Abstract
Purpose of Review
Deprescribing, systematically discontinuing unnecessary or harmful medications, gains importance in healthcare. With rising polypharmacy concerns, optimizing medication management is crucial. This article explores deprescribing within interprofessional teams emphasizing collaborative efforts to address polypharmacy and improve patient outcomes. It examines the necessity and effectiveness of interprofessional collaboration in deprescribing initiatives, with a focus on diverse healthcare professionals optimizing medication regimens.
Recent Findings
Polypharmacy, characterized by the simultaneous use of multiple medications, poses significant challenges, highlighting the importance of deprescribing. Interprofessional collaboration, supported by evidence, has demonstrated efficacy in reducing polypharmacy and improving patient outcomes. Furthermore, diverse providers contribute valuable expertise in identifying patients who may benefit from deprescribing and non-pharmacological interventions.
Summary
Successful deprescribing relies on interprofessional collaboration to assess medication appropriateness, mitigate risks, and tailor plans to patient preferences. Screening tools identify inappropriate polypharmacy, while frameworks and action steps guide implementation. Integrating non-pharmacological interventions and prioritizing patient safety enhance care quality for older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deprescribing, a term that has gained prominence in recent years, refers to the process of a proactive and intentional reduction or cessation of medications that may no longer be necessary or could be causing harm. Deprescribing involves more than simply halting medication usage; it entails a systematic approach to identifying and discontinuing medications where the potential risks outweigh the benefits, all while considering the patient's health objectives and preferences [1]. This process can take various forms, such as ceasing medication use altogether, reducing dosages, or switching medications to enhance the patient's medication regimen. While traditional healthcare practices have often emphasized prescribing medications as a common component of treatment, the evolving landscape of healthcare recognizes the risks associated with polypharmacy and unnecessary medication use. The purpose of this review is to explore the role of deprescribing within the context of interprofessional teams and person-centered care. With an aging population and increased prevalence of polypharmacy-related issues [2], it is imperative to explore how interprofessional collaboration can optimize medication management, aligning with individual patient goals and preferences.
The Need for Deprescribing: Recognizing Polypharmacy
Before delving into deprescribing and the role of the interprofessional team, it's crucial to establish a clear understanding of polypharmacy. Polypharmacy refers to the concurrent use of multiple medications, often involving more medications than clinically necessary, appropriate, or indicated for a given individual. While there is no consensus on this criterion, the threshold for defining polypharmacy is commonly cited as having > 5 medications [2]. Data from the CDC highlight the prevalence of polypharmacy among older adults, with estimates suggesting that nearly 1 in 5 individuals aged 65 and older concurrently take five or more prescription medications [3]. However, this criterion may vary depending on the specific context and patient characteristics. Nevertheless, it generally signifies a scenario wherein the potential risks associated with numerous medications outweigh their benefits [2, 4] and providers should emphasize the importance of thoroughly completing medication reviews to identify any potentially harmful medications. This approach should take precedence over solely focusing on the number of medications, as some individuals may necessitate deprescribing even if they are on fewer than 5 medications. The CDC data notes that lipid-lowering drugs emerged as the most frequently prescribed medication type, followed closely by antidiabetic agents [3]. Other commonly prescribed medications, reflective of the most reported diseases, include those for heart disease, non-steroidal anti-inflammatory drugs (NSAIDs), and proton pump inhibitors (PPIs), some of which the American Geriatrics Society Health in Aging Foundation recommends that older people avoid whenever possible [3, 5,6,7].
Polypharmacy is particularly prevalent among older adults, not solely due to advancing age, but rather because of multiple age-related comorbidities, geriatric syndromes, and changes in pharmacokinetics associated with aging [8,9,10]. Additionally, the management of medications becomes increasingly complex as individuals with multiple comorbidities often receive care from multiple healthcare providers. Patients receiving care from various providers across different healthcare settings may experience disjointed communication and coordination, resulting in gaps in medication management. This often leads to a fragmented approach to care, resulting in insufficient coordination and issues such as duplicate prescriptions, adverse medication interactions, and inadequate monitoring. Furthermore, systemic factors, such as inaccurate medical records including discontinued medications, automated refill services, and a focus on disease-specific quality metrics in prescribing, contribute to the accumulation of medications over time [11].
Patients dealing with polypharmacy encounter challenges in managing multiple medications, leading to confusion, non-adherence, and adverse drug events [12]. Certainly, the accumulating cost of multiple medications can also pose a considerable barrier to treatment adherence and overall health outcomes. Uncoordinated healthcare management of these medications can also lead to unnecessary or duplicate medications or, in some cases, trigger a "prescribing cascade," as depicted in Fig. 1, where additional medications are prescribed to address the adverse effects of existing ones. Symptoms of adverse effects are often attributed solely to aging, leading to the oversight of potential medication-related issues such as constipation, increased falls, confusion, loss of appetite, or fatigue.
