Abstract
Background:
The development and use of human embryonic stem cells (hESCs) in regenerative medicine have been revolutionary, offering significant advancements in treating various diseases. These pluripotent cells, derived from early human embryos, are central to modern biomedical research. However, their application is mired in ethical and regulatory complexities related to the use of human embryos.
Method:
This review utilized key databases such as ClinicalTrials.gov, EU Clinical Trials Register, PubMed, and Google Scholar to gather recent clinical trials and studies involving hESCs. The focus was on their clinical application in regenerative medicine, emphasizing clinical trials and research directly involving hESCs.
Results:
Preclinical studies and clinical trials in various areas like ophthalmology, neurology, endocrinology, and reproductive medicine have demonstrated the versatility of hESCs in regenerative medicine. These studies underscore the potential of hESCs in treating a wide array of conditions. However, the field faces ethical and regulatory challenges, with significant variations in policies and perspectives across different countries.
Conclusion:
The potential of hESCs in regenerative medicine is immense, offering new avenues for treating previously incurable diseases. However, navigating the ethical, legal, and regulatory landscapes is crucial for the continued advancement and responsible application of hESC research in the medical field. Considering both scientific potential and ethical implications, a balanced approach is essential for successfully integrating hESCs into clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The field of stem cell research has undergone a significant transformation with the advent of human embryonic stem cells (hESCs). Since their pioneering isolation in 1998, hESCs have been at the forefront of scientific inquiry due to their unique ability for self-renewal and pluripotency [1, 2]. This comprehensive review article delves into the advancements, challenges, and ethical considerations surrounding hESCs and their implications for regenerative medicine.
Over the past two decades, the potential of hESCs to revolutionize the treatment of various diseases has been increasingly recognized [3, 4]. Their capacity to differentiate into diverse cell types offers promising prospects for repairing or replacing damaged tissues, especially in conditions where current treatments are limited [5,6,7,8]. However, the journey of hESC research is not without its complexities. Ethical considerations regarding the use of human embryos have sparked intense debates and have had a profound impact on public perception and the regulatory framework governing hESC research [9, 10].
The therapeutic applications of hESCs encompass both systemic and localized approaches, including intravenous or intramuscular injections and surgical implantation, sometimes combined with bioscaffolds [11]. These strategies are broadly classified into transient dosing for temporary therapeutic effects and permanent implantation for long-term tissue repair and regeneration [12, 13]. Despite these advancements, challenges in ensuring consistency in hESC properties across different experimental settings continue to pose hurdles in translating laboratory findings into clinical therapies [14, 15].
While induced pluripotent stem cells (iPSCs) have emerged as an alternative, hESCs still hold distinct advantages, particularly in the understanding of genetic diseases and human development [16, 17]. Despite the ethical complexities and slower pace of clinical research compared to iPSCs, hESCs remain a crucial tool in biomedical research [18, 19]. Their unique position in providing insights into early human development and genetic disorders underscores their invaluable role in medical science [17].
This review aims to provide an in-depth analysis of the current state of clinical trials involving hESCs, emphasizing their role in regenerative medicine. We explore the evolving landscape of hESC research, highlighting the need for ongoing scientific exploration, ethical deliberation, and regulatory guidance to fully realize the therapeutic potential of hESCs in improving patient care and advancing medical science.
2 Methodology
This narrative review was conducted to assess the clinical applications of hESCs. The primary aim was to gather and analyze data from various sources to understand the current state and advancements in hESC research.
For database search, we utilized ClinicalTrials.gov (https://clinicaltrials.gov/) and EU Clinical Trials Register (https://www.clinicaltrialsregister.eu/) for identifying ongoing and completed clinical trials involving hESCs. Also, we used PubMed and Google Scholar to retrieve published clinical trial reports and peer-reviewed articles on hESCs. Studies and trials were included based on their focus on the clinical application of hESCs. Those not directly involving hESCs or outside the scope of clinical application were excluded. The review primarily targeted articles and trials published or conducted in the last five years to maintain contemporary relevance.
For data extraction and analysis, key information extracted included the study title, indication, participant number, study site, study period, study design, and NCT number. This data was organized systematically to provide a clear overview of the current trends and progress in the field of hESC research in clinical applications.
2.1 Overview of clinical trials in hESC research
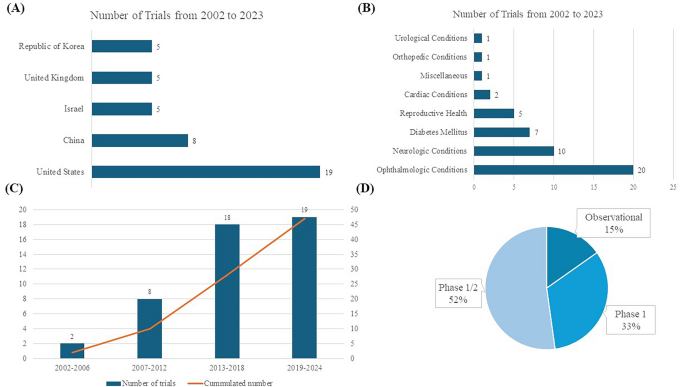
Figure 1 displays key aspects of hESC clinical trials included in this review. The first clinical trial registration was in 2002, and the largest number of registered trials were in the United States (19, 40.4%), followed by China (8, 17.0%; Fig. 1A). By disease category, the largest number of trials were related to ophthalmologic conditions (20, 42.6%), followed by neurologic conditions (10, 21.3%), and clinical studies were mainly conducted on diabetes mellitus (7, 14.9%; Fig. 1B). Figure 1C shows the number of trial registrations and the cumulative number of clinical studies by year. There has been a sharp increase since 2012. (Fig. 1C), and by study design, phase 1 or phase 1/2 designs predominate, accounting for 88% (Fig. 1D). When looking at studies by a specific disease, dry age-related macular degeneration (AMD) is the most common with 8 (18.2%), followed by type 1 diabetes mellitus (T1DM, 7, 15.9%) and Stargardt Macular Dystrophy (SMD, 5, 11.4%).
