Abstract
Osteoarthritis is a degenerative joint disease characterized by pain and disability. It involves all ages and 70% of people aged >65 have some degree of osteoarthritis. Natural cartilage repair is limited because chondrocyte density and metabolism are low and cartilage has no blood supply. The results of joint-preserving treatment protocols such as debridement, mosaicplasty, perichondrium transplantation and autologous chondrocyte implantation vary largely and the average long-term result is unsatisfactory. One reason for limited clinical success is that most treatments require new cartilage to be formed at the site of a defect. However, the mechanical conditions at such sites are unfavorable for repair of the original damaged cartilage. Therefore, it is unlikely that healthy cartilage would form at these locations. The most promising method to circumvent this problem is to engineer mechanically stable cartilage ex vivo and to implant that into the damaged tissue area. This review outlines the issues related to the composition and functionality of tissue-engineered cartilage. In particular, the focus will be on the parameters cell source, signaling molecules, scaffolds and mechanical stimulation. In addition, the current status of tissue engineering of cartilage will be discussed, with the focus on extracellular matrix content, structure and its functionality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis is a degenerative joint disease characterized by pain and disability (Temenoff and Mikos 2000). It involves all ages and 70% of people aged >65 have some degree of osteoarthritis (Engel 1968). Natural cartilage repair is limited because the intrinsic regenerative ability of the tissue is low and cartilage lesions in case of trauma or diseases tend to progressively degrade (Hunziker 2002; Buckwalter and Mankin 1998). Current clinical treatment strategies like mosaicplasty, autologous chondrocytes injection and microfracture have varying success rates, but average long-term results are unsatisfactory (Kreuz et al. 2006; Redman et al. 2005; Bentley et al. 2003; Hunziker 2002; Buckwalter and Mankin 1998). A general drawback of these therapeutic strategies is that the newly formed tissue lacks the structural organization of cartilage and has inferior mechanical properties compared to native tissue, and is therefore prone to failure (Hunziker 2009). The contribution that in vitro cartilage tissue engineering can make is to create a more durable and functional replacement of the degenerated tissue, which is therefore more likely to survive the mechanical conditions in a joint after implantation. One ultimate goal in this field of research is to develop a replacement that has a structure and composition resembling native cartilage, yielding similar mechanical behavior and which fully restores joint functionality.
This review will focus on issues related to functionality of tissue-engineered cartilage. First, we discuss the most important parameters for cartilage tissue engineering studies, including cell source, signaling molecules, scaffolds and mechanical stimulation. Second, we will discuss the current status of tissue engineering of cartilage, focusing on ECM content, structure and its functionality. Finally, we identify common limitations and provide further recommendations for future approaches to engineer a cartilage matrix in vitro that can provide a functional replacement of damaged articular cartilage in vivo.
Important parameters for cartilage tissue engineering studies: cell source, signaling molecules, scaffolds and mechanical stimulation
Cell source
The ideal cell source for cartilage tissue engineering is one that can easily be isolated and expanded, and which synthesizes abundant cartilage-specific extra-cellular matrix components, e.g., aggrecan and type II collagen. The most investigated cell sources for their potential in cartilage tissue engineering are chondrocytes and stem cells (for a detailed overview, we refer to Table 1 in Chung and Burdick 2008).
Chondrocytes
Chondrocytes are the most obvious cell source. They are able to produce, maintain and remodel the cartilage ECM in vitro. However, only a small number of autologous chondrocytes are available, and cells harvested from diseased joints are relatively inactive. Unfortunately, chondrocyte expansion in monolayer causes dedifferentiation, characterized by decreased proteoglycan synthesis and type II collagen expression and increased type I collagen expression (Darling and Athanasiou 2005b; Goessler et al. 2004; Goessler et al. 2005). The age of chondrocytes is also an issue that needs to be considered. In most cartilage tissue engineering studies, chondrocytes from immature animals are used, which proliferate faster and have increased chondrogenic potential compared to chondrocytes from older human donors (Hidaka et al. 2006; Pestka et al. 2011). Unfortunately, chondrocytes from older (OA) patients are metabolically less active in vitro (Wenger et al. 2006; Dehne et al. 2009). Even though these limitations can be partly counteracted with altered culture condition,s such as rotating bioreactor cultures (Marlovits et al. 2003), culture in serum-free media (Giannoni et al. 2005), culture with reduced oxygen tension (Foldager et al. 2011; Strobel et al. 2010) and the addition of growth factors (Barbero et al. 2004; Terada et al. 2005), the use of these cells for cartilage repair is not favorable. Another disadvantage of the use of isolated articular chondrocytes is morbidity at the donor site and loss of joint function.
Stem cells
A possible solution for overcoming the limited supply of primary chondrocytes is the use of multipotent stem cells, mainly from bone marrow and adipose tissue. Bone marrow-derived stem cells (BMSCs) can be easily obtained and can be induced to differentiate into cartilage, even after expansion (Song et al. 2004; Boeuf and Richter 2010). Chondrogenic differentiation of BMSCs for cartilage tissue engineering purposes is facilitated by the application of TGF-β in various 3D culture environments (Worster et al. 2001; Mauck et al. 2006; Angele et al. 1999; Li et al. 2005; Coleman et al. 2007; Williams et al. 2003; Meinel et al. 2004; Wang et al. 2005; Chen et al. 2004; Buxton et al. 2011; Alves da Silva et al. 2010). The main limitation of the use of BMSCs for cartilage tissue engineering is that matrix accumulation and the subsequent mechanical properties of BMSC-laden constructs are lower than those of chondrocyte-seeded constructs (Erickson et al. 2009; Mauck et al. 2007; Thorpe et al. 2010; Vinardell et al. 2010). A possible explanation could be that during culture in vitro MSCs increase expression of collagen type X, which is a hypertrophic chondrocyte marker (Barry et al. 2001; Koga et al. 2009). Some reports have shown that the expression of hypertrophic-related genes could lead to cell death or calcification followed by vascularization when implanted (De Bari et al. 2004). Furthermore, MSCs continue to express collagen type I (Steck et al. 2005). Recently, several promising results have been published that show the feasibility of inhibiting collagen type I and X expression and thereby controlling the chondrogenic differentiation pathway of MSCs (Rampersad et al. 2011; Petit et al. 2011; Bian et al. 2011; Fischer et al. 2010).
Adipose-derived stem cells (ADSCs) have been shown to be capable of differentiating into chondrocytes in 3D culture systems in the presence of ascorbate, dexamethasone and TGF-β (Estes and Guilak 2011; Ronziere et al. 2010; Puetzer et al. 2010; Buckley et al. 2010; Diekman et al. 2010). In these studies, production of cartilage-specific matrix components was shown as well as increased mechanical properties. Even though ADSCs are able to differentiate into chondrocytes, their chondrogenic potential is lower compared to BMSCs, which suggests that more research needs to be done to improve the chondrogenic potential of these cells.
Besides bone marrow and adipose tissue, other sources such as muscle, synovium and periosteum are also being investigated for cartilage tissue engineering purposes, all of which have been shown to have chondrogenic potential, but which is still lower compared to BMSCs and/or ADSCs (Salgado et al. 2006; Li et al. 2011; O'Driscoll 1999).
Signaling molecules
Several cytokines, hormones and growth factors are known to influence the anabolic and catabolic processes by chondrocytes. Therefore, a number of growth factors, including transforming growth factor (TGF-β), insulin-like growth factor (IGF-1), bone morphogenetic proteins (BMPs), and to a lesser extent fibroblast growth factors (FGFs) and epidermal growth factor (EGF), have been used in cartilage tissue engineering studies in vitro to promote the chondrogenic phenotype, to stimulate ECM production and to promote chondrogenesis of MSCs (for a detailed overview, we refer to Table 2 in Ahmed and Hincke 2010). Members of the TGF-β superfamily play a major role in cartilage development and repair. Mainly, the isoforms TGF-β1, 2 and 3 enhance chondrocyte proliferation and increase ECM synthesis by chondrocytes (Morales 1991; Bujia et al. 1996; van der Kraan et al. 1992). Further, TGF-β1 and 3 promote chondrogenesis of MSCs (Grimaud et al. 2002; Li et al. 2005; Schulz et al. 2008; Puetzer et al. 2010; Xu et al. 2008). IGF-1 can stimulate the anabolic activity of chondrocytes and can induce chondrogenesis of MSC cell types (Yoon and Fisher 2008; Veilleux and Spector 2005; Kurth et al. 2007; Indrawattana et al. 2004; Fukumoto et al. 2003; Gooch et al. 2001; Seifarth et al. 2009). BMPs, especially BMP-2 and BMP-7, promote chondrogenesis of MSCs and increase matrix production by chondrocytes and MSCs (Kurth et al. 2007; Park et al. 2005; Hicks et al. 2007; Kaps et al. 2002).
Combinations of signaling molecules
Administration of a combination of growth factors to chondrocyte and MSC cultures in vitro may increase their impact. For example, combinations of IGF-1/TGF-β1, IGF-1/TGF-β2, IGF-1/BMP-2 and IGF-1/bFGF/TGF-β2 exerted additive anabolic effects on chondrocytes and stimulated ECM synthesis (Chua et al. 2004; Seifarth et al. 2009; Wiegandt et al. 2007; Elder and Athanasiou 2009; Yasuda et al. 2006). However, other studies have reported that combinations of IGF-1/TGF-β, bFGF/ TGF-β and FGF-2/IGF-1 did not further improve histological features or mechanical performance of the engineered cartilage (Arevalo-Silva et al. 2001; Veilleux and Spector 2005).
Combinations of growth factors have also been used to induce chondrogenic differentiation of MSCs. For example, a combination of IGF-1 and TGF-β1 induced chondrogenic differentiation of MSCs (Xiang et al. 2007) and combinations of TGF-β2/BMP-7, TGFβ2/BMP-6, TGF-β2/BMP-2 and TGF-β2/IGF-1 promoted chondrogenesis of MSCs, with TGF-β2/BMP-7 being most effective (Kim and Im 2009; Im et al. 2006). Also, combinations of TGF-β3 with BMP-2, BMP-4, BMP-6 and IGF-1 have been shown effective, both in monolayer and 3D cultures (Sekiya et al. 2005; Hennig et al. 2007; Indrawattana et al. 2004; Takagi et al. 2007).
