Abstract
Purpose of Review
To consolidate information on the obesogenic and cardiometabolic effects of prenatal exposure to cannabis.
Recent Findings
A PubMed search strategy updated from January 1, 2014, through 14 June 2023, produced a total of 47 epidemiologic studies and 12 animal studies. Prenatal exposure to cannabis is consistently associated with small for gestational age and low birth weight. After birth, these offspring gain weight rapidly and have increased adiposity and higher glucose (fat mass percentage) in childhood. More preclinical and prospective studies are needed to deepen our understanding of whether these associations vary by sex, dose, timing, and composition of cannabis (e.g., ratio of delta-Δ9-tetrahydrocannabinol [Δ9-THC] to cannabidiol [CBD]). Addressing these gaps may help to solidify causality and identify intervention strategies.
Summary
Based on the available data, clinicians and public health officials should continue to caution against cannabis use during pregnancy to limit its potential obesogenic and adverse cardiometabolic effects on the offspring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amid increasing legality and growing cultural acceptance, cannabis use in pregnancy is becoming increasingly common. Self-reported data from the 2018 National Survey on Drug Use and Health estimate that 3.7% of pregnant people use cannabis [1]. The survey data further shows a higher prevalence among pregnant people who were younger (13.1%) [1] or with a cognitive disability (13.0%) [2] or depression (12.7%) [1]. However, these estimates likely suffer from underreporting. In fact, bioanalytic data from urban hospital settings suggest that up to 30% of pregnant people use or are exposed to cannabis [3, 4].
The reasons for cannabis use vary [5]. Pregnant people report using cannabis to manage nausea, to cope with stress or anxiety, and/or for relaxation and enjoyment [6]. There are risks to the offspring that should be weighed in the decision to use cannabis during pregnancy. Prenatal exposure to cannabis was associated with adverse birth outcomes, such as lower birth weight, smaller head circumference, lower Apgar scores, and an increased risk for admission to the neonatal intensive care unit (NICU), as well as altered neurobehavioral traits among older child offspring [7,8,9,10,11].
More recently, evidence suggests that prenatal exposure to cannabis may predispose the offspring to obesity, altered glucose homeostasis, and impaired cardiac function [12], but there is a need to better understand this growing science. Thus, the goals of this review are to (1) establish the obesogenic and cardiometabolic risks of prenatal exposure to cannabis; (2) recontextualize the cannabis-birth weight literature with respect to childhood obesity and metabolic disorders; (3) propose biological mechanisms underlying these associations; (4) compare the effects of common cannabinoids, namely, delta-Δ9-tetrahydrocannabinol (Δ9-THC) and cannabidiol (CBD); and (5) highlight critical gaps in knowledge that are needed to infer causality and identify opportunities for intervention.
Methods
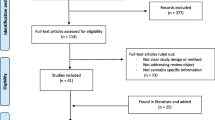
A PubMed search strategy was updated through 14 June 2023. The search algorithm included all possible combinations of keywords from the following three groups: (1) “cannabis,” “marijuana,” “THC,” or “CBD”; and (2) “pregnancy,” “prenatal,” “in utero,” “fetal,” “offspring,” “infant” or “early life”; and (3) “birth outcomes,” “birth weight,” “weight,” “obes*,” “body mass index,” “fat mass,” “adipo*,” “glucose,” “insulin,” “metabolic syndrome,” “cardio*,” “cardiac,” “blood pressure,” “cholesterol,” “hypertension,” or “lipid.” This review focused on papers published since 2014, given the increasing legality of cannabis for recreational use over the past decade and changes in cannabis potency [13].
Results
The PubMed search identified 1898 publications. After removing duplicates, 491 unique publications were screened. Of these, 432 were excluded for the following reasons: commentaries or reviews (n = 71); neurodevelopment, cognitive, or behavioral outcomes (n = 72); other unrelated health outcomes (n = 86); studies of hemp oil, synthetic or endogenous cannabinoids, or the endocannabinoid system (n = 36); polysubstance use or drugs other than cannabis (n = 24); characteristics or reasons for cannabis use (n = 43); prevalence studies (n = 18); biomarker studies (n = 16); cessation or prevention studies (n = 9); health policy analyses (n = 3); effects of pre-conception cannabis use (n = 3); abstracts or reports presenting insufficient data (n = 2); and papers focused entirely on unrelated exposures and outcomes (n = 50). Thus, 47 epidemiologic studies [3, 4, 14,15,16,17,18, 19••, 20,21,22,23,24,25,26,27,28, 29•, 30,31,32,33, 34••, 35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58] and 12 animal models [59, 60••, 61, 62, 63••, 64, 65••, 66•, 67,68,69,70] presenting original data met the inclusion criteria for this review.
Evidence from Human Studies
Table 1 summarizes the 47 human epidemiologic studies [3, 4, 14,15,16,17,18, 19••, 20,21,22,23,24,25,26,27,28, 29•, 30,31,32,33, 34••, 35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]. The most common study design was a retrospective medical record review, followed by a prospective cohort study. Cannabis exposure was most often ascertained through self-report (n = 22; 47%), though many studies measured Δ9-THC in maternal urine collected in pregnancy (n = 17; 36%). Four studies captured exposure through Δ9-THC detected in meconium or umbilical cord tissue homogenate collected at delivery (9%). Cannabis use disorder was the primary exposure of interest in three studies (6%). The prevalence of cannabis use or exposure during pregnancy in the absence of other substances ranged from 2.0 to 38.9%. Co-use of cannabis and other drugs of abuse is common. In a case-control study, Kong et al. [29•] reported that co-use of tobacco and cannabis in pregnancy was nearly 41.3%. Three studies estimated that cannabis use among opioid-dependent pregnant people ranged from 9.4% [40] to 40.0% [36].
Forty-four studies examined the associations between prenatal exposure to cannabis and birth weight (as a continuous measure), low birth weight (< 2500 g), or small for gestational age (SGA; < 10th percentile). Prenatal exposure to cannabis was associated with a 55 to 732 g reduction in birth weight, with most studies (17 out of the 21) showing a statistically significant reduction in birth weight, independent of gestational age and sex. Roca and colleagues [38] reported that prenatal exposure to cannabis was associated with a 40 g increase in birth weight among NICU-admitted neonates. However, consistent with findings by Sturrock and colleagues [42], they reported that prenatal exposure to cannabis was associated with a lower birth weight percentile. No effect was noted in a retrospective medical record review of opioid-dependent pregnant people [36], in a population-based case-control study of stillbirths [45], or in a cross-sectional analysis of Pregnancy Risk Assessment Monitoring System (PRAMS) data [28].
Prenatal exposure to cannabis was associated with a statistically significant increase in odds of LBW (adjusted odds ratios [aORs] ranging from 0.9 to 3.9; 11 out of 16 studies showing statistical significance) and SGA (aORs ranging from 1.1 to 2.0; 12 of 17 studies showing statistical significance). The effects were generally independent of gestational age, sex, tobacco/substance in pregnancy, and socioeconomic covariates, such as household income or maternal education. However, the potential for confounding remains moderate. Two studies presented unadjusted models [32, 36], few studies adjusted for maternal pre-pregnancy body mass index (BMI) or gestational weight gain, and none adjusted for maternal diet in pregnancy.
