Abstract
Introduction
Real-world data on the efficacy of risankizumab (RZB) in clinical moderate-to-severe plaque psoriasis (PsO) are limited. The RAPID study assessed real-world clinical and patient-reported outcomes in RZB-treated PsO patients using data collected from dermatologists in Canada, the Czech Republic, Germany, Japan, and Poland.
Methods
This ongoing, retrospective chart review collected data from medical records of RZB-treated adults with moderate-to-severe PsO (09/2022–06/2023). Eligible patients received RZB, had ≥ 12 months of medical records after RZB initiation (index date), and had Psoriasis Area and Severity Index (PASI), Investigator Global Assessment (IGA), or static Physician’s Global Assessment (sPGA) scores ≥ 3 months before and up to 18 months after the index date. The proportion of patients achieving a clear/almost clear PsO (IGA/sPGA = 0/1), PASI ≤ 1, Dermatology Life Quality Index (DLQI) = 0/1, and a 90%/100% improvement from baseline in PASI as well as the mean changes in PASI, DLQI, itch, and skin pain scores at 12 and 18 months were reported for patients with non-missing assessments at baseline and 12 months.
Results
Most patients (66.4%) were male, 74.0% were biologic naïve, and 73.0% had scalp PsO. Mean baseline IGA/sPGA was 3.7 ± 0.5, with a mean PASI of 23.3 ± 11.8. After 12 months, 86.1% of patients reported IGA/sPGA ≤ 1, and 75.7% achieved PASI90; these further increased to 91.1% and 80.5% at 18 months. DLQI, itch, and skin pain scores improved over time.
Conclusions
These data demonstrated the durable, real-world effectiveness of RZB in patients with moderate-to-severe PsO through continued improvement in disease and symptom severity over 18 months, with most of the patients reporting clear/almost clear skin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The efficacy and safety of risankizumab in the treatment of moderate-to-severe plaque psoriasis has been demonstrated in phase 3 clinical trials. |
Data on the efficacy of risankizumab in the treatment of moderate-to-severe plaque psoriasis in clinical practice are limited, especially outside the United States. |
This study assessed clinical and patient-reported outcomes in patients with psoriasis using data collected from dermatologists in the RAPID study, a retrospective, multi-country (Czech Republic, Germany, Japan, Poland, and Canada) medical chart review. |
What was learned from this study? |
In this real-world analysis of data from patients with moderate-to-severe psoriasis, those who received treatment with risankizumab demonstrated significant improvements in disease severity at 12 and 18 months. |
Most patients reported clear or almost clear skin after risankizumab treatment, which was accompanied by marked improvements in patient-reported quality of life and patient-reported itch and skin pain. |
Introduction
Psoriasis (PsO) is an autoimmune disease characterized by distinct, scaly, and itchy skin lesions [1,2,3]. Treatment targets generally include decreasing the body surface area affected by PsO lesions, which has also been shown to greatly improve patient-reported health-related quality of life (HRQoL) [1,2,3,4].
Both the American Academy of Dermatology and the National Psoriasis Foundation recommend that patients with PsO who have an inadequate response/intolerance to topical therapies as well as phototherapy should receive advanced therapies (i.e., systemic nonbiologic or biologic agents) to help manage disease [5, 6]. However, it is recommended that patients with moderate-to-severe disease that are not expected to respond to, or have contraindications to, nonbiologic systemic agents receive biologic therapies as first-line treatments [6, 7]. There are several biologic treatment options for patients with moderate-to-severe PsO, including tumor necrosis factor (TNF) inhibitors (e.g., adalimumab, etanercept, infliximab, certolizumab), interleukin (IL)-17 inhibitors (e.g., ixekizumab, secukinumab, brodalumab, bimekizumab), and IL-23 inhibitors (e.g., risankizumab [RZB], ustekinumab, guselkumab, tildrakizumab) [6].
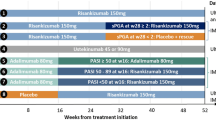
In 2019, risankizumab (RZB) was approved for use in patients with moderate-to-severe PsO who are candidates for systemic therapy or phototherapy. The efficacy and safety of RZB had been demonstrated in several large, randomized phase 3 clinical trials (i.e., IMMerge [NCT03478787], ULTIMMA-1 [NCT02684370], ULTIMMA-2 [NCT02684357], IMMHANCE [NCT02672852], and IMMVENT [NCT02694523]) [8,9,10,11]. In these studies, RZB-treated patients reported high rates of skin clearance, with most patients reporting clear and/or almost clear skin [8,9,10,11,12]. Moreover, RZB demonstrated significantly greater efficacy compared to adalimumab [11] and secukinumab [8].
