Abstract
Background
BCG vaccination, originally used to prevent tuberculosis, is known to “train” the immune system to improve defence against viral respiratory infections. We investigated whether a previous BCG vaccination is associated with less severe clinical progression of COVID-19
Methods
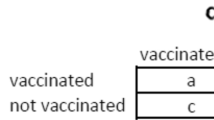
A case-control study comparing the proportion with a BCG vaccine scar (indicating previous vaccination) in cases and controls presenting with COVID-19 to health units in Brazil. Cases were subjects with severe COVID-19 (O2 saturation < 90%, severe respiratory effort, severe pneumonia, severe acute respiratory syndrome, sepsis, and septic shock). Controls had COVID-19 not meeting the definition of “severe” above. Unconditional regression was used to estimate vaccine protection against clinical progression to severe disease, with strict control for age, comorbidity, sex, educational level, race/colour, and municipality. Internal matching and conditional regression were used for sensitivity analysis.
Results
BCG was associated with high protection against COVID-19 clinical progression, over 87% (95% CI 74–93%) in subjects aged 60 or less and 35% (95% CI − 44–71%) in older subjects.
Conclusions
This protection may be relevant for public health in settings where COVID-19 vaccine coverage is still low and may have implications for research to identify vaccine candidates for COVID-19 that are broadly protective against mortality from future variants. Further research into the immunomodulatory effects of BCG may inform COVID-19 therapeutic research.
Similar content being viewed by others
Background
Bacillus Calmette-Guérin (BCG) vaccine is safe and low-cost. Currently, recommendations for BCG vaccination are based on local incidence of tuberculosis (TB) at birth, in childhood, or for target groups.
BCG vaccination has well-known non-specific effects. These can be therapeutic or preventive. Immunotherapy with BCG has been the standard treatment for bladder cancer for 50 years [1]. Similarly, BCG vaccination can protect against early mortality in low-income/high-infant mortality countries, probably via protection against respiratory viral infections [2,3,4,5], including respiratory syncytial virus [6]. It is suggested that the non-specific effect of BCG is mediated through immunomodulation or “trained immunity” [4, 7, 8].
Given the evidence for non-specific effects of BCG against viral respiratory infections, the hypothesis that BCG vaccination might offer some protection against COVID-19 was raised early in the epidemic, and a number of analyses of existing data were conducted, with conflicting results [9,10,11,12,13]. More recently, original research was conducted, again with conflicting results [14,15,16,17,18,19,20,21,22].
The reason for conflicting results is not clear. It is of interest that in studies of COVID-19-specific vaccines, protection against infection, clinical progression, or severe or fatal forms differ. Likewise, the protection conferred by BCG against tuberculosis is complex and differs according to whether it is protection against infection or progression from infection to disease [23] against different forms and whether it is given at birth/to people never exposed or at a later age/after exposure to non TB mycobacteria [24, 25].
The biological mechanism behind BCG reduction in non-specific morbidity and mortality, including against COVID-19, is poorly understood, with ongoing experimental research and theoretical explanations put forward [16, 18, 26,27,28].
Here, we present the results of an epidemiological study estimating the effect of neonatal BCG vaccination on reducing the risk of clinical progression from symptomatic COVID-19 to severe forms of the disease in individuals who did not receive a COVID-19 vaccination.
Methods
Study design
Initially, the study design is unmatched case-control study. We conducted an unplanned sensitivity analysis, with subsequent strict internal matching. Data collection was carried out during 2020 and 2021.
Study population
The study population is cases of COVID-19 (confirmed by positive RT-PCR) presenting at COVID-19 referral hospital/health care units in the cities of Salvador, BA; São Paulo, SP; and Recife, PE, with no age restriction.
Exclusion criteria
Past vaccination against COVID-19. Recruitment started before vaccination against COVID-19 was available; after vaccination was introduced, subjects who had received any dose of any COVID-19 vaccine were not recruited. COVID-19 vaccination status was ascertained by card or patient history.
