysis was conducted in February 2024, and covering the study period from January 1, 2021, to December 31, 2022. Patients or the public WERE NOT involved in the design, or conduct, or reporting, or dissemination plans of our research.
Study design
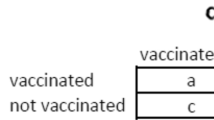
This retrospective cohort study employed data from the TriNetX database, a comprehensive global health research network offering access to electronic medical records from various healthcare organizations. It aimed to evaluate the association between COVID-19 vaccination/infection and the incidence of new-onset asthma in children. Figure 1 presents the flow chart detailing the process of our cohorts’ construction. The study constructed two cohorts comprising children aged 5 to 18 who underwent SARS-CoV-2 RT-PCR testing between January 1, 2021, and December 31, 2022. The index date was set as the day of the COVID-19 RT-PCR test.
Cohort 1 included children who had not received the COVID-19 vaccine before the index date and excluded those with a prior history of COVID-19 infection, asthma, neoplasms, or death before or up to one month after the PCR test. The objective of this cohort was to compare COVID-19-infected unvaccinated children with uninfected unvaccinated children. Cohort 2 consisted of children who had received at least one vaccine dose against COVID-19 before the index date, excluding those with prior COVID-19 infection, asthma, neoplasms, or death before the index date or up to one month after the PCR test. This analysis aimed to compare COVID-19 infected vaccinated children with uninfected vaccinated children.
Baseline characteristics and comorbidities were assessed from records dating one year prior to the index date. The baseline characteristics examined included age, gender, ethnicity, race, medical utilization (outpatient or inpatient services), socioeconomic status (problems related to housing and economic circumstances, factors influencing health status and contact with health services, problems related to education and literacy), lifestyle (nicotine dependence, alcohol related disorders), and comorbidities. Comorbidities comprised essential hypertension, diabetes mellitus, ischemic heart disease, mental, behavioral, and neurodevelopmental disorders, diseases of the nervous system, disorders of lipoprotein metabolism and other lipidemia, liver disease, chronic kidney disease, allergic rhinitis, gastro-esophageal reflux disease, atopic dermatitis, overweight and obesity, malnutrition, disorders of newborn related to short gestation and low birth weight.
Propensity Score Matching (PSM) is a statistical technique used to balance two groups in our study, addressing covariates that could bias the analysis results. We have selected several covariates for matching, including the baseline characteristics and comorbidities, which may be potential risk factors related to the outcome of interest. Balancing them between the study and comparison groups helps mitigate selection bias. On the TriNetX platform, selected demographics, ICD-10-PCS codes for procedures (medical utilization), and ICD-10 codes for comorbidities are set according to these criteria. The time window was set from 365 days to 1 day before the index event (PCR date). After identifying and matching these covariates using a 1:1 ratio, the balance of the matched samples is assessed using Standardized Mean Differences (SMDs). An SMD of < 0.1 indicated that there is no significant difference between the two groups.
To calculate the required sample size, we searched for literature related to our current study, we referenced a document by James P. Senter on asthma caused by SARS-CoV-2 virus [8]. We computed the required sample size analysis using a z-test in G*Power software [14]. The required sample sizes were 59,208 for both the COVID-19 and non-COVID-19 groups. Similarly, we used G*Power software with a z-test to analyze the statistical power.
Outcomes
The primary outcome was the incidence of new-onset asthma or death, identified by ICD-10 codes in the database; the secondary outcome was the use of anti-asthmatic drugs or death. To mitigate the effects of competing risks and survivorship bias, we utilized a combination of ICD-10 codes and relevant medications to define composite outcomes. Given the potential confusion between post-COVID-19 respiratory symptoms and new-onset asthma, our study focuses on the risk of developing new-onset asthma within an 11-month period, from day 30 to day 365 following the index date.
Subgroup analyses
Subgroup analyses were conducted on TriNetX separately to explore the differential risk of new-onset asthma based on sex (female, male), age groups (5–12 years, 13–18 years), and race (White, Black or African American, Asian, and other races), and disease severity. Severe COVID-19 is defined as requiring hospital inpatient services, ICU admission, or mechanical ventilation within one month of infection.