2.2 Disease-specific analysis
2.2.1 Ophthalmologic diseases
Retinal degeneration is a significant ophthalmologic disease that affects the eye and vision, including dry AMD, SMD, wet AMD, retinitis pigmentosa (RP), diabetic retinopathy, and myopic macular degeneration, among others [20,21,22]. These conditions often lead to severe vision impairment or blindness. Traditional treatments primarily focus on slowing the progression of these diseases but generally fall short of providing substantial visual improvement. For instance, while laser therapy is beneficial in the early stages, there is no established treatment for late-stage dry AMD [23]. In cases of wet AMD, therapies such as anti-VEGF can be administered through intravitreal infusion (e.g., ranibizumab, bevacizumab, aflibercept, and brolucizumab), yet this disease requires continuous treatment and monitoring due to its chronic nature [24,25,26,27]. Stem cell therapy, particularly involving retinal pigment epithelium (RPE) degeneration, has emerged as a promising approach in eye diseases [28]. The RPE is vital for maintaining photoreceptor health and is tasked with recycling photopigments and clearing shed photoreceptor segments [29]. hESCs have shown significant potential in rescuing photoreceptors and enhancing vision in preclinical macular degeneration models [30]. One of the initial forays into stem cell therapy using hESCs was directed at treating dry AMD using hESC-derived RPE. Several key factors contributed to this early focus on retinal conditions. Primarily, the unique immune privilege of the eye, reinforced by the blood-ocular barrier, significantly lowers the risk of rejection of transplanted cells—a crucial aspect in the success of any stem cell-based therapy [31, 32]. Moreover, the eye's transparency permits the non-invasive tracking of the introduced cells through methods like optical coherence tomography or microperimetry, enabling continuous monitoring and evaluation of the therapy's effectiveness [33]. The eye's distinct and isolated structure also minimizes the spread of these cells to other body parts, thereby reducing the likelihood of unintended systemic effects [34]. Furthermore, the absence of synaptic layers in retinal cells aids in their smoother integration [29]. Lastly, the irreversible progression of many retinal disorders and the absence of adequate existing treatments have necessitated the development of innovative therapeutic strategies, thereby placing retinal ailments at the forefront of hESC research and application.
Dry AMD, a prevalent and progressive ophthalmologic disease affecting elderly patients, is characterized by the degeneration of the RPE layer and impairment of central vision [21]. The pivotal role of RPE in the pathophysiology of dry AMD makes it a prime target for therapeutic interventions. The potential of stem cells, especially hESCs, in this context, lies in their ability to differentiate into RPE cells, thereby offering the possibility of replacing damaged or degenerated RPE with healthy, functional cells. Preclinical studies in animal models and in vitro experiments have provided substantial evidence supporting the role of stem cells, including hESCs, in treating dry AMD [35,36,37].
For example, in Yucatan minipigs, a preclinical study assessed CPCB-RPE1, a hESC-derived retinal pigment epithelium monolayer [35]. The study successfully placed CPCB-RPE1 implants in the subretinal space without breakage, and histological analysis confirmed the survival of hESC-RPE cells as an intact monolayer for one month [35]. Another study used differentiated hESC-RPE replacement therapy on albino rabbit eyes induced with NaIO3, employing a 25-gauge transvitreal pars plana vitrectomy (PPV) technique [36]. Xeno-free hESC-RPE monolayer on a polyester substrate survived and retained functionality for up to four weeks with short-term immunosuppression in a rabbit dry AMD model [37]. These studies demonstrate the feasibility of generating RPE cells from stem cells and their potential to integrate into the retina, potentially restoring RPE function and rescuing photoreceptors. Also, the critical advantage of hESC-RPE is their reduced risk of uncontrolled proliferation, as they are fully differentiated.
Clinical trials have been conducted to test the safety and feasibility of hESC-derived RPE for dry AMD, as outlined in Table 1. Dry AMD has been the subject of the most significant number of clinical trials, with studies dating back to 2011 (Table 1). The first study involved MA09-hRPE (NCT01344993; NCT01674829; NCT02122159), derived from the MA09 hESC line, a xenograft product with ex vivo exposure to mouse embryonic cells [38]. Produced by isolating RPE patches when embryoid body formation was confirmed, this treatment was tested in three different dose cohorts (50,000, 100,000, and 150,000 cells) for patients with dry AMD and SMD [39]. Encouragingly, the study revealed no signs of adverse events like cell proliferation or immune rejection. In addition, the best-corrected visual acuity improved in 10 eyes, and measures related to vision-related quality of life showed enhancements [39]. In a clinical trial of MA09-hESC-derived RPE cells conducted with an Asian population, which included four participants, there was no evidence of adverse proliferation or tumorigenesis [40]. Furthermore, one patient experienced improved visual acuity, while the remaining three maintained stable visual acuity throughout the trial [40]. In the USA, a phase 1/2 clinical study was conducted using CPCB-RPE1, a composite implant consisting of a synthetic parylene substrate and a polarized monolayer of adherent hESC-RPE cells (NCT02590692). This study demonstrated safety and tolerability in legally blind patients with dry AMD [41, 42]. However, graft survival remains a significant challenge, influenced by factors like aging of Bruch's membrane, subretinal scarring, para-inflammation, and choroid ischemia [33].