Only one published study has examined the association between prenatal exposure to cannabis and postnatal growth. Using data from a New York–based prospective cohort, Kong et al. [29•] reported that co-exposure to tobacco and cannabis was associated with rapid BMI growth from birth through mid-childhood. However, the effects of cannabis could not be isolated from the effects of tobacco. In an unpublished manuscript, I (along with my co-authors) showed that prenatal exposure to cannabis was associated with rapid BMI growth from birth through age 3 years in the Healthy Start study. Together, these studies suggest that cannabis-exposed infants are smaller at birth, grow rapidly in infancy, and exceed the BMI of unexposed offspring by ~9 months of age. This pattern of growth is often associated with an increased risk for obesity [71], metabolic syndrome [72], and type 2 diabetes [73] later in life.
In the Generation R Study, Cajachagua-Torres and colleagues [19••] reported that maternal or paternal self-report of cannabis use during pregnancy was associated with higher triglycerides and BMI among 10-year-old offspring. This finding is supported by the work of Moore et al. [34••] and Kong et al. [29•], which reported higher adiposity (fat mass percentage) among Δ9-THC-exposed children. However, there is some uncertainty around the effects on metabolic outcomes. Cajachagua-Torres and colleagues [19••] reported no association with non-fasting glucose. Conversely, Moore and colleagues [34••] showed that prenatal exposure to cannabis was associated with increased fasting glucose at age 5 years.
Evidence from Animal Studies
Table 2 summarizes the 12 animal studies included in this review [59, 60••, 61,62,63,64,65,66,67,68,69,70]. Wistar rats were the most common model, followed by C57BL/6 J mice and Sprague-Dawley rats. All but one study included both sexes in their experiments. The route of exposure varied, with most experiments utilizing intraperitoneal injection or oral administration. Exposure typically occurred between 6 and 22 days gestation, though some studies included exposure during mating and through weaning.
The doses administered to the rodents ranged from 2 to 10 mg/Kg of Δ9-THC per day and 3 to 20 mg/Kg of CBD per day. This dose mimics moderate recreational cannabis use in human adults (13 to 63 ng/mL), which results in a fetal dose between 4 and 287 ng/mL [60••].
Seven of the eight animal studies reported lower birth weights among offspring with prenatal exposure to Δ9-THC. Breit and colleagues [59] found no association, though the Sprague-Dawley rats were exposed only once (30 min of cannabis smoke at gestational day 20). This may provide insight about how frequency and dose may influence offspring birth weight and later-life adiposity.
Both Δ9-THC and CBD appear to impact postnatal growth. Compared to non-exposed offspring, Δ9-THC-exposed offspring are born smaller, “catch-up” in as little as 12 days [60••, 62], and begin to surpass the size of non-exposed offspring by age 6 months [65••]. Prenatal CBD may impact postnatal growth in a sex-specific manner, with males being more susceptible to this environmental insult [61, 67], but the evidence is not conclusive [70].
Prenatal exposure to Δ9-THC impacts many aspects of offspring’s cardiovascular and metabolic health. Robinson and colleagues [66•] demonstrated that C57BL/6 J mice with prenatal exposure to Δ9-THC had myocardial valve thickening and ventricular septal defect. These structural changes to the fetal heart may have long-lasting impacts on cardiovascular function. Indeed, Lee and colleagues [63••] demonstrated that prenatal Δ9-THC was associated with lower stroke volume and cardiac output. Additional animal studies conducted at the University of Western Ontario revealed that prenatal Δ9-THC was associated with increased glucose intolerance at age 5 months among female offspring only [60••] and higher hepatic triglycerides at age 6 months among male offspring only [65••]. Taken together, studies provide some evidence that prenatal exposure to Δ9-THC may predispose offspring to dyslipidemia and hyperglycemia across the life course.
Discussion
Biological Mechanisms
An important tenet of the causal inference framework is to establish the biological plausibility of the observed associations. Figure 1 summarizes the possible biological mechanisms linking prenatal exposure to cannabis with offspring obesity, cardiovascular health, and metabolic disorders.
Potential mechanisms underlying the associations between prenatal exposure to cannabinoids with child obesity and cardiometabolic health. Images were obtained from the free medical site http://smart.servier.com/ by Servier licensed under a Creative Commons Attribution 3.0 Unported License
Preclinical studies show that Δ9-THC leads to placental insufficiency [15, 64, 74], which may hinder fetal growth. When fetal growth restriction is followed by rapid infant growth, the offspring may be predisposed to abdominal obesity, type 2 diabetes, and cardiovascular disease [75]. However, Metz and colleagues [45] theorized that the adverse birth effects induced by prenatal exposure to cannabis may be independent of abnormal placental pathology. Thus, other mechanisms may be involved.
Fetal programming in mesenchymal stem cells (MSCs) may play an important role in the cannabis-obesity association. Both Δ9-THC [76] and CBD [77] promote adipogenesis in human and mouse MSCs via peroxisome proliferator–activated receptor gamma (PPARγ) activation. Excessive adipogenesis of fetal MSCs may contribute to obesity later in life, regardless of offspring birth weight [78].
Cannabinoids may alter RNA regulation of dopamine receptor genes, as demonstrated by DiNieri et al. [79] and proposed by de Almeida and Devi [80]. Dysregulation of this key reward pathway may alter appetite and satiety and contribute to disinhibited eating. Murine models further showed that Δ9-THC-exposed male, but not female, offspring impacts mesolimbic dopamine function [81, 82]. This may explain the sex-specific effects of CBD on postnatal growth, as reported by Iezzi and colleagues [61].
The endocannabinoid system may be integral to the development of the pancreas. The endocannabinoid system is a complex signaling pathway involved in brain development [83], metabolism [84], and glucose homeostasis [85]. Cannabinoid type 1 (CB1) receptors are abundant in both glucagon-producing α-cells and insulin-producing β-cells [86]. In a mouse model, Malenczyk and colleagues [87] showed that 2-arachidonoylglycerol (2-AG, an endocannabinoid that is functionally similar to Δ9-THC) influenced islet morphology by increasing the number of pancreatic α-cells, which would promote glucagon release, oppose insulin action, and increase blood glucose in exposed pups. In a separate mouse model, Gillies and colleagues [60••] reported that prenatal exposure to Δ9-THC was associated with a significant reduction (41%) of pancreatic β-cells and increased glucose intolerance in female Wistar rats at a postnatal age of 5 months. Asadi and colleagues [68] provide compelling evidence that prenatal exposure to Δ9-THC reprograms fetal islet endocrine hormone profile among female rat offspring. Specifically, stathmin-2 (Stmn2) may play a role in regulating offspring glucose through its interaction with glucagon. Taken together, these studies illustrate how prenatal exposure to cannabis may disrupt the balanced molecular control of insulin and glucagon release via the endocannabinoid system.
Individual Cannabinoids
Cannabis is a complex mixture of over 100 cannabinoids [88]. Δ9-THC and CBD are the most abundant and most studied cannabinoids. Disentangling the effects of Δ9-THC and CBD may have important health implications. Over the past two decades, there has been a dramatic shift in the composition of commercial cannabis products. Δ9-THC potency has increased three-fold, while the concentration of CBD has been halved [13]. CBD use is often perceived as safe among pregnant people and even some obstetrics-related medical professionals [89], which may explain why one in five pregnant people report CBD use while pregnant [90].
