Abstract
Purpose of Review
The purpose of this study is to evaluate the effectiveness of eHealth interventions for weight loss and weight loss maintenance among adults with overweight or obesity through a systematic review of systematic reviews.
Recent Findings
This study included 26 systematic reviews, covering a total of 338 original studies, published between 2018 and 2023. The review indicates that eHealth interventions are more effective than control interventions or no care and comparable to face-to-face interventions. The effect sizes remain relatively small when comparing eHealth interventions to any control conditions, with mean differences of weight loss results from − 0.12 kg (95% CI − 0.64 to 0.41 kg) in a review comparing eHealth interventions to face-to-face care to − 4.32 kg (− 5.08 kg to − 3.57 kg) in a review comparing eHealth interventions to no care. The methodological quality of the included studies varies considerably. However, it can be concluded that interventions with human contact work better than those that are fully automated.
Summary
In conclusion, this systematic review of systematic reviews provides an updated understanding of the development of digital interventions in recent years and their effectiveness for weight loss and weight loss maintenance among adults with overweight or obesity. The findings suggest that eHealth interventions can be a valuable tool for delivering obesity care to more patients economically. Further research is needed to determine which specific types of eHealth interventions are most effective and how to best integrate them into clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A range of health complications, including type 2 diabetes, cardiovascular disease, hypertension, sleep apnea, certain forms of cancer, and increased mortality, are associated with obesity [1]. According to the World Health Organization, more than one billion people worldwide are living with obesity, and the number is still increasing [2]. As such, reducing overweight and obesity is the key to public health.
Lifestyle changes, such as adopting a healthy diet and increasing physical activity, are known to be challenging but feasible for achieving long-term weight management or weight loss [3, 4]. Behavioral weight management interventions have been found to result in approximately 2–2.5 kg more weight loss than control conditions at the 12–18 month mark [5, 6]. However, the long-term success in maintaining weight loss is limited, with only about 20% of individuals estimated to keep the weight off for a year or more [7, 8]. Despite this, these interventions are crucial due to their additional advantages, such as preventing diabetes and premature mortality [9].
The multifactorial causes of obesity necessitate targeting different levels of contributing factors (e.g., social support, favorable environment, individual factors) in obesity treatment. However, there are several challenges in delivering these services in primary care. Weight counseling is perceived as laborious by health professionals, and there is a limited understanding of obesity care and uncertainty about how to initiate a discussion on weight and what is the appropriate terminology and language to use [10, 11]. Effective weight loss requires time, as frequent contact between healthcare professionals and patients is associated with greater weight loss outcomes [5]. Limited time and resources, including the organization of weight management groups or provision of constructive support, are frequently cited as obstacles to individual-level obesity treatment [10, 11].
Digital health, defined by the World Health Organization as the use of information and communication technologies for improving health, has been proposed as a solution to promote healthy lives and well-being for people of all ages [12]. This novel approach is also suitable for reducing obesity as it can recognize the complexity of obesity and provide patient-centered, multidisciplinary care that considers the personalized needs of individuals living with obesity. Digital health technologies also have the potential to reach a considerable number of people and improve access to obesity care as well as reduce the costs of healthcare systems as they are cost-effective [13, 14]. Furthermore, digital health tools are accessible to a wide range of people regardless of their location or physical abilities and are flexibly available in terms of time.
The COVID-19 pandemic expedited the need and development of healthcare provided in ways other than in person. The interest in eHealth grew, and new innovations emerged. This time also prompted a welcomed uprising in eHealth research. Obesity was early on recognized as a risk factor for COVID-19 complications [15]. Thus, digital weight loss interventions were of more interest than ever before.
Even prior to the pandemic, digital weight loss and weight maintenance programs were already gaining popularity. As more trials were conducted, numerous systematic reviews were published to conclude their effectiveness and components. This article aims to review the past five years of systematic reviews on eHealth weight loss and weight maintenance interventions to provide an updated understanding of the development of digital interventions in recent years. Our primary focus is to offer a comprehensive overview of the effectiveness of eHealth interventions for weight loss and weight loss maintenance among adults with overweight or obesity.
Methods
We followed guidelines for conducting systematic reviews of systematic reviews suggested by Smith et al. [16] as well as the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [17]. We followed a pre-defined, albeit not prospectively registered, protocol.
Inclusion and Exclusion Criteria
We followed the PICOS (population, intervention, control, outcome, study design) framework when formulating our inclusion and exclusion criteria (Table 1). We defined eHealth interventions as interventions delivered via websites, mobile phone applications, or other kinds of online programs with electronic components. This excluded interventions delivered solely through, e.g., phone or video calls, short messaging services (SMS), electronic chats, social media groups, or email, or the use of wearable devices without an accompanying eHealth intervention. We also excluded digital tools used outside an eHealth intervention design (e.g., meal logging applications combined with standard care) and interventions without interactivity (e.g., information-only website). We included only interventions for weight loss or weight loss maintenance rather than interventions for treating any specific underlying disease (e.g., type 2 diabetes, metabolic syndrome, hypertension, cardiovascular risk factors, or cancer). We also excluded studies focusing on lifestyle change, rather than weight loss or weight loss maintenance (such as interventions focusing solely on increasing vegetable and fruit intake, reducing sedentary behavior, or increasing physical activity).