Dose and timing of administration
It has become clear that the effect of application of signaling molecules is not only dependent on the type of factor that is applied but other parameters are also involved, such as dose and timing of administration and the cell type on which they act. For example, transient application of TGF-β3 resulted in higher compressive properties and GAG content of chondrocyte-laden hydrogels (Lima et al. 2007; Byers et al. 2008) and MSC-laden constructs (Huang et al. 2009; Mehlhorn et al. 2006; Caterson et al. 2001), compared to continuous application of TGF-β3. It has been suggested that TGF-β may act to ‘prime the pump’, which makes continuous application superfluous. Other studies have employed sequential growth factor addition with the goal of first increasing proliferation within the constructs with a combination of FGF-2/TGF-β1 followed by enhancing matrix production with IGF-1 (Pei et al. 2002). In most cartilage tissue engineering studies, the commonly used concentration of growth factors such as TGF-β, FGF-2 and BMPs is 10 ng/ml (Ahmed and Hincke 2010). However, continuous treatment of chondrocytes in agarose with 1, 2.5, 5 and 10 ng/ml TGF-β resulted in comparable enhancement of both physical and biochemical properties (Byers et al. 2008).
Mechanical stimulation
A well-established cue for improving the mechanical properties of tissue-engineered cartilage is mechanical stimulation. Bioreactors have been developed to apply mechanical loading regimes to cell-seeded constructs (for a detailed overview, we refer to tables and figures in Schulz and Bader 2007). Direct confined or unconfined compression and hydrostatic pressure are the two most investigated loading regimes in cartilage tissue engineering studies. Direct dynamic compression applied to chondrocyte-seeded constructs generally induces increased ECM production and/or proliferation and has been shown to improve compressive properties of the engineered tissue (Bian et al. 2010; Kock et al. 2009; Kelly et al. 2006; Kisiday et al. 2004; Mauck et al. 2002). More recently, dynamic compression has been applied to MSC-seeded constructs, where it stimulated the accretion of cartilage-like extra-cellular matrix (ECM) components relative to unloaded controls (Mauck et al. 2007; Kisiday et al. 2009; Park et al. 2006; Thorpe et al. 2010). Application of hydrostatic pressure in vitro has improved the properties of tissue-engineered cartilage (Hu and Athanasiou 2006b; Miyanishi et al. 2006a, b). However, as with direct compression, the outcomes of these studies depend largely on the loading parameters used. Besides the effect on metabolic activity of the cells, hydrostatic pressure also stimulates the chondrocytic phenotype of chondrocytes in vitro (Candiani et al. 2008; Heyland et al. 2006; Kawanishi et al. 2007). Furthermore, hydrostatic pressure has been used to stimulate chondrogenic differentiation of bone marrow-derived (Luo and Seedhom 2007; Miyanishi et al. 2006a, b; Wagner et al. 2008), adipose-derived (Ogawa et al. 2009), and synovium-derived stem cells (Sakao et al. 2008) with promising results. Other loading regimes that have been investigated are shear loading, sliding/rolling indentation loading, tensile loading, centrifugal force, and gravity (Darling and Athanasiou 2003a, b; Schulz and Bader 2007; Khoshgoftar et al. 2011; Sun et al. 2010; Wimmer et al. 2009) with mixed results. In conclusion, it is necessary to investigate which specific (combinations of) mechanical stimuli, as well as their parameters, result in optimal response of the cells in cultured constructs.
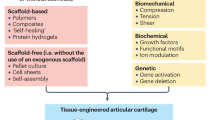
Scaffolds
The goal of the use of biomaterial scaffolds in cartilage tissue engineering is to provide the cells with a comfortable niche which stimulates cells to synthesize cartilage matrix, and to (temporarily) replace the function of the native matrix until new cartilage has formed. To fulfill that function, the scaffold should preferably (1) be biodegradable in a controlled way without toxic byproducts, (2) have a porosity that allows diffusion of nutrients and waste products, (3) support cell viability, proliferation, differentiation and ECM production, (4) be able to fix to and integrate with the tissue at the defect site, and (5) give mechanical support to the engineered tissue. Many natural and synthetic polymers have been used as scaffold material in cartilage tissue engineering (for a detailed overview, we refer to Table 1 in Ahmed and Hincke 2010).
Types of scaffold
Natural polymers can be subdivided into protein-based, such as silk, fibrin and collagen, and carbohydrate based, such agarose, alginate, hyaluronan and chitosan. Many of these are hydrogels, which makes them appropriate for engineering tissues such as cartilage, which have high water content. These can be designed as injectable in liquid form, which mixes well with chondrogenic cells. The most attractive feature of hydrogels is that cells encapsulated in the scaffold maintain their spherical chondrocyte phenotype and do not (de)differentiate. Hydrogels are interesting for studies in which mechanical loading is used, because they are able to transduce mechanical loads such that forces can be exerted on the cells (Spiller et al. 2011). Finally, natural scaffold materials, particularly fabricated by biologics, are believed to permit natural ECM remodeling with construct maturation (Chung et al. 2006; Burdick et al. 2005; Li et al. 2005; Welsch et al. 2010).
The most widely used synthetic polymeric scaffolds in cartilage tissue engineering are the poly-α-hydroxy esters, especially polylactic acid (PLA) and polyglycolic acid (PGA), because of their biodegradability and US Food and Drug Administration (FDA) approval for clinical use (Yoon and Fisher 2006). Scaffolds made of these polymers have better mechanical strength than hydrogels, which makes it easier to fix them in a defect and improves their load-bearing properties (Munirah et al. 2008). In addition, it is easier to modify the properties of these scaffolds, which makes it easier to tune, for example, their degradation characteristics, structure and mechanical strength. A disadvantage of synthetic polymers is that cells often do not maintain their chondrocytic phenotype and produce ECM with inferior properties (Chen et al. 2003).
Scaffold architecture, porosity and stiffness
Porosity, pore size and interconnectivity of scaffold materials are important since these properties influence cell migration and diffusion of oxygen, nutrients, waste products and signaling molecules (Nuernberger et al. 2011). For example, inhomogeneous oxygen delivery from the periphery towards the center of cell-seeded constructs may lead to cell death in the central regions but not in the periphery (Volkmer et al. 2008; Malda et al. 2004; Sengers et al. 2005a, b).
In addition, a porous material improves mechanical interlocking between the implant and the surrounding natural cartilage, providing a greater mechanical stability at the interface. Porosity and permeability have a remarkable effect on proliferation and phenotype of chondrocytes (Lien et al. 2009; Stenhamre et al. 2010; Jeong and Hollister 2010). The pore size for scaffolds to promote proliferation is optimal between 100 and 500 μm (Ikada 2006; Lien et al. 2009). Porosity and architecture can also be used to induce topographical organization. Woodfield et al. (2005) produced a 100% interconnected pores scaffold with pore size gradients, which promoted an inhomogeneous cell distribution and zonal distribution of GAGs and collagen type II.
Stiffness of scaffolds also influences the mechanical environment of the seeded cells which in turn can influence cell differentiation and tissue growth in culture (Kelly and Prendergast 2006). Increasing substrate stiffness influences chondrocyte morphology which changed from a rounded shape with nebulous actin on weaker substrates to a predominantly flat morphology with actin stress fibers on stiffer substrates (Genes et al. 2004). Further, the load on cartilage is a stress and not a strain, hence the strain applied to the cells at first is a function of the scaffold stiffness and then a combination of scaffold and ECM properties as the tissue is produced. For example, high agarose concentrations (3%) yield initially stiffer tissue constructs, presumably due to more efficient retention of matrix products, but long-term tissue properties become significantly inferior to those with 2% agarose (Ng et al. 2005).
Biodegradability
Spatially and temporally controlled degradation of the scaffold can affect production and deposition of new tissue. Optimal degradation kinetics ensures initial stability and shape of the scaffold, but do not hinder new cartilaginous ECM deposition. Several degradable scaffolds have been adopted for cartilage tissue engineering (Freed et al. 1994). It has been shown that scaffolds that degrade slowly lead to increased and more homogeneous ECM deposition compared to fast degrading scaffolds (Meinel et al. 2004; Solchaga et al. 2005; Bryant and Anseth 2002). Further, degradation of the scaffold allows for integration and remodeling of the new tissue into the surrounding cartilage after implantation (Bryant and Anseth 2003). To direct temporal degradation of scaffolds, hydrolytically degradable components (Bryant and Anseth 2003), matrix metalloproteinase (MMP)-sensitive peptides (Lutolf et al. 2003; Park et al. 2004), and exogeneous enzymes (Ng et al. 2009a; Rice and Anseth 2007) have been introduced. For example, Ng et al. (2009a) has shown that controlled degradation of agarose scaffold with the enzyme agarase resulted in increased collagen content and dynamic mechanical properties relative to control over time in culture, which they hypothesize to be the result of enhanced nutrient transport and increased space for collagen fibril development with time of culture. In addition, it has been shown that, in evolving MSC-laden hydrogels with mesh sizes that change over time due to crosslink degradation, GAG and collagen II content were increased, and mechanical properties were superior to non-evolving hydrogels (Chung et al. 2009).
Tissue-engineered cartilage: content, structure and functionality
The joint is mechanically a very demanding environment. For a tissue-engineered cartilage implant to survive those conditions, it needs to have sufficient material properties to withstand or respond to normal joint loading. This does not necessarily mean that the engineered tissue is an exact copy of the natural tissue; the tissue may further develop and adapt properties post-implantation. The questions arise, what exactly are these ‘sufficient material properties’, and how much do we need to improve our current tissue-engineered cartilage.
Proteoglycan content
Several studies have been able to engineer cartilage constructs in vitro with native sGAG content and equilibrium compressive properties (Lima et al. 2006, 2007; Elder and Athanasiou 2008; Bastiaansen-Jenniskens et al. 2008; Waldman et al. 2006). sGAG content and compressive properties improved with increasing culture duration and cell seeding density (Chang et al. 2001; Mauck et al. 2002; Puelacher et al. 1994), and with addition of anabolic growth factors and/or increased serum supplementation (Pei et al. 2002; Gooch et al. 2001; Mauck et al. 2003). Interestingly, the deposition of sGAG was significantly enhanced when dynamic loading was applied to chondrocytes-seeded constructs (Chowdhury et al. 2003; Mauck et al. 2000).