Figure 1 provides an illustrative case example of a patient treated by this author. The figure illustrates a deprescribing cascade starting with the prescription of anticholinergic medication for urinary leakage due to BPH. This results in a side effect of urinary retention, necessitating an alpha blocker prescription, which then resulted in patient reports of sexual dysfunction. A vasodilator was then prescribed to address this side effect. This cascade highlights the unintended consequences and complexities of medication management and additionally how each of these medications also have side effects with increased risk of falls.
One strategy to tackle these issues involves improving coordination and communication among interprofessional team members. Moreover, it's valuable for these professionals to explore deprescribing options with their patients. Notably, a recent survey conducted by the Institute for Healthcare Policy Innovation revealed that 80% of older adults on prescription medication are open to discontinuing one or more medications under their healthcare provider's guidance. Particularly, medications for heart disease, diabetes, and pain management were commonly identified for potential cessation [13].
The Interprofessional Deprescribing Team: An Evidence-Based Approach
Reducing the number of medications or adjusting their doses through deprescribing can effectively mitigate polypharmacy and address previously mentioned medication management concerns. Evidence suggests that a thorough medication review and proactive discontinuation strategies can lead to a reduction in potentially inappropriate medication use by up to 30 to 60 percent or more [14,15,16]. This reduction in medication burden may enhance adherence to the remaining medications [17]. Particularly valuable in deprescribing efforts is an interprofessional collaborative approach, where healthcare professionals from diverse disciplines come together to optimize medication regimens, assess the appropriateness of medications, identify potential risks and benefits of deprescribing, develop tailored deprescribing plans, and consider non-pharmacological approaches to care aligned with the patient's goals and preferences. This approach has been found to minimize medication errors, reduce hospitalizations, and improve overall outcomes [18].
To further explore the potential roles of each provider as part of an interprofessional collaborative team in supporting deprescribing efforts and reducing polypharmacy-related risk a review of the literature since 2018 was completed. A systematic literature search was conducted using PubMed, Medline, and Google Scholar to identify relevant articles written in English and published within the last five years. The search strategy focused on “deprescribing”, utilizing clinical trial, meta-analysis, randomized controlled trial, or systematic review methodologies. The search was then further limited to studies emphasizing “interprofessional”, “interdisciplinary”, or “multidisciplinary” collaboration in healthcare settings. Articles that specifically addressed deprescribing interventions or strategies involving older adults or populations were included in the review. After applying the search criteria, a total of 16 articles were reviewed. The workflow of the literature review is summarized in Fig. 2.
The literature search since yielded a range of research focused on deprescribing interventions among older adults, particularly those living with frailty, undergoing surgery, or residing in nursing homes. These studies demonstrated the effectiveness and feasibility of deprescribing strategies in improving patient outcomes and reducing risks associated with polypharmacy. Interestingly, the majority of the studies were conducted in inpatient facilities outside of the United States, with only one study representing outpatient clinics. Throughout the selected articles, there was a consistent emphasis on the importance of interprofessional collaboration and pharmacist involvement in medication management. While specific disciplines beyond physicians, pharmacists, and nurses were not explicitly noted in the literature, "other providers" were mentioned. Collectively, the findings supported the idea that deprescribing efforts can lead to reductions in inappropriate polypharmacy, medication-related adverse events, and healthcare costs, ultimately enhancing the quality of care for older adults. Additionally, the findings underscored the critical role of interprofessional collaboration in deprescribing initiatives [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33].
The Interprofessional Deprescribing Team: Members and Roles
The key figure within the healthcare team is undoubtedly the patient, with their understanding and cooperation being pivotal for successful outcomes, along with the involvement of their care partners when appropriate. Patients must actively engage in collaborative decision-making, openly discussing their medications, concerns, and preferences with healthcare providers through the patient interview process[34]. Older patients with higher levels of health literacy and those who engage in discussions with their providers are more inclined to consider deprescribing [35, 36].
Physicians and nursing teams undoubtedly play a pivotal role in deprescribing practices within healthcare teams. They initiate and conduct thorough medication reviews, make necessary changes to medication regimens, engage in shared decision-making with patients, and ensure ongoing collaboration with other healthcare professionals. Collaboration with pharmacists, through comprehensive medication management practices, can alleviate time pressures and optimize medication optimization. Pharmacists, with their specialized knowledge in pharmacology and medication management, conduct comprehensive medication reviews, identify potential drug interactions, and offer valuable insights into medication appropriateness.