Search Methods
We searched several databases, including PubMed, Ovid Medline, PsycNet, Scopus, Web of Science, Cochrane Library, Global Index Medicus, and the Centre for Review and Dissemination.
To make the searches as comprehensive as possible, we identified several search term synonyms for population (obesity, obese, overweight) and intervention (telemedicine, telehealth, digital health, eHealth, mHealth, web-based), utilizing and expanding Medical Subject Headings (MeSH) keywords whenever possible. We also combined these search terms with Boolean operators to account for different combinations. While our keywords were in English, we did not limit the search results to any specific language. When possible, we limited the search based on article type (reviews only) and publication date (from January 1st 2018 to February 27th 2023).
We went through the reference lists of included studies to find possible articles not found through our electronic searches. Additionally, we searched the reference lists of non-systematic reviews and umbrella reviews encountered through our primary search. We also searched through several potential databases and registries for gray literature.
A full search strategy, including all searched databases and registries, can be found in the Online Resource.
Selection Process
Two reviewers (SK and AJ) independently screened all records comparing them to the pre-existing inclusion and exclusion criteria. The selection process was carried out in two phases: first, clearly ineligible records were excluded based on their titles and abstracts. Then, full texts were retrieved and analyzed. If the reviewers did not reach consensus on any given reference, a third reviewer (LS) made the decision.
Data Extraction
We extracted basic information from the reviews, including aims, inclusion criteria, number of studies included, age, percentage of women, body mass index (BMI; calculated as weight in kilograms divided by height in meters squared), duration, country or ethnicity of participants, outcomes, behavior change technique employed, and funding sources. For reviews with meta-analysis, we extracted key values such as heterogeneity, arms compared, and effect sizes. Two independent reviewers (SK and AJ) extracted the data used in this study.
Several primary studies were included in multiple meta-analyses included in this review, making a meta-analysis of meta-analyses not viable due to issues related to statistical independence [16].
Methodological Quality Assessment
We evaluated the overall confidence of the results of each review using the AMSTAR 2 tool [18]. It is feasible for evaluating reviews consisting of not only randomized controlled trials (RCTs) but also non-randomized studies of interventions (NRSIs). It consists of 16 items, 13 of which focusing on the review itself and 3 on meta-analysis. The tool is not meant to produce a summary score. Instead, the aim is to evaluate whether the review has one or multiple critical flaws (i.e., suboptimal literature review, risk of bias not discussed adequately, poorly chosen methodology for meta-analysis) or non-critical flaws (i.e., data extraction leaving out important domains, authors not selecting studies or extracting data in duplicate, no list of excluded studies). To score high, the review needs to have no critical weaknesses, and to score moderate, only one critical weakness is accepted. Multiple non-critical weaknesses lower the overall quality of the study.
The developers of AMSTAR 2 encourage that researchers adapt the tool to their specific requirements. For the purpose of this review, we deemed that not including a reference list of excluded studies should not be considered a critical quality flaw. While only a minority of reviews included a reference list of excluded studies, most had stated the number of excluded references for each reason, suggesting that they had documented the reasons for exclusions even if not explicitly reported.
Results
Included Reviews
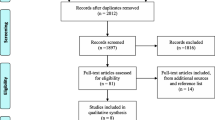
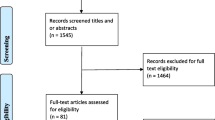
Through our searches, we found 2933 reports in total (Fig. 1). We excluded 581 duplicate reports and 2215 reports not fulfilling our inclusion criteria based on the information provided by their title and abstract. For the remaining 137 reports, we retrieved the full text for further evaluation. After this final evaluation, we included 26 systematic reviews in this review. The exclusion reasons for the other articles retrieved for full text screening can be found in the Online Resource. The 26 included reviews covered a total of 338 original studies (Online Resource).
Description of Included Reviews
Tables 2 and 3 describe the characteristics of the included reviews. Funding information can be found in the Online Resource. Fourteen studies focused on eHealth interventions in a general sense [19,20,21,22,23,24,25,26,27,28,29,30,31,32], five on interventions delivered through mobile phones [33••, 34,35,36,37], and three on interventions combining eHealth and human-delivered care [38•, 39, 40]. One compared web-based interventions to mobile phone applications [41]. One investigated a variety of behavioral and pharmacotherapy weight loss and weight loss maintenance interventions, 20 of which were technology-based [6]. Three studies focused on weight loss maintenance through eHealth interventions [34, 42, 43].
Fourteen of the studies included only RCTs or quasi-RCTs. Most reviews included a majority of trials concluded in the USA, Australia, or the UK. One review focused on only Asian populations [33••]. Most reviews that included information on the gender characteristics reported that a majority of the participants were women. The duration of the interventions ranged from 3 weeks to 24 months. Social cognitive theory was the most often reported theory framework used. Common characteristics of included interventions were self-monitoring, goal setting, social support, and feedback. The methods for follow-up and outcome measures varied considerably between studies. While some studies incorporated scales utilizing wireless communication, most outcome data were self-reported.