Despite strong evidence from clinical trials, there is limited real-world evidence on patient outcomes following treatment with RZB, especially outside of the United States. Thus, this study sought to describe characteristics and clinical outcomes of patients with PsO using data collected from the RisAnkizumab for the treatment of moderate-to-severe Psoriasis—An International meDical chart review (RAPID) study, which recruited physicians from an existing panel of dermatologists in Canada, the Czech Republic, Germany, Japan, and Poland.
Methods
Study Design and Participants
This retrospective, multi-country medical chart review study started collecting data in 09/2022. Data on adult patients with PsO were collected from licensed dermatologists who had actively treated adult patients with PsO for ≥ 3 years and had direct access to patient medical charts. Medical chart data were abstracted by eligible dermatologists from Canada, Germany, Japan, Poland, and the Czech Republic. Dermatologists were recruited from a physician panel that included the Leaders in Medicine Atlas, a large directory of > 3.5 million physician profiles. To be eligible for the study, patients had to fulfill the following criteria: (1) they were initiating treatment with RZB on or after 01/2019, (2) they had medical records available for ≥ 6 months pre-index date, and (3) they had medical records available for ≥ 12 months post-index date. For this analysis, the index date was defined as the date of RZB treatment initiation. All patients were required to have moderate-to-severe PsO, as defined by a baseline Investigator Global Assessment (IGA) or static Physician’s Global Assessment (sPGA) score ≥ 3. Patients were required to have at least three recorded Psoriasis Area and Severity Index (PASI), IGA, or sPGA scores, with one score recorded ≤ 3 months before the index date, one score recorded ≤ 6 months after the index date, and one score recorded between 7 and 18 months post-index date. For this analysis, patients were included only if they had non-missing IGA/sPGA scores at baseline and at 12 months. Likewise, patients were required to have ≥ 1 Dermatology Life Quality Index (DLQI) score within 3 months pre-index date and ≥ 1 recorded DLQI score within 18 months post-index date.
Ethics Statement
This study was conducted in accordance with ethical principles that have their origin in the current Declaration of Helsinki and was consistent with International Conference on Harmonization Good Clinical Practice, Good Epidemiology Practices, and applicable regulatory requirements. This study received approval from a central institutional review board to use de-identified data from electronic health records for this analysis.
Outcomes
This study assessed the impact of RZB treatment on disease severity (measured by IGA and/or sPGA), skin clearance (measured by PASI), patient-reported HRQoL (measured by DLQI), and symptom improvement (measured by the visual analog scale [VAS]). IGA is a physician-rated assessment of disease severity scored on a 0- to 5-point scale; higher scores denote greater disease severity [13]. Similarly, sPGA is a physician-rated, point-in-time measure that assesses disease severity on a 0- to 4-point scale, with higher scores denoting greater disease severity [14]. PASI is an assessment widely used in PsO clinical trials to assess disease severity by separately assessing four body regions (i.e., head, upper extremities, trunk, and lower extremities). Scores can range from 0 to 72, with higher scores denoting disease activity and scores ≥ 10 denoting moderate-to-severe disease [14]. All of the aforementioned disease severity measures specifically assess erythema, scaling, and induration [13, 14]. The DLQI has a total score range of 0–30, with higher scores indicating poorer HRQoL; scores of 0–1, 2–5, 6–10, 11–20, and 21–30 indicate no, small, moderate, very large, and extremely large effects on patient HRQoL, respectively [14]. Skin pain and itch were assessed on VAS, wherein each patient scored their symptoms from 0 to 10, with higher scores denoting more severe symptoms [15].
Outcomes related to disease severity were the proportion of patients achieving clear and/or almost clear PsO (defined as IGA/sPGA = 0 and/or 1) as well as a 90% or 100% improvement in Psoriasis Activity and Severity Index (PASI) scores from baseline to follow-up (i.e., PASI 90 or PASI 100, respectively). The proportion of patients achieving an absolute PASI (aPASI) score of 0 and/or 1, as well as the mean change from baseline to follow-up in aPASI scores, is also reported. Similarly, the mean change from baseline to follow-up in DLQI scores as well as the proportion of patients achieving DLQI = 0/1 (i.e., little to no disease-related quality of life impairment) were determined. Mean scores for patient-reported itch and skin pain at baseline and follow-up are also reported. All outcomes were assessed at 12 and 18 months post-index date. Only those patients with non-missing data at baseline and 12 months were included in this analysis.