Collagen content
The major shortcoming of tissue-engineered cartilage is believed to be the lack of collagen content and consequently its poor tensile properties. Collagen reaches only 15–35% of the native content after 5–12 weeks (Hu and Athanasiou 2006a; Miot et al. 2006; Eyrich et al. 2007). Culture conditions that have a significant impact on collagen synthesis in vitro include cell source (Waldman et al. 2003), cell seeding density (Williams et al. 2005; Revell et al. 2008), scaffold properties (Woodfield et al. 2005), growth factors (Darling and Athanasiou 2005a; Jenniskens et al. 2006; Blunk et al. 2002) and mechanical stimulation (Mauck et al. 2000; Waldman et al. 2006; Hu and Athanasiou 2006b; Elder et al. 2006; Elder and Athanasiou 2008; Kock et al. 2010). A possible hypothesis that may explain low collagen contents in constructs is that GAGs, which are initially rapidly synthesized, impede increased collagen content. Altered transport pathways of nutrients (Asanbaeva et al. 2007), or reduction of cell straining by environmental loading may cause decreased collagen synthesis. Altered transport of synthesised products (Asanbaeva et al. 2007) or altered extracellular biochemical environment may modulate collagen self-assembly (Saeidi et al. 2009). Finally, altered cellular mechanical stimulation may induce MMP expression, resulting in collagen degradation. Also, collagen type I in vitro degradation has been demonstrated to be strain-dependent (Huang and Yannas 1977), and this likely also holds for collagen type II (Flynn et al. 2010). If so, then it is worthwhile to explore strains in cartilage tissue engineering constructs, to evaluate whether these strain conditions would either prevent or induce enzymatic collagen degradation. In the latter case, we may proceed to seek loading conditions that would prevent collagen degradation from occurring.
Furthermore, the excessive amounts of GAGs compared to collagens in tissue-engineered cartilage are believed to negatively influence tensile properties of the tissue (Responte et al. 2007). Studies involving the application of the enzyme chondroitinase-ABC, which degrades GAGs (Prabhakar et al. 2006) and thus reduces stress on the collagen network, have demonstrated increased tensile properties of cartilage explants (Asanbaeva et al. 2007) and self-assembled tissue-engineered cartilage (Natoli et al. 2009; Bian et al. 2009). This effect is likely due to more or altered crosslinking, larger fibril size or altered fibril orientation (Responte et al. 2007).
Collagen orientation
The importance of the arcade-like collagen structure for the load-bearing properties of native cartilage is well-emphasized in literature (Korhonen and Herzog 2008; Owen and Wayne 2006; Wilson et al. 2007; Shirazi and Shirazi-Adl 2008; Shirazi et al. 2008; Bevill et al. 2010). It is logical to assume that this collagen architecture reproduced in engineered cartilage tissue would lead to superior mechanical properties. However, only a few studies have focused on the importance of depth-dependent material properties in engineered cartilage. However, using depth-dependent scaffold properties or cell sources did not lead to an arcade-like collagen structure (Kim et al. 2003; Malda et al. 2005; Ng et al. 2005, 2006; Klein et al. 2007; Moutos et al. 2007). Mechanical loading could be another stimulus for obtaining an anisotropic distribution of collagen in engineered cartilage. The rationale is that, at birth, cartilage contains a random collagen structure. However, a few months after animals start to walk, cartilage develops its arcade-like structure (van Turnhout et al. 2010). Radial confinement of self-assembled constructs increased collagen organization in the direction perpendicular to the articular surface, with no change in collagen or GAG content (Elder and Athanasiou 2008). Furthermore, using polarized light microscopy, it has been shown that unconfined compression aligns collagen fibers perpendicular to the compressive loading direction (Kelly et al. 2006), i.e. aligned with the direction in which it cyclically elongates due to Poissons effects and incompressibility of the tissue. The strain field generated by applying unconfined compression may be useful to generate a superficial zone with collagen fibers parallel to the surface or higher modulus near the surface (Kelly et al. 2006; Khoshgoftar et al. 2011). However, a physiological collagen network with additional vertical fibers in the deep zone may not be produced by this loading regime, since vertical strains are absent. A numerical study by Khoshgoftar et al. (2011) suggests that a loading regime involving indentation with subsequent sliding of the indenter can stimulate the formation of an appropriate superficial zone with parallel collagen fibers. Adding lateral compression to this loading regime may stimulate the formation of a deep zone with perpendicularly aligned fibers, creating an arcade-like collagen architecture. Currently, in our group, experiments are pending in which this loading regime is applied to chondrocyte-seeded agarose constructs in order to create a physiological collagen network in the engineered cartilage. This particular sliding indentation setup has already been shown to stimulate collagen synthesis in periosteum tissue (Fig. 1) (Kock et al. 2010). In that study, periosteal explants were embedded in between agarose layers, which induced cartilage formation, confirmed by synthesis of sGAG and collagen type II (Fig. 1a, e). Addition of TGF-β1 to the culture medium did not further enhance this chondrogenic response (Fig. 1b, f). Applying sliding indentation only to the periosteum inbetween agarose layers enhanced the production of collagen type I, leading to the formation of fibrous tissue without any evidence of cartilage formation (Fig. 1c, g). However, when stimulated by both TGF-β1 and sliding indentation, collagen production was still enhanced, but now it was collagen type II, while sGAG was found to be similar to TGF-β1 or unloaded samples (Fig. 1d, h).
Sections of cultured periosteal explants, stained with Safranin-O (red, proteoglycans)/Fast Green (blue, collagen) (a–d, magnification ×40) and with antibodies for collagen types I and II (e–h, magnification ×40). Cartilage was produced by the explants between agarose layers, with and without addition of TGF-β1 (a, b) and collagen type II was synthesized in this cartilage (e–f). Only collagen type I was visible in explants that were cultured under tension by dynamic loading and no cartilage was formed (c, g). When dynamic loading was combined with TGF-β1 supplementation, cartilage formation was visible (d) and collagen type II could be seen in the chondrogenic area (h)
Zonal organization
Articular cartilage engineering studies typically use homogeneous cell mixtures from juvenile animals that produce cartilage tissue with large amounts of ECM, but lack zonal organization and structure. Considering the prevalence and importance of zonal variations in normal articular cartilage, recent studies have aimed at engineering cartilage with zonal structure, function, or both. Approaches to mimic the zonal structure and function include cell-based, scaffold-based, a combination of cells and scaffold (hybrid), and methods based on application of depth-dependent strain fields.
Cell-based methods typically replicate the native distribution of chondrocyte populations by isolation of zonal chondrocytes, which are employed in specific regions of a construct and are shown to preserve their zone-specific phenotype and to secrete specific zonal markers (Kim et al. 2003; Klein et al. 2003; Waldman et al. 2003; Schuurman et al. 2009; Malda et al. 2010). However, in those studies, the depth-dependent material properties of the engineered cartilage were generally not comparable to native cartilage (Klein et al. 2007).
Scaffold-based methods include porous gradient scaffolds and multilayer hydrogels. An anisotropic pore architecture within 3D PEGT/PBT copolymer scaffolds developed using a 3D fiber deposition technique promoted anisotropic cell distribution, and GAGs and collagen type II distribution, like that in the superficial, middle, and lower zones of immature bovine articular cartilage (Woodfield et al. 2005). Other studies have used bi- or multilayered hydrogels to support the cartilage production by the different zonal subpopulations. Using zonal populations of chondrocytes seeded into layers of 2 and 3% agarose, bi-layered cartilage constructs were produced with zonal chondrocyte organization and depth-dependent biochemical content, qualitatively similar to native cartilage (Ng et al. 2009b). Interestingly, this depth-dependent effect was not seen when full-depth chondrocytes were used in the same culture set-up, emphasizing the need for cells with typical zonal characteristics (Ng et al. 2005). Very recently, hydrogel-based bio-printing approaches have become available which provide organization via both scaffold architecture and controlled deposition of cells at predefined locations (Klein et al. 2009a, b; Cohen et al. 2006).
Recently, researchers have combined cell- and scaffold-based methods to induce spatially-varying properties into tissue-engineered cartilage constructs. Nguyen et al. (2011a, b) demonstrated that layer-by-layer organization of specific combinations of natural and synthetic biomaterials can direct MSCs to differentiate into zone-specific chondrocytes and creates a native-like articular cartilage with mechanical and biochemical properties varying with depth.
A different approach to induce depth-varying inhomogeneity within chondrocyte-seeded agarose constructs is based on application of mechanical loading. We hypothesized that by applying depth-dependent mechanical cues to the chondrocytes, the tissue would be stimulated to form depth-dependent material properties. For this, we developed a custom-built bioreactor that indents constructs with a bar, which moves over the construct without relieving the indentation strain, a loading regime we refer to as sliding indentation (Kock et al. 2010). The sliding indentation protocol induced depth-dependent ECM deposition, leading to the highest GAG content in the top half of the construct (Fig. 2), which receives high strains according to numerical simulations (Khoshgoftar et al. 2011). This confirms the hypothesis that depth-dependent mechanical cues give rise to depth-dependent matrix content. Currently, experiments are running to further investigate the effect of depth-dependent strain magnitudes and orientations on collagen production and orientation, since this is the major depth-varying component in articular cartilage, which is known to significantly contribute to the mechanical properties of the tissue.
Sliding with an indenter over an chondrocyte-seeded agarose construct (1). The sliding indentation protocol led to a depth-dependent strain field (maximal principal strains) (2), with highest strains in the superficial zone (SZ) and the middle zone (MZ) and lowest strains in the deep zone (DZ). The sliding indentation protocol induced depth-dependent ECM deposition (3), leading to the highest GAG content in the top half of the construct (SZ and MZ), which receives high strains according to numerical simulations. *p < 0.0017
Conclusions and future directions
Current treatments for in vivo repair of articular cartilage damage, including mosaicplasty, microfracture, and autologous chondrocytes injection, have successfully been shown to relieve pain and improve joint function, but long-term results are unsatisfactory. The major drawback of these methods is that these mostly result in the formation of fibrocartilage with inferior mechanical properties, which is likely to degrade over time because of its insufficient load-bearing capacity. Tissue engineering has been proposed as a promising solution to circumvent this problem. The major advantages of engineering cartilage in vitro are that culture conditions can be precisely controlled and that its material properties can be evaluated during culture, in contrast to in vivo approaches which greatly depend on the conditions at the donor site. Implantation of a construct with properties that enable it to withstand in vivo loads will have a higher probability for success.