Case definition and recruitment
Individuals were hospitalised in intensive care units with severe COVID-19. Severity was defined according to the Brazilian Ministry of Health clinical management protocol for hospitalisation for COVID-19: O2 saturation < 90%, severe respiratory effort, severe pneumonia, severe acute respiratory syndrome (SRAG), sepsis, and septic shock [29].
Control definition and recruitment
Individuals with COVID-19 present at the same health unit as cases who did not meet the above criteria for severity and were not hospitalised or were hospitalised in general wards. An exception was the final period of data collection in the city of Salvador, Bahia. The referral hospital in Salvador modified its routine to receive only severe COVID-19 patients—i.e. only those who met the criteria to be a case in the study. During this period in Salvador, controls were recruited at a primary attention referral centre that was receiving subjects with COVID-19 that did not require intensive care. A sensitivity analysis was conducted excluding cases and controls from Salvador.
Exposure variable
Past intradermal BCG vaccination status was ascertained through the examination of the left or right upper arm for the presence or absence of a BCG vaccine scar.
Post hoc internal matching for sensitivity analyses
City, age (within 2 years interval or less), and presence of any comorbidity.
Data collection
Examination of the arm for a BCG scar was conducted on admission to the health unit, by a doctor or nurse from the staff. In case of doubt, the research team member responsible for the local data collection carried out another inspection. The ascertainment of BCG scar was conducted before the patients were classified as cases or controls. We did not enquire about the history of oral BCG. Information on the date of onset of symptoms and clinical, epidemiological, and laboratory data was collected from medical records, in consultation with the laboratory environment manager and when necessary, from telephone contacts.
Sample size
The required sample was estimated as 1250 (625 cases and 625 controls) using Kelsey’s formula for unpaired case-control studies [30] and considering an alpha value of 5%, power 80%, exposure (BCG scar) in controls 65%, vaccine efficacy 30%, and the same number of cases and controls, with 20% losses.
Analyses
The summary OR was estimated using the Mantel-Haenszel method for unpaired samples. Modelling with logistic regression used unconditional regression analysis to control for age (in 10-year intervals), race/colour, sex, educational level, presence of comorbidity, and city; sensitivity analysis was conducted using conditional regression analysis after rigorous matching of cases and controls by age (2 years of age difference or less), presence or absence of comorbidity, and municipality. Interactive terms were added to investigate if protection varied with age and with the presence of comorbidity. The protective vaccine efficacy (VE) was 1 − OR. To fit the best model, Akaike estimator was performed [31].
Results
We included 497 cases and 670 controls, from three Brazilian cities (São Paulo, SP; Salvador, BA; Recife, PE). The mean age for cases and controls were 55.8 [± 18.3] and 41.3 [± 14.7], respectively. Cases were older than controls (41.8% of cases and 9.3% of controls were aged above 60); 59.6% of the cases and 43.2% of the controls were male. 58.7% of cases and 92.1% of controls had a BCG scar. Controls had higher education levels (33.0%) than cases (11.8%). Brown race/colour was predominant in both cases (70.1%) and controls (47.6%). Comorbidity was present in 80.2% of cases and 33.8% of controls. For all variables above, the differences were statistically significant (Table 1). The crude odds ratio (OR) of BCG vaccination was 0.12 (95% confidence interval (95% CI): 0.09–0.17) corresponding to an overall protective effect of 88% (95% CI: 83.0–91.3%). After adjusting by race/colour, schooling, sex, age, municipality, and presence of comorbidity, the OR was 0.27 (95% CI: 0.17–0.44) corresponding to an overall protective effect of 73% (95% CI: 56.0–83.0%) (Table 2). In a sensitivity analysis using matched data on age and comorbidity, the overall crude protective effect remained similar, 65%, OR= 0.35 (95% CI: 0.21–0.58) and 72% OR = 0.28 (95% CI: 0.13–0.58), when further adjusted for sex, education, and race/colour. In an analysis of matched data on age, comorbidity, and municipality, the overall crude protective effect was 70%, OR = 0.30 (95% CI: 0.17–0.53). After adjusting by race/colour, schooling, and sex, this protective effect was 70% OR = 0.30 (95% CI: 0.14–0.63) (Table 2).