SMD, a prevalent retinal dystrophy affecting young individuals, is characterized by progressive vision loss, primarily caused by mutations in the ABCA4 gene, which leads to dysfunction of the ABCR protein expressed in retinal photoreceptors [43]. Currently, there are no established treatments to effectively improve vision in SMD, similar to the situation in dry AMD. Promising outcomes have been observed in preclinical models, including the safe subretinal injection of retinal pigment epithelium (RPE) derived from hESC. This approach was tested in a phase 1 clinical trial in the USA (NCT02941991). The WA-099 hESC line demonstrated the ability to spontaneously differentiate into RPE cells, with subsequent isolation of pigmentation cells. A suspension of these hESC-derived RPE cells, containing 1.0 × 10^6 cells in 0.1 mL, was surgically implanted subretinally in all eyes using a pars plana vitrectomy (PPV) approach [44]. The study's findings indicated no adverse events during the one-year postoperative follow-up period. Additionally, the treated eyes had no significant improvement in visual acuity [44]. In China, researchers Li et al. evaluated the Q-CTS-hESC-2 cell line-derived RPE in a 5-year follow-up study on seven patients and reported no significant adverse reactions and some temporary improvements in visual function, though two patients showed a long-term decrease in vision (NCT02749734) [45]. Sung et al., from the Republic of Korea, reported a 3-year study on Asian patients, also finding no serious adverse events and reporting stable or improved BCVA in some patients (NCT01625559) [46].
RP is a group of inherited retinal disorders characterized by the progression of vision loss due to photoreceptor degeneration, affecting approximately 1 in 4,000 individuals worldwide [47, 48]. A Phase 1/2 clinical trial of RP with monogenic mutations is ongoing (NCT03963154), with interim analysis showing no adverse events in seven patients [49]. While these studies confirm the long-term safety and tolerability of hESC-RPE cell transplantation, they also highlight the need for further research to improve efficacy, including better patient selection and treatment methodologies, as significant and consistent improvements in visual function are yet to be established.
2.2.2 Neurologic diseases
The utilization of stem cell therapy derived from hESCs in treating neurological disorders is an emerging and promising area of research. As illustrated in Fig. 1B, neurologic diseases are among the most researched applications in this field. This branch of medical science addresses a diverse spectrum of neurological conditions, including Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), spinal cord injuries (SCI), and multiple sclerosis. These disorders present considerable treatment challenges, largely due to the complexity of the nervous system and the typically permanent nature of neuronal damage involved. Ongoing studies are displayed in Table 2.
The first-in-patient clinical trial on neurologic disease was conducted on SCI patients [50]. Oligodendrocyte progenitor cells (LCTOPC1), which are also nomenclature as AST-OPC1 or GRNOPC1, is the world's first hESC-derived therapy, and the phase 1 trial was approved by US-FDA in 2009, and the first patient was enrolled in 2011 (NCT01217008) [50, 51]. Recent 10-year follow-up study results on five participants who received intraparenchymal injections of LCTOPC1 showed no serious adverse effects during follow-up, with 80% of patients showing MRI evidence of tissue matrix formation at the injury site [51]. This pivotal study, leading to a subsequent cervical dose escalation trial (NCT02302157), demonstrated the safety of hESC-derived therapies using LCTOPC1. In the trial, 25 participants with C4-7 spinal injuries received a single dose of 2, 10, or 20 million LCTOPC1 cells and low-dose tacrolimus for 60 days [52]. Despite some adverse events, including 29 serious ones, the treatment was well tolerated, with MRI scans showing no significant complications, and at a 1-year follow-up, 96% of participants improved by at least one level of neurological function, and 32% improved by two or more levels [52].
Additionally, research has shown that neural precursor cells marked by polysialic acid-neural cell adhesion molecule (PSA-NCAM), derived from hESC, can enhance neural tissue integrity in a rat stroke model [53]. Building on these findings, a phase 1/2a clinical trial (NCT04812431) is currently underway to assess the safety and efficacy of PSA-NCAM( +)-NPC for patients with sub-acute C4-C7 level spinal cord injuries. In this trial, the cells will be delivered intrathecally across five sites, and participants will be monitored for one year and five months as part of a follow-up study.
PD is a neurodegenerative disease characterized primarily by the loss of dopaminergic neurons in the substantia nigra, a region of the brain integral to controlling body movement. This loss leads to the classic symptoms of PD, including tremors, rigidity, bradykinesia, and postural instability [54]. The potential of hESC-based therapies in PD lies in their ability to differentiate into dopaminergic neurons, the type of cell lost in the disease [55]. The goal of transplanting hESC-derived cells in PD treatment is to replace the depleted neurons and normalize dopamine levels in the brain, which could help alleviate PD symptoms. MSK-DA01, a midbrain dopamine neuron cell derived from hESCs, is currently undergoing a Phase 1 trial in the United States (NCT04802733). A preclinical study on MSK-DA01 demonstrated successful graft survival and improved behavior in rats with 6-hydroxydopamine-induced lesions, a model for PD. Importantly, these studies revealed no adverse effects related to the graft cells and no unexpected cell proliferation outside the brain, indicating a promising safety profile for this innovative therapy [56].
STEM-PD, another product consisting of dopaminergic neuronal progenitor cells derived from hESCs, has also been evaluated in a preclinical study [57]. This study showed the precise stereotactic injection of STEM-PD into a pig model and demonstrated effective innervation of the targeted brain regions. Additionally, this intervention led to a reversal of motor deficits in the pig model of Parkinson's disease, demonstrating the potential efficacy of STEM-PD in addressing the symptoms associated with this neurodegenerative disorder [57]. Presently, STEM-PD is the subject of a phase 1 clinical trial in the United Kingdom, which is in the process of recruiting eight patients, and this trial marks a significant step in evaluating the safety and potential efficacy of STEM-PD in human subjects, specifically targeting the treatment of PD (NCT05635409).
A research team in China successfully derived dopaminergic neurons from hESCs and demonstrated sustained behavioral improvements over two years in a monkey model of PD [58]. This significant advancement in stem cell research has led to the registration of a Phase 1 clinical trial (NCT03119636). However, the current status of this trial remains unknown.