In the past decades, enormous progress has been made in the optimization of strategies for tissue engineering of functional articular cartilage. However, there are still many issues to be addressed before engineered cartilage can be used as a clinical therapy. Finding an optimal cell source is the first critical issue. Although primary native chondrocytes perform best, their limited availability makes their use unrealistic. Preventing loss of phenotype when chondrocytes are expanded is a major challenge. Stem cells seem to be a promising alternative, but they produce cartilage tissue with inferior properties compared to chondrocytes. In the next years, it will become clear whether, and if so which, stem cells could be the optimal cell source for cartilage tissue engineering studies. The second issue involves the choice for scaffold material. Natural and synthetic materials have been investigated, but until now none of these fulfill all the necessary requirements. Third, appropriate biochemical and/or mechanical triggers for matrix production and tissue organization are needed. It remains challenging to derive optimal stimuli that can promote proliferation and differentiation of cells and stimulate the synthesis of proper and sufficient ECM components and the secretion of enzymes that can remodel the produced ECM.
In this respect, the most important questions that remain are: which characteristics should the engineered cartilage possess in order to function as well as the healthy tissue, and how do we get there? It is clear that ECM content is important, but it is unclear to what extent we need to reproduce the native matrix components in engineered cartilage implants pre-implantation. It is possible to obtain native amounts of GAG in engineered cartilage, but collagen content is still far below native. In our opinion, future research should particularly focus on approaches to increase collagen content, which is essential for proper mechanical functioning of the tissue. Further, in order for tissue-engineered cartilage to be mechanically functional, we think that it is essential that the depth-dependent matrix organization, especially the arcade-like collagen architecture, should be reproduced to some extent. But how can this be best achieved? Some attempts have been made, but the native structural ECM organization has not yet been reproduced. Finally, for successful repair, complete integration of the neo-cartilage with the surrounding tissue is required, which is an aspect that demands opposite properties from those required for mechanical load bearing.
Exploring all these different aspects experimentally will be challenging, costly and time-consuming. We would progress faster if we could reduce the number of experimental conditions to explore. This may be achieved if we could refine or enhance the interpretation of experimental results, or if we were able to predict the outcome of particular experimental conditions and thereby discriminate promising protocols from those with poor potential. One way to achieve this is through theoretical modeling (Fig. 3). Models may provide insight into aspects that are difficult to assess during the experiment. For example, the profiles of glucose, lactate and oxygen throughout a tissue engineering construct in time are difficult to measure, but can be computed based on nutrient utilization data. These computed profiles allowed extended interpretation of measurements related to compromised nutrition in the core of engineered cartilage (Sengers et al. 2005b), and explained why mixing of culture medium in rotating wall vessel bioreactors partly compensates for this compromised nutrition (Sengers et al. 2005a). Numerical studies have also been dedicated to understanding how mechanical loading applied at the macroscopic level would perturb chondrocytes at the microscopic level. These perturbations depend on the properties of the scaffold (Appelman et al. 2011) and the pericellular matrix (Guilak and Mow 2000). The premise is that such insight could be used to optimize scaffold properties, or the mechanical stimulation protocols for tissue engineering. However, application of these insights is difficult, because the cellular microenvironment changes with time during tissue development. To incorporate cartilage matrix development is a major challenge that modelers are currently exploring (Sengers et al. 2004; Klisch et al. 2008; van Donkelaar et al. 2011). Models that take into account the actual, measurable tissue composition (Wilson et al. 2006; Klisch et al. 2008) are of particular interest, because these allow direct translation between predicted proteoglycan and collagen contents and biochemical data, or between predicted matrix distributions and histology. The next step in these developments is to add effects of mechanical perturbation to these growth and development models, in order to predict tissue content, distribution, and collagen orientation depending on the applied loading protocol (Khoshgoftar et al. 2011). Once this has been established, it will be possible to predict the effects of loading protocols on functional tissue development. Such predictions may lead to the design of promising tissue engineering protocols, and reduce the number of experiments with poor potential (Fig. 4).
Outlook on the approaches for tissue engineering of cartilage with sufficient ECM amounts, ECM organization and mechanical properties. The traditional approach relies on experimentally exploring the effect of (a combination of) different input parameters (1, 2). These experiments are very time consuming, labor intensive and therefore expensive. We propose a computer-aided approach which includes theoretical and computational evaluation of the influence of different input parameters in a modeling approach (3). With such models, it is possible to discriminate promising protocols from those with poor potential via in silico experiments. In addition, the outcome of experiments could be used for optimization and validation of the theoretical and computational models (4). This approach is less based on trial and error, less time consuming and therefore cheaper
Determining optimized mechanical loading regimes for engineering functional cartilage involves understanding how mechanical loading at the macroscopic levels perturbs cells at the microscopic level, how that perturbation stimulates the chondrocyte to adjust its pericellular matrix by matrix turnover, and how that microscopic tissue development modulates the functional properties at the macroscopic scale. Ultimately, modeling will need to cross these scales to predict how mechanical perturbation would modulate tissue properties with time of culture
In summary, cell source, scaffolds, signaling molecules and mechanical loading are considered to be the most important parameters to optimize for improved tissue engineering cartilage. Ultimately, the combination of these factors should result in mechanically functional tissue-engineered cartilage with sufficient collagen content and depth-dependent matrix organization, which can be implanted and which will withstand the mechanically demanding in vivo environment. Cell source and signaling molecules may be essential to enhance total matrix contents. However, these are not likely to trigger tissue orientation. Therefore, we postulate that only by controlling the mechanical cues will we be able to engineer a cartilage with its particular collagen fiber orientation and inhomogeneous matrix distribution.
References
Ahmed TAE, Hincke MT (2010) Strategies for articular cartilage lesion repair and functional restoration. Tissue Eng Part B Rev 16:305–329
Alves da Silva ML, Martins A, Costa-Pinto AR, Costa P, Faria S, Gomes M, Reis RL, Neves NM (2010) Cartilage tissue engineering using electrospun PCL nanofiber meshes and MSCs. Biomacromolecules 11:3228–3236
Angele P, Kujat R, Nerlich M, Yoo J, Goldberg V, Johnstone B (1999) Engineering of osteochondral tissue with bone marrow mesenchymal progenitor cells in a derivatized hyaluronan-gelatin composite sponge. Tissue Eng 5:545–554
Appelman TP, Mizrahi J, Seliktar D (2011) A finite element model of cell-matrix interactions to study the differential effect of scaffold composition on chondrogenic response to mechanical stimulation. J Biomech Eng 133:041010
Arevalo-Silva CA, Cao Y, Weng Y, Vacanti M, Rodriguez A, Vacanti CA, Eavey RD (2001) The effect of fibroblast growth factor and transforming growth factor-beta on porcine chondrocytes and tissue-engineered autologous elastic cartilage. Tissue Eng 7:81–88
Asanbaeva A, Masuda K, Thonar EJM, Klisch SM, Sah RL (2007) Mechanisms of cartilage growth: modulation of balance between proteoglycan and collagen in vitro using chondroitinase ABC. Arthritis Rheum 56:188–198
Barbero A, Grogan S, Schafer D, Heberer M, Mainil-Varlet P, Martin I (2004) Age related changes in human articular chondrocyte yield, proliferation and post-expansion chondrogenic capacity. Osteoarthr Cartil 12:476–484
Barry F, Boynton RE, Liu B, Murphy JM (2001) Chondrogenic differentiation of mesenchymal stem cells from bone marrow: differentiation-dependent gene expression of matrix components. Exp Cell Res 268:189–200
Bastiaansen-Jenniskens YM, Koevoet W, de Bart ACW, van der Linden JC, Zuurmond AM, Weinans H, Verhaar JAN, van Osch GJVM, Degroot J (2008) Contribution of collagen network features to functional properties of engineered cartilage. Osteoarthr Cartil 16:359–366