Although physicians, pharmacists, and nurses traditionally oversee medication management, including prescribing and deprescribing, a diverse range of healthcare professionals, such as physical therapists, occupational therapists, speech and language pathologists, dietitians, nutritionists, and mental health professionals, as well as others, also contribute their expertise to address this broader aspect of patient care. These professionals play pivotal roles in identifying patients who may benefit from medication review, deprescribing, and non-pharmacological interventions. For instance, physical therapists are movement experts and assess mobility issues, pain, fall risks, and functional limitations and overall physical health that may be enhanced or inhibited by certain medications. Occupational therapists focus on enhancing activities of daily living, and address cognitive, physical, and environmental factors that influence medication adherence. Speech and language pathologists evaluate communication and swallowing disorders, which may affect medication administration and adherence. Nutritionists evaluate dietary patterns and nutritional status, identifying potential interactions between diet and medications. Mental health professionals assess and treat underlying psychological factors influencing medication adherence or response to deprescribing efforts. Interprofessional collaboration amongst these professions as well as other not mentioned further facilitates the identification and mitigation of potential risks associated with polypharmacy.
Figure 3 illustrates an Interprofessional Collaborative Approach to Deprescribing Medications.
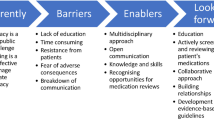
While the role of other healthcare professionals as members of the interprofessional team in deprescribing is promising these healthcare providers may face the following challenges:
-
Limited authority: Non-prescribing providers may lack the authority in the decision making processes regarding medication changes, which can hinder their ability to actively participate in deprescribing discussions.
-
Knowledge gaps: These providers may have limited pharmacological knowledge compared to prescribing providers, making assessing the appropriateness of medications and identifying potential risks and benefits challenging.
-
Communication barriers: Non-prescribing providers may struggle to effectively communicate their concerns, recommendations, and observations related to medication management to prescribing providers and other team members.
-
Role ambiguity: Non-prescribing providers may experience uncertainty about their roles and responsibilities within the interprofessional team, leading to confusion and inefficiencies in collaborative deprescribing efforts.
-
Time constraints: Non-prescribing providers often have competing demands on their time, which may limit their availability to actively participate in deprescribing discussions and follow-up activities.
To address these challenges, it is essential to foster a collaborative team environment, commit to ongoing education and skill development, clarify roles and responsibilities within the team [37, 38], promote effective communication strategies, and cultivate a culture of mutual respect, psychological safety, and trust among team members. Action items to consider before participation in interprofessional deprescribing partnership as a non-prescribing healthcare professional are as follows:
Education and Training:
-
Participate in ongoing education and training to increase knowledge on foundational pharmacology and to stay updated on advancements in medication management.
-
Utilize quickly available resources such as apps to enhance knowledge about medications. Many apps offer accessible information on dosage, side effects, interactions.
Assessment and Monitoring:
-
Always include medications reviews with all patients evaluated to ensure a comprehensive understanding of the pharmacological interventions being utilized.
-
Inquire about potential side effects and adverse reactions related to prescribed medications during patient assessments.
-
Monitor changes in patient presentation following changes in medications (new, discontinued, or reduced).
Communication and Collaboration:
-
Contribute insights on the impact of medications on cognitive, functional, and physical abilities during medication reviews/rounds, drawing from areas of expertise.
-
Request medication reviews from prescribing providers when concerns arise regarding the appropriateness or necessity of specific medications.
-
Seek opportunities to collaborate with other healthcare professionals to develop comprehensive, individualized deprescribing plans prioritizing patient safety and well-being.
Advocacy:
-
Advocate to prescribing providers for the possibility of adjustment or cessation of medications that may contribute to decline or impairments.
-
Promote awareness of current clinical practice guidelines and evidence-based practices to support non-pharmacological interventions.
-
Share positive case studies and success stories highlighting the impact of non-pharmacological interventions on patient outcomes.
Utilizing Screening Tools and Action Frameworks in Deprescribing Practices
There is no one-size-fits-all approach to deprescribing, but it is recommended to include monitoring patients' active medication lists and deprescribing any unnecessary medications to reduce pill burden, adverse drug events, and financial hardship. One effective method is to utilize a conceptual framework typically involving medication review, risk assessment, goal setting, and implementation of a deprescribing plan [39]. It is crucial to educate and incorporate patient/caregiver perspectives on goals and preferences into this process, aiming to slow disease progression, prevent health decline, effectively address symptoms, and maximize overall function and quality of life [40, 41].
