Abstract
Electrospun scaffolds with diameter fibers compared to those in the extracellular matrix were produced with poly(lactic acid) (PLA) and non-denatured collagen from bovine dentin (DCol). DCol was obtained through an improved version of the Longin method by acid erosion of the hydroxyapatite of the roots of teeth from a 2-year-old cattle. The dentin collagen was characterized by energy dispersive X-ray spectroscopy (EDS), and carbon, nitrogen, and oxygen were found to be the main elements of the protein. Infrared analysis revealed the typical bands of collagen at about 3300, 1631, 1539, and 1234 cm−1 for amides A, I, II, and III, respectively. Calorimetric and infrared analyses also demonstrated that the collagen was non-denatured. With scanning electron microscopy, it was found that the thinnest fibers with a diameter comparable to that of fibers in the extracellular matrix were obtained when dentin collagen and acetic acid (AAc) were added to the solution of PLA in trifluoroethanol (TFE). The scaffolds with the thinnest diameter had also the highest porosity, and we considered that they could be beneficial in the growth of dentin cell. Human placenta-derived mesenchymal stem cells were seeded onto electrospun scaffolds. After 24, 48 and 96 h of culture, cell proliferation was evaluated by two independent strategies. In both assays, it was found that the pl-MSCs were capable of adhering and proliferating in different scaffolds. It was also observed that cell adhesion and proliferation increased significantly in scaffolds containing collagen, although the addition of AAc slightly decreased this effect on all scaffolds.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tissue engineering (TE) deals with the design and production of new tissues to replace the lost parts of human beings [1, 2] as a result of traumas, syndromes, accidents, or diseases with identical tissue. To this end, TE promotes complete rehabilitation, which involves the replacement of damaged tissue [3] for the regeneration of functions [4,5,6]. This discipline requires a support, cells, and growth factors and differentiation. In TE, the supports are called scaffolds, which are porous matrices made of different materials (often polymers). They are required for consecutive cell adhesion, migration, proliferation, differentiation, and viability [5, 7, 8].
Growth factors are normally added to scaffolds, and researchers are searching for their new sources to increase the rate of tissue culture. A maximum diameter of less than one micron is required for the scaffold fibers to better simulate the extracellular matrix, and one of the most common methods to obtain them is by electrospinning. Electrospinning allows us to produce scaffolds formed by fine polymer filaments [9] to control the diameter of scaffold fibers and to add growth factors [10,11,12].
Various polymers have been used for the manufacture of scaffolds by electrospinning, such as poly(ε-caprolactone) (PCL) [13] poly(glycolic acid) (PGA) [14], and poly(lactic acid) [15,16,17]. However, PLA is often selected as a provisional extracellular matrix because it is aliphatic that typically degrades within 30 and 50 weeks to metabolize by-products in the human body, such as water and lactic acid. Furthermore, it is approved by the US Food and Drug Administration (FDA) and has a high tensile strength [20]. Growth and differentiation factors that are added to scaffolds for cell growth include peptides and proteins like collagen and elastin.
Collagen is a natural polymer that consists of three polypeptide chains: two α1 (I) chains and one α2 (I) chain. Each chain is formed by a sequence of glycine, proline, and hydroxyproline. The sequences of these peptides give rise to different types of collagens present in living beings [19]. Collagen is used in the manufacture of scaffolds because it is a component of the extracellular matrix of several tissues, thus promoting the growth and differentiation of cells, in addition to being biocompatible [20,21,22].
As in humans, collagen is part of the extracellular matrix of bovine dentin, which mainly presents collagen type I, and is very similar to the collagen in human dentin [23,24,25]. Although collagen from human dentin would be more suitable to clinical applications, scarcity of donators of extracted healthy teeth, ethical aspects in postmortem extraction and possible trade of dental organs make the research work more difficult in this field. In that matter, bovine teeth are easily obtained, have no caries, and may arise as a solution to innumerable research work [23]. The dentin root contains 20% collagen, 70% inorganic matter, and 10% water. Therefore, dental pieces of bovine origin are a suitable raw material for extracting this protein. It is necessary to use acidic solutions for the extraction of collagen from mineralized tissues. In 1971, Longin used HCl to extract collagen from the bones of archaeological human remains [26]. Afterwards, this method has been modified several times. In the last modification, extraction of collagen from dental tissue is reported to be applied in archaeological specimen [27]. Following that, we worked in a new modification of Longin method to obtain collagen from fresh dentin of bovine teeth to be used in the production of electrospun scaffolds. PLA electrospun scaffolds have been produced in combination with collagen. Chiu et al. [28] functionalized the electrospun scaffolds of PLA by adding small amounts of calf skin collagen to potentiate the growth and differentiation of osteoblastic cells. Kije´nska et al. [29] produced scaffolds of poly(lactic acid-co-ε-caprolactone) and collagen types I and II for the favorable generation of nerve tissue. Thus far, bovine dentin collagen has not been used in the production of electrospun scaffolds for the regeneration of dental tissue. Therefore, the objective of this study was to extract collagen from bovine dentin with an improved Longin method to produce electrospun scaffolds with fiber diameters comparable to those in the extracellular matrix using PLA mixed with this protein in TFE/AAc, the new solvent system, and to select those with the better features to support the growth of dentin cells.
Experimental
Materials
Lower anterior teeth from bovines were provided by the Municipal Slaughterhouse of San Martin Texmelucan, Mexico. The reagents were reagent-hydrochloric acid grade, trifluoroethanol, deionized water, 99% acetic acid (Sigma Aldrich), poly(lactic acid) (Nature Works Co, MW 253,088), and collagen from calf skin, SCol (Elastin Products Co.), which was used for comparison.
