Abstract
Background and purpose
The goal of this study was to systematically review the metabolic profile of meningiomas using magnetic resonance spectroscopy in comparison to gliomas, as measured by mean metabolite ratios.
Methods
Following the PRISMA guidelines, a systematic literature review was performed using the PubMed, Ovid Embase, Web of Science, and the Cochrane databases from inception to May 2021. Studies were selected based on predetermined inclusion and exclusion criteria.
Results
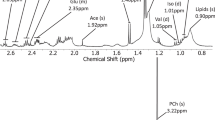
Eight studies were ultimately selected with 207 patients included. Fifty-nine patients were diagnosed with meningioma (age = 48.4, 66.7% female) and 148 patients diagnosed with glioma (age = 56.4, 49.2% female). Three studies reported elevated Cho/Cr in meningiomas compared to gliomas (5.71 vs. 1.46, p < 0.05, 7.02 vs. 2.62, p < 0.05, and 4.64 vs. 2.52, p = 0.001). One study reported Ala/Cr to be significantly elevated in meningiomas compared to gliomas (1.30 vs. undetectable, p < 0.001). One study reported myo-Inositol/Cr to be significantly elevated in meningiomas in comparison to gliomas (1.44 vs. 1.08, p < 0.05). One study reported Glu/Cr to be significantly elevated in meningiomas in comparison to gliomas (3.47 vs. 0.89, p = 0.002). Two studies reported Cho/NAA to be significantly elevated in meningiomas in comparison to gliomas (4.46 vs. 2.6, p = 0.004, and 5.8 vs. 2.55, p < 0.05). Two studies reported NAA/Cr was significantly elevated in gliomas compared to meningiomas (undetectable vs. 1.54, p < 0.001 and undetectable vs. 0.58, p < 0.05).
Conclusions
Significant differences in metabolite ratios between tumor types were reported in Cho/Cr, Ala/Cr, Glu/Cr, Cho/NAA, myoI/Cr and NAA/Cr between meningiomas and gliomas.

Similar content being viewed by others
References
Ostrom QT, Gittleman H, Xu J et al (2016) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009–2013. Neuro Oncol 18(5):v1–v75
Ward EM, Sherman RL, Henley SJ et al (2019) Annual report to the nation on the status of cancer, featuring cancer in men and women age 20–49 years. JNCI J Nat Cancer Inst 111(12):1279–1297. https://doi.org/10.1093/jnci/djz106
Michaud D, Schiff D, Batchelor T. Incidence of primary brain tumors. U: UpToDate, Loeffler JS, Wen PJ ed UpToDate [Internet]. Published online 2020.
Lapointe S, Perry A, Butowski NA (2018) Primary brain tumours in adults. Lancet 392(10145):432–446
Jagannathan NR, Sharma U (2017) Breast tissue metabolism by magnetic resonance spectroscopy. Metabolites 7(2):25
van der Graaf M (2010) In vivo magnetic resonance spectroscopy: basic methodology and clinical applications. Eur Biophys J 39(4):527–540
Barker P, Gillard J, Waldman A (2009) Fundamentals of MR spectroscopy. In: Gillard JH, Waldman AD, Barker PB (eds) Clinical MR neuroimaging: diffusion, perfusion and spectroscopy Fundamentals of MR spectroscopy. Cambridge University Press, pp 7–26
Herminghaus S, Pilatus U, Möller-Hartmann W et al (2002) Increased choline levels coincide with enhanced proliferative activity of human neuroepithelial brain tumors. NMR Biomed Int J Devot Dev Appl Mag Res Vivo 15(6):385–392
Gillies RJ, Morse DL (2005) In vivo magnetic resonance spectroscopy in cancer. Annu Rev Biomed Eng 7:287–326
Glunde K, Bhujwalla ZM, Ronen SM (2011) Choline metabolism in malignant transformation. Nat Rev Cancer 11(12):835–848
Manton D, Chaturvedi A, Hubbard A et al (2006) Neoadjuvant chemotherapy in breast cancer: early response prediction with quantitative MR imaging and spectroscopy. Br J Cancer 94(3):427–435
Haddadin IS, McIntosh A, Meisamy S et al (2009) Metabolite quantification and high-field MRS in breast cancer. NMR Biomed Int J Devot Dev Appl Mag Res Vivo 22(1):65–76
Nelson SJ, Graves E, Pirzkall A et al (2002) In vivo molecular imaging for planning radiation therapy of gliomas: an application of 1H MRSI. J Mag Res Imaging Off J Int Soc Mag Res Med 16(4):464–476
Howe F, Barton S, Cudlip S et al (2003) Metabolic profiles of human brain tumors using quantitative in vivo 1H magnetic resonance spectroscopy. Mag Res Med Off J Int Soc Mag Res Med 49(2):223–232
Opstad KS, Murphy MM, Wilkins PR, Bell BA, Griffiths JR, Howe FA (2004) Differentiation of metastases from high-grade gliomas using short echo time 1H spectroscopy. J Mag Res Imaging Off J Int Soc Mag Res Med 20(2):187–192
Ohba S, Murayama K, Nishiyama Y et al (2019) Clinical and radiographic features for differentiating solitary fibrous tumor/hemangiopericytoma from meningioma. World Neurosurg 130:e383–e392
Nowosielski M, Galldiks N, Iglseder S et al (2017) Diagnostic challenges in meningioma. Neuro Oncol 19(12):1588–1598
Kousi E, Tsougos I, Fountas K et al (2012) Distinct peak at 3.8 ppm observed by 3T MR spectroscopy in meningiomas, while nearly absent in high-grade gliomas and cerebral metastases. Mol Med Rep 5(4):1011–1018
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ Clin Res 339:b2535. https://doi.org/10.1136/bmj.b2535