Several screening tools can also be utilized in clinical practice to aid healthcare professionals in optimizing medication management and deprescribing efforts for older adults, with the AGS Beers Criteria® and the Screening Tool to Alert doctors to Right Treatment (START) and Screening Tool of Older Persons' Prescriptions (STOPP) criteria being prominent examples. The AGS Beers Criteria®, developed by the American Geriatrics Society (AGS), offers comprehensive guidance in identifying Potentially Inappropriate Medications (PIMs) by highlighting disease-specific considerations, drug interactions, and medications with anticholinergic properties. However, despite its usefulness, the AGS Beers Criteria® may overlook less commonly prescribed drugs and lack patient-specific considerations, potentially omitting alternative therapies [5]. The START/STOPP criteria, offers a systematic approach to identify potentially inappropriate medications based on physiological systems. The START criteria focus on underprescribed medications beneficial for older adults, while the STOPP criteria highlight potentially inappropriate or harmful medications, promoting more balanced medication regimens [42].
Moreover, the Medication Appropriateness Index serves as a structured rating scale to assess medication appropriateness in older patients. Although user-friendly, it may not comprehensively cover all drug interactions or adverse reactions. Nevertheless, these screening tools may play a role in guiding healthcare professionals towards safer and more effective medication management for older adults, promoting patient safety and optimizing therapeutic outcomes [43].
In practice, this author has achieved positive outcomes using an adapted version of the CDC STEADI RX (Stopping Elderly Accidents, Deaths, and Injuries - Prescription Tool), an evidence-based framework developed by the Centers for Disease Control and Prevention (CDC) originally designed to prevent falls among older adults.[44]. Adapted from existing medication therapy management tools used by pharmacists, the STEADI RX framework follows the SAFE process: Screen, Assess, Formulate, and Educate. While initially intended for fall prevention, this framework presents a structured approach that can be extended to deprescribing efforts. For example, consider the following implementation:
Screen
All providers systematically assess medication lists for potential concerns, including medications contributing to reported adverse effects, abnormal lab values, and long term consequences associated with chronic use placing patients at risk of cognitive or functional decline. Embracing differing perspectives may uncover out-of-the-box opportunities.
Assess
Comprehensive patient assessments conducted by each provider should consider medical history, current health status, risk factors, and cognitive and physical abilities. Additionally, has the patient had other changes such as recently weight loss or gain which may impact the dosing. Assessments should also include evaluating responses to alternative non-pharmacological approaches to care. Important questions to ask during assessments and subjective intact includes:
-
When did you start each medication and why?
-
How does it help or impact you either positively or negatively and has this changed over time?
-
Are there any medications you may consider not taking?
Formulate
Collaborate as an interprofessional team to develop a tailored deprescribing plan based on screening and assessment findings, potentially involving dose reduction, discontinuation of ineffective or risky medications, and consideration of alternative therapies. Non-prescribing providers can assist with monitoring side effects and withdrawal symptoms and offer adjunctive therapies for positive outcomes. Ensure all involved are informed of medication changes and provide suggestions as needed.
Educate
Customize education to the patient's health literacy, addressing concerns and empowering them to manage their health. Topics may include addressing fears, behavior change strategies, action plan implementation, reasons for medication changes, specialist referrals, and other methods to reduce medication. A teach back method can aid in verifying understanding [45].
Non-Pharmacological Considerations
There is a growing recognition of the importance of nonpharmacological approaches in tandem with deprescribing practices. While medications have historically served as foundational elements in managing diverse health conditions, the rising recognition of nonpharmacological interventions signifies a paradigm shift towards a more holistic and person centered approach to care. These interventions may offer a complementary or even a primary means of addressing patient needs, highlighting the significance of holistic care that encompasses physical, psychological, and social dimensions.
Interprofessional collaboration can enhance the effectiveness and safety of deprescribing efforts by integrating a diverse range of approaches to patient care, with each professional bringing a unique set of expertise and skills to the table. This collaborative approach enables healthcare teams to identify potential risks associated with certain medications, particularly those that may contribute to functional or cognitive decline in patients. For instance, numerous medications have been linked to sarcopenia, a condition characterized by muscle loss in older adults. Corticosteroids, statins, antidepressants, proton pump inhibitors, antipsychotics, and opioids are among the medications that can exacerbate the risk of sarcopenia by causing muscle weakness, decreased mobility, and reduced physical activity levels [46]. Corticosteroids, for example, can lead to muscle wasting over time [47], while statins have been associated with muscle-related side effects such as myopathy [48]. Similarly, medications like proton pump inhibitors and antipsychotics may increase the risk of fractures and possibly further impair function [49, 50]. While these medications may provide benefits in managing underlying health conditions, it is crucial to carefully weigh their potential impact on muscle health, especially in older adults who may be more susceptible to sarcopenia.