Sensitivity analyses
The sensitivity analyses for the two cohorts utilized varying follow-up periods, from day 30 to day 730 post-index date, to test the reliability of the study’s outcomes. Additionally, our study used the COVID-19 Research Network within TriNetX,, which comprises 92 HCOs on the TriNetX platform. applying the same settings and propensity score matching (PSM) methodology as a sensitivity test to confirm the results’ global applicability.
Statistical analyses
All procedures for data management and hazard ratio (HR) calculations, including 95% confidence intervals (CIs), were conducted within the TriNetX system. Baseline characteristics and comorbidities across all cohorts were evaluated, as detailed in Tables 1 and 2. Propensity score matching was employed for 1:1 matching based on age at index date, gender, ethnicity, race, medical utilization, socioeconomic status, lifestyle, and comorbidities to ensure balanced groups. Standardized mean differences (SMDs) of < 0.1 indicate that there is no significant difference between the two groups. Following this, HRs (95% CIs) were calculated using a Cox proportional hazards model, and p-values were determined via the log-rank test, with values below 0.05 considered statistically significant. Kaplan-Meier analysis estimated event rates over time, and the log-rank test examined differences in survival rates, offering a detailed statistical comparison of the groups.
To address potential biases and confounders, Propensity Score Matching (PSM) was utilized to control for confounding by pairing participants with similar likelihoods of exposure. This method aimed to mitigate bias, and the effectiveness of the matching process was evaluated by examining any residual imbalances. Several sensitivity analyses were conducted to ensure robustness. These included using different networks, such as the COVID-19 Research Network, which consists of 92 healthcare organizations on the TriNetX platform. Additionally, the follow-up period was extended to 730 days, and analyses were stratified by severe COVID-19 infection to explore the impact of geography and infection severity. Model diagnostics were performed to assess the robustness of the statistical outcomes. To address survival and competition biases, each outcome of interest was combined with death in the analysis. This method provided a more accurate representation of the overall effects and minimized potential distortions in the results.
Ethical considerations
This retrospective study has received approval from the Institutional Review Board of Chung Shan Medical University Hospital (IRB reference number CS1-23211). In conducting research using the TriNetX database, we maintained stringent adherence to ethical guidelines. All data were de-identified to protect patient privacy, and the study involved no direct contact with patients. Furthermore, given that the research relied on pre-existing anonymized data, a waiver for patient informed consent was obtained. We are committed to upholding high ethical standards throughout all stages of the research, ensuring both the integrity of the study and the safety of participants.
Results
Baseline characteristics of the study individuals
Figure 1 displays the flowchart for cohort selection and construction, with baseline characteristics of the subjects summarized in Tables 1 and 2. Before Propensity Score Matching (PSM), significant differences were observed between the COVID-19 and non-COVID-19 groups in terms of age at the index date, medical utilization, factors influencing health status, and contact with health services in Cohort 1, as well as medical utilization, factors influencing health status, endocrine, nutritional and metabolic diseases, and allergic rhinitis in Cohort 2. After matching, the study identified an equal number of children in both the COVID-19 and non-COVID-19 groups: 128,753 in Cohort 1 and 23,497 in Cohort 2. A standardized mean difference (SMD) of less than 0.1 indicated minimal and negligible differences in covariates between the two groups. In the COVID-19 infected children group, the mean age at the index date was approximately 11.72 ± 4.09 years in Cohort 1 and 12.20 ± 3.94 years in Cohort 2 at the index date. The majority were female (Cohort 1, 50.68%; Cohort 2, 51.84%) and predominantly of White race (Cohort 1, 56.17%; Cohort 2, 50.57%).