The protective effect of BCG vaccination was higher in those without comorbidities 85% (95% CI: 71.0– 91.6%) than in those with comorbidities 76% (95% CI: 62.0–85.0%). Table 3 shows that the protective effect was low in those aged over 60, 35.0% (95% CI: − 44–71%), and very high in those aged 60 years or less, 87% (95% CI: 74.1–93.1%) (Table 3).
Discussion
In our study, a previous intradermal BCG vaccination indicated by the presence of scar conferred protection against progression to severe COVID-19 in (COVID-19 unvaccinated) subjects in all age groups, 87% in individuals aged 60 or less, and 35% in older subjects.
The study has some strengths and limitations. Case-control studies are vulnerable to bias, which in this study would have been introduced if ascertainment of BCG vaccination was different in cases and controls. This was prevented by ascertaining the presence of BCG vaccination scar at arrival at the referral hospital/health unit for individuals with COVID-19, before they were allocated to an ICU (more severe, cases) or not (controls). An exception was the final period of data collection in the city of Salvador. Because of a change in admission policy, the final controls were selected from a referral centre who was receiving subjects with COVID-19 that did not require intensive care; sensitivity analysis including and excluding those showed very little change.
Another related concern is whether BCG scar is a good indicator of previous intradermal BCG vaccination. There is good evidence that scar correlates well with intradermal vaccination until at least the age of 14 years in Brazil [32]. Even if scars were not a good indicator of previous intradérmic BCG vaccination, and this was unrelated to the subject being a case or a control, such nondifferential misclassification could only underestimate vaccine protection in the control group [33].
Another potential limitation is that we used scar as the only indication of previous BCG vaccination; information on oral BCG was not collected. Intradermal BCG was introduced in Brazil in 1968; so individuals born before that year, who would have been 56 or over at the time of the study, could have received oral BCG. This has two implications: first, the few people aged 56 or older in the study classified as vaccinated had a BCG scar, so they must have received intradermal BCG, either at school age, during a catch-up vaccination, or because a potential exposure, for example, as a worker in health care settings. Second, if oral BCG (like intradérmic BCG) has an effect in decreasing COVID-19 severity, and a proportion of people aged 56 or older without a BCG scar had received oral BCG, this would artificially decrease the estimated effect of BCG scar in the older group.
A second potential vulnerability in case-control studies is selection bias, which is introduced when the selection of cases is influenced by exposure status. In this study, this would have been introduced if knowledge of BCG vaccination influenced whether a subject was selected as a case or a control. Classification into case or control followed a rigorous objective criteria based on measurable clinical and laboratory data as cases and controls were enrolled at the hospital emergency room/admission, so selection bias is unlikely. Data related to COVID-19 infection was retrieved from medical records available at the hospitals; they were mostly completed independent of enrollment as a case or not in the study. Differences in characteristics associated with COVID-19 severity—age, presence of comorbidity—were very marked between cases and controls as expected from clinical data. This was addressed initially by controlling in the analyses; the efficacy remained high in a sensitivity analysis conducted matching internally closely for age, comorbidity, and city. Residual confounding is not a likely explanation to our findings as the protective effect remained remarkably stable in the sensitivity analysis with cases and controls closely matched by age, co-morbidity, and municipality. Finally, our study did not measure BCG immunological correlates of protection of BCG as none is known.
How to interpret the strong variation in protection with age? We offer four possible explanations. First, the small number of subjects in the older age group. Since intradermal BCG vaccination was introduced in Brazil, the proportion of people over 60 years vaccinated with BCG is small, and thus, the power of the study to detect protection in this age group was limited. Second, the possibility that individuals in that age group considered unvaccinated because they did not have a BCG scar had in fact received oral BCG; this would artificially decrease the measured protection. Third, there is evidence that the duration of immunity conferred by BCG decreases with time [24, 34]. Finally, the severity of COVID-19 increases very markedly in those aged 60 and over, and the effect BCG on preventing progression may interact with the biological mechanism behind the effect of age on COVID-19 severity.