While structurally similar, Δ9-THC and CBD have different molecular targets. As such, they produce distinct and sometimes opposing effects. For instance, Δ9-THC is widely accepted as orexogenic [91], whereas CBD is often associated with reduced appetite and weight loss [92]. To date, there is very little published data regarding the metabolic effects of individual cannabinoids. This is almost certainly due to the scheduling status of the drug, which restricts access to cannabis for research purposes. A 1974 randomized controlled trial reported that a single intravenous administration of Δ9-THC (6 mg) induced glucose intolerance among healthy adult volunteers [93]. Case studies from 1969–1970 further showed that higher doses of Δ9-THC can lead to glycosuria [94] and diabetic ketoacidosis [95]. By contrast, a recent clinical trial shows that a 10:1 ratio of CBD to Δ9-THC (100 µg CBD and 10 µg Δ9-THC) improves the lipid profile and glycemic control after 8 weeks among patients with type 2 diabetes [96]. Several clinical trials are underway examining the metabolic impacts of Δ9-THC or CBD administration (e.g., NCT05322213, NCT05618756, NCT04114903), which may further elucidate the metabolic effects of Δ9-THC and CBD.
Despite this growing body of evidence, it is not clear whether prenatal exposure to Δ9-THC and CBD would produce similar cardiometabolic effects on the offspring or whether these cannabinoids impose opposite effects, as it does in adult active users. Furthermore, there are other common cannabinoids that may influence glycemic control. For instance, a recent double-blind randomized controlled trial showed that tetrahydrocannabivarin (THCV) decreased fasting plasma glucose and improved pancreatic β-cell function in adult patients with type 2 diabetes [97]. Large prospective cohorts with sufficiently large subgroups of offspring with prenatal exposure to Δ9-THC, CBD, and other common cannabinoids are needed to explore this question more conclusively in humans.
Windows of Susceptibility
Timing may be an important factor in the associations between prenatal exposure to cannabis and offspring adiposity and cardiometabolic health. For instance, early gestation exposure may alter pancreatic development [87], whereas late gestation exposure, when the majority of fat accretion occurs [98], may have a more profound effect on birth weight and child adiposity. Few studies have attempted to examine whether early vs. late gestation exposure impacts offspring birth outcomes. Three epidemiologic studies reported no effect on birth weight or child metabolic health if the mother quit cannabis early in the pregnancy [19••, 23, 37]. A fourth study reported that cannabis use in the first trimester alone was associated with offspring birth weight, though the effects were more severe if cannabis use was sustained throughout the entire pregnancy [46]. Given this paucity of data, there remains a need to quantify exposure at multiple time points throughout pregnancy to formally assess trimester-specific effects.
Beyond the prenatal period, pre-conception exposure may predispose offspring to later-life obesity and cardiometabolic disease, but the evidence is inconsistent. Two human epidemiologic studies reported that pre-conception exposure to cannabis was associated with lower birth weight [99, 100]. This may occur through the disruption of oocyte maturation [101] or through epigenetic changes to sperm among paternal cannabis users [102]. However, this hypothesis is inconsistent with a preclinical study, which found no effect on birth weight among offspring of male Wistar rats exposed to Δ9-THC while mating [103]. More research is needed to clarify whether the epidemiologic findings are due to pre-conception exposure alone or rather a continuation of cannabis use in early pregnancy.
Childhood exposure to cannabis is also a growing concern. Self-reported data from the 2015 National Survey on Drug Use and Health estimates that 12% of adults with children in the home use cannabis [104]. Bioanalytical studies confirm that at least this many children are exposed, though the prevalence may be higher in younger children. Prospective data from a Colorado-based study indicates that 13% of children, aged 5 years, had detectable levels of CBD in urine [105]. Cross-sectional data from Denver, CO [106] and New York City, NY [107] suggest that nearly 20% of children under 3 years of age had detectable Δ9-THC concentrations in urine. Given the age of these children, it is not clear whether these exposures occur through breast milk (in which Δ9-THC readily accumulates [108]), through dermal exposure (as cannabinoids are known to accumulate on surfaces [109] and young children exhibit increased hand-to-mouth activity [110]), or through ambient exposure (an important route of exposure given children’s faster ventilation rates [111]).
Mode, Dose, and Frequency of Use
Bioavailability varies widely based on the mode of cannabis use. Cannabinoids exhibit similar pharmacokinetics when administered via inhalation or intravenous injection: peak plasma concentrations occur rapidly (under 10 min) [112] and bioavailability is moderate (10–35%) [113]. Due to hepatic first-pass metabolism, the bioavailability of orally consumed Δ9-THC is very poor, < 20% for edible gelatin capsules and as low as 6% for baked goods [114]. As such, oral administration results in lower and more erratic plasma concentrations [112]. Given that edibles are the second most common mode of administration among pregnant people [115], it may be important to consider the mode of use in future studies examining the cardiometabolic effects of prenatal exposure to cannabis.
Few studies have evaluated potential dose-response effects, which represents an important gap in knowledge. Robinson and colleagues [66•] showed clear dose-dependent effects for 5 and 10 mg/kg Δ9-THC per day. Frequency of use may also impact these associations. Two epidemiologic studies have reported that the cannabis-birth weight association was only evident among frequent users but not among infrequent users (less than once a month) [48, 116]. Additional dose-response studies are needed to identify threshold effects and solidify the casual nature of these associations.
Sex-Specific Effects
The published literature provides some evidence of sexually dimorphic associations between prenatal exposure to cannabinoids and offspring cardiometabolic health, though the patterns and mechanisms are not yet clear.
Males appear to be more susceptible to cannabis-induced impacts on growth. In a longitudinal epidemiologic analysis, Massey and colleagues [56] reported that prenatal exposure to cannabis was associated with lower birth weight among male offspring, but not female offspring. This observation is supported by the fact that males are generally more susceptible to early-life environmental insults [117]. Furthermore, in a mouse model, Benevenuto and colleagues [69] showed that prenatal exposure to cannabis smoke was associated with a lower fetal-placental weight ratio in male rat offspring only, which may imply sex-specific placental insufficiency.
Prenatal CBD appears to have little effect on postnatal growth, though there is some indication of a sex-specific effect. Iezzi and colleagues [61] reported that male offspring with developmental exposure to CBD had increased postnatal weights, whereas both Iezzi et al. [61] and Wanner et al. [67] reported no difference in postnatal weight among female offspring, and Maciel et al. [70] reported no difference in either sex. Sex-specific weight differences may be due to increased bioaccumulation of CBD among males [70] or CBD potentially exaggerating differences in postnatal growth trajectories among boys and girls [118].
Prenatal Δ9-THC has been linked to increased glucose intolerance among female offspring only [60••], which may be attributable to sex-specific differences in the development of the endocannabinoid system [119] (which plays a key role in metabolism [84] and glucose homeostasis [85]) or insulin resistance (which tends to be higher in prepubertal girls as compared to prepubertal boys [120]). On the other hand, prenatal Δ9-THC has also been linked to higher hepatic triglycerides among male offspring only [65••]. Oke and colleagues [65••] further showed that male, but not female, rat offspring exhibit decreased expression of miR-203a-3p and miR-29a/b/c, both involved in mitochondrial homeostasis in the liver. Beyond epigenetic mechanisms, this sexually dimorphic association may be attributed to differences in lipogenesis and lipolysis [121, 122].
These observations highlight the need for more animal models and larger epidemiologic studies with robust sample sizes that allow for effect modification by sex, which would help to make stronger inferences about the causal links between prenatal exposure and cannabis and the risk of childhood cardiometabolic health.