Incidence of new-onset asthma in the COVID-19 and non-COVID-19 groups
Regardless of vaccination status, the COVID-19 infected group exhibited a higher incidence of outcomes compared to the non-infected group. The incidence of new-onset asthma or death was illustrated in the COVID-19 infected group compared to non-infected group across various cohorts (see Table 3). In Cohort 1, 4.7% of COVID-19 infected unvaccinated children developed new-onset asthma or death, compared to 2.0% in their non-COVID-19 counterparts within a year. For Cohort 2, COVID-19 infected vaccinated children exhibited an 8.3% incidence of new-onset asthma or death, which was higher than the 3.1% observed in those who were not infected. The COVID-19 infected group exhibited a 126% increased risk (HR = 2.26; 95% CI = 2.158–2.367) of developing new-onset asthma or death compared to the non-infected group in Cohort 1 and 174% increased risk (HR = 2.745; 95% CI = 2.521–2.99) in Cohort 2. For the secondary outcome, in Cohort 1, 21.1% of COVID-19-infected unvaccinated children were either prescribed anti-asthmatic drugs or died, compared to 16.7% in the non-COVID-19 group (HR = 1.236; 95% CI = 1.214–1.259). In contrast, Cohort 2 exhibited a slightly higher incidence, with 28.3% of COVID-19-infected vaccinated children experiencing the same outcomes compared to 21.7% in their non-infected counterparts (HR = 1.375; 95% CI = 1.325–1.426). Regarding the composite outcomes, Cohort 1 observed a 22.0% incidence among COVID-19-infected unvaccinated children versus 17.3% in the non-infected group (HR = 1.218; 95% CI = 1.196–1.24). Cohort 2 exhibited a further elevated incidence of 27.5% in COVID-19-infected vaccinated children compared to 21.7% in the non-infected group (HR = 1.342; 95% CI = 1.293–1.392). These results show that children who are infected with COVID-19 after being vaccinated against COVID-19 are at a higher risk of developing asthma than children who are infected with COVID-19 who are not vaccinated against COVID-19.
*The achieved power of this study is calculated to be approximately 1 for all tests.
Initially, to address survival bias and competition bias, we combined each outcome of interest with death for the analysis. We independently analyzed ‘death’ and recreated the table, which is presented in Table S2. We found that COVID-19 infection had a non-significant statistical impact on child mortality within one year. However, the other outcomes of interest, including new-onset asthma, the use of asthma medication, and the composite outcome, all showed an increased risk.
Figure 2 presents Kaplan-Meier curves for the incidence of new-onset asthma, the use of any anti-asthmatic drugs, and a composite outcome, all curves show a trend of increasing incidence over time. The log-rank test revealed a significant difference between the COVID-19 group and non-COVID-19 group (p < 0.001). Supplementary Table S1 shows the survival probability calculated on TriNetX on the 30th, 60th, 90th, 180th, and 365th days after the index date in Cohort 1 and Cohort 2.
Subgroup analysis
We further examined the risk of incident asthma in subgroups based on sex, age, and race, as detailed in Tables 4 and 5. Subgroup analysis revealed a higher risk of new-onset asthma or death among males, children aged 5–12 years, and those who are Black or African American, regardless of vaccination status. Specifically, for Cohort 1, the HR for asthma or death among males was 2.308 (95% CI = 2.168–2.456), compared to females with an HR of 2.212 (95% CI = 2.071–2.364). For children aged 5–12 years, the HR was 1.883 (95% CI = 1.786–1.985), and for Black or African American individuals, the HR was 2.204 (95% CI = 2.029–2.393). In Cohort 2, similar trends were observed. The HR for asthma or death among males was 2.747 (95% CI = 2.463–3.068), and for children aged 5–12 years, the HR was 2.517 (95% CI = 2.272–2.788). Black or African American individuals in this cohort had an HR of 2.948 (95% CI = 2.512–3.46) for asthma or death.
When restricting the analysis to severe COVID-19 infections, defined by hospital inpatient stays, intensive care unit stays, or mechanical ventilation within one month after infection, there was a significantly higher risk of asthma during the follow-up period for both Cohort 1 (HR = 3.743; 95% CI = 2.975–4.71) and Cohort 2 (HR = 2.964; 95% CI = 2.046–4.293) (Table S3).
Sensitivity analysis
In the sensitivity analysis of two cohorts, when extending the follow-up time to 2 years, the COVID-19 group exhibited a consistent trend of higher risk for new-onset asthma compared with the non-COVID-19 group. Moreover, this study utilized the COVID-19 Research Network on TriNetX and yielded results that were consistent with the primary approach (Table S4, Figure S1).