ALS, a severe neurodegenerative condition, is characterized by the deterioration of both upper and lower motor neurons (MNs), resulting in the progressive paralysis of muscles controlled by these neurons [59]. While FDA-approved treatments like riluzole have demonstrated some efficacy in prolonging survival, there remains a significant unmet need for more effective ALS therapies [60]. Recent evidence points to the involvement of astrocytes in the pathogenesis of ALS [61]. AstroRx®, a novel cell therapy derived from hESCs, has shown promise in addressing this gap, as evidenced by the outcomes of its recent Phase 1/2a clinical trial [62]. AstroRx®, administered as a single intrathecal injection, was tested in two cohorts of ALS patients—a low-dose and a high-dose group, each consisting of five patients (NCT03482050). The administration of AstroRx® showed a clinically significant impact lasting for three months post-treatment, with particularly notable effects observed in a group of rapid progressors [62].
NR1, an hESC-derived neural stem cell, is under investigation for chronic ischemic stroke patients who are 6–60 months post-ischemic subcortical mid-cerebral artery stroke (NCT04631406). Six patients underwent transplantation with NR1, and there was a notable improvement in the Mugl-Meyer motor score. Additionally, all six patients exhibited a transient flair signal that resolved within two months, which correlated with neurological recovery [63].
2.2.3 Diabetes mellitus
Type 1 Diabetes Mellitus (T1DM) commonly manifests in childhood and adolescence and is marked by a chronic autoimmune condition leading to the loss of insulin-producing beta cells in the pancreas [64]. Unlike Type 2 DM, which often relates to lifestyle and insulin resistance, T1DM is primarily driven by an autoimmune response [64]. In stem cell therapy for T1DM, two main strategies have emerged: one involves replacing the missing insulin-producing beta cells, while the other focuses on immunomodulation to safeguard existing beta cells from further autoimmune destruction [65]. Seven registered clinical trials for stem cell-based treatment of T1DM using hESC are summarized in Table 3.
Schulz and colleagues described the creation of the VC-01 composite product utilizing pancreatic endoderm cells (PEC-01) obtained from CyT49 hESCs with a retrievable semi-permeable encapsulating device drug delivery system [66]. VC-02, developed in 2017, is an advanced model featuring multiple large pores across the membrane to facilitate vascularization while maintaining immune isolation [67]. VC-01 was investigated in phase 1/2 trial (NCT02239354; NCT04678557; NCT02939118) and VC-02 was investigated in phase 1/2 trial (NCT03163511). In the phase 1/2 study of the VC-01 product, immunosuppressants were not administered, leading to a host reaction against the implant, ultimately resulting in its destruction, and the study was terminated [68]. A Phase 1/2 study involving 17 patients with T1DM was carried out following a modification in the VC-02 device. This study demonstrated successful engraftment and insulin release in 63% of the cases, and as early as six months post-implantation, 35.3% of the participants showed positive C-peptide levels. These results indicate the potential of VC-02 as a viable alternative for T1DM treatment. However, it's important to note that some reported adverse events were primarily related to the surgical procedures of implanting or explanting the device and the side effects of immunosuppression therapy [69]. VCTX210A represents an innovative approach that uses pancreatic endodermal cells (PEC210A) derived from hESC. These cells have been genetically modified using the CRISPR/Cas9 (Clustered Regularly Interspaced Short Palindromic Repeats/CRISPR-associated protein 9) technology. This modification enhances the cells' survival against the patient's immune system, thereby addressing the challenge of graft versus host disease [70]. Additionally, VX880, a fully differentiated pancreatic islet cell product derived from hESC designed to treat T1DM, is undergoing clinical investigation (NCT04786262). Interim data analysis from this study has yielded positive results, indicating that the treatment successfully restored insulin production in the first two patients enrolled in the trial [71].
2.2.4 Female reproductive organ and genitourinary disease
The field of female reproductive organ disorders is increasingly looking towards stem cell therapy and cutting-edge biomedical technologies for potential treatments, as shown in Table 4. Intravenous injection of hESC-derived mesenchymal cells (hESC-MCs) showed restoration of ovarian function induced by the chemotherapeutic agent in a murine model [72, 73]. A product, hESC-MC, has been explored by a Chinese research group for treating moderate to severe intrauterine adhesion (NCT04232592). Additionally, a therapy involving hESC-MC product is currently being investigated as a potential treatment for primary ovarian insufficiency (NCT03877471). Additionally, Table 5 showcases the application of hESC-derived mesenchymal stem cell therapy, specifically MR-MVC-01, which is currently under investigation for treating interstitial cystitis, as per the clinical trial registered under NCT04610359.
2.2.5 Cardiovascular disease
In the field of heart failure treatment, the innovative application of human embryonic stem cells (hESCs) offers a promising alternative to conventional therapies. Table 5 also highlights hESC-derived cardiac progenitor cell-based products in treating heart failure and ischemic heart disease, as illustrated in the clinical trials registered under NCT02057900 and NCT05068674. The ESCORT trial (NCT02057900), conducted in France, marked a pioneering venture in employing hESC-derived cardiomyocytes for heart failure treatment, setting a precedent that has been followed by the HECTOR trial (NCT05068674) in the United States, initiated in 2022. The ESCORT trial, focusing on patients with severe ischemic left ventricular dysfunction, demonstrated the feasibility and safety of using hESC-derived cardiovascular progenitor cells, embedded in a fibrin patch, applied to the damaged heart areas during coronary artery bypass surgery [74]. The results, including the production of a highly purified batch of progenitor cells and significant symptomatic improvements in patients, though with instances of silent alloimmunization, have laid the groundwork for future explorations in this domain. The HECTOR trial in the U.S. is building upon this foundation with a novel approach, utilizing hESC-derived cardiomyocytes (hESC-CMs) to enhance survival and cardiac function in patients with chronic left ventricular dysfunction secondary to myocardial infarction. This phase I dose-escalation pilot study is designed as an initial safety assessment to determine the maximum tolerated dose (MTD) before proceeding to a phase II randomized, double-blinded, placebo-controlled study. Approximately eighteen patients who are scheduled for cardiac catheterization and meet all inclusion/exclusion criteria will participate in this initial phase. The HECTOR trial represents a significant step forward in the application of hESC-CMs in cardiac therapy, with great anticipation for its potential to revolutionize the treatment of heart failure and related conditions.