Statistical Analysis of Data
All outcomes are reported for patients with moderate-to-severe PsO who met the inclusion criteria. Data are reported at baseline, 12 months, and 18 months. The paired t test (for normally distributed outcomes) or Wilcoxon signed-rank test (for non-normally distributed outcomes) were used to compare the outcomes (i.e., mean aPASI, DLQI, itch, and pain scores) at baseline and follow-up (i.e., 12 and 18 months) for patients who had both baseline and 12-month outcome measures. The comparisons of outcomes (PASI, DLQI, itch VAS, pain VAS) between baseline and 12 months as well as between baseline and 18 months were adjusted for multiple comparisons using the Bonferroni approach (adjusted p value = 0.05/2). All analyses were performed using R Statistical Software under the RStudio environment (v4.2.3; RStudio Team 2023, Boston, MA, USA).
Results
Baseline Demographic and Clinical Characteristics
A total of 296 patients with moderate-to-severe PsO, as defined by an IGA/sPGA score ≥ 3 at baseline, were included in the analysis (Table 1). The mean (± SD) age was 48.7 ± 12.1 years, with a mean of 10.2 ± 10.2 years since PsO diagnosis, and two-thirds (66.6%) were male. Overall, one-third of patients were located in Japan (n = 98; 33.1%), with 23.6% (n = 70), 22.0% (n = 65), 20.9% (n = 62), and 0.3% (n = 1) of patients located in Canada, Poland, Germany, and the Czech Republic, respectively. The mean IGA/sPGA score was 3.7 ± 0.5, with a mean percent body surface area affected by PsO of 26.4 ± 15.7 and a mean aPASI of 23.3 ± 11.8. Most patients were biologic naïve (n = 219; 74.0%). Of those with prior biologic exposure (n = 77), the majority had received a TNF inhibitor (n = 46; 63.6%). Nearly half of patients had a family history of PsO (n = 139; 47.0%), with most patients reporting PsO lesions on their scalp (n = 216; 73.0%); 43.9%, 38.2%, and 37.2% reported PsO lesions on their nails, face, and skin folds, respectively. The mean DLQI score was 15.7 ± 7.2 (i.e., a very large effect on HRQoL), with mean itch and skin pain scores of 7.4 ± 6.0 and 5.2 ± 5.6, respectively.
Achievement of Clear or Almost Clear Skin Through 18 Months
After 12 months of RZB treatment, more than half of the patients (n/N = 164/296; 55.4%) achieved clear skin (i.e., IGA/sPGA = 0; Fig. 1a); 86.1% (n/N = 255/296) achieved clear or almost clear skin (i.e., IGA/sPGA ≤ 1). The proportion of patients achieving clear and/or almost clear skin continued to increase through 18 months of treatment (clear skin: n/N = 102/168, 60.7%; clear/almost clear skin: n/N = 153/168, 91.1%).
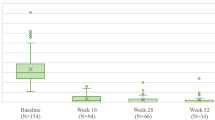
Proportion of patients achieving clear or almost clear skin and mean change in PASI through 18 months of treatment with RZB. The proportion of patients achieving clear or almost clear skin as measured by a IGA/sPGA = 0 or IGA/sPGA ≤ 1, b mean aPASI, c aPASI = 0 or aPASI ≤ 1, and d a 90% or 100% improvement in PASI score compared to baseline. The proportions of patients achieving aPASI = 0 and PASI 100 differ slightly due to differences in reporting (i.e., some providers only provided one or the other, not both). Patients included in the analysis had non-missing values at both baseline and 12 months. IGA Investigator Global Assessment, (a)PASI (absolute) Psoriasis Area and Severity Index, sPGA static Physician’s Global Assessment. p values represent significant differences from baseline
The mean (± SD) aPASI score at baseline was 23.4 ± 11.9 (median [IQR]: 20.0 [15.2–29.0]) and was significantly (P < 0.001) reduced to 1.7 ± 3.2 (median [IQR]: 1.0 [0.0–2.0]) and 0.7 ± 1.4 (median [IQR]: 0.0 [0.0–1.0]) at 12 and 18 months, respectively (Fig. 1b). Overall, 47.0% and 67.6% of the patients achieved clear (aPASI = 0) or clear/almost clear skin (aPASI ≤ 1) at 12 months, respectively, which increased to 57.1% and 82.1%, respectively, at 18 months (Fig. 1c). In this analysis, most patients achieved a 90% improvement in disease severity (i.e., PASI 90) at 12 (75.7%) and 18 months (80.5%; Fig. 1d). Nearly half of the patients (46.8%) achieved a 100% improvement in PASI (i.e., PASI 100) at 12 months, with 57.1% of patients achieving PASI 100 at 18 months.