Discussion
This large retrospective cohort study utilized TriNetX, a real-world database, to evaluate the impact of COVID-19 infection and vaccination on the incidence of new-onset asthma in children. Regardless of vaccination status, groups infected with COVID-19 exhibited a significantly increased incidence of new-onset asthma, anti-asthmatic drug use and composite outcomes compared to those not infected, from the 30th to the 365th day following the index date, over a period of 11 months. The subgroup analysis was consistent across gender, age, and racial groups.
The link between viral infections and asthma exacerbation is well-established, but the association with new-onset asthma, particularly in the context of COVID-19, is a relatively novel area of research. Our findings support the increasing evidence that COVID-19 may trigger asthma development. This corresponds to findings from research on other respiratory viruses, such as rhinovirus (RV) and respiratory syncytial virus (RSV), which are recognized for triggering asthma in individuals with a genetic predisposition. In a Finnish study, rhinoviruses were also identified as significant inducers of wheezing [15]. A systematic review of 28 articles revealed an increased risk of asthma following hospitalization for RSV in infancy and childhood [16]. Also, the findings of a meta-analysis suggested that experiencing wheezing illness caused by RV during the first 3 years of life was linked to the later development of wheezing or asthma [17]. Rhinoviruses infection promotes the secretion of cytokines from epithelial cells, such as IL-6, IL-8, IL-11, and GM-CSF, which may trigger the onset of asthma [18,19,20,21]. In a large, population-based, birth cohort study (INSPIRE), not being infected with RSV in the first year of life was associated with a 26% lower risk of asthma at age 5 compared to those who were infected with RSV (adjusted RR = 0.74, 95% CI = 0.58–0.94, p = 0.014).22 Furthermore, RSV infection in infants has been shown to affect T-cell memory responses and airway epithelium development [23]. The interaction of viral virulence factors, individual genetic susceptibilities, and environmental factors—such as exposure to the airway microbiome—plays a significant role in the aggravation of wheezing illnesses and the increased risk of asthma development [24, 25].
Some literature has indicated the impact of COVID-19 on individuals with asthma following infection. The interaction of the virus with the ACE2 receptor, which is variably expressed in asthma patients, may influence the severity of COVID-19 and could potentially exacerbate asthma symptoms [26]. One study highlighted the importance of host factors in both asthma and COVID-19, discovering shared genetic and molecular pathways in the two conditions through the analysis of bronchoalveolar lavage fluid, suggests that COVID-19 may contribute to the exacerbation or onset of asthma in affected patients [27].
To date, there are few studies that explore the issue of new-onset asthma caused by COVID-19 infection. A nationwide, population-based cohort study emphasized that adults who were infected with COVID-19 had a higher incidence of new-onset asthma compared to those uninfected [5]. This suggests a potential risk factor for developing asthma following COVID-19 infection. However, earlier research has been limited by smaller sample sizes and relatively brief observation periods.
A review article found that many viruses, particularly single-stranded RNA viruses, can cause asthma [28]. SARS-CoV, also a single-stranded RNA virus, may have similar effects or mechanism. Research shows that certain viruses can cause epithelial cells to produce pro-Th2 cytokines such as IL-25 and IL-33, activating ILC2s, DCs, and Th2 cells, thereby promoting allergic inflammation [29, 30]. It has been reported that serum IL-33 levels are elevated in COVID-19 patients. This cytokine increases neutrophil activity via the IL-33/ST2 pathway and inhibits IFN-I secretion by pDCs. Additionally, IL-33 disrupts the Th17/Treg balance in the lungs, leading to cytokine storms and immune damage. IL-33 also causes hyperactivation of ILC2s, differentiation of M2 macrophages, and secretion of TGF-β and IL-13 [31]. Common coronavirus infections in children trigger host responses similar to those induced by other viruses, such as increased expression of IL6 and ACE2 [32]. COVID-19 infection can also trigger an imbalanced immune response, characterized by a cytokine storm and overproduction of pro-inflammatory cytokines [33,34,35]. Additionally, the infection may impair mucociliary clearance, a vital respiratory defense, leading to mucus and pathogen accumulation in the airways [33]. In COVID-19 patients, there’s a marked increase in IL-4 expression and a rise in M2 macrophages, suggesting a significant Th2 immune response and anti-inflammatory activity that potentially leads to airway remodeling [36]. Unlike the limited Th1/Th17 response, the strong Th2 response in SARS-CoV-2 induced lung injury suggests a mechanism that favors airway remodeling [36].