2.3 Challenges and ethical considerations
As we explore the burgeoning field of hESC research and its clinical applications, it becomes crucial to examine the accompanying ethical and practical challenges thoroughly. While this area of research offers groundbreaking possibilities in treating various diseases, it is intertwined with complex ethical, legal, and social issues, particularly due to the involvement of human embryos.
2.3.1 Derivation of hESC
In the field of hESC research, the ethical implications surrounding the derivation of these cells from embryos are paramount. hESCs are typically harvested from embryos at the blastocyst stage approximately 5–6 days post-fertilization. This stage of development is critical because it leads to the inevitable destruction of the embryo, a primary ethical concern in this field of research [19, 75,76,77].
Due to their pluripotency, the significant potential of hESCs makes them a valuable asset in understanding disease mechanisms, drug testing, and potential regenerative therapies [78]. Moreover, hESCs are obtained early in induced pluripotent development, making them crucial for studying human developmental processes and various diseases [17]. They play a vital role, especially when embryos are discarded after positive preimplantation genetic testing (PGT) results, contributing to our understanding of genetic abnormalities and disease ecology [17].
Regarding the moral status of the embryo, there are varying views. The Catholic perspective often sees life beginning at fertilization, while Judaism and Islam view the blastocyst as having the potential for life but not as fully alive [79, 80]. Hinduism and Buddhism do not provide a clear doctrinal definition of life's beginning, adopting a more philosophical and spiritual perspective [81].
The use of surplus IVF embryos in hESC research is often defended under the principle of proportionality. This approach favors using them for stem cell research due to the broader potential benefits compared to enhancing IVF techniques [17]. The utilization of embryos with monogenic defects (PGT-M) or aneuploidies (PGT-A) for deriving disease-specific stem cells is seen as a promising avenue for advancing the understanding of specific diseases and developing targeted treatments [9, 17].
In summary, hESC research presents a complex ethical landscape. The scientific and medical benefits of hESCs must be balanced against the moral considerations surrounding the use of human embryos, necessitating a nuanced approach to this rapidly evolving field.
2.3.2 Regulatory issues
In the realm of research involving hESCs, regulatory issues play a crucial role, varying significantly across different countries. Obtaining approval from institutional review boards (IRBs) and adhering to regulations set by authoritative bodies are pivotal steps in developing and progressing hESC-related research and development.
Procedures involving the transfer of stem cells are subject to specific regulations. This encompasses the process of transferring stem cell materials, which requires careful adherence to legal and ethical guidelines [15, 82]. It's essential to ensure that the transfer agreements are comprehensive, detailing any restrictions and obligations related to using the materials and associated data [83, 84]. Such transfers must respect donor rights and comply with the regulatory frameworks of both the donating and receiving entities.
The process of creating stem cell products that are safe for clinical use involves several critical steps. This includes extensive testing for genetic stability and absence of contaminants, ensuring the cells' identity and functionality, and verifying that they meet the stringent safety standards required for clinical application [82]. These procedures are designed to safeguard patient safety and ensure the efficacy of the stem cell products.
Overall, the development and research involving hESCs must navigate a complex landscape of regulatory requirements. These regulations are in place to ensure the ethical use of human stem cells, the protection of donor rights, and the safety and efficacy of stem cell-based therapies. Compliance with these regulations is not only a legal requirement but also a cornerstone in maintaining the integrity and credibility of stem cell research.
3 Conclusion
The exploration of hESCs over the past two decades has opened new frontiers in medical science, particularly in the fields of regenerative medicine and cell-based therapies. The landmark discovery and subsequent developments have brought immense potential for understanding and treating a wide range of diseases, from genetic disorders to degenerative conditions.
However, the journey of hESC research is intertwined with a plethora of ethical, legal, and regulatory challenges. The ethical considerations, primarily regarding the use of human embryos, highlight the delicate balance between scientific advancement and moral imperatives. Different religious and cultural perspectives on embryo status underline this debate's complexity. As we have seen, approaches to this issue vary significantly worldwide, influencing the regulatory landscape and research in different countries.
The advancements in hESC research also underscore the importance of robust regulatory frameworks and adherence to ethical standards. From acquiring embryonic materials to developing stem cell-based products for clinical use, each step requires careful consideration of ethical guidelines, safety standards, and regulatory compliance. The involvement of IRBs and adherence to international standards and guidelines are critical in ensuring that the research is conducted responsibly and with the utmost respect for human life and dignity.
Looking ahead, the field of hESC research holds immense promise. With continued technological advancements and a deeper understanding of stem cells' capabilities, we stand on the brink of revolutionary medical breakthroughs. However, the path forward must be navigated with a commitment to ethical principles, regulatory compliance, and public engagement. By upholding these standards, the scientific community can ensure that the benefits of hESC research are realized in a manner that respects human values and contributes positively to human health and well-being.
In conclusion, hESC research represents scientific innovation, ethical reflection, and regulatory prudence. As we continue to advance in this field, it is imperative to maintain a balanced approach that fosters scientific discovery while honoring ethical obligations and regulatory requirements. The future of hESC research, promising as it is, depends on our collective ability to navigate these complex and multifaceted challenges.
Data availability statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–7.
Oh SK, Kim HS, Ahn HJ, Seol HW, Kim YY, Park YB, et al. Derivation and characterization of new human embryonic stem cell lines: SNUhES1, SNUhES2, and SNUhES3. Stem Cells. 2005;23:211–9.
Doğan A. Embryonic stem cells in development and regenerative medicine. Adv Exp Med Biol. 2018;1079:1–15.