Improvement in Health-Related Quality of Life and Disease-Related Symptoms Through 18 Months
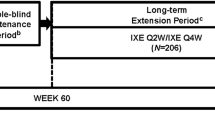
Patients receiving RZB reported a marked improvement in health-related quality of life, as measured by DLQI. Among those with non-missing IGA/sPGA data at baseline and 12 months, the mean ± SD DLQI at baseline was 15.7 ± 7.2, which significantly (P < 0.001) decreased to 1.6 ± 2.7 (median [IQR]: 1.0 [0.0–2.0]) and 0.9 ± 1.8 (median [IQR]: 0.0 [0.0–1.0]) at 12 and 18 months, respectively (Fig. 2a). Thus, the mean change from baseline to follow-up at 12 months (− 14.1 points) was sustained out to 18 months (− 14.8 points). Likewise, the proportion of patients reporting little to no disease-related quality of life impairment at 12 months was 70.2%, which increased to 79.5% at 18 months (Fig. 2b).
Change in patient-reported quality of life, itch, and skin pain scores through 18 months. Change in patient-reported quality of life as measured by a the change in mean DLQI score from baseline to follow-up, b the proportion of patients achieving DLQI = 0/1, and c the changes in mean itch and skin pain scores from baseline to follow-up. Patients included in the analysis has non-missing values at both baseline and 12 months. DLQI Dermatology Life Quality Index, VAS visual analogue scale. p values represent significant differences from baseline
Patients that received RZB also reported a marked improvement in disease-related symptoms (Fig. 2c). At baseline, patients reported mean (± SD) itch and pain scores of 7.4 ± 6.0 and 5.2 ± 5.6, respectively. By 12 months, the mean ± SD itch and pain scores were significantly (P < 0.001) reduced to 0.7 ± 1.2 (median [IQR]: 0.0 [0.0–1.0]) and 1.0 ± 1.1 (median [IQR]: 0.5 [0.0–2.0]), respectively; these scores further decreased to 0.5 ± 0.8 (median [IQR]: 0.0 [0.0–1.0]; P < 0.001) and 0.3 ± 0.5 (median [IQR]: 0.0 [0.0–1.0]; P = 0.009), respectively, by 18 months.
Discussion
This real-world analysis of patients with moderate-to-severe PsO demonstrated that RZB treatment resulted in high rates of skin clearance after 12 and 18 months of treatment. Indeed, more than half of the patients in this study achieved clear skin (i.e., IGA/sPGA = 0) at 12 months, a proportion which increased to 60.7% by 18 months. Moreover, improvements in skin clearance were also associated with improved patient-reported outcomes and disease-related symptoms. After 18 months of treatment, 79.5% of patients reported little to no disease-related quality of life impairment (i.e., DLQI = 0/1); 80.5% of patients demonstrated a 90% improvement in PASI scores by 18 months. Likewise, after 18 months of RZB treatment, patients reported mean scores of 0.5 and 0.3 (scale: 0–10) for disease-related itch and skin pain severity, respectively. These data highlight the robust real-world benefits of RZB treatment in patients with moderate-to-severe PsO.