In the United States, the Pfizer-BioNTech COVID-19 vaccine was authorized for those 16 and older on December 11, 2020, and approved by the FDA on August 23, 2021. Its use expanded to 12–15 year-olds on May 10, 2021, and to children 5–11 on October 29, 2021. By July 6, 2022, CDC data showed 37% of 5–11 year-olds and 70% of 12–17 year-olds had received at least one vaccine dose. Two case reports have indicated that the SARS-CoV-2 vaccine could potentially exacerbate asthma, suggesting that repeated vaccinations might be a risk factor for severe asthma flare-ups. This association is thought to involve inflammatory and immunological responses [37, 38].
To date, there have been several cohort studies that have linked COVID-19 infection in both adults and children. Kim utilized the Korean National Health Insurance claim-based database to design three cohorts for adults and found that 1.6% of the COVID-19 group and 0.7% of the non-infected group developed asthma during the 6-month observation period. The COVID-19 cohort faced a higher risk of new-onset asthma (aHR 2.14; 95% CI 1.88–2.45) than matched controls, aligning with our findings. Kim noted that vaccinated infected individuals had a lower asthma risk compared to their unvaccinated counterparts (aHR 0.82; 95% CI 0.76–0.89). However, vaccination did not reduce asthma risk in those uninfected by COVID-19 (aHR 0.95; 95% CI 0.87–1.04) [6]. A study with cohorts from South Korea, Japan, and the UK shows a significant rise in allergic diseases like asthma and allergic rhinitis after COVID-19, persisting over six months and worsening with disease severity. Vaccination with at least two COVID-19 doses provided protection [7]. As for children, there is limited and inconclusive literature on the risk of asthma following COVID-19 infection in children. A small sample size retrospective chart review revealed that most children diagnosed with COVID-19 had normal spirometry and plethysmography results [39]. Furthermore, a retrospective cohort study using EHR data from a single institution within the Children’s Hospital of Philadelphia Care Network found no association between SARS-CoV-2 PCR positivity and new asthma diagnoses in children aged 1–16 over an 18-month follow-up period (HR: 0.96; P = 0.79).8 Interestingly, another study indicated that an asthma diagnosis was negatively associated with COVID-19-related hospitalization in children [9]. To date, no strong evidence has been published in the literature to suggest a positive or negative association between COVID-19 and new-onset asthma in children.
However, our study reveals contrasting results, indicating that children vaccinated against COVID-19 who contracted the virus had an increased risk of developing new-onset asthma (HR = 2.745, 95% CI = 2.521, 2.99). This could be attributed to various factors, including immune response to the vaccine, the interaction between the vaccine and the virus, or other unrelated environmental or genetic factors.
Our subgroup analysis identified higher risks among younger age groups and Black or African American individuals. Following COVID-19 infection, infants developed a strong mucosal immune response marked by inflammatory cytokines, IFN-α, and Th-17 and neutrophil markers like IL-17, IL-8, and CXCL1 [40]. This response led to further respiratory inflammation and associated symptoms, which may explain why younger age groups have a higher risk of developing asthma. Regarding ethnicity, a large database analysis of adults across three national cohorts (UK, South Korea, Japan) found consistent results, indicating that post-COVID-19 effects on allergic diseases are not influenced by race [7]. However, the above study focused on adults and mainly included data from Asian countries. For children, we speculate that the immune response of Black individuals after COVID-19 infection may be influenced by genetics, socioeconomic status, and health disparities, but more research is needed to confirm this.
The strengths of our study include its use of a large, nationwide, population-based cohort and rigorous statistical analyses, including propensity score matching, to reduce selection bias. Moreover, our research provides valuable insights into the association between COVID-19 vaccination/infection and the incidence of new-onset asthma in children, an area currently seldom explored.