Although a number of studies of BCG preventing clinical progression of symptomatic COVID-19 to severe COVID-19 were conducted, with varying results, this is by far the largest conducted with original data. Our results are broadly consistent with two other large studies examining the effect of previous BCG on clinical progression. The first, conducted by Weng, followed a cohort of 120 COVID-19 patients, predominantly of Hispanic origin, in the USA. The study was completed before COVID-19 vaccine was introduced, so study participants were unvaccinated [18]. Eighty-two participants (68.3%) had a previous BCG vaccination. Individuals with BCG vaccination were less likely to require hospital admission during the disease course (3.7% vs. 15.8%, P = 0.019), after adjusting for demographics and comorbidities. This corresponds to a protection of 76% against clinical progression to severity (our calculation). The second, conducted by Sinha [35] is a multi-centre quadruple-blind, parallel assignment randomised control trial. It was found as a secondary outcome that significantly more patients in the placebo group (who did not receive BCG) progressed to severe COVID-19 pneumonia and required hospitalisation and oxygen [35]. These results suggest that BCG protection against clinical progression is so similar in these 3 studies, given that two estimated the effect of previous BCG and the third had BCG as a recent intervention.
While the mechanism of BCG vaccine-related reductions in non-specific morbidity and mortality is poorly understood, there are several postulated explanations. First is trained immunity, where BCG vaccination induces epigenetic reprogramming of monocytes through histone modifications in regulatory elements of specific genes, resulting in increased cytokine production following subsequent exposure to pathogens [36]. Second, in addition to this innate immune mechanism, an adaptive immune response through cross-reactivity and bystander activation of T cells may have a role. Cross-reactivity involves a reaction to a different antigen with amino acid similarity (BCG contains similar 9-amino acid sequences with SARS-CoV-2) [37], while a bystander response occurs via a neighbouring, unrelated T cell with a different specificity to the one using involved. Although the exact duration of protection based on either mechanism is not known, strong production of Th1 and Th17 immune response to non-mycobacterial antigens in trained immunity [38] and a specific BCG-associated DNA methylation signature involved in viral response pathways have been reported for over a year after BCG vaccination. Cellular immunity is an important determinant of COVID-19 disease outcomes and infections caused by coronavirus infections more broadly [39]. Indeed, multiple COVID-19 vaccines and prior infection by SARS-CoV-2 variants provide protection against severe outcomes following subsequent exposure. There is evidence of virus-specific cellular responses without virus-specific antibodies suggesting that in some individuals [40, 41], an infection may be cleared by the cellular immune system before it is fully established. Consequently, it is plausible that the non-specific effects of BCG vaccination may also have a role in initial protection and the subsequent clinical course of COVID-19.
Conclusions
In conclusion, our results suggest a protective effect of the BCG vaccine against progression to severe COVID-19 in people who did not receive COVID-19 vaccines. This confirms the findings of the two other large studies. More studies to be conducted in different epidemiological scenarios are needed to confirm or rule out this specific strong association. In addition to the protective effect against clinical progression, relevant research questions should explore whether the time elapsed since BCG vaccination and age at BCG vaccination affect protection and whether this explains the lack of protection in older people in our study. It would also be interesting to investigate if the same protection is present in people who received COVID-19 vaccines. We reiterate the importance of discriminating studies that estimate the protection of BCG vaccination against infection with COVID-19, symptomatic COVID-19, clinical progression to severity, and severe disease. We hope that the specificity of the finding (protection against progression) might inform the immunological study of non-specific effects of BCG and the mechanisms behind the marked increase in the severity of COVID-19 in the elderly.