Kolios G, Moodley Y. Introduction to stem cells and regenerative medicine. Respiration. 2013;85:3–10.
Jarrige M, Frank E, Herardot E, Martineau S, Darle A, Benabides M, et al. The future of regenerative medicine: cell therapy using pluripotent stem cells and acellular therapies based on extracellular vesicles. Cells. 2021;10:240.
Kidha DK. Human embryonic stem cell research in transplantation and regenerative medicine: a principlist assessment; 2020.
Kim YY, Ku SY, Liu HC, Cho HJ, Oh SK, Moon SY, et al. Cryopreservation of human embryonic stem cells derived-cardiomyocytes induced by BMP2 in serum-free condition. Rep Sci. 2011;18:252–60.
Kim YY, Min H, Kim H, Choi YM, Liu HC, Ku SY. Differential MicroRNA expression profile of human embryonic stem cell-derived cardiac lineage cells. Tissue Eng Regen Med. 2017;14:163–9.
Douglas T, Savulescu J. Destroying unwanted embryos in research. Talking Point on morality and human embryo research. EMBO Rep. 2009;10:307–12.
Fan R. The ethics of human embryonic stem cell research and the of the family. In: Lee SC, editor. The family, medical decision-making, and biotechnology: Critical reflections on Asian moral perspectives. The MIT Press: Springer; 2007. p. 127–48.
Turksen K. Cell biology and translational medicine. vol. 11. Berlin: Springer; 2021.
Singh MS, Park SS, Albini TA, Canto-Soler MV, Klassen H, MacLaren RE, et al. Retinal stem cell transplantation: balancing safety and potential. Prog Retin Eye Res. 2020;75:100779.
Song MJ, Bharti K. Looking into the future: using induced pluripotent stem cells to build two and three dimensional ocular tissue for cell therapy and disease modeling. Brain Res. 2016;1638:2–14.
Lefkopoulos S. Enhancing reproducibility in human stem cell research. Nat Cell Biol. 2023;25:1237–9.
Ludwig TE, Andrews PW, Barbaric I, Benvenisty N, Bhattacharyya A, Crook JM, et al. ISSCR standards for the use of human stem cells in basic research. Stem Cell Rep. 2023;18:1744–52.
Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–72.
Salari S, Adashi EY, Keller L, Johnson TRB, Smith GD. Human embryos donated for human embryonic stem cell derivation. Fertil Steril. 2023;119:3–10.
King NM, Perrin J. Ethical issues in stem cell research and therapy. Stem Cell Res Ther. 2014;5:85.
Banja JD. Ethical considerations in stem cell research on neurologic and orthopedic conditions. PM R. 2015;7:S66-75.
Fleckenstein M, Mitchell P, Freund KB, Sadda S, Holz FG, Brittain C, et al. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125:369–90.
Chakravarthy U, Bailey CC, Johnston RL, McKibbin M, Khan RS, Mahmood S, et al. Characterizing disease burden and progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125:842–9.
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–60.
Guymer RH, Wu Z, Hodgson LAB, Caruso E, Brassington KH, Tindill N, et al. Subthreshold nanosecond laser intervention in age-related macular degeneration: the LEAD randomized controlled clinical trial. Ophthalmology. 2019;126:829–38.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–31.
Rosenfeld PJ, Moshfeghi AA, Puliafito CA. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Lasers Imaging. 2005;36:331–5.
Heier JS, Brown DM, Chong V, Korobelnik JF, Kaiser PK, Nguyen QD, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119:2537–48.
Pearce I, Amoaku W, Bailey C, Downey L, Gale R, Ghanchi F, et al. The changing landscape for the management of patients with neovascular AMD: brolucizumab in clinical practice. Eye (Lond). 2022;36:1725–34.
George SM, Lu F, Rao M, Leach LL, Gross JM. The retinal pigment epithelium: development, injury responses, and regenerative potential in mammalian and non-mammalian systems. Prog Retin Eye Res. 2021;85:100969.
Strauss O. The retinal pigment epithelium in visual function. Physiol Rev. 2005;85:845–81.
Sharma A, Jaganathan BG. Stem cell therapy for retinal degeneration: the evidence to date. Biologics. 2021;15:299–306.
Idelson M, Alper R, Obolensky A, Yachimovich-Cohen N, Rachmilewitz J, Ejzenberg A, et al. Immunological properties of human embryonic stem cell-derived retinal pigment epithelial cells. Stem Cell Rep. 2018;11:681–95.
Yamasaki S, Sugita S, Horiuchi M, Masuda T, Fujii S, Makabe K, et al. Low immunogenicity and immunosuppressive properties of human ESC- and iPSC-derived retinas. Stem Cell Rep. 2021;16:851–67.
Qiu TG. Transplantation of human embryonic stem cell-derived retinal pigment epithelial cells (MA09-hRPE) in macular degeneration. NPJ Regen Med. 2019;4:19.
Tomita M, Lavik E, Klassen H, Zahir T, Langer R, Young MJ. Biodegradable polymer composite grafts promote the survival and differentiation of retinal progenitor cells. Stem Cells. 2005;23:1579–88.
Koss MJ, Falabella P, Stefanini FR, Pfister M, Thomas BB, Kashani AH, et al. Subretinal implantation of a monolayer of human embryonic stem cell-derived retinal pigment epithelium: a feasibility and safety study in Yucatán minipigs. Graefes Arch Clin Exp Ophthalmol. 2016;254:1553–65.
Petrus-Reurer S, Bartuma H, Aronsson M, Westman S, Lanner F, Kvanta A. Subretinal transplantation of human embryonic stem cell derived-retinal pigment epithelial cells into a large-eyed model of geographic atrophy. J Vis Exp. 2018.
Ilmarinen T, Thieltges F, Hongisto H, Juuti-Uusitalo K, Koistinen A, Kaarniranta K, et al. Survival and functionality of xeno-free human embryonic stem cell-derived retinal pigment epithelial cells on polyester substrate after transplantation in rabbits. Acta Ophthalmol. 2019;97:e688–99.