Conclusions
Cannabis use during pregnancy is on the rise and may soon surpass tobacco use. Between 2002 and 2016, tobacco use during pregnancy decreased by 40%, whereas the prevalence of cannabis use during pregnancy nearly doubled [123]. This is concerning, as the consequences of cannabis use during pregnancy mirror that of tobacco use during pregnancy: offspring are more likely to be born small, grow rapidly in infancy, and have a higher risk of obesity later in life. While the literature has rapidly expanded since 2014, key gaps in knowledge remain. More data is needed to understand whether these associations are cannabinoid-, timing-, dose-, or sex-specific, which would help to strengthen the biological plausibility and reinforce the need for cannabis cessation efforts in pregnant populations. For the time being, the current recommendations to limit cannabis use during pregnancy should continue. Healthcare providers should have open discussions with pregnant patients about the potential risks of cannabis use during pregnancy and provide evidence-based recommendations for safer alternatives when possible.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Goodwin RD, Zhu J, Heisler Z, Metz TD, Wyka K, Wu M, et al. Cannabis use during pregnancy in the United States: the role of depression. Drug Alcohol Depend. 2020;210:107881. https://doi.org/10.1016/j.drugalcdep.2020.107881.
Kitsantas P, Aljoudi SM, Gimm G. Marijuana use in pregnant women with disabilities in the United States. Matern Child Health J. 2022;26(2):242–9.
Jones MJ, Lotfi A, Lin A, Gievers LL, Hendrickson R, Sheridan DC. Prenatal marijuana exposure and neonatal outcomes: a retrospective cohort study. BMJ Open. 2022;12(9):e061167. https://doi.org/10.1136/bmjopen-2022-061167.
Mark K, Desai A, Terplan M. Marijuana use and pregnancy: prevalence, associated characteristics, and birth outcomes. Arch Womens Ment Health. 2016;19(1):105–11. https://doi.org/10.1007/s00737-015-0529-9.
Volkow ND, Han B, Compton WM, McCance-Katz EF. Self-reported medical and nonmedical cannabis use among pregnant women in the United States. JAMA. 2019;322(2):167–9. https://doi.org/10.1001/jama.2019.7982.
Vanstone M, Taneja S, Popoola A, Panday J, Greyson D, Lennox R, et al. Reasons for cannabis use during pregnancy and lactation: a qualitative study. CMAJ. 2021;193(50):E1906–14. https://doi.org/10.1503/cmaj.211236.
Marchand G, Masoud AT, Govindan M, Ware K, King A, Ruther S, Brazil G, Ulibarri H, Parise J, Arroyo A, Coriell C, Goetz S, Karrys A, Sainz K. Birth outcomes of neonates exposed to marijuana in utero: a systematic review and meta-analysis. JAMA Netw Open. 2022;4(5):e2145653. https://doi.org/10.1001/jamanetworkopen.2021.45653. PMCID: PMC8796018.
Conner SN, Bedell V, Lipsey K, Macones GA, Cahill AG, Tuuli MG. Maternal marijuana use and adverse neonatal outcomes: a systematic review and meta-analysis. Obstet Gynecol. 2016;128(4):713–23. https://doi.org/10.1097/aog.0000000000001649.
Wu CS, Jew CP, Lu HC. Lasting impacts of prenatal cannabis exposure and the role of endogenous cannabinoids in the developing brain. Future Neurol. 2011;6(4):459–80. https://doi.org/10.2217/fnl.11.27.
Grant KS, Conover E, Chambers CD. Update on the developmental consequences of cannabis use during pregnancy and lactation. Birth Defects Research. 2020;112(15):1126–38. https://doi.org/10.1002/bdr2.1766.
Warner TD, Roussos-Ross D, Behnke M. It’s not your mother’s marijuana: effects on maternal-fetal health and the developing child. Clin Perinatol. 2014;41(4):877–94. https://doi.org/10.1016/j.clp.2014.08.009.
Lee K, Hardy DB. Metabolic consequences of gestational cannabinoid exposure. Int J Mol Sci. 2021 Sep 2;22(17):9528. https://doi.org/10.3390/ijms22179528. PMID: 34502436; PMCID: PMC8430813.
ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC. Changes in cannabis potency over the last 2 decades (1995–2014): analysis of current data in the United States. Biol Psychiat. 2016;79(7):613–9. https://doi.org/10.1016/j.biopsych.2016.01.004.
Bailey BA, Wood DL, Shah D. Impact of pregnancy marijuana use on birth outcomes: results from two matched population-based cohorts. J Perinatol. 2020;40(10):1477–82. https://doi.org/10.1038/s41372-020-0643-z.
Brar BK, Patil PS, Jackson DN, Gardner MO, Alexander JM, Doyle NM. Effect of intrauterine marijuana exposure on fetal growth patterns and placental vascular resistance. J Matern Fetal Neonatal Med. 2021;34(20):3330–4. https://doi.org/10.1080/14767058.2019.1683541.
Brik M, Sandonis M, Gil J, Hernandez-Fleury A, Parramón-Puig G, Maiz N, et al. Intrauterine cannabis exposure and fetal and maternal blood flow: a case-control study. Acta Obstet Gynecol Scand. 2022;101(11):1207–14. https://doi.org/10.1111/aogs.14439.
Brown SJ, Mensah FK, Kit JA, Stuart-Butler D, Glover K, Leane C, et al. Use of cannabis during pregnancy and birth outcomes in an aboriginal birth cohort: a cross-sectional, population-based study. BMJ Open. 2016;6(2):e010286. https://doi.org/10.1136/bmjopen-2015-010286.
Bruno AM, Blue NR, Allshouse AA, Haas DM, Shanks AL, Grobman WA, et al. Marijuana use, fetal growth, and uterine artery Dopplers. J Matern Fetal Neonatal Med. 2022;35(25):7717–24. https://doi.org/10.1080/14767058.2021.1960973.
•• Cajachagua-Torres KN, El Marroun H, Reiss IKM, Santos S, Jaddoe VWV. Foetal tobacco and cannabis exposure, body fat and cardio-metabolic health in childhood. Pediatr Obes. 2022;17(3):e12863. https://doi.org/10.1111/ijpo.12863. This is the first human study to examine the cardiometabolic effects of prenatal exposure to cannabis. Self-reported maternal or paternal cannabis use during pregnancy was associated with higher body mass index (BMI) among the 10-year-old offspring. However, they reported no association with nonfasting glucose or lipids.
Conner SN, Carter EB, Tuuli MG, Macones GA, Cahill AG. Maternal marijuana use and neonatal morbidity. Am J Obstet Gynecol. 2015;213(3):422.e1-4. https://doi.org/10.1016/j.ajog.2015.05.050.
Crume TL, Juhl AL, Brooks-Russell A, Hall KE, Wymore E, Borgelt LM. Cannabis use during the perinatal period in a state with legalized recreational and medical marijuana: the association between maternal characteristics, breastfeeding patterns, and neonatal outcomes. J Pediatr. 2018;197:90–6. https://doi.org/10.1016/j.jpeds.2018.02.005.
Gabrhelík R, Mahic M, Lund IO, Bramness J, Selmer R, Skovlund E, et al. Cannabis use during pregnancy and risk of adverse birth outcomes: a longitudinal cohort study. Eur Addict Res. 2021;27(2):131–41. https://doi.org/10.1159/000510821.
Grzeskowiak LE, Grieger JA, Andraweera P, Knight EJ, Leemaqz S, Poston L, et al. The deleterious effects of cannabis during pregnancy on neonatal outcomes. Med J Aust. 2020;212(11):519–24. https://doi.org/10.5694/mja2.50624.
Howard DS, Dhanraj DN, Devaiah CG, Lambers DS. Cannabis use based on urine drug screens in pregnancy and its association with infant birth weight. J Addict Med. 2019;13(6):436–41. https://doi.org/10.1097/adm.0000000000000516.