Bentley G, Biant LC, Carrington RWJ, Akmal M, Goldberg A, Williams AM, Skinner JA, Pringle J (2003) A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br 85:223–230
Bevill SL, Thambyah A, Broom ND (2010) New insights into the role of the superficial tangential zone in influencing the microstructural response of articular cartilage to compression. Osteoarthr Cartil 18:1310–1318
Bian L, Crivello KM, Ng KW, Xu D, Williams DY, Ateshian GA, Hung CT (2009) Influence of temporary chondroitinase ABC-induced glycosaminoglycan suppression on maturation of tissue-engineered cartilage. Tissue Eng Part A 15:2065–2072
Bian L, Fong JV, Lima EG, Stoker AM, Ateshian GA, Cook JL, Hung CT (2010) Dynamic mechanical loading enhances functional properties of tissue-engineered cartilage using mature canine chondrocytes. Tissue Eng Part A 16:1781–1790
Bian L, Zhai DY, Mauck RL, Burdick JA (2011) Coculture of human mesenchymal stem cells and articular chondrocytes reduces hypertrophy and enhances functional properties of engineered cartilage. Tissue Eng Part A 17:1137–1145
Blunk T, Sieminski AL, Gooch KJ, Courter DL, Hollander AP, Nahir AM, Langer R, Vunjak-Novakovic G, Freed LE (2002) Differential effects of growth factors on tissue-engineered cartilage. Tissue Eng 8:73–84
Boeuf S, Richter W (2010) Chondrogenesis of mesenchymal stem cells: role of tissue source and inducing factors. Stem Cell Res Ther 1:31
Bryant SJ, Anseth KS (2002) Hydrogel properties influence ECM production by chondrocytes photoencapsulated in poly(ethylene glycol) hydrogels. J Biomed Mater Res 59:63–72
Bryant SJ, Anseth KS (2003) Controlling the spatial distribution of ECM components in degradable PEG hydrogels for tissue engineering cartilage. J Biomed Mater Res A 64:70–79
Buckley CT, Vinardell T, Thorpe SD, Haugh MG, Jones E, McGonagle D, Kelly DJ (2010) Functional properties of cartilaginous tissues engineered from infrapatellar fat pad-derived mesenchymal stem cells. J Biomech 43:920–926
Buckwalter JA, Mankin HJ (1998) Articular cartilage repair and transplantation. Arthritis Rheum 41:1331–1342
Bujia J, Pitzke P, Kastenbauer E, Wilmes E, Hammer C (1996) Effect of growth factors on matrix synthesis by human nasal chondrocytes cultured in monolayer and in agar. Eur Arch Otorhinolaryngol 253:336–340
Burdick JA, Chung C, Jia X, Randolph MA, Langer R (2005) Controlled degradation and mechanical behavior of photopolymerized hyaluronic acid networks. Biomacromolecules 6:386–391
Buxton AN, Bahney CS, Yoo JU, Johnstone B (2011) Temporal exposure to chondrogenic factors modulates human mesenchymal stem cell chondrogenesis in hydrogels. Tissue Eng Part A 17:371–380
Byers BA, Mauck RL, Chiang IE, Tuan RS (2008) Transient exposure to transforming growth factor beta 3 under serum-free conditions enhances the biomechanical and biochemical maturation of tissue-engineered cartilage. Tissue Eng Part A 14:1821–1834
Candiani G, Raimondi MT, Aurora R, Lagana' K, Dubini G (2008) Chondrocyte response to high regimens of cyclic hydrostatic pressure in 3-dimensional engineered constructs. Int J Artif Organs 31:490–499
Caterson EJ, Nesti LJ, Li WJ, Danielson KG, Albert TJ, Vaccaro AR, Tuan RS (2001) Three-dimensional cartilage formation by bone marrow-derived cells seeded in polylactide/alginate amalgam. J Biomed Mater Res 57:394–403
Chang SC, Rowley JA, Tobias G, Genes NG, Roy AK, Mooney DJ, Vacanti CA, Bonassar LJ (2001) Injection molding of chondrocyte/alginate constructs in the shape of facial implants. J Biomed Mater Res 55:503–511
Chen G, Sato T, Ushida T, Hirochika R, Shirasaki Y, Ochiai N, Tateishi T (2003) The use of a novel PLGA fiber/collagen composite web as a scaffold for engineering of articular cartilage tissue with adjustable thickness. J Biomed Mater Res A 67:1170–1180
Chen G, Liu D, Tadokoro M, Hirochika R, Ohgushi H, Tanaka J, Tateishi T (2004) Chondrogenic differentiation of human mesenchymal stem cells cultured in a cobweb-like biodegradable scaffold. Biochem Biophys Res Commun 322:50–55
Chowdhury TT, Bader DL, Shelton JC, Lee DA (2003) Temporal regulation of chondrocyte metabolism in agarose constructs subjected to dynamic compression. Arch Biochem Biophys 417:105–111
Chua KH, Aminuddin BS, Fuzina NH, Ruszymah BHI (2004) Interaction between insulin-like growth factor-1 with other growth factors in serum depleted culture medium for human cartilage engineering. Med J Malaysia 59:7–8
Chung C, Burdick JA (2008) Engineering cartilage tissue. Adv Drug Deliv Rev 60:243–262
Chung C, Mesa J, Randolph MA, Yaremchuk M, Burdick JA (2006) Influence of gel properties on neocartilage formation by auricular chondrocytes photoencapsulated in hyaluronic acid networks. J Biomed Mater Res A 77:518–525
Chung C, Beecham M, Mauck RL, Burdick JA (2009) The influence of degradation characteristics of hyaluronic acid hydrogels on in vitro neocartilage formation by mesenchymal stem cells. Biomaterials 30:4287–4296
Cohen DL, Malone E, Lipson H, Bonassar LJ (2006) Direct freeform fabrication of seeded hydrogels in arbitrary geometries. Tissue Eng 12:1325–1335
Coleman RM, Case ND, Guldberg RE (2007) Hydrogel effects on bone marrow stromal cell response to chondrogenic growth factors. Biomaterials 28:2077–2086
Darling EM, Athanasiou KA (2003a) Articular cartilage bioreactors and bioprocesses. Tissue Eng 9:9–26
Darling EM, Athanasiou KA (2003b) Biomechanical strategies for articular cartilage regeneration. Ann Biomed Eng 31:1114–1124
Darling EM, Athanasiou KA (2005a) Growth factor impact on articular cartilage subpopulations. Cell Tissue Res 322:463–473
Darling EM, Athanasiou KA (2005b) Rapid phenotypic changes in passaged articular chondrocyte subpopulations. J Orthop Res 23:425–432
De Bari C, Dell'Accio F, Luyten FP (2004) Failure of in vitro-differentiated mesenchymal stem cells from the synovial membrane to form ectopic stable cartilage in vivo. Arthritis Rheum 50:142–150
Dehne T, Karlsson C, Ringe J, Sittinger M, Lindahl A (2009) Chondrogenic differentiation potential of osteoarthritic chondrocytes and their possible use in matrix-associated autologous chondrocyte transplantation. Arthritis Res Ther 11:R133
Diekman BO, Rowland CR, Lennon DP, Caplan AI, Guilak F (2010) Chondrogenesis of adult stem cells from adipose tissue and bone marrow: induction by growth factors and cartilage-derived matrix. Tissue Eng Part A 16:523–533
Elder BD, Athanasiou KA (2008) Effects of confinement on the mechanical properties of self-assembled articular cartilage constructs in the direction orthogonal to the confinement surface. J Orthop Res 26:238–246
Elder BD, Athanasiou KA (2009) Systematic assessment of growth factor treatment on biochemical and biomechanical properties of engineered articular cartilage constructs. Osteoarthr Cartil 17:114–123
Elder SH, Sanders SW, McCulley WR, Marr ML, Shim JW, Hasty KA (2006) Chondrocyte response to cyclic hydrostatic pressure in alginate versus pellet culture. J Orthop Res 24:740–747
Engel A (1968) Osteoarthritis and body measurements. Vital Health Stat 11: 1–37
Erickson IE, Huang AH, Chung C, Li RT, Burdick JA, Mauck RL (2009) Differential maturation and structure-function relationships in mesenchymal stem cell- and chondrocyte-seeded hydrogels. Tissue Eng Part A 15:1041–1052
Estes BT, Guilak F (2011) Three-dimensional culture systems to induce chondrogenesis of adipose-derived stem cells. Methods Mol Biol 702:201–217
Eyrich D, Wiese H, Maier G, Skodacek D, Appel B, Sarhan H, Tessmar J, Staudenmaier R, Wenzel MM, Goepferich A, Blunk T (2007) In vitro and in vivo cartilage engineering using a combination of chondrocyte-seeded long-term stable fibrin gels and polycaprolactone-based polyurethane scaffolds. Tissue Eng 13:2207–2218
Fischer J, Dickhut A, Rickert M, Richter W (2010) Human articular chondrocytes secrete parathyroid hormone-related protein and inhibit hypertrophy of mesenchymal stem cells in coculture during chondrogenesis. Arthritis Rheum 62:2696–2706
Flynn BP, Bhole AP, Saeidi N, Liles M, Dimarzio CA, Ruberti JW (2010) Mechanical strain stabilizes reconstituted collagen fibrils against enzymatic degradation by mammalian collagenase matrix metalloproteinase 8 (MMP-8). PLoS One 5:e12337
Foldager CB, Nielsen AB, Munir S, Ulrich-Vinther M, Soballe K, Bunger C, Lind M (2011) Combined 3D and hypoxic culture improves cartilage-specific gene expression in human chondrocytes. Acta Orthop 82:234–240
Freed LE, Vunjak-Novakovic G, Biron RJ, Eagles DB, Lesnoy DC, Barlow SK, Langer R (1994) Biodegradable polymer scaffolds for tissue engineering. Biotechnology (N Y) 12:689–693
Fukumoto T, Sperling JW, Sanyal A, Fitzsimmons JS, Reinholz GG, Conover CA, O'Driscoll SW (2003) Combined effects of insulin-like growth factor-1 and transforming growth factor-beta1 on periosteal mesenchymal cells during chondrogenesis in vitro. Osteoarthr Cartil 11:55–64
Genes NG, Rowley JA, Mooney DJ, Bonassar LJ (2004) Effect of substrate mechanics on chondrocyte adhesion to modified alginate surfaces. Arch Biochem Biophys 422:161–167
Giannoni P, Pagano A, Maggi E, Arbico R, Randazzo N, Grandizio M, Cancedda R, Dozin B (2005) Autologous chondrocyte implantation (ACI) for aged patients: development of the proper cell expansion conditions for possible therapeutic applications. Osteoarthr Cartil 13:589–600