Gajewicz W, Papierz W, Szymczak W, Goraj B (2003) The use of proton MRS in the differential diagnosis of brain tumors and tumor-like processes. Med Sci Monit 9(9):MT97–MT1105
Kumar A, Kaushik S, Tripathi R, Kaur P, Khushu S (2003) Role of in vivo proton MR spectroscopy in the evaluation of adult brain lesions: our preliminary experience. Neurol India 51(4):474
Falini A, Calabrese G, Origgi D et al (1996) Proton magnetic resonance spectroscopy and intracranial tumours: clinical perspectives. J Neurol 243(10):706–714
Salzedo E, Cortes M, Melançon D, Tampieri D (2009) Myoinositol trends in different types of brain lesions. Neuroradiol J 22(1):16–21
Darweesh AMN, Badawy ME, Hamesa M, Saber N (2014) Magnetic resonance spectroscopy and diffusion imaging in the evaluation of neoplastic brain lesions. Egypt J Radiol Nucl Med 45(2):485–493
Hazany S, Hesselink JR, Healy JF, Imbesi SG (2007) Utilization of glutamate/creatine ratios for proton spectroscopic diagnosis of meningiomas. Neuroradiology 49(2):121–127
Horská A, Barker PB (2010) Imaging of brain tumors: MR spectroscopy and metabolic imaging. Neuroimaging Clin 20(3):293–310
Bulik M, Jancalek R, Vanicek J, Skoch A, Mechl M (2013) Potential of MR spectroscopy for assessment of glioma grading. Clin Neurol Neurosurg 115(2):146–153
Jaskólski DJ, Fortuniak J, Stefańczyk L et al (2013) Differential diagnosis of intracranial meningiomas based on magnetic resonance spectroscopy. Neurol Neurochir Pol 47(3):247–255
Yue Q, Isobe T, Shibata Y et al (2008) New observations concerning the interpretation of magnetic resonance spectroscopy of meningioma. Eur Radiol 18(12):2901–2911
Demir MK, Iplikcioglu AC, Dincer A, Arslan M, Sav A (2006) Single voxel proton MR spectroscopy findings of typical and atypical intracranial meningiomas. Eur J Radiol 60(1):48–55
Brandão LA, Castillo M (2016) Adult brain tumors: clinical applications of magnetic resonance spectroscopy. Mag Res Imaging Clin 24(4):781–809
Urenjak J, Williams SR, Gadian DG, Noble M (1992) Specific expression of N-acetylaspartate in neurons, oligodendrocyte-type-2 astrocyte progenitors, and immature oligodendrocytes in vitro. J Neurochem 59(1):55–61
Ijare OB, Hambarde S, Brasil da Costa FH et al (2022) Glutamine anaplerosis is required for amino acid biosynthesis in human meningiomas. Neuro Oncol 24(4):556–568
Kudo H, Mio T, Kokunai T, Tamaki N, Sumino K, Matsumoto S (1990) Quantitative analysis of glutathione in human brain tumors. J Neurosurg 72(4):610–615
Barba I, Moreno Á, Martínez-Pérez I et al (2001) Magnetic resonance spectroscopy of brain hemangiopericytomas: high myoinositol concentrations and discrimination from meningiomas. J Neurosurg 94(1):55–60. https://doi.org/10.3171/jns.2001.94.1.0055
Kantarci K, Jack C, Xu Y et al (2000) Regional metabolic patterns in mild cognitive impairment and Alzheimer’s disease: a 1H MRS study. Neurology 55(2):210–217
Catani M, Cherubini A, Howard R et al (2001) 1H-MR spectroscopy differentiates mild cognitive impairment from normal brain aging. NeuroReport 12(11):2315–2317
Wattjes M, Harzheim M, Lutterbey G, Klotz L, Schild H, Träber F (2007) Axonal damage but no increased glial cell activity in the normal-appearing white matter of patients with clinically isolated syndromes suggestive of multiple sclerosis using high-field magnetic resonance spectroscopy. Am J Neuroradiol 28(8):1517–1522
Lyndon D, Lansley JA, Evanson J, Krishnan AS (2019) Dural masses: meningiomas and their mimics. Insights Imaging 10(1):1–22
Yan PF, Yan L, Zhang Z et al (2016) Accuracy of conventional MRI for preoperative diagnosis of intracranial tumors: A retrospective cohort study of 762 cases. Int J Surg 36:109–117
Zhai X, Zhou M, Chen H et al (2019) Differentiation between intraspinal schwannoma and meningioma by MR characteristics and clinic features. Radiol Med (Torino) 124(6):510–521
Chen T, Jiang B, Zheng Y et al (2020) Differentiating intracranial solitary fibrous tumor/hemangiopericytoma from meningioma using diffusion-weighted imaging and susceptibility-weighted imaging. Neuroradiology 62(2):175–184
Öz G, Alger JR, Barker PB et al (2014) Clinical proton MR spectroscopy in central nervous system disorders. Radiology 270(3):658–679
García-Figueiras R, Baleato-González S, Padhani AR et al (2016) Proton magnetic resonance spectroscopy in oncology: the fingerprints of cancer? Diagn Interv Radiol 22(1):75
Funding
No external funding was awarded for this study or publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential competing interest was reported by the authors.
Ethical approval/Informed consent
No IRB approval or patient informed consent was necessary for this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
De Stefano, F.A., Morell, A.A., Smith, G. et al. Unique magnetic resonance spectroscopy profile of intracranial meningiomas compared to gliomas: a systematic review. Acta Neurol Belg 123, 2077–2084 (2023). https://doi.org/10.1007/s13760-022-02169-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-022-02169-8