In our view, it is too soon to recommend BCG vaccination to help prevent severe COVID-19, but if protection is confirmed, it may be an alternative, particularly in settings with low COVID-19 vaccine coverage. Our findings may also have implications for research to identify vaccine candidates for COVID-19 that are broadly protective against mortality from future variants. Future work to understand the immunomodulatory effects of BCG may also inform therapeutic research.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author (florisneide@gmail.com) upon reasonable request.
Abbreviations
- BCG:
-
Bacillus Calmette-Guérin
- CI:
-
Confidence interval
- O2:
-
Oxygen
- OR:
-
Odds ratio
- RT-PCR:
-
Reverse transcriptase polymerase chain reaction
- SRAG:
-
Severe acute respiratory syndrome
References
Guallar-Garrido S, Julián E. Bacillus Calmette-Guérin (BCG) therapy for bladder cancer: an update. ImmunoTargets Ther. 2020;9:1–11.
Moorlag SJCFM, Arts RJW, van Crevel R, Netea MG. Non-specific effects of BCG vaccine on viral infections. Clin Microbiol Infect. 2019;25:1473–8.
Aaby P, Roth A, Ravn H, Napirna BM, Rodrigues A, Lisse IM, et al. Randomized trial of BCG vaccination at birth to low-birth-weight children: beneficial nonspecific effects in the neonatal period? J Infect Dis. 2011;204:245–52.
Prentice S, Nassanga B, Webb EL, Akello F, Kiwudhu F, Akurut H, et al. BCG-induced non-specific effects on heterologous infectious disease in Ugandan neonates: an investigator-blind randomised controlled trial. Lancet Infect Dis. 2021;21:993–1003.
Biering-Sørensen S, Aaby P, Napirna BM, Roth A, Ravn H, Rodrigues A, et al. Small randomized trial among low-birth-weight children receiving bacillus Calmette-Guérin vaccination at first health center contact. Pediatr Infect Dis J. 2012;31:306–8.
Stensballe LG, Nante E, Jensen IP, Kofoed P-E, Poulsen A, Jensen H, et al. Acute lower respiratory tract infections and respiratory syncytial virus in infants in Guinea-Bissau: a beneficial effect of BCG vaccination for girls community based case-control study. Vaccine. 2005;23:1251–7.
Ferluga J, Yasmin H, Al-Ahdal MN, Bhakta S, Kishore U. Natural and trained innate immunity against Mycobacterium tuberculosis. Immunobiology. 2020;225: 151951.
Bannister S, Kim B, Domínguez-Andrés J, Kilic G, Ansell BRE, Neeland MR, et al. Neonatal BCG vaccination is associated with a long-term DNA methylation signature in circulating monocytes. Sci Adv. 2022;8:eabn4002.
Escobar LE, Molina-Cruz A, Barillas-Mury C. BCG vaccine protection from severe coronavirus disease 2019 (COVID-19). Proc Natl Acad Sci U S A. 2020;117:17720–6.
Berg MK, Yu Q, Salvador CE, Melani I, Kitayama S. Mandated Bacillus Calmette-Guérin (BCG) vaccination predicts flattened curves for the spread of COVID-19. Sci Adv. 2020;6:eabc1463.
Urashima M, Otani K, Hasegawa Y, Akutsu T. BCG vaccination and mortality of COVID-19 across 173 countries: an ecological study. Int J Environ Res Public Health. 2020;17(15):5589.
Wassenaar TM, Buzard GS, Newman DJ. BCG vaccination early in life does not improve COVID-19 outcome of elderly populations, based on nationally reported data. Lett Appl Microbiol. 2020;71:498–505.
Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, Otazu GH. Correlation between universal BCG vaccination policy and reduced mortality for COVID-19. medRxiv. 2020. https://doi.org/10.1101/2020.03.24.20042937.
Pépin J, Labbé A-C, Carignan A, Parent M-E, Yu J, Grenier C, et al. Does BCG provide long-term protection against SARS-CoV-2 infection? a case-control study in Quebec. Canada Vaccine. 2021. https://doi.org/10.1016/j.vaccine.2021.08.019.