Janisse JJ, Bailey BA, Ager J, Sokol RJ. Alcohol, tobacco, cocaine, and marijuana use: relative contributions to preterm delivery and fetal growth restriction. Subst Abuse. 2014;35(1):60–7. https://doi.org/10.1080/08897077.2013.804483.
Joseph-Lemon L, Thompson H, Verostick L, Shizuka Oura H, Jolles DR. Outcomes of cannabis use during pregnancy within the American Association of Birth Centers Perinatal Data Registry 2007–2020: opportunities within midwifery-led care. J Perinat Neonatal Nurs. 2022;36(3):264–73. https://doi.org/10.1097/jpn.0000000000000668.
Kharbanda EO, Vazquez-Benitez G, Kunin-Batson A, Nordin JD, Olsen A, Romitti PA. Birth and early developmental screening outcomes associated with cannabis exposure during pregnancy. J Perinatol. 2020;40(3):473–80. https://doi.org/10.1038/s41372-019-0576-6.
Ko JY, Tong VT, Bombard JM, Hayes DK, Davy J, Perham-Hester KA. Marijuana use during and after pregnancy and association of prenatal use on birth outcomes: a population-based study. Drug Alcohol Depend. 2018;187:72–8. https://doi.org/10.1016/j.drugalcdep.2018.02.017.
• Kong KL, Lee JK, Shisler S, Thanos PK, Huestis MA, Hawk L, et al. Prenatal tobacco and cannabis co-exposure and offspring obesity development from birth to mid-childhood. Pediatr Obes. 2023;18(5):e13010. https://doi.org/10.1111/ijpo.13010. This epidemiologic study demonstrated that co-exposure to tobacco and cannabis may influence postnatal growth. Girls appeared to be more susceptible than boys. However, the effects of cannabis could not be differentiated from that of tobacco.
Koto P, Allen VM, Fahey J, Kuhle S. Maternal cannabis use during pregnancy and maternal and neonatal outcomes: a retrospective cohort study. BJOG. 2022;129(10):1687–94. https://doi.org/10.1111/1471-0528.17114.
Luke S, Hobbs AJ, Smith M, Riddell C, Murphy P, Agborsangaya C, et al. Cannabis use in pregnancy and maternal and infant outcomes: a Canadian cross-jurisdictional population-based cohort study. PLoS ONE. 2022;17(11):e0276824. https://doi.org/10.1371/journal.pone.0276824.
Mark K, Crimmins S. Maternal and infant cannabis testing and associated birth outcomes. Arch Gynecol Obstet. 2023 May 11. https://doi.org/10.1007/s00404-023-07009-5. Epub ahead of print. PMID: 37166490.
Michalski CA, Hung RJ, Seeto RA, Dennis CL, Brooks JD, Henderson J, et al. Association between maternal cannabis use and birth outcomes: an observational study. BMC Pregnancy Childbirth. 2020;20(1):771. https://doi.org/10.1186/s12884-020-03371-3.
•• Moore BF, Sauder KA, Shapiro ALB, Crume T, Kinney GL, Dabelea D. Fetal Exposure to Cannabis and childhood metabolic outcomes: the Healthy Start Study. J Clin Endocrinol Metab. 2022;107(7):e2862–9. https://doi.org/10.1210/clinem/dgac101. This epidemiologic study demonstrated that biomarker-confirmed fetal exposure to cannabis was associated with increased adiposity and fasting glucose levels in early childhood.
Nguyen VH, Harley KG. Prenatal cannabis use and infant birth outcomes in the Pregnancy Risk Assessment Monitoring System. J Pediatr. 2022;240:87–93. https://doi.org/10.1016/j.jpeds.2021.08.088.
O’Connor AB, Kelly BK, O’Brien LM. Maternal and infant outcomes following third trimester exposure to marijuana in opioid dependent pregnant women maintained on buprenorphine. Drug Alcohol Depend. 2017;180:200–3. https://doi.org/10.1016/j.drugalcdep.2017.08.012.
Paul SE, Hatoum AS, Fine JD, Johnson EC, Hansen I, Karcher NR, et al. Associations between prenatal cannabis exposure and childhood outcomes: results from the ABCD Study. JAMA Psychiat. 2021;78(1):64–76. https://doi.org/10.1001/jamapsychiatry.2020.2902.
Roca A, Jarque P, Gomila I, Marchei E, Tittarelli R, Elorza M, et al. Clinical features and risk factors associated with prenatal exposure to drugs of abuse. An Pediatr (Engl Ed). 2021;95(5):307–20. https://doi.org/10.1016/j.anpede.2020.08.013.
Shi Y, Zhu B, Liang D. The associations between prenatal cannabis use disorder and neonatal outcomes. Addiction. 2021;116(11):3069–79. https://doi.org/10.1111/add.15467.
Stein Y, Hwang S, Liu CL, Diop H, Wymore E. The association of concomitant maternal marijuana use on health outcomes for opioid exposed newborns in Massachusetts, 2003–2009. J Pediatr. 2020;218:238–42. https://doi.org/10.1016/j.jpeds.2019.10.071.
Straub HL, Mou J, Drennan KJ, Pflugeisen BM. Maternal marijuana exposure and birth weight: an observational study surrounding recreational marijuana legalization. Am J Perinatol. 2021;38(1):65–75. https://doi.org/10.1055/s-0039-1694793.
Sturrock S, Williams E, Ambulkar H, Dassios T, Greenough A. Maternal smoking and cannabis use during pregnancy and infant outcomes. J Perinat Med. 2020;48(2):168–72. https://doi.org/10.1515/jpm-2019-0422.
Umer A, Watson E, Lilly C, Woods S, Lefeber C, Breyel J, et al. Substance exposure and adverse neonatal outcomes: a population-based cohort study. J Pediatr. 2023;256:70–6. https://doi.org/10.1016/j.jpeds.2022.11.040.
Warshak CR, Regan J, Moore B, Magner K, Kritzer S, Van Hook J. Association between marijuana use and adverse obstetrical and neonatal outcomes. J Perinatol. 2015;35(12):991–5. https://doi.org/10.1038/jp.2015.120.
Metz TD, Allshouse AA, Pinar H, Varner M, Smid MC, Hogue C, et al. Maternal marijuana exposure, feto-placental weight ratio, and placental histology. Am J Perinatol. 2022;39(5):546–53. https://doi.org/10.1055/s-0040-1717092.
Dodge P, Nadolski K, Kopkau H, Zablocki V, Forrestal K, Bailey BA. The impact of timing of in utero marijuana exposure on fetal growth. Front Pediatr. 2023 May 16;11:1103749. https://doi.org/10.3389/fped.2023.1103749. PMID: 37260795; PMCID: PMC10228645.
Coleman-Cowger VH, Oga EA, Peters EN, Mark K. Prevalence and associated birth outcomes of co-use of cannabis and tobacco cigarettes during pregnancy. Neurotoxicol Teratol. 2018;68:84–90. https://doi.org/10.1016/j.ntt.2018.06.001.
Haight SC, King BA, Bombard JM, Coy KC, Ferré CD, Grant AM, et al. Frequency of cannabis use during pregnancy and adverse infant outcomes, by cigarette smoking status - 8 PRAMS states, 2017. Drug Alcohol Depend. 2021;220:108507. https://doi.org/10.1016/j.drugalcdep.2021.108507.
Prewitt KC, Hayer S, Garg B, Benson AE, Hedges MA, Caughey AB, Lo JO. Impact of prenatal cannabis use disorder on perinatal outcomes. J Addict Med. 2023 May-Jun 01;17(3):e192–e198. https://doi.org/10.1097/ADM.0000000000001123. Epub 2022 Dec 13. PMID: 37267181; PMCID: PMC10248186.