Methods
Extraction of dentin collagen
The lower anterior teeth of bovines were removed from slaughtered cows, and the crown was separated from the root. The root was used to isolate the collagen from the dentin. First, the teeth were washed with deionized water, and the periodontal tissue and cementum were removed with a curette. The tooth neck was cut across the cross section to separate the crown with the enamel from the root, and the radicular pulp was extracted. The obtained dentin of the roots was washed and kept at 4 °C in deionized water according to standard method ISO/TS 1145 (2003). The dentin roots were ground in a planetary ball mill (PM100) to a mean particle size of 27 µm to extract the collagen. Based on the Longin method [26], the collagen from the dentin was obtained as follows. The ground dentin (100 mg) was treated with 0.6 molar HCl (10 mL) for 24 h for decalcification. The suspension was centrifuged at 8000 rpm for 10 min. After repeating this procedure three times, the collagen was washed in deionized water and centrifuged. The compacted bovine dentin collagen (DCol) obtained in the centrifuge tube was freeze-dried.
Characterization of the dentin collagen
Morphological analysis of the DCol was conducted by scanning electronic microscopy (SEM) with a Jeol JSM-7600 F. Energy-dispersive X-ray spectroscopy (EDS) was also used to detect carbon, nitrogen, and oxygen in the collagen using the same equipment used for SEM coupled with an X-ray detector. Furthermore, DCol was also analyzed with a Fourier transform infrared spectrometer with an accessory for attenuated total reflectance (Thermo Scientific Nicolet 6700 ATR-FTIR). The analyses were performed directly on the DCol without prior preparation.
The thermal transitions of DCol were studied by differential scanning calorimetry (DSC; TA Instruments Q2000-DSC) under nitrogen atmosphere. The samples were heated from 0 to 300 °C at a heating rate of 10 °C/min. The results were used to determine the temperature at which changes in physical state occurred, such as the glass transition temperature (Tg), crystallization temperature (Tc), melting temperature (Tm), and the denaturalization temperature of the DCol. The mass loss due to the evaporation of moisture and degradation of DCol and SCol was determined by thermogravimetric analysis (TGA) (Q5000 IR TA Instruments TGA). Approximately 5 mg of each sample was heated from 30 to 600 °C at a rate of 10 °C/min under nitrogen atmosphere.
Pristine PLA and its blends with both collagens (DCol and SCol) were used to make electrospun scaffolds. The polymer solutions were electrospun in the presence of an intense electric field, which was applied between the spinneret and a conductive collector. The polymer scaffolds were prepared at room temperature using a home-made setup (Fig. 1a scheme, and Fig. 1b experimental setup), which has been described elsewhere [30]. The ratio of PLA to collagen was 30:1. The mixtures were stirred at room temperature for 24 h to obtain homogeneous solutions. The solutions were prepared using polymer concentrations of 13% and 16% (w/v), TFE solvent and a mixture of TFE/AAc (99:1 v/v). The typical processing parameters to obtain scaffolds of PLA and its mixtures with collagen were a voltage of 13–15 kV, distancing from the tip of the needle to the collector of 10, 15, and 25 cm, a flow rate of 0.4 mL/h, and a needle diameter of 0.80 mm.
Chemical and physical analyses of polymers and scaffolds
For the morphological analysis, the electrospun scaffolds were cut into pieces of 0.5 cm × 0.5 cm and coated with gold using plasma-assisted deposition. The micrographs were processed with the digitization program Image J (National Institute of Health, USA) to determine the diameter of the fibers. An average from 30 measurements was considered. To estimate the porosity, a rectangle of 1350 µm2 was analyzed. The mechanical properties were obtained from samples that were cut from the scaffolds using a die according to ASTM D1078. The properties were tested at 10 mm/min in a mechanical testing machine (Instron-R5500).
Cell proliferation
Mesenchymal stem cells obtained from human placenta were kindly donated by the Immunotherapy and Tissue Engineering Laboratory of UNAM School of Medicine. From each scaffold, discs of 0.5 cm in diameter, each, were cut, and were conditioned in an aqueous environment by immersion in Hanks balanced salt solution (HBSS) for 2 h and subsequently sterilized by UV radiation for another 2 h. The scaffolds discs were transferred into 96-well culture plates, placing one disc per well, the excess of HBSS was removed and subsequently 1 × 104 MSCs were seeded in each well. The cultures were fed with DMEM-F12 medium supplemented with 10% FBS/streptomycin–amphotericin, under environmental conditions of temperature 37 °C, atmosphere with 5% CO2 and humidity at saturation. Cultures were maintained for 24, 48 and 96 h.
At the end of each culture, one disk from each experimental scaffold was used for proliferation colorimetric assay by determination of resazurin reduction (Presto blue Cat. No. A13261 Thermo Fisher Scientific). Briefly, each disk was transferred to a new well with 100 µL of Presto blue reagent solution, which was kept in incubation for 2.5 h. The supernatants were collected, and using a plate reader their absorbance at 570 nm was determined, and with it the cell density. On the other hand, another disc of each condition was removed from the culture, and subsequently incubated in 100 µL of a solution of calcein–ethidium homodimer (LIVE/DEAD viability/cytotoxicity Kit (Cat. No. L3224) Thermo Fishes Scientific) and it was kept in incubation for 30 min. Finally, each disc was observed on a fluorescence microscope to determine the cell number and viability.