Methodological Quality of Included Reviews
We rated two reviews as being of moderate methodological quality [6, 37], 13 as low [19, 20, 23, 25,26,27, 29, 31, 32, 33••, 34, 38•, 43], and 11 as critically low [21, 22, 24, 28, 30, 35, 36, 39,40,41,42]. A detailed evaluation of each AMSTAR 2 criteria can be found in the Online Resource. A considerable number of studies were rated as lower quality because the authors did not justify language restrictions in their search or included studies, did not include a list of excluded studies, or did not justify why they restricted their scope to only some study designs (notably RCTs only). If even one of these issues applicable had been addressed, both studies rated “moderate” and one rated “low” would have been rated “high,” and five of the studies rated “low” would have scored “moderate”. All studies evaluated as being of critically low quality had other substantial flaws and would not have risen in quality appraisal even if the authors addressed these aforementioned issues.
Efficacy of eHealth Interventions for Weight Loss
The effect sizes of individual meta-analyses are reported in Table 4. It also includes measures of heterogeneity, sample size, and number of studies included in the analyses. All in all, eHealth interventions were concluded to have a positive impact on weight loss results. However, across the reviews, effect sizes range from small to moderate, implying that although statistical significance was achieved, the clinical impact may not be substantial. All reviews highlighted notable heterogeneity among the results of the included studies. The results of interventions delivered via smartphone were similar to those delivered via computer.
The results of narrative reviews are described in Table 5. Overall, they concluded that eHealth interventions are associated with weight loss outcomes that are at least comparable, and in some cases superior, to those achieved through control conditions.
eHealth Interventions vs. Any Control Conditions
Seventeen reviews reported weight loss outcomes by comparing intervention effects to any control conditions, including standard care, waitlists, paper-based communication, or minimal interventions such as an educational website or a single face-to-face educational session [19, 20, 22,23,24,25,26,27,28, 30, 31, 34,35,36,37, 40, 42].
The results favored eHealth interventions, with mean differences of statistically significant (P < 0.05) weight loss outcomes ranging from − 1.07 (95% CI − 1.92, − 0.21) kg to − 3.10 (− 4.05, − 2.15) kg for absolute weight change and from − 0.12 (− 0.64, 0.41) kg/m2 to − 0.92 (− 1.10, − 0.74) kg/m2 for changes in BMI. Of the 15 reviews that included meta-analysis, only two did not find significant differences between weight loss outcomes [19, 24]. All 8 narrative reviews concluded that eHealth interventions reach at least similar and often even greater weight loss results than control conditions.
eHealth Interventions vs. No or Minimal Interventions
Three reviews compared eHealth interventions to minimal interventions, finding the former to be more effective. The control conditions varied, but they included no interventions (e.g., waitlist or no care) or minimal interventions (e.g., newsletter or information pamphlet). Podina et al. found effect sizes to be small but consistent across trials (Hedge’s g 0.34 (0.24, 0.44)) [29]. Beleigoli et al. found those in the eHealth intervention to achieve better weight loss results than those on a wait-list (mean difference (MD) − 2.14 (− 2.65, − 1.64) kg, P < 0.001) [19]. Moreover, Varela et al. reported that those in an eHealth intervention with professional feedback at least weekly reached the strongest outcomes compared to those on a wait-list (MD − 4.32 (− 5.08, − 3.57) kg, P < 0.001) while those in a mostly automated eHealth intervention reached slightly weaker results (MD − 3.23 (− 3.80, − 2.66) kg, P < 0.001) [32].
eHealth Interventions Combined with Professional Contact
All three reviews examining the effects of feedback found that eHealth interventions with personalized feedback provided by a health professional were significantly more effective than interventions with no or machine-generated feedback, with mean differences in weight loss outcomes as great as − 4.3 kg (95% CI − 5.08, − 3.57 kg) [25, 26, 32]. Similarly, Varela et al. concluded that web-based interventions with professional contact were more effective than self-help websites (MD − 1.79 (− 2.33, − 1.24) kg) [32].
Both in-person and e-counseling were found to increase intervention success. Puigdomènech et al. concluded that interventions including face-to-face elements obtained the most successful outcomes [37], while Shi et al. found that eHealth interventions with e-counseling had better results than those without (standardized mean difference (SMD) − 0.42 (− 0.75, − 0.08) kg, P = 0.04) [31]. This finding was supported by O’Boyle et al., who found that phone calls, text messages, and e-feedback also enhance intervention success [41]. Besson et al. stated mixed results, where some studies found hybrid interventions to be more effective than eHealth interventions only, while others did not find a difference [21].
Combining face-to-face interventions with an eHealth intervention also leads to enhanced weight loss results. Berry and Sala et al. found that combining human coaching with an automated digital intervention provided better results than coaching alone (MD − 2.18 (− 4.39 kg to − 0.03 kg) and − 2.21% (− 4.49 to 0.08%) in body weight from baseline) [39]. Similarly, both Ang et al. and Antoun et al. found that combining usual care with a mobile application was more effective than usual care alone (Hedge’s g − 0.28 (− 0.47, − 0.09); P < 0.01 and MD − 2.80 (− 3.03, -2.56) kg; P < 0.001, respectively) [33••, 38•]. Surprisingly, Berry and Sala et al. concluded that combined interventions with lower duration or frequency of coach contact (< 10 h) provided better results than interventions with more intensive coaching (> 10 h) (SMD 0.11 (− 0.24, 0.45) kg vs. 0.86 (0.20, 1.52) kg, P = 0.05).
eHealth Interventions vs. Face-to-Face Interventions
Four reviews reported weight loss outcomes in eHealth interventions compared with face-to-face interventions, such as usual care without an eHealth component. Beleigoli et al. found that stand-alone web-based interventions had poorer weight loss outcomes than in-person interventions (MD 0.82 (0.06, 1.59) kg, P = 0.04) [19]. Similarly, Podina et al. found active control groups to have more beneficial results than eHealth groups (Hedge’s g − 0.31 (− 0.43, − 0.20)). On the other hand, Besson et al. found that eHealth interventions could be as successful as active offline comparison interventions or even more effective in the short term [21].
