Abstract
Objectives
The objective of the study was to determine any identifiable clinical utility of the practice of universal maternal and infant tetrahydrocannabinol (THC) testing at the time of birth.
Methods
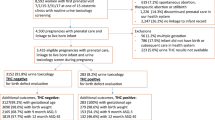
This was cross-sectional, retrospective cohort study comparing the following birth outcomes in relation to maternal and infant tetrahydrocannabinol (THC): APGAR scores, cord gases, NICU admission and need for immediate resuscitation. All births at the University of Maryland Medical Center between January 1, 2018 and December 31, 2020 were reviewed. Those that had either maternal or infant test results missing were excluded. Statistical analysis was performed using STATA v27. Birth outcomes were adjusted for gestational age at delivery and tobacco use. Infant resuscitation was considered the need for any respiratory support.
Results
A total of 4260 maternal/infant pairs were included. Of these, 314 (7.4%) birthing parents and 161 (3.8%) of infants tested positive for THC. Of the birth parents who tested positive for THC, 51.3% of their infants also tested positive for THC. Maternal/infant pairs that both tested positive for THC had the lowest need for immediate resuscitation and Neonatal Intensive Care Unit admission. Cord gases and APGAR scores were similar between the groups. Birth parents who tested positive for THC delivered infants at an earlier gestational age (37w6d v 38w5d, p = 0.001) and lower mean birth weight (2690gm v 3061gm, p = 0.001) than those who tested negative even after adjusting for confounders. When limited to only term births and broken down by weeks completed gestation, the mean birth weights were lower for every week in those who tested positive for THC versus those who tested negative.
Conclusions
Our study shows that maternal and neonatal testing for THC at the time of birth is not predictive of important neonatal outcome parameters. Therefore, even though it is likely that there are some effects of in utero THC exposure on the neonate, we did not find any clinical benefits that would justify routine maternal and/or infant testing for THC at the time of birth.

Similar content being viewed by others
Data availability
Data supporting this study are available upon request.
References
Volkow ND et al (2019) Self-reported medical and nonmedical cannabis use among pregnant women in the United States. JAMA 322(2):167–169
Gunn JK et al (2016) Prenatal exposure to cannabis and maternal and child health outcomes: a systematic review and meta-analysis. BMJ Open 6(4):e009986
Conner SN et al (2016) Maternal Marijuana Use and adverse neonatal outcomes: a systematic review and meta-analysis. Obstet Gynecol 128(4):713–723
Metz TD, Borgelt LM (2018) Marijuana use in pregnancy and while breastfeeding. Obstet Gynecol 132(5):1198–1210
Corsi DJ et al (2020) Maternal cannabis use in pregnancy and child neurodevelopmental outcomes. Nat Med 26(10):1536–1540
El Marroun H et al (2018) An epidemiological, developmental and clinical overview of cannabis use during pregnancy. Prev Med 116:1–5
Richardson KA, Hester AK, McLemore GL (2016) Prenatal cannabis exposure - The “first hit” to the endocannabinoid system. Neurotoxicol Teratol 58:5–14
Committee Opinion No (2017) 722: Marijuana use during pregnancy and lactation. Obstet Gynecol 130(4):e205–e209
Medicine, A.S.O.A. Public Policy Statement on Substance Use, Misuse, and Use Disorders During and Following Pregnancy, with an Emphasis on Opioids.; Available from: https://www.asam.org/docs/default-source/public-policy-statements/substance-use-misuse-and-use-disorders-during-and-following-pregnancy.pdf?sfvrsn=644978c2_4#:~:text=Screening%2FPrevention&text=the%20postpartum%20period.-,b.,who%20meet%20criteria%20for%20SUDs. Accessed 9 Jan 2023
Committee opinion no (2015) 633: Alcohol abuse and other substance use disorders: ethical issues in obstetric and gynecologic practice. Obstet Gynecol 125(6):1529–1537
Wood KE, Smith P, Krasowski MD (2017) Newborn drug testing practices in Iowa birthing hospitals. J Neonatal Perinatal Med 10(4):445–450
Miller C et al (2014) Screening, testing, and reporting for drug and alcohol use on labor and delivery: a survey of Maryland birthing hospitals. Soc Work Health Care 53(7):659–669
Mark K et al (2021) Concordance and discordance between maternal and newborn drug test results. Am J Obstet Gynecol MFM 3(4):100366
El Marroun H et al (2009) Intrauterine cannabis exposure affects fetal growth trajectories: the generation R study. J Am Acad Child Adolesc Psychiatry 48(12):1173–1181
Funding
The authors declare that no funds, grants or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
KM: protocol/project development, data collection, and manuscript preparation. SC: data analysis and manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no relevant conflicts of interest. The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
None.
Informed consent
Informed consent was waived as the study was retrospective and determined to be minimal risk.
IRB
IRB approval was obtained for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mark, K., Crimmins, S. Maternal and infant cannabis testing and associated birth outcomes. Arch Gynecol Obstet 309, 1903–1907 (2024). https://doi.org/10.1007/s00404-023-07009-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-07009-5