Oni HT, Buultjens M, Mohamed AL, Islam MM. Neonatal outcomes of infants born to pregnant women with substance use disorders: a multilevel analysis of linked data. Subst Use Misuse. 2022;57(1):1–10. https://doi.org/10.1080/10826084.2021.1958851.
Luke S, Hutcheon J, Kendall T. Cannabis use in pregnancy in British Columbia and selected birth outcomes. J Obstet Gynaecol Can. 2019;41(9):1311–7. https://doi.org/10.1016/j.jogc.2018.11.014.
Rodriguez CE, Sheeder J, Allshouse AA, Scott S, Wymore E, Hopfer C, et al. Marijuana use in young mothers and adverse pregnancy outcomes: a retrospective cohort study. BJOG. 2019;126(12):1491–7. https://doi.org/10.1111/1471-0528.15885.
Leemaqz SY, Dekker GA, McCowan LM, Kenny LC, Myers JE, Simpson NA, et al. Maternal marijuana use has independent effects on risk for spontaneous preterm birth but not other common late pregnancy complications. Reprod Toxicol. 2016;62:77–86. https://doi.org/10.1016/j.reprotox.2016.04.021.
Dotters-Katz SK, Smid MC, Manuck TA, Metz TD. Risk of neonatal and childhood morbidity among preterm infants exposed to marijuana. J Matern Fetal Neonatal Med. 2017;30(24):2933–9. https://doi.org/10.1080/14767058.2016.1269165.
Metz TD, Allshouse AA, Hogue CJ, Goldenberg RL, Dudley DJ, Varner MW, et al. Maternal marijuana use, adverse pregnancy outcomes, and neonatal morbidity. Am J Obstet Gynecol. 2017;217(4):478.e1–.e8. https://doi.org/10.1016/j.ajog.2017.05.050.
Massey SH, Mroczek DK, Reiss D, Miller ES, Jakubowski JA, Graham EK, et al. Additive drug-specific and sex-specific risks associated with co-use of marijuana and tobacco during pregnancy: evidence from 3 recent developmental cohorts (2003–2015). Neurotoxicol Teratol. 2018;68:97–106. https://doi.org/10.1016/j.ntt.2018.06.002.
Corsi DJ, Walsh L, Weiss D, Hsu H, El-Chaar D, Hawken S, et al. Association between self-reported prenatal cannabis use and maternal, perinatal, and neonatal outcomes. JAMA. 2019;322(2):145–52. https://doi.org/10.1001/jama.2019.8734.
Shah DS, Turner EL, Chroust AJ, Duvall KL, Wood DL, Bailey BA. Marijuana use in opioid exposed pregnancy increases risk of preterm birth. J Matern Fetal Neonatal Med. 2022;35(25):8456–61. https://doi.org/10.1080/14767058.2021.1980532.
Breit KR, Rodriguez CG, Lei A, Thomas JD. Combined vapor exposure to THC and alcohol in pregnant rats: maternal outcomes and pharmacokinetic effects. Neurotoxicol Teratol. 2020;82:106930. https://doi.org/10.1016/j.ntt.2020.106930.
•• Gillies R, Lee K, Vanin S, Laviolette SR, Holloway AC, Arany E, et al. Maternal exposure to Δ9-tetrahydrocannabinol impairs female offspring glucose homeostasis and endocrine pancreatic development in the rat. Reprod Toxicol. 2020;94:84–91. https://doi.org/10.1016/j.reprotox.2020.04.070. In this Wistar rat model, fetal exposure to Δ9-THC was associated with female-specific impairments in glucose homeostasis. These findings were later supported in human study (see Moore et al. 2022).
Iezzi D, Caceres-Rodriguez A, Chavis P, Manzoni OJJ. In utero exposure to cannabidiol disrupts select early-life behaviors in a sex-specific manner. Transl Psychiatry. 2022;12(1):501. https://doi.org/10.1038/s41398-022-02271-8.
Lallai V, Manca L, Sherafat Y, Fowler CD. Effects of prenatal nicotine, THC, or co-exposure on cognitive behaviors in adolescent male and female rats. Nicotine Tob Res. 2022;24(8):1150–60. https://doi.org/10.1093/ntr/ntac018.
•• Lee K, Laviolette SR, Hardy DB. Exposure to Δ9-tetrahydrocannabinol during rat pregnancy leads to impaired cardiac dysfunction in postnatal life. Pediatr Res. 2021;90(3):532–9. https://doi.org/10.1038/s41390-021-01511-9. This study found that prenatal exposure to Δ9-THC was associated with fetal growth restriction and impaired cardiac function in the Wistar rat offspring.
Natale BV, Gustin KN, Lee K, Holloway AC, Laviolette SR, Natale DRC, et al. Δ9-Tetrahydrocannabinol exposure during rat pregnancy leads to symmetrical fetal growth restriction and labyrinth-specific vascular defects in the placenta. Sci Rep. 2020;10(1):544. https://doi.org/10.1038/s41598-019-57318-6.
•• Oke SL, Lee K, Papp R, Laviolette SR, Hardy DB. In utero exposure to Δ9-tetrahydrocannabinol leads to postnatal catch-up growth and dysmetabolism in the adult rat liver. Int J Mol Sci. 2021 Jul 13;22(14):7502. https://doi.org/10.3390/ijms22147502. PMID: 34299119; PMCID: PMC8305322. The study demonstrated that prenatal exposure to Δ9-THC is associated with long-term dyslipidemia and provides evidence for plausible biological mechansims (enhanced hepatic lipogenesis, mitochondrial dysfunction, and epigenetic mechanisms).
• Robinson GI, Ye F, Lu X, Laviolette SR, Feng Q. Maternal delta-9-tetrahydrocannabinol exposure induces abnormalities of the developing heart in mice. Cannabis Cannabinoid Res. 2022 Oct 17. https://doi.org/10.1089/can.2022.0180. Epub ahead of print. PMID: 36255470. This mouse model demonstrated that prenatal exposure to Δ9-THC may result in abnormalities in fetal heart development in mice, leading to postnatal cardiac dysfunction. These results are consistent with the work of Lee et al. (2021) and provide a potnetial mechanism for the cannabis-cardiovascular association.
Wanner NM, Colwell M, Drown C, Faulk C. Developmental cannabidiol exposure increases anxiety and modifies genome-wide brain DNA methylation in adult female mice. Clin Epigenetics. 2021;13(1):4. https://doi.org/10.1186/s13148-020-00993-4.
Asadi F, Fernandez Andrade JA, Gillies R, Lee K, Dhanvantari S, Hardy DB, et al. Sex-dependent effect of in-utero exposure to Δ(9-)tetrahydrocannabinol on glucagon and stathmin-2 in adult rat offspring. Can J Diabetes. 2022;46(8):851–62. https://doi.org/10.1016/j.jcjd.2022.06.009.
Benevenuto SG, Domenico MD, Martins MAG, Costa NS, de Souza ARL, Costa JL, et al. Recreational use of marijuana during pregnancy and negative gestational and fetal outcomes: an experimental study in mice. Toxicology. 2017;376:94–101. https://doi.org/10.1016/j.tox.2016.05.020.
Maciel IS, Abreu GHD, Johnson CT, Bonday R, Bradshaw HB, Mackie K, et al. Perinatal CBD or THC exposure results in lasting resistance to fluoxetine in the forced swim test: reversal by fatty acid amide hydrolase inhibition. Cannabis Cannabinoid Res. 2022;7(3):318–27. https://doi.org/10.1089/can.2021.0015.
de Wit CC, Sas TC, Wit JM, Cutfield WS. Patterns of catch-up growth. J Pediatr. 2013;162(2):415–20. https://doi.org/10.1016/j.jpeds.2012.10.014.