Results and discussion
Extraction of bovine dentin collagen
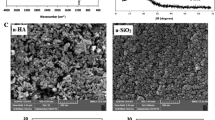
It has been widely reported that PLA is a suitable polymer for tissue engineering. Chen [19] demonstrated for the first time that PLA electrospun scaffolds with collagen type I from calf skin presented higher adhesion and migration than scaffolds made with pristine PLA. As in most organs, the collagen from bovine skin is quite similar to the human skin collagen as they present similarity higher than 95% in the peptides content. The peptides found in the skins of the two mammalians are identical, and there are 18 peptides; the main peptides in descending order of content are glycine, proline, alanine, hydroxyproline and glutamic acid. These five peptides account for 75% of the total [31, 32]. Thus, we expected that collagen obtained from bovine dentin may be better suited for restoring the damaged dental tissue. The morphology of dentin has a characteristic tubular pattern [24, 33]. As a result of a transversal cut of the tubules in dentin to extract the collagen, we confirmed that its surface has a pattern like a hole, as shown in the micrograph in Fig. 2a. The average holes diameter was 3.7 ± 0.77 μm. The morphology of the bovine collagen did not present a defined shape, but rather a discontinuous pattern of irregular shaped sheets with a few twisted or coiled fibers (Fig. 2b). In contrast, the commercial calf skin-collagen used as a control looks like a film with a smooth surface (Fig. 2c), probably because of the method used to obtain it. The percentages of the elements present in the DCol analyzed by EDS are shown in Table 1. The constituents of the dentin collagen were carbon, nitrogen, and oxygen only. The percentages agree with those previously reported for collagen from human dentin [34]. From these results, it was found that the modified Longin method was effective to obtain the dentin collagen without bone components. The Longin method [26] is a process to obtain collagen from ancient bones and it is used in archeology to search for information about the evolutionary process. The method consists of the demineralization of bones with hydrochloric acid to separate the collagen from the hydroxyapatite. Later, the protein is gelatinized, and archeological analyses are conducted. In this work, the Longin method was modified to improve its efficiency to obtain the collagen from bovine dentin. The modification consisted of reducing the demineralization times so as not to gelatinize the protein. These results agree with the report of Maspero [35], who mentioned that this process with ethylenediamine tetra-acetic acid (EDTA) is appropriate because it completely demineralizes the inorganic matter of the bone. According to Magne [34], hydrochloric acid also removes most non-collagenous proteins from dentin.
Characterization of collagen by ATR-FTIR
The characteristic bands from ATR-FTIR corresponding to lyophilized collagen from the bovine dentin spectrum and commercial calf skin type I collagen are displayed in Fig. 3. Both spectra present great similarity. A considerable wide band was detected between 2900 and 3600 cm−1, which presented a maximum near 3300 cm−1. At lower wavelengths between this maximum and 1700 cm−1, no significant bands were found. However, at 1631 cm−1, there was an intense and narrow band. Afterward, another band with a slightly lower intensity at 1539 cm−1 was found. The next significant band was located at 1234 cm−1, which was less intense than the previous bands. The different important bands in these spectra and their assignments in descending order can be seen in Table 2. Comparing them in detail, the band at 1539 cm−1 from the spectrum of DCol appears in the spectrum of SCol at 1546 cm−1, which is in agreement with Benjakul [36]. This implies a 7 cm−1 shift between the spectra, which was probably due to the different origins of the collagens. According to a study by Maspero [35], who obtained collagen from bovine bone, the characteristic vibration bands with a maximum at about 3300 cm−1 were associated to amide A, while the band at 1631 cm−1 corresponded to amide I. The signal present at 1539 cm−1 was due to amide II, and that at 1234 cm−1 was due to amide III. These signals as a whole are typical of collagen because they correspond to the vibrations of the functional groups of this protein. Table 2 also shows the absence of the assigned bands of the bovine dentin in the ATR-FTIR spectrum of the obtained collagen. Thus, the inorganic material of the bovine dentin was completely eliminated since the characteristic vibrations of hydroxyapatite were not observed, which was expected at 3572 cm−1 (associated with O–H vibration), 1085, 1016 cm−1, 961 cm−1 (corresponding to P–O), 872 cm−1 (C–O link), 562 cm−1, and 373 cm−1 (to O–P–O vibration) [35]. The results from the ATR-FTIR spectra confirmed the presence of pure collagen and the absence of hydroxyapatite in the obtained final product. The results coincided with those reported by Maspero [35] and in agreement with the EDS analysis, which confirmed the absence of Ca and P in the collagen obtained; the main components of the hydroxyapatite from bovine dentin. Our method presents advantages compared with that of Ferreira [37]. Ferreira used EDTA for 4 weeks to demineralize inorganic matter, whereas the method performed in this work only required 72 h. Zhang [38] used AAc with trypsin to dissolve bovine collagen, and the collagen was precipitated with sodium chloride. However, in the collagen obtained, they found residues of sodium chloride. The denaturation of collagen implies the loss of the triple-helix α-chains in the supramolecular structure of the collagen. From the ATR-FTIR spectrum, we examined whether the collagen obtained was denatured. The bands at 3300, 1631, 1539, and 1234 cm−1 corresponded to amides A, I, II and III, respectively, as typical bands of collagen. Based on the description by Ferreira, the band at 1631 cm−1 was related to amide I, which is associated with the structure of the α-chains of non-denatured collagen. This band was present in the DCol. When the collagen has its triple-helix structure, there should be a ratio of 1.0 between the absorbance intensities of the band corresponding to amide III at 1234 cm−1 and the band at 1450 cm−1 [39]. This means that the collagen is not denatured. This ratio was calculated between the absorbance heights of the bands at 1234 and 1450 cm−1 for both DCol and SCol, and the ratio was around of 1.0. Therefore, the obtained DCol was not denatured. Furthermore, both DCol and SCol were found not to be hydrolyzed because of the absence of a band at 1725 cm−1, which appears upon the hydrolysis of this protein [35]. Infrared analysis confirmed the modified method of Login used in this work and showed that pure dentin collagen without hydroxyapatite residues did not denature in a shorter time.