Efficacy of eHealth Interventions for Weight Loss Maintenance
The outcomes of eHealth interventions on weight loss maintenance seem less pronounced than on initial weight loss. Mamalaki et al. found that eHealth interventions produced similar results than minimal interventions while leading to greater weight regain in comparison with in-person care [43]. In contrast, Podina et al. found eHealth interventions to be more effective in weight loss maintenance than passive control conditions, although the effect sizes remained small (Hedge’s g = 0.25 (0.05, 0.46) before and 0.15 (0.02, 0.27) after sensitivity analysis) [29].
Chew et al. found that only 6% (1 out of 16 studies) of included mobile application interventions reported significant weight loss at both 18- and 24-month follow-up [34]. On the other hand, Holmes et al. concluded that digital health technologies aided in weight loss maintenance in short time periods (3–24 months), with four out of seven RCTs reporting significant improvements compared to no contact or in-person care [42].
Discussion
This review article summarizes 26 systematic reviews, covering a total of 338 original studies, that evaluate the efficacy of web-based interventions for weight loss or weight loss maintenance. The review indicates that eHealth interventions are more effective than control interventions or no care and comparable to face-to-face interventions. The effect sizes remain relatively small when comparing eHealth interventions to any control conditions, with mean differences of weight loss results from − 0.12 kg (95% CI − 0.64 to 0.41 kg) in a review comparing eHealth interventions to face-to-face care to − 4.32 kg (− 5.08 kg to − 3.57 kg) in a review comparing eHealth interventions to no care. The methodological quality of the included studies varies considerably. However, it can be concluded that interventions with human contact work better than those that are fully automated.
Features Enhancing Intervention Effect
Features linking effective interventions together were individual feedback, tailored content, self-monitoring, and the use of multiple intervention modalities. A common finding was that interventions with human contact performed better than fully automated interventions. The contact does not have to be time-consuming: Varela et al. found that weekly tailored feedback provided by a professional resulted in more favorable outcomes than no or fully automated feedback [32]. Furthermore, Berry et al. found that when combined with a fully automated intervention, a lighter amount of additional coaching led to greater weight loss results than more intensive coaching [39]. Additionally, personal support has been shown to increase adherence to eHealth interventions [44•, 45,46,47].
The Importance of Cultural and Social Awareness
In cultures that value community and interpersonal relationships, close contact with service providers may lead to more favorable outcomes and greater acceptance of interventions. For instance, Ang et al. [33••] discovered that mobile applications developed for Asian populations were typically culturally adapted and commonly enabled patient-professional communication, whereas applications designed for Western populations often relied on self-directed learning. The authors also emphasized the significance of proper localization, including culturally appropriate advice, locally adapted educational content, and the use of native language. Similarly, Rosenbaum et al. noted that racial minorities were more likely to enroll in trials that used both smartphones and in-person care, suggesting that these populations were seeking social support or a sense of connection to service providers [48].
Cultural and social awareness may also improve the feasibility of eHealth interventions when treating vulnerable groups such as immigrants, aging populations, people with low health literacy, or people with low socioeconomic status [4, 44•, 49, 50••, 51]. It is critical to successfully engage these populations in eHealth interventions because these may provide certain advantages over non-eHealth interventions. For example, because eHealth interventions are multimodal, they can deliver information not only in text but also in video or audio format. Moreover, they may alleviate the burden of limited transportation or caregiving duties [48]. eHealth can also enhance healthcare accessibility for previously underserved populations [52].
From Statistical Significance to Clinical Significance
The majority of trials included in the present reviews reported absolute change in weight (kg) or BMI (kg/m2). While results based on these measures may achieve statistical significance, their clinical significance remains uncertain, particularly given inconsistent reporting of participants’ weight at baseline. We need to know what to compare the results to in order to make meaningful assumptions about the clinical significance based on absolute weight change. For example, a 2 kg weight loss in a person who weighs 70 kg at baseline may be significant, but it is not in a person who weighs 120 kg at baseline.
One way to support the evaluation of clinical significance is to report relative weight change (Δ% from baseline). Although this approach is not without limitations, it does produce more useful results. A 5% weight loss is generally considered clinically significant, and even a 3% weight loss is likely to result in positive health changes [53]. Reporting relative weight change also mitigates distortion of final results caused by participants with widely different baseline weights. It acknowledges that people with higher baseline weights require greater absolute weight loss to achieve clinically significant relative weight loss.
We must also keep in mind that reported effect sizes from meta-analyses only show differences between groups, not how patients’ weight changed from baseline. For example, a mean difference only reflects the difference in means between groups, not the difference in means within groups from baseline. Similarly, when reporting standardized mean differences, the assumption should be that the differences in standard deviations are due to different measurement scales rather than real differences and high variability within study populations. Trials may include participants with a broader range of baseline characteristics, leading to higher standard deviation. Given that the included studies in this review exhibited high heterogeneity, it is reasonable to assume that at least some of the differences in standard deviation were due to this variability. Therefore, effect sizes alone do not provide a reliable estimate of the clinical impact of the interventions.