Cettour-Rose P, Samec S, Russell AP, Summermatter S, Mainieri D, Carrillo-Theander C, et al. Redistribution of glucose from skeletal muscle to adipose tissue during catch-up fat: a link between catch-up growth and later metabolic syndrome. Diabetes. 2005;54(3):751–6. https://doi.org/10.2337/diabetes.54.3.751.
Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia. 1993;36(1):62–7. https://doi.org/10.1007/bf00399095.
Chang X, Li H, Li Y, He Q, Yao J, Duan T, et al. RhoA/MLC signaling pathway is involved in Δ9-tetrahydrocannabinol-impaired placental angiogenesis. Toxicol Lett. 2018;285:148–55. https://doi.org/10.1016/j.toxlet.2017.12.031.
Dulloo AG. Regulation of fat storage via suppressed thermogenesis: a thrifty phenotype that predisposes individuals with catch-up growth to insulin resistance and obesity. Horm Res. 2006;65(Suppl 3):90–7. https://doi.org/10.1159/000091512.
Teixeira D, Pestana D, Faria A, Calhau C, Azevedo I, Monteiro R. Modulation of adipocyte biology by δ(9)-tetrahydrocannabinol. Obesity (Silver Spring, Md). 2010;18(11):2077–85. https://doi.org/10.1038/oby.2010.100.
Chang RC, Thangavelu CS, Joloya EM, Kuo A, Li Z, Blumberg B. Cannabidiol promotes adipogenesis of human and mouse mesenchymal stem cells via PPARγ by inducing lipogenesis but not lipolysis. Biochem Pharmacol. 2022;197:114910. https://doi.org/10.1016/j.bcp.2022.114910.
Desai M, Beall M, Ross MG. Developmental origins of obesity: programmed adipogenesis. Curr Diab Rep. 2013;13(1):27–33. https://doi.org/10.1007/s11892-012-0344-x.
DiNieri JA, Wang X, Szutorisz H, Spano SM, Kaur J, Casaccia P, et al. Maternal cannabis use alters ventral striatal dopamine D2 gene regulation in the offspring. Biol Psychiat. 2011;70(8):763–9. https://doi.org/10.1016/j.biopsych.2011.06.027.
de Almeida DL, Devi LA. Diversity of molecular targets and signaling pathways for CBD. Pharmacol Res Perspect. 2020;8(6):e00682. https://doi.org/10.1002/prp2.682.
Traccis F, Serra V, Sagheddu C, Congiu M, Saba P, Giua G, Devoto P, Frau R, Cheer JF, Melis M. Prenatal THC does not affect female mesolimbic dopaminergic system in preadolescent rats. Int J Mol Sci. 2021;22(4). https://doi.org/10.3390/ijms22041666. PMID: 33562259; PMCID: PMC7914408.
Frau R, Miczán V, Traccis F, Aroni S, Pongor CI, Saba P, et al. Prenatal THC exposure produces a hyperdopaminergic phenotype rescued by pregnenolone. Nat Neurosci. 2019;22(12):1975–85. https://doi.org/10.1038/s41593-019-0512-2.
Fernández-Ruiz J, Berrendero F, Hernández ML, Ramos JA. The endogenous cannabinoid system and brain development. Trends Neurosci. 2000;23(1):14–20. https://doi.org/10.1016/s0166-2236(99)01491-5.
Rossi F, Punzo F, Umano GR, Argenziano M, Miraglia Del Giudice E. Role of cannabinoids in obesity. Int J Mol Sci. 2018;19(9):2690. https://doi.org/10.3390/ijms19092690.
Nogueiras R, Rohner-Jeanrenaud F, Woods SC, Tschöp MH. The endocannabinoid system and the control of glucose homeostasis. J Neuroendocrinol. 2008;20(Suppl 1):147–51. https://doi.org/10.1111/j.1365-2826.2008.01692.x.
Bermúdez-Silva FJ, Suárez J, Baixeras E, Cobo N, Bautista D, Cuesta-Muñoz AL, et al. Presence of functional cannabinoid receptors in human endocrine pancreas. Diabetologia. 2008;51(3):476–87. https://doi.org/10.1007/s00125-007-0890-y.
Malenczyk K, Keimpema E, Piscitelli F, Calvigioni D, Björklund P, Mackie K, et al. Fetal endocannabinoids orchestrate the organization of pancreatic islet microarchitecture. Proc Natl Acad Sci USA. 2015;112(45):E6185–94. https://doi.org/10.1073/pnas.1519040112.
Klawitter J, Sempio C, Morlein S, De Bloois E, Klepacki J, Henthorn T, et al. An atmospheric pressure chemical ionization MS/MS assay using online extraction for the analysis of 11 cannabinoids and metabolites in human plasma and urine. Ther Drug Monit. 2017;39(5):556–64. https://doi.org/10.1097/ftd.0000000000000427.
Selzer S, Morrison G, Bensadigh BM, Gelber K, Geller AW, Zakowski MI. Cannabidiol in pregnancy: attitudes of obstetric-related healthcare providers and women 18–44 years-old in California.
De Genna NM, Kennon-McGill S, Goldschmidt L, Richardson GA, Chang JC. Factors associated with ever using cannabidiol in a cohort of younger pregnant people. Neurotoxicol Teratol. 2023;96:107162. https://doi.org/10.1016/j.ntt.2023.107162.
Foltin RW, Fischman MW, Byrne MF. Effects of smoked marijuana on food intake and body weight of humans living in a residential laboratory. Appetite. 1988;11(1):1–14. https://doi.org/10.1016/s0195-6663(88)80017-5.
Pinto JS, Martel F. Effects of cannabidiol on appetite and body weight: a systematic review. Clin Drug Investig. 2022;42(11):909–19. https://doi.org/10.1007/s40261-022-01205-y.
Hollister LE, Reaven GM. Delta-9-tetrahydrocannabinol and glucose tolerance. Clin Pharmacol Ther. 1974;16(2):297–302. https://doi.org/10.1002/cpt1974162297.
King AB, Cowen DL. Effect of intravenous injection of marihuana. JAMA. 1969;210(4):724–5. https://doi.org/10.1001/jama.1969.03160300064021.
Hughes JE, Steahly LP, Bier MM. Marihuana and the diabetic coma. JAMA. 1970;214(6):1113–4.
Afshar S, Khalili S, Amin G, Abbasinazari M. A phase I randomized, double-blind, placebo-controlled study on efficacy and safety profile of a sublingually administered cannabidiol /delta 9-tetrahydrocannabidiol (10: 1) regimen in diabetes type 2 patients. Iran J Pharm Res. 2022;21(1):e132647. https://doi.org/10.5812/ijpr-132647.
Jadoon KA, Ratcliffe SH, Barrett DA, Thomas EL, Stott C, Bell JD, et al. Efficacy and safety of cannabidiol and tetrahydrocannabivarin on glycemic and lipid parameters in patients with type 2 Diabetes: a randomized, double-blind, placebo-controlled, parallel group pilot study. Diabetes Care. 2016;39(10):1777–86. https://doi.org/10.2337/dc16-0650.
Symonds ME, Pope M, Sharkey D, Budge H. Adipose tissue and fetal programming. Diabetologia. 2012;55(6):1597–606. https://doi.org/10.1007/s00125-012-2505-5.