Additionally, certain other medications can affect physical activity and functional independence in older adults and should be closely monitored. Benzodiazepines and other sedative-hypnotics, for example, may cause drowsiness, dizziness, and impaired balance, increasing the risk of falls and limiting mobility [51]. Anticholinergic medications, commonly used for conditions like overactive bladder, allergies, and Parkinson's disease, can lead to side effects such as dry mouth, blurred vision, and confusion[52]. Similarly, certain antihypertensive medications, particularly beta-blockers, may cause fatigue, weakness, and decreased exercise tolerance, potentially hindering engagement in physical activities [53]. Chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs) can also impact function by causing gastrointestinal issues, renal impairment, and fluid retention [54]. While these medications may be essential for managing health conditions, it's crucial to consider their potential impact on muscle health and overall functional abilities. Regular reassessment of their necessity is important, as circumstances may change over time. An important question to routinely ask is: just because they were needed and effective at one point, are they still necessary?
In addition to acknowledging changes in cognition or function and subsequently addressing any adverse effects such as falls, the same members of the team may be able to offer non-pharmacological alternatives. These alternatives could provide an opportunity for the patient to have medication discontinued or reduced. Physical therapists, occupational therapists, and speech and language pathologists, in particular, bring a multifaceted approach to patient care by employing various techniques. For example, studies have shown successful patient outcomes through physical therapy for pain management [55,56,57], reducing the need for opioids, edema management [58], reducing the need for NSAIDs, addressing sleep quality reducing the need for sleep aids [59], and potentially reducing the need for anticholinergics by addressing pelvic floor strengthening exercises to address urinary incontinence [60], just to name a few. Furthermore, exercises and physical activity have been consistently cited in the literature to demonstrate the added benefits beyond physical health - by positively impacting cognitive function, mental health, and overall well-being [61, 62].
Conclusion
The evolving landscape of healthcare recognizes and is supported by the literature, the necessity for deprescribing practices within the context of interprofessional teams and person-centered care. However, the implementation of a diverse interprofessional approach is still in its infancy. Having a diverse interprofessional team of prescribing and non-prescribing providers to address polypharmacy ensures a wide array of treatment options to support deprescribing efforts are offered and considered, taking into account various perspectives and expertise. Collaborative efforts among healthcare professionals, including physicians, pharmacists, nurses, and a diverse range of non-prescribing providers, should prioritize the utilization of current screening and assessment tools. These tools are continuously evolving to better meet the needs of healthcare teams. While no single tool may be perfect, leveraging existing resources provides a solid foundation for deprescribing initiatives, guiding healthcare providers in identifying potential risks and tailoring interventions to individual patient needs.
Data Availability
No datasets were generated or analysed during the current study.
References
Engi Z, Matuz M, Soós G, Hajnal F, Szökő É, Viola R, Csupor D, Benkő R. Gyógyszerrosta: a racionális gyógyszeres terápia meghatározó eleme [Deprescribing: an essential part of rational pharmacotherapy]. Orv Hetil. 2023;164(24):931–41. https://doi.org/10.1556/650.2023.32782.
Pazan F, Wehling M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. European geriatric medicine. 2021;12(3):443–52. https://doi.org/10.1007/s41999-021-00479-3.
Hales CM, Servais J, Martin CB, Kohen D. Prescription Drug Use Among Adults Aged 40–79 in the United States and Canada. NCHS data brief. 2019;347:1–8.
Wastesson JW, Morin L, Tan ECK, Johnell K. An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf. 2018;17(12):1185–96. https://doi.org/10.1080/14740338.2018.1546841.
2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;2023(71):2052. Includes a set of guidelines developed by the American Geriatrics Society to identify potentially inappropriate medications for older adults.
O’Mahony D, Cherubini A, Guiteras AR, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 3. Eur Geriatr Med. 2023;14:625. Includes information on a tool designed to identify potentially inappropriate prescribing in older adults (STOPP) and potential prescribing omissions (START), aiding in optimizing medication management.
Marinho JMDS, Medeiros KBA, Fonseca RNS, Araujo TS, Barros WCTDS, Oliveira LPBA. Standard drug consumption: a study with elderly people in Primary Health Care. Rev Bras Enferm. 2021;74(3): e20200729. https://doi.org/10.1590/0034-7167-2020-0729.
Maher D, Ailabouni N, Mangoni AA, et al. Alterations in drug disposition in older adults: a focus on geriatric syndromes. Expert Opin Drug Metab Toxicol. 2021;17:41.
Mehta RS, Kochar BD, Kennelty K, Ernst ME, Chan AT. Emerging approaches to polypharmacy among older adults. Nature aging. 2021;1(4):347–56. https://doi.org/10.1038/s43587-021-00045-3.
Schmidt SJ, Wurmbach VS, Lampert A, Bernard S, HIOPP-6 Consortium, Haefeli WE, Seidling HM, Thürmann PA. Individual factors increasing complexity of drug treatment-a narrative review. Eur J Clin Pharmacol. 2020;76(6):745–54. https://doi.org/10.1007/s00228-019-02818-7.