These findings are in line with previous reports of real-world clinical outcomes in RZB-treated patients with PsO. One Italian study of patients with PsO receiving treatment from the Psoriasis Care Centre of Dermatology in Naples demonstrated that 83% of patients achieved a 90% improvement in PASI at 52 weeks, which increased to 88% at 88 weeks [16]. A second study, conducted among patients with PsO receiving care from the dermatology unit of the IRCCS Humanitas Research Hospital in Milan, demonstrated that 79% of patients achieved a 90% improvement in PASI at 52 weeks [17]. A third study, which leveraged data from the CorEvitas Psoriasis Registry, showed that 65.6% of patients with PsO achieved a 90% improvement in PASI after approximately 12 months of RZB treatment; when stratified by prior biologic exposure, 78.9% of biologic-naïve patients versus 53.9% of biologic-experienced patients achieved this milestone [18]. Interestingly, all of those studies consisted of patients with milder disease severity, as determined by aPASI, than that of the patients included in this analysis (mean baseline aPASI: 15.3 ± 5.9 [16], 13.5 ± 8.1 [17], and 10.1 ± 6.9 [18] vs. 23.3 ± 11.8). The results of this analysis, which showed that 80.5% of patients reached PASI 90 at 18 months, are also consistent with data from RZB clinical trials. In the IMMerge trial, which compared RZB to secukinumab in patients with moderate-to-severe PsO, 86.6% of RZB-treated patients achieved PASI 90 at week 52 [8]. In the UltIMMa-1 and UltIMMa-2 trials, which compared RZB to ustekinumab, 81.9% and 80.6% of RZB-treated patients, respectively, achieved PASI 90 [9]. Likewise, 57.6% and 59.5% of RZB-treated patients in UltIMMa-1 and UltIMMa-2, respectively, reached sPGA = 0 at week 52 [9]; 60.7% of patients in this analysis had IGA/sPGA = 0 at 18 months. This analysis also included patients with worse disease severity at baseline than that of patients included in clinical trials (mean baseline PASI: 19.8 ± 6.3 [IMMerge] [8] vs. 20.6 ± 7.7 [UltIMMa-1] [9] vs. 20.5 ± 7.8 [UltIMMa-2] [9] vs. 23.3 ± 11.8). Altogether, these data highlight the durable therapeutic benefits of RZB treatment for patients with PsO, regardless of disease severity.
The current analysis demonstrated a marked improvement in health-related quality of life, as measured by DLQI and disease-related itch and skin pain. These data are consistent with other reports which have demonstrated that achieving greater levels of skin clearance was associated with better quality of life, reduced work impairment, and reduced symptom severity [19]. Clinical trials for RZB demonstrated that 80% of patients achieved DLQI ≤ 1 (i.e., little to no disease-related impairment in quality of life) at 52 weeks [20], which is comparable to the proportion of patients with moderate-to-severe PsO achieving that milestone in this analysis.
This is one of the first studies to analyze real-world treatment outcomes in RZB-treated patients with moderate-to-severe PsO from several countries (i.e., the Czech Republic, Germany, Japan, Poland, and Canada). Likewise, this study is the first to analyze long-term (i.e., 18 months) real-world treatment outcomes and is supported by recent analyses of the ongoing phase 3 LIMMitless trial, which showed that up to 5 years of RZB treatment has durable efficacy and is well tolerated [21]. Compared to clinical trials and other studies, the patients included in this analysis had worse disease severity, as determined by baseline PASI scores (i.e., mean aPASI scores in this analysis were 8.0–13.2 points greater than other real-world studies and approximately 3 points higher than that from clinical trials), prior to treatment initiation and yet still demonstrated significant and robust improvements in disease severity and quality of life, highlighting the therapeutic benefits of RZB. A limitation of this analysis is that it only included those patients who were receiving treatment by experienced dermatologists and thus may not be fully generalizable to a larger PsO population. While non-random chart selection may introduce sampling bias, we aimed to minimize this through the implementation of a randomization tool that was used as part of the data collection process. Nonetheless, the non-randomized, retrospective design of this study could still have resulted in residual bias.
Conclusions
This analysis demonstrated the long-term, durable, real-world effectiveness of RZB in patients with moderate-to-severe PsO. Patients in this analysis demonstrated continued improvements in disease and symptom severity over 18 months, with > 90% of patients reporting clear or almost clear skin. Moreover, 80% of patients reported little to no impact of the disease on their quality of life after 18 months of RZB treatment. This study is currently ongoing and aims to assess these outcomes in a larger population in the future.
Data Availability
The data reported in this study are available from the corresponding author upon reasonable request.
References
Kivelevitch D, Frieder J, Watson I, Paek SY, Menter MA. Pharmacotherapeutic approaches for treating psoriasis in difficult-to-treat areas. Expert Opin Pharmacother. 2018;19(6):561–75.