Thermal analysis of collagen by TGA and DSC
The thermogravimetric behavior of DCol and SCol obtained by TGA is shown in Fig. 4. DCol showed a first weight loss of 14.6% between 30 and 100 °C. This was mainly due to water evaporation which was in agreement with Cucos [40]. A second weight loss of 62.1% was observed between 220 and 430 °C. The calf skin collagen showed similar behavior (Fig. 4). A first weight loss of 13.1% was observed between 30 and 100 °C, mainly due to water evaporation. Subsequently, a second weight loss of 69.9% occurred between 217 and 425 °C. The second weight loss stage observed in both types of samples was attributed to thermal denaturation and degradation of the collagen. The DSC analysis of DCol showed two endothermic peaks (Fig. 5). The first was a broad peak and had a maximum value at 86 °C. Subsequently, the second endothermic peak had a maximum value at 227 °C. The SCol showed similar behavior: the first peak had a maximum value at 99 °C, and the second had one at 217 °C. Thus, there was a 10 °C difference between the degradation temperatures of DCol and SCol, which probably occurred because they come from different organs. The DSC thermograms of the dentin collagen showed a denaturation temperature of 227 °C, and that of SCol was above 217 °C. These results are in agreement with a previous report [41]. Both TGA and DSC analyses showed a denaturation followed by a degradation stage. In addition, the results of the thermal and spectroscopic analysis are consistent regarding the bovine dentin collagen obtained not being denatured.
Morphology of PLA and PLA/collagen scaffolds in SEM
The electrospinning technique allows us to produce scaffolds of different polymers with thin fiber diameters. The diameter and morphology of the fibers can be handled by controlling either the solution concentration or the parameters of the process of electrospinning. When the concentration of the polymer in the solution is low, it renders thinner fibers because it takes more time to solidify the jet of a diluted solution during electrospinning. In the process, the jet is lengthened and thins over time, resulting in smaller diameters.
The morphologies of the electrospun scaffolds obtained from pristine PLA and PLA/DCol solutions are shown in Fig. 6. The initial concentration of a solution of pristine PLA and PLA/DCol in TFE was 13%; and then it was increased to 16%. The scaffolds were obtained with voltages of 10 and 13 kV, and the flow rate was constant at 0.4 mL/h for all scaffolds. It can be observed that the fibers from the scaffolds of pristine PLA and its blends with DCol were randomly oriented. Most of the scaffolds with thicker diameters were prepared with pristine PLA, as shown in Fig. 6a, b, g, h, m and n. The thinnest fibers were prepared with PLA/DCol solutions at 13% PLA/DCol (Figs. 6c, d, i, j, p and o). However, these samples presented bulbs in the fibers, and indicated with ellipses. The bulb formation was avoided by raising the solution concentration from 13 to 16%. The effect of voltage at 10 and 13 kV in solutions of 13% and 16% PLA and PLA/DCol in TFE showed no tendency regarding the fiber diameter. However, the standard deviation increased noticeably in most of the scaffolds electrospun at 13 kV. Liu [42] found that by increasing the voltage, several jets of different diameters were formed at the exit of the capillary, which induced an increase in standard deviation of the fibers’ diameter. The solutions of PLA/DCol at 13% electrospun at 10 kV resulted in the smallest diameters in this group of samples, while the electrospun scaffolds with 16% PLA in TFE had bigger diameters. This behavior can be compared to the results of Huang [43], who electrospun gelatin protein derived from collagen at concentrations of 5%, 7.5%, 10%, 12.5%, and 15% in TFE. The diameter of fibers became bigger when the concentration of PLA/DCol was increased from 13 to 16% with no bulbs observed, and increasing the voltage reduced the fiber diameters.
The effect of using TFE:AAc in the electrospinning of PLA/DCol and PLA/SCol upon the morphology is displayed in Fig. 7. AAc was added to the electrospinning solutions because, according to Enis [44], it considerably reduced the fiber diameter in electrospun fibers of PCL, another polyester. An overview of the morphology confirmed that the addition of AAc considerably reduced the diameter of the fiber of the scaffolds of pristine PLA (Fig. 7a, b, g and h), as observed previously in PCL. The reduction in diameter was also observed in the samples of PLA with both collagens when AAc was added; DCol (Fig. 7c, i, o, j and p) and SCol (Fig. 7e, k, q, f, l and r). The addition of collagen also reduced the diameter of the fibers further (Fig. 7c, i and o). This is in agreement with a previous report by Ravichandran [45], who found a reduction in diameter of electrospun fibers because of the addition of collagen type I, III, and poly-(α,β)-DL-aspartic acid to PLA compared to scaffolds of pristine PLA. The scaffolds prepared with PLA/DCol in TFE:AAc had the smallest diameters (Fig. 7d, j and p). Specifically, the scaffold prepared with DCol and AAc at a needle–collector distance of 10 cm had the smallest diameter (437 ± 222 nm), which was in the range of fibers in the extracellular matrix of bone tissue, 50 to 500 nm, mentioned by Zang et al. [46]. In contrast, the scaffold made of pristine PLA without AAc or collagen electrospun at 15 cm presented the thickest diameter (1211 ± 327 nm) (Fig. 7g). The electrospun scaffolds made of PLA with DCol and SCol at 15 cm were selected as a promising candidate for cell growth because of their thinner fibers and lower standard deviation (Fig. 7j and l). Table 3 summarizes the six scaffolds that we consider suitable to study dentin cell growth. Molamma et al. [47] electrospun poly(L-lactic acid) (PLLA) with 1,1,1,3,3,3-hexafluor-2-isopropanol (HFIP) at a concentration of 16% (w/v), a voltage of 10 kV, and a needle–collector distance of 15 cm. They obtained fibers of 860 ± 110 nm. However, the scaffolds that we electrospun with TFE as a solvent under the same conditions mentioned above had an average fiber diameter of 813 ± 351 nm, although a greater standard deviation was observed than the previous work. The fiber diameters with DCol were smaller than the fiber diameters of the solutions with SCol, and a further reduction in fiber diameters was observed when AAc was included as a solvent.