Goessler UR, Bugert P, Bieback K, Baisch A, Sadick H, Verse T, Kluter H, Hormann K, Riedel F (2004) Expression of collagen and fiber-associated proteins in human septal cartilage during in vitro dedifferentiation. Int J Mol Med 14:1015–1022
Goessler UR, Bieback K, Bugert P, Naim R, Schafer C, Sadick H, Hormann K, Riedel F (2005) Human chondrocytes differentially express matrix modulators during in vitro expansion for tissue engineering. Int J Mol Med 16:509–515
Gooch KJ, Blunk T, Courter DL, Sieminski AL, Bursac PM, Vunjak-Novakovic G, Freed LE (2001) IGF-I and mechanical environment interact to modulate engineered cartilage development. Biochem Biophys Res Commun 286:909–915
Grimaud E, Heymann D, Redini F (2002) Recent advances in TGF-beta effects on chondrocyte metabolism. Potential therapeutic roles of TGF-beta in cartilage disorders. Cytokine Growth Factor Rev 13:241–257
Guilak F, Mow VC (2000) The mechanical environment of the chondrocyte: a biphasic finite element model of cell-matrix interactions in articular cartilage. J Biomech 33:1663–1673
Hennig T, Lorenz H, Thiel A, Goetzke K, Dickhut A, Geiger F, Richter W (2007) Reduced chondrogenic potential of adipose tissue derived stromal cells correlates with an altered TGFbeta receptor and BMP profile and is overcome by BMP-6. J Cell Physiol 211:682–691
Heyland J, Wiegandt K, Goepfert C, Nagel-Heyer S, Ilinich E, Schumacher U, Portner R (2006) Redifferentiation of chondrocytes and cartilage formation under intermittent hydrostatic pressure. Biotechnol Lett 28:1641–1648
Hicks DL, Sage AB, Shelton E, Schumacher BL, Sah RL, Watson D (2007) Effect of bone morphogenetic proteins 2 and 7 on septal chondrocytes in alginate. Otolaryngol Head Neck Surg 136:373–379
Hidaka C, Cheng C, Alexandre D, Bhargava M, Torzilli PA (2006) Maturational differences in superficial and deep zone articular chondrocytes. Cell Tissue Res 323:127–135
Hu JC, Athanasiou KA (2006a) A self-assembling process in articular cartilage tissue engineering. Tissue Eng 12:969–979
Hu JC, Athanasiou KA (2006b) The effects of intermittent hydrostatic pressure on self-assembled articular cartilage constructs. Tissue Eng 12:1337–1344
Huang C, Yannas IV (1977) Mechanochemical studies of enzymatic degradation of insoluble collagen fibers. J Biomed Mater Res 11:137–154
Huang AH, Stein A, Tuan RS, Mauck RL (2009) Transient exposure to transforming growth factor beta 3 improves the mechanical properties of mesenchymal stem cell-laden cartilage constructs in a density-dependent manner. Tissue Eng Part A 15:3461–3472
Hunziker EB (2002) Articular cartilage repair: basic science and clinical progress. A review of the current status and prospects. Osteoarthr Cartil 10:432–463
Hunziker EB (2009) The elusive path to cartilage regeneration. Adv Mater 21:3419–3424
Ikada Y (2006) Challenges in tissue engineering. J R Soc Interface 3:589–601
Im GI, Jung NH, Tae SK (2006) Chondrogenic differentiation of mesenchymal stem cells isolated from patients in late adulthood: the optimal conditions of growth factors. Tissue Eng 12:527–536
Indrawattana N, Chen G, Tadokoro M, Shann LH, Ohgushi H, Tateishi T, Tanaka J, Bunyaratvej A (2004) Growth factor combination for chondrogenic induction from human mesenchymal stem cell. Biochem Biophys Res Commun 320:914–919
Jenniskens YM, Koevoet W, de Bart ACW, Weinans H, Jahr H, Verhaar JAN, Degroot J, van Osch GJVM (2006) Biochemical and functional modulation of the cartilage collagen network by IGF1, TGFbeta2 and FGF2. Osteoarthr Cartil 14:1136–1146
Jeong CG, Hollister SJ (2010) Mechanical and biochemical assessments of three-dimensional poly(1,8-octanediol-co-citrate) scaffold pore shape and permeability effects on in vitro chondrogenesis using primary chondrocytes. Tissue Eng Part A 16:3759–3768
Kaps C, Bramlage C, Smolian H, Haisch A, Ungethum U, Burmester GR, Sittinger M, Gross G, Haupl T (2002) Bone morphogenetic proteins promote cartilage differentiation and protect engineered artificial cartilage from fibroblast invasion and destruction. Arthritis Rheum 46:149–162
Kawanishi M, Oura A, Furukawa K, Fukubayashi T, Nakamura K, Tateishi T, Ushida T (2007) Redifferentiation of dedifferentiated bovine articular chondrocytes enhanced by cyclic hydrostatic pressure under a gas-controlled system. Tissue Eng 13:957–964
Kelly DJ, Prendergast PJ (2006) Prediction of the optimal mechanical properties for a scaffold used in osteochondral defect repair. Tissue Eng 12:2509–2519
Kelly TA, Ng KW, Wang CCB, Ateshian GA, Hung CT (2006) Spatial and temporal development of chondrocyte-seeded agarose constructs in free-swelling and dynamically loaded cultures. J Biomech 39:1489–1497
Khoshgoftar M, van Donkelaar CC, Ito K (2011) Mechanical stimulation to stimulate formation of a physiological collagen architecture in tissue-engineered cartilage: a numerical study. Comput Methods Biomech Biomed Engin 14:135–144
Kim HJ, Im GI (2009) Combination of transforming growth factor-beta2 and bone morphogenetic protein 7 enhances chondrogenesis from adipose tissue-derived mesenchymal stem cells. Tissue Eng Part A 15:1543–1551
Kim TK, Sharma B, Williams CG, Ruffner MA, Malik A, McFarland EG, Elisseeff JH (2003) Experimental model for cartilage tissue engineering to regenerate the zonal organization of articular cartilage. Osteoarthr Cartil 11:653–664
Kisiday JD, Jin M, DiMicco MA, Kurz B, Grodzinsky AJ (2004) Effects of dynamic compressive loading on chondrocyte biosynthesis in self-assembling peptide scaffolds. J Biomech 37:595–604
Kisiday JD, Frisbie DD, McIlwraith CW, Grodzinsky AJ (2009) Dynamic compression stimulates proteoglycan synthesis by mesenchymal stem cells in the absence of chondrogenic cytokines. Tissue Eng Part A 15:2817–2824
Klein TJ, Schumacher BL, Schmidt TA, Li KW, Voegtline MS, Masuda K, Thonar EJM, Sah RL (2003) Tissue engineering of stratified articular cartilage from chondrocyte subpopulations. Osteoarthr Cartil 11:595–602
Klein TJ, Chaudhry M, Bae WC, Sah RL (2007) Depth-dependent biomechanical and biochemical properties of fetal, newborn, and tissue-engineered articular cartilage. J Biomech 40:182–190
Klein TJ, Malda J, Sah RL, Hutmacher DW (2009a) Tissue engineering of articular cartilage with biomimetic zones. Tissue Eng Part B Rev 15:143–157
Klein TJ, Rizzi SC, Reichert JC, Georgi N, Malda J, Schuurman W, Crawford RW, Hutmacher DW (2009b) Strategies for zonal cartilage repair using hydrogels. Macromol Biosci 9:1049–1058
Klisch SM, Asanbaeva A, Oungoulian SR, Masuda K, Thonar EJM, Davol A, Sah RL (2008) A cartilage growth mixture model with collagen remodeling: validation protocols. J Biomech Eng 130:031006
Kock LM, Schulz RM, van Donkelaar CC, Thummler CB, Bader A, Ito K (2009) RGD-dependent integrins are mechanotransducers in dynamically compressed tissue-engineered cartilage constructs. J Biomech 42:2177–2182
Kock LM, Ravetto A, van Donkelaar CC, Foolen J, Emans PJ, Ito K (2010) Tuning the differentiation of periosteum-derived cartilage using biochemical and mechanical stimulations. Osteoarthr Cartil 18:1528–1535
Koga H, Engebretsen L, Brinchmann JE, Muneta T, Sekiya I (2009) Mesenchymal stem cell-based therapy for cartilage repair: a review. Knee Surg Sports Traumatol Arthrosc 17:1289–1297
Korhonen RK, Herzog W (2008) Depth-dependent analysis of the role of collagen fibrils, fixed charges and fluid in the pericellular matrix of articular cartilage on chondrocyte mechanics. J Biomech 41:480–485
Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M, Sudkamp N (2006) Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthr Cartil 14:1119–1125
Kurth T, Hedbom E, Shintani N, Sugimoto M, Chen FH, Haspl M, Martinovic S, Hunziker EB (2007) Chondrogenic potential of human synovial mesenchymal stem cells in alginate. Osteoarthr Cartil 15:1178–1189
Li W-JW-J, Tuli R, Okafor C, Derfoul A, Danielson KGK, Hall DJD, Tuan RSR (2005) A three-dimensional nanofibrous scaffold for cartilage tissue engineering using human mesenchymal stem cells. Biomaterials 26:599–609
Li Q, Tang J, Wang R, Bei C, Xin L, Zeng Y, Tang X (2011) Comparing the chondrogenic potential in vivo of autogeneic mesenchymal stem cells derived from different tissues. Artif Cells Blood Substit Immobil Biotechnol 39:31–38
Lien SM, Ko LY, Huang TJ (2009) Effect of pore size on ECM secretion and cell growth in gelatin scaffold for articular cartilage tissue engineering. Acta Biomater 5:670–679
Lima EG, Bian L, Mauck RL, Byers BA, Tuan RS, Ateshian GA, Hung CT (2006) The effect of applied compressive loading on tissue-engineered cartilage constructs cultured with TGF-beta3. Conf Proc IEEE Eng Med Biol Soc 1:779–782
Lima EG, Bian L, Ng KW, Mauck RL, Byers BA, Tuan RS, Ateshian GA, Hung CT (2007) The beneficial effect of delayed compressive loading on tissue-engineered cartilage constructs cultured with TGF-beta3. Osteoarthr Cartil 15:1025–1033
Luo ZJ, Seedhom BB (2007) Light and low-frequency pulsatile hydrostatic pressure enhances extracellular matrix formation by bone marrow mesenchymal cells: an in-vitro study with special reference to cartilage repair. Proc Inst Mech Eng H 221:499–507
Lutolf MP, Lauer-Fields JL, Schmoekel HG, Metters AT, Weber FE, Fields GB, Hubbell JA (2003) Synthetic matrix metalloproteinase-sensitive hydrogels for the conduction of tissue regeneration: engineering cell-invasion characteristics. Proc Natl Acad Sci USA 100:5413–5418