Our retrospective cohort analysis faced several limitations. The generalizability of our findings is affected by regional bias and variations in healthcare systems within the TriNetX database, which primarily includes U.S. data. This limits the applicability of our results to regions with different healthcare systems and demographics. Additionally, missing data is an issue, as some asthmatic patients, particularly children, may not have sought care from HCOs in the TriNetX network. Confounding bias is another concern; although we used Propensity Score Matching (PSM) to control for biases, unmeasured confounders such as family history of asthma and environmental exposures may still influence the results. Misclassification bias was mitigated by restricting COVID-19 diagnoses to PCR-positive cases. However, relying solely on ICD-10 codes without pulmonary function tests can reduce diagnostic accuracy. Using asthma medications as a secondary outcome helped enhance diagnostic precision. The study also overlooked the impact of COVID-19 variants and vaccination timing or type, which could significantly affect immune responses and asthma risk. Despite these efforts, the observational nature of our study limits the ability to confirm causality.
Conclusion
This study identifies a significant link between COVID-19 infection and an increased incidence of new-onset asthma in children, with higher risk in vaccinated individuals. These findings underscore the need for ongoing monitoring and targeted healthcare strategies to mitigate long-term respiratory impacts in children.
Public health actions should focus on enhanced surveillance of respiratory health post-COVID-19 infection, regardless of vaccination status. Tools like the ISAAC (International Study of Asthma and Allergies in Childhood) questionnaire, the GINA (Global Initiative for Asthma) symptom control tool, and the PACS (Pediatric Asthma Control Score) can help identify high-risk children early.
Clinicians should be aware of new-onset asthma in pediatric patients post-COVID-19 and implement preventive measures and early interventions. This includes providing asthma education for parents, educators, and children, and offering professional asthma management plans with personalized medication guidance and environmental control advice. Healthcare systems should establish asthma databases to track incidence, treatment outcomes, and health results to guide policymaking. As the virus continues to mutate, it is essential to closely monitor whether the long-term prevalence of COVID-19 affects asthma risk in children.
Further research is necessary to explore causal pathways linking COVID-19 to asthma development, refine public health guidelines, and better protect children’s health in future pandemics.
Data availability
The de-identified data in the TriNetX federated network database can only be accessed by researchers who are either part of the network or have a collaboration agreement with TriNetX. We utilized data from the TriNetX database under a no-cost collaboration agreement between Chung Shan Medical University Hospital and TriNetX. Under this agreement, we accessed de-identified data in accordance with the agreements and institutional approvals already in place between TriNetX and their partner institutions. The data utilized in this study can be obtained from TriNetX by future researchers who establish a collaboration with TriNetX.
References
Vargas Centanaro G, Calle Rubio M, Álvarez-Sala Walther JL, Martinez-Sagasti F, Albuja Hidalgo A, Herranz Hernández R, Rodríguez Hermosa JL. Long-term outcomes and recovery of patients who survived COVID-19: LUNG INJURY COVID-19 study. Open Forum Infect Dis. 2022;9(4):ofac098.
Fletcher JM, Green JC, Neidell MJ. Long term effects of childhood asthma on adult health. J Health Econ. 2010;29(3):377–87.
Hayashi Y, Sada M, Shirai T, Okayama K, Kimura R, Kondo M et al. Rhinovirus infection and Virus-Induced Asthma. Viruses. 2022;14(12).
Mikhail I, Grayson MH. Asthma and viral infections: an intricate relationship. Ann Allergy Asthma Immunol. 2019;123(4):352–8.
Kim BG, Lee H, Yeom SW, Jeong CY, Park DW, Park TS et al. Increased risk of New-Onset Asthma after COVID-19: a Nationwide Population-based Cohort Study. J Allergy Clin Immunol Pract. 2023.
Lee H, Kim BG, Chung SJ, Park DW, Park TS, Moon JY, et al. New-onset asthma following COVID-19 in adults. J Allergy Clin Immunol Pract. 2023;11(7):2228–31.
Oh J, Lee M, Kim M, Kim HJ, Lee SW, Rhee SY, et al. Incident allergic diseases in post-COVID-19 condition: multinational cohort studies from South Korea, Japan and the UK. Nat Commun. 2024;15(1):2830.