Rivas MN, Ebinger JE, Wu M, Sun N, Braun J, Sobhani K, et al. BCG vaccination history associates with decreased SARS-CoV-2 seroprevalence across a diverse cohort of health care workers. J Clin Invest. 2021;131(2):e145157.
Patella V, Sanduzzi A, Bruzzese D, Florio G, Brancaccio R, Fabbrocini G, et al. A survey among Italian physicians during COVID-19 outbreak. could Bacillus Calmette–Guérin vaccine be effective against SARS-CoV2? Front Pharmacol. 2021;12:646570.
Liu S, Yuan C, Lin J, Gao W, Tian D, Cai X, et al. Association between vaccinations and clinical manifestations in children with COVID-19. Transl Pediatr. 2021;10:17–25.
Weng CH, Saal A, Butt WW, Bica N, Fisher JQ, Tao J, et al. Bacillus Calmette-Guérin vaccination and clinical characteristics and outcomes of COVID-19 in Rhode Island, United States: a cohort study. Epidemiol Infect. 2020;148:e140.
Hamiel U, Kozer E, Youngster I. SARS-CoV-2 rates in BCG-vaccinated and unvaccinated young adults. JAMA. 2020;323:2340–1.
Upton CM, van Wijk RC, Mockeliunas L, Simonsson USH, McHarry K, van den Hoogen G, et al. Safety and efficacy of BCG re-vaccination in relation to COVID-19 morbidity in healthcare workers: a double-blind, randomised, controlled, phase 3 trial. eClinicalMedicine. 2022;48:101414.
Tsilika M, Taks E, Dolianitis K, Kotsaki A, Leventogiannis K, Damoulari C, et al. ACTIVATE-2: a double-blind randomized trial of BCG vaccination against COVID-19 in individuals at risk. Front Immunol. 2022;13: 873067.
Bates MN, Herron TJ, Lwi SJ, Baldo JV. BCG vaccination at birth and COVID-19: a case-control study among U.S. military Veterans. Hum Vaccin Immunother. 2022;18:1981084.
Roy A, Eisenhut M, Harris RJ, Rodrigues LC, Sridhar S, Habermann S, et al. Effect of BCG vaccination against Mycobacterium tuberculosis infection in children: systematic review and meta-analysis. BMJ. 2014;349:4643.
Abubakar I, Pimpin L, Ariti C, Beynon R, Mangtani P, Sterne JAC, et al. Systematic review and meta-analysis of the current evidence on the duration of protection by bacillus Calmette-Guérin vaccination against tuberculosis. Health Technol Assess. 2013;17(1–372):v–vi.
Mangtani P, Abubakar I, Ariti C, Beynon R, Pimpin L, Fine PEM, et al. Protection by BCG vaccine against tuberculosis: a systematic review of randomized controlled trials. Clin Infect Dis an Off Publ Infect Dis Soc Am. 2014;58:470–80.
Lee M-H, Kim B-J. COVID-19 vaccine development based on recombinant viral and bacterial vector systems: combinatorial effect of adaptive and trained immunity. J Microbiol. 2022;60:321–34.
Aspatwar A, Gong W, Wang S, Wu X, Parkkila S. Tuberculosis vaccine BCG: the magical effect of the old vaccine in the fight against the COVID-19 pandemic. Int Rev Immunol. 2022;41:283–96.
Ziogas A, Netea MG. Trained immunity-related vaccines: innate immune memory and heterologous protection against infections. Trends Mol Med. 2022;28:497–512.
Brasil. Ministério da Saúde. Secretaria de Atenção Especializada à Saúde. Departamento de Atenção Hospitalar D e de U. Protocolo de Manejo Clínico da Covid-19. 2020;1:1–48.
Rossiter CE, Schlesselman JJ. Case-control studies. design, conduct, analysis. Biometrics. 1983;39.
Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;19(6):716–23.
Pereira SM, Bierrenbach AL, Dourado I, Barreto ML, Yury Ichihara M, Hijjar MA, et al. Sensibility and specificity of the BCG scar reading. Rev Saude Publica. 2003;37:254–9.