Lanna C, Galluzzi C, Zangrilli A, Bavetta M, Bianchi L, Campione E. Psoriasis in difficult to treat areas: treatment role in improving health-related quality of life and perception of the disease stigma. J Dermatol Treat. 2022;33(1):531–4.
Lanna C, Zangrilli A, Bavetta M, Campione E, Bianchi L. Efficacy and safety of adalimumab in difficult-to-treat psoriasis. Dermatol Ther. 2020;33(3): e13374.
Aldredge LM, Higham RC. Manifestations and management of difficult-to-treat psoriasis. J Dermatol Nurses Assoc. 2018;10(4):189–97.
Menter A, Gelfand JM, Connor C, Armstrong AW, Cordoro KM, Davis DMR, et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82(6):1445–86.
Menter A, Strober BE, Kaplan DH, Kivelevitch D, Prater EF, Stoff B, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–72.
Nast A, Smith C, Spuls PI, Avila Valle G, Bata-Csorgo Z, Boonen H, et al. EuroGuiDerm guideline on the systemic treatment of psoriasis vulgaris—Part 1: treatment and monitoring recommendations. J Eur Acad Dermatol Venereol. 2020;34(11):2461–98.
Warren RB, Blauvelt A, Poulin Y, Beeck S, Kelly M, Wu T, et al. Efficacy and safety of risankizumab vs. secukinumab in patients with moderate-to-severe plaque psoriasis (IMMerge): results from a phase III, randomized, open-label, efficacy-assessor-blinded clinical trial. Br J Dermatol. 2021;184(1):50–9.
Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392(10148):650–61.
Suleiman AA, Khatri A, Oberoi RK, Othman AA. Exposure–response relationships for the efficacy and safety of risankizumab in Japanese subjects with psoriasis. Clin Pharmacokinet. 2020;59(5):575–89.
Reich K, Gooderham M, Thaci D, Crowley JJ, Ryan C, Krueger JG, et al. Risankizumab compared with adalimumab in patients with moderate-to-severe plaque psoriasis (IMMvent): a randomised, double-blind, active-comparator-controlled phase 3 trial. Lancet. 2019;394(10198):576–86.
Banaszczyk K. Risankizumab in the treatment of psoriasis—literature review. Reumatologia. 2019;57(3):158–62.
Papp K, Reich K, Leonardi CL, Kircik L, Chimenti S, Langley RG, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol. 2015;73(1):37–49.
Canadian Agency for Drugs and Technologies in Health. Appendix 5: validity of outcome measures 2019 [updated June 2019]. https://www.ncbi.nlm.nih.gov/books/NBK544841/.
Strand V, Boers M, Idzerda L, Kirwan JR, Kvien TK, Tugwell PS, et al. It’s good to feel better but it’s better to feel good and even better to feel good as soon as possible for as long as possible. Response criteria and the importance of change at OMERACT 10. J Rheumatol. 2011;38(8):1720–7.
Megna M, Ruggiero A, Battista T, Marano L, Cacciapuoti S, Potestio L. Long-term efficacy and safety of risankizumab for moderate to severe psoriasis: a 2-year real-life retrospective study. J Clin Med. 2023;12(9):3233.
Gargiulo L, Ibba L, Pavia G, Vignoli CA, Piscazzi F, Valenti M, et al. Real-life effectiveness and safety of risankizumab in 131 patients affected by moderate-to-severe plaque psoriasis: a 52-week retrospective study. Dermatol Ther (Heidelb). 2022;12(10):2309–24.
Strober B, Ferris L, Callis Duffin K, Janak JC, Sima AP, Eckmann T, et al. Real-world effectiveness of risankizumab in patients with moderate-to-severe psoriasis using the CorEvitas Psoriasis Registry. J Am Acad Dermatol. 2024;90(1):82–90.
Korman NJ, Malatestinic W, Goldblum OM, Murage MJ, Renda L, Lin CY, et al. Assessment of the benefit of achieving complete versus almost complete skin clearance in psoriasis: a patient’s perspective. J Dermatol Treat. 2022;33(2):733–9.
Gooderham M, Pinter A, Ferris LK, Warren RB, Zhan T, Zeng J, et al. Long-term, durable, absolute Psoriasis Area and Severity Index and health-related quality of life improvements with risankizumab treatment: a post hoc integrated analysis of patients with moderate-to-severe plaque psoriasis. J Eur Acad Dermatol Venereol. 2022;36(6):855–65.