Malda J, Rouwkema J, Martens DE, Le Comte EP, Kooy FK, Tramper J, van Blitterswijk CA, Riesle J (2004) Oxygen gradients in tissue-engineered PEGT/PBT cartilaginous constructs: measurement and modeling. Biotechnol Bioeng 86:9–18
Malda J, Woodfield TBF, van der Vloodt F, Wilson C, Martens DE, Tramper J, van Blitterswijk CA, Riesle J (2005) The effect of PEGT/PBT scaffold architecture on the composition of tissue engineered cartilage. Biomaterials 26:63–72
Malda J, ten Hoope W, Schuurman W, van Osch GJVM, van Weeren PR, Dhert WJA (2010) Localization of the potential zonal marker clusterin in native cartilage and in tissue-engineered constructs. Tissue Eng Part A 16:897–904
Marlovits S, Tichy B, Truppe M, Gruber D, Vecsei V (2003) Chondrogenesis of aged human articular cartilage in a scaffold-free bioreactor. Tissue Eng 9:1215–1226
Mauck RL, Soltz MA, Wang CC, Wong DD, Chao PH, Valhmu WB, Hung CT, Ateshian GA (2000) Functional tissue engineering of articular cartilage through dynamic loading of chondrocyte-seeded agarose gels. J Biomech Eng 122:252–260
Mauck RL, Seyhan SL, Ateshian GA, Hung CT (2002) Influence of seeding density and dynamic deformational loading on the developing structure/function relationships of chondrocyte-seeded agarose hydrogels. Ann Biomed Eng 30:1046–1056
Mauck RL, Nicoll SB, Seyhan SL, Ateshian GA, Hung CT (2003) Synergistic action of growth factors and dynamic loading for articular cartilage tissue engineering. Tissue Eng 9:597–611
Mauck RL, Yuan X, Tuan RS (2006) Chondrogenic differentiation and functional maturation of bovine mesenchymal stem cells in long-term agarose culture. Osteoarthr Cartil 14:179–189
Mauck RL, Byers BA, Yuan X, Tuan RS (2007) Regulation of cartilaginous ECM gene transcription by chondrocytes and MSCs in 3D culture in response to dynamic loading. Biomech Model Mechanobiol 6:113–125
Mehlhorn AT, Schmal H, Kaiser S, Lepski G, Finkenzeller G, Stark GB, Sudkamp NP (2006) Mesenchymal stem cells maintain TGF-beta-mediated chondrogenic phenotype in alginate bead culture. Tissue Eng 12:1393–1403
Meinel L, Hofmann S, Karageorgiou V, Zichner L, Langer R, Kaplan D, Vunjak-Novakovic G (2004) Engineering cartilage-like tissue using human mesenchymal stem cells and silk protein scaffolds. Biotechnol Bioeng 88:379–391
Miot S, Scandiucci de Freitas P, Wirz D, Daniels AU, Sims TJ, Hollander AP, Mainil-Varlet P, Heberer M, Martin I (2006) Cartilage tissue engineering by expanded goat articular chondrocytes. J Orthop Res 24:1078–1085
Miyanishi K, Trindade MCD, Lindsey DP, Beaupre GS, Carter DR, Goodman SB, Schurman DJ, Smith RL (2006a) Dose- and time-dependent effects of cyclic hydrostatic pressure on transforming growth factor-beta3-induced chondrogenesis by adult human mesenchymal stem cells in vitro. Tissue Eng 12:2253–2262
Miyanishi K, Trindade MCD, Lindsey DP, Beaupre GS, Carter DR, Goodman SB, Schurman DJ, Smith RL (2006b) Effects of hydrostatic pressure and transforming growth factor-beta 3 on adult human mesenchymal stem cell chondrogenesis in vitro. Tissue Eng 12:1419–1428
Morales TI (1991) Transforming growth factor-beta 1 stimulates synthesis of proteoglycan aggregates in calf articular cartilage organ cultures. Arch Biochem Biophys 286:99–106
Moutos FT, Freed LE, Guilak F (2007) A biomimetic three-dimensional woven composite scaffold for functional tissue engineering of cartilage. Nat Mater 6:162–167
Munirah S, Kim SH, Ruszymah BH, Khang G (2008) The use of fibrin and poly(lactic-co-glycolic acid) hybrid scaffold for articular cartilage tissue engineering: an in vivo analysis. Eur Cell Mater 15:41–52
Natoli RM, Revell CM, Athanasiou KA (2009) Chondroitinase ABC treatment results in greater tensile properties of self-assembled tissue-engineered articular cartilage. Tissue Eng Part A 15:3119–3128
Ng KW, Wang CCB, Mauck RL, Kelly TA, Chahine NO, Costa KD, Ateshian GA, Hung CT (2005) A layered agarose approach to fabricate depth-dependent inhomogeneity in chondrocyte-seeded constructs. J Orthop Res 23:134–141
Ng KW, Mauck RL, Statman LY, Lin EY, Ateshian GA, Hung CT (2006) Dynamic deformational loading results in selective application of mechanical stimulation in a layered, tissue-engineered cartilage construct. Biorheology 43:497–507
Ng KW, Kugler LE, Doty SB, Ateshian GA, Hung CT (2009a) Scaffold degradation elevates the collagen content and dynamic compressive modulus in engineered articular cartilage. Osteoarthr Cartil 17:220–227
Ng KW, Ateshian GA, Hung CT (2009b) Zonal chondrocytes seeded in a layered agarose hydrogel create engineered cartilage with depth-dependent cellular and mechanical inhomogeneity. Tissue Eng Part A 15:2315–2324
Nguyen LH, Kudva AK, Guckert NL, Linse KD, Roy K (2011a) Unique biomaterial compositions direct bone marrow stem cells into specific chondrocytic phenotypes corresponding to the various zones of articular cartilage. Biomaterials 32:1327–1338
Nguyen LH, Kudva AK, Saxena NS, Roy K (2011b) Engineering articular cartilage with spatially-varying matrix composition and mechanical properties from a single stem cell population using a multi-layered hydrogel. Biomaterials 32:6946–6952
Nuernberger S, Cyran N, Albrecht C, Redl H, Vecsei V, Marlovits S (2011) The influence of scaffold architecture on chondrocyte distribution and behavior in matrix-associated chondrocyte transplantation grafts. Biomaterials 32:1032–1040
O'Driscoll SW (1999) Articular cartilage regeneration using periosteum. Clin Orthop Relat Res 367(suppl):S186–S203
Ogawa R, Mizuno S, Murphy GF, Orgill DP (2009) The effect of hydrostatic pressure on three-dimensional chondroinduction of human adipose-derived stem cells. Tissue Eng Part A 15:2937–2945
Owen JR, Wayne JS (2006) Influence of a superficial tangential zone over repairing cartilage defects: implications for tissue engineering. Biomech Model Mechanobiol 5:102–110
Park Y, Lutolf MP, Hubbell JA, Hunziker EB, Wong M (2004) Bovine primary chondrocyte culture in synthetic matrix metalloproteinase-sensitive poly(ethylene glycol)-based hydrogels as a scaffold for cartilage repair. Tissue Eng 10:515–522
Park Y, Sugimoto M, Watrin A, Chiquet M, Hunziker EB (2005) BMP-2 induces the expression of chondrocyte-specific genes in bovine synovium-derived progenitor cells cultured in three-dimensional alginate hydrogel. Osteoarthr Cartil 13:527–536
Park SH, Sim WY, Park SW, Yang SS, Choi BH, Park SR, Park K, Min BH (2006) An electromagnetic compressive force by cell exciter stimulates chondrogenic differentiation of bone marrow-derived mesenchymal stem cells. Tissue Eng 12:3107–3117
Pei M, Seidel J, Vunjak-Novakovic G, Freed LE (2002) Growth factors for sequential cellular de- and re-differentiation in tissue engineering. Biochem Biophys Res Commun 294:149–154
Pestka JM, Schmal H, Salzmann G, Hecky J, Sudkamp NP, Niemeyer P (2011) In vitro cell quality of articular chondrocytes assigned for autologous implantation in dependence of specific patient characteristics. Arch Orthop Trauma Surg 131:779–789
Petit A, Demers CN, Girard-Lauriault PL, Stachura D, Wertheimer MR, Antoniou J, Mwale F (2011) Effect of nitrogen-rich cell culture surfaces on type X collagen expression by bovine growth plate chondrocytes. Biomed Eng Online 10:4
Prabhakar V, Capila I, Raman R, Srinivasan A, Bosques CJ, Pojasek K, Wrick MA, Sasisekharan R (2006) The catalytic machinery of chondroitinase ABC I utilizes a calcium coordination strategy to optimally process dermatan sulfate. Biochemistry 45:11130–11139
Puelacher WC, Kim SW, Vacanti JP, Schloo B, Mooney D, Vacanti CA (1994) Tissue-engineered growth of cartilage: the effect of varying the concentration of chondrocytes seeded onto synthetic polymer matrices. Int J Oral Maxillofac Surg 23:49–53
Puetzer JL, Petitte JN, Loboa EG (2010) Comparative review of growth factors for induction of three-dimensional in vitro chondrogenesis in human mesenchymal stem cells isolated from bone marrow and adipose tissue. Tissue Eng Part B Rev 16:435–444
Rampersad S, Ruiz JC, Petit A (2011) Stem cells, nitrogen-rich plasma-polymerized culture surfaces, and type X collagen suppression. Tissue Eng Part A (in press)
Redman SN, Oldfield SF, Archer CW (2005) Current strategies for articular cartilage repair. Eur Cell Mater 9:23–32
Responte DJ, Natoli RM, Athanasiou KA (2007) Collagens of articular cartilage: structure, function, and importance in tissue engineering. Crit Rev Biomed Eng 35:363–411
Revell CM, Reynolds CE, Athanasiou KA (2008) Effects of initial cell seeding in self assembly of articular cartilage. Ann Biomed Eng 36:1441–1448
Rice MA, Anseth KS (2007) Controlling cartilaginous matrix evolution in hydrogels with degradation triggered by exogenous addition of an enzyme. Tissue Eng 13:683–691
Ronziere MC, Perrier E, Mallein-Gerin F, Freyria AM (2010) Chondrogenic potential of bone marrow- and adipose tissue-derived adult human mesenchymal stem cells. Biomed Mater Eng 20:145–158
Saeidi N, Sander EA, Ruberti JW (2009) Dynamic shear-influenced collagen self-assembly. Biomaterials 30:6581–6592
Sakao K, Takahashi KA, Arai Y, Inoue A, Tonomura H, Saito M, Yamamoto T, Kanamura N, Imanishi J, Mazda O, Kubo T (2008) Induction of chondrogenic phenotype in synovium-derived progenitor cells by intermittent hydrostatic pressure. Osteoarthr Cartil 16:805–814
Salgado AJ, Oliveira JT, Pedro AJ, Reis RL (2006) Adult stem cells in bone and cartilage tissue engineering. Curr Stem Cell Res Ther 1:345–364