Porosity of scaffolds
The porosity of scaffolds is important for cell colonization. It was estimated as the percentage of free average area in the scaffolds from the SEM micrographs. The porosity of the scaffolds is shown in Table 4. The morphology of the scaffolds prepared in the conditions shown in Table 3 was used to determine the porosity and mechanical properties. The PLA/TFE scaffolds had a porosity of 56.5%. The addition of AAc produced scaffolds with 62% porosity, while the addition of collagen to the scaffolds decreased the porosity to 61.8% compared to the scaffolds made of PLA in TFE. When both AAc and collagen were added, the porosity of the scaffolds considerably increased. Kock et al. [48] found that a high porous scaffold is essential for cell migration, diffusion of oxygen and nutrients. The highest porosity of 77.6% was achieved with PLA, DCol, and AAc. According to Fig. 7 and Table 4, the porosity of the scaffolds increased as the diameter of the fibers decreased.
Mechanical properties in tension
The scaffolds obtained under the conditions shown in Table 3 were tested in uniaxial tension according to D1708 ASTM standard method. Their tensile stress and Young's modulus were evaluated. The scaffold made of pristine PLA dissolved in TFE presented the highest mechanical properties with a tensile stress of 3.71 ± 0.39 MPa and a Young's modulus of 93.8 ± 14.6 MPa. The scaffolds prepared from solutions of PLA dissolved in TFE/AAc had a tensile stress of 2.11 ± 0.37 MPa and a Young's modulus of 22.7 ± 3.9 MPa, which were considerably smaller than the mechanical properties of the scaffolds prepared without AAc. The scaffolds made of PLA/DCol in TFE presented a tensile stress of 1.51 ± 0.36 MPa and a Young's modulus of 14.1 ± 4.6 MPa. The Young's modulus decreased 84.9% compared to that of pristine PLA in TFE (93.8 MPa). The tensile stress of 1.26 ± 0.25 MPa and the Young's modulus of 10.6 ± 3.2 MPa corresponded to the PLA/SCol scaffolds in TFE/AAc. The addition of AAc considerably reduced the mechanical properties of the scaffolds. Both types of collagens also reduced the mechanical properties of the blends further. This effect could be attributed to the poor adhesion between collagen and PLA [49, 50] as a result of low miscibility between these two polymers. This undesirable decrease in mechanical properties contrasted with the desirable decrease in the diameters of the fibers. However, the selected scaffolds (Table 3) had the thinnest fibers comparable to the fibers in the extracellular matrix produced when dentin collagen and acetic acid were added to PLA, and were the most regular fibers with the lowest standard deviation and the highest porosity; it is expected to be the most suitable ones for culturing dentin cells. In this study, we extracted collagen from dentine bovine.
MSCs cell proliferation
In each different culture, 1 × 104 MSCs was seeded and all of them were tested by PrestoBlue and Live/Dead kits to determine cell density and viability at 24, 48 and 96 h. The data obtained on cell density and viability percentage on different culture conditions are shown in Table 5.
In the control groups of PLA–TFE and PLA–TFE–AAc scaffolds, the least cell adhesion was observed; however, they showed an adequate proliferative capacity of the adhered cells, showing a notable increasing on cell density at 48 h as well as 96 h of culture. Regarding the cell cultures carried out on the scaffolds supplemented with collagen, a much higher cell density was observed, with respect to the control groups, in this sense, the cell cultures carried out on the scaffold supplemented with SCol were the ones that showed a better initial cell adhesion as can be seen at 24 h; however, when monitoring cell density at 48 and 96 h of culture, the cultures performed on the scaffold supplemented with DCol were the ones that showed the greatest proliferative activity (Fig. 8a and b, and Table 5). In all cases, it can be seen that the addition of AAc leads to a slight reduction in proliferative activity, although this is not statistically significant. When we evaluated the cytotoxicity of MSCs, we found that the DCol-supplemented scaffold showed the least cytotoxicity effect with cell viability percentage of 80.36%, 81.31% and 78.27% at 24, 48 and 96 h, respectively, whereas the lowest cell viability was observed in non-supplemented scaffolds. As well as on cell density assays, a slight reduction, but not significant reduction, was detected on all AAc-supplemented scaffolds (Fig. 8c and d). In case of using these scaffolds in clinical applications, they must be protected from a possible application of a high load during the mastication, and contamination with bacteria should be avoided.
Proliferation and cell viability assay in MSC cultures seeded on PLA–TFE–collagen electrospun scaffolds: a quantification of cells per mm2 for each type of scaffold. Cell density was estimated by converting the absorbance obtained at 570 nm. In all the scaffolds, an increasing in cell density can be seen, which is more notable at 96 h, b Comparison of the cell density estimated in all the scaffolds at 24, 48 and 96 h of culture. Note that the greatest increase in cell density was observed in the groups that have collagen, it can also be seen that the inclusion of acetic acid induced a slight decrease in the cell density in all groups, c determination of cell viability was expressed in percentages. In all groups, a percentage of viability greater than 50% was observed at 24 h, which increased at 48 and 96 h, d representative images of viability determination by staining with calcein and ethidium homodimer. Green cells are stained with calcein and represent the living cells, while red cells are stained with ethidium homodimer and are dead cells, cells with green and red stain are damaged cells or dying cells
Conclusion
Electrospun scaffolds with diagonal fibers comparable to the extracellular matrix were produced with pure collagen from bovine dentin. Collagen without inorganic matter, non-denatured was successfully obtained in a short time using a new modification of the Longin method. In this study, we extracted collagen from dentine bovine. However, the yielding of Longin method was 3.2%, which is low considering the total collagen content of 20% in the dentine. The characteristic ATR-FTIR bands were related to the presence of pure collagen, which was also found by EDS. Thermal analyses showed a behavior for pure dentin collagen without denaturation as well. PLA with dentin collagen produced the scaffolds with the highest porosity and regular fibers with the lowest standard deviation. The diameter of the fibers decreased even more when the new solvent system for PLA TFE/AAc was used. The scaffold with both dentin and calf skin collagens dissolved in the TFE/AAc solvent system had the smallest fiber diameters and the highest porosity. The scaffolds with calf skin and dentin collagen showed the highest cell proliferation and viability, although the addition of AAc induced a slight reduction, which was not significant, and they were chosen as the most suitable ones for cell culture to regenerate lost dental tissue.