We Need More Research in Real-Life Settings
While randomized controlled trials are often regarded as the gold standard for intervention research, including non-randomized studies on intervention effects may help us understand how these interventions work in clinical practice. They may be more feasible when addressing long-term outcomes, outcomes in different populations or settings, or alternative methods of intervention delivery. We also know that retention rates may differ between trial and real-life interventions [54]. Subsequently, efficacy information based solely on RCTs conducted in non-real-world settings may not be widely applicable or generalizable when transitioning from trials to healthcare.
Several trials excluded participants with chronic diseases or underlying diagnoses. In reality, many patients with obesity also have concomitant or comorbid diseases such as hypertension, asthma, type 2 diabetes, or heart disease. A recent real-life cohort study by Kupila et al. with nearly 1300 patients enrolled in a digital obesity management program demonstrated that weight loss success was not affected by the number of concurrent diagnoses or medications [55•]. Enrolling a wider selection of patients would likely result in larger trial populations and more clinically generalizable data without introducing significant confounding factors.
Furthermore, we require more long-term research to ascertain the effects of eHealth interventions in managing obesity. Several studies included in the reviews had brief study and follow-up periods. Although these study designs may demonstrate if an eHealth intervention initially works, obesity care and weight management demand long-term and sustainable solutions that integrate into patients’ daily lives. Short-term study durations fail to provide information on how these interventions function in the long run or if their effects last.
We Need a Change from Theory to Practice
Examining a large body of evidence invites us to consider its practical implications. Many trials employ eHealth interventions created specifically for research purposes. While this approach provides valuable information about eHealth interventions themselves, it does not facilitate the much-needed step towards digitalization, unless interventions are developed for use in clinical practice.
The question “does it work?” has been extensively researched, but there is limited knowledge on “how does it work?”. Simply observing impact or efficacy does not help us develop more effective interventions. Many reviews explore and discuss various aspects of successful interventions. While this information is welcome, we need more trials examining underlying factors that influence intervention success. Weight loss outcomes may vary based on intervention details such as theoretical frameworks used, components, amount of human contact, or modes of delivery. They may also vary due to population differences such as age, socioeconomic status, gender, or baseline health status. We need to know what works and with whom in order to not only develop interventions but also deliver them to those who will most likely benefit from them. On the other hand, we must be able to identify those who may need more face-to-face support.
There is relatively little research on intervention acceptability. Not only is an effective intervention necessary, but users must also accept it as part of their care. Reviews have highlighted that eHealth interventions may work, but only if the users adhere. Developing interventions from top to bottom, from researchers and developers to end-users, may overlook any hidden needs or wishes of patients or professionals. This raises critical unanswered questions, such as which types of interventions patients and professionals believe will benefit them the most, what types of feedback or human contact will best support lifestyle change, and what will help users commit to the intervention and empower them to take agency over their own health and care?
Risk of Bias in the Included Studies
The majority of the included reviews excluded studies published in languages other than English. Furthermore, the vast majority of studies were conducted in the USA or Europe, which limits the generalizability of their findings to other populations. Although we searched the Global Index Medicus for potential sources published in low- to middle-income countries, we found none that met our inclusion criteria. Nevertheless, it is important to note that we identified thousands of original articles published in languages other than English when we searched with the same keywords but with no restrictions on publication type.
This suggests that existing systematic reviews may overlook a significant number of available publications by restricting their search language. Consequently, this may introduce language and publication bias and skew our understanding of the impact of eHealth innovations by only considering their impact in Western populations.
Most authors provided the number of full-text articles that were excluded and their reasons for doing so. However, only a few authors provided a list of articles excluded after full-text examination. This lack of transparency reduces the credibility of research findings. Therefore, we suggest that authors include a list of excluded articles in future reviews.
We know that a disproportionate number of weight loss intervention participants drop out during the intervention [56]. We did not examine the attrition rates of included reviews as this was not the purpose of this review. However, for an intervention to be effective, its participants must adhere to it. Weight loss results from only those who completed an intervention may be reported in the absence of an intent-to-treat analysis. When applied to a real-world situation, the outcomes will likely differ. Thus, if attrition rates were reported in the original trials, it would be beneficial to report them in future reviews. This would aid the reader in reaching a deeper understanding of the interventions in question.
Although most reviews with meta-analysis observed no significant publication bias, often concluded by visually inspecting forest plots, only a few reviews in this study compared eHealth research interventions to real-life interventions. This raises the question of whether this is due to a lack of study designs that allow for such comparisons or whether it is an indication of publication bias due to potentially unfavorable results. Furthermore, many reviews limited their search language to English or did not search for gray literature (research produced by organizations outside of the traditional commercial or academic publishing), potentially increasing publication bias. While it could be argued that these restrictions would not have affected the final results in a meaningful way, we have no way of knowing what the true impact would have been in the context of any individual review.
Heterogeneity in the Included Studies
The included reviews generally exhibited a high degree of heterogeneity. The terms “eHealth” and “digital health” lack clear definitions, leading authors to interpret them in their own ways. A single review could have included a variety of intervention modalities, such as phone or video calls, websites, DVDs, rapid messaging, mobile phone applications, or social media. Furthermore, the duration and intensity of the interventions varied, and the participants ranged in age, background, and health status.