Papp KA, Blauvelt A, Puig L, Ohtsuki M, Beissert S, Gooderham M, et al. Long-term safety and efficacy of risankizumab for the treatment of moderate-to-severe plaque psoriasis: Interim analysis of the LIMMitless open-label extension trial up to 5 years of follow-up. J Am Acad Dermatol. 2023;89(6):1149–58.
Acknowledgements
The authors would like to thank the participants of the study.
Medical Writing/Editorial Assistance
Medical writing services were provided by Samantha Francis Stuart, PhD, of Fishawack Facilitate Ltd, part of Avalere Health, and funded by AbbVie.
Funding
AbbVie funded the study as well as the journal’s Rapid Service and Open Access fees. AbbVie participated in the study design, research, interpretation of the data, review, and approval. All authors had access to the relevant data and participated in the drafting, review, and approval of the abstract. No honoraria or payments were made for authorship.
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting and critically revising the manuscript for intellectual content, and all authors have read and approved the final version. Ahmed M. Soliman substantially contributed to study conception and design. Ahmed M. Soliman, Irina Pivneva, Roksana Ghanbariamin, and Min Yang contributed to data acquisition. Irina Pivneva, Roksana Ghanbariamin, Min Yang, and Bang Truong contributed to data analysis, and Irina Pivneva, Roksana Ghanbariamin, Min Yang, Bang Truong, and Ahmed M. Soliman contributed to data interpretation.
Corresponding author
Ethics declarations
Conflict of Interest
Andreas Pinter has served as an advisor and/or speaker and/or received grants and/or served as an investigator for AbbVie, Almirall Hermal, Amgen, Biogen, BMS, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Eli Lilly, Eva Pharma, Galderma, Hexal, Janssen, LEO Pharma, MC2, Medac, Merck Serono, Mitsubishi, MSD, Novartis, Pascoe, Pfizer, Tigercat Pharma, Regeneron, Roche, Sandoz Biopharmaceuticals, Sanofi Genzyme, Schering-Plough, UCB, and Zuellig Pharma. Luis Puig has received consultancy/speaker’s honoraria from and/or participated in clinical trials sponsored by AbbVie, Almirall, Amgen, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Janssen, LEO Pharma, Lilly, Novartis, Pfizer, Sandoz, Sanofi, and UCB. Mark Lebwohl is an employee of Mount Sinai and receives research funds from: AbbVie, Amgen, Arcutis, Avotres, Boehringer Ingelheim, Cara Therapeutics, Dermavant Sciences, Eli Lilly, Incyte, Janssen Research & Development, LLC, Ortho Dermatologics, Regeneron, and UCB, Inc., and is a consultant for Aditum Bio, Almirall, AltruBio Inc., AnaptysBio, Arcutis, Inc., Aristea Therapeutics, Avotres Therapeutics, Brickell Biotech, Boehringer Ingelheim, Bristol Myers Squibb, Cara Therapeutics, Castle Biosciences, Celltrion, CorEvitas, Dermavant Sciences, Dr. Reddy, EPI, Evommune, Inc., Facilitatation of International Dermatology Education, Forte Biosciences, Foundation for Research and Education in Dermatology, Galderma, Helsinn, Incyte, LEO Pharma, Meiji Seika Pharma, Mindera, Pfizer, Seanergy, Strata, Trevi, and Verrica. Irina Pivneva, Roksana Ghanbariamin, and Min Yang are employees of Analysis Group, Inc., which has received consultancy fees from AbbVie. Ahmed M. Soliman and Bang Truong are full-time employees of AbbVie and may hold AbbVie stocks, stock options, or patents.
Ethical Approval
This study was conducted in accordance with ethical principles that have their origin in the current Declaration of Helsinki and was consistent with International Conference on Harmonization Good Clinical Practice, Good Epidemiology Practices, and applicable regulatory requirements. This study utilized de-identified data from electronic health records, so no ethics committee approval was required.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pinter, A., Soliman, A.M., Pivneva, I. et al. Real-World Long-Term Effectiveness of Risankizumab Among Patients with Moderate-to-Severe Psoriasis: Analysis from an International Medical Chart Review (RAPID) Study. Dermatol Ther (Heidelb) 14, 1259–1271 (2024). https://doi.org/10.1007/s13555-024-01164-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01164-6