Data availability
We do have all datasets of the experiments of our current study and those generated during their analysis, and are available from the corresponding author on reasonable request.
References
Chen L, Yu Q, Jia Y, Xu M, Wang Y, Wang J, Wen T, Wang L (2022) Micro-and-nanometer topological gradient of block copolymer fibrous scaffolds towards region-specific cell regulation. J Colloid Interf Sci 606:248–260. https://doi.org/10.1016/j.jcis.2021.08.021
Hu T, Shi M, Zhao X, Liang Y, Bi L, Zhang Z, Liu S, Chen B, Duan X, Guo B (2022) Biomimetic 3D aligned conductive tubular cryogel scaffolds with mechanical anisotropy for 3D cell alignment, differentiation and in vivo skeletal muscle regeneration. Chem Eng J 428:131017. https://doi.org/10.1016/j.cej.2021.131017
Sobczak-Kupiec A, Drabczyk A, Florkiewicz W, Gł M, Kudłacik-Kramarczyk S, Słota D, Tomala-Tyliszczak B (2021) Review of the applications of biomedical compositions containing hydroxyapatite and collagen modified by bioactive components. Materials 14:2096. https://doi.org/10.3390/ma14092096
Kim DS, Lee JK, Jung JW, Baek SW, Kim JH, Heo Y, Kim TH, Han DK (2021) Promotion of bone regeneration using bioinspired PLGA/MH/ECM scaffold combined with bioactive PDRN. Materials 14:4149. https://doi.org/10.3390/ma14154149
Navarro RS, Jiang L, Ouyang Y, Luo J, Liu Z, Yang Y, Qiu P, Kuroda K, Chen YE, Ma PX, Yang B (2021) Biomimetic tubular scaffold with heparin conjugation for rapid degradation in in situ regeneration of a small diameter neoartery. Biomaterials 274:20874. https://doi.org/10.1016/j.biomaterials.2021.120874
Lee S, Nagata F, Kato K, Kasuga T, Nakano T (2021) Development of orthophosphosilicate glass/poly (lactic acid) composite anisotropic scaffolds for simultaneous reconstruction of bone quality and quantity. J Biomed Mat Res A 109:788–803. https://doi.org/10.1002/jbm.a.37067
Moradi Y, Atyabi SA, Ghiassadin A, Bakhshi H, Irani S, Atyabi SM, Dadgar N (2021) Cold atmosphere plasma modification on Beta-carotene-loaded nanofibers to enhance osteogenic differentiation. Fibers Polym 23:18–27. https://doi.org/10.1007/s12221-021-0033-y
Nahanmoghadam A, Asemani M, Goodarzi V, Ebrahimi-Barough S (2021) In vivo investigation of PCL/PHBV/Hydroxyapatite nanocomposite scaffold in regeneration of critical-sized bone defects. Fibers Polym 22:2507–2516. https://doi.org/10.1007/s12221-021-1243-z
Rahmania M, Khanib MM, Rabbanid S, Mashaghie A, Noorizadehg F, Faridi-Majidia R, Ghanbari H (2020) Development of poly (mannitol sebacate)/poly (lactic acid) nanofibrous scaffolds with potential applications in tissue engineering. Mat Sci Eng C 110:110626. https://doi.org/10.1016/j.msec.2020.110626
Tolba E (2020) Diversity of electrospinning approach for vascular implants: multilayered tubular scaffolds. Regen Eng Transl Med 6:383–397. https://doi.org/10.1007/s40883-020-00157-z
González-Martínez E, Díaz-Águila CR, Cruz-Rodríguez M, Sánchez-Ramírez B, Albor-Aguilera ML, González-Alfaro Y, Yee-Madeira H (2020) Growing spheroids of lung adenosquamous carcinoma on electrospun poly (ε-caprolactone). Bioinspired Biomim Nanobiomat 9:252–256. https://doi.org/10.1680/jbibn.20.00054
Baek J, Lee EE, Lotz MK, D’Lima D (2020) Bioactive proteins delivery through core-shell nanofibers for meniscal tissue regeneration. Nanomed Nanotechnol 23:102090. https://doi.org/10.1016/j.nano.2019.102090
Choi E, Bae S, Kim D, Yang GH, Lee K, Youd HJ, Kange HJ, Gwakf SJ, An S, Jeon H (2021) Characterization and intracellular mechanism of electrospun poly (ε-caprolactone) (PCL) fibers incorporated with bone-dECM powder as a potential membrane for guided bone regeneration. J Ind Eng Chem 94:282–291. https://doi.org/10.1016/j.jiec.2020.11.001
Jin S, Xia X, Huang J, Yuan C, Zuo Y, Li Y, Li J (2021) Recent advances in PLGA-based biomaterials for bone tissue regeneration. Acta Biomater 127:56–79. https://doi.org/10.1016/j.reactfunctpolym.2020.10450
Gangolphe L, Leon-Valdivieso CY, Nottelet B, Dejean S, Bethry A, Pinese C, Bossard F, Garric X (2021) Electrospun microstructured PLA-based scaffolds featuring relevant anisotropic, mechanical and degradation characteristics for soft tissue engineering. Mater Sci Eng C 129:112339. https://doi.org/10.1016/j.msec.2021.112339
Alisir SH, Ozdemir N, Burgaz E, Dege N, Canavar YE (2021) Fabrication and antimicrobial activity of poly (lactic acid) nanofibers containing firstly synthesized silver diclofenac complex with (2-methylimidazole) for wound dressing applications. Fibers Polym 22:2738–2749. https://doi.org/10.1007/s12221-021-0166-z
Abazari MF, Nasiri N, Nejati F, Kohandani M, Hajati-Birgani N, Sadeghi S, Piri P, Soleimanifar F, Rezaei-Tavirani M, Mansouri V (2021) Acceleration of osteogenic differentiation by sustained release of BMP2 in PLLA/graphene oxide nanofibrous scaffold. Polym Adv Tech 32:272–281. https://doi.org/10.1016/j.mtcomm.2020.101812