With a more focused research question, the included interventions could be narrowed down, resulting in a more uniform review synthesis. This could also be accomplished with adequate subgroup analysis. Combining various interventions in meta-analyses produces non-generalizable results that cannot be interpreted in any specific context. This makes it difficult for clinicians and policymakers to make meaningful recommendations based on available research.
The interventions examined in these reviews were based on a variety of behavior change theories (e.g., the Social Cognitive Theory, the Self-Determination Theory, the Theory of Planned Behavior). It is plausible that frameworks that are effective in real-life settings are also applicable in virtual settings. However, as with most therapeutic interventions, the therapeutic alliance may be a more significant determinant of treatment outcomes than any particular theoretical model [57, 58].
Strengths and Limitations
We only included systematic reviews in this review because they follow a robust and reproducible methodology that aims to find all relevant trials available. Additionally, we screened the reference lists of other reviews of reviews, both systematic and non-systematic, to identify any additional reviews that could be included. With the large number of systematic reviews found, and our extensive search of gray literature, we are confident that our scope is sufficiently broad and comprehensive.
To ensure the reliability of our review, we followed a predetermined protocol and conducted both reference searches and data extraction in duplicate. We also aimed to report our review process and findings as transparently as possible, with the aid of the additional material included in the Appendix.
We included reviews published in 2018 or later. Although the majority of the trials included in these reviews were published relatively recently, a few were published as early as 2001. This could have partially influenced the results because we know that newer eHealth interventions, specifically those developed in the 2010s or later, yield better results than older interventions [31]. This could be attributed to the rise of digitalization, which has resulted in improved technology literacy and advancements in device and application design.
As previously discussed, the included reviews generally had a high or moderate risk of bias, as well as high heterogeneity among the included trials and results. This must be taken into consideration when interpreting the findings of this study.
Conclusion
The review indicates that eHealth interventions are more effective than control interventions or no care and comparable to face-to-face interventions. Notably, the most significant weight loss results have been observed in eHealth interventions that combine a digital program with personal counseling or coaching from a qualified professional, delivered either remotely or in-person. Common features of effective interventions include individual feedback, personalized content, self-monitoring, and the utilization of various intervention modalities. However, studies focusing on the maintenance of weight loss are limited, leaving a gap in knowledge regarding the long-term effectiveness of eHealth interventions for weight loss and weight loss maintenance.
Change history
14 October 2023
A Correction to this paper has been published: https://doi.org/10.1007/s13679-023-00530-3
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
World Health Organization. Obesity and overweight. [cited 2023 Apr 25]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Varkevisser RDM, van Stralen MM, Kroeze W, Ket JCF, Steenhuis IHM. Determinants of weight loss maintenance: a systematic review. Obes Rev. 2019;20:171–211.
McLean B, Hossain N, Donison V, Gray M, Durbano S, Haase K, et al. Providing medical information to older adults in a web-based environment: systematic review. JMIR Aging. 2021;4:e24092.
Madigan CD, Graham HE, Sturgiss E, Kettle VE, Gokal K, Biddle G, et al. Effectiveness of weight management interventions for adults delivered in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2022;377:e069719.
LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: updated evidence report and systematic review for the US preventive services task force. JAMA United States. 2018;320:1172–91.
Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ. 2014;348:g2646.
Montesi L, El Ghoch M, Brodosi L, Calugi S, Marchesini G, Dalle GR. Long-term weight loss maintenance for obesity: a multidisciplinary approach. Diabetes Metab Syndr Obes. 2016;9:37–46.
Ma C, Avenell A, Bolland M, Hudson J, Stewart F, Robertson C, et al. Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta-analysis. BMJ. 2017;359:j4849.
Blackburn M, Stathi A. Moral discourse in general practitioners’ accounts of obesity communication. Soc Sci Med. 2019;230:166–73.
Blackburn M, Stathi A, Keogh E, Eccleston C. Raising the topic of weight in general practice: perspectives of GPs and primary care nurses. BMJ Open. 2015;5:e008546.
World Health Organization. Digital health. [cited 2023 Apr 26]. Available from: https://www.who.int/health-topics/digital-health.
Pappa GL, Cunha TO, Bicalho PV, Ribeiro A, Couto Silva AP, Meira W, et al. Factors associated with weight change in online weight management communities: a case study in the LoseIt Reddit community. J Med Internet Res. 2017;19:e17.
Gentili A, Failla G, Melnyk A, Puleo V, Tanna GLD, Ricciardi W, et al. The cost-effectiveness of digital health interventions: a systematic review of the literature. Front Public Health. 2022;10. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85137319829&doi=10.3389%2ffpubh.2022.787135&partnerID=40&md5=61a716abe696bfa8b9926cc34e289fed.
Gao M, Piernas C, Astbury NM, Hippisley-Cox J, O’Rahilly S, Aveyard P, et al. Associations between body-mass index and COVID-19 severity in 6·9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 2021;9:350–9.
Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11:15.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Beleigoli AM, Andrade AQ, Cançado AG, Paulo MN, Diniz MDFH, Ribeiro AL. Web-based digital health interventions for weight loss and lifestyle habit changes in overweight and obese adults: systematic review and meta-analysis. Canada. J Med Internet Res. 2019;21:e298.
Berry R, Kassavou A, Sutton S. Does self-monitoring diet and physical activity behaviors using digital technology support adults with obesity or overweight to lose weight? A systematic literature review with meta-analysis. England. Obes Rev. 2021;22:e13306.