Schwartz SD, Hubschman J-P, Heilwell G, Franco-Cardenas V, Pan CK, Ostrick RM, et al. Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet. 2012;379:713–20.
Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet. 2015;385:509–16.
Song WK, Park KM, Kim HJ, Lee JH, Choi J, Chong SY, et al. Treatment of macular degeneration using embryonic stem cell-derived retinal pigment epithelium: preliminary results in Asian patients. Stem Cell Rep. 2015;4:860–72.
Kashani AH, Lebkowski JS, Rahhal FM, Avery RL, Salehi-Had H, Chen S, et al. One-year follow-up in a phase 1/2a clinical trial of an allogeneic RPE cell bioengineered implant for advanced dry age-related macular degeneration. Transl Vis Sci Technol. 2021;10:13.
Kashani AH, Uang J, Mert M, Rahhal F, Chan C, Avery RL, et al. Surgical method for implantation of a biosynthetic retinal pigment epithelium monolayer for geographic atrophy: experience from a phase 1/2a Study. Ophthalmol Retina. 2020;4:264–73.
Hussain RM, Ciulla TA, Berrocal AM, Gregori NZ, Flynn HW Jr, Lam BL. Stargardt macular dystrophy and evolving therapies. Expert Opin Biol Ther. 2018;18:1049–59.
Brant Fernandes RA, Lojudice FH, Zago Ribeiro L, Santos da Cruz NF, Polizelli MU, Cristovam PC, et al. Transplantation of subretinal stem cell-derived retinal pigment epithelium for Stargardt disease: a phase I clinical trial. Retina. 2023;43:263–74.
Li SY, Liu Y, Wang L, Wang F, Zhao TT, Li QY, et al. A phase I clinical trial of human embryonic stem cell-derived retinal pigment epithelial cells for early-stage Stargardt macular degeneration: 5-years’ follow-up. Cell Prolif. 2021;54:e13100.
Sung Y, Lee MJ, Choi J, Jung SY, Chong SY, Sung JH, et al. Long-term safety and tolerability of subretinal transplantation of embryonic stem cell-derived retinal pigment epithelium in Asian Stargardt disease patients. Br J Ophthalmol. 2021;105:829–37.
Becherucci V, Bacci GM, Marziali E, Sodi A, Bambi F, Caputo R. The new era of therapeutic strategies for the treatment of retinitis pigmentosa: a narrative review of pathomolecular mechanisms for the development of cell-based therapies. Biomedicines. 2023;11:2656.
Lozano B LL, Cervantes A LA. Development of experimental treatments for patients with retinitis pigmentosa. Arch Soc Esp Oftalmol (Engl Ed). 2023;98:646–55.
Monville C, Bertin S, Devisme C, Brazhnikova E, Jaillard C, Walter H, et al. Phase I/II open-label study of implantation into one eye of hESC-derived RPE in patients with retinitis pigmentosa due to monogenic mutation: first safety results. Invest Ophthalmol Vis Sci. 2023;64:3829–929.
Lebkowski J. GRNOPC1: the world’s first embryonic stem cell-derived therapy. Interview with Jane Lebkowski. Regen Med. 2011;6:11–3.
McKenna SL, Ehsanian R, Liu CY, Steinberg GK, Jones L, Lebkowski JS, et al. Ten-year safety of pluripotent stem cell transplantation in acute thoracic spinal cord injury. J Neurosurg Spine. 2022. https://doi.org/10.3171/2021.12.Spine21622
Fessler RG, Ehsanian R, Liu CY, Steinberg GK, Jones L, Lebkowski JS, et al. A phase 1/2a dose-escalation study of oligodendrocyte progenitor cells in individuals with subacute cervical spinal cord injury. J Neurosurg Spine. 2022;37:812–20.
Kim HS, Choi SM, Yang W, Kim DS, Lee DR, Cho SR, et al. PSA-NCAM(+) neural precursor cells from human embryonic stem cells promote neural tissue integrity and behavioral performance in a rat stroke model. Stem Cell Rev Rep. 2014;10:761–71.
Hayes MT. Parkinson’s Disease and Parkinsonism. Am J Med. 2019;132:802–7.
Sonntag KC, Song B, Lee N, Jung JH, Cha Y, Leblanc P, et al. Pluripotent stem cell-based therapy for Parkinson’s disease: current status and future prospects. Prog Neurobiol. 2018;168:1–20.
Piao J, Zabierowski S, Dubose BN, Hill EJ, Navare M, Claros N, et al. Preclinical efficacy and safety of a human embryonic stem cell-derived midbrain dopamine progenitor product, MSK-DA01. Cell Stem Cell. 2021;28:217-29.e7.
Kirkeby A, Nelander J, Hoban DB, Rogelius N, Bjartmarz H, Storm P, et al. Preclinical quality, safety, and efficacy of a human embryonic stem cell-derived product for the treatment of Parkinson’s disease. STEM-PD Cell Stem Cell. 2023;30:1299-314.e9.
Wang YK, Zhu WW, Wu MH, Wu YH, Liu ZX, Liang LM, et al. Human clinical-grade parthenogenetic ESC-derived dopaminergic neurons recover locomotive defects of nonhuman primate models of Parkinson’s disease. Stem Cell Reports. 2018;11:171–82.
Feldman EL, Goutman SA, Petri S, Mazzini L, Savelieff MG, Shaw PJ, et al. Amyotrophic lateral sclerosis. Lancet. 2022;400:1363–80.
Jaiswal MK. Riluzole and edaravone: a tale of two amyotrophic lateral sclerosis drugs. Med Res Rev. 2019;39:733–48.
Brandebura AN, Paumier A, Onur TS, Allen NJ. Astrocyte contribution to dysfunction, risk and progression in neurodegenerative disorders. Nat Rev Neurosci. 2023;24:23–39.