Giesecke J. Modern infectious disease epidemiology: third edition. CRC Press; 2017.
Nguipdop-Djomo P, Heldal E, Rodrigues LC, Abubakar I, Mangtani P. Duration of BCG protection against tuberculosis and change in effectiveness with time since vaccination in Norway: a retrospective population-based cohort study. Lancet Infect Dis. 2016;16:219–26.
Sinha S, Ajayababu A, Thukral H, Gupta S, Guha SK, Basu A, et al. Efficacy of Bacillus Calmette-Guérin (BCG) vaccination in reducing the incidence and severity of COVID-19 in high-risk population (BRIC): a phase III, multi-centre, quadruple-blind randomised control trial. Infect Dis Ther. 2022;11:2205–17.
Netea MG, Quintin J, van der Meer JWM. Trained immunity: a memory for innate host defense. Cell Host Microbe. 2011;9:355–61.
Frankild S, de Boer RJ, Lund O, Nielsen M, Kesmir C. Amino acid similarity accounts for T cell cross-reactivity and for “holes” in the T cell repertoire. PLoS One. 2008;3: e1831.
Kleinnijenhuis J, Quintin J, Preijers F, Benn CS, Joosten LAB, Jacobs C, et al. Long-lasting effects of BCG vaccination on both heterologous Th1/Th17 responses and innate trained immunity. J Innate Immun. 2014;6:152–8.
Moss P. The T cell immune response against SARS-CoV-2. Nat Immunol. 2022;23:186–93.
Sekine T, Perez-Potti A, Rivera-Ballesteros O, Strålin K, Gorin J-B, Olsson A, et al. Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19. Cell. 2020;183:158-168.e14.
Nelde A, Bilich T, Heitmann JS, Maringer Y, Salih HR, Roerden M, et al. SARS-CoV-2-derived peptides define heterologous and COVID-19-induced T cell recognition. Nat Immunol. 2021;22:74–85.
Acknowledgements
The authors thank the following institutions: Institute Couto Maia, Municipal Health Department of Camaçari, Bahia; Institute of Infectology Emílio Ribas-SES-SP, São Paulo, SP, Brazil; and Federal University of Pernambuco, Medical Sciences Center, Postgraduate in Tropical Medicine – Recife (PE), Brazil, who contributed with the project, allowing the team access to data and/or the institution’s facilities, thus enabling data collection.
We are grateful to all patients, health workers, and interviewers that participated or contributed to the study.
Funding
This research was supported by funding by Conselho Nacional de Desenvolvimento Científico e Tecnológico/National Council for Scientific and Technological Development-CNPq, Ministério da Ciência, Tecnologia e Inovações (MCTI)/Ministry of Science, Technology and Innovations, Grant numbers: 401624/2020-0.
Author information
Authors and Affiliations
Contributions
SMP, FRB, CATS, MP, ESP, MSN, JMP, CN, MYI, MD, AT, MB-N, MLB, RAAX, and LCR conceptualised the study. SMP, FRB, ESP, AT, MB-N, IA, MLB, RAAX, and LCR wrote the manuscript. SMP, FRB, RAS, CATS, MLB, RAAX, and LCR performed the statistical analysis. SMP, FRB, RAS, CAST, MP, ESP, CCOJL, MSN, AABPL, EGF, EBCJ, JMP, KVFA, FMS, EAB, CN, MYI, MD, AT, MB-N, IA, MLB, RAAX, and LCR interpreted the data and revised the manuscript critically. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This project was approved by the Ethics Committee of the Institute of Collective Health (ISC), Federal University of Bahia, Brazil (Registration number 4,067,252) and by the Ethics Committee of the Universidade Federal de Pernambuco (Registration number 5,509,828).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pereira, S.M., Barreto, F.R., de Souza, R.A. et al. Previous BCG vaccination is associated with less severe clinical progression of COVID-19. BMC Med 21, 145 (2023). https://doi.org/10.1186/s12916-023-02859-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-023-02859-x