Braga Proença L, Pinheiro Pena CA, Vieira da Silva G, da CamargoCunha ILB, Branciforti MC (2020) Study of the antibacterial property of tea tree oil and its incorporation into poly (lactic acid)-montmorillonite clay bionanocomposites. Macromol Symp 394:2000073. https://doi.org/10.1002/masy.202000073
Chen JP, Li SF, Chiang YP (2010) Bioactive collagen-grafted poly-L-lactic acid nanofibrous membrane for cartilage tissue engineering. J NanosciNanotechnol 10:5393–5398. https://doi.org/10.1166/jnn.2010.1945
Lin Z, Zhao C, Lei Z, Zhang Y, Huang R, Lin B, Dong Y, Zhang H, Li J, Li X (2021) Epidermal stem cells maintain stemness via a biomimetic micro/nanofiber scaffold that promotes wound healing by activating the notch signaling pathway. Stem Cell Res Ther Int (SCRTI) 12:341. https://doi.org/10.1186/s13287-021-02418-2
Rastogi K, Vashishtha R, Dan S (2022) Scientific advances and pharmacological applications of marine derived-collagen and chitosan. Biointerf Res Appl Chem 12:3540–3558. https://doi.org/10.33263/BRIAC123.35403558
Kong B, Sun L, Liu R, Chen Y, Shang Y, Tan H, Zhao Y, Sun L (2022) Recombinant human collagen hydrogels with hierarchically ordered microstructures for corneal stroma regeneration. Chem Eng J 428:131012. https://doi.org/10.1016/j.cej.2021.131012
Camargo CHR, Siviero M, Afonso Camargo SE, de Oliveira SHG, Carvalho CAT, Valera MC (2007) Topographical, diametral, and quantitative analysis of dentin tubules in the root canals of human and bovine teeth. J Endod 33:422–426. https://doi.org/10.1016/j.joen.2006.12.011
Posada MC, Sánches CF, GallegoGJ VAP, Restrepo LF, López JD (2006) Dientes de bovino como sustituto de dientes humanos para uso en la odontología. Rev CES Odontologia 19:63–69. https://doi.org/10.21615/cesodon
Marshall WG, Marshall SJ, Kinneyt JH, Balooch M (1997) The dentin substrate: structure and properties related to bonding. J Dent 25:441–458. https://doi.org/10.1016/s0300-5712(96)00065-6
Longin R (1971) New method of collagen extraction for radiocarbon dating. Nature 230:241–242. https://doi.org/10.1038/230241a0
Harmston NI, Linduska EJ, Tomco PL (2019) Stable isotope and compositional analysis of Alaska caribou teeth embedded in polymethyl-methacrylate (PMMA). J Archaeol Sci 111:105016. https://doi.org/10.1016/j.jas.2019.105016
Chiu JB, Liu C, Hsiao BS, Chu B, Hadjiargyrou M (2007) Functionalization of poly (L-lactide) nanofibrous scaffolds with bioactive collagen molecules. J Biomed Mater Res A 83:1117–1127. https://doi.org/10.1002/jbm.a.31279
Kijeńska E, Prabhakaran MP, Swieszkowski W, Kurzydlowski KJ, Ramakrishna S (2012) Electrospun bio-composite P (LLA-CL)/collagen I/collagen III scaffolds for nerve tissue engineering. J Biomed Mater Res B Appl Biomater 100:1093–1102. https://doi.org/10.1002/jbm.b.32676
Gómez Pachón EY, ArévaloFM S, Sabina FJ, Maciel-Cerda A, Montiel Campos R, Batina N, Morales-Reyes I, Vera-Graziano R (2013) Characterisation and modelling of the elastic properties of poly (lactic acid) nanofibre scaffolds. J Mater Sci 48:8308–8319. https://doi.org/10.1007/s10853-013-7644-7
Click EM, Bornstein P (1970) Isolation and characterization of the cyanogen bromide peptides from the α1 and α2chains of human skin collagen. Biochemistry 4:4699–4706. https://doi.org/10.1021/bi00826a012
Veis A, Volpin D (1971) Isolation and characterization of the cyanogen bromide peptides from the α1 and α2chains of acid-soluble bovine skin collagen. Biochemistry 10:1751–1755. https://doi.org/10.1021/bi00786a003
Gotliv BA, Veis A (2005) Peritubular dentin, a vertebrate apatitic mineralized tissue without collagen: role of a phospholipid-proteolipid complex. Calcified Tissue Int 81:191–205. https://doi.org/10.1007/s00223-007-9053-x
Magne D, Weiss P, Bouler JM, Laboux O, Daculsi G (2001) Study of the maturation of the organic (type I collagen) and mineral (nonstoichiometric apatite) constituents of a calcified tissue (dentin) as a function of location: a Fourier transform infrared microspectroscopic investigation. J Bone Miner Res 16:750–757. https://doi.org/10.1359/jbmr.2001.16.4.750
Maspero F, Sala S, Fedi ME, Martini M, Papagni AA (2011) New procedure for extraction of collagen from modern and archaeological bones for 14C dating. Anal Bioanal Chem 401:2019–2023. https://doi.org/10.1007/s00216-011-5252-4
Benjakul AM (2010) Extraction and characterisation of pepsin-solubilised collagen from the skin of unicorn leatherjacket (Aluterusmonocerous). Food Chem 120:817–824. https://doi.org/10.1016/j.foodchem.2009.11.019