Besson M, Gurviez P, Carins J. Using digital devices to help people lose weight: a systematic review. Emerald Publishing Limited. J Soc Mark. 2020;10:289–319.
Houser S, Joseph R, Puro N, Burke D. Use of technology in the management of obesity: a literature review. Perspect Health Inf Manag. 2019;16:1c.
Huang J-W, Lin Y-Y, Wu N-Y. The effectiveness of telemedicine on body mass index: a systematic review and meta-analysis. J Telemed Telecare. 2019;25:389–401.
Jahangiry L, Farhangi MA. Obesity paradigm and web-based weight loss programs: an updated systematic review and meta-analysis of randomized controlled trials. Bangladesh. J Health Popul Nutr. 2021;40:16.
Lahtio H, Rintala A, Immonen J, Sjogren T. The Effectiveness of physical activity-promoting web- and mobile-based distance weight loss interventions on body composition in rehabilitation settings: systematic review, meta-analysis, and meta-regression analysis. Canada. J Med Internet Res. 2022;24:e25906.
Lau Y, Chee DGH, Chow XP, Cheng LJ, Wong SN. Personalised eHealth interventions in adults with overweight and obesity: a systematic review and meta-analysis of randomised controlled trials. United States. Prev Med. 2020;132:106001.
Lee Y, Lee NY, Lim HJ, Sung S. Weight reduction interventions using digital health for employees with obesity: a systematic review. Diabetes Metab Syndr Obes. 2022;15:3121–31.
Mata-Gonzalez E, Meza-Pena C, Garcia C. Intervention programs through the Internet for weight loss in adults with overweight and obesity: a systematic review. Rev Esp Nutr Hum. 2020;24:324–35.
Podina IR, Fodor LA. Critical review and meta-analysis of multicomponent behavioral e-health interventions for weight loss. US: American Psychological Association. Health Psychol. 2018;37:501–15.
Rumbo-Rodriguez L, Sanchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blazquez N, Ferrer-Cascales R, Zaragoza-Marti A. Use of technology-based interventions in the treatment of patients with overweight and obesity: a systematic review. Nutrients. 2020;12.
Shi Y, Wakaba K, Kiyohara K, Hayashi F, Tsushita K, Nakata Y. Effectiveness and components of web-based interventions on weight changes in adults who were overweight and obese: a systematic review with meta-analyses. Switzerland. Nutrients. 2022;15.
Varela C, Oda-Montecinos C, Andrés A, Saldaña C. Effectiveness of web-based feedback interventions for people with overweight and obesity: systematic review and network meta-analysis of randomized controlled trials. J Eat Disord. 2021;9:75.
•• Ang SM, Chen J, Liew JH, Johal J, Dan YY, Allman-Farinelli M, et al. Efficacy of interventions that incorporate mobile apps in facilitating weight loss and health behavior change in the Asian population: systematic review and meta-analysis. J Med Internet Res. 2021;23:e28185. Multicomponent interventions that incorporate apps produce a small to moderate effect in reducing weight, BMI, and waist circumference in Asian populations. Main factors for intervention success and adherence are patient-professional communication, self-monitoring, and cultural adaptation.
Chew HSJ, Koh WL, Ng JSHY, Tan KK. Sustainability of weight loss through smartphone apps: systematic review and meta-analysis on anthropometric, metabolic, and dietary outcomes. Canada. J Med Internet Res. 2022;24:e40141.
Dounavi K, Tsoumani O. Mobile health applications in weight management: a systematic literature review. Am J Prev Med. 2019;56:894–903.
Islam MM, Poly TN, Walther BA, Jack Li Y-C. Use of mobile phone app interventions to promote weight loss: meta-analysis. Canada. JMIR Mhealth Uhealth. 2020;8:e17039.
Puigdomenech Puig E, Robles N, Saigi-Rubio F, Zamora A, Moharra M, Paluzie G, et al. Assessment of the efficacy, safety, and effectiveness of weight control and obesity management mobile health interventions: systematic review. JMIR Mhealth Uhealth. 2019;7.
• Antoun J, Itani H, Alarab N, Elsehmawy A. The effectiveness of combining nonmobile interventions with the use of smartphone apps with various features for weight loss: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2022;10:e35479. Mobile phone applications have a role in weight loss management, especially when used in conjunction with usual care. Combining an mHealth intervention with human-delivered coaching led to most favorable weight loss results at 6 months.
Berry MP, Sala M, Abber SR, Forman EM. Incorporating automated digital interventions into coach-delivered weight loss treatment: a meta-analysis. US: American Psychological Association. Health Psychol. 2021;40:534–45.
Novaes Oliveira AC, Menezes Guariente SM, Zazula R, Mesas AE, Coral Oliveira CE, Vissosi Reiche EM, et al. Hybrid and remote psychosocial interventions focused on weight and sedentary behavior management among patients with severe mental illnesses: a systematic review. Psychiatr Q. 2022;93:813–40.
O’Boyle J, Davidson P. The effects of mhealth versus eHealth on weight loss in adults: a systematic review. Top Clin Nutr. 2022;37:69.
Holmes WS, Moorhead SA, Coates VE, Bond RR, Zheng H. Impact of digital technologies for communicating messages on weight loss maintenance: a systematic literature review. Eur J Pub Health. 2019;29:320–8.