Hines LA, Spry EA, Moreno-Betancur M, Mohamad Husin H, Becker D, Middleton M, et al. Cannabis and tobacco use prior to pregnancy and subsequent offspring birth outcomes: a 20-year intergenerational prospective cohort study. Sci Rep. 2021;11(1):16826. https://doi.org/10.1038/s41598-021-95460-2.
Kaforau LS, Tessema GA, Jancey J, Bugoro H, Pereira G. Prevalence and factors associated with low birth weight in the Solomon Islands: evidence from the 2015 Solomon Islands demographic and Health survey data. Asia Pac J Public Health. 2023;35(2–3):136–44. https://doi.org/10.1177/10105395231158868.
Misner MJ, Taborek A, Dufour J, Sharifi L, Khokhar JY, Favetta LA. Effects of delta-9 tetrahydrocannabinol (THC) on oocyte competence and early embryonic development. Front Toxicol. 2021;3:647918. https://doi.org/10.3389/ftox.2021.647918.
Murphy SK, Itchon-Ramos N, Visco Z, Huang Z, Grenier C, Schrott R, et al. Cannabinoid exposure and altered DNA methylation in rat and human sperm. Epigenetics. 2018;13(12):1208–21. https://doi.org/10.1080/15592294.2018.1554521.
Levin ED, Hawkey AB, Hall BJ, Cauley M, Slade S, Yazdani E, et al. Paternal THC exposure in rats causes long-lasting neurobehavioral effects in the offspring. Neurotoxicol Teratol. 2019;74:106806. https://doi.org/10.1016/j.ntt.2019.04.003.
Goodwin RD, Kim JH, Cheslack-Postava K, Weinberger AH, Wu M, Wyka K, et al. Trends in cannabis use among adults with children in the home in the United States, 2004–2017: impact of state-level legalization for recreational and medical use. Addiction. 2021;116(10):2770–8. https://doi.org/10.1111/add.15472.
Moore BF, Salmons KA, Hoyt AT, Swenson KS, Bates EA, Sauder KA, et al. Associations between prenatal and postnatal exposure to cannabis with cognition and behavior at age 5 years: the Healthy Start Study. Int J Environ Res Public Health. 2023;20(6):4880. https://doi.org/10.3390/ijerph20064880.
Wilson KM, Torok MR, Wei B, Wang L, Robinson M, Sosnoff CS, et al. Detecting biomarkers of secondhand marijuana smoke in young children. Pediatr Res. 2017;81(4):589–92. https://doi.org/10.1038/pr.2016.261.
Sangmo L, Braune T, Liu B, Wang L, Zhang L, Sosnoff CS, et al. Secondhand marijuana exposure in a convenience sample of young children in New York City. Pediatr Res. 2021;89(4):905–10. https://doi.org/10.1038/s41390-020-0958-7.
Sempio C, Wymore E, Palmer C, Bunik M, Henthorn TK, Christians U, et al. Detection of cannabinoids by LC-MS-MS and ELISA in breast milk. J Anal Toxicol. 2021;45(7):686–92. https://doi.org/10.1093/jat/bkaa142.
Sempio C, Lindley E, Klawitter J, Christians U, Bowler RP, Adgate JL, et al. Surface detection of THC attributable to vaporizer use in the indoor environment. Sci Rep. 2019;9(1):18587. https://doi.org/10.1038/s41598-019-55151-5.
Xue J, Zartarian V, Moya J, Freeman N, Beamer P, Black K, et al. A meta-analysis of children’s hand-to-mouth frequency data for estimating nondietary ingestion exposure. Risk Anal. 2007;27(2):411–20. https://doi.org/10.1111/j.1539-6924.2007.00893.x.
Fleming S, Thompson M, Stevens R, Heneghan C, Plüddemann A, Maconochie I, et al. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet (London, England). 2011;377(9770):1011–8. https://doi.org/10.1016/S0140-6736(10)62226-X.
Ohlsson A, Lindgren JE, Wahlen A, Agurell S, Hollister LE, Gillespie HK. Plasma delta-9 tetrahydrocannabinol concentrations and clinical effects after oral and intravenous administration and smoking. Clin Pharmacol Ther. 1980;28(3):409–16. https://doi.org/10.1038/clpt.1980.181.
Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42(4):327–60. https://doi.org/10.2165/00003088-200342040-00003.
Gaston TE, Friedman D. Pharmacology of cannabinoids in the treatment of epilepsy. Epilepsy Behav. 2017;70(Pt B):313–8. https://doi.org/10.1016/j.yebeh.2016.11.016.
Young-Wolff KC, Adams SR, Wi S, Weisner C, Conway A. Routes of cannabis administration among females in the year before and during pregnancy: results from a pilot project. Addict Behav. 2020;100:106125. https://doi.org/10.1016/j.addbeh.2019.106125.
Hatch EE, Bracken MB. Effect of marijuana use in pregnancy on fetal growth. Am J Epidemiol. 1986;124(6):986–93. https://doi.org/10.1093/oxfordjournals.aje.a114488.
Rosen TS, Bateman D. Chapter 1 - the effects of gender in neonatal medicine. In: Legato MJ, editor. Principles of Gender-Specific Medicine. 2nd ed. San Diego: Academic Press; 2010. p. 3–17.
Broere-Brown ZA, Baan E, Schalekamp-Timmermans S, Verburg BO, Jaddoe VW, Steegers EA. Sex-specific differences in fetal and infant growth patterns: a prospective population-based cohort study. Biol Sex Differ. 2016;7:65. https://doi.org/10.1186/s13293-016-0119-1.
Craft RM, Marusich JA, Wiley JL. Sex differences in cannabinoid pharmacology: a reflection of differences in the endocannabinoid system? Life Sci. 2013;92(8–9):476–81. https://doi.org/10.1016/j.lfs.2012.06.009.
Jeffery SC, Hosking J, Jeffery AN, Murphy MJ, Voss LD, Wilkin TJ, et al. Insulin resistance is higher in prepubertal girls but switches to become higher in boys at age 16: a cohort study (EarlyBird 57). Pediatr Diabetes. 2018;19(2):223–30. https://doi.org/10.1111/pedi.12571.
Pramfalk C, Pavlides M, Banerjee R, McNeil CA, Neubauer S, Karpe F, et al. Sex-specific differences in hepatic fat oxidation and synthesis may explain the higher propensity for NAFLD in men. J Clin Endocrinol Metab. 2015;100(12):4425–33. https://doi.org/10.1210/jc.2015-2649.
Tran C, Jacot-Descombes D, Lecoultre V, Fielding BA, Carrel G, Lê KA, et al. Sex differences in lipid and glucose kinetics after ingestion of an acute oral fructose load. Br J Nutr. 2010;104(8):1139–47. https://doi.org/10.1017/s000711451000190x.
Agrawal A, Rogers CE, Lessov-Schlaggar CN, Carter EB, Lenze SN, Grucza RA. Alcohol, cigarette, and cannabis use between 2002 and 2016 in pregnant women from a nationally representative sample. JAMA Pediatr. 2019;173(1):95–6. https://doi.org/10.1001/jamapediatrics.2018.3096.
Funding
This study is funded (R00ES028711).
Author information
Authors and Affiliations
Contributions
B.F.M. designed and implemented the study design, wrote the paper, and prepared all tables and figures.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moore, B.F. Prenatal Exposure to Cannabis: Effects on Childhood Obesity and Cardiometabolic Health. Curr Obes Rep 13, 154–166 (2024). https://doi.org/10.1007/s13679-023-00544-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-023-00544-x