Schulz RM, Bader A (2007) Cartilage tissue engineering and bioreactor systems for the cultivation and stimulation of chondrocytes. Eur Biophys J 36:539–568
Schulz RM, Zscharnack M, Hanisch I, Geiling M, Hepp P, Bader A (2008) Cartilage tissue engineering by collagen matrix associated bone marrow derived mesenchymal stem cells. Biomed Mater Eng 18:S55–S70
Schuurman W, Gawlitta D, Klein TJ, ten Hoope W, van Rijen MHP, Dhert WJA, van Weeren PR, Malda J (2009) Zonal chondrocyte subpopulations reacquire zone-specific characteristics during in vitro redifferentiation. Am J Sports Med 37:97S–104S
Seifarth C, Csaki C, Shakibaei M (2009) Anabolic actions of IGF-I and TGF-beta1 on Interleukin-1beta-treated human articular chondrocytes: evaluation in two and three dimensional cultures. Histol Histopathol 24:1245–1262
Sekiya I, Larson BL, Vuoristo JT, Reger RL, Prockop DJ (2005) Comparison of effect of BMP-2, -4, and −6 on in vitro cartilage formation of human adult stem cells from bone marrow stroma. Cell Tissue Res 320:269–276
Sengers BG, van Donkelaar CC, Oomens CWJ, Baaijens FPT (2004) The local matrix distribution and the functional development of tissue engineered cartilage, a finite element study. Ann Biomed Eng 32:1718–1727
Sengers BG, van Donkelaar CC, Oomens CWJ, Baaijens FPT (2005a) Computational study of culture conditions and nutrient supply in cartilage tissue engineering. Biotechnol Prog 21:1252–1261
Sengers BG, Heywood HK, Lee DA, Oomens CWJ, Bader DL (2005b) Nutrient utilization by bovine articular chondrocytes: a combined experimental and theoretical approach. J Biomech Eng 127:758–766
Shirazi R, Shirazi-Adl A (2008) Deep vertical collagen fibrils play a significant role in mechanics of articular cartilage. J Orthop Res 26:608–615
Shirazi R, Shirazi-Adl A, Hurtig M (2008) Role of cartilage collagen fibrils networks in knee joint biomechanics under compression. J Biomech 41:3340–3348
Solchaga LA, Temenoff JS, Gao J, Mikos AG, Caplan AI, Goldberg VM (2005) Repair of osteochondral defects with hyaluronan- and polyester-based scaffolds. Osteoarthr Cartil 13:297–309
Song L, Baksh D, Tuan RS (2004) Mesenchymal stem cell-based cartilage tissue engineering: cells, scaffold and biology. Cytotherapy 6:596–601
Spiller KL, Maher SA, Lowman AM (2011) Hydrogels for the repair of articular cartilage defects. Tissue Eng Part B Rev 17:281–299
Steck E, Bertram H, Abel R, Chen B, Winter A, Richter W (2005) Induction of intervertebral disc-like cells from adult mesenchymal stem cells. Stem Cells 23:403–411
Stenhamre H, Nannmark U, Lindahl A, Gatenholm P, Brittberg M (2010) Influence of pore size on the redifferentiation potential of human articular chondrocytes in poly(urethane urea) scaffolds. J Tissue Eng Regen Med (in press)
Strobel S, Loparic M, Wendt D, Schenk AD, Candrian C, Lindberg RLP, Moldovan F, Barbero A, Martin I (2010) Anabolic and catabolic responses of human articular chondrocytes to varying oxygen percentages. Arthritis Res Ther 12:R34
Sun M, Lv D, Zhang C, Zhu L (2010) Culturing functional cartilage tissue under a novel bionic mechanical condition. Med Hypotheses 75:657–659
Takagi M, Umetsu Y, Fujiwara M, Wakitani S (2007) High inoculation cell density could accelerate the differentiation of human bone marrow mesenchymal stem cells to chondrocyte cells. J Biosci Bioeng 103:98–100
Temenoff JS, Mikos AG (2000) Review: tissue engineering for regeneration of articular cartilage. Biomaterials 21:431–440
Terada S, Fuchs JR, Yoshimoto H, Fauza DO, Vacanti JP (2005) In vitro cartilage regeneration from proliferated adult elastic chondrocytes. Ann Plast Surg 55:196–201
Thorpe SD, Buckley CT, Vinardell T, O'Brien FJ, Campbell VA, Kelly DJ (2010) The response of bone marrow-derived mesenchymal stem cells to dynamic compression following TGF-beta3 induced chondrogenic differentiation. Ann Biomed Eng 38:2896–2909
van der Kraan P, Vitters E, van den Berg W (1992) Differential effect of transforming growth factor beta on freshly isolated and cultured articular chondrocytes. J Rheumatol 19:140–145
van Donkelaar CC, Chao G, Bader DL, Oomens CWJ (2011) A reaction-diffusion model to predict the influence of neo-matrix on the subsequent development of tissue-engineered cartilage. Comput Methods Biomech Biomed Engin 14:425–432
van Turnhout MC, Schipper H, Engel B, Buist W, Kranenbarg S, van Leeuwen JL (2010) Postnatal development of collagen structure in ovine articular cartilage. BMC Dev Biol 10:62
Veilleux N, Spector M (2005) Effects of FGF-2 and IGF-1 on adult canine articular chondrocytes in type II collagen-glycosaminoglycan scaffolds in vitro. Osteoarthr Cartil 13:278–286
Vinardell T, Buckley CT, Thorpe SD, Kelly DJ (2010) Composition-function relations of cartilaginous tissues engineered from chondrocytes and mesenchymal stem cells isolated from bone marrow and infrapatellar fat pad. J Tissue Eng Regen Med (in press)
Volkmer E, Drosse I, Otto S, Stangelmayer A, Stengele M, Kallukalam BC, Mutschler W, Schieker M (2008) Hypoxia in static and dynamic 3D culture systems for tissue engineering of bone. Tissue Eng Part A 14:1331–1340
Wagner DR, Lindsey DP, Li KW, Tummala P, Chandran SE, Smith RL, Longaker MT, Carter DR, Beaupre GS (2008) Hydrostatic pressure enhances chondrogenic differentiation of human bone marrow stromal cells in osteochondrogenic medium. Ann Biomed Eng 36:813–820
Waldman SD, Grynpas MD, Pilliar RM, Kandel RA (2003) The use of specific chondrocyte populations to modulate the properties of tissue-engineered cartilage. J Orthop Res 21:132–138
Waldman SD, Couto DC, Grynpas MD, Pilliar RM, Kandel RA (2006) A single application of cyclic loading can accelerate matrix deposition and enhance the properties of tissue-engineered cartilage. Osteoarthr Cartil 14:323–330
Wang Y, Kim UJ, Blasioli DJ, Kim HJ, Kaplan DL (2005) In vitro cartilage tissue engineering with 3D porous aqueous-derived silk scaffolds and mesenchymal stem cells. Biomaterials 26:7082–7094
Welsch GH, Mamisch TC, Zak L, Blanke M, Olk A, Marlovits S, Trattnig S (2010) Evaluation of cartilage repair tissue after matrix-associated autologous chondrocyte transplantation using a hyaluronic-based or a collagen-based scaffold with morphological MOCART scoring and biochemical T2 mapping: preliminary results. Am J Sports Med 38:934–942
Wenger R, Hans MG, Welter JF, Solchaga LA, Sheu YR, Malemud CJ (2006) Hydrostatic pressure increases apoptosis in cartilage-constructs produced from human osteoarthritic chondrocytes. Front Biosci 11:1690–1695
Wiegandt K, Goepfert C, Portner R (2007) Improving in vitro generated cartilage-carrier-constructs by optimizing growth factor combination. Open Biomed Eng J 1:85–90
Williams CG, Kim TK, Taboas A, Malik A, Manson P, Elisseeff J (2003) In vitro chondrogenesis of bone marrow-derived mesenchymal stem cells in a photopolymerizing hydrogel. Tissue Eng 9:679–688
Williams GM, Klein TJ, Sah RL (2005) Cell density alters matrix accumulation in two distinct fractions and the mechanical integrity of alginate-chondrocyte constructs. Acta Biomater 1:625–633
Wilson W, Huyghe JM, van Donkelaar CC (2006) A composition-based cartilage model for the assessment of compositional changes during cartilage damage and adaptation. Osteoarthr Cartil 14:554–560
Wilson W, Huyghe JM, van Donkelaar CC (2007) Depth-dependent compressive equilibrium properties of articular cartilage explained by its composition. Biomech Model Mechanobiol 6:43–53
Wimmer MA, Alini M, Grad S (2009) The effect of sliding velocity on chondrocytes activity in 3D scaffolds. J Biomech 42:424–429
Woodfield TBF, van Blitterswijk CA, De Wijn J, Sims TJ, Hollander AP, Riesle J (2005) Polymer scaffolds fabricated with pore-size gradients as a model for studying the zonal organization within tissue-engineered cartilage constructs. Tissue Eng 11:1297–1311
Worster AA, Brower-Toland BD, Fortier LA, Bent SJ, Williams J, Nixon AJ (2001) Chondrocytic differentiation of mesenchymal stem cells sequentially exposed to transforming growth factor-beta1 in monolayer and insulin-like growth factor-I in a three-dimensional matrix. J Orthop Res 19:738–749
Xiang Y, Zheng Q, Jia Bb, Huang Gp, Xu Yl, Wang Jf, Pan Zj (2007) Ex vivo expansion and pluripotential differentiation of cryopreserved human bone marrow mesenchymal stem cells. J Zhejiang Univ Sci B 8:136–146
Xu J, Wang W, Ludeman M, Cheng K, Hayami T, Lotz JC, Kapila S (2008) Chondrogenic differentiation of human mesenchymal stem cells in three-dimensional alginate gels. Tissue Eng Part A 14:667–680
Yasuda A, Kojima K, Tinsley KW, Yoshioka H, Mori Y, Vacanti CA (2006) In vitro culture of chondrocytes in a novel thermoreversible gelation polymer scaffold containing growth factors. Tissue Eng 12:1237–1245
Yoon DM, Fisher JP (2006) Chondrocyte signaling and artificial matrices for articular cartilage engineering. Adv Exp Med Biol 585:67–86
Yoon DM, Fisher JP (2008) Effects of exogenous IGF-1 delivery on the early expression of IGF-1 signaling molecules by alginate embedded chondrocytes. Tissue Eng Part A 14:1263–1273
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported with funding from the Dutch Technology Foundation STW (VIDI-07970).
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Kock, L., van Donkelaar, C.C. & Ito, K. Tissue engineering of functional articular cartilage: the current status. Cell Tissue Res 347, 613–627 (2012). https://doi.org/10.1007/s00441-011-1243-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-011-1243-1