Halli-Tierney AD, Scarbrough C, Carroll D. Polypharmacy: Evaluating risks and deprescribing. Am Fam Physician. 2019;100(1):32–8.
Kurczewska-Michalak M, Lewek P, Jankowska-Polańska B, et al. Polypharmacy management in the older adults: A scoping review of available interventions. Front Pharmacol. 2021;12: 734045. https://doi.org/10.3389/fphar.2021.734045.
Vordenberg S, Singer D, Kirch M, Solway E, Roberts S, Smith E, Hutchens L, Malani P, Kullgren J. Views on medication deprescribing among adults age 50–80. University of Michigan National Poll on Healthy Aging. 2023. https://doi.org/10.7302/7128.
Kua CH, Mak VSL, Huey Lee SW. Health outcomes of deprescribing interventions among older residents in nursing homes: A systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20:362.
Martin P, Tamblyn R, Benedetti A, et al. Effect of a Pharmacist-Led Educational Intervention on Inappropriate Medication Prescriptions in Older Adults: The D-PRESCRIBE Randomized Clinical Trial. JAMA. 1889;2018:320.
Bloomfield HE, Greer N, Linsky AM, et al. Deprescribing for community-dwelling older adults: a systematic review and meta-analysis. J Gen Intern Med. 2020;35:3323.
Ulley J, Harrop D, Ali A, et al. Deprescribing interventions and their impact on medication adherence in community-dwelling older adults with polypharmacy: a systematic review. BMC Geriatr. 2019;19:15.
Omuya H, Nickel C, Wilson P, Chewning B. A systematic review of randomised-controlled trials on deprescribing outcomes in older adults with polypharmacy. Int J Pharm Pract. 2023;31(4):349–68. https://doi.org/10.1093/ijpp/riad025.
Ibrahim K, Cox NJ, Stevenson JM, Lim S, Fraser SDS, Roberts HC. A systematic review of the evidence for deprescribing interventions among older people living with frailty. BMC Geriatr. 2021;21(1):258. https://doi.org/10.1186/s12877-021-02208-8.
Lee JW, Li M, Boyd CM, Green AR, Szanton SL. Preoperative deprescribing for medical optimization of older adults undergoing surgery: A systematic review. JAm Med Dir Assoc. 2022;4:528-536.e2. https://doi.org/10.1016/j.jamda.2021.11.005.
Costello A, Hudson E, Morrissey S, Sharma D, Kelly D, Doody O. Management of psychotropic medications in adults with intellectual disability: a scoping review. Ann Med. 2022;54(1):2486–99. https://doi.org/10.1080/07853890.2022.2121853.
Cateau D, Ballabeni P, Niquille A. Effects of an interprofessional deprescribing intervention in Swiss nursing homes: the Individual Deprescribing Intervention (IDeI) randomised controlled trial. BMC Geriatr. 2021;21(1):655. https://doi.org/10.1186/s12877-021-02465-7.
Mena S, Moullin JC, Schneider M, Niquille A. Implementation of interprofessional quality circles on deprescribing in Swiss nursing homes: an observational study. BMC Geriatr. 2023;23(1):620. https://doi.org/10.1186/s12877-023-04335-w.
Wong APY, Ting TW, Charissa EJM, Boon TW, Heng KY, Leng LL. Feasibility & Efficacy of Deprescribing rounds in a Singapore rehabilitative hospital- a randomised controlled trial. BMC Geriatr. 2021;21(1):584. https://doi.org/10.1186/s12877-021-02507-0.
Kua CH, Yeo CYY, Tan PC, Char CWT, Tan CWY, Mak V, Leong IY, Lee SWH. Association of deprescribing with reduction in mortality and hospitalization: A pragmatic stepped-wedge cluster-randomized controlled trial. J Am Med Dir Assoc. 2021;22(1):82–9. https://doi.org/10.1016/j.jamda.2020.03.012.
Cateau D, Ballabeni P, Niquille A. Effects of an interprofessional QualityCircle-Deprescribing Module (QC-DeMo) in Swiss nursing homes: a randomised controlled trial. BMC Geriatr. 2021;21(1):289. https://doi.org/10.1186/s12877-021-02220-y.
Clarkson L, Hart L, Lam AK, Khoo TK. Reducing inappropriate polypharmacy for older patients at specialist outpatient clinics: a systematic review. Curr Med Res Opin. 2023;39(4):545–54. https://doi.org/10.1080/03007995.2023.2185390.
Balsom C, Pittman N, King R, Kelly D. Impact of a pharmacist-administered deprescribing intervention on nursing home residents: a randomized controlled trial. Int J Clin Pharm. 2020;42(4):1153–67. https://doi.org/10.1007/s11096-020-01073-6.