Senter JP, Aisenberg LK, Dudley JW, Luan X, Huang J, Kenyon CC, Hill DA. COVID-19 and Asthma Onset in Children. Pediatrics. 2024;153(5).
Floyd GC, Dudley JW, Xiao R, Feudtner C, Taquechel K, Miller K, et al. Prevalence of asthma in hospitalized and non-hospitalized children with COVID-19. J Allergy Clin Immunol Pract. 2021;9(5):2077–e92.
Echaide M, Chocarro de Erauso L, Bocanegra A, Blanco E, Kochan G, Escors D. mRNA vaccines against SARS-CoV-2: advantages and caveats. Int J Mol Sci. 2023;24(6).
Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risk of Myocarditis after sequential doses of COVID-19 vaccine and SARS-CoV-2 infection by Age and Sex. Circulation. 2022;146(10):743–54.
Lessans N, Rottenstreich A, Stern S, Gilan A, Saar TD, Porat S, Dior UP. The effect of BNT162b2 SARS-CoV-2 mRNA vaccine on menstrual cycle symptoms in healthy women. Int J Gynaecol Obstet. 2023;160(1):313–8.
Català M, Mercadé-Besora N, Kolde R, Trinh NTH, Roel E, Burn E, et al. The effectiveness of COVID-19 vaccines to prevent long COVID symptoms: staggered cohort study of data from the UK, Spain, and Estonia. Lancet Respir Med. 2024;12(3):225–36.
Kang H. Sample size determination and power analysis using the G*Power software. J Educ Eval Health Prof. 2021;18:17.
Kotaniemi-Syrjänen A, Vainionpää R, Reijonen TM, Waris M, Korhonen K, Korppi M. Rhinovirus-induced wheezing in infancy–the first sign of childhood asthma? J Allergy Clin Immunol. 2003;111(1):66–71.
Szabo SM, Levy AR, Gooch KL, Bradt P, Wijaya H, Mitchell I. Elevated risk of asthma after hospitalization for respiratory syncytial virus infection in infancy. Paediatr Respir Rev. 2013;13(Suppl 2):S9–15.
Liu L, Pan Y, Zhu Y, Song Y, Su X, Yang L, Li M. Association between rhinovirus wheezing illness and the development of childhood asthma: a meta-analysis. BMJ Open. 2017;7(4):e013034.
Subauste MC, Jacoby DB, Richards SM, Proud D. Infection of a human respiratory epithelial cell line with rhinovirus. Induction of cytokine release and modulation of susceptibility to infection by cytokine exposure. J Clin Invest. 1995;96(1):549–57.
Einarsson O, Geba GP, Zhu Z, Landry M, Elias JA. Interleukin-11: stimulation in vivo and in vitro by respiratory viruses and induction of airways hyperresponsiveness. J Clin Invest. 1996;97(4):915–24.
Gern JE, Vrtis R, Grindle KA, Swenson C, Busse WW. Relationship of upper and lower airway cytokines to outcome of experimental rhinovirus infection. Am J Respir Crit Care Med. 2000;162(6):2226–31.
Gern JE, Busse WW. Association of rhinovirus infections with asthma. Clin Microbiol Rev. 1999;12(1):9–18.
Rosas-Salazar C, Chirkova T, Gebretsadik T, Chappell JD, Peebles RS Jr., Dupont WD, et al. Respiratory syncytial virus infection during infancy and asthma during childhood in the USA (INSPIRE): a population-based, prospective birth cohort study. Lancet. 2023;401(10389):1669–80.
Chirkova T, Rosas-Salazar C, Gebretsadik T, Jadhao SJ, Chappell JD, Peebles RS Jr., et al. Effect of infant RSV infection on memory T cell responses at Age 2–3 years. Front Immunol. 2022;13:826666.
Jartti T, Gern JE. Role of viral infections in the development and exacerbation of asthma in children. J Allergy Clin Immunol. 2017;140(4):895–906.
Bottau P, Liotti L, Laderchi E, Palpacelli A, Calamelli E, Colombo C, et al. Something is changing in viral infant Bronchiolitis Approach. Front Pediatr. 2022;10:865977.