Gotkine M, Caraco Y, Lerner Y, Blotnick S, Wanounou M, Slutsky SG, et al. Safety and efficacy of first-in-man intrathecal injection of human astrocytes (AstroRx®) in ALS patients: phase I/IIa clinical trial results. J Transl Med. 2023;21:122.
Steinberg GK, Bet A, Williams J, McDonald K, Diaz R, Samos C, et al. First-in-human phase 1/2a study of intracerebral transplantation using embryonic-derived neural stem cells (NR1) for chronic ischemic stroke. Stroke. 2023;54:A147–247.
Acharjee S, Ghosh B, Al-Dhubiab BE, Nair AB. Understanding type 1 diabetes: etiology and models. Can J Diabetes. 2013;37:269–76.
Chen S, Du K, Zou C. Current progress in stem cell therapy for type 1 diabetes mellitus. Stem Cell Res Ther. 2020;11:1–13.
Schulz TC. Concise review: manufacturing of pancreatic endoderm cells for clinical trials in type 1 diabetes. Stem Cells Transl Med. 2015;4:927–31.
Dang HP, Chen H, Dargaville TR, Tuch BE. Cell delivery systems: toward the next generation of cell therapies for type 1 diabetes. J Cell Mol Med. 2022;26:4756–67.
Pullen LC. Stem cell-derived pancreatic progenitor cells have now been transplanted into patients: report from IPITA 2018. Am J Transplant. 2018;18:1581–2.
Shapiro AMJ, Thompson D, Donner TW, Bellin MD, Hsueh W, Pettus J, et al. Insulin expression and C-peptide in type 1 diabetes subjects implanted with stem cell-derived pancreatic endoderm cells in an encapsulation device. Cell Rep Med. 2021;2: 100466.
Ellis CE, Mojibian M, Ida S, Fung VCW, Skovsø S, McIver E, et al. Human A2-CAR T cells reject HLA-A2 + human islets transplanted into mice without inducing graft-versus-host disease. Transplantation. 2023;107:e222–33.
Reichiman TW, Ricordi C, Naji A, Markmann JF, Perkins BA, Wijkstrom M, et al. 836-P: Glucose-dependent insulin production and insulin-independence in type 1 diabetes from stem cell–derived, fully differentiated islet cells—updated data from the VX-880 cinical trial. Diabetes. 2023. https://doi.org/10.2337/db23-836-P
Yoon SY, Yoon JA, Park M, Shin EY, Jung S, Lee JE, et al. Recovery of ovarian function by human embryonic stem cell-derived mesenchymal stem cells in cisplatin-induced premature ovarian failure in mice. Stem Cell Res Ther. 2020;11:255.
Bahrehbar K, Rezazadeh Valojerdi M, Esfandiari F, Fathi R, Hassani SN, Baharvand H. Human embryonic stem cell-derived mesenchymal stem cells improved premature ovarian failure. World J Stem Cells. 2020;12:857–78.
Menasché P, Vanneaux V, Hagège A, Bel A, Cholley B, Parouchev A, et al. Transplantation of human embryonic stem cell-derived cardiovascular progenitors for severe ischemic left ventricular dysfunction. J Am Coll Cardiol. 2018;71:429–38.
de Wert G, Mummery C. Human embryonic stem cells: research, ethics and policy. Hum Reprod. 2003;18:672–82.
Volarevic V, Markovic BS, Gazdic M, Volarevic A, Jovicic N, Arsenijevic N, et al. Ethical and safety issues of stem cell-based therapy. Int J Med Sci. 2018;15:36–45.
Lo B, Parham L. Ethical issues in stem cell research. Endocr Rev. 2009;30:204–13.
Liu G, David BT, Trawczynski M, Fessler RG. Advances in pluripotent stem cells: history, mechanisms, technologies, and applications. Stem Cell Rev Rep. 2020;16:3–32.
Walters L. Human embryonic stem cell research: an intercultural perspective. Kennedy Inst Ethics J. 2004;14:3–38.
Neaves W. The status of the human embryo in various religions. Development. 2017;144:2541–3.
Sivaraman MAF, Noor SNM. Human embryonic stem cell research: ethical views of Buddhist, Hindu and Catholic Leaders in Malaysia. Sci Eng Ethics. 2016;22:467–85.
International Society for Stem Cell Research. Standards for human stem Cell use in research. https://www.isscr.org/s/ISSCR_Standards_09_FINAL.pdf.
Bubela T, Guebert J, Mishra A. Use and misuse of material transfer agreements: lessons in proportionality from research, repositories, and litigation. PLoS Biol. 2015;13:e1002060.
Lovell-Badge R, Anthony E, Barker RA, Bubela T, Brivanlou AH, Carpenter M, et al. ISSCR guidelines for stem cell research and clinical translation: the 2021 update. Stem Cell Rep. 2021;16:1398–408.
Acknowledgements
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: HI22C1424) and the Grants of the Ministry of ICT Grants and the Ministry of Education, Republic of Korea (2020R1A2C1010293).
Funding
Open Access funding enabled and organized by Seoul National University.
Author information
Authors and Affiliations
Contributions
SJP: conceptualization, methodology, formal analysis, resources, data curation, investigations, visualization, Writing—Original Draft, Visualization, project administration, funding acquisition. YYK: methodology, validation, Writing—Review & Editing, Supervision. JYH: methodology, investigation, validation, supervision. SWK: methodology, investigation, validation, supervision. HK: methodology, investigation, validation, supervision. S-YK: conceptualization, methodology, project administration, funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare nothing to disclose.
Ethical statement
There are no animal experiments carried out for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, S.J., Kim, Y.Y., Han, J.Y. et al. Advancements in Human Embryonic Stem Cell Research: Clinical Applications and Ethical Issues. Tissue Eng Regen Med 21, 379–394 (2024). https://doi.org/10.1007/s13770-024-00627-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-024-00627-3