Smith NI, Martinez AI, Huffmyer M, Eckmann L, George R, Abner EL, Jicha GA, Moga DC. Acceptability of patient-centered, multi-disciplinary medication therapy management recommendations: results from the INCREASE randomized study. BMC Geriatr. 2023;23(1):137. https://doi.org/10.1186/s12877-023-03876-4.
Quek HW, Etherton-Beer C, Page A, McLachlan AJ, Lo SY, Naganathan V, Kearney L, Hilmer SN, Comans T, Mangin D, Lindley RI, Potter K. Deprescribing for older people living in residential aged care facilities: Pharmacist recommendations, doctor acceptance and implementation. Arch Gerontol Geriatr. 2023;107: 104910. https://doi.org/10.1016/j.archger.2022.104910.
Greiver M, Dahrouge S, O’Brien P, Manca D, Lussier MT, Wang J, Burge F, Grandy M, Singer A, Twohig M, Moineddin R, Kalia S, Aliarzadeh B, Ivers N, Garies S, Turner JP, Farrell B. Improving care for elderly patients living with polypharmacy: protocol for a pragmatic cluster randomized trial in community- based primary care practices in Canada. Implement Sci. 2019;14(1):55. https://doi.org/10.1186/s13012-019-0904-4.
de Oliveira AM, Varallo FR, Rodrigues JPV, Aguilar GJ, da Costa Lima NK, Leira Pereira LR. Contribution of pharmaceutical care to person-centered health care and the safety of pharmacotherapy for hospitalized older individuals in Brazil: An investigative single-arm intervention trial. Curr Drug Saf. 2023;18(2):253–63. https://doi.org/10.2174/1574886317666220614140433.
Moga DC, Beech BF, Abner EL, Schmitt FA, El Khouli RH, Martinez AI, Eckmann L, Huffmyer M, George R, Jicha GA. INtervention for Cognitive Reserve Enhancement in delaying the onset of Alzheimer’s Symptomatic Expression (INCREASE), a randomized controlled trial: rationale, study design, and protocol. Trials. 2019;20(1):806. https://doi.org/10.1186/s13063-019-3993-0.
Kari H, Kortejärvi H, Airaksinen M, Laaksonen R. Patient involvement is essential in identifying drug-related problems. Br J Clin Pharmacol. 2018;84(9):2048–58. https://doi.org/10.1111/bcp.13640.
Gillespie R, Mullan J, Harrison L. Exploring older adult health literacy in the day-to-day management of polypharmacy and making decisions about deprescribing: A mixed methods study. Health Lit Res Pract. 2023;7(1):e14–25. https://doi.org/10.3928/24748307-20221216-01.
Gillespie R, Mullan J, Harrison L. Attitudes towards deprescribing and the influence of health literacy among older Australians. Prim Health Care Res Dev. 2019;20: e78. https://doi.org/10.1017/S1463423618000919.
Furr S, Lane SH, Martin D, Brackney DE. Understanding roles in health care through interprofessional educational experiences. British journal of nursing (Mark Allen Publishing). 2020;29(6):364–72. https://doi.org/10.12968/bjon.2020.29.6.364.
Mozer C, Gilbertson J, Robinson M, Kelemen L, Kostas T. Understanding the roles of physical therapists on the care team: An interprofessional education experience for first-year medical students. J Interprofessional Educ Pract. 2021;24: 100463. https://doi.org/10.1016/j.xjep.2021.100463.
Bayliss EA, Albers K, Gleason K, et al. Recommendations for outcome measurement for deprescribing intervention studies. J Am Geriatr Soc. 2022;70(9):2487–97. https://doi.org/10.1111/jgs.17894.
Doherty AJ, Boland P, Reed J, et al. Barriers and facilitators to deprescribing in primary care: a systematic review. BJGP Open. 2020;4(3):bjgpopen20X101096. https://doi.org/10.3399/bjgpopen20X101096.
Rozsnyai Z, Jungo KT, Reeve E, et al. What do older adults with multimorbidity and polypharmacy think about deprescribing? The LESS study - a primary care-based survey. BMC Geriatr. 2020;20(1):435. https://doi.org/10.1186/s12877-020-01843-x.
O’Mahony D. STOPP/START criteria for potentially inappropriate medications/potential prescribing omissions in older people: origin and progress. Expert Rev Clin Pharmacol. 2020;13(1):15–22. https://doi.org/10.1080/17512433.2020.1697676.
Hanlon JT, Schmader KE. The medication appropriateness index: A clinimetric measure. Psychother Psychosom. 2022;91(2):78–83. https://doi.org/10.1159/000521699.
Ferreri SP, Blalock SJ, Robinson JM, Renfro CP, Busby-Whitehead J, Burns ER, Haddad Y. STEADI-Rx Older Adult Fall Prevention Guide for Community Pharmacists. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2020. Retrieved Jan 2024.