Mamalaki E, Poulimeneas D, Tsiampalis T, Kouvari M, Karipidou M, Bathrellou E, et al. The effectiveness of technology-based interventions for weight loss maintenance: a systematic review of randomized controlled trials with meta-analysis. England. Obes Rev. 2022;23:e13483.
• Arsenijevic J, Tummers L, Bosma N. Adherence to electronic health tools among vulnerable groups: systematic literature review and meta-analysis. Canada. J Med Internet Res. 2020;22:e11613. eHealth interventions with multimodal content and direct communication between patients and healthcare providers increase intervention adherence among vulnerable groups.
Jakob R, Harperink S, Rudolf AM, Fleisch E, Haug S, Mair JL, et al. Factors influencing adherence to mHealth apps for prevention or management of noncommunicable diseases: systematic review. J Med Internet Res. 2022;24.
Asbjornsen RA, Smedsrod ML, Nes LS, Wentzel J, Varsi C, Hjelmesaeth J, et al. Persuasive system design principles and behavior change techniques to stimulate motivation and adherence in electronic health interventions to support weight loss maintenance: scoping review. J Med Internet Res. 2019;21.
Mohr D, Cuijpers P, Lehman K. Supportive accountability: a model for providing human support to enhance adherence to ehealth interventions. J Med Internet Res. 2011;13:e1602.
Rosenbaum DL, Piers AD, Schumacher LM, Kase CA, Butryn ML. Racial and ethnic minority enrollment in randomized clinical trials of behavioural weight loss utilizing technology: a systematic review. Obes Rev. 2017;18:808–17.
Bodie GD, Dutta MJ. Understanding health literacy for strategic health marketing: eHealth literacy, health disparities, and the digital divide. Health Mark Q. 2008;25:175–203.
•• Sung M, He J, Zhou Q, Chen Y, Ji JS, Chen H, et al. Using an integrated framework to investigate the facilitators and barriers of health information technology implementation in noncommunicable disease management: systematic review. J Med Internet Res. 2022;24:e37338. eHealth interventions are convenient, improve the quality of care, and increase the accessibility of healthcare. Implementation success is facilitated by well-designed applications with easy usability as well as social support and communication with healthcare providers.
Coupe N, Cotterill S, Peters S. Tailoring lifestyle interventions to low socio-economic populations: a qualitative study. BMC Public Health. 2018;18:967.
Vasselli JR, Juray S, Trasino SE. Success and failures of telehealth during COVID-19 should inform digital applications to combat obesity. Obes Sci Pract. 2021. https://doi.org/10.1002/osp4.551.
Cefalu WT, Bray GA, Home PD, Garvey WT, Klein S, Pi-Sunyer FX, et al. Advances in the science, treatment, and prevention of the disease of obesity: reflections from a diabetes care editors’ expert forum. Diabetes Care. 2015;38:1567–82.
Burgess E, Hassmén P, Pumpa KL. Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review. Clinical Obesity. 2017;7:123–35.
• Kupila SKE, Venäläinen MS, Suojanen L-U, Rosengård-Bärlund M, Ahola AJ, Elo LL, et al. Weight loss trajectories in healthy weight coaching: cohort study. JMIR Form Res. 2022;6:e26374. In this study conducted in a real-life clinical setting, patients enrolled in an eHealth intervention lost on average 4.6% (SE 0.5%) of their initial body weight at the 12-month time point. Baseline medication use, baseline health status, age, or sex was not significantly associated with weight loss results.
Colombo O, Ferretti VVV, Ferraris C, Trentani C, Vinai P, Villani S, et al. Is drop-out from obesity treatment a predictable and preventable event? Nutr J. 2014;13:13.
Flückiger C, Del Re AC, Wampold BE, Horvath AO. The alliance in adult psychotherapy: a meta-analytic synthesis. Psychotherapy (Chic). 2018;55:316–40.
Sturgiss EA, Sargent GM, Haesler E, Rieger E, Douglas K. Therapeutic alliance and obesity management in primary care – a cross-sectional pilot using the Working Alliance Inventory. Clin Obes. 2016;6:376–9.
Funding
Open Access funding provided by University of Helsinki including Helsinki University Central Hospital. This study was supported by Academy of Finland, grant numbers 335443, 314383, 272376, 266286; Finnish Medical Foundation, grant number 5891; Gyllenberg Foundation; Novo Nordisk Foundation, grant numbers NNF20OC0060547, NNF17OC0027232, NNF10OC1013354; Finnish Diabetes Research Foundation; Finnish Foundation for Cardiovascular Research; Government Research Funds; Helsinki University Hospital; and University of Helsinki. The funders had no role in study design, data collection and analysis, Cmdecision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Sakris Kupila and Anu Joki performed the literature search and data extraction with Laura Suojanen resolving potential discrepancies. Sakris Kupila formatted the tables and figures. The first draft of the manuscript was written by Sakris Kupila and Anu Joki. All authors reviewed and edited the manuscript. All authors read and approved the final manuscript. The project was administered by Sakris Kupila and supervised by Kirsi Pietiläinen.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kupila, S.K.E., Joki, A., Suojanen, LU. et al. The Effectiveness of eHealth Interventions for Weight Loss and Weight Loss Maintenance in Adults with Overweight or Obesity: A Systematic Review of Systematic Reviews. Curr Obes Rep 12, 371–394 (2023). https://doi.org/10.1007/s13679-023-00515-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-023-00515-2