Ferreira AM, Gentile P, Sartori S, Pagliano C, Cabrele C, Chiono V, Ciardelli G (2012) Biomimetic soluble collagen purified from bones. J Biotechnol 7:1386–1394. https://doi.org/10.1002/biot.201200184
Zhang Z, Liu W, Li D, Li G (2007) Physicochemical properties of succinylated calfskin pepsin-solubilized collagen. Biosci Biotechnol Biochem 71:2057–2060. https://doi.org/10.1271/bbb.70055
Nazeer RA, Kavitha R, Jai Ganesh R, Naqash SY, Sampath Kumar NS, Ranjith R (2014) Detection of collagen through FTIR and HPLC from the body and foot of Donaxcuneatus Linnaeus. J Food Sci Technol 51:750–755. https://doi.org/10.1007/s13197-011-0539-1
Budrugeac A, Cucos P (2014) Simultaneous TG/DTG-DSC-FTIR characterization of collagen in inert and oxidative atmospheres. J Therm Anal Calorim 115:2079–2057. https://doi.org/10.1007/s10973-013
Lozano LF, Ocotlán JF, Goméz CA, Vázquez R, Belío IA, Bucio L (2003) Thermal analysis study of human bone. J Mater Sci 38:4777–4785. https://doi.org/10.1023/A:1027483220584
Liu Y, Dong L, Fan J, Wang R, Yu JY (2011) Effect of applied voltage on diameter and morphology of ultrafine fibers in bubble electrospinning. J Appl Polym Sci 120:592–598. https://doi.org/10.1002/app.33203
Huang ZM, Zhang YZ, Ramakrishna S, Lim CT (2004) Electrospinning and mechanical characterization of gelatin nanofibers. Polymer 45:5361–5068. https://doi.org/10.1016/j.polymer.2004.04.005
Enis YI, Vojtech J, Sadikoglu TG (2017) Alternative solvent systems for polycaprolactone nanowebs via electrospinning. J Ind Text 47:57–60. https://doi.org/10.1177/1528083716634032
Ravichandran R, Venugopal JR, Sundarrajan S, Mukherjee S, Sridhar R, Ramakrishna S (2012) Composite poly-L-lactic acid/poly-(α, β)-DL-aspartic acid/collagen nanofibrous scaffolds for dermal tissue regeneration. Mater Sci Eng C Mater Biol Appl 32:1443–1451. https://doi.org/10.1016/j.msec.2012.04.024
Zang JT, Xin QI, Li SQ, Li DS, Gong YB, Yang C, Xu F, Liu JG (2010) Fabrication of novel scaffolds containing collagen I/polylactic acid/nanohydroxyapatite via co-electrospinning methods. Chem Res Chinese Univ 26:662–666; http://crcu.jlu.edu.cn/EN/Y2010/V26/I4/662
Molamma PP, Venugopal J, Ramakrishna S (2009) Electrospun nanostructured scaffolds for bone tissue engineering. Acta Biomater 5:2884–2893. https://doi.org/10.1016/j.actbio.2009.05.007
Kock L, Van Donkelaar CC, Ito K (2012) Tissue engineering of functional articular cartilage: the current status. Cell Tissue Res 347:613–627. https://doi.org/10.1007/s00441-011-1243-1
Hajikhani M, Emam-Djomeh Z, Askari G (2021) Fabrication and characterization of mucoadhesive bioplastic patch via coaxial polylactic acid (PLA) based electrospun nanofibers with antimicrobial and wound healing application. Int J Biol Macromol 172:143–153. https://doi.org/10.1007/s00441-011-1243-1
Ospina-Orejarena A, Vera-Graziano R, Castillo-Ortega M, Hinestroza JP, Rodriguez-Gonzalez M, Palomares-Aguilera L, Morales-Moctezuma M, Maciel-Cerda A (2016) Grafting collagen on poly (lactic acid) by a simple route to produce electrospun scaffolds, and their cell adhesion evaluation. Tissue Eng Regen Med 13:375–387. https://doi.org/10.1007/s13770-016-9097-y
Acknowledgements
The authors thank Dr. Miguel Ángel Herrera-Enriquez, Dra. Katia Jarquín-Yáñez, Dr. Omar Novelo Peralta, M. en C. Guillermina González Mancera, Q. Damaris Cabrero Palomino, M. en C. Esteban Fregoso Reinoso, Dr. Jesús Angel Arenas Alatorre, L. A. P. Cristina Navarro Cerón and Q. Miguel Ángel Canseco Martínez, Caín González, Oralia Jiménez, Teresa Vázquez for their invaluable technical support.
Funding
This work was supported by CONACYT, Grant No. CF-14061 and DGAPA-UNAM, Grant No. IG100220.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study design, preparation of the manuscript, and all have read and approved the final version. The specific activities of them were Aurora Navarro-Cerón: methodology, conducting the research, preparation of the paper. Federico Humberto Barceló-Santana: planning, execution, mentorship. Ricardo Vera-Graziano: financial support, visualization of data, preparation of the paper. Filiberto Rivera-Torres: ideas formulation, evolution of research goals and aims. Alberto Jiménez-Ávila: sample analysis and discussion. Raúl Rosales-Ibáñez: Design of methodology. Elizabeth Navarro-Cerón: data analysis, paper preparation. Andrés Eliu Castell-Rodríguez: methodology and discussion of data. Alfredo Maciel-Cerda: project leading, discussion of data, preparation of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Navarro-Cerón, A., Barceló-Santana, F.H., Vera-Graziano, R. et al. Bovine dentin collagen/poly(lactic acid) scaffolds for teeth tissue regeneration. Iran Polym J 32, 469–481 (2023). https://doi.org/10.1007/s13726-023-01139-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13726-023-01139-y