Yen PH, Leasure AR. Use and effectiveness of the teach-back method in patient education and health outcomes. Fed Pract. 2019;36(6):284–9.
Prokopidis K, Giannos P, Reginster JY, et al. Sarcopenia is associated with a greater risk of polypharmacy and number of medications: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2023;14(2):671–83. https://doi.org/10.1002/jcsm.13190.
Hasselgren PO, Alamdari N, Aversa Z, Gonnella P, Smith IJ, Tizio S. Corticosteroids and muscle wasting: role of transcription factors, nuclear cofactors, and hyperacetylation. Curr Opin Clin Nutr Metab Care. 2010;13(4):423–8. https://doi.org/10.1097/MCO.0b013e32833a5107.
Bouitbir J, Sanvee GM, Panajatovic MV, Singh F, Krähenbühl S. Mechanisms of statin-associated skeletal muscle-associated symptoms. Pharmacol Res. 2020;154: 104201. https://doi.org/10.1016/j.phrs.2019.03.010.
Nassar Y, Richter S. Proton-pump inhibitor use and fracture risk: An updated systematic review and meta-analysis. J Bone Metab. 2018;25(3):141–51. https://doi.org/10.11005/jbm.2018.25.3.141.
Azimi Manavi B, Stuart AL, Pasco JA, et al. Antipsychotic medication use and fracture: a case-control study. Sci Rep. 2023;13(1):13709. https://doi.org/10.1038/s41598-023-40762-w.
Edinoff AN, Nix CA, Hollier J, et al. Benzodiazepines: Uses, dangers, and clinical considerations. Neurol Int. 2021;13(4):594–607. https://doi.org/10.3390/neurolint13040059.
Ghossein N, Kang M, Lakhkar AD. Anticholinergic Medications. [Updated 2023 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
Loprinzi PD, Loenneke JP. The effects of antihypertensive medications on physical function. Prev Med Rep. 2016;3:264–9. https://doi.org/10.1016/j.pmedr.2016.03.009.
Davis A, Robson J. The dangers of NSAIDs: look both ways. Br J Gen Pract. 2016;66(64):172–3. https://doi.org/10.3399/bjgp16X684433.
George SZ, Goode AP. Physical therapy and opioid use for musculoskeletal pain management: competitors or companions? Pain Rep. 2020;5(5): e827.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Global Health; Board on Health Sciences Policy; Global Forum on Innovation in Health Professional Education; Forum on Neuroscience and Nervous System Disorders, Stroud C, Posey Norris SM, Bain L (Eds.). The Role of Nonpharmacological Approaches to Pain Management: Proceedings of a Workshop. National Academies Press (US). 2019.
Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of physicians. Ann Intern Med. 2017;166:514–30.
Thorlund JB, Simic M, Pihl K, et al. Similar effects of exercise therapy, nonsteroidal anti-inflammatory drugs, and opioids for knee osteoarthritis pain: A systematic review with network meta-analysis. J Orthop Sports Phys Ther. 2022;52(4):207–16. https://doi.org/10.2519/jospt.2022.10490.
Fank F, Pereira FDS, Dos Santos L, de Mello MT, Mazo GZ. Effects of exercise on sleep in older adults: An overview of systematic reviews and meta-analyses. J Aging Phys Act. 2022;30(6):1101–17. https://doi.org/10.1123/japa.2021-0444.
Jalalinia SF, Raei M, Naseri-Salahshour V, Varaei S. The effect of pelvic floor muscle strengthening exercise on urinary incontinence and quality of life in patients after prostatectomy: a randomized clinical trial. J Caring Sci. 2020;9(1):33–8. https://doi.org/10.34172/jcs.2020.006.
Posadzki P, Pieper D, Bajpai R, et al. Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews. BMC Public Health. 2020;20(1):1724. https://doi.org/10.1186/s12889-020-09855-3.
Schuch FB, Vancampfort D. Physical activity, exercise, and mental disorders: it is time to move on. Trends Psychiatry Psychother. 2021;43(3):177–84. https://doi.org/10.47626/2237-6089-2021-0237.
Funding
Open access funding provided by Northeastern University Library
Author information
Authors and Affiliations
Contributions
AP wrote the entire manuscript. No other authors. Figure provided is original.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclosures
American Physical Therapy Association Academy of Neurology Practice Committee member and payment chair. American Physical Therapy Association of Massachusetts - Board of Directors as Chief Assembly Representative of Southeastern District and State Delegate at Large. Receive royals as speaker for Medbridge Inc and STREAMED.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Perron, A.E. Towards a Prescription for Change: Interprofessional Management of Polypharmacy and Deprescribing. Curr Geri Rep (2024). https://doi.org/10.1007/s13670-024-00420-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s13670-024-00420-z