Branco A, Sato MN, Alberca RW. The possible dual role of the ACE2 receptor in Asthma and Coronavirus (SARS-CoV2) infection. Front Cell Infect Microbiol. 2020;10:550571.
Jiang Y, Yan Q, Liu CX, Peng CW, Zheng WJ, Zhuang HF, et al. Insights into potential mechanisms of asthma patients with COVID-19: a study based on the gene expression profiling of bronchoalveolar lavage fluid. Comput Biol Med. 2022;146:105601.
Novak N, Cabanillas B. Viruses and asthma: the role of common respiratory viruses in asthma and its potential meaning for SARS-CoV-2. Immunology. 2020;161(2):83–93.
Jackson DJ, Makrinioti H, Rana BM, Shamji BW, Trujillo-Torralbo MB, Footitt J, et al. IL-33-dependent type 2 inflammation during rhinovirus-induced asthma exacerbations in vivo. Am J Respir Crit Care Med. 2014;190(12):1373–82.
Beale J, Jayaraman A, Jackson DJ, Macintyre JDR, Edwards MR, Walton RP, et al. Rhinovirus-induced IL-25 in asthma exacerbation drives type 2 immunity and allergic pulmonary inflammation. Sci Transl Med. 2014;6(256):256ra134.
Gao Y, Cai L, Li L, Zhang Y, Li J, Luo C et al. Emerging effects of IL-33 on COVID-19. Int J Mol Sci. 2022;23(21).
Sajuthi SP, DeFord P, Li Y, Jackson ND, Montgomery MT, Everman JL, et al. Type 2 and interferon inflammation regulate SARS-CoV-2 entry factor expression in the airway epithelium. Nat Commun. 2020;11(1):5139.
Bridges JP, Vladar EK, Huang H, Mason RJ. Respiratory epithelial cell responses to SARS-CoV-2 in COVID-19. Thorax. 2022;77(2):203–9.
Guo TJF, Singhera GK, Leung JM, Dorscheid DR. Airway Epithelial-Derived Immune mediators in COVID-19. Viruses. 2023;15(8).
Harne R, Williams B, Abdelal HFM, Baldwin SL, Coler RN. SARS-CoV-2 infection and immune responses. AIMS Microbiol. 2023;9(2):245–76.
de Vaz CB, de Azevedo MLV, Nagashima S, Martins APC, Malaquias MAS, Miggiolaro A, et al. IL-4/IL-13 remodeling pathway of COVID-19 lung injury. Sci Rep. 2020;10(1):18689.
Colaneri M, De Filippo M, Licari A, Marseglia A, Maiocchi L, Ricciardi A, et al. COVID vaccination and asthma exacerbation: might there be a link? Int J Infect Dis. 2021;112:243–6.
Ando M, Satonaga Y, Takaki R, Yabe M, Kan T, Omote E, et al. Acute asthma exacerbation due to the SARS-CoV-2 vaccine (Pfizer-BioNTech BNT162b2 messenger RNA COVID-19 vaccine [Comirnaty(®)]). Int J Infect Dis. 2022;124:187–9.
Leftin Dobkin SC, Collaco JM, McGrath-Morrow SA. Protracted respiratory findings in children post-SARS-CoV-2 infection. Pediatr Pulmonol. 2021;56(12):3682–7.
Wimmers F, Burrell AR, Feng Y, Zheng H, Arunachalam PS, Hu M, et al. Multi-omics analysis of mucosal and systemic immunity to SARS-CoV-2 after birth. Cell. 2023;186(21):4632–e5123.
Funding
No external funding was received for this study.
Author information
Authors and Affiliations
Contributions
CYY: Study design, data acquisition and analysis, manuscript drafting.YHS: Accessed data and verified it.CCL: Data interpretation and critically revised the manuscript.All authors: Revised the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Competing interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, CY., Shih, YH. & Lung, CC. The association between COVID-19 vaccine/infection and new-onset asthma in children - based on the global TriNetX database. Infection (2024). https://doi.org/10.1007/s15010-024-02